In 2014, the American Heart Association (AHA) announced the funding of a Strategically Focused Research Network (SFRN) focused on hypertension. Hypertension was chosen for a SFRN because interdisciplinary hypertension research has great potential to impact the AHA’s mission and 2020 goals of improving the cardiovascular health of all Americans by 20% while reducing deaths from CVD and stroke by 20% by 2020. Four centers with highly integrated basic, clinical and population science projects were selected for the AHA SFRN: Cincinnati Children’s Hospital, Medical College of Wisconsin (MCW), University of Alabama at Birmingham (UAB), and University of Iowa (UI). The Cincinnati center is studying ambulatory blood pressure and hypertensive target organ damage in adolescents. The MCW center is studying epigenetics of hypertension by conducting studies of genome-wide DNA methylation patterns. The UAB center is studying racial differences in the prevalence and determinants of abnormal diurnal blood pressure patterns. The UI center is studying copeptin, a possible early biomarker for preeclampsia and vascular endothelial function and arterial stiffness changes occurring prior to and during preeclampsia. In this article, we provide an overview of the science being conducted at each center and describe the innovative training program incorporated into the SFRN. A goal of the Hypertension SFRN is to facilitate collaborative research. Therefore, we describe opportunities and resources available to researchers interested in collaborating with SFRN investigators. The AHA Hypertension SFRN has the potential to identify new approaches for the prevention and treatment of hypertension and, ultimately, improve the cardiovascular health of Americans.
The Strategically Focused Research Network (SFRN) is a mechanism initiated by the American Heart Association (AHA) to address key strategic issues as determined by the AHA Board of Directors. In 2014, hypertension was selected for a SFRN because improvement in its prevention and treatment has the potential to impact the AHA’s mission and 2020 goals: to improve the cardiovascular health of all Americans by 20% while reducing deaths from CVD and stroke by 20% by the year 2020. The AHA announced that it would be supporting four centers focused on research in the field of hypertension for a period of four years. This award mechanism embraces a Network “Center” concept. Each Center was required to propose a designated Center Director, basic, clinical and population science projects that are synergistic and related to the topic of hypertension, and a research postdoctoral fellowship training component.
After peer-review, four SFRN hypertension centers were awarded: Cincinnati Children’s Hospital, Medical College of Wisconsin, the University of Alabama at Birmingham and the University of Iowa. This brief review provides an introduction to the AHA Hypertension SFRN, which was launched in April of 2015. We review the science proposed by each of the funded centers (Figure 1). A major focus of the SFRN is building collaborations to advance the science of hypertension. Therefore, we describe opportunities for collaborative research and the shared resources available through the science being conducted to build partnerships through the Hypertension SFRN. Lastly, we provide an overview of the innovative training component for post-doctoral fellows in the Hypertension SFRN.
Figure 1.
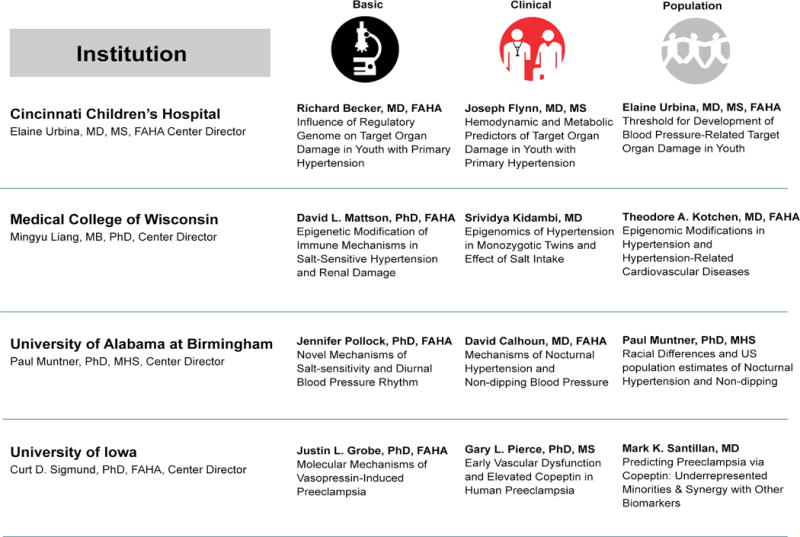
Overview of the Hypertension Strategically Focused Research Network science.
Hypertension SFRN Science
Cincinnati Children’s Hospital Center
The goals of the Study of High Blood Pressure In Pediatrics: Adult Hypertension Onset in Youth (SHIP AHOY) are to 1) redefine the thresholds for childhood hypertension, based on evidence, 2) better define the clinical phenotype of blood pressure (BP) associated target organ (TOD) damage, and 3) shift the paradigm from regarding high BP as a risk factor for subsequent cardiovascular disease to an actual disease-causing condition in the young. Investigators will conduct an integrated series of population, clinical and basic science research studies.
The population science project, “Threshold for Development of Blood Pressure-Related Target Organ Damage in Youth,” will attempt to advance our knowledge about the timing of hypertension-induced TOD development, with the hypothesis that hypertensive cardiovascular injury is not limited to long standing hypertension in adults, but emerges at an early phase of primary hypertension. The specific aims of this project are to 1) demonstrate an increase in measures of TOD from low-, to mid-, to high-risk BP levels, 2) determine the prevalence and BP threshold for hypertensive left ventricular hypertrophy (LVH) in a cohort of adolescents with normal, mid- and high-risk BP, and 3) determine the prevalence and BP threshold for secondary measures of TOD (i.e. microalbuminuria, increased pulse wave velocity).
The clinical science project, “Hemodynamic and Metabolic Predictors of Target Organ Damage in Youth with Primary Hypertension” will provide further evidence on the evolution of hypertensive cardiovascular disease in youth by testing the hypothesis that a combination of BP (hemodynamic) phenotype and metabolic phenotype (i.e. lipids and glycemic control) will be superior to clinic BP in predicting underlying TOD in adolescents with high risk BP. The specific aims of this project are to 1) determine if BP phenotype, based on a combination of casual (clinic) and ambulatory BP readings, predicts underlying TOD in asymptomatic adolescents, and 2) determine if there is a metabolic phenotype that is predictive of TOD.
The basic science project, “Influence of Regulatory Genome on Target Organ Damage in Hypertensive Youth,” will allow a better understanding of the transition points from risk factors for disease to measureable TOD to true clinical disease in patients with systemic hypertension. It will test the hypothesis that the presence of systemic hypertension, on a genetic background and in the presence of common intermediate-phenotypes, including obesity and metabolic abnormalities, leads to TOD in primary hypertension in youth. The specific aims of this project are to 1) demonstrate that epigenetic modifications of candidate genes associated with hypertension and LVH are linked to the presence or absence of disease-modifying conditions or intermediate phenotypes, and 2) demonstrate that there is altered expression of potentially disease-modifying miRNAs, specifically those miRNAs associated with LVH, among youth with hypertension.
Medical College of Wisconsin (MCW) Center
The MCW Center focuses on investigating the epigenomics of hypertension. Hypertension, the leading identifiable cause of death worldwide, in most cases, is the result of interactions between genetic background and environmental factors, including diet and other lifestyle choices.1 BP is one of the most notable examples in which DNA polymorphisms, identified by Genome Wide Association Studies, account for only a very small fraction of the variation of the trait. The missing heritability of BP variation may be due to several reasons, including epigenetics.2
Epigenetic studies examine molecular changes, called epigenetic marks or mediators, and associated phenotypes that are mitotically inheritable but do not involve changes in the DNA sequence, while epigenomics is defined as the study of epigenetic marks or mechanisms at a genome or near-genome scale. Major types of epigenetic mediators include DNA methylation, histone modification, non-coding RNA and chromatin structure.3 A significant role of epigenetic modifications in the development of hypertension is supported by numerous studies.2, 3 For example, studies have shown that parental exposure to a specific environment, fetal exposure to a specific in utero environment as well as early life environment can affect the development of hypertension in adulthood. Epigenetic changes in several genes, such as 11beta-hydroxysteroid dehydrogenase type 2 and angiotensin converting enzyme, are associated with the development of hypertension;3 however, studies of epigenetic modifications in hypertension at the genome or near-genome scale are just beginning to emerge.3 The epigenomics of hypertension remains a large, open field, and with recent technological advances, this field of study appears ripe for paradigm-shifting discoveries in hypertension research.
The main objective of the MCW Center program is to carry out a systematic investigation of the relevance of genome-wide DNA methylation patterns to hypertension. The overall hypothesis is that dietary salt intake and other lifestyle factors, maternal dietary exposures and gene-environment interactions cause genome-wide changes in DNA methylation, which contribute to the development of hypertension and can be used as predictive or diagnostic markers of hypertension and related diseases. The basic science project will test the general hypothesis that the maternal dietary environment alters the epigenomic program in immune cells in salt-sensitive rats and their de novo methylation response to an increased salt intake later in adult life, which in turn affects immune cell infiltration and activation in the kidney and modifies salt-sensitive hypertension and renal disease. The clinical project will examine the effects of lifestyle factors, including dietary salt intake on epigenomic changes in human subjects, and whether such effects can reveal potential mechanisms of hypertension. The population project will investigate whether DNA methylation patterns are associated with levels of BP and predict the development of hypertension and related cardiovascular events in an African-American cohort. All three projects will analyze DNA methylation at near-genome-wide scale using the technology of reduced representation bisulfite sequencing (RRBS) as described previously.4
University of Alabama at Birmingham (UAB) Center
Ambulatory blood pressure monitoring (ABPM) allows for the determination of several BP measures that cannot be ascertained in the clinic or through home monitoring.5 ABPM can assess diurnal BP patterns including nocturnal hypertension and non-dipping BP (i.e., when BP does not decline by the usual 10–20% at night). Studies from Europe and Asia have reported strong associations between nocturnal hypertension and a non-dipping BP pattern with an increased risk for CVD and all-cause mortality.6–8 Preliminary data suggest that African Americans may have higher nocturnal BP and may be more likely to be non-dippers compared with whites.9, 10 The UAB SFRN investigators are conducting an integrated series of research studies on diurnal BP patterns.
The population science project, “Racial differences and US population estimates of nocturnal hypertension and non-dipping”, involves the examination of racial differences in the prevalence of nocturnal hypertension and non-dipping blood pressure. This project will determine if the association of risk factors, including psychosocial factors and sleep disordered breathing, with these phenotypes differ by race as well as determining the association of nocturnal hypertension and non-dipping blood pressure on target organ damage. For this study, ABPM will be conducted in 700 African American and white participants at the Year 30 Coronary Artery Risk Development in Young Adults (CARDIA) study visit.11 Additionally, questionnaires on sleep, anxiety and stress will be completed by the participants. The US population burden of nocturnal hypertension and non-dipping BP will also be estimated using simulation methods.
The clinical science project, “Mechanisms of nocturnal hypertension and non-dipping blood pressure”, will identify the effect of dietary sodium restriction on nocturnal BP and non-dipping and assess whether the effects are due to improvements in obstructive sleep apnea. Whether aldosterone levels potentiate the response of nocturnal BP, non-dipping BP, and severity of sleep apnea to dietary sodium will also be determined. This project involves a randomized cross-over feeding trial enrolling 60 participants (30 African American and 30 white) with nocturnal hypertension identified from the population project. Participants will be fed 10 days of a low or high sodium diet followed by a washout period and then 10 days of the opposite diet. During the last two days of each feeding period, participants will collect buccal cells every four hours for use in the basic science project.
The basic science project, “Novel mechanisms of salt-sensitivity and diurnal blood pressure rhythm”, will address three aims: (1) elucidate whether high salt diet induces renal microvascular dysfunction through the activity of histone deacetylase 1 (HDAC1) leading to reduced nitric oxide (NO) and/or increased reactive oxygen species (ROS), (2) determine the impact of dietary salt intake on BP rhythms in a rat model of nocturnal hypertension, the Dahl salt-sensitive rat, and whether the non-dipping is related to renal vascular ROS production, and (3) analyze changes in the expression of clock genes (CLOCK, Bmal1, per1, per2, cry1, and cry2) in the buccal cells during consumption of low versus high sodium diets from human participants in the clinical science project.
University of Iowa (UI) Center
Preeclampsia, a rapidly progressive condition characterized by high BP and proteinuria, affects 8% of all pregnancies. Often not diagnosed until late pregnancy, it is the cause of 76,000 maternal and 500,000 infant deaths per year.12 Absence of a robust, early biomarker of preeclampsia which directs mechanistic research and treatment for the disorder represents a fundamental gap in knowledge and clinical practice.
The UI Center proposal was based on three seminal observations. First, high circulating copeptin, a stable, easily detectable biomarker for arginine vasopressin (AVP), robustly predicts development of preeclampsia very early in pregnancy.13–16 Second, women who have elevated copeptin in the first trimester of pregnancy demonstrate reduced endothelial function and increased arterial stiffness in the second trimester compared with women with low copeptin. Third, UI investigators have developed a new mouse model in which chronic low-dose AVP infusion during pregnancy phenocopies preeclampsia. Collectively these findings lead to the hypotheses that copeptin represents a novel and powerful predictive diagnostic test for preeclampsia, and that AVP may play a causal role in the early pathogenesis of the disorder.17 The goal of the UI SFRN is to translate these findings and develop preventative, therapeutic, and curative modalities against preeclampsia.
The Population Project, “Predicting Preeclampsia via Copeptin: Underrepresented Minorities & Synergy with Other Biomarkers,” will assess the predictive power of copeptin in diverse populations and compare it with current biomarkers of preeclampsia. The central hypotheses are: 1) copeptin will be predictive of preeclampsia in the first trimester of pregnancy regardless of comorbidities or demographics, and 2) copeptin will serve as an earlier and better predictor of preeclampsia than other biomarkers.
The Clinical Project, “Early Vascular Dysfunction and Elevated Copeptin in Human Preeclampsia,” will assess temporal changes in vascular endothelial function and arterial stiffness throughout pregnancy in women stratified to either high or low copeptin measured in the first trimester of pregnancy. This project addresses two main hypotheses: Compared to women with low copeptin 1) early- and mid- gestation women with elevated copeptin will demonstrate reduced vascular endothelial function and elevated aortic stiffness prior to traditional signs of preeclampsia, and 2) women with high copeptin and reduced vascular function will have a higher incidence of preeclampsia.
The Basic Project, “Molecular Mechanisms of Vasopressin-Induced Preeclampsia,” uses a novel mouse model of preeclampsia to examine the mechanisms of vascular dysfunction in preeclamptic mothers and adult offspring. This model will be used to: 1) examine the importance of vascular dysfunction in the mother and adult offspring from preeclamptic pregnancies complicated by AVP infusion, 2) identify the tissue targets of AVP, and the receptors at those tissues that mediate phenotypes, and 3) examine if there is any role for copeptin itself in the development of preeclampsia.
Collaboration
The AHA SFRN program is characterized by its emphasis on collaborative and team science, which will serve as a paradigm for interaction within each center, across the four centers and with the hypertension research community more broadly. An oversight Advisory Committee, assembled by the AHA, is available to guide interactions between the centers and facilitate collaborations between SFRN centers and other hypertension researchers.
Investigators at each center are enthusiastic to collaborate with researchers within and beyond the Hypertension SFRN to fully utilize the vast amount of resources being assembled and data being collected in the research studies (Table 1). The concept of Interest Groups has been proposed to encourage collaboration and the design of new collaborative studies. While these Interest Groups are still in a nascent phase, they may involve conference calls, a SharePoint site and in-person meetings at national conferences (e.g., AHA Council on Hypertension meeting). As Interest Groups are initiated, involvement by investigators from outside of the SFRN will be encouraged to participate. Resources beyond those directly being used in the scientific projects are available at each of the four centers to conduct collaborative research and advance the science of hypertension (Table 2).
Table 1.
Resources being generated through the American Heart Association Hypertension Strategically Focused Research Network.
| Hypertension SFRN Center | Data being collected/resources being generated |
|---|---|
|
Cincinnati Children’s Hospital (n=500, age 13–17 years, ~1/3 non-Caucasian; same cohort for all projects) |
|
| Population science project | Echocardiogram for left ventricular mass, diastolic function, strain, pulse wave velocity, urine for microalbumin, cognitive function tests, questionnaires: food frequency, exercise, socioeconomic status |
| Clinical science project | Casual/office BP, Ambulatory BP monitoring, metabolic parameters (lipids, insulin, glucose) |
| Basic science project | DNA methylation and micro RNAs related to hypertension and cardiac fibrosis |
| Medical College of Wisconsin | |
| Population science project (original African American cohort n=3,000; 50% w/hypertension) | Follow-up blood pressure and 10–20 year cardiovascular morbidity and mortality events; base-resolution DNA methylation data |
| Clinical science project Aim 1: Identical twins: ~300 pairs Aim 2: Unrelated subjects: ~60 subjects |
Aim 1: Questionnaires (activity level, socioeconomic status, sodium screener, anthropometrics, blood pressure levels, blood and urine for electrolytes, and DNA from various cellular components. Aim 2: All of the above parameters, 24 hour urine collection for electrolytes pre- and post-low sodium diet. Base-resolution DNA methylation data in both aims. |
| Basic science project | Sodium-dependent and –independent effects on arterial blood pressure, heart rate, renal disease phenotypes, RNA expression and DNA methylation in T lymphocytes in the circulation and the kidney, and the expression of cytokines in the T lymphocytes. |
| University of Alabama at Birmingham | |
| Population science project (n=700; 350 whites; 350 African Americans) |
Ambulatory blood pressure monitoring, actigraphy, sleep questionnaires, psychosocial questionnaires for CARDIA participants |
| Clinical science project (n=60; 30 whites and 30 African Americans) |
Four home sleep studies, four 24-hour urine collections, four ambulatory blood pressure monitoring periods, renin, aldosterone and buccal cell collections of CARDIA participants with nocturnal hypertension |
| Basic science project | Circadian blood pressure, heart rate, activity monitoring in genetically modified Dahl salt-sensitive rats as well as diurnal sodium excretion patterns. Expression of clock genes in buccal cells from clinical project. |
| University of Iowa | |
| Population science project | Iowa SFRN Population Study Bank: First trimester maternal blood and urine that are deeply clinically annotated from hospitals throughout the state of Iowa spanning different socioeconomic and racial distributions. |
| Clinical science project (n=248 pregnant women; n=124 with high copeptin and n=124 with low copeptin) |
In vivo data obtained in pregnant women once each trimester and 6 weeks postpartum including: brachial artery flow-mediated dilation, pulse wave velocity, central blood pressure, augmentation index, common carotid artery compliance, cardiac baroreflex sensitivity, 24-hr ambulatory blood pressure, lipids/glucose, plasma/serum for vasopressin, copeptin, and pregnancy outcome data. |
| Basic science project | Development of novel clinically-relevant animal models, and exploration of clinical drug repurposing for use in preeclampsia. Blood pressure, renal, vascular, and immune functions in preeclampsia. Human blood and tissue samples made possible through interactions with Clinical and Population projects. |
CARDIA – Coronary artery risk development in young adults.
Table 2.
Additional resources available for potential collaboration with the Hypertension Strategically Focused Research Network centers.
| Center and Project | Resource |
|---|---|
| Cincinnati Children’s Hospital | |
| Population science project | Princeton study, National Growth and Health Study (longitudinal studies of cardiovascular risk factors since youth) |
| Clinical science project | International Pediatric Hypertension Association headquarters brings together experts in Pediatric hypertension and ambulatory blood pressure monitoring |
| Basic science project | Center for Pediatric Genomics including DNA sequencing & genotyping core, Pyrosequencing lab, Gene expression core, metabolomics core |
| Medical College of Wisconsin | Technologies for DNA methylation sequencing, RNA-seq and data analysis |
| Population science project | DNA in original African American cohort (n=3,000), extensive phenotyping in 550 of the cohort |
| Clinical science project | In vivo and in vitro vascular function studies in human subjects |
| Basic science project | Experiments to assess arterial blood pressure and renal disease phenotypes in conscious rats and mice. |
| University of Alabama at Birmingham | |
| Population science project | Jackson Heart Study Vanguard center, Reasons for Geographic and Racial Differences in Stroke (REGARDS) study, Coronary Artery Risk Development in Young Adults (CARDIA), ABPM and HBPM data though Hypertension SFRN partnership with Columbia University investigators |
| Clinical science project | Antihypertensive Lipid-Lowering to Prevent Heart Attack Trial (ALLHAT) network lead Systolic Blood Pressure Intervention Trial (SPRINT) network lead Studies of resistant and refractory hypertension |
| Basic science project | Studies of renal function and measurements of nitric oxide and reactive oxygen species in animal models of hypertension |
| University of Iowa | |
| Population science project | University of Iowa Maternal Fetal Tissue Bank: Prospectively collected maternal, paternal, and fetal biosamples throughout gestation including blood, urine, amniotic fluid, placenta, and cord blood that are deeply clinically annotated from UI patients as previously described (Santillan 2014, see footnote); biomarker identification, testing, and analysis; immunologic and primary placental mechanistic studies; preclinical therapeutic studies in preeclampsia. |
| Clinical science project | Cross-sectional and various short-term intervention studies with vascular, autonomic, metabolic, dietary, physical activity and cellular/tissue (serum/plasama endothelial, adipose, blood mononuclear) outcomes in humans with obesity, prehypertension/hypertension, prediabetes, aging, pregnancy or chronic anxiety. |
| Basic science project | UI Center for Hypertension Research which includes studies of autonomic and vascular function in animal models of hypertension and development of novel pharmacological and genetic models of hypertensive disorders |
Santillan MK, Leslie KK, Hamilton WS, Boese BJ, Ahuja M, Hunter SK, Santillan DA. “Collection of a lifetime: A practical approach to developing a longitudinal collection of women’s healthcare biological samples”. European journal of obstetrics, gynecology, and reproductive biology. 2014;179:94–99
The Hypertension SFRN has been invited to provide an overview of the network activities, science and opportunities for collaboration at the 2016 American Society of Hypertension Scientific Meeting (May 14–17, 2016). Investigators interested in learning more about shared resources and opportunities for collaboration with the SFRN are encouraged to attend this meeting. Also, in September 2015, investigators from each center presented research at the 26th annual UAB Vascular Biology and Hypertension Symposium in Birmingham, AL. This gathering resulted in scientific exchange and the opportunity to begin the development of collaborations. The 27th annual symposium is being planned for Fall 2016 and is open to all hypertension researchers and trainees. Through collaborations, the Hypertension SFRN will provide networking opportunities for trainees, share knowledge and methods, and provide a stimulating atmosphere to develop and conduct novel research.
Hypertension SFRN Training Program
The goal of the Hypertension SFRN Training Program is to train the next generation of hypertension researchers and provide post-doctoral fellows with knowledge and hands-on experience to lead focused investigations in basic, clinical and population science as well as cross-disciplinary research studies. The four Centers in the Hypertension SFRN will collectively train 12 fellows over the 4-year project period, building the capacity for future research to advance the science of hypertension. In addition to the fellow’s primary mentor, a team of senior investigators with training expertise will help the fellow to maximize the training opportunity and overcome unanticipated barriers. There are two aspects to these Centers’ training programs that distinguish them from more customary programs: interdisciplinary training and opportunities for cross-Center collaborations.
The integrated nature of the basic, clinical, and population science projects within each Center will serve as the training ground for the Centers’ fellows, and fellows will have some experience in each of these projects, regardless of their own primary research discipline. The more usual approach to training would encourage the fellow to develop expertise in only one area of science, whether basic, clinical, or population. We are taking a different approach in recognition of the growing need for scientists who can thrive in large teams across multiple disciplines. Each fellow will have their own project and focus area within one of the Center’s three research projects, but will also have a meaningful training experience within the other two projects. These latter experiences may include spending physical time becoming integrated into the project teams by taking on a specific role (e.g., performing a research test such as ABPM or flow-mediated dilation on the study participants for the clinical or population project or learning to perform a specific assay for the basic science project). These experiences will be substantial enough to assure that the Fellow has become conversant in the language and traditions of scientific domains outside of their own area of focus, assuring readiness to participate and excel in team science in the future.
A second unique feature of the Hypertension SFRN training programs is the opportunity for cross-Center collaborations and training experiences. The fellows will learn of each Center’s projects and expertise available at the centers through monthly conference calls and annual in-person Hypertension SFRN meetings. Fellows will present their own work, and the work they are doing within their own Centers population, clinical and basic science projects. Through these interactions, Fellows will be given opportunities to broaden their own professional networks by getting to know each other as well as scientists at the other Centers. They will be encouraged to develop cross-Center projects, possibly even spending time at the other Centers to learn specific skills. In this way, the hypertension SFRN Center fellows will develop broad skills not only through interactions within their own Centers but across Centers, building a solid foundation for successful careers in hypertension research. Further information on training opportunities at the four Hypertension SFRN Centers can be obtained by contacting the Center or training directors (Table 3).
Table 3.
Contact information for the center directors, training directors and scientific project principal investigators.
| Affiliation | Contact and email address |
|---|---|
| AHA Program Officer | Augusta Lloyd; augusta.lloyd@heart.org |
| Hypertension SFRN Oversight Committee Chair | Dan lackland; lackland@musc.edu |
| Cincinnati Children’s Hospital | |
| Center director | Elaine M. Urbina; elaine.urbina@cchmc.org |
| Training director | Mark Mitsnefes; mark.mitsnefes@cchmc.org |
| Population project Principal Investigator | Elaine M. Urbina; elaine.urbina@cchmc.org |
| Clinic project Principal Investigator | Joseph Flynn; joseph.flynn@seattlechildrens.org |
| Basic project Principal Investigator | Richard Becker; BECKERRC@ucmail.uc.edu |
| Medical College of Wisconsin | |
| Center director | Mingyu Liang; mliang@mcw.edu |
| Training director | Allen W. Cowley, Jr.; Cowley@mcw.edu |
| Population project Principal Investigator | Theodore A. Kotchen; tkotchen@mcw.edu |
| Clinic project Principal Investigator | Srividya Kidambi; skidambi@mcw.edu |
| Basic project Principal Investigator | David L. Mattson; dmattson@mcw.edu |
| University of Alabama at Birmingham | |
| Center director | Paul Muntner; pmuntner@uab.edu |
| Training director | Monika Safford; msafford@uab.edu |
| Population project Principal Investigator | Paul Muntner; pmuntner@uab.edu |
| Clinic project Principal Investigator | David Calhoun; dcalhoun@uab.edu |
| Basic project Principal Investigator | Jennifer Pollock; pollockj@uab.edu |
| University of Iowa | |
| Center director | Curt D. Sigmund; curt-sigmund@uiowa.edu |
| Training director | Kimberly K. Leslie; kimerly-leslie@uiowa.edu |
| Population project Principal Investigator | Mark K. Santillan; mark-santillan@uiowa.edu |
| Clinic project Principal Investigator | Gary L. Pierce; gary-pierce@uiowa.edu |
| Basic project Principal Investigator | Justin L. Grobe; justin-grobe@uiowa.edu |
Perspectives
The AHA initiated the SFRN program with the explicit goal of addressing key strategic issues and improving the cardiovascular health of all Americans. Given its high prevalence and the excess CHD and stroke risk it confers, hypertension was a natural choice for a SFRN. The four funded centers incorporate research studies that cover hypertension throughout the life course from fetal exposures, through childhood, in pregnancy, and adulthood. Investigators within the SFRN are beginning to develop collaborations and welcome opportunities to develop new partnerships with investigators outside of the SFRN to leverage the infrastructure being developed and data being generated. The Hypertension SFRN has a dedicated program to train the next generation of hypertension researchers. In conclusion, the AHA Hypertension SFRN provides the opportunity to greatly increase our knowledge of hypertension, identify new approaches for its prevention, treatment, and, ultimately, improve the cardiovascular health of Americans.
Acknowledgments
Funding
Paul Muntner, David Calhoun, Daian Chen, Jennifer S. Pollock, Monika M. Safford, and Stephen J. Thomas are supported by grant 15SFRN2390002 from the American Heart Association. Allen W. Cowley Jr., Srividya Kidambi, Theodore A. Kotchen, Yingchuan Li, Mingyu Liang, and David L. Mattson are supported by grant 15SFRN23910002 from the American Heart Association. Justin L. Grobe, Kimberly K. Leslie, Anand Nair, Gary L. Pierce, Mark K. Santillan and Curt D. Sigmund are supported by grant 15SFRN23480000 from the American Heart Association. Richard C Becker, Joseph T Flynn, Brenda Mendizabal, Mark Mitsnefes, Elaine M. Urbina are supported by grant 15SFRN23680000 from the American Heart Association. Augusta Lloyd is employed by the American Heart Association. The project from the University of Cincinnati was supported by Grant 8 UL1 TR000077 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health.
Disclosures
Dr. Muntner receives research grant support unrelated to the topic of this manuscript from Amgen Inc. (>$10,000). Ms. Lloyd is employed by the American Heart Association. None of the other co-authors have disclosures.
References
- 1.Kotchen TA, Cowley AW, Jr, Liang M. Ushering hypertension into a new era of precision medicine. JAMA. 2016 doi: 10.1001/jama.2015.18359. Published online January 14, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cowley AW, Jr, Nadeau JH, Baccarelli A, Berecek K, Fornage M, Gibbons GH, Harrison DG, Liang M, Nathanielsz PW, O’Connor DT, Ordovas J, Peng W, Soares MB, Szyf M, Tolunay HE, Wood KC, Zhao K, Galis ZS. Report of the national heart, lung, and blood institute working group on epigenetics and hypertension. Hypertension. 2012;59:899–905. doi: 10.1161/HYPERTENSIONAHA.111.190116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liang M, Cowley AW, Jr, Mattson DL, Kotchen TA, Liu Y. Epigenomics of hypertension. Semin Nephrol. 2013;33:392–399. doi: 10.1016/j.semnephrol.2013.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu Y, Liu P, Yang C, Cowley AW, Jr, Liang M. Base-resolution maps of 5-methylcytosine and 5-hydroxymethylcytosine in dahl s rats: Effect of salt and genomic sequence. Hypertension. 2014;63:827–838. doi: 10.1161/HYPERTENSIONAHA.113.02637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shimbo D, Abdalla M, Falzon L, Townsend RR, Muntner P. Role of ambulatory and home blood pressure monitoring in clinical practice: A narrative review. Annals of internal medicine. 2015;163:691–700. doi: 10.7326/M15-1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fan HQ, Li Y, Thijs L, Hansen TW, Boggia J, Kikuya M, Bjorklund-Bodegard K, Richart T, Ohkubo T, Jeppesen J, Torp-Pedersen C, Dolan E, Kuznetsova T, Stolarz-Skrzypek K, Tikhonoff V, Malyutina S, Casiglia E, Nikitin Y, Lind L, Sandoya E, Kawecka-Jaszcz K, Imai Y, Ibsen H, O’Brien E, Wang J, Staessen JA, International Database on Ambulatory Blood Pressure In Relation to Cardiovascular Outcomes I Prognostic value of isolated nocturnal hypertension on ambulatory measurement in 8711 individuals from 10 populations. J Hypertens. 2010;28:2036–2045. doi: 10.1097/HJH.0b013e32833b49fe. [DOI] [PubMed] [Google Scholar]
- 7.Hansen TW, Thijs L, Li Y, Boggia J, Kikuya M, Bjorklund-Bodegard K, Richart T, Ohkubo T, Jeppesen J, Torp-Pedersen C, Dolan E, Kuznetsova T, Stolarz-Skrzypek K, Tikhonoff V, Malyutina S, Casiglia E, Nikitin Y, Lind L, Sandoya E, Kawecka-Jaszcz K, Imai Y, Wang J, Ibsen H, O’Brien E, Staessen JA. Prognostic value of reading-to-reading blood pressure variability over 24 hours in 8938 subjects from 11 populations. Hypertension. 2010;55:1049–1057. doi: 10.1161/HYPERTENSIONAHA.109.140798. [DOI] [PubMed] [Google Scholar]
- 8.Hansen TW, Li Y, Boggia J, Thijs L, Richart T, Staessen JA. Predictive role of the nighttime blood pressure. Hypertension. 2011;57:3–10. doi: 10.1161/HYPERTENSIONAHA.109.133900. [DOI] [PubMed] [Google Scholar]
- 9.Muntner P, Lewis CE, Diaz KM, Carson AP, Kim Y, Calhoun D, Yano Y, Viera AJ, Shimbo D. Racial differences in abnormal ambulatory blood pressure monitoring measures: Results from the coronary artery risk development in young adults (cardia) study. Am J Hypertens. 2015;28:640–648. doi: 10.1093/ajh/hpu193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Profant J, Dimsdale JE. Race and diurnal blood pressure patterns: A review and meta-analysis. Hypertension. 1999;33:1099–1104. doi: 10.1161/01.hyp.33.5.1099. [DOI] [PubMed] [Google Scholar]
- 11.Friedman GD, Cutter GR, Donahue RP, Hughes GH, Hulley SB, Jacobs DR, Jr, Liu K, Savage PJ. Cardia: Study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41:1105–1116. doi: 10.1016/0895-4356(88)90080-7. [DOI] [PubMed] [Google Scholar]
- 12.Duley L. The global impact of pre-eclampsia and eclampsia. Seminars in perinatology. 2009;33:130–137. doi: 10.1053/j.semperi.2009.02.010. [DOI] [PubMed] [Google Scholar]
- 13.Balanescu S, Kopp P, Gaskill MB, Morgenthaler NG, Schindler C, Rutishauser J. Correlation of plasma copeptin and vasopressin concentrations in hypo-, iso-, and hyperosmolar states. The Journal of clinical endocrinology and metabolism. 2011;96:1046–1052. doi: 10.1210/jc.2010-2499. [DOI] [PubMed] [Google Scholar]
- 14.Santillan MK, Santillan DA, Scroggins SM, Min JY, Sandgren JA, Pearson NA, Leslie KK, Hunter SK, Zamba GK, Gibson-Corley KN, Grobe JL. Vasopressin in preeclampsia: A novel very early human pregnancy biomarker and clinically relevant mouse model. Hypertension. 2014;64:852–859. doi: 10.1161/HYPERTENSIONAHA.114.03848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yeung EH, Liu A, Mills JL, Zhang C, Mannisto T, Lu Z, Tsai MY, Mendola P. Increased levels of copeptin before clinical diagnosis of preelcampsia. Hypertension. 2014;64:1362–1367. doi: 10.1161/HYPERTENSIONAHA.114.03762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cornelius DC. Copeptin: A new biomarker that is specific for preeclampsia? Hypertension. 2014;64:1189–1191. doi: 10.1161/HYPERTENSIONAHA.114.04255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sandgren JA, Scroggins SM, Santillan DA, Devor EJ, Gibson-Corley KN, Pierce GL, Sigmund CD, Santillan MK, Grobe JL. Vasopressin: The missing link for preeclampsia? American journal of physiology. Regulatory, integrative and comparative physiology. 2015;309:R1062–1064. doi: 10.1152/ajpregu.00073.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]


