Abstract
Curcumin, the major constituent of Curcuma longa L. (Zingiberaceae family) or turmeric, commonly used for cooking in Asian cuisine, is known to possess a broad range of pharmacological properties at relatively nontoxic doses. Curcumin is found to be effective against Staphylococcus aureus (S. aureus). As demonstrated by in vitro experiment, curcumin exerts even more potent effects when used in combination with various other antibacterial agents. Hence, curcumin which is a natural product derived from plant is believed to have profound medicinal benefits and could be potentially developed into a naturally derived antibiotic in the future. However, there are several noteworthy challenges in the development of curcumin as a medicine. S. aureus infections, particularly those caused by the multidrug-resistant strains, have emerged as a global health issue and urgent action is needed. This review focuses on the antibacterial activities of curcumin against both methicillin-sensitive S. aureus (MSSA) and methicillin-resistant S. aureus (MRSA). We also attempt to highlight the potential challenges in the effort of developing curcumin into a therapeutic antibacterial agent.
1. Introduction
Curcumin or diferuloylmethane is the major phytochemical of Curcuma longa L. (Zingiberaceae family), which is commonly known as turmeric. Curcumin is the polyphenolic compound that gives the yellow colour of the herb. Turmeric is mainly cultivated in tropical and subtropical regions and is mainly produced by India. Traditionally, it has been used to flavour food, dye cloths, and treat various human ailments [1]. Curcumin is extracted from turmeric by solvent extraction (preferably with ethanol) through various methods (e.g., Soxhlet, ultrasonic, microwave, and supercritical carbon dioxide) followed by purification via column chromatography [2, 3]. Ever since the identification of curcumin as the main constituent of turmeric, multiple pharmacological activities of curcumin that include antimicrobial, antidiabetic, anti-inflammatory, anticancer, and antioxidant have been reported [4–6]. More excitingly, when combined with other drugs, curcumin has been found to enhance the effects of antibacterial [7–9], antifungal [10, 11], anticancer [12, 13], and antioxidant [14, 15] activities.
Curcumin usually exhibits low to no toxicity at the active doses. A systematic review from the MEDLINE computerized database (1966 to 2002) has shown that curcumin is safe when consumed up to 8 g each day consecutively for 3 months in a phase I human trial that involved 25 subjects [16]. Similarly, the dose of 8 g per day was safe when used in combination with gemcitabine that showed marked therapeutic effects in pancreatic cancer patients [17, 18]. Interestingly, curcumin is also able to reverse the Aflatoxin B1-induced toxicity and iron-overloaded liver toxicity in rats [19–21]. Despite being extensively studied, the exact mechanism(s) of curcumin's multiple biological and pharmacological activities remains to be explored. Based on the available literature, there are two hypotheses describing the poly-pharmacological effects of curcumin. First, curcumin is known to act on multiple targets [4, 5, 22–24], hence having diverse roles in regulating various cellular processes. Secondly, products resulting from the curcumin degradation have been shown to be highly diverse depending on the chemical or biochemical reactions involved [25–27]. Most of these products are stable and function differently that may lead to the multiple effects.
The most studied activity of the curcumin in the past 10 years is the anticancer effects [28]. However, the first paper describing the biological action of curcumin was its antibacterial activity against various bacteria: S. aureus, Trichophyton gypseum, Salmonella paratyphi, and Mycobacterium tuberculosis [29]. To date, studies on the antibacterial activity of curcumin that indicate inhibition properties of a wide range of bacteria are increasingly documented [6, 23, 30]. Recent publications have also reported that curcumin is active against a plethora of drug-resistant bacterial strains [8, 9, 31, 32]. S. aureus infection is a major problem in many developing countries, especially in hospitals where the MRSA spreading is difficult to control [33]. Over the years, the multidrug-resistant S. aureus infection has increased the global morbidity and mortality [34, 35]. Due to the difficulty in treating the infection, it has consequently imposed an elevating burden on healthcare resources [36–38]. Cumulative findings in recent years have shown that curcumin is active against both MSSA and MRSA [8, 9, 30, 32, 39, 40]. In view of the need for a more efficacious and safe therapeutic modality towards the drug-resistant S. aureus, we discuss the reported antibacterial activities of curcumin against S. aureus and its potentials and limitations to be developed into a potent antibiotic.
2. Curcumin-Mediated Inhibition of S. aureus
Curcumin inhibits the growth of both Gram-positive and Gram-negative bacteria [6, 23, 30]. S. aureus is one of the Gram-positive strains that is susceptible to curcumin-mediated inhibition. S. aureus is a pathogen that causes various infections including infective endocarditis (IE), bacteremia, skin and soft tissue, osteoarticular, and pleuropulmonary infections [33]. Over the years, S. aureus has evolved and developed multiple strategies to evade human immune system and to resist antibiotics treatment. This has given rise to the evolution of MRSA, and the emergence of healthcare-associated (HA) and community-associated (CA) MRSA has caused a major problem to the human society [45, 46]. In this section, we discuss the past and current works that show the curcumin-mediated killings of MSSA and MRSA (summarized in Table 1).
Table 1.
Antibacterial activity of curcumin against S. aureus.
| Compound (solvent) | MIC (µg/mL) | S. aureus strain | Test method | Reference |
|---|---|---|---|---|
| Curcumin (DMSO) | 187.5 | MSSA (ATCC 25923) | Broth macrodilution | [42] |
| Indium curcumin (DMSO) | 93.8 | |||
|
| ||||
| Curcumin (DMSO) | 125–250 | MSSA (ATCC 25923) MRSA (ATCC 33591) MRSA (4 Clinical isolates) MRSA (4 from CCARM)# |
Broth microdilution | [9] |
|
| ||||
| Curcumin-1 (DMSO) | 250 | MSSA (MTCC 902)∗ | Broth microdilution | [41] |
|
| ||||
| Curcumin (DMF) | 250 | MSSA (ATCC 25923) MRSA (ATCC 43300) MSSA (1 Clinical isolates) MSSA (10 Env. isolates) |
Broth microdilution | [8] |
|
| ||||
| Curcumin-1 (DMSO) | 18.42 | MSSA (ATCC 29213) | Colony counting method | [30] |
|
| ||||
| Curcumin (ethanol) | 219 | MSSA (ATCC 29213) | Broth macrodilution | [47] |
| 217 | MRSA (ATCC 43300) | |||
|
| ||||
| Curcumin (ethanol) | 125 | MSSA (ATCC 25923) | Broth macrodilution | [49] |
|
| ||||
| Curcumin (DMSO) | 256 | MSSA (USA 300) MSSA (8325-4) |
Broth microdilution | [40] |
#CCARM: culture collection of antimicrobial resistant microbes.
∗Purchased from Microbial Type Culture Collection Centre (MTCC), IMTECH, Chandigarh, India.
Env.: environmental.
Mun et al. [9] showed that the minimal inhibitory concentrations (MICs) of curcumin against 10 strains of S. aureus (including 2 ATCC MSSA and MRSA standard strains, 4 MRSA clinical isolates, and 4 MRSA from culture collection) ranged from 125 to 250 μg/mL while a study by Wang et al. [40] showed the MIC of 256 μg/mL against MSSA. Using a broth microdilution assay, our group [8] also showed that 250 μg/mL curcumin was required to kill the two ATCC MSSA (#25923) and MRSA (#43300) strains. However, another study demonstrated that the MICs against the ATCC standard MSSA and MRSA were 219 and 217 μg/mL, respectively, that are slightly lower than the former study [47]. Recently, Kali et al. [48] showed the mean curcumin MIC of 126.9 μg/mL against 15 Gram-positive bacterial isolates including thirteen S. aureus and two Enterococcus faecalis. Nonetheless, this study is not used for comparison in Table 1 because the obtained MIC might not be representative for curcumin's effect against S. aureus as the study was carried out in combination with Enterococcus faecalis.
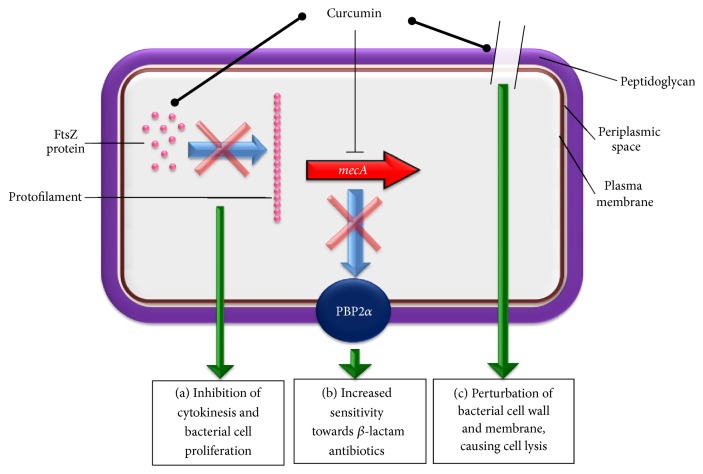
A more potent inhibition was achieved when curcumin-1 (CUR-1), a major component of commercial preparations of curcumin (purity > 98%), was used against S. aureus. The chemical structure of curcumin-1 is shown in Figure 1. Tyagi et al. [30] showed that the curcumin-1 was active against MSSA at concentration of as low as 25 μM (equivalent to 9.21 μg/mL), as it killed 50% of the bacteria after 2 hr incubation. The activity was time- and dose-dependent, and 100% killing was achieved at 50 μM (equivalent to 18.42 μg/mL) after 2 hr exposure [30]. In contrast, Sasidharan et al. [41] showed that the same compound had a MIC of 250 μg/mL against S. aureus, which is comparable to the native curcumin [8, 9]. In an in vivo mouse model, administration of 100 mg/kg curcumin was shown to protect the mice infected with both MSSA and MRSA from pneumonia by targeting the α-hemolysin (HIa) protein of S. aureus [40]. In summary, the curcumin MICs against S. aureus ranged from 18.42 to 256 μg/mL (refer to Table 1). The variation could be due to (i) strain difference (i.e., MRSA versus MSSA); (ii) source of bacterial strains (i.e., ATCC standard strains versus clinical isolates); (iii) type of antibacterial assay (i.e., disk diffusion versus broth microdilution); and (iv) type of curcumin and its solvent (i.e., commercial compound versus in-house purified compound). Overall, the cumulative findings showed that there is no difference of MICs against MSSA and MRSA, suggesting that the sensitivity towards curcumin treatment is not altered by the multidrug resistance machinery in S. aureus.
Figure 1.
Chemical structures of antibacterial curcumin analogues against S. aureus. Upper panel shows the structure of curcumin-1 [30, 41] while the lower panel shows the metal complexes of curcumin, indium curcumin [42, 43]. The chemical structures above were drawn using a free online tool, ChemWriter (http://chemwriter.com/).
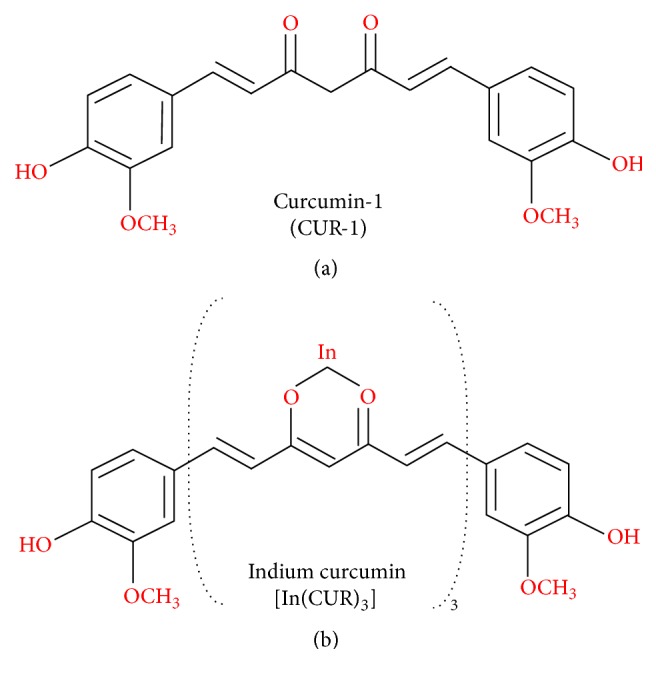
There have been several explanations on how curcumin acts and kills the bacteria which are illustrated in Figure 2. Rai et al. [44] have demonstrated that curcumin interacts with FtsZ (prokaryotic homologue of eukaryotic cytoskeletal protein tubulin) in vitro and inhibits the assembly of FtsZ protofilaments in Bacillus subtilis 168. Although it has not been examined directly on S. aureus, it is believed that inhibiting the assembly dynamics of FtsZ is one of the main mechanisms of curcumin in inhibiting bacterial cell proliferation. FtsZ is also believed to be a novel target for the development of antibacterial drugs against S. aureus. [63, 64]. Mun et al. [32] showed that the antibacterial action of curcumin against both MSSA and MRSA was markedly enhanced when used in combination with ATPase inhibitors and mild detergents that compromise ATP-binding cassette (ABC) transporters and cytoplasmic membrane integrity, respectively. The same study has also shown that curcumin binds to peptidoglycan (PGN), and the increasing concentrations of PGN block the curcumin antibacterial activity. Tyagi et al. [30] also showed that curcumin-1 inhibited S. aureus growth by perturbing the bacterial membrane integrity. In this study, the bacterial membrane of S. aureus was examined using two fluorescent probes: propidium iodide and calcein. The membrane leakage upon exposure to curcumin was also evaluated by fluorescence and scanning electron microscopies. Although existing evidence suggests that curcumin inhibits S. aureus mainly by damaging the bacterial membrane, further investigation is required to identify additional bacterial target proteins besides FtsZ and PGN. This is important not only to enhance the understanding of the curcumin interaction with its target proteins, but also to further improve the activity of curcumin against S. aureus, particularly the MRSA strains. Similar studies should also be performed on the curcumin derivatives such as curcumin-1 (curcumin with highest purity >98%) and indium curcumin (metal complex with curcumin) which have shown more potent antibacterial effects than the native curcumin. The chemical structures of curcumin-1 and indium curcumin are shown in Figure 1.
Figure 2.
The potential mechanisms underlying the antibacterial effect of curcumin against S. aureus. Circle-shaped arrow indicates binding whereas blocked arrow represents inhibition. (a) Curcumin may bind into FtsZ proteins, thereby inhibiting the assembly of FtsZ protofilaments. This, in turn, suppresses the formation of Z-ring leading to inhibition of cytokinesis and bacterial proliferation [44]. (b) In the case of MRSA, curcumin could inhibit the mecA gene transcription, causing reduced expression of PBP2α proteins. As a result, MRSA can be sensitized towards the antibacterial action of β-lactam antibiotics such as Penicillin and Methicillin [32]. (c) The binding between curcumin and peptidoglycan on S. aureus cell wall could trigger damage on the cell wall and membrane, leading to cell lysis of S. aureus [30, 32].
3. Synergism of Curcumin with Antibiotics against S. aureus
In addition to showing potent antibacterial activity when used alone, curcumin also exerts marked activity against S. aureus when used at subinhibitory dose in combination with various other antibiotics [8, 9, 31, 32]. These findings are interesting since curcumin is naturally derived from turmeric, which is one of the major ingredients of Asian cuisine [1, 23]. Of note, crude turmeric extracts have previously shown marked antibacterial activities against S. aureus [6, 65, 66]. This section discusses the synergistic antibacterial activity of curcumin with antibiotics against MSSA and MRSA. Table 2 summarizes studies that demonstrated the synergism of antibiotics-curcumin. In this table, we include the information of curcumin type, solvent, and concentration, type of bacteria-killing assay, and S. aureus strains for comparison.
Table 2.
Synergism of curcumin against S. aureus.
| Compound (solvent) | Subinhibitory concentration | Antibiotics | S. aureus strain | Test method | Reference |
|---|---|---|---|---|---|
| Curcumin (not reported) | 500 µg/disc | Cefixime Cephotaxime Vancomycin Tetracycline |
MSSA (1 clinical isolate) | Disk diffusion | [31] |
|
| |||||
| Curcumin (DMSO) | Checkerboard (various serial dilutions) | Oxacillin Ampicillin Ciprofloxacin Norfloxacin |
MSSA (ATCC 25923) MRSA (ATCC 33591) MRSA (1 clinical isolate) |
Broth microdilution | [9] |
|
| |||||
| Curcumin-1 (DMSO) | Checkerboard (various serial dilutions) | Cefaclor Cefodizime Cefotaxime |
MSSA (MTCC 902)∗ | Broth microdilution | [41] |
|
| |||||
| Curcumin (DMF) | 25 µg/mL | Gentamicin Amikacin Ciprofloxacin |
MSSA (ATCC 25923) MRSA (ATCC 43300) MSSA (1 clinical isolate) MSSA (10 environ. isolates) |
Disk diffusion & broth microdilution | [8] |
|
| |||||
| Curcumin (DMSO) | 32 µg/mL | Penicillin Erythromycin Ciprofloxacin |
MSSA (ATCC 25923) MSSA (13 clinical isolates) |
Disk diffusion | [48] |
∗Purchased from Microbial Type Culture Collection Centre (MTCC), IMTECH, Chandigarh, India.
The first study that reported the synergism of curcumin against S. aureus was seven years ago by Moghaddam et al. [31]. Using a disk diffusion method, Moghaddam et al. [31] showed that 500 μg/disc of curcumin exerted synergistic antibacterial effect on the MSSA when used in combination with four antibiotics. Combination with cefotaxime, cefixime, tetracycline, and vancomycin resulted in increase of inhibition zone of 52.6, 24.9, 26.5, and 24.4%, respectively. This was then followed by Mun et al. [9] study in 2013 that showed curcumin's synergism with Oxacillin, Ampicillin, Ciprofloxacin, and Norfloxacin against the MRSA. This study employed checkerboard broth microdilution assay method to determine the synergistic activity. This method allows more standardised testing and is less laborious and suitable for studies with multiple concentrations of test compounds [67]. Other studies also showed the synergistic antibacterial effect of curcumin against both MSSA and MRSA when used in combination with antibiotics such as Cefaclor, Cefodizime, Cefotaxime, Gentamicin, Amikacin, Penicillin, and Erythromycin (refer to Table 2). Based on reported findings, the curcumin synergism in combination with antibiotics appears to be relatively nonspecific. Antibiotics classes that have shown synergism with curcumin include β-lactams, Cephalosporins, Aminoglycosides, Glycopeptides, Tetracyclines, and Fluoroquinolones. This might due to the multitargeting action of curcumin or their undetermined breakdown products as pointed out in the previous section. More studies are needed to evaluate the mechanism of curcumin synergism based on the different classes of antibiotics. In addition to antibacterial action, curcumin also reverses the drug resistance when used in combination with other anticancer agents such as cisplatin, 5-fluorouracil, oxaliplatin, and doxorubicin in multiple types of cancer cells including breast [68], colon [69], head and neck [70], and ovary [71]. The curcumin may have acted on the target or pathway related to the development of drug resistance, hence restoring the killing effect of the drugs [72, 73]. This may be one of the mechanisms on how curcumin enhances the effect of antibacterial drugs, especially when they are targeting S. aureus-infected human cells.
In recent years, MRSA infection has emerged as a serious infection due to its multidrug resistance (MDR) especially in the hospital setting [74]. The MRSA infection may spread rapidly especially when the disease is not well controlled. Curcumin exhibits potent activity against MRSA, not only when used alone, but also in combination with other antibiotics. In an effort to understand the curcumin's anti-MRSA effect, Mun et al. [32] showed that the Tris and Triton X-100 inhibited the bacterial growth to 63% and 59%, respectively, when used together with curcumin. This suggests that bacterial membrane permeability is partly responsible in regulating the antibacterial efficacy of curcumin against MRSA. The same group has also shown that ATPase inhibitors (DCCD and NaN3) which block the ATP-binding cassette (ABC) enhanced the MRSA killing when used together with curcumin. The importance of membrane permeability/integrity in curcumin effect was also confirmed when the increase of peptidoglycan (PGN) concentration successively blocked the curcumin antibacterial activity [32]. These findings suggest that any drug or inhibitor that primarily acts on the bacterial membrane has higher chance of showing enhanced activity when used together with curcumin. It is also noteworthy that the expression of Penicillin-binding protein 2α (PBP2α), a protein responsible in conferring resistance towards β-lactam antibiotics, was downregulated in MRSA upon curcumin treatment [32]. This protein which is encoded by MecA, a nonnative gene in MRSA has significantly reduced affinity for β-lactam antibiotics such as Methicillin and Penicillin. Cell-wall biosynthesis, the target of β-lactam, could therefore carry on in MRSA despite the presence of potent doses of these antibiotics [75]. The detailed mode of action of curcumin in inhibiting PBP2α expression in MRSA is not clear at this juncture. It is plausible that curcumin may act on the transcription of MecA gene, thereby blocking the expression of PBP2α protein (Figure 2).
In addition to antibiotics, there are evidences showing that curcumin augments the activity of other natural compounds against MSSA and MRSA. Balan et al. [76] demonstrated that combination of curcumin and whey proteins markedly inhibited S. aureus growth in vitro. Sharma et al. [77] have also previously reported the combination effect of curcumin with several phytochemicals such as cinnamaldehyde, ellagic acid, and eugenol against Staphylococcus epidermidis (S. epidermidis), which is closely related to S. aureus. The combination activities as such against S. aureus remain to be investigated. Indeed, there have been many studies showing the potent antibacterial action of other natural compounds against S. aureus such as thymoquinone [78], rhein [79], emodin [80], silibinin [81], osthol [82], tannic acid [83], and epigallocatechin gallate [84]. These findings warrant the potential use of abovementioned compounds in combination with curcumin against S. aureus.
4. The Challenges of Using Curcumin as Antibiotic
Cumulative findings suggest that curcumin has broad-spectrum antibacterial activities and has synergistic effects with other antibiotics in combination therapies in vitro [1, 6, 85]. Curcumin has also shown potent antibacterial action in the mouse model [40]. Nonetheless, the curcumin antibacterial activity has never been evaluated in clinical trials with an aim of using it as a future antibiotic. In this section, we discuss the underlying challenges from the clinical perspectives in developing curcumin into a potential antibiotic.
While curcumin is known to possess the pharmacological activities at relatively low doses, several studies have evidenced some cytotoxicity of curcumin [50–54, 86]. The first study that demonstrated the curcumin toxicity was by Goodpasture and Arrighi [50]. They showed that turmeric resulted in an induction of chromosome aberrations in tested cell lines starting from 10 μg/mL. Other studies have also shown the toxic effects of curcumin mainly on the DNA damage and chromosome aberrations [51–53]. While DNA alteration is the starting point of carcinogenesis, the use of curcumin under abovementioned conditions might be an issue. In other words, curcumin treatment may cause cancers even though the anticancer action of curcumin is well documented. In 1993, a study has concluded that turmeric oleoresin (turmeric extract containing 79–85% of curcumin) has carcinogenic property in rats and mice [54]. Mice taking 0.2 mg/kg body weight of curcumin daily average were found to have carcinomas in their small intestines. Curcumin has also shown to promote lung cancer in another study [55]. The tumour-promoting activity of curcumin has been linked to the induction of reactive oxygen species (ROS) production such as superoxide anion and hydrogen peroxide [87–89].
As curcumin is an active iron chelator, it may potentially affect systemic iron metabolism especially those who have suboptimal iron status [56]. Furthermore, curcumin has been reported to block the enzymes that metabolize drugs such as cytochrome P450s [57, 58]. This may lead to the accumulation of nonmetabolized drugs in blood and result in undesired toxicity. In human, nonetheless, the side effects of curcumin have been relatively mild. A human trial has shown that curcumin ranging from 0.9 to 3.6 g per day up to 4 months only caused some adverse effects that included nausea, diarrhea, and increased serum alkaline phosphatase and lactate dehydrogenase [90]. In 2010, Balaji and Chempakam [91] have predicted a few toxigenic and potent compounds from turmeric using a cost-effective cheminformatics approach. This method can be adopted to select the effective but nontoxic curcumin or its derivatives for further biological studies. However, the selected compound has to be evaluated in a long-term study at its active dose against S. aureus in order to confirm the safety of using curcumin as a potential antibiotic.
Curcumin is usually extracted from turmeric plant mainly by solvent extraction followed by column-based purification [2, 3]. Curcumin is sparingly soluble in water (<0.1 mg/mL) and is mainly dissolved in organic solvents such as DMSO, DMF, or ethanol (Tables 1 and 2). This may be the major concern when it is administered into human system as human plasma is composed of 92% of water. The water-insoluble nature may affect curcumin bioavailability and hence affect its pharmacological potential [26, 27, 61]. To this end, several methods have been developed in recent years to circumvent the poor solubility and stability of curcumin, thereby maximizing its pharmacological or biological actions. For example, it has been reported that the use of heat could enhance the curcumin solubility [59, 60]. Kurien et al. [59] have reported the improved water solubility of curcumin from 0.6 to 7.4 μg/mL, without displaying heat-mediated destruction of the chemical structure. Development of curcumin bioconjugates has also shown to be an effective method of enhancing the curcumin solubility. For instances, conjugation of curcumin with hyaluronic acid formed micelles in aqueous phase at physiological pH and appeared to be nontoxic [92]. Dey and Sreenivasan have also conjugated curcumin with alginate, a natural polysaccharide product, in order to increase its stability and bioavailability [93]. Other macromolecules that could serve as carrier systems for curcumin include beta-casein [94], chitosan/Tween 20 [95], emulsomes [96], sodium caseinate [97], and albumin [98, 99]. The development of curcumin nanoformulations has been extensively reviewed in light of its anticancer action [100–102]. While increasing number of curcumin nanoformulation is being introduced into the therapeutic field, it is important to ensure that the bioconjugates or nanoformulations do not diminish the antibacterial effects of curcumin at the expense of improved bioavailability in order to develop them into effective antibiotics in the future.
In addition to potential toxicity, poor solubility, and low bioavailability, curcumin encounters multiple challenges when it is administered either through oral or intravenous route due to the nature of body system [26, 59, 61, 62]. A large amount of curcumin may get degraded in the presence of detoxifying and metabolic enzymes, or it may bind to the circulatory proteins such as albumin which may potentially reduce its activity. Contradictorily, there have been evidences showing that degraded products from curcumin are responsible of its pharmacological activities [26, 27]. Furthermore, it has been shown that albumin-bound curcumin exerted similar level of activity compared to the DMSO-dissolved curcumin in serum [103]. Of note, the curcumin degradation and binding with physiological proteins have not been evaluated in light of the curcumin antibacterial action. Whether or not these factors would affect the activity of curcumin, further investigations are required. Notably, development of the curcumin bioconjugates, nanoformulations, or derivatives could be the key to overcome the challenges mentioned above (summarized in Table 3). The development of modified curcumin has been recently reviewed [62, 100, 101].
Table 3.
Challenges of curcumin use in clinical setting.
| Challenge | References |
|---|---|
| Cytotoxicity | |
| DNA damage and chromosome aberrations | [50–53] |
| Carcinogenesis | |
| Promote tumour formation in vivo | [54, 55] |
| Iron chelation | |
| Alter systemic iron metabolism | [56] |
| Enzyme inhibition | |
| Inhibit drug-metabolizing enzymes | [57, 58] |
| Solubility | |
| Hydrophobic nature does not support water solubility | [59, 60] |
| Bioavailability | |
| Degradation by plasma protease and nonspecific protein binding | [26, 27, 61, 62] |
5. Conclusion
Curcumin has shown potent antibacterial activity and other pharmacological actions in the past 50 years. Curcumin has been marketed globally as a health supplement mainly for its antioxidant and anti-inflammatory properties. In addition, it also has high potential to be developed into an antibiotic against S. aureus and other bacterial strains in the future. However, the challenges mentioned in the preceding sections should be taken into consideration to open the door for the development of more biologically active curcumin derivatives. To the best of our understanding, this is the first review that compares and summarizes the curcumin antibacterial activity against S. aureus. More investigation is required in order to better understand the broad action of curcumin prior to develop this compound or its derivatives into a potential antibiotic.
Acknowledgments
The authors would like to thank the Director General of Health Malaysia for permission to publish this study and the Director of the Institute for Medical Research for her support.
Competing Interests
The authors declared that there are no competing interests.
References
- 1.Goel A., Kunnumakkara A. B., Aggarwal B. B. Curcumin as ‘Curecumin’: from kitchen to clinic. Biochemical Pharmacology. 2008;75(4):787–809. doi: 10.1016/j.bcp.2007.08.016. [DOI] [PubMed] [Google Scholar]
- 2.Li M., Ngadi M. O., Ma Y. Optimisation of pulsed ultrasonic and microwave-assisted extraction for curcuminoids by response surface methodology and kinetic study. Food Chemistry. 2014;165:29–34. doi: 10.1016/j.foodchem.2014.03.115. [DOI] [PubMed] [Google Scholar]
- 3.Priyadarsini K. I. The chemistry of curcumin: from extraction to therapeutic agent. Molecules. 2014;19(12):20091–20112. doi: 10.3390/molecules191220091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gupta S. C., Prasad S., Kim J. H., et al. Multitargeting by curcumin as revealed by molecular interaction studies. Natural Product Reports. 2011;28(12):1937–1955. doi: 10.1039/c1np00051a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maheshwari R. K., Singh A. K., Gaddipati J., Srimal R. C. Multiple biological activities of curcumin: a short review. Life Sciences. 2006;78(18):2081–2087. doi: 10.1016/j.lfs.2005.12.007. [DOI] [PubMed] [Google Scholar]
- 6.Moghadamtousi S. Z., Kadir H. A., Hassandarvish P., Tajik H., Abubakar S., Zandi K. A review on antibacterial, antiviral, and antifungal activity of curcumin. BioMed Research International. 2014;2014:12. doi: 10.1155/2014/186864.186864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bansal S., Chhibber S. Curcumin alone and in combination with augmentin protects against pulmonary inflammation and acute lung injury generated during Klebsiella pneumoniae B5055-induced lung infection in BALB/c mice. Journal of Medical Microbiology. 2010;59(4):429–437. doi: 10.1099/jmm.0.016873-0. [DOI] [PubMed] [Google Scholar]
- 8.Teow S.-Y., Ali S. A. Synergistic antibacterial activity of curcumin with antibiotics against Staphylococcus aureus . Pakistan Journal of Pharmaceutical Sciences. 2015;28(6):2109–2114. [PubMed] [Google Scholar]
- 9.Mun S.-H., Joung D.-K., Kim Y.-S., et al. Synergistic antibacterial effect of curcumin against methicillin-resistant Staphylococcus aureus . Phytomedicine. 2013;20(8-9):714–718. doi: 10.1016/j.phymed.2013.02.006. [DOI] [PubMed] [Google Scholar]
- 10.Garcia-Gomes A. S., Curvelo J. A. R., Soares R. M. A., Ferreira-Pereira A. Curcumin acts synergistically with fluconazole to sensitize a clinical isolate of Candida albicans showing a MDR phenotype. Medical Mycology. 2012;50(1):26–32. doi: 10.3109/13693786.2011.578156. [DOI] [PubMed] [Google Scholar]
- 11.Sharma M., Manoharlal R., Negi A. S., Prasad R. Synergistic anticandidal activity of pure polyphenol curcumin i in combination with azoles and polyenes generates reactive oxygen species leading to apoptosis. FEMS Yeast Research. 2010;10(5):570–578. doi: 10.1111/j.1567-1364.2010.00637.x. [DOI] [PubMed] [Google Scholar]
- 12.Patel B. B., Majumdar A. P. N. Synergistic role of curcumin with current therapeutics in colorectal cancer: minireview. Nutrition and Cancer. 2009;61(6):842–846. doi: 10.1080/01635580903285106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boztas A. O., Karakuzu O., Galante G., et al. Synergistic interaction of paclitaxel and curcumin with cyclodextrin polymer complexation in human cancer cells. Molecular Pharmaceutics. 2013;10(7):2676–2683. doi: 10.1021/mp400101k. [DOI] [PubMed] [Google Scholar]
- 14.Aftab N., Vieira A. Antioxidant activities of curcumin and combinations of this curcuminoid with other phytochemicals. Phytotherapy Research. 2010;24(4):500–502. doi: 10.1002/ptr.2960. [DOI] [PubMed] [Google Scholar]
- 15.Naksuriya O., Okonogi S. Comparison and combination effects on antioxidant power of curcumin with gallic acid, ascorbic acid, and xanthone. Drug Discoveries and Therapeutics. 2015;9(2):136–141. doi: 10.5582/ddt.2015.01013. [DOI] [PubMed] [Google Scholar]
- 16.Chainani-Wu N. Safety and anti-inflammatory activity of curcumin: a component of tumeric (Curcuma longa) Journal of Alternative and Complementary Medicine. 2003;9(1):161–168. doi: 10.1089/107555303321223035. [DOI] [PubMed] [Google Scholar]
- 17.Kanai M., Yoshimura K., Asada M., et al. A phase I/II study of gemcitabine-based chemotherapy plus curcumin for patients with gemcitabine-resistant pancreatic cancer. Cancer Chemotherapy and Pharmacology. 2011;68(1):157–164. doi: 10.1007/s00280-010-1470-2. [DOI] [PubMed] [Google Scholar]
- 18.Dhillon N., Aggarwal B. B., Newman R. A., et al. Phase II trial of curcumin in patients with advanced pancreatic cancer. Clinical Cancer Research. 2008;14(14):4491–4499. doi: 10.1158/1078-0432.ccr-08-0024. [DOI] [PubMed] [Google Scholar]
- 19.Poapolathep S., Imsilp K., Machii K., Kumagai S., Poapolathep A. The effects of curcumin on aflatoxin B1- induced toxicity in rats. Biocontrol Science. 2015;20(3):171–177. doi: 10.4265/bio.20.171. [DOI] [PubMed] [Google Scholar]
- 20.Messner D. J., Sivam G., Kowdley K. V. Curcumin reduces the toxic effects of iron loading in rat liver epithelial cells. Liver International. 2009;29(1):63–72. doi: 10.1111/j.1478-3231.2008.01793.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Badria F. A., Ibrahim A. S., Badria A. F., Elmarakby A. A. Curcumin attenuates iron accumulation and oxidative stress in the liver and spleen of chronic iron-overloaded rats. PLoS ONE. 2015;10(7) doi: 10.1371/journal.pone.0134156.e0134156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Teiten M.-H., Eifes S., Dicato M., Diederich M. Curcumin-the paradigm of a multi-target natural compound with applications in cancer prevention and treatment. Toxins. 2010;2(1):128–162. doi: 10.3390/toxins2010128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gupta S. C., Patchva S., Koh W., Aggarwal B. B. Discovery of curcumin, a component of golden spice, and its miraculous biological activities. Clinical and Experimental Pharmacology and Physiology. 2012;39(3):283–299. doi: 10.1111/j.1440-1681.2011.05648.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhou H., Beevers C. S., Huang S. The targets of curcumin. Current Drug Targets. 2011;12(3):332–347. doi: 10.2174/138945011794815356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schneider C., Gordon O. N., Edwards R. L., Luis P. B. Degradation of curcumin: from mechanism to biological implications. Journal of Agricultural and Food Chemistry. 2015;63(35):7606–7614. doi: 10.1021/acs.jafc.5b00244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shen L., Ji H.-F. The pharmacology of curcumin: Is it the degradation products? Trends in Molecular Medicine. 2012;18(3):138–144. doi: 10.1016/j.molmed.2012.01.004. [DOI] [PubMed] [Google Scholar]
- 27.Shen L., Liu C.-C., An C.-Y., Ji H.-F. How does curcumin work with poor bioavailability? Clues from experimental and theoretical studies. Scientific Reports. 2016;6 doi: 10.1038/srep20872.20872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ghosh D., Bagchi D., Konishi T. Clinical Aspects of Functional Foods and Nutraceuticals. CRC Press/Taylor and Francis Group; 2014. [DOI] [Google Scholar]
- 29.Schraufstätter E., Bernt H. Antibacterial action of curcumin and related compounds. Nature. 1949;164(4167):456–457. doi: 10.1038/164456a0. [DOI] [PubMed] [Google Scholar]
- 30.Tyagi P., Singh M., Kumari H., Kumari A., Mukhopadhyay K. Bactericidal activity of curcumin I is associated with damaging of bacterial membrane. PLoS ONE. 2015;10(3) doi: 10.1371/journal.pone.0121313.e0121313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moghaddam K., Iranshahi M., Yazdi M., Shahverdi A. The combination effect of curcumin with different antibiotics against Staphylococcus aureus. International Journal of Green Pharmacy. 2009;3(2):141–143. doi: 10.4103/0973-8258.54906. [DOI] [Google Scholar]
- 32.Mun S.-H., Kim S.-B., Kong R., et al. Curcumin reverse methicillin resistance in Staphylococcus aureus . Molecules. 2014;19(11):18283–18295. doi: 10.3390/molecules191118283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tong S. Y. C., Davis J. S., Eichenberger E., Holland T. L., Fowler V. G. Staphylococcus aureus infections: epidemiology, pathophysiology, clinical manifestations, and management. Clinical Microbiology Reviews. 2015;28(3):603–661. doi: 10.1128/cmr.00134-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Boucher H. W., Corey G. R. Epidemiology of methicillin-resistant Staphylococcus aureus . Clinical Infectious Diseases. 2008;46(supplement 5):S344–S349. doi: 10.1086/533590. [DOI] [PubMed] [Google Scholar]
- 35.Klein E., Smith D. L., Laxminarayan R. Hospitalizations and deaths caused by methicillin-resistant Staphylococcus aureus, United States, 1999-2005. Emerging Infectious Diseases. 2007;13(12):1840–1846. doi: 10.3201/eid1312.070629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tarai B., Das P., Kumar D. Recurrent challenges for clinicians: emergence of methicillin-resistant Staphylococcus aureus, vancomycin resistance, and current treatment options. Journal of Laboratory Physicians. 2013;5(2):71–78. doi: 10.4103/0974-2727.119843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ventola C. L. The antibiotic resistance crisis—part 1: causes and threats. Pharmacy and Therapeutics. 2015;40(4):277–283. [PMC free article] [PubMed] [Google Scholar]
- 38.Rasmussen R. V., Fowler V. G., Jr., Skov R., Bruun N. E. Future challenges and treatment of Staphylococcus aureus bacteremia with emphasis on MRSA. Future Microbiology. 2011;6(1):43–56. doi: 10.2217/fmb.10.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ribeiro A. P. D., Pavarina A. C., Dovigo L. N., et al. Phototoxic effect of curcumin on methicillin-resistant Staphylococcus aureus and L929 fibroblasts. Lasers in Medical Science. 2013;28(2):391–398. doi: 10.1007/s10103-012-1064-9. [DOI] [PubMed] [Google Scholar]
- 40.Wang J., Zhou X., Li W., Deng X., Deng Y., Niu X. Curcumin protects mice from Staphylococcus aureus pneumonia by interfering with the self-assembly process of α-hemolysin. Scientific Reports. 2016;6 doi: 10.1038/srep28254.28254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sasidharan N. K., Sreekala S. R., Jacob J., Nambisan B. In vitro synergistic effect of curcumin in combination with third generation cephalosporins against bacteria associated with infectious diarrhea. BioMed Research International. 2014;2014:8. doi: 10.1155/2014/561456.561456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tajbakhsh S., Mohammadi K., Deilami I., et al. Antibacterial activity of indium curcumin and indium diacetylcurcumin. African Journal of Biotechnology. 2008;7(21):3832–3835. [Google Scholar]
- 43.Mohammadi K., Thompson K. H., Patrick B. O., et al. Synthesis and characterization of dual function vanadyl, gallium and indium curcumin complexes for medicinal applications. Journal of Inorganic Biochemistry. 2005;99(11):2217–2225. doi: 10.1016/j.jinorgbio.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 44.Rai D., Singh J. K., Roy N., Panda D. Curcumin inhibits FtsZ assembly: an attractive mechanism for its antibacterial activity. Biochemical Journal. 2008;410(1):147–155. doi: 10.1042/bj20070891. [DOI] [PubMed] [Google Scholar]
- 45.Liu G. Y. Molecular pathogenesis of Staphylococcus aureus infection. Pediatric Research. 2009;65(5, part 2):71R–77R. doi: 10.1203/pdr.0b013e31819dc44d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Miller L. G., Kaplan S. L. Staphylococcus aureus: a community pathogen. Infectious Disease Clinics of North America. 2009;23(1):35–52. doi: 10.1016/j.idc.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 47.Gunes H., Gulen D., Mutlu R., Gumus A., Tas T., Topkaya A. E. Antibacterial effects of curcumin: an in vitro minimum inhibitory concentration study. Toxicology and Industrial Health. 2016;32(2):246–250. doi: 10.1177/0748233713498458. [DOI] [PubMed] [Google Scholar]
- 48.Kali A., Bhuvaneshwar D., Charles P. V., Seetha K. Antibacterial synergy of curcumin with antibiotics against biofilm producing clinical bacterial isolates. Journal of Basic and Clinical Pharmacy. 2016;7(3):93–96. doi: 10.4103/0976-0105.183265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sandikci Altunatmaz S., Yilmaz Aksu F., Issa G., Basaran Kahraman B., Dulger Altiner D., Buyukunal S. Antimicrobial effects of curcumin against L. monocytogenes, S. aureus, S. Typhimurium and E. coli O157 : H7 pathogens in minced meat. Veterinární Medicína. 2016;61(5):256–262. doi: 10.17221/8880-vetmed. [DOI] [Google Scholar]
- 50.Goodpasture C. E., Arrighi F. E. Effects of food seasonings on the cell cycle and chromosome morphology of mammalian cells in vitro with special reference to turmeric. Food and Cosmetics Toxicology. 1976;14(1):9–14. doi: 10.1016/S0015-6264(76)80356-2. [DOI] [PubMed] [Google Scholar]
- 51.Cao J., Jia L., Zhou H.-M., Liu Y., Zhong L.-F. Mitochondrial and nuclear DNA damage induced by curcumin in human hepatoma G2 cells. Toxicological Sciences. 2006;91(2):476–483. doi: 10.1093/toxsci/kfj153. [DOI] [PubMed] [Google Scholar]
- 52.Urbina-Cano P., Bobadilla-Morales L., Ramírez-Herrera M. A., et al. DNA damage in mouse lymphocytes exposed to curcumin and copper. Journal of Applied Genetics. 2006;47(4):377–382. doi: 10.1007/bf03194648. [DOI] [PubMed] [Google Scholar]
- 53.Verschoyle R. D., Steward W. P., Gescher A. J. Putative cancer chemopreventive agents of dietary origin-how safe are they? Nutrition and Cancer. 2007;59(2):152–162. doi: 10.1080/01635580701458186. [DOI] [PubMed] [Google Scholar]
- 54.National Toxicology Program. NTP toxicology and carcinogenesis studies of turmeric oleoresin (CAS No. 8024-37-1) (major component 79%-85% curcumin, CAS No. 458-37-7) in F344/N rats and B6C3F1 mice (feed studies) National Toxicology Program Technical Report Series. 1993;427:1–275. [PubMed] [Google Scholar]
- 55.Dance-Barnes S. T., Kock N. D., Moore J. E., et al. Lung tumor promotion by curcumin. Carcinogenesis. 2009;30(6):1016–1023. doi: 10.1093/carcin/bgp082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jiao Y., Wilkinson J., IV, Di X., et al. Curcumin, a cancer chemopreventive and chemotherapeutic agent, is a biologically active iron chelator. Blood. 2009;113(2):462–469. doi: 10.1182/blood-2008-05-155952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Appiah-Opong R., Commandeur J. N. M., van Vugt-Lussenburg B., Vermeulen N. P. E. Inhibition of human recombinant cytochrome P450s by curcumin and curcumin decomposition products. Toxicology. 2007;235(1-2):83–91. doi: 10.1016/j.tox.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 58.Thapliyal R., Maru G. B. Inhibition of cytochrome P450 isozymes by curcumins in vitro and in vivo . Food and Chemical Toxicology. 2001;39(6):541–547. doi: 10.1016/s0278-6915(00)00165-4. [DOI] [PubMed] [Google Scholar]
- 59.Kurien B. T., Singh A., Matsumoto H., Scofield R. H. Improving the solubility and pharmacological efficacy of curcumin by heat treatment. Assay and Drug Development Technologies. 2007;5(4):567–576. doi: 10.1089/adt.2007.064. [DOI] [PubMed] [Google Scholar]
- 60.Kurien B. T., Scofield R. H. Heat-solubilized curcumin should be considered in clinical trials for increasing bioavailability. Clinical Cancer Research. 2009;15(2):p. 747. doi: 10.1158/1078-0432.CCR-08-1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Anand P., Kunnumakkara A. B., Newman R. A., Aggarwal B. B. Bioavailability of curcumin: problems and promises. Molecular Pharmaceutics. 2007;4(6):807–818. doi: 10.1021/mp700113r. [DOI] [PubMed] [Google Scholar]
- 62.Prasad S., Tyagi A. K., Aggarwal B. B. Recent developments in delivery, bioavailability, absorption and metabolism of curcumin: the golden pigment from golden spice. Cancer Research and Treatment. 2014;46(1):2–18. doi: 10.4143/crt.2014.46.1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Matsui T., Yamane J., Mogi N., et al. Structural reorganization of the bacterial cell-division protein FtsZ from Staphylococcus aureus . Acta Crystallographica Section D: Biological Crystallography. 2012;68(9):1175–1188. doi: 10.1107/s0907444912022640. [DOI] [PubMed] [Google Scholar]
- 64.Singh P., Panda D. FtsZ inhibition: a promising approach for anti-staphylococcal therapy. Drug News and Perspectives. 2010;23(5):295–304. doi: 10.1358/dnp.2010.23.5.1429489. [DOI] [PubMed] [Google Scholar]
- 65.Gul P., Bakht J. Antimicrobial activity of turmeric extract and its potential use in food industry. Journal of Food Science and Technology. 2015;52(4):2272–2279. doi: 10.1007/s13197-013-1195-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gupta A., Mahajan S., Sharma R. Evaluation of antimicrobial activity of Curcuma longa rhizome extract against Staphylococcus aureus . Biotechnology Reports. 2015;6:51–55. doi: 10.1016/j.btre.2015.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Foweraker J. E., Laughton C. R., Brown D. F., Bilton D. Comparison of methods to test antibiotic combinations against heterogeneous populations of multiresistant Pseudomonas aeruginosa from patients with acute infective exacerbations in cystic fibrosis. Antimicrobial Agents and Chemotherapy. 2009;53(11):4809–4815. doi: 10.1128/aac.00269-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sen G. S., Mohanty S., Hossain D. M. S., et al. Curcumin enhances the efficacy of chemotherapy by tailoring p65NFκB-p300 cross-talk in favor of p53–p300 in breast cancer. The Journal of Biological Chemistry. 2011;286(49):42232–42247. doi: 10.1074/jbc.m111.262295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ruiz de Porras V., Bystrup S., Martínez-Cardús A., et al. Curcumin mediates oxaliplatin-acquired resistance reversion in colorectal cancer cell lines through modulation of CXC-Chemokine/NF-κB signalling pathway. Scientific Reports. 2016;6, article 24675 doi: 10.1038/srep24675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sivanantham B., Sethuraman S., Krishnan U. M. Combinatorial effects of curcumin with an anti-neoplastic agent on head and neck squamous cell carcinoma through the regulation of EGFR-ERK1/2 and apoptotic signaling pathways. ACS Combinatorial Science. 2016;18(1):22–35. doi: 10.1021/acscombsci.5b00043. [DOI] [PubMed] [Google Scholar]
- 71.Wahl H., Tan L., Griffith K., Choi M., Liu J. R. Curcumin enhances Apo2L/TRAIL-induced apoptosis in chemoresistant ovarian cancer cells. Gynecologic Oncology. 2007;105(1):104–112. doi: 10.1016/j.ygyno.2006.10.050. [DOI] [PubMed] [Google Scholar]
- 72.Saha S., Adhikary A., Bhattacharyya P., Das T., Sa G. Death by design: where curcumin sensitizes drug-resistant tumours. Anticancer Research. 2012;32(7):2567–2584. [PubMed] [Google Scholar]
- 73.Nabekura T. Overcoming multidrug resistance in human cancer cells by natural compounds. Toxins. 2010;2(6):1207–1224. doi: 10.3390/toxins2061207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Köck R., Becker K., Cookson B., et al. Methicillin-resistant Staphylococcus aureus (MRSA): burden of disease and control challenges in Europe. Euro Surveillance. 2010;15(41) doi: 10.2807/ese.15.41.19688-en.19688 [DOI] [PubMed] [Google Scholar]
- 75.Peacock S. J., Paterson G. K. Mechanisms of methicillin resistance in Staphylococcus aureus . Annual Review of Biochemistry. 2015;84:577–601. doi: 10.1146/annurev-biochem-060614-034516. [DOI] [PubMed] [Google Scholar]
- 76.Balan P., Mal G., Das S., Singh H. Synergistic and additive antimicrobial activities of curcumin, Manuka honey and whey proteins. Journal of Food Biochemistry. 2016;40(5):647–654. doi: 10.1111/jfbc.12249. [DOI] [Google Scholar]
- 77.Sharma G., Raturi K., Dang S., Gupta S., Gabrani R. Combinatorial antimicrobial effect of curcumin with selected phytochemicals on Staphylococcus epidermidis . Journal of Asian Natural Products Research. 2014;16(5):535–541. doi: 10.1080/10286020.2014.911289. [DOI] [PubMed] [Google Scholar]
- 78.Chaieb K., Kouidhi B., Jrah H., Mahdouani K., Bakhrouf A. Antibacterial activity of Thymoquinone, an active principle of Nigella sativa and its potency to prevent bacterial biofilm formation. BMC Complementary and Alternative Medicine. 2011;11, article 29 doi: 10.1186/1472-6882-11-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Joung D.-K., Joung H., Yang D.-W., et al. Synergistic effect of rhein in combination with ampicillin or oxacillin against methicillin-resistant Staphylococcus aureus. Experimental and Therapeutic Medicine. 2012;3(4):608–612. doi: 10.3892/etm.2012.459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lee Y.-S., Kang O.-H., Choi J.-G., et al. Synergistic effect of emodin in combination with ampicillin or oxacillin against methicillin-resistant Staphylococcus aureus . Pharmaceutical Biology. 2010;48(11):1285–1290. doi: 10.3109/13880201003770150. [DOI] [PubMed] [Google Scholar]
- 81.Kang H.-K., Kim H.-Y., Cha J.-D. Synergistic effects between silibinin and antibiotics on methicillin-resistant Staphylococcus aureus isolated from clinical specimens. Biotechnology Journal. 2011;6(11):1397–1408. doi: 10.1002/biot.201000422. [DOI] [PubMed] [Google Scholar]
- 82.Joshi P., Singh S., Wani A., et al. Osthol and curcumin as inhibitors of human Pgp and multidrug efflux pumps of Staphylococcus aureus: reversing the resistance against frontline antibacterial drugs. MedChemComm. 2014;5(10):1540–1547. doi: 10.1039/c4md00196f. [DOI] [Google Scholar]
- 83.Akiyama H., Fujii K., Yamasaki O., Oono T., Iwatsuki K. Antibacterial action of several tannins against Staphylococcus aureus . Journal of Antimicrobial Chemotherapy. 2001;48(4):487–491. doi: 10.1093/jac/48.4.487. [DOI] [PubMed] [Google Scholar]
- 84.Zhao W.-H., Hu Z.-Q., Okubo S., Hara Y., Shimamura T. Mechanism of synergy between epigallocatechin gallate and β-lactams against methicillin-resistant Staphylococcus aureus . Antimicrobial Agents and Chemotherapy. 2001;45(6):1737–1742. doi: 10.1128/aac.45.6.1737-1742.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gupta S. C., Patchva S., Aggarwal B. B. Therapeutic roles of curcumin: lessons learned from clinical trials. AAPS Journal. 2013;15(1):195–218. doi: 10.1208/s12248-012-9432-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Burgos-Morón E., Calderón-Montaño J. M., Salvador J., Robles A., López-Lázaro M. The dark side of curcumin. International Journal of Cancer. 2010;126(7):1771–1775. doi: 10.1002/ijc.24967. [DOI] [PubMed] [Google Scholar]
- 87.McNally S. J., Harrison E. M., Ross J. A., Garden O. J., Wigmore S. J. Curcumin induces heme oxygenase 1 through generation of reactive oxygen species, p38 activation and phosphatase inhibition. International Journal of Molecular Medicine. 2007;19(1):165–172. [PubMed] [Google Scholar]
- 88.Kang J., Chen J., Shi Y., Jia J., Zhang Y. Curcumin-induced histone hypoacetylation: the role of reactive oxygen species. Biochemical Pharmacology. 2005;69(8):1205–1213. doi: 10.1016/j.bcp.2005.01.014. [DOI] [PubMed] [Google Scholar]
- 89.Atsumi T., Fujisawa S., Tonosaki K. Relationship between intracellular ROS production and membrane mobility in curcumin- and tetrahydrocurcumin-treated human gingival fibroblasts and human submandibular gland carcinoma cells. Oral Diseases. 2005;11(4):236–242. doi: 10.1111/j.1601-0825.2005.01067.x. [DOI] [PubMed] [Google Scholar]
- 90.Sharma R. A., Euden S. A., Platton S. L., et al. Phase I clinical trial of oral curcumin: biomarkers of systemic activity and compliance. Clinical Cancer Research. 2004;10(20):6847–6854. doi: 10.1158/1078-0432.ccr-04-0744. [DOI] [PubMed] [Google Scholar]
- 91.Balaji S., Chempakam B. Toxicity prediction of compounds from turmeric (Curcuma longa L) Food and Chemical Toxicology. 2010;48(10):2951–2959. doi: 10.1016/j.fct.2010.07.032. [DOI] [PubMed] [Google Scholar]
- 92.Manju S., Sreenivasan K. Conjugation of curcumin onto hyaluronic acid enhances its aqueous solubility and stability. Journal of Colloid and Interface Science. 2011;359(1):318–325. doi: 10.1016/j.jcis.2011.03.071. [DOI] [PubMed] [Google Scholar]
- 93.Dey S., Sreenivasan K. Conjugation of curcumin onto alginate enhances aqueous solubility and stability of curcumin. Carbohydrate Polymers. 2014;99:499–507. doi: 10.1016/j.carbpol.2013.08.067. [DOI] [PubMed] [Google Scholar]
- 94.Esmaili M., Ghaffari S. M., Moosavi-Movahedi Z., et al. Beta casein-micelle as a nano vehicle for solubility enhancement of curcumin; food industry application. LWT—Food Science and Technology. 2011;44(10):2166–2172. doi: 10.1016/j.lwt.2011.05.023. [DOI] [Google Scholar]
- 95.O'Toole M. G., Henderson R. M., Soucy P. A., et al. Curcumin encapsulation in submicrometer spray-dried chitosan/Tween 20 particles. Biomacromolecules. 2012;13(8):2309–2314. doi: 10.1021/bm300564v. [DOI] [PubMed] [Google Scholar]
- 96.Ucisik M. H., Küpcü S., Schuster B., Sleytr U. B. Characterization of CurcuEmulsomes: nanoformulation for enhanced solubility and delivery of curcumin. Journal of Nanobiotechnology. 2013;11(1, article 37) doi: 10.1186/1477-3155-11-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Pan K., Zhong Q., Baek S. J. Enhanced dispersibility and bioactivity of curcumin by encapsulation in casein nanocapsules. Journal of Agricultural and Food Chemistry. 2013;61(25):6036–6043. doi: 10.1021/jf400752a. [DOI] [PubMed] [Google Scholar]
- 98.Thomas C., Pillai L. S., Krishnan L. Evaluation of albuminated curcumin as soluble drug form to control growth of cancer cells in vitro . Journal of Cancer Therapy. 2014;5(7):723–734. doi: 10.4236/jct.2014.57081. [DOI] [Google Scholar]
- 99.Kim T. H., Jiang H. H., Youn Y. S., et al. Preparation and characterization of water-soluble albumin-bound curcumin nanoparticles with improved antitumor activity. International Journal of Pharmaceutics. 2011;403(1-2):285–291. doi: 10.1016/j.ijpharm.2010.10.041. [DOI] [PubMed] [Google Scholar]
- 100.Yallapu M. M., Jaggi M., Chauhan S. C. Curcumin nanoformulations: a future nanomedicine for cancer. Drug Discovery Today. 2012;17(1-2):71–80. doi: 10.1016/j.drudis.2011.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Yallapu M. M., Jaggi M., Chauhan S. C. Curcumin nanomedicine: a road to cancer therapeutics. Current Pharmaceutical Design. 2013;19(11):1994–2010. doi: 10.2174/138161213805289219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ghalandarlaki N., Alizadeh A. M., Ashkani-Esfahani S. Nanotechnology-applied curcumin for different diseases therapy. BioMed Research International. 2014;2014:23. doi: 10.1155/2014/394264.394264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Quitschke W. W. Differential solubility of curcuminoids in serum and albumin solutions: implications for analytical and therapeutic applications. BMC Biotechnology. 2008;8, article 84 doi: 10.1186/1472-6750-8-84. [DOI] [PMC free article] [PubMed] [Google Scholar]