Abstract
Purpose:
To evaluate the changes and predictability of higher order aberrations (HOAs) after personalized laser in situ keratomileusis (LASIK) and personalized photorefractive keratectomy (PRK) for simple myopia and compound myopic astigmatism.
Methods:
In this prospective cross-sectional study, 100 eyes were included. A total of 50 eyes underwent personalized LASIK and 50 eyes underwent personalized PRK. Preoperative and postoperative wavefront data were compared between the two groups. The influential factors and predictability of HOAs were also assessed.
Result:
Total HOA increased in the amount of 0.01 ± 0.14 μm for the 5 mm pupil (P = 0.55) and 0.08 ± 0.22 μm for the 6 mm pupil (P = 0.02) after PRK; however after LASIK the corresponding values for the 5 and 6 mm pupil sizes were 0.05 ± 0.12 and 0.15 ± 0.18 μm, respectively (P < 0. 001). Mean changes were not significantly different between the PRK and LASIK groups for both 5 and 6 mm pupil sizes (P = 0.21 and P = 0.13, respectively). Spherical aberration increased following LASIK more than following PRK (P < 0.001). Changes in the root mean square (RMS) of total HOA had a statistically significant negative correlation (P < 0.001) with its preoperative value. HOA and spherical aberration reduced in majority of eyes when the preoperative spherical equivalent refraction was low.
Conclusion:
For the 6mm pupil size, the total HOA increased following both personalized PRK and LASIK with no significant difference between the two groups. Change of the total HOA RMS was influenced by the preoperative values. The known influencing factors could predict nearly 50% of the changes in total HOA.
Keywords: Wavefront-guided, High Order Aberration, Spherical Aberration, Laser in situ keratomileusis, Photorefractive Keratectomy, Personalized
INTRODUCTION
Keratorefractive surgeries successfully reduce the spherocylindrical refractive errors, however they may introduce a significant deterioration in the quality of vision. An increase in the total higher order aberrations (HOA) has been reported after radial keratotomy,[1,2] laser in situ keratomileusis (LASIK),[3,4,5,6] and photorefractive keratectomy (PRK).[4,5,6,7] This increase in HOA after corneal refractive surgery is related to the pupil size; pupil dilation from 3.0 to 7.0 mm significantly increases the optical aberrations.[7] Many visual symptoms that patients experience postoperatively may be secondary to increase in the HOAs.[8,9,10]
Both conventional PRK and LASIK may possibly increase the total HOA, spherical, and coma aberrations.[3,4,5,6,7,11] There are various parameters such as attempted optical zone, flap creation, and decentered ablation which can influence the postoperative changes in HOA.[12,13,14,15] Wavefront-guided LASIK and PRK can theoretically reduce the pre-existing HOAs after corneal refractive surgery. However, undercorrection and even induction of new HOAs are possible complications.[16,17,18] The aim of this study was to evaluate and compare changes of HOA after wavefront-guided LASIK and PRK and also to assess the factors which can predict changes in HOAs after wavefront-guided LASIK and PRK for simple myopia and compound myopic astigmatism using personalized treatment (Zyoptix, Bausch & lomb/Technolas, Munich, Germany).
METHODS
Patient Selection
This prospective cross-sectional study comprised of one hundred eyes of 50 healthy individuals including 16 male and 34 female subjects with a mean age of 29.42 ± 6.81 (range, 19–53) years. These patients were referred to Binagostar Eye Center, Shiraz, Iran for refractive surgery. All patients completed a 12 month follow-up period. Informed consent was obtained from all individuals and the Ethics Committee of Shiraz University of Medical Sciences, Shiraz, Iran approved the study. All enrolled patients had simple myopia or compound myopic astigmatism. Patients with a history of any ocular disease, previous corneal or intraocular surgery, wound healing disorder, and connective tissue diseases were excluded from the study. Other exclusion criteria were a cornea thinner than 500 micrometer, a postoperative residual stromal thickness of less than 400 micrometer, pregnancy or breastfeeding, and being on immunosuppressive medications. In addition, individuals who needed retreatment, those who developed significant corneal haze and patients with flap complications and/or or recurrent epithelial defects were excluded. The same number of 50 eyes from 25 healthy individuals were randomly assigned to undergo personalized LASIK and PRK in each group.
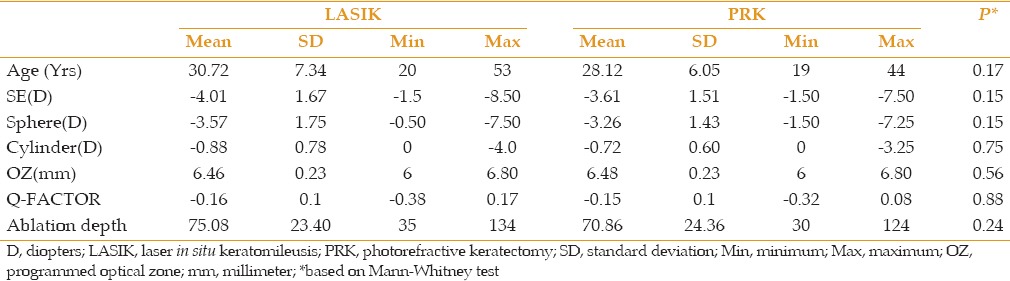
Age, sex, baseline manifest refraction, optical zone diameter, ablation depth, and baseline HOA were matched between the two groups. Demographic and refractive data are shown in Table 1.
Table 1.
Demographic and refractive data
Soft and hard contact lenses were discontinued for at least 2 and 4 weeks, respectively. Preoperative examination included uncorrected visual acuity (UCVA) and best corrected visual acuity (BCVA) assessment, manifest and cycloplegic refraction, scotopic pupil size, slit lamp examination, dilated funduscopy, applanation tonometry, ultrasonic pachymetry, and slit-scanning tomography (Bausch & Lomb Orbscan IIz Topographer, Rochester, NY, USA).
Aberrometry was performed using a Hartmann-Shack wavefront sensor (Zywave П aberrometer, Bausch & Lomb/Technolas, Munich, Germany) before and 12 months after the surgery. This aberrometer uses a 780 nm laser beam and measures approximately 70–78 locations within the pupil. Zywave examinations consisted of three consecutive examinations, 30 seconds apart, with an undilated pupil under standardized light condition. One of the three measurements that matched with the manifest refraction of the undilated pupil was chosen for treatment. Wavefront map was reported for 5 and 6 mm pupil sizes. Zywave calculates Zernike polynomials from the second to the fifth order aberrations.
Both LASIK and PRK were performed with Technolas 217z (Bausch & Lomb/Technolas, Munich, Germany), using a personalized ablation algorithm (Zyoptix, version 4.41). Laser parameters were as follows: wavelength: 193 nm; spot profile: Flat-top; spot size: 1 mm; radiant exposure (fluence): 120 mJ/cm2; and pulse repetition rate: 100 Hz. In the LASIK group, superior hinged flap was created using the Hansatome microkeratome (Zyoptix xp, Rochester, NY, USA) with a 120 μm head and 8.5 or 9.5 mm ring. PRK was performed after mechanical removal of the epithelium. If indicated, mitomycin C was applied in the PRK group after ablation.
At the completion of PRK or LASIK procedure, ciprofloxacin and prednisolone acetate 1.0% eye drops were instilled. In the PRK group, ciprofloxacin eye drop was continued 4 times a day until complete epithelial healing was achieved, by the time the bandage contact lens was removed. Subsequently, chloramphenicol eye drop and prednisolone acetate 1.0% were administered 4 times daily for the first postoperative month. Fluorometholone ophthalmic eye drop 0.1% was administered 3 times a day, twice a day, and once a day in the second, third, and fourth postoperative months, respectively. Patients were examined postoperatively on days one, 4, 7, and 14, and at months one, 3, 6, and 12. In the LASIK group, prednisolone acetate 1.0% was continued every two hours on the first 3 days after surgery and then 4 times a day for 15 days. Chloramphenicol eye drop was administered 4 times daily for the first postoperative month, as well.
Statistical Analysis
The Mann–Whitney U test was applied to compare the preoperative and postoperative HOAs in each study group. The Wilcoxon test for matched pairs was performed to analyze the surgically induced changes in Zernike terms and the root mean square (RMS) values. The increased factor of RMS was defined as the change of a wavefront error in relation to the preoperative value. Also, multiple stepwise regression analyses were performed to evaluate factors with possible effects on changes in HOA. All statistical analyses were performed using SPSS software (version 17.0, SPSS. Inc. IBM, Chicago, IL, USA).
RESULTS
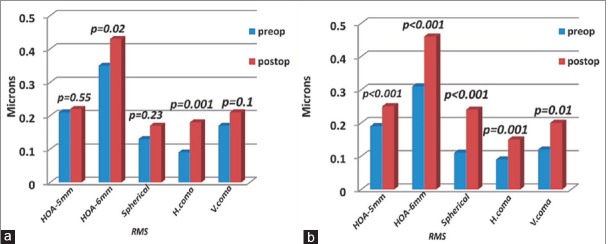
Mean postoperative spherical equivalent (SE) was −0.08 ± 0.44 diopters (D) in the PRK group and −0.18 ± 0.44 D in the LASIK group. At the 12-month follow-up visit, all (100%) eyes showed refraction within ±1.0 D of attempted SE [Figure 1]. Mean changes in the total HOA RMS are summarized in Table 2. In the eyes undergoing PRK, there was no significant change in the total HOA for the pupil size of 5 mm postoperatively (P = 0.55) whereas, it increased significantly (P < 0.02) for the 6 mm pupil size. In the LASIK group, the total HOA was increased significantly for both 5 and 6 mm pupil zone (P < 0.001). The change in total HOA did not significantly differ between the PRK and LASIK groups for both 5 and 6 mm pupil sizes (P = 0.21 and P = 0.13, respectively). In the PRK group, the total HOA RMS was reduced or remained unchanged in 24 (48%) and 21 (42%) eyes for 5 and 6 mm pupil sizes, respectively, at month 12. In the LASIK group, the total HOA RMS reduced or did not change in 14 (28%) and 10 (20%) eyes for 5 and 6 mm pupil sizes, respectively. The mean changes of spherical aberration, and vertical and horizontal coma are shown in Table 3, and Figures 2a and 2b. Spherical aberration (Z4, 0) was increased significantly in the LASIK group for the 6 mm pupil size (P < 0.001); however its increase was not significant in the PRK group (P = 0.23). The increase in spherical aberration was significantly greater in in the LASIK group than in the PRK group (P = 0.001). Spherical aberration shifted into negative values in both study groups. Compared to the baseline, horizontal coma was significantly increased in both groups (P = 0.001), but the change did not significantly differ between the LASIK and PRK groups (P = 0.69). The direction of horizontal coma was reversed in the LASIK group from a negative value to a positive one; however the value remained negative after PRK.
Figure 1.
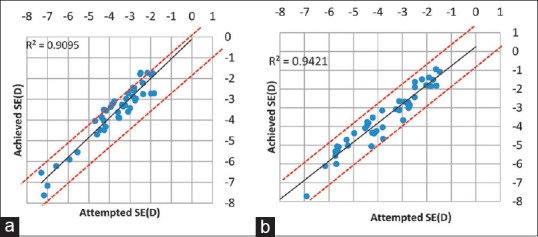
Attempted versus achieved spherical equivalent (Δ SE) one year after PRK (a) and LASIK (b) (predictability).
Table 2.
Mean changes of total HOA RMS
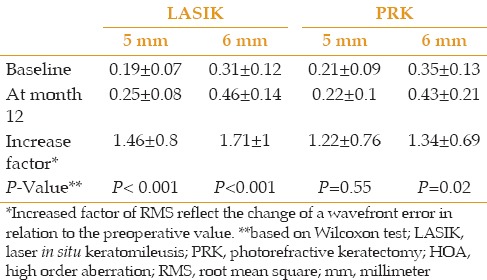
Table 3.
Mean changes of wavefront data (6 mm)
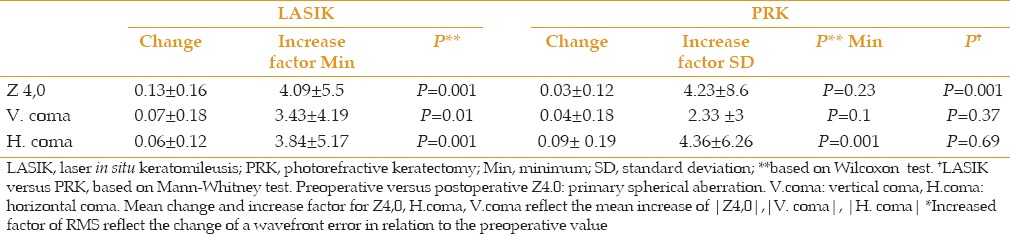
Figure 2a.
Changes of HOAs after PRK (a) and LASIK (b); (RMS: root mean square).
Figure 2b.
Comparison of HOA changes after PRK and LASIK (RMS: root mean square).
Compared to the baseline, induction of vertical coma was significant for 6 mm pupil size in the LASIK group (P = 0.01) but not in the PRK group (P = 0.10). The change in the vertical coma did not significantly differ between the two groups (P = 0.37). In both groups, the mean direction of vertical coma was reversed and changed from negative to positive values.
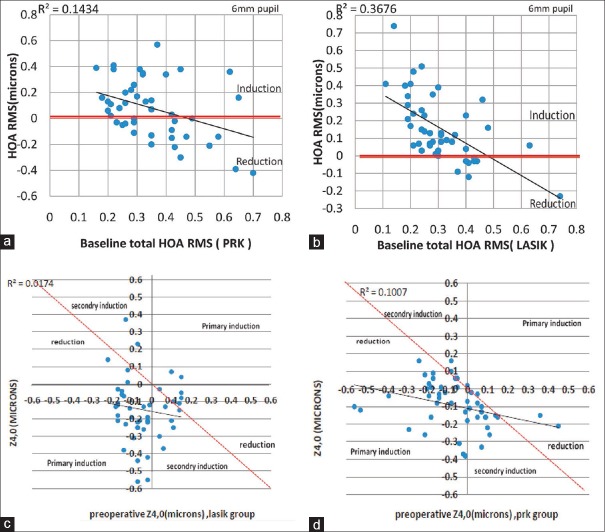
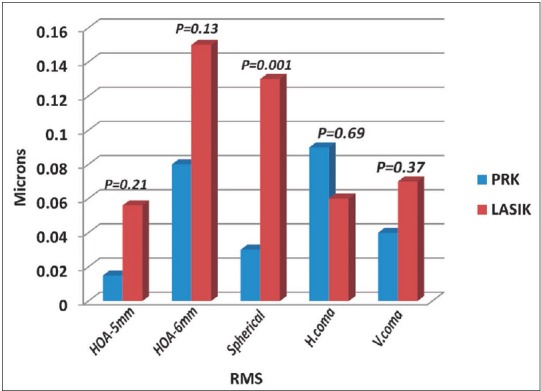
The mean change in total HOA RMS and spherical aberration significantly correlated with its preoperative value in the LASIK and PRK groups (P < 0.001) [Figure 3]. When the preoperative total HOA for 6 mm pupil size was <0.29 μm, the mean change of total HOA was 0.13 ± 0.15 μm and 0.23 ± 0.18 μm in the PRK and LASIK groups, respectively (P = 0.02). When preoperative total HOA for 6 mm pupil size was ≥0.29 μm, the mean change was 0.05 ± 0.25 μm and 0.06 ± 0.13 μm in the PRK and LASIK groups, respectively (P = 0.73).
Figure 3.
Change (Δ) in higher order aberrations as a function of its preoperative value for the 6 mm pupil. (a) the total HOA RMS of PRK group; (b) the total HOA RMS of LASIK group; (c) spherical aberration of LASIK group; (d) spherical aberration of PRK group.
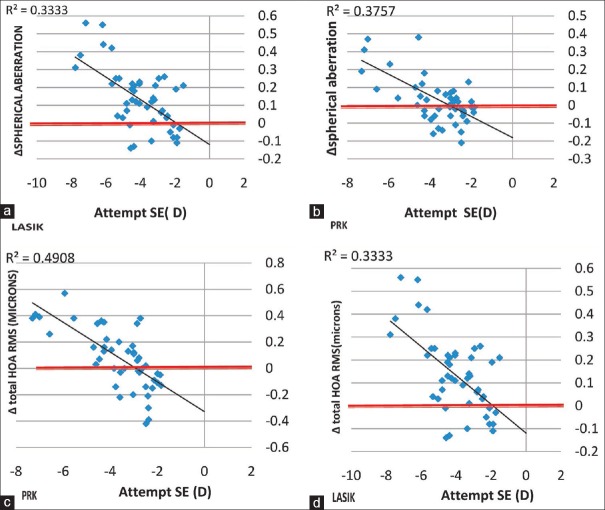
Influential factors on total HOA RMS including attempted correction, preoperative sphere, cylinder, and optical zone were assessed using multiple stepwise regression analysis. These factors accounted for 51% (R2 = 0.51) and 42% (R2 = 0.42) of the variance of changes in total HOA RMS for 6 mm pupil zone in the PRK and LASIK groups, respectively. For the change of spherical aberration and influential factors, R2 value was 0.041 and 0.039 for the PRK and LASIK groups, respectively. For the change of horizontal coma, 42% (R2 = 0.42) and 16% (R2 = 0.16) of the variance could be explained by the influential factors in the PRK and LASIK groups, respectively. R2 value, correlation between the vertical coma and influential factors, was lower for vertical coma (0.16 for PRK and 0.15 for LASIK groups). The linear regression analysis revealed that the attempted SE significantly affected the increase in the postoperative spherical aberration (b = 0.60; P < 0.001), total HOA RMS (b = 0.70; P < 0.001) [Figure 4], horizontal coma, (b = 0.36; P < 0.001), and vertical coma (b = 0.35; P < 0.01) in the PRK group. Attempted SE also significantly affected the increase in postoperative spherical aberration (b = 0.54; P < 0.001), total HOA RMS (b = 0.57; P < 0.001), vertical coma (b = 0.31; P = 0.02), but not horizontal coma (b = 0.14; P = 0.18) in the LASIK group [Figure 4].
Figure 4.
Change in total HOA RMS and spherical aberration as a function of the attempted spherical equivalent in both PRK (b and c) and LASIK (a and d) groups.
DISCUSSION
Corneal wavefront profiles provide important information regarding the optical quality of vision. It is generally believed that wavefront-guided refractive surgery can decrease the amount of HOAs. Several studies[19,20] have also demonstrated better visual outcomes with wavefront-guided PRK and wavefront-guided LASIK than with respective comes back to the conventional platforms (PRK and wavefront-guided LASIK); nonetheless, the increase in HOA is still a concern even with customized ablations.[21,22] According to our results, both personalized Zyoptix PRK and LASIK significantly increased the total HOA RMS for a 6 mm pupil size. The increase was 1.71 for 6 mm pupil size which is similar to that reported by Moshirfar et al (1.74) and slightly more than that was reported by Kohnen et al (1.52).[17,22]
Our results demonstrated that the mean change of total HOA between wavefront-guided PRK and wavefront-guided LASIK was not statistically significant for both pupil sizes although each technique had different influences on Zernike coefficients. To the best of our knowledge, few studies have compared wavefront-guided PRK and wavefront-guided LASIK. Our results were in contrast to a previous study by Moshirifar et al who showed that wavefront-guided PRK induced fewer HOAs than wavefront-guided LASIK.[22] In a bilateral prospective randomized clinical trial, Wallau and Campos also showed a lower mean HOA in the PRK eyes compared with the LASIK eyes.[23] The difference observed between our study and the above-mentioned studies can be explained by the follow-up period which was longer in our study (12 months) than their studies (6 months). Manche et al showed that wavefront-guided LASIK was superior to wavefront-guided PRK with respect to the increase in total HOAs at postoperative month 1. At 3 months postoperatively, however, this difference was not statistically significant.[5] In a prospective, comparative, contralateral study, Hatch et al did not find a significant difference between PRK and thin-flap LASIK in terms of the increase in HOA.[24] The absence of postoperative pain and rapid visual recovery are the advantages for LASIK. PRK eliminates complications related to the corneal flap and reduces the risk of iatrogenic ectasia. The results of the present study and other studies indicate that PRK and LASIK are comparable in visual outcomes and alterations in HOAs.[22,25] These features make PRK a more favorable refractive procedure. In our study, spherical aberration was induced more for LASIK eyes compared to PRK eyes.
In the present study, spherical aberration was shifted to a negative value after LASIK and PRK. In the LASIK group, the total HOA RMS for a 6 mm pupil reduced or remained unchanged in 20% of the eyes. This rate is similar to the rate (20.6%) previously reported by Kohnen et al.[17] The total HOA RMS for 5 and 6 mm pupil sizes reduced or remained unchanged in more proportion of eyes that underwent PRK compared to those that received LASIK. These outcomes can be attributed to the creation of the LASIK flap and its effect on induction of aberrations.
Our results showed that the change in total HOA RMS had a significant correlation with its preoperative value; the lower the preoperative HOA RMS, the higher increase in the postoperative value. When preoperative total HOA RMS was <0.29 μm, the mean change in total HOA RMS was 0.13 ± 0.15 μm and 0.23 ± 0.18 μm in the PRK and LASIK groups, respectively. However, when for baseline total HOA RMS was ≥0.29 μm, the change was not statistically significant. Considering patients with higher preoperative HOA values, Kirwan et al compared HOA after conventional LASIK and laser epithelial keratomileusis for myopia and found a 13.8% decrease in HOA after conventional LASIK and a 48.5% decrease in HOA after laser-assisted subepithelial keratectomy.[26] Other studies using other platforms reported similar results.[27] Although these studies did not involve wavefront-guided PRK, the findings suggested that wavefront-guided technology provides the greatest benefit for patients with larger preoperative HOA values.
Moshirifar et al also stratified the preoperative total HOA RMS values to <0.2 μm, between 0.2 and 0.4 μm, and >0.4 μm and reported no decrease or increase trend in postoperative total HOA RMS based on the preoperative values.
When we classified our patients based on the preoperative total HOA, we found a significant association between the change of total HOA RMS and its preoperative value. This may reflect either the effect of different ablation depths on HOAs or better ability of personalized ablation to correct HOA in patients with preoperative high amounts of HOA. In fact, wavefront-guided ablation induces some amount of new HOAs and corrects some amount of preexisting HOAs. In patients with lower baseline total HOA, the net effect was an increase in the postoperative HOA value, and more induction of new HOAs than correction of baseline HOAs. In patients with higher preoperative HOA values, the net effect was no significant change in the postoperative HOA values.
Multiple stepwise regression analysis showed that the influential factors including attempted correction, preoperative sphere, cylinder, and optical zone only predicted 51% and 42% of the variance of change in total higher aberration for 6mm pupil for the PRK and LASIK groups, respectively. The contribution of spherical aberration, horizontal and vertical coma, was even lower. This means that other factors such as decentered ablation, flap reconstruction, wound healing, and epithelial hyperplasia may influence these changes. In addition, inconstant laser fluence per pulse and potential misalignment of measurement and treatment may contribute to undercorrection and induction of aberrations.[3,17,26,28] Zywave measures 70–78 point in the pupil area. This means that each measured point has a surface area of nearly 0.50 mm² for a 6 mm pupil zone, but laser spot size is 1 mm².[26] This spot size is not fine for ablation and, therefore, undercorrection or induction of aberrations may occur. R2 value was lower for vertical and horizontal coma than spherical aberration. These findings uncover the fact that factors may exist which affect more on coma induction such as decentered ablation and corneal dehydration. Low coma R2 value for LASIK compared to its PRK value suggests that coma may be induced mainly as a function of factors related to flap creation and its possible complications such as flap decentration.
According to our results, attempted spherical equivalent correction has had a significant correlation with the change of total HOA RMS. In the majority of the eyes with low myopia, compared to baseline values, total higher order aberration reduced in both LASIK and PRK groups but for the eyes with moderate and high myopia, total HOA increased. A similar change was seen for spherical aberration. In eyes with low myopia correction, spherical aberration was decreased, however, the opposite effect occurred for moderate and high myopic correction. It can be concluded that, slightly steeper slope of the regression line for PRK indicates that the change of HOA and spherical aberration per diopter spherical equivalent (SE) treatment is more predictable than LASIK. This may be due to the flap creation in LASIK. Change in coma aberration is more influenced by the attempted correction in the PRK group. This may again show the effect of flap creation in the LASIK group.
In conclusion, both wavefront-guided LASIK and PRK induce higher order aberrations. For the 5 mm pupil size, the total HOA did not change after wavefront-guided PRK but it increased after wavefront-guided LASIK; for the 6 mm pupil size, both personalized PRK and LASIK led to an increase in the total HOA with no significant difference between the two groups (P = 0.21, P = 0.13 for pupil size of 5 and 6 mm, respectively). Change of total HOA RMS had a significant correlation with its preoperative value for both LASIK and PRK groups. Wavefront-guided treatment was successful for reduction of HOA in low myopia however, new HOAs were induced postoperatively especially in eyes with low preoperative HOA.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
REFERENCES
- 1.Hjortdal JØ, Olsen H, Ehlers N. Prospective randomized study of corneal aberrations 1 year after radial keratotomy or photorefractive keratectomy. J Refract Surg. 2002;18:23–29. doi: 10.3928/1081-597X-20020101-03. [DOI] [PubMed] [Google Scholar]
- 2.Applegate RA, Howland HC, Sharp RP, Cottingham AJ, Yee RW. Corneal aberrations and visual performance after radial keratotomy. J Refract Surg. 1998;14:397–407. doi: 10.3928/1081-597X-19980701-05. [DOI] [PubMed] [Google Scholar]
- 3.Kohnen T, Mahmoud K, Bühren J. Comparison of corneal higher-order aberrations induced by myopic and hyperopic LASIK. Ophthalmology. 2005;112:1692. doi: 10.1016/j.ophtha.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 4.Ivarsen A, Hjortdal J. Seven-year changes in corneal power and aberrations after PRK or LASIK. Invest Ophthalmol Vis Sci. 2012;53:6011–6016. doi: 10.1167/iovs.12-10208. [DOI] [PubMed] [Google Scholar]
- 5.Manche EE, Haw WW. Wavefront-guided laser in situ keratomileusis (Lasik) versus wavefront-guided photorefractive keratectomy (Prk): A prospective randomized eye-to-eye comparison (an American Ophthalmological Society thesis) Trans Am Ophthalmol Soc. 2011;109:201–220. [PMC free article] [PubMed] [Google Scholar]
- 6.Oshika T1, Klyce SD, Applegate RA, Howland HC, El Danasoury MA. Comparison of corneal wavefront aberrations after photorefractive keratectomy and laser in situ keratomileusis. Am J Ophthalmol. 1999;127:1–7. doi: 10.1016/s0002-9394(98)00288-8. [DOI] [PubMed] [Google Scholar]
- 7.Martínez CE1, Applegate RA, Klyce SD, McDonald MB, Medina JP, Howland HC. Effect of pupillary dilation on corneal optical aberrations after photorefractive keratectomy. Arch Ophthalmol. 1998;116:1053–1062. doi: 10.1001/archopht.116.8.1053. [DOI] [PubMed] [Google Scholar]
- 8.Sharma M, Wachler BS, Chan CC. Higher order aberrations and relative risk of symptoms after LASIK. Refract Surg. 2007;23:252–256. doi: 10.3928/1081-597X-20070301-07. [DOI] [PubMed] [Google Scholar]
- 9.Yamane N, Miyata K, Samejima T, Hiraoka T, Kiuchi T, Okamoto F, et al. Ocular higher-order aberrations and contrast sensitivity after conventional laser in situ keratomileusis. Invest Ophthalmol Vis Sci. 2004;45:3986–3990. doi: 10.1167/iovs.04-0629. [DOI] [PubMed] [Google Scholar]
- 10.Chalita MR, Chavala S, Xu M, Krueger RR. Wavefront analysis in post-LASIK eyes and its correlation with visual symptoms, refraction, and topography. Ophthalmology. 2004;111:447–453. doi: 10.1016/j.ophtha.2003.06.022. [DOI] [PubMed] [Google Scholar]
- 11.Wang Y, Zhao KX, He JC, Jin Y, Zuo T. Ocular higher-order aberrations features analysis after corneal refractive surgery. Chin Med J. 2007;120:269–273. [PubMed] [Google Scholar]
- 12.Endl MJ, Martinez CE, Klyce SD, McDonald MB, Coorpender SJ, Applegate RA, et al. Effect of larger ablation zone and transition zone on corneal optical aberrations after photorefractive keratectomy. Arch Ophthalmol. 2001;119:1159–1164. doi: 10.1001/archopht.119.8.1159. [DOI] [PubMed] [Google Scholar]
- 13.McAlinden C, Moore JE. Comparison of higher order aberrations after LASIK and LASEK for myopia. J Refract Surg. 2010;26:45–51. doi: 10.3928/1081597X-20101215-07. [DOI] [PubMed] [Google Scholar]
- 14.Waheed S, Chalita MR, Xu M, Krueger RR. Flap-induced and laser-induced ocular aberrations in a two-step LASIK procedure. J Refract Surg. 2005;21:346–352. doi: 10.3928/1081-597X-20050701-08. [DOI] [PubMed] [Google Scholar]
- 15.Buzzonetti L, Petrocelli G, Valente P, Tamburrelli C, Mosca L, Laborante A, et al. Comparison of corneal aberration changes after laser in situ keratomileusis performed with mechanical microkeratome and IntraLase femtosecond laser: 1-year follow-up. Cornea. 2008;27:174–179. doi: 10.1097/ICO.0b013e31815a50bf. [DOI] [PubMed] [Google Scholar]
- 16.Subbaram MV, MacRae S, Slade SG, Durrie DS. Customized LASIK treatment for myopia: Relationship between preoperative higher order aberrations and refractive outcome. J Refract Surg. 2006;22:746–753. doi: 10.3928/1081-597X-20061001-04. [DOI] [PubMed] [Google Scholar]
- 17.Kohnen T, Bühren J, Kühne C, Mirshahi A. Wavefront-guided LASIK with the Zyoptix 3.1 system for the correction of myopia and compound myopic astigmatism with 1-year follow-up: Clinical outcome and change in higher order aberrations. Ophthalmology. 2004;111:2175–2185. doi: 10.1016/j.ophtha.2004.06.027. [DOI] [PubMed] [Google Scholar]
- 18.Randleman JB, Perez-Straziota CE, Hu MH, White AJ, Loft ES, Stulting RD. Higher-order aberrations after wavefront-optimized photorefractive keratectomy and laser in situ keratomileusis. J Cataract Refract Surg. 2009;35:260–264. doi: 10.1016/j.jcrs.2008.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wigledowska-Promienska D, Zawojska I. Changes in higher order aberrations after wavefront-guided PRK for correction of low to moderate myopia and myopic astigmatism: Two-year follow-up. Eur J Ophthalmol. 2007;17:507–514. doi: 10.1177/112067210701700405. [DOI] [PubMed] [Google Scholar]
- 20.Zhang J, Zhou YH, Wang NL, Li R. Comparison of visual performance between conventional LASIK and wavefront-guided LASIK with iris-registration. Chin Med J. 2008;121:137–142. [PubMed] [Google Scholar]
- 21.Smadja D, Santhiago MR, Mello GR, Touboul D, Mrochen M, Krueger RR. Corneal higher order aberrations after myopic wavefront-optimized ablation. J Refract Surg. 2013;29:42–48. doi: 10.3928/1081597X-20121210-03. [DOI] [PubMed] [Google Scholar]
- 22.Moshirfar M, Schliesser JA, Chang JC, Oberg TJ, Mifflin MD, Townley R, et al. Visual outcomes after wavefront-guided photorefractive keratectomy and wavefront-guided laser in situ keratomileusis: Prospective comparison. J Cataract Refract Surg. 2010;36:1336–1343. doi: 10.1016/j.jcrs.2010.02.012. [DOI] [PubMed] [Google Scholar]
- 23.Wallau AD, Campos M. Photorefractive keratectomy with mitomycin C versus LASIK in custom surgeries for myopia: A bilateral prospective randomized clinical trial. J Refract Surg. 2008;24:326–336. doi: 10.3928/1081597X-20080401-03. [DOI] [PubMed] [Google Scholar]
- 24.Hatch BB1, Moshirfar M, Ollerton AJ, Sikder S, Mifflin MD. A prospective, contralateral comparison of photorefractive keratectomy (PRK) versus thin-flap LASIK: Assessment of visual function. Clin Ophthalmol. 2011;5:451–457. doi: 10.2147/OPTH.S18967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shortt AJ, Allan BDS. Photorefractive keratectomy (PRK) versus laser-assisted in-situ keratomileusis (LASIK) for myopia. Cochrane Database Syst Rev. 2006 doi: 10.1002/14651858.CD005135.pub2. CD005135. [DOI] [PubMed] [Google Scholar]
- 26.Kirwan C, O’Keefe M. Comparative study of higher-order aberrations after conventional laser in situ keratomileusis and laser epithelial keratomileusis for myopia using the Technolas 217z laser platform. Am J Ophthalmol. 2009;147:77–83. doi: 10.1016/j.ajo.2008.07.014. [DOI] [PubMed] [Google Scholar]
- 27.Schallhorn SC1, Farjo AA, Huang D, Boxer Wachler BS, Trattler WB, Tanzer DJ, et al. Wavefrontguided LASIK for the correction of primary myopia and astigmatism; a report by the American Academy of Ophthalmology (Ophthalmic Technology Assessment) Ophthalmology. 2008;115:1249–1261. doi: 10.1016/j.ophtha.2008.04.010. [DOI] [PubMed] [Google Scholar]
- 28.Nuijts RM, Nabar VA, Hament WJ, Eggink FA. Wavefront-guided versus standard laser in situ keratomileusis to correct low to moderate myopia. J Cataract Refract Surg. 2002;28:1907–1913. doi: 10.1016/s0886-3350(02)01511-0. [DOI] [PubMed] [Google Scholar]