Abstract
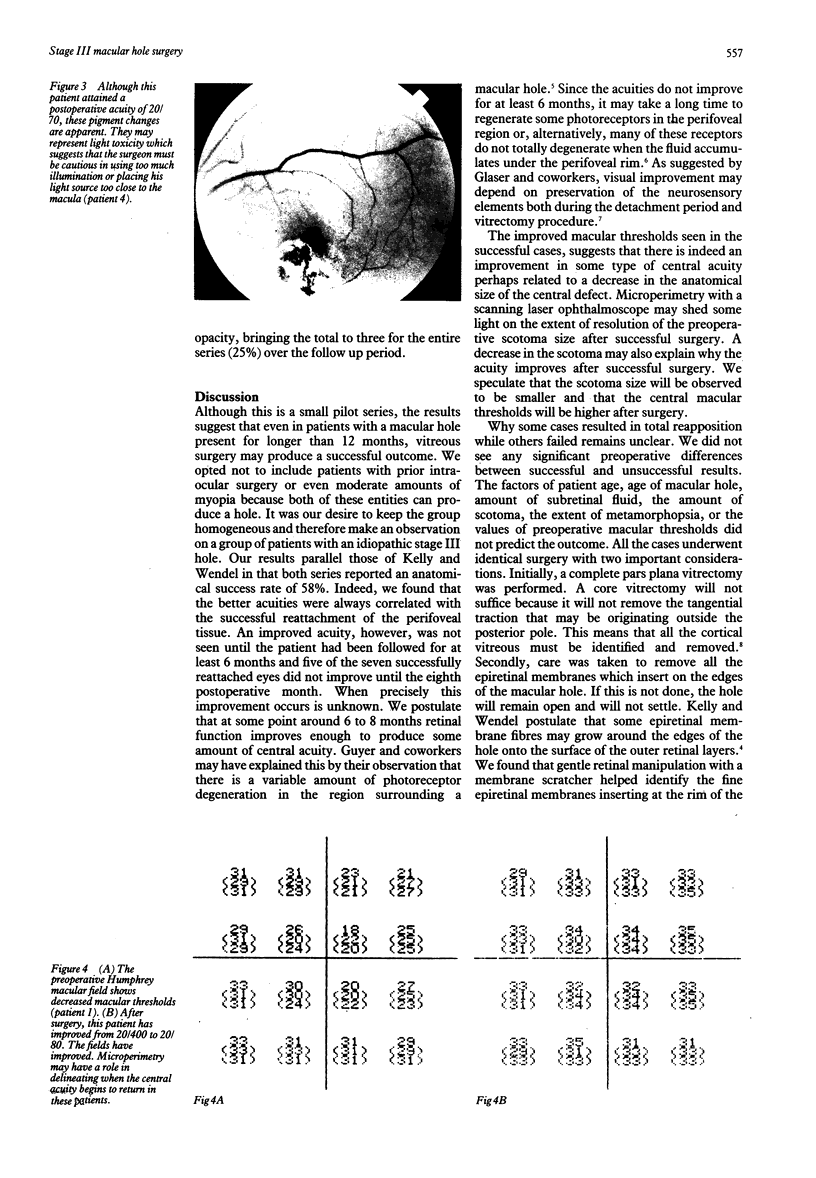
Twelve macular holes in 12 patients underwent a pars plana vitrectomy and epiretinal membrane resection with intravitreal gas tamponade for repair of their macular holes. The patients had stage III macular holes and had previously undergone a normal funduscopic examination within 2 years. The patients have been followed for a mean of 14 months (range 12-18 months) postoperatively. The results show that visual acuity improvements were not seen until at least 6 months after surgery if the hole was closed successfully. Seven holes were closed (58.3%) and all improved their best corrected visual acuity by more than two Snellen lines. In the five eyes that did not demonstrate hole closure (41.6%), one eye improved by two lines as well. The other four eyes remained at their preoperative acuity. One eye developed a dialysis which responded to a fluid air exchange and cryopexy (8.3%). Three eyes developed minimal lenticular opacities during the follow up period (25%). One eye demonstrated an altered perifoveal pigment epithelium perhaps related to intraoperative light toxicity. Macular hole surgery can restore some central acuity even in patients with longstanding holes.
Full text
PDF


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Fine S. L. Vitreous surgery for macular hole in perspective. Is there an indication? Arch Ophthalmol. 1991 May;109(5):635–636. doi: 10.1001/archopht.1991.01080050049026. [DOI] [PubMed] [Google Scholar]
- Frangieh G. T., Green W. R., Engel H. M. A histopathologic study of macular cysts and holes. Retina. 1981;1(4):311–336. [PubMed] [Google Scholar]
- Gass J. D. Idiopathic senile macular hole. Its early stages and pathogenesis. Arch Ophthalmol. 1988 May;106(5):629–639. doi: 10.1001/archopht.1988.01060130683026. [DOI] [PubMed] [Google Scholar]
- Glaser B. M., Michels R. G., Kuppermann B. D., Sjaarda R. N., Pena R. A. Transforming growth factor-beta 2 for the treatment of full-thickness macular holes. A prospective randomized study. Ophthalmology. 1992 Jul;99(7):1162–1173. doi: 10.1016/s0161-6420(92)31837-8. [DOI] [PubMed] [Google Scholar]
- Guyer D. R., Green W. R., de Bustros S., Fine S. L. Histopathologic features of idiopathic macular holes and cysts. Ophthalmology. 1990 Aug;97(8):1045–1051. doi: 10.1016/s0161-6420(90)32465-x. [DOI] [PubMed] [Google Scholar]
- Han D. P., Abrams G. W., Aaberg T. M. Surgical excision of the attached posterior hyaloid. Arch Ophthalmol. 1988 Jul;106(7):998–1000. doi: 10.1001/archopht.1988.01060140144042. [DOI] [PubMed] [Google Scholar]
- Johnson R. N., Gass J. D. Idiopathic macular holes. Observations, stages of formation, and implications for surgical intervention. Ophthalmology. 1988 Jul;95(7):917–924. doi: 10.1016/s0161-6420(88)33075-7. [DOI] [PubMed] [Google Scholar]
- Kelly N. E., Wendel R. T. Vitreous surgery for idiopathic macular holes. Results of a pilot study. Arch Ophthalmol. 1991 May;109(5):654–659. doi: 10.1001/archopht.1991.01080050068031. [DOI] [PubMed] [Google Scholar]
- Morgan C. M., Schatz H. Involutional macular thinning. A pre-macular hole condition. Ophthalmology. 1986 Feb;93(2):153–161. doi: 10.1016/s0161-6420(86)33767-9. [DOI] [PubMed] [Google Scholar]
- Schocket S. S., Lakhanpal V., Miao X. P., Kelman S., Billings E. Laser treatment of macular holes. Ophthalmology. 1988 May;95(5):574–582. doi: 10.1016/s0161-6420(88)33137-4. [DOI] [PubMed] [Google Scholar]
- Sheta S. M., Hida T., McCuen B. W., 2nd Cyanoacrylate tissue adhesive in the management of recurrent retinal detachment caused by macular hole. Am J Ophthalmol. 1990 Jan 15;109(1):28–32. doi: 10.1016/s0002-9394(14)75574-6. [DOI] [PubMed] [Google Scholar]