Abstract
Background: Despite exercise capacity and quality-of-life benefits, pulmonary rehabilitation (PR) and cardiac rehabilitation (CR) programmes are not easily accessed because of several barriers. A solution may be telerehabilitation (TR), in which patients exercise in their communities while they are monitored via teletechnology. However, the benefits of TR for the purposes of PR and CR have not been systematically reviewed. Objective: To determine whether the benefits of the exercise component of PR and CR using TR are comparable to usual-care (UC) programmes. Methods: A comprehensive literature search was performed of the Medline, Embase, and CINAHL databases up to July 13, 2015. Meta-analyses were performed for peak oxygen consumption, peak workload, exercise test duration, and 6-minute walk test (6MWT) distance using the I2 statistic and forest plots displaying standardized mean difference (SMD). Results: Of 1,431 citations found, 8 CR studies met the inclusion criteria. No differences were found in exercise outcomes between UC and TR groups for CR studies, except in exercise test duration, which slightly favoured UC (SMD 0.268, 95% CI: 0.002, 0.534, p<0.05). Only 1 PR study was included, and it showed similar improvements on the 6MWT between the UC and TR groups. Conclusion: TR for patients with cardiac conditions provided benefits similar to UC with no adverse effects reported. Similar studies of TR for patients with pulmonary conditions need to be conducted.
Key Words : chronic obstructive pulmonary disease, heart diseases, rehabilitation, systematic review, telemedicine, telerehabilitation
Abstract
Contexte : malgré leurs effets positifs sur la capacité d'effort et la qualité de vie, les programmes de réadaptation pulmonaire (PR) et de réadaptation cardiaque (CR) ne sont pas faciles d'accès en raison de divers obstacles. La téléréadaptation permet aux patients de faire de l'exercice dans leur communauté tout en étant suivis grâce aux télétechnologies. Or, les bienfaits de la téléréadaptation pulmonaire et cardiaque n'ont pas encore été recensés de façon systématique. Objectif : déterminer si les effets du volet exercice de la réadaptation pulmonaire et cardiaque par téléréadaptation se comparent à ceux que l'on observe chez les patients recevant des soins habituels. Méthodes : une recherche exhaustive a été effectuée sur les banques de données Medline, Embase et CINAHL en amont du 13 juillet 2015. Des méta-analyses ont été effectuées pour la consommation maximale d'oxygène, la charge de travail maximale, la durée du test d'effort et la distance marchée lors du test de 6 minutes de marche au moyen de la statistique I2 et de graphiques en forêt affichant la différence moyenne normalisée (DMN). Résultats : parmi les 1431 articles relevés, huit études en réadaptation cardiaque satisfaisaient aux critères. Aucune différence notable n'a été observée dans les effets de l'exercice entre les groupes recevant des soins traditionnels et les groupes en téléréadaptation dans les études de réadaptation cardiaque, sauf pour la durée du test d'effort, où les résultats des soins traditionnels étaient légèrement meilleurs (DMN: 0,268, intervalle de confiance de 95%, 0,002 à 0,534; p<0,05). Une seule étude sur la réadaptation pulmonaire a été retenue; les améliorations observées au test de marche de 6 minutes étaient semblables pour les groupes en soins traditionnels et en téléréadaptation. Conclusion : la téléréadaptation procure aux patients souffrant de problèmes cardiaques des bienfaits semblables aux soins traditionnels sans effets indésirables signalés. Il faudra réaliser des études similaires sur des patients atteints de problèmes pulmonaires.
Mots clés : maladie pulmonaire obstructive chronique, maladies cardiaques, réadaptation, télémédecine, téléréadaptation
Cardiac rehabilitation (CR) and pulmonary rehabilitation (PR) are recommended for patients with cardiovascular disease (CVD) and chronic obstructive pulmonary disease (COPD), respectively, who have disabling symptoms, poor exercise capacity, reduced quality of life, the need for chronic disease management skills, or all of these.1–4 The typical location for CR and PR programmes is within a hospital or health centre setting, with supervision from physiotherapists or other health care professionals and access to a variety of exercise and monitoring equipment. These programmes increase quality of life, exercise capacity, and muscle strength.2,4–11 The hallmark feature of CR and PR is aerobic training, typically delivered in a group format; both types of rehabilitation also include education and behavioural modification.2–4,12
In Canada, fewer than 2% of COPD patients have access to PR.13,14 This low percentage is comparable to that in the United Kingdom, where fewer than 1.5% of patients with COPD have access to a PR programme in their community, with only 68 programmes nationwide in 2004.15,16 With respect to CR, fewer than 30% of cardiac patients who were qualified for CR in the United Kingdom attended a rehabilitation programme,17 despite all hospitals with an acute cardiac department providing access to a CR programme.17
Telerehabilitation (TR) has been proposed as a health service option to enable more patients to receive care regardless of where they live.18 TR programmes with exercise components that include telemonitoring may improve exercise-related outcomes, better ensure patient safety during exercise, and ultimately improve access to rehabilitation interventions, yet to date the benefits of CR or PR with telemonitoring have not been thoroughly systematically reviewed. TR for cardiac or pulmonary patients has been evaluated in several trials.19–24 Some of these studies have included telemonitored aerobic exercise that included the acquisition and transfer of data on the physiological responses to exercise, such as heart rate.19,22,25
Physiotherapists are key members of the CR and PR teams and use a combination of clinical reasoning, knowledge of the pathophysiology of disease, objective measures of exercise response, and patient-reported outcomes to monitor and progress exercise programmes for individuals with heart or lung disease.2,4,14 In a TR setting, it is likely that physiotherapists would facilitate and adjust exercise programmes on the basis of a variety of information, including data from telemonitoring devices.7,18,24
A systematic review conducted by Hwang and colleagues26 on randomized controlled trials of TR home-based CR and PR compared with centre-based CR and PR programmes found that 6-minute walk test (6MWT), oxygen consumption, and quality of life improved similarly in each.26 Although promising, this review included only randomized controlled trials in which telephone calls were the form of telemonitoring used. This systematic review and meta-analysis seeks to add strength to the TR knowledge base by exploring studies that used more sophisticated telemonitoring interventions. It is important to confirm the exercise benefits and safety aspects of TR in heart and lung disease patients compared with traditional CR and PR. This is particularly relevant to physiotherapists given that they are the primary health care professionals involved in CR and PR exercise monitoring and progression. Therefore, the purpose of this systematic review and meta-analysis was to determine and compare the exercise capacity changes from exercise programmes delivered via pulmonary or cardiac TR with telemonitoring compared with those from usual-care (UC) rehabilitation.
Methods
Literature search
A systematic review of randomized and non-randomized controlled trials that compared TR with UC rehabilitation for cardiac and lung disease patients was conducted. Literature searches were performed in Medline, EMBASE, and CINAHL. The subject TR is termed telemedicine in Medline's database. Databases were searched up to July 13, 2015. Citation index searches were conducted on related systematic reviews and included studies. Grey literature was searched through the University of British Columbia Library database. Only full-text studies written in English were included.
The search terms used were as follows: pulmonary or airway or airflow or lung or bronch* or respire* (terms were used adjacent to the derivative of obstruct*) or chronic or pulmonary emphysema or hyperlucent lung; or heart or cardiac or myocardial (terms were used adjacent to disease* or failure* or attack* or decompensation* or infarction*) or arrhythmia; AND telemedicine or telehealth or ehealth or telerehabilitation or health mobile or home care services or rehabilitation or exercise or walking or exercise therapy or physical fitness or exercise movement techniques or exercise* (adjacent to) train* or strength* (adjacent to) train* or physiothe* or physical therap*.
Study selection and eligibility
Our systematic review was registered with PROSPERO (registration no. CRD42014346). Full-text articles were retrieved and reviewed on the basis of inclusion criteria. Included studies were randomized and non-randomized controlled trials that compared TR with UC rehabilitation for CR and PR populations. Included studies (1) enrolled adult participants aged at least 18 years with physician-diagnosed COPD or CVD; (2) included people eligible for outpatient CR or PR; (3) delivered rehabilitation programmes that included exercise; (4) involved an experimental arm that provided TR with telemonitoring to assess signs, symptoms, and exercise parameters; and (5) compared TR with UC, which was defined as a rehabilitation programme located in a hospital, clinic, or community centre in which health care practitioner supervision was delivered in person. Real-time transmission of data to an off-site practitioner was not a requirement.
Article review and data abstraction
Studies were screened for inclusion by two authors who assessed titles and abstracts independently before a third reviewer completed a consensus. Reasons for exclusion were recorded. Two reviewers performed data extraction of the included studies using a data extraction form; they recorded inclusion criteria, intervention descriptions, patient characteristics, all outcome measures, and the study's conclusion. The primary outcome of exercise capacity was evaluated by timed walk test distance, peak workload, exercise duration, and peak oxygen consumption (VO2 peak). Secondary outcomes were health-related quality-of-life scores, adverse events, compliance rates, and complications with TR sessions. The two reviewers tested the data collection form on two included studies to ensure they recorded all desired data in the same way. Minor changes were made to the form before it was used with all included studies.
Risk of bias within studies
Risk of bias within studies was assessed using the Physiotherapy Evidence Database (PEDro) Scale because it is a valid scale for measuring the quality of randomized and non-randomized clinical trials.27 The scale mainly evaluates whether a study was randomized; used blinded participants, therapists, and assessors; adequately collected data; and compared results between intervention groups. Studies that received scores of at least 8 out of 10 were considered good quality; studies that received scores less than 8 were considered weak to moderate quality.
Meta-analysis
Meta-analysis was performed using Comprehensive Meta-Analysis software (Biostat, Englewood, NJ). I2 values less than 50% were used to indicate sufficient homogeneity between studies for meta-analysis,28 and I2 values less than 30% resulted in a fixed-effect model in the meta-analysis. Effect sizes for each intervention group were calculated using standardized mean differences (SMDs) for the main exercise outcomes of VO2 peak, peak workload achieved on a maximal exercise test, exercise duration during a maximal exercise test, and 6MWT distance. SMD calculations incorporated TR and UC post-intervention sample size and pre- and post-intervention means and standard deviations for each outcome measure. Forest plots displaying SMD and 95% CIs were used to compare effects between intervention groups. SMDs less than ±0.2 are interpreted as small effects, those ranging from ±0.2 to ±0.8 as medium effects, and those greater than ±0.8 as large effects.29 The study by Sparks and colleagues23 did not report numeric data and was therefore not included in the meta-analysis.
Results
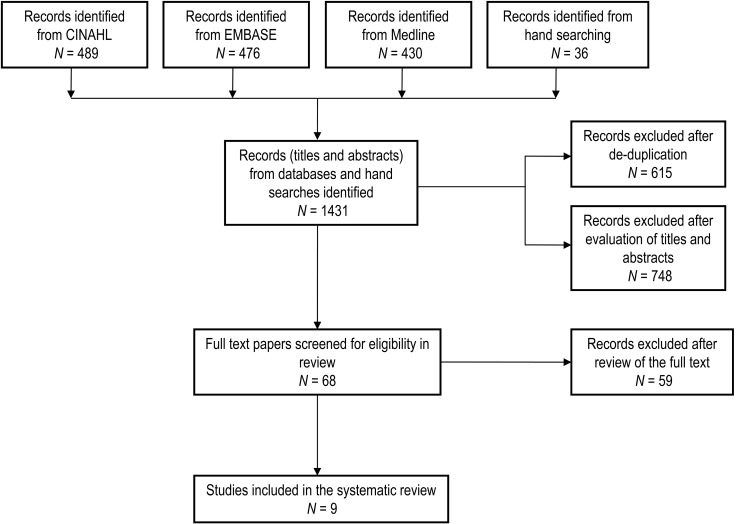
Figure 1 diagrams the selection process. The literature search produced 1,431 citations, leading to 9 articles eligible for the systematic review. The main reasons for exclusion were lack of exercise monitoring using teletechnology in the TR group and the absence of a UC group for comparison.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram of included studies
Summaries of study participant characteristics and exercise prescriptions are found in Tables 1 and 2, respectively. Eight studies found were based on CR; only one study based on PR for people with COPD met all inclusion criteria. Study participants' cardiovascular diagnoses or procedures were acute myocardial infarction, coronary artery bypass grafting, coronary angioplasty and other transcatheter procedures, cardiac transplantation, and post-valve surgery. The study on people with COPD included those who had previously completed a PR programme or were familiar with PR. Five studies were non-randomized controlled trials, and four were randomized controlled trials. All studies were of outpatient programmes and reported on patient demographics and health characteristics. However, each study reported different measures of exercise capacity and health-related quality of life.
Table 1.
Study Participant Characteristics
| Group age, mean (SD) y |
Total men, % |
||||
|---|---|---|---|---|---|
| First author and study year | N (TR/UC) | TR | UC | TR | UC |
| Sparks (1993)23 | 20 (10/10) | 50.0 (8.5) | 53.3 (7.3) | 100 | 100 |
| Ades (2000)30 | 133 (50/83) | 56 (9) | 58 (12) | 90 | 76 |
| Giallauria (2006)25 | 30 (15/15) | 60 (6) | 54 (8) | 100 | 100 |
| Dalleck (2010)31 | 226 (53/173) | 68 (9) | 67 (11) | 55 | 58 |
| Paneroni (2015)32 | 36 (18/18) | 65.7 (10.5) | 66.3 (6) | 89 | 83 |
| Piotrowicz (2010)33 | 131 (75/56) | 56.4 (10.9) | 60.5 (8.8) | 85 | 95 |
| Koreniowska-Kubacka (2011)22 | 62 (30/32) | 55.5 (8.1) | 55.2 (7.7) | 100 | 100 |
| Kraal (2014)19 | 50 (25/25) | 60.6 (7.5) | 56.1 (8.7) | 88 | 84 |
| Varnfield (2014)34 | 94 (53/41) | 56.2 (10.1) | 54.9 (9.6) | 90 | 83 |
| Total | 782 (329/453) | 84 | 75 | ||
TR/UC=telerehabilitation/usual care.
Table 2.
Study Exercise Prescriptions (Cardiac Rehabilitation)
| First author and study year |
TR intervention description/monitoring |
TR exercise prescription | UC exercise prescription |
|---|---|---|---|
| Sparks (1993)23 |
• Scott Care Tele-Rehab transtelephonic system monitored ECGs during exercise | • Cycle ergometer 3 d/wk for 12 wk for a maximum of 35 min/session at 60%–75% max HR reserve achieved during a cardiopulmonary exercise test | • Same as TR group |
| • Patients in direct telephone contact with the practitioner and other patient participants during exercise | |||
| Ades (2000)30 |
• Scott Care Tele-Rehab transtelephonic system monitored ECGs during exercise | • Cycle ergometer continuous or intermittent for 15–25 min/session at 65% maximal measured HR | • Treadmill exercise for 36 sessions over 3 mo at 25–30 min/session. |
| • Patients in direct telephone contact with the practitioner and other patient participants during exercise | • 5–10 min of another apparatus | ||
| Giallauria (2006)25 |
• Sorin Life Watch CG 6106 used to record and transmit ECG, at baseline and during exercise | • 8 wk home-based CR with telecardiology monitoring | • Standard in-hospital 8 wk CR monitored by a cardiologist |
| • ECG transmitted to a call centre by home telephone, then sent to clinic centre by email within minutes | • 3 sessions/wk, 30 min cycling at 75% peak HR | • 3 sessions/wk, 30 min cycling at 75% peak HR in baseline exercise stress test | |
| Dalleck (2010)31 |
• Rural patients travelled to a setting closer to them where on-site junior exercise physiologist monitored pulse oximetry, blood pressure, and RPE via portable telemetry | • 4–7 d/wk, RPE of 11–13 on a scale of 6–20, 20–60 min/d | • Same as TR group |
| • Telemetry was also monitored by an exercise physiologist at the conventional site | • Exercises designed to patient preferences, included stepper, arm ergometer, cycle ergometer, elliptical cross-trainer, and treadmill | ||
| • Site had 2 large video displays, 2 videoconferencing units, and 1 video visualizer camera | |||
| Paneroni (2015)32 |
• IGEA-SAT platform involved a remote control with interactive television monitor that screened participants for dyspnea, leg fatigue, and oxygen saturation (portable pulse oximeter used) before and after exercise sessions | • 28 exercise sessions over 40 days, 100 min/session. | • Same as TR group. |
| • Practitioner periodically called or videoconferenced to collect clinical data, supervise, support, and reinforce the rehabilitation program. Practitioner contacts were gradually tapered off. | • 40 min incremental cycle ergometer, 40 min muscle strength exercises, 20 min stretching and relaxation | ||
| • Exercise prescription was updated every 2 d on the basis of symptoms and outcomes | |||
| Piotrowicz (2010)33 |
• EHO 3 device to record ECG data from 3 pre-cordial leads and transmit the data to a monitoring centre via a mobile phone | • 5–10 min warm-up, 10–30 continuous walking training, 5 min cool down | • 8 wk endurance training was interval training on a cycle ergometer |
| • Before training, answered questions on phone about condition (fatigue, dyspnoea, BP, body mass, and medications) | • Same intensity prescription as UC | • Target training HR was 40%–70% of the HR reserve and/or max of 11 on the Borg Scale (6–20). | |
| • Exercise programs were adjusted on the basis of exercise results and symptoms | • Started at 10 or 15 min/session, twice daily, or 20 min/session/d, depending on baseline VO2 peak | • Started at 10–15 min/session/d (1–3 min exercise followed by 1–2 min active recovery) | |
| Koreniowska- Kubacka (2011)22 |
• EHO 3 device to record ECG data from 3 pre-cordial leads and transmit the data to a monitoring centre via a mobile phone | • Walking training: 3 10 min walk exercises with 2 min rest in between. | • Cycle ergometer 3 times/wk for 8 wk, 40 min/session. |
| • ECG assessed for HR, arrhythmias, changes in ST segment, and other cardiac disturbances | • 4 min warm-up, 6 4 min bouts of exercise with 2 min rest in between, 10 min cool down. | ||
| • ECG, HR, and BP were measured at baseline, at the end of each interval, and at recovery. | |||
| Kraal (2014)19 |
• Garmin Forerunner 70 HR monitor recorded HR and exercise data | • 3 exercise sessions at main site, followed by individualized walking or jogging for 12 wk | • Treadmill or cycle ergometry 2 times/wk for 12 weeks at 70%–85% max HR for 45–60 min/session |
| • Data uploaded to a web application called Garmin Connect for review by practitioners during weekly telephone calls | |||
| Varnfield (2014)34 |
• CAP-CR used a Nokia N96 smartphone with WellnessDiary and StepCounter applications | • Moderate walking (Borg scale 11–13) for 6 wk on most days of the week for at least 30 min/time | • Light to moderate intensity (Borg scale 6–13) cardiovascular and strengthening routine consisting of a mixture of treadmill, rower, resistance bands, weights, squats, and modified push-ups 2 times/wk for 6 wk |
| • WellnessDiary tracked daily blood pressure, weight, and other lifestyle habits. | |||
| • StepCounter monitored steps, duration, and intensity during exercise | |||
| • Data sent using a mobile 3G network to a mentor who provided feedback during weekly telephone consultations |
TR=telerehabilitation; UC=usual care; ECG=electrocardiogram; HR=heart rate; CR=cardiac rehabilitation; RPE=rating of perceived exertion; BP=blood pressure; VO2 peak=peak oxygen consumption; CAP=care assessment platform.
All studies followed existing guidelines used in clinical rehabilitation programmes in prescribing aerobic exercise for the TR interventions.2,3 However, none of the CR exercise prescriptions included resistance exercise. Flexibility training was also not included, and only two studies included details about warm-up and cool-down times.30,31 In addition, three studies used walking training in their TR group but used cycle ergometers and other machines in their UC groups.22,30,33 Despite these differences in exercise intervention, no differences were found in changes in exercise capacity between groups, indicating no training specificity from these exercise prescription differences.
Risk of bias
Studies scored between 4 and 6 out of 10 on the PEDro Scale (Table 3), which classified them as weak- to moderate-quality studies. Thus, results cannot be considered objectively valid and free of major biases within and across studies without further investigation into each study. The major reason for low quality was a lack of randomization and blinding.
Table 3.
PEDro Scale
| PEDro ratings |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| First author | 1* | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total† |
| Ades30 | Yes | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| Dalleck31 | Yes | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 4 |
| Giallauria25 | Yes | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| Koreniowska-Kubacka22 | Yes | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| Kraal19 | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Paneroni32 | Yes | 1 | 1 | 1 | 1 | 1 | 5 | |||||
| Piotrowicz33 | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 5 |
| Sparks23 | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 5 |
| Varnfield34 | Yes | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 6 |
Note: Mean (SD) of the Total Pedro ratings is 5.1 (0.6).
The first item refers to external validity, but is not included in the total PEDro score.
Each item is given 1 point for a yes answer. Maximum total score is 10.
PEDro=Physiotherapy Exercise Database.
Technologies used
Five studies used electrocardiography to monitor TR participants (Table 2). The studies by Korzeniowska-Kubacka and colleagues22 and Piotrowicz and colleagues33 used the Pro Plus (Warsaw, Poland) EHO 3 device. This device uses four electrodes to record three-channel electrocardiograms (ECGs). Data were sent to a mobile phone and then transmitted to a monitoring centre for assessment by a health care practitioner. ECGs and pre-exercise screening calls monitored for arrhythmias, ST segment changes, and other cardiac symptoms. The EHO 3 also had pre-programmed training sessions for participants that outlined exercise duration, breaks, and ECG recording. Studies led by Ades30 and Sparks23 used the Scott Care (Cleveland, OH) Tele-Rehab system, and the study led by Giallauria25 used a Sorin (Milan, Italy) Life Watch CG 6106. Both devices used an ECG to monitor exercise, and home telephone connections were used to communicate ECGs to practitioners.
The study by Dalleck and colleagues31 used supervising staff along with video cameras at TR sites to monitor exercise, but off-site staff did not communicate with patients or TR site staff during exercise. The study by Kraal and colleagues19 used the Garmin Forerunner 70, which recorded heart rate along with exercise data. These data were communicated to the rehabilitation centre and used for weekly progress calls via a web application called Garmin Connect. Varnfield and colleagues34 implemented a smartphone system called the Care Assessment Platform (CAP) that used a Nokia (Espoo, Finland) N96 smartphone equipped with applications to monitor exercise intensity and record daily health status measurements. Data transmission to a practitioner used a mobile network and was followed by weekly telephone calls. The PR study by Paneroni and colleagues32 implemented an interactive television monitor and remote control system called the IGEA-SAT (Kell, s.r.l., Milan, Italy) platform that monitored dyspnea, leg fatigue, and oxygen saturation before and after exercise sessions on a cycle ergometer.
Exercise outcomes
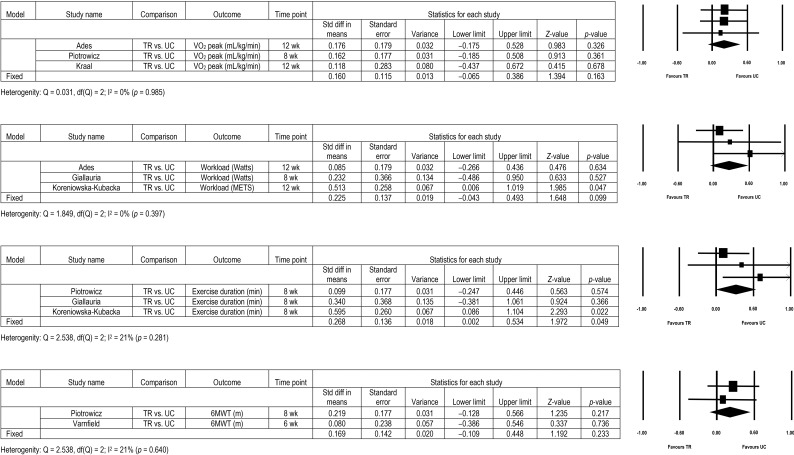
Pre- and post-intervention outcome measures are summarized in Table 4. Studies headed by Ades,30 Kraal,19 Piotrowicz,33 and Sparks23 found significant improvements in VO2 peak for both groups, ranging from increases of 1.1 ml/kg/minute to 4.9 ml/kg/minute (Sparks did not include the right kind of numeric data so could not be included in the meta-analysis and this table). Overall, the cumulative I2 statistic was 0%, and the SMD between the TR and UC groups was 0.160 (95% CI: −0.065, 0.386; p=0.16), indicating no difference between the groups (Figure 2).
Table 4.
Baseline and Post-Intervention Outcome Measures
| TR |
UC |
p-value between groups, p<0.05 |
|||
|---|---|---|---|---|---|
| Outcome and first author | Pre- intervention, mean (SD) |
Post- intervention, mean (SD) |
Pre- intervention, mean (SD) |
Post- intervention, mean (SD) |
|
| VO2 peak (ml/kg/min) | |||||
| Ades30 | 19.2 (5.5) | 22.7* (7.3) | 21.2 (5.6) | 26.1* (8.3) | NS |
| Piotrowicz33 | 17.8 (4.1) | 19.7* (5.2) | 17.9 (4.4) | 19.0* (4.6) | NS |
| Kraal19 | 22.8 (4.2) | 26.0* (5.9) | 23.7 (6.4) | 26.1* (7.6) | NS |
| Peak workload (W or MET) | |||||
| Ades30 | 106 W (36) | 131 W* (40) | 131 W (34) | 159 W* (32) | NS |
| Giallauria25 | 100 W (24.5) | 123 W* (20.7) | 94 W (16.4) | 112 W (22.4)* | 0.01 |
| Koreniowska-Kubacka22 | 8.5 METs (1.8) | 9.9 METs* ( 2.2) | 7.3 METs (1.4) | 7.8 METs* ( 1.2) | NS |
| Kraal19 | 181.1 W (49) | 200.2 W* (53.3) | 179.6 W (53.9) | 202.4 W* (68.2) | NS |
| Energy expenditure (kcal/week) | |||||
| Dalleck31 | 307 (359) | 1,225 (664) | 209 (307) | 1,181* (676) | Not reported |
| 6MWT distance (m) | |||||
| Paneroni32 | 380 (86) | 414.2 (50.8) | 397 (57) | 430.6 (39.2) | NS |
| Piotrowicz33 | 418 (92) | 462* (91) | 398 (91) | 462* (92) | 0.05 |
| Varnfield34 | 520 (78) | 570* (80) | 527 (86) | 584* (99) | NS |
| Exercise duration (min) | |||||
| Giallauria25 | 5.8 (2.1) | 7.6* (2.5) | 3.6 (1.2) | 4.6* (2.2) | 0.01 |
| Piotrowicz33 | 6.8 (2.3) | 8.0* (2.7) | 7.1 (2.3) | 8.0* (2.3) | NS |
| Koreniowska-Kubacka22 | 10.9 (3.6) | 12.5* (4.1) | 10.1 (2.0) | 13.5* (1.4) | NS |
Statistically significant difference between pre- and post-intervention (p<0.05).
TR=telerehabilitation; UC=usual care; VO2 peak=peak oxygen consumption; NS=not statistically significant; MET=metabolic equivalent of task; 6MWT=six-minute walk test.
Figure 2.
Meta-analysis and forest plot of peak oxygen consumption, peak workload, exercise test duration, and 6-minute walk test distance.
TR=telerehabilitation; UC=usual care, VO2=peak oxygen consumption; MET=metabolic equivalent of task; 6MWT=6-minute walk test.
Ades and colleagues,30 Sparks and colleagues,23 and Koreniowska-Kubacka and colleagues22 showed similar improvements in peak workload between TR and UC groups. Meanwhile, Giallauria and colleagues25 found greater improvements in peak workload among the TR group. Interestingly, this study included a third intervention group that performed unmonitored home exercise, which did not show an improvement (data not included in meta-analysis).25 The I2 was 0% over the three studies. Overall, there was no difference between TR and UC groups based on a SMD of 0.225 (95% CI: −0.043, 0.493; p=0.10; Figure 2).
Three studies investigated exercise duration outcomes between groups.22,25,33 The I2 value indicated low heterogeneity at 21.2%. Figure 2 shows that the SMD was statistically significant at 0.268 in favour of UC (95% CI: 0.002, 0.534; p<0.05).
Studies led by Piotrowicz33 and Varnfield34 showed statistically significant improvements in 6MWT distance in both groups with no significant differences between intervention groups. The two studies produced an I2 value of 0%, and the SMD was 0.169 (95% CI: −0.109, 0.448; p=0.23), suggesting no difference between groups (Figure 2).33,34 The lone PR study by Paneroni and colleagues32 found statistically significant improvements in both groups (UC: means=397–430.6 m, SDs=57–39.2; p=0.002; TR: means=380–414.2 m, SDs=86–50.8; p=0.008). There was no significant difference between groups (p=0.91), indicating similar changes.
Secondary outcomes
Adverse events and compliance
Adverse events were examined in seven of the eight CR studies and in the PR study with no reported adverse events during any exercise sessions. Challenges related to using devices in the TR group were examined in only two studies.30,33 Ades and colleagues30 reported that 7 of 3,100 exercise sessions in the TR group were stopped due to abnormal symptoms recorded by the monitoring equipment. Piotrowicz and colleagues33 reported no complications or cancelled sessions. Intervention compliance rates were reported in six studies, with each having good compliance throughout. The studies spearheaded by Kraal19 and Piotrowicz33 had perfect compliance in the TR group, with 86% and 80% compliance in the UC group, respectively, for. Sparks and colleagues23 had 93% compliance in the TR group and 83% compliance in the UC group. Paneroni and colleagues32 reported TR group compliance at 82%, compared with 100% for the UC group, and Varnfield and colleagues34 had 94% compliance in the TR group and 68% compliance in the UC group. Dalleck and colleagues31 reported similar compliance rates between groups, with rates at 81% in the TR group and 83% in the UC group.
Self-reported quality of life and health status
Five studies measured quality of life or psychological profile.19,25,30,31,34 Using the Health Status Questionnaire, Ades and colleagues30 reported significant improvements in both groups in all eight domains except health perception and mental health. Giallauria and colleagues25 used four different questionnaires, the State–Trait Anxiety Inventory Form Y1 (STAI-Y-1; state anxiety), State–Trait Anxiety Inventory Form Y2 (trait anxiety), Beck Depression Inventory (BDI), and Medical Outcomes Study 36-Item Short-Form Health Survey. Only the TR group improved their STAI-Y-1 and BDI scores. Dalleck and colleagues31 reported reductions in stress scores in both groups. The study led by Varnfield34 found significant improvements in depression and anxiety scores in both groups using the Depression, Anxiety and Stress Scale, but only the TR group significantly improved on the Kessler 10 for psychological distress and the EuroQol 5 Dimensions tool. Kraal and colleagues19 used the MacNew Questionnaire and found significant improvements in all three domains in the UC group, but only in the physical and social domains for the TR group, because emotional improvements were not significant. Last, Paneroni and colleagues32 found similar statistically significant improvements in both groups in the St. George's Respiratory Questionnaire's total score.
Discussion
This systematic review reports on the impact of cardiac and pulmonary TR, versus traditional hospital-based or UC rehabilitation, on exercise and quality-of-life–related outcomes. We found that, in general, cardiac and pulmonary TR interventions resulted in outcomes similar to those of traditional CR and PR, except for exercise duration, which slightly favoured UC. There were no reported adverse events, hospitalizations, or mortality during telemonitored exercise. However, included studies were of poor to moderate quality; thus, findings should be viewed with caution. In addition, only one PR study that met all inclusion criteria was found.
Many of the TR trials in this systematic review used sophisticated technology such as ECG to monitor their participants during the exercise sessions. This level of monitoring may have encouraged the participants to exercise at a higher intensity than they may have without the monitoring, because quantitative values could influence or moderate feelings of discomfort and risk from exercise. It is important to note that in other trials of unmonitored home-based PR and CR, the investigators developed exercise prescriptions that were of lower intensity than would have been used in the traditional setting because of safety concerns.21,26,28 This review also demonstrated that health-related quality-of-life improvements were not different between TR and UC groups despite the lack of direct contact with health care providers and less interaction with other participants in the TR groups. In addition, three studies reported similar levels of adherence to exercise between groups. It is possible that despite the lack of in-person supervision to monitor symptoms (as would be found in a clinical environment), the inclusion of ECG monitoring in the TR group may have had the same effects in increasing the participants' self-efficacy for exercise, resulting in high adherence rates and improved quality of life.3,9 Future research should explore how telemonitoring versus in-person supervision affects exercise self-efficacy.
The main limitation of the review was a low number of articles that met the inclusion criteria, especially only one on PR. More TR research on PR is needed because the findings from CR cannot necessarily be generalized to the population with COPD. In our clinical experience, the monitoring requirements, disease severity, and patient characteristics between these two patient populations are often quite different.
Another limitation of the review was the poor to moderate score in terms of bias (PEDro Scale) primarily from lack of blinding of therapists and participants. Although blinding of therapists and participants would be difficult in TR, studies used standardized tests to evaluate changes in exercise capacity as a way to minimize any potential biases. However, when reviewing findings in the TR groups, it should be noted that therapist expectations and data collection biases may have inflated results. Thus, still remains a need for more randomized controlled trials or blinding of researchers to increase the quality of evidence and decrease potential outcome biases.
Conclusion
With an increasing need for better access to rehabilitation for patients with CVD and COPD, TR interventions may offer a feasible, effective, and safe option. In this systematic review of nine studies, TR interventions in which a health care practitioner monitored patient symptoms before and during exercise appeared to offer similar benefits to the standard exercise components of CR and PR programmes. The findings from this systematic review and meta-analysis suggest that physiotherapists who are interested in developing TR interventions for their patients with CVD and COPD can expect similar exercise and quality-of-life outcomes for their patients, provided the technology and level of monitoring are similar to those used in the studies presented here. Researchers should also continue to explore the different barriers and factors at play in implementing TR interventions in CR and PR, including both quantitative and qualitative research to explore and identify solutions to barriers to TR programme implementation and participant motivation.
Key Messages
What is already known on this topic
Cardiac rehabilitation (CR) and pulmonary rehabilitation (PR) programmes are effective in improving exercise capacity, quality of life, and chronic disease management, but home-based delivery of rehabilitation programmes may lack practitioner monitoring and safety. Telerehabilitation is a health service option that can potentially increase the capacity and reach of CR and PR programmes to those without access.
What this study adds
This systematic review and meta-analysis found that telemonitored PR and CR studies comparing telerehabilitation with usual-care (UC) methods of delivery had similar exercise capacity benefits (6-minute walk test, peak workload, maximal exercise test duration, and peak oxygen consumption) between intervention groups, with no adverse events reported in the telerehabilitation groups. Only one study comparing telerehabilitation with UC for PR was included, with the study finding similar improvements on the 6-minute walk test between intervention groups.
References
- 1. Celli BR, MacNee W, Agusti A, et al. ; ATS/ERS Task Force. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004;23(6):932–46. http://dx.doi.org/10.1183/09031936.04.00014304. Medline:15219010 [DOI] [PubMed] [Google Scholar]
- 2. Spruit MA, Singh SJ, Garvey C, et al. ; ATS/ERS Task Force on Pulmonary Rehabilitation. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13–64. http://dx.doi.org/10.1164/rccm.201309-1634ST. Medline:24127811 [DOI] [PubMed] [Google Scholar]
- 3. Balady GJ, Ades PA, Comoss P, et al. . Core components of cardiac rehabilitation/secondary prevention programs: A statement for healthcare professionals from the American Heart Association and the American Association of Cardiovascular and Pulmonary Rehabilitation Writing Group. Circulation. 2000;102(9):1069–73. http://dx.doi.org/10.1161/01.CIR.102.9.1069. Medline:10961975 [DOI] [PubMed] [Google Scholar]
- 4. Balady GJ, Williams MA, Ades PA, et al. . Core components of cardiac rehabilitation/secondary prevention programs: 2007 update: a scientific statement from the American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee, the Council on Clinical Cardiology; the Councils on Cardiovascular Nursing, Epidemiology and Prevention, and Nutrition, Physical Activity, and Metabolism; and the American Association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2007;115(20):2675–82. http://dx.doi.org/10.1161/CIRCULATIONAHA.106.180945. Medline:17513578 [DOI] [PubMed] [Google Scholar]
- 5. Royal College of Physicians. Chronic obstructive pulmonary disease: management of chronic obstructive pulmonary disease in adults in primary and secondary care: update guideline. NICE clinical guidelines no. 101 London: Royal College of Physicians; 2010. [PubMed] [Google Scholar]
- 6. Puhan MA, Gimeno-Santos E, Scharplatz M, et al. . Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2011;(10):CD005305 Medline:21975749 [DOI] [PubMed] [Google Scholar]
- 7. Hailey D, Roine R, Ohinmaa A, et al. . Evidence of benefit from telerehabilitation in routine care: a systematic review. J Telemed Telecare. 2011;17(6):281–7. http://dx.doi.org/10.1258/jtt.2011.101208. Medline:21844172 [DOI] [PubMed] [Google Scholar]
- 8. Troosters T, Gosselink R, Decramer M. Short- and long-term effects of outpatient rehabilitation in patients with chronic obstructive pulmonary disease: a randomized trial. Am J Med. 2000;109(3):207–12. http://dx.doi.org/10.1016/S0002-9343(00)00472-1. Medline:10974183 [DOI] [PubMed] [Google Scholar]
- 9. McCarthy B, Casey D, Devane D, et al. . Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2015:(2):CD003793 http://dx.doi.org/10.1002/14651858.CD003793.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Couser JI Jr, Guthmann R, Hamadeh MA, et al. . Pulmonary rehabilitation improves exercise capacity in older elderly patients with COPD. Chest. 1995;107(3):730–4. http://dx.doi.org/10.1378/chest.107.3.730. Medline:7874945 [DOI] [PubMed] [Google Scholar]
- 11. Garcia-Aymerich J, Lange P, Benet M, et al. . Regular physical activity reduces hospital admission and mortality in chronic obstructive pulmonary disease: a population based cohort study. Thorax. 2006;61(9):772–8. http://dx.doi.org/10.1136/thx.2006.060145. Medline:16738033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cooper CB. Exercise in chronic pulmonary disease: aerobic exercise prescription. Med Sci Sports Exerc. 2001;33(7 Suppl):S671–9. http://dx.doi.org/10.1097/00005768-200107001-00005. Medline:11462076 [DOI] [PubMed] [Google Scholar]
- 13. Brooks D, Lacasse Y, Goldstein RS. Pulmonary rehabilitation programs in Canada: national survey. Can Respir J. 1999;6(1):55–63. Medline:10202221 [PubMed] [Google Scholar]
- 14. Brooks D, Sottana R, Bell B, et al. . Characterization of pulmonary rehabilitation programs in Canada in 2005. Can Respir J. 2007;14(2):87–92. Medline:17372635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Yohannes AM, Connolly MJ. Pulmonary rehabilitation programmes in the UK: a national representative survey. Clin Rehabil. 2004;18(4):444–9. http://dx.doi.org/10.1191/0269215504cr736oa. Medline:15180129 [DOI] [PubMed] [Google Scholar]
- 16. Yohannes A, Stone R, Lowe D, et al. . Pulmonary rehabilitation in the United Kingdom. Chron Respir Dis. 2011;8(3):193–9. http://dx.doi.org/10.1177/1479972311413400. Medline:21724662 [DOI] [PubMed] [Google Scholar]
- 17. Bethell H, Lewin R, Dalal H. Cardiac rehabilitation in the United Kingdom. Heart. 2009;95(4):271–5. http://dx.doi.org/10.1136/hrt.2007.134338. Medline:18208830 [DOI] [PubMed] [Google Scholar]
- 18. Brooks D. Telehealth technology: an emerging method of delivering pulmonary rehabilitation to patients with chronic obstructive pulmonary disease. Can Respir J. 2011;18(4):196 Medline:22059177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kraal JJ, Peek N, Van den Akker-Van Marle ME, et al. . Effects of home-based training with telemonitoring guidance in low to moderate risk patients entering cardiac rehabilitation: short-term results of the FIT@Home study. Eur J Prev Cardiol. 2014;21(2 Suppl):26–31. http://dx.doi.org/10.1177/2047487314552606. Medline:25354951 [DOI] [PubMed] [Google Scholar]
- 20. Holland A. Telehealth reduces hospital admission rates in patients with COPD. J Physiother. 2013;59(2):129 http://dx.doi.org/10.1016/S1836-9553(13)70168-1. Medline:23663801 [DOI] [PubMed] [Google Scholar]
- 21. Stickland M, Jourdain T, Wong EY, et al. . Using telehealth technology to deliver pulmonary rehabilitation in chronic obstructive pulmonary disease patients. Can Respir J. 2011;18(4):216–20. Medline:22059179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Koreniowska-Kubacka I, Dobraszkiewicz-Wasilewska B, Bilińska M, et al. . Two models of early cardiac rehabilitation in male patients after myocardial infarction with preserved left ventricular function: comparison of standard out-patient versus hybrid training programmes. Kardiol Pol. 2011;69(3):220–6. Medline:21432787 [PubMed] [Google Scholar]
- 23. Sparks KE, Shaw DK, Eddy D, et al. . Alternatives for cardiac rehabilitation patients unable to return to a hospital-based program. Heart Lung. 1993;22(4):298–303. Medline:8360063 [PubMed] [Google Scholar]
- 24. Maltais F, Bourbeau J, Shapiro S, et al. ; Chronic Obstructive Pulmonary Disease Axis of Respiratory Health Network, Fonds de recherche en santé du Québec. Effects of home-based pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: a randomized trial. Ann Intern Med. 2008;149(12):869–78. http://dx.doi.org/10.7326/0003-4819-149-12-200812160-00006. Medline:19075206 [DOI] [PubMed] [Google Scholar]
- 25. Giallauria F, Lucci R, Pilerci F, et al. . Efficacy of telecardiology in improving the results of cardiac rehabilitation after acute myocardial infarction. Monaldi Arch Chest Dis. 2006;66(1):8–12. Medline:17125041 [DOI] [PubMed] [Google Scholar]
- 26. Hwang R, Bruning J, Morris N, et al. . A systematic review of the effects of telerehabilitation in patients with cardiopulmonary diseases. J Cardiopulm Rehabil Prev. 2015;35(6):380–9. http://dx.doi.org/10.1097/HCR.0000000000000121. Medline:26034937 [DOI] [PubMed] [Google Scholar]
- 27. PEDro Scale [Internet]. Missenden (NSW): Centre for Evidence-Based Physiotherapy Musculoskeletal Division, George Institute for Global Health; 1999. [cited 2015 May 12]. Available from: http://www.pedro.org.au/wp-content/uploads/PEDro_scale.pdf [Google Scholar]
- 28. Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, et al. . Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods. 2006;11(2):193–206. http://dx.doi.org/10.1037/1082-989X.11.2.193. Medline:16784338 [DOI] [PubMed] [Google Scholar]
- 29. Takeshima N, Sozu T, Tajika A, et al. . Which is more generalizable, powerful and interpretable in meta-analyses, mean difference or standardized mean difference? BMC Med Res Methodol. 2014;14(1):30 http://dx.doi.org/10.1186/1471-2288-14-30. Medline:24559167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ades PA, Pashkow FJ, Fletcher G, et al. . A controlled trial of cardiac rehabilitation in the home setting using electrocardiographic and voice transtelephonic monitoring. Am Heart J. 2000;139(3):543–8. http://dx.doi.org/10.1016/S0002-8703(00)90100-5. Medline:10689271 [DOI] [PubMed] [Google Scholar]
- 31. Dalleck LC, Schmidt LK, Lueker R. Cardiac rehabilitation outcomes in a conventional versus telemedicine-based programme. J Telemed Telecare. 2011;17(5):217–21. http://dx.doi.org/10.1258/jtt.2010.100407. Medline:21508077 [DOI] [PubMed] [Google Scholar]
- 32. Paneroni M, Colombo F, Papalia A, et al. . Is telerehabilitation a safe and viable option for patients with COPD? A feasibility study. COPD. 2015;12(2):217–25. http://dx.doi.org/10.3109/15412555.2014.933794. Medline:25093419 [DOI] [PubMed] [Google Scholar]
- 33. Piotrowicz E, Baranowski R, Bilinska M, et al. . A new model of home-based telemonitored cardiac rehabilitation in patients with heart failure: effectiveness, quality of life, and adherence. Eur J Heart Fail. 2010;12(2):164–71. http://dx.doi.org/10.1093/eurjhf/hfp181. Medline:20042423 [DOI] [PubMed] [Google Scholar]
- 34. Varnfield M, Karunanithi M, Lee CK, et al. . Smartphone-based home care model improved use of cardiac rehabilitation in postmyocardial infarction patients: results from a randomised controlled trial. Heart. 2014;100(22):1770–9. http://dx.doi.org/10.1136/heartjnl-2014-305783. Medline:24973083 [DOI] [PubMed] [Google Scholar]