Abstract
Introduction
Many college students engage in nonmedical use of prescription stimulants (NPS) because they believe it provides academic benefits, but studies are lacking to support or refute this belief.
Methods
Using a longitudinal design, 898 undergraduates who did not have an ADHD diagnosis were studied. Year 3 GPA (from college records) of four groups was compared: Abstainers (did not engage in NPS either year; 68.8%); Initiators (NPS in Year 3 but not Year 2; 8.7%); Desisters (NPS in Year 2 but not Year 3; 5.8%); and Persisters (NPS in both years; 16.7%). Generalized estimating equations regression was used to estimate the association between NPS and change in GPA, controlling for sex and Year 2 GPA.
Results
GPA increased significantly within Abstainers (p<.05), but did not change significantly within the other groups. Overall, the relationship between NPS pattern group and change in GPA was not statistically significant (p=.081). NPS was generally infrequent, but Persisters used more frequently than Desisters (11.7 versus 3.4 days in Year 2) and Initiators (13.6 versus 4.0 days in Year 3, both ps<.001), controlling for sex and Year 2 GPA.
Conclusions
We cannot rule out the possibility that NPS prevented declines in GPA, but we can conclude that students who engaged in NPS showed no increases in their GPAs and gained no detectable advantages over their peers. The results suggest that prevention and intervention strategies should emphasize that the promise of academic benefits from NPS is likely illusory.
Keywords: Academic performance, College students, drug abuse, prescription drug abuse, substance use
1. Introduction
Prescription stimulants such as Adderall® or Ritalin® are beneficial for the treatment of Attention-deficit/hyperactivity disorder (ADHD; Chavez et al., 2009; Faraone, Biederman, Spencer, & Aleardi, 2006; Pliszka, 2005; Wilens, 2006). Clinical trials of such drugs utilizing samples of adolescents with ADHD have demonstrated improvements in attention and decreased hyperactivity symptoms (Bostic et al., 2000; Chan, Fogler, & Hammerness, 2016; Wilens et al., 2006). Even better results have been obtained from combining pharmacologic therapies with behavioral strategies to improve classroom behavior and schoolwork completion (Fabiano et al., 2007).
Nonmedical use of prescription stimulants (NPS) occurs when these medications are taken without having a prescription or in a way that is inconsistent with a physician’s orders. NPS has been the topic of a wide variety of studies in recent years, although NPS by college students was documented as early as 1937 (Rasmussen, 2006). The prevalence of NPS varies by age, with the highest estimates of use reported for college students (Substance Abuse and Mental Health Services Administration, 2015; Wilens et al., 2008). National data from 2015 estimate that 10.7% of college students used Adderall® nonmedically during the past year (Miech, Johnston, O'Malley, Bachman, & Schulenberg, 2016). Prevalence estimates of lifetime NPS vary widely from 5.3% to 33.8% across studies of college students (DeSantis, Webb, & Noar, 2008; DuPont, Coleman, Bucher, & Wilford, 2008; Weyandt et al., 2013), owing in part to the characteristics of the schools studied, the demographic composition of the samples, and the methods used to assess nonmedical use.
One finding that is highly consistent across all studies of college students is that the primary motive for NPS is to improve academic performance. Students report that NPS is driven by study motives, such as increasing the ability to concentrate while studying or by increasing the amount of time they can sustain focus (DuPont et al., 2008; Garnier-Dykstra, Caldeira, Vincent, O'Grady, & Arria, 2012; Rabiner et al., 2009; Teter, McCabe, Cranford, Boyd, & Guthrie, 2005; Teter, McCabe, LaGrange, Cranford, & Boyd, 2006). Whether or not these purported changes in attention and focus while studying results in better performance on tests has not been examined in real-world settings.
The belief that these drugs can improve cognitive skills among individuals without ADHD is widespread among college students and has been in large part perpetuated by extensive attention in the popular media on neuroenhancement, calling the drugs “smart drugs,” “smart pills,” or “brain steroids” (Forlini & Racine, 2009; Partridge, Bell, Lucke, Yeates, & Hall, 2011). Several recent reviews of the literature have called into question cognitive performance benefits of these drugs for non-ADHD individuals (Advokat, 2010; Hall & Lucke, 2010; Repantis, Schlattmann, Laisney, & Heuser, 2010). Experimental studies have shown little benefit of these drugs over placebo among those without an ADHD diagnosis (Advokat, 2010; Chamberlain et al., 2011; Ilieva, Boland, & Farah, 2013; Volkow et al., 2008). For example, Volkow and colleagues (2008) tested the hypothesis that stimulant medication (methylphenidate) reduces cerebral activity by increasing efficiency utilizing a balanced placebo design. The results suggest that when neuronal resources are optimally distributed, stimulants might actually result in deterioration in performance.
In addition to experimental studies that have cast doubt on the benefits of NPS, several cross- sectional studies have observed that college students who engage in NPS have lower grade point averages (GPA), skip more classes, and have higher levels of other drug use and excessive drinking than non-users (Arria, O'Grady, Caldeira, Vincent, & Wish, 2008b; McCabe, Knight, Teter, & Wechsler, 2005; Rabiner et al., 2009; Teter, McCabe, Boyd, & Guthrie, 2003). Longitudinal research has demonstrated that marijuana and alcohol use are related to increases in skipping class and decreases in GPA (Arria et al., 2008b; Rabiner et al., 2009), and that NPS appears to be a compensatory “last ditch” attempt to improve grades among individuals who are experiencing such declines in academic performance (Arria et al., 2013b).
Although research has shown that students who engage in NPS have lower grades than non-users, the question that remains is whether or not they are, in fact, obtaining better grades than they would have if they did not engage in NPS. Farah and colleagues (2014) emphasize the lack of data from real-world investigations that examine the relationship between NPS and purported enhanced cognitive performance.
The purpose of this study was to examine prospectively the possible association between NPS and GPA. Our approach was to examine longitudinal changes in college GPA using a within-subjects design. Two consecutive years of data were used. We sought to test two hypotheses: (1) that students might increase their GPA after starting NPS (Initiators), relative to their counterparts who abstain from NPS (Abstainers), and (2) that students might experience a drop in GPA after stopping NPS (Desisters), relative to their counterparts who continue NPS (Persisters). Based on prior research, our prediction was that no improvements in GPA would be observed among Initiators and that no declines in GPA would be observed among Desisters. Because stimulant medications are thought to affect individuals differentially depending on whether or not they have ADHD (Chamberlain et al., 2011), we elected to focus our analyses on the subset of students who had never been diagnosed with ADHD.
2. Methods
2.1. Study design
The study uses data from the second and third annual assessments of the College Life Study, a longitudinal prospective study that began assessing a cohort of 1,253 individuals in 2004 during their first year of college at one large public university (Arria et al., 2008a; Vincent et al., 2012). Individuals who had used an illicit drug or nonmedically used a prescription drug at least once during high school were oversampled based on their responses to a pre-college survey (N=3,401, 89% response rate), in order to ensure adequate statistical power for analyses of drug use during college. Eligibility was restricted to first-time, first-year students 17 to 19 years of age at college entry. Each annual assessment consisted of a two-hour interview and self-administered questionnaires measuring substance use and other health-related constructs. The response rate at baseline was 87% (n=1,253), and high follow-up rates were achieved in both Years 2 (91%; n=1,142) and 3 (88%; n=1,101). Participants were paid for each assessment. Informed consent was obtained for the study and specifically to collect GPA from school records rather than self-report. All study procedures were approved by the university’s IRB, and participants received further protections under a federal Certificate of Confidentiality.
2.2. Participants
The analysis sample was first restricted to the 975 individuals who were still enrolled at the home university by Year 3 and had valid data on GPA from both years. The 77 individuals who had been diagnosed with ADHD by their Year 3 assessment were excluded, leaving a final sample size of 898. The inclusion sample was not significantly different from the rest of the overall sample (N=1,253) with respect to race or parental education, but was slightly under-representative of men (46% vs. 54%, p=.01).
2.3. Measures
2.3.1. GPA change
For each semester (i.e., fall, spring), the number of credit hours and GPA were obtained from the registrar’s office, as allowed by participants’ informed consent. For each individual, annual GPA was then computed by averaging the two semester GPA values, after weighting them for the number of credit hours. GPA values of zero were treated as missing because they were indistinguishable from placeholders that were automatically assigned to students whose grades were incomplete or were studying abroad. In cases where only one valid semester GPA (i.e., non-zero value) was available for a given year, the non-missing value was used as the annual GPA; this affected 22 individuals in Year 2 and 138 in Year 3, corresponding to the typical timing of study abroad experiences. Finally, GPA change scores were computed as the difference between the two annual GPA values. A small number of outliers (n=3) whose GPA increased or decreased by 2.0 or more were excluded from further analyses.
2.3.2. NPS pattern groups
In Years 2 and 3, participants were asked how many days during the past year they had used any prescription stimulant nonmedically using standard measures from national surveys (Substance Abuse and Mental Health Services Administration, 2003). Longitudinal NPS patterns were operationalized as a four-level categorical variable based on whether or not NPS occurred at least once during each year: Abstainers (used neither year), Initiators (used Year 3 but not Year 2), Desisters (used Year 2 but not Year 3), and Persisters (used both years).
2.3.3. Background characteristics
Sex was coded as observed at baseline. Race and ethnicity were self-reported in Year 3 (allowing for endorsement of multiple categories) and later dichotomized as non-Hispanic white versus all others. Parents’ highest educational attainment was self-reported at baseline. Neighborhood income was abstracted from publicly available data on the mean adjusted gross income corresponding to the ZIP code of participants’ parental home during their last year of high school (MelissaDATA, 2003).
2.4. Statistical analysis
First, descriptive statistics were computed within the four NPS pattern groups and the overall sample (Table 1). Bivariate associations with NPS pattern group membership were evaluated using chi-square tests of independence for categorical variables and one-way ANOVA for scale and count variables (Table 1). GPA change scores were analyzed using a generalized estimating equations (GEE) regression to obtain estimated marginal means for the four NPS pattern groups, controlling for sex and Year 2 GPA (Table 2).
Table 1.
Sample characteristics, by nonmedical use of prescription stimulants (NPS) pattern group.
| Overall (N=898) |
NPS pattern group |
|||||
|---|---|---|---|---|---|---|
| Abstainers (n=618) |
Initiators (n=78) |
Desisters (n=52) |
Persisters (n=150) |
p | ||
|
|
||||||
| % Male | 46.3 | 43.5 | 50.0 | 48.1 | 55.3 | .062 |
| % White | 72.8 | 69.4 | 83.3 | 65.4 | 84.0 | .004 |
| % with college- educated parent(s) |
85.8 | 84.2 | 87.8 | 93.8 | 88.4 | .197 |
| Mean (SD) neighborhood income in high school in $10K |
7.3 (3.3) | 7.1 (3.1) | 7.8 (4.0) | 8.4 (4.0) | 7.7 (3.4) | .004 |
| Mean (SD) frequency of NPS |
||||||
| Year 2 | 9.5 (13.5) | -- | -- | 3.4 (3.8) | 11.7 (15.0) | <.001 |
| Year 3 | 10.3 (13.4) | -- | 4.0 (4.2) | -- | 13.6 (15.3) | <.001 |
| Mean (SD) Annual GPA | ||||||
| Year 2 | 3.2 (0.6) | 3.3 (0.6) | 3.2 (0.6) | 3.3 (0.5) | 3.1 (0.6) | .015 |
| Year 3 | 3.3 (0.6) | 3.3 (0.6) | 3.2 (0.6) | 3.3 (0.5) | 3.1 (0.6) | <.001 |
Note. Annual GPA was computed for individuals with GPA>0.0 in at least one semester of a given year. P-values are reported for overall Χ2 tests for categorical variables, and for one-way ANOVA tests for scale variables.
Table 2.
Estimated marginal means for change in GPA from Year 2 to Year 3, by nonmedical use of prescription stimulants (NPS) pattern group.
| Adjusted Estimates |
|||||
|---|---|---|---|---|---|
| NPS pattern group | n | Mean | SE | 95% Confidence Interval | |
| Lower | Upper | ||||
| Abstainers | 618 | .0529 | .01563 | .0223 | .0836 |
| Initiators | 78 | −.0249 | .04377 | −.1107 | .0609 |
| Desisters | 52 | .0157 | .05357 | −.0893 | .1207 |
| Persisters | 150 | −.0248 | .03165 | −.0868 | .0373 |
| Overall | 898 | .0048 | .01940 | −.0333 | .0428 |
Note. Results adjusted for Year 2 GPA and sex. Overall Wald Χ2 (df) p for the NPS pattern variable was not statistically significant [6.726 (3) .081].
3. Results
Two-thirds of the sample (n=618, 68.8%) never engaged in NPS in either Year 2 or Year 3, and were classified as Abstainers. Among those who did engage in NPS (n=280), more than half did so during both years (n=150, 53.6%) and were classified as Persisters, representing 16.7% of the overall sample. The rest of the sample were classified as Initiators (8.7%, n=78) or Desisters (5.8%, n=52) because they engaged in NPS during one year but not the other.
NPS pattern group membership was significantly associated with race and neighborhood income, (both ps<.05; see Table 1). White individuals were overrepresented among Initiators and Persisters. Neighborhood incomes tended to be higher among the three NPS groups than the Abstainers. NPS pattern group membership was not significantly associated with sex or parents’ education.
Not surprisingly, NPS tended to be more frequent for individuals who persisted in the behavior relative to those who only engaged in NPS during one year or the other. For example, in Year 2 when both Persisters and Desisters were engaging in NPS, the Desisters used significantly less often (3.4 versus 11.7 days). Similarly, in Year 3, Persisters and Initiators were all engaging in NPS, yet Initiators used significantly less often (4.0 versus 13.6 days, both ps<.001).
After adjusting for sex and Year 2 GPA, there was no significant association between NPS pattern group membership and change in GPA (overall Χ2(3)=6.7, p>.08; see Table 2). Based on the results of a single-sample t test, small but statistically significant improvements in GPA were evident in the Abstainers (mean=.05, 95% CI=.02 to .08; see Figure 1), but GPA changes were not significantly different from zero in any of the other three NPS pattern groups or among the overall sample. Average change in GPA was lowest in the Persisters and Initiators (both means=−.025), with the Desisters in an intermediate position (.016).
Fig 1.
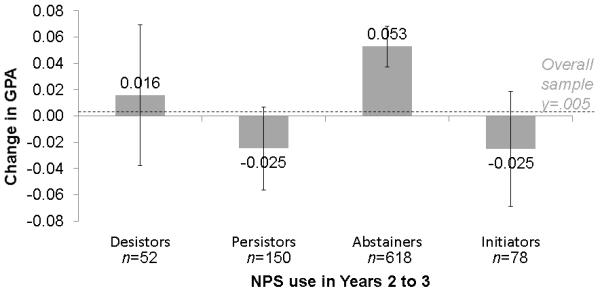
Estimated marginal means and standard error bars for change in GPA during Years 2 to 3 of college, by nonmedical use of prescription stimulants (NPS) pattern group (n=898)
Note. Sample is restricted to individuals who were never diagnosed with ADHD by Year 3. Change in GPA is computed as the difference between Year 3 GPA and Year 2 GPA, which were averaged from semesters 3-4 and 5-6, respectively. Results are adjusted for the effects of sex and Year 2 GPA. Normal distribution was assumed for GPA change score. Zero values for semester GPA were treated as missing because they cannot be distinguished from missing data due to studying abroad.
4. Discussion
The present study sought to examine whether NPS results in improvements in GPA using a longitudinal sample of second and third year college students. An important strength of the study is the use of administrative data on GPA from university records, which are not susceptible to bias related to recall or social desirability. Findings are also strengthened by the high follow-up rates (>87% annually) achieved in Years 2 and 3 of the study.
No statistically significant improvement in GPA was observed in association with either starting NPS or continuing NPS relative to individuals who did not engage in NPS in either year or relative to individuals who stopped engaging in NPS. To the contrary, GPA appeared to increase significantly from Year 2 to 3 within the group who abstained from NPS during both years. Among this cohort, the majority of students did not engage in NPS, although those who did tended to persist in this behavior across both study years. NPS pattern group membership was positively associated with race (non-Hispanic white) and neighborhood income, but not sex or parents’ educational attainment. Moreover, frequency of NPS was generally low, but was significantly more frequent among the Persisters than Desisters or Initiators.
Prior studies among both this sample and other samples have shown that NPS usually manifests as part of a broader pattern of polysubstance use (Arria et al., 2013b; Garnier-Dykstra et al., 2012; Sweeney, Sembower, Ertischek, Shiffman, & Schnoll, 2013). This study was focused on providing a very basic description of the relationship between NPS and changes in GPA. As such, we deliberately did not examine other substance use in relation to GPA changes. Our prior research using longitudinal modeling has shown that increasing marijuana use is associated prospectively with GPA declines, and that skipping class is an important mediator of that relationship, even after adjustment for other potentially confounding variables (Arria, Caldeira, Bugbee, Vincent, & O'Grady, 2015). Other studies by our investigative team have reported that students who engage in NPS as a study aid tended to exhibit a pattern of declines in both class attendance and grades that was associated with their increasing alcohol and marijuana problems (Arria et al., 2013b). The present study extends our prior work by using a within-subjects design to examine changes in GPA associated with starting, stopping, or continuing NPS relative to students who abstain during the course of one year in college.
The present findings confirm and extend prior experimental studies that show little to no benefit to cognitive performance associated with prescription stimulants when administered to individuals who do not have a diagnosis of ADHD. Interestingly, some research supports that there might be a “placebo effect” associated with NPS (Ilieva et al., 2013; Looby & Earleywine, 2011). Ilieva, et al., (2013) observed that individuals believed that their cognitive performance was enhanced when they received a stimulant, relative to placebo, even though the effects on their performance were small. Similarly, Looby and Earleywine (2011) found that individuals felt subjectively more stimulated when administered a stimulant, relative to when receiving a placebo, but did not perform differently on cognitive tests. Further research is needed to examine how expectancies might play a role in improving academic performance.
Findings must be interpreted in the context of the study’s limitations. By definition, changes in GPA could not be evaluated for individuals who experienced significant gaps in their college enrollment (i.e., not enrolled for two or more consecutive semesters), dropped out, or were missing GPA data because they transferred to a different institution. We adopted a conservative approach by disregarding zero values for GPA as missing, and excluding three individuals with extreme changes in GPA (i.e., >∣2.0∣). Therefore, the sample represents a population of relatively high-functioning college students, and excludes individuals with the most severe academic problems such as academic failure, discontinuous enrollment, and dropout. Although the observed differences in GPA were relatively small in this study, it is plausible that NPS might be associated with more severe problems, especially given our prior findings that other forms of substance use predicted discontinuous enrollment among this sample (Arria et al., 2013a). Moreover, GPA is likely to be influenced by numerous factors that could not be accounted for in this study, such as major, adjustment to college life, mental health issues, and study skills. Future studies should expand to include such variables in their analysis. Another limitation is that, because participants were recruited from one university, generalizability to students at other types of institutions might be limited.
It is both timely and critical to conduct research to identify and test the efficacy of both prevention and intervention strategies addressing NPS using randomized controlled trials, ideally conducted across different types of college and university settings. The present findings highlight the need to incorporate information about the illusory nature of the putative academic benefit of NPS into interventions to reduce NPS. Reducing concomitant substance use among students that engage in NPS should be a central piece of intervention strategies to improve academic performance. NPS appears to be a maladaptive response to academic difficulties, especially given the present findings that NPS does not appear to confer benefit.
Abbreviations
- NPS
nonmedical use of prescription stimulants
- GPA
grade point average
References
- Advokat C. What are the cognitive effects of stimulant medications? Emphasis on adults with attention-deficit/hyperactivity disorder (ADHD) Neurosci Biobehav Rev. 2010;34(8):1256–1266. doi: 10.1016/j.neubiorev.2010.03.006. [DOI] [PubMed] [Google Scholar]
- Arria AM, Caldeira KM, Bugbee BA, Vincent KB, O'Grady KE. The academic consequences of marijuana use during college. Psychol Addict Behav. 2015;29(3):564–575. doi: 10.1037/adb0000108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arria AM, Caldeira KM, O'Grady KE, Vincent KB, Fitzelle DB, Johnson EP, Wish ED. Drug exposure opportunities and use patterns among college students: Results of a longitudinal prospective cohort study. Subst Abus. 2008a;29(4):19–38. doi: 10.1080/08897070802418451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arria AM, Garnier-Dykstra LM, Caldeira KM, Vincent KB, Winick ER, O’Grady KE. Drug use patterns and continuous enrollment in college: Results from a longitudinal study. J Stud Alcohol Drugs. 2013a;74(1):71–83. doi: 10.15288/jsad.2013.74.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arria AM, O'Grady KE, Caldeira KM, Vincent KB, Wish ED. Nonmedical use of prescription stimulants and analgesics: Associations with social and academic behaviors among college students. J Drug Issues. 2008b;38(4):1045–1060. doi: 10.1177/002204260803800406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arria AM, Wilcox HC, Caldeira KM, Vincent KB, Garnier-Dykstra LM, O’Grady KE. Dispelling the myth of “smart drugs”: Cannabis and alcohol use problems predict nonmedical use of prescription stimulants for studying. Addict Behav. 2013b;38(3):1643–1650. doi: 10.1016/j.addbeh.2012.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostic JQ, Biederman J, Spencer TJ, Wilens TE, Prince JB, Monuteaux MC, Sienna M, Polisner DA, Hatch M. Pemoline treatment of adolescents with attention deficit hyperactivity disorder: A short-term controlled trial. J Child Adolesc Psychopharmacol. 2000;10(3):205–216. doi: 10.1089/10445460050167313. [DOI] [PubMed] [Google Scholar]
- Chamberlain SR, Robbins TW, Winder-Rhodes S, Müller U, Sahakian BJ, Blackwell AD, Barnett JH. Translational approaches to frontostriatal dysfunction in attention-deficit/hyperactivity disorder using a computerized neuropsychological battery. Biol Psychiatry. 2011;69(12):1192–1203. doi: 10.1016/j.biopsych.2010.08.019. [DOI] [PubMed] [Google Scholar]
- Chan E, Fogler JM, Hammerness PG. Treatment of attention-deficit/hyperactivity disorder in adolescents: A systematic review. JAMA. 2016;315(18):1997–2008. doi: 10.1001/jama.2016.5453. [DOI] [PubMed] [Google Scholar]
- Chavez B, Sopko MA, Jr., Ehret MJ, Paulino RE, Goldberg KR, Angstadt K, Bogart GT. An update on central nervous system stimulant formulations in children and adolescents with attention-deficit/hyperactivity disorder. Ann Pharmacother. 2009;43(6):1084–1095. doi: 10.1345/aph.1L523. [DOI] [PubMed] [Google Scholar]
- DeSantis AD, Webb EM, Noar SM. Illicit use of prescription ADHD medications on a college campus: A multimethological approach. J Am Coll Health. 2008;57(3):315–323. doi: 10.3200/JACH.57.3.315-324. [DOI] [PubMed] [Google Scholar]
- DuPont RL, Coleman JJ, Bucher RH, Wilford BB. Characteristics and motives of college students who engage in nonmedical use of methylphenidate. Am J Addict. 2008;17(3):167–171. doi: 10.1080/10550490802019642. [DOI] [PubMed] [Google Scholar]
- Fabiano GA, Pelham WE, Gnagy EM, Burrows-Maclean L, Coles EK, Chacko A, et al. The single and combined effects of multiple intensities of behavior modification and methylphenidate for children with attention deficit hyperactivity disorder in a classroom setting. School Psych Rev. 2007;36(2):195–216. [Google Scholar]
- Farah MJ, Smith ME, Ilieva I, Hamilton RH. Cognitive enhancement. Wiley Interdiscip Rev Cogn Sci. 2014;5(1):95–103. doi: 10.1002/wcs.1250. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Biederman J, Spencer TJ, Aleardi M. Comparing the efficacy of medications for ADHD using meta-analysis. MedGenMed. 2006;8(4):4–4. [PMC free article] [PubMed] [Google Scholar]
- Forlini C, Racine E. Disagreements with implications: Diverging discourses on the ethics of non-medical use of methylphenidate for performance enhancement. BMC Med Ethics. 2009;10(1):1–13. doi: 10.1186/1472-6939-10-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garnier-Dykstra LM, Caldeira KM, Vincent KB, O'Grady KE, Arria AM. Nonmedical use of prescription stimulants during college: Four-year trends in exposure opportunity, use, motives, and sources. J Am Coll Health. 2012;60(3):226–234. doi: 10.1080/07448481.2011.589876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall WD, Lucke JC. The enhancement use of neuropharmaceuticals: More scepticism and caution needed. Addiction. 2010;105(12):2041–2043. doi: 10.1111/j.1360-0443.2010.03211.x. [DOI] [PubMed] [Google Scholar]
- Ilieva I, Boland J, Farah MJ. Objective and subjective cognitive enhancing effects of mixed amphetamine salts in healthy people. Neuropharmacology. 2013;64:496–505. doi: 10.1016/j.neuropharm.2012.07.021. [DOI] [PubMed] [Google Scholar]
- Looby A, Earleywine M. Expectation to receive methylphenidate enhances subjective arousal but not cognitive performance. Exp Clin Psychopharmacol. 2011;19(6):433–444. doi: 10.1037/a0025252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Knight JR, Teter CJ, Wechsler H. Non-medical use of prescription stimulants among US college students: Prevalence and correlates from a national survey. Addiction. 2005;99(1):96–106. doi: 10.1111/j.1360-0443.2005.00944.x. [DOI] [PubMed] [Google Scholar]
- MelissaDATA [Retrieved May 28, 2008];Income tax statistics lookup. 2003 from http://www.melissadata.com/lookups/taxzip.asp.
- Miech RA, Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future: National survey results on drug use, 1975-2015: Volume I: Secondary school students. Institute for Social Research, The University of Michigan; Ann Arbor, MI: 2016. [Google Scholar]
- Partridge BJ, Bell SK, Lucke JC, Yeates S, Hall WD. Smart drugs “as common as coffee”: Media hype about neuroenhancement. PLoS One. 2011;6(11):e28416–e28416. doi: 10.1371/journal.pone.0028416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pliszka SR. The neuropsychopharmacology of attention-deficit/hyperactivity disorder. Biol Psychiatry. 2005;57(11):1385–1390. doi: 10.1016/j.biopsych.2004.08.026. [DOI] [PubMed] [Google Scholar]
- Rabiner DL, Anastopoulos AD, Costello EJ, Hoyle RH, McCabe SE, Swartzwelder HS. Motives and perceived consequences of nonmedical ADHD medication use by college students: Are students treating themselves for attention problems? J Atten Disord. 2009;13(3):259–270. doi: 10.1177/1087054708320399. [DOI] [PubMed] [Google Scholar]
- Rasmussen N. Making the first anti-depressant: Amphetamine in American medicine, 1929–1950. J Hist Med Allied Sci. 2006;61(3):288–323. doi: 10.1093/jhmas/jrj039. [DOI] [PubMed] [Google Scholar]
- Repantis D, Schlattmann P, Laisney O, Heuser I. Modafinil and methylphenidate for neuroenhancement in healthy individuals: A systematic review. Pharmacol Res. 2010;62(3):187–206. doi: 10.1016/j.phrs.2010.04.002. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration . 2002 National Survey on Drug Use and Health Questionnaire. Office of Applied Studies; Rockville, MD: 2003. [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Results from the 2014 National Survey on Drug Use and Health: Detailed tables. US Department of Health and Human Services, Office of Applied Studies; Rockville, MD: 2015. [Google Scholar]
- Sweeney CT, Sembower MA, Ertischek MD, Shiffman S, Schnoll SH. Nonmedical use of prescription ADHD stimulants and preexisting patterns of drug abuse. J Addict Dis. 2013;32(1):1–10. doi: 10.1080/10550887.2012.759858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teter CJ, McCabe SE, Boyd CJ, Guthrie SK. Illicit methylphenidate use in an undergraduate student sample: Prevalence and risk factors. Pharmacotherapy. 2003;23(5):609–617. doi: 10.1592/phco.23.5.609.34187. [DOI] [PubMed] [Google Scholar]
- Teter CJ, McCabe SE, Cranford JA, Boyd CJ, Guthrie SK. Prevalence and motives for illicit use of prescription stimulants in an undergraduate student sample. J Am Coll Health. 2005;53(6):253–262. doi: 10.3200/JACH.53.6.253-262. [DOI] [PubMed] [Google Scholar]
- Teter CJ, McCabe SE, LaGrange K, Cranford JA, Boyd CJ. Illicit use of specific prescription stimulants among college students: Prevalence, motives, and routes of administration. Pharmacotherapy. 2006;26(10):1501–1510. doi: 10.1592/phco.26.10.1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vincent KB, Kasperski SJ, Caldeira KM, Garnier-Dykstra LM, Pinchevsky GM, O’Grady KE, Arria AM. Maintaining superior follow-up rates in a longitudinal study: Experiences from the College Life Study. Int J Mult Res Approach. 2012;6(1):56–72. doi: 10.5172/mra.2012.6.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, Fowler JS, Wang G-J, Telang F, Logan J, Wong C, Ma J, Pradhan K, Benveniste H, Swanson JM. Methylphenidate decreased the amount of glucose needed by the brain to perform a cognitive task. PLoS One. 2008;3(4):e2017–e2017. doi: 10.1371/journal.pone.0002017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weyandt LL, Marraccini ME, Gudmundsdottir BG, Zavras BM, Turcotte KD, Munro BA, Amoroso AJ. Misuse of prescription stimulants among college students: A review of the literature and implications for morphological and cognitive effects on brain functioning. Exp Clin Psychopharmacol. 2013;21(5):385–407. doi: 10.1037/a0034013. [DOI] [PubMed] [Google Scholar]
- Wilens TE. Mechanism of action of agents used in attention-deficit/hyperactivity disorder. J Clin Psychiatry. 2006;67(Suppl 8):32–38. [PubMed] [Google Scholar]
- Wilens TE, Adler LA, Adams J, Sgambati S, Rotrosen J, Sawtelle R, Utzinger L, Fusillo S. Misuse and diversion of stimulants prescribed for ADHD: A systematic review of the literature. J Am Acad Child Adolesc Psychiatry. 2008;47(1):21–31. doi: 10.1097/chi.0b013e31815a56f1. [DOI] [PubMed] [Google Scholar]
- Wilens TE, McBurnett K, Bukstein O, McGough J, Greenhill L, Lerner M, et al. Multisite controlled study of OROS methylphenidate in the treatment of adolescents with attention-deficit/hyperactivity disorder. Arch Pediatr Adolesc Med. 2006;160(1):82–90. doi: 10.1001/archpedi.160.1.82. [DOI] [PubMed] [Google Scholar]


