Abstract
Aim
The complex interplay of externalizing and internalizing problems in substance use risk is not well understood. This study tested whether the relationship of conduct problems and several internalizing disorders with future substance use is redundant, incremental, or interactive in adolescents.
Methods
Two semiannual waves of data from the Happiness and Health Study were used, which included 3,383 adolescents (M age = 14.1 years old; 53% females) in Los Angeles who were beginning high school at baseline. Logistic regression models tested the likelihood of past six-month alcohol, tobacco, marijuana, and any substance use at follow-up conditional on baseline conduct problems, symptoms of one of several internalizing disorders (i.e., Social Phobia and Major Depressive, Generalized Anxiety, Panic, and Obsessive-Compulsive Disorder), and their interaction adjusting for baseline use and other covariates.
Findings
Conduct problems were a robust and consistent risk factor of each substance use outcome at follow-up. When adjusting for internalizing-conduct comorbidity, depressive symptoms were the only internalizing problem whose risk for alcohol, tobacco, and any substance use was incremental to conduct problems. With the exception of social phobia, antagonistic interactive relationships between each internalizing disorder and conduct problems when predicting any substance use were found; internalizing symptoms was a more robust risk factor for substance use in teens with low (vs. high) conduct problems.
Conclusions
Although internalizing and externalizing problems both generally increase risk of substance use, a closer look reveals important nuances in these risk pathways, particularly among teens with comorbid externalizing and internalizing problems.
Keywords: Conduct Problems, Internalizing Symptomatology, Substance Use, Drugs, Depression, Anxiety
1. INTRODUCTION
Substance use often co-occurs with a range of externalizing problems throughout adolescence (Brown et al., 1996; Maslowsky et al., 2013; Merikangas et al., 2010). Although Conduct Problems (CPs) and other externalizing problems are well-established risk factors for adolescent substance use (King et al., 2004; Maslowsky et al., 2013), the role of internalizing symptomatology (IntSx) in teen substance use risk is less clear. Some research shows that anxiety and depression are associated with subsequent substance use in adolescents (Buckner et al., 2008; Crum et al., 2008; King et al., 2004; Sartor et al., 2007); however, results are not always replicated (Pardini et al., 2007) and do not appear to be as strong as the corresponding risk of substance use associated with CPs (King et al., 2004; Maslowsky and Schulenberg, 2013). Further complicating matters, there is considerable comorbidity between CPs and IntSx in teens (Lewinsohn et al., 1993). Hence, the interplay between CP and IntSx in adolescent substance use risk may be multifaceted.
1.1 The interplay of Conduct Problems and Internalizing Symptomatology in adolescent substance use
There are several ways in which CPs and IntSx may interplay in teen substance use risk. If the association of IntSx with substance use risk is mostly explained by the overlap with CPs, this would suggest that the internalizing pathway to substance use risk is redundant with CPs, whereby, both CPs and IntSx explain the same variance in substance use risk. If the association of IntSx with substance use risk occurs over and above overlapping risk accounted for by CPs, this would suggest that the internalizing pathway to substance use risk is incremental and that some meaningful degree of risk is conferred by IntSx even in the absence of high levels of CPs. These two patterns of results can be discerned by models of substance use risk in which IntSx and CPs are included as simultaneous predictors to control for their overlapping variance.
A third pattern regarding the interplay between CPs and IntSx in substance use risk can be determined by models of substance use testing the interaction between the IntSx and CPs. This interactive association could be expressed in one of two ways: (1) a synergistic interaction - the combination of having both high CPs and high IntSx is associated with a disproportionately larger increase in risk than what would be expected based on the risk carried by IntSx or CPs alone; and (2) an antagonistic interaction - the combination of having both high CPs and high IntSx is associated with a disproportionately smaller risk than what would be expected based on the risk carried by IntSx or CPs alone.
1.2 Research gaps on the interplay of Conduct Problems and Internalizing Symptomatology in substance use risk
Thus far, research on the CP-IntSx comorbidity has primarily focused on Conduct Disorder and Major Depressive Disorder as risk factors for substance use. To date, evidence indicates that both forms of psychopathology are associated with substance use independent of one another (Connor et al., 2004; Crum et al., 2008; Ingoldsby et al., 2006; King et al., 2004), incrementally to one another (Brook et al., 2015; Ingoldsby et al., 2006; Lansford et al., 2008), and interactively (e.g., Marmorstein and Iacono, 2001; Maslowsky and Schulenberg, 2013). These latter studies of adolescents have found that high levels of both CPs and depressive symptoms are associated with a disproportionately larger increase in risk for substance use than either disorder independently (i.e., synergistic interaction; Marmorstein and Iacono, 2001; Maslowsky and Schulenberg, 2013; Miller-Johnson et al., 1998; Pardini et al., 2007). However, research has yet to examine whether this interactive relationship exists between CPs and other forms of IntSx, such as the various type of anxiety disorder symptoms often present in adolescents (Grant et al., 2004). Understanding how the internalizing-externalizing interplay in substance use risk present across multiple forms of IntSx can elucidate whether additional IntSx beyond depression are needed in risk prediction modeling, developmental psychopathology theories, and prevention strategies that target affect.
1.3 The present study
The present study examines CPs and IntSx at the beginning of 9th grade to predict transitions in substance use by a six-month follow-up period. This period, which reflects the first year of high school, provides insight into this significant developmental period marked by social transitions, new academic demands, and access to older peer groups, and therefore is a high-risk period for substance use onset and escalation (Eaton et al., 2010; SAMHSA, 2009). We first examine relationships of CPs and multiple forms of IntSx (i.e., Major Depressive Disorder, Generalized Anxiety Disorder, Social Phobia, Panic Disorder, and Obsessive-Compulsive Disorder) to adolescent substance use risk in isolation from one another to replicate and extend past findings. We then address the primary aim of this paper which is to examine whether relations involving CPs and IntSx to substance use risk are redundant, incremental, or interactive. It is hypothesized that a synergistic interaction exists between depressive symptomatology and CPs on substance use given recent findings showing a synergistic association rather than the antagonistic kind (Maslowsky et al., 2013; Maslowsky and Schulenberg, 2013). No a priori hypotheses were put forth regarding how the other IntSx symptoms associate with substance use risk in the context of possible CP comorbidity.
2. METHODS
2.1 Participants and procedures
The current study utilizes survey data from a cohort of 9th grade students enrolled in 10 public high schools in the Greater Los Angeles area assessed at baseline (fall 2013) and again at a six-month follow up (spring 2014). Participating schools were selected based on their representation of diverse demographic characteristics. Students who were not enrolled in a special education program (e.g., severe learning disabilities) or English as a Second Language Programs were eligible to participate (N=4,100). Among those eligible, 3,874 (94.5%) assented to participate in the study, of whom 3,383 (82.5%) provided active written parental consent and enrolled in the study at baseline. The study had a 97% retention rate between baseline and follow-up with a total of 3,293 teens participating at follow-up. Paper-and-pencil surveys were administered during in-class 60-minute survey administrations. Researchers communicated to students that their responses would be strictly confidential and not shared with their teachers, parents, or school staff. Students were not individually compensated; however, each participating school was compensated for their general activity fund. Questionnaires were administered in a random order and some students did not complete the entire survey within the time allotted or were absent on one of the assessment days. Consequently, participants who did not complete key IntSx, CP, and substance use measures used in this report were not included in the final sample used in analyses. Depending on the particular analyses, sample size ranged from 2,896 to 3,229. The study was approved by the Institutional Review Board at the University of Southern California.
2.2 Measures
2.2.1 Conduct Problems
CPs were assessed at the baseline assessment using an 11-item measure of past six-month behavior (e.g., stealing, lying to parents, running away; Lloyd-Richardson et al., 2002; Resnick et al., 1997; Thompson et al., 2007). Six of the 11 items assessed are behaviors consistent with a Conduct Disorder diagnosis. The frequency of each behavior is ascertained with six ordinal response options varying from never to 10 or more times in the past six-months (scored 1 to 6, respectively) and a weighted sum score is computed across the 11 items. A weighted sum score of CPs was used in the analyses to most accurately reflect CPs endorsed. A weighted score is optimal given both a mean and a sum score would include individuals who had missing data on items and thus not accurately reflect a true endorsement of 11 CP items. The CP scale exhibited good internal consistency in the sample (α = .79) and exhibited characteristic patterns of association with IntSx symptoms and substance use, suggesting good evidence of construct validity.
2.2.2 Internalizing Symptomatology
The Revised Children’s Anxiety and Depression Scale (RCADS) was administered at baseline to assess Major Depressive Disorder, Generalized Anxiety Disorder, Social Phobia, Panic Disorder, and Obsessive-Compulsive Disorder symptoms (Chorpita et al., 2000). The Major Depressive scale included 10 items relating to depressive symptoms (e.g., “I feel sad or empty”). The Generalized Anxiety Disorder scale included six items relating to worry about the future (e.g., “I worry about things”). The Social Phobia scale includes nine items relating to fear of being evaluated negatively by others (e.g., I feel worried when I think someone is angry with me”). The Panic Disorder scale has nine items that assess bodily symptoms of a panic attack (e.g., “When I have a problem, I get a funny feeling in my stomach”). The Obsessive-Compulsive Disorder scale has six items relating to obtrusive thoughts (e.g., I have to think of special thoughts (like numbers or words) to stop bad things from happening.”). The frequency of each behavior is ascertained with four ordinal response options ranging from Never to Always. Similar to CPs, a weighted sum score was used for each of the five internalizing disorders.
The RCADS showed strong internal consistency (see Table 1 for psychometric properties for each form of IntSx), correspondence with DSM-based diagnoses, and convergent and discriminant validity in prior samples of teens (Chorpita et al., 2000). Table 2 shows that there was a moderate correlation between each form of IntSx, indicating discriminant validity between each construct in the current sample as well.
Table 1.
Sample characteristics among the overall sample.
| Overall Sample (N = 3,383) | |
|---|---|
| Age, M (SD) | 14.1 (0.42) |
| Gender, % | |
| Female | 53.0% |
| Male | 46.2% |
| Ethnicity, % | |
| American Indian/Alaska Native | 0.9% |
| Asian | 15.8% |
| Black/African American | 4.9% |
| Hispanic or Latino | 45.9% |
| Native Hawaiian/Pacific Islander | 3.3% |
| White | 15.3% |
| Other | 5.6% |
| Multiracial | 5.9% |
| Highest parental education, % | |
| High school graduate or less | 25.8% |
| Some college or more | 60.5% |
| RCADS- MDD, M (SD)/α | 7.8 (7.0)/.93 |
| RCADS- GAD Symptoms, M (SD)/α | 8.1 (4.7)/.89 |
| RCADS- PD Symptoms, M (SD)/α | 4.4 (5.3)/.92 |
| RCADS- SP Symptoms, M (SD)/α | 11.9 (7.3)/.90 |
| RCADS- OCD Symptoms, M (SD)/α | 4.4 (3.9)/.82 |
| CPs, M (SD)/α | 15.8 (5.5)/.79 |
| Substance Use, Past six-month use at Follow-Up/Baseline/Baseline Lifetime, % | |
| Any Substance | 37.2%/26.2%/40.2% |
| Alcohol | 21.1%/14.3%/26.1% |
| Marijuana | 14.5%/9.1%/15.3% |
| Tobacco | 28.2%/19.6%/29.5% |
Note. Data from ninth grade students in Los Angeles, California, USA collected in 2013–2014. CP = Conduct Problems; RCADS = Revised Children’s Anxiety And Depression Scale; MDD =Major Depressive Disorder; GAD = Generalized Anxiety Disorder; PD = Panic Disorder; SP = Social Phobia; OCD = Obsessive-Compulsive Disorder
Table 2.
Correlation matrix of key study variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 Past 6-mo Any Substance Use at Follow-Up | |||||||||||||||||
| 2 Past 6-mo Alcohol at Follow-Up | .67 | ||||||||||||||||
| 3 Past 6-mo Marijuana at Follow-Up | .53 | .48 | |||||||||||||||
| 4 Past 6-mo Tobacco Use at Follow-Up | .81 | .53 | .55 | ||||||||||||||
| 5. CP | .32 | .30 | .36 | .34 | |||||||||||||
| 6. MDD | .14 | .12 | .08 | .11 | .21 | ||||||||||||
| 7. GAD | .08 | .06 | .04 | .08 | .16 | .42 | |||||||||||
| 8. PD | .10 | .07 | .07 | .09 | .19 | .49 | .37 | ||||||||||
| 9. SP | .03 | .00 | −.04 | −.01 | .06 | .41 | .45 | .35 | |||||||||
| 10. OCD | .07 | .05 | .04 | .04 | .15 | .41 | .35 | .39 | .37 | ||||||||
| 11. Gender | −.00 | −.03 | .00 | .01 | −.02 | −.20 | −.05 | −.12 | −.16 | −.08 | |||||||
| 12. Ethnicity | .02 | −.01 | .04 | .04 | .03 | .01 | −.01 | .00 | −.00 | −.00 | .47 | ||||||
| 13. Parental Education | −.01 | −.03 | .03 | .00 | .01 | −.01 | −.01 | −.03 | −.02 | .00 | .18 | .14 | |||||
| 14 Past 6-mo Any Substance Use at Baseline | .48 | .42. | .41 | .45 | .39 | .13 | .13 | .13 | .01 | .06 | .02 | .01 | −.05 | ||||
| 15. Past 6-mo Alcohol at Baseline | .37 | .42 | .36 | .37 | .37 | .13 | .11 | .12 | −.00 | .06 | −.00 | .03 | .01 | .53 | |||
| 16. Past 6-mo Marijuana at Baseline | .31 | .32 | .45 | .40 | .43 | .10 | .08 | .10 | −.01 | .06 | .00 | .03 | .01 | .53 | .44 | ||
| 17. Past 6-mo Tobacco Use at Baseline | .37 | .34 | .40 | .46 | .42 | .11 | .10 | .12 | −.01 | .08 | −.00 | .02 | −.01 | .67 | .47 | .64 |
Note. All coefficients are Pearson correlations except the correlation between Parental Education and all other variables are Spearman correlations, as Parental Education is an ordinal variable. Shaded cells note correlations that were not statistically significant at p < .05. Ns range from 3,028 to 3,313. CP = Conduct Problems. Gender is coded as male = 1 and female = 0. Ethnicity is coded as Hispanic = 1, Non-Hispanic = 0. Parental Education is coded as 1 = High school education or less, 0 = At least some college education
2.2.3 Substance Use
Adolescent substance use was assessed using standard validated items used in prior epidemiologic surveys (Johnston et al., 2014). For past six-month use, in particular, students were asked whether they had used any of the 24 listed substances for recreational purposes or to get “high”. Adolescents who endorsed use of any substance were coded as past six-month users (26.2% of the sample). For substance specific analyses, binary past six-month alcohol, tobacco, and marijuana use variables were used. The binary tobacco use category variable included those who smoked a cigarette, smokeless tobacco, big cigars, little cigars or cigarillos, hookah water pipe, blunts, or other forms of tobacco (19.1%). The combined marijuana use category variable included those who smoked blunts (9.1%). A composite binary variable was used for primary analyses based on endorsement of any one of these substances.
2.2.4 Covariates
Demographic factors including gender, parental education (high school diploma or less vs. some college education or greater), and ethnicity (Hispanic vs. Not Hispanic) were included as covariates. These factors may be associated with substance use, and therefore, confound key associations (Anthony et al., 1994; Haberstick et al., 2013; Merikangas and McClair, 2012). Baseline past six-month use (yes/no) of each substance was also included as a covariate in all analyses. Age was not considered due to restricted range (all were in same grade). There were less than seven teens across the analyses that did not have the demographic covariates examined in the current set of analyses.
2.3 Analytical Approach1
The primary approach involved mixed-effects logistic regression models in which past six-month use of any substance, alcohol, tobacco, and marijuana at the follow-up served as the outcomes and CPs and/or IntSx were modeled as continuous predictor variables (both standardized with a mean of zero and standard deviation of one to facilitate interpretation of parameter estimates across variables with different scales). Each regression was modeled with a random intercept for school to account for the clustering of students within schools (Hubbard et al., 2010). Missing data on covariates were accounted for using dummy variable adjustment, which creates a dummy variable to code for missingness, to allow inclusion of the entire sample in analyses. Supplementary Table 12 presents a table of sample size and available data across all study variables. There were approximately 534 adolescents that had some amount of missing data across all key measures. These teens tended to be male, non-Hispanic, and slightly less educated.
All models were tested in four stages: (1) CPs as the sole predictor, (2) a single IntSx index as the sole predictor, (3) CPs and a single IntSx index as simultaneous predictors (to test for redundant or incremental relationships), and (4) CPs, the IntSx index, and the interaction term between CPs and IntSx index as simultaneous predictors (to test for interactive associations). Each of these models were run twice: (1) an unadjusted model that only included baseline reports of past six-month substance use for the respective substance under study as the sole covariate and (2) adjusted model that further included demographic covariates, including gender, ethnicity, and highest parental education in addition to baseline substance use as a covariate. Furthermore, this modeling strategy was repeated five times, whereby, we substituted in one of the five the different RCADS scale as the internalizing symptom predictor. This approach allowed us to compare each internalizing syndrome as a possible redundant, incremental, or interactive risk factor to CPs. We did not include multiple internalizing syndrome scales in the same model because of concerns about partialling out construct-relevant shared variance among the internalizing pathologies that might be accounted for by a common underlying internalizing dimension.
All analyses were conducted in Stata version 13.1, Stata Corp LP (College Station, TX). Results from the mixed-effects logistic regression models are reported as Odds Ratios (OR+95% CIs) and significance was set to .05 (two-tailed).
3. RESULTS
Table 1 presents descriptive statistics and Table 2 presents correlations among demographic and key study variables, which showed significant relations between all key study variables except Social Phobia with all substance use variables.
3.1 Primary analyses of Conduct Problems and Internalizing Symptom Indexes as predictors of substance use at follow-up
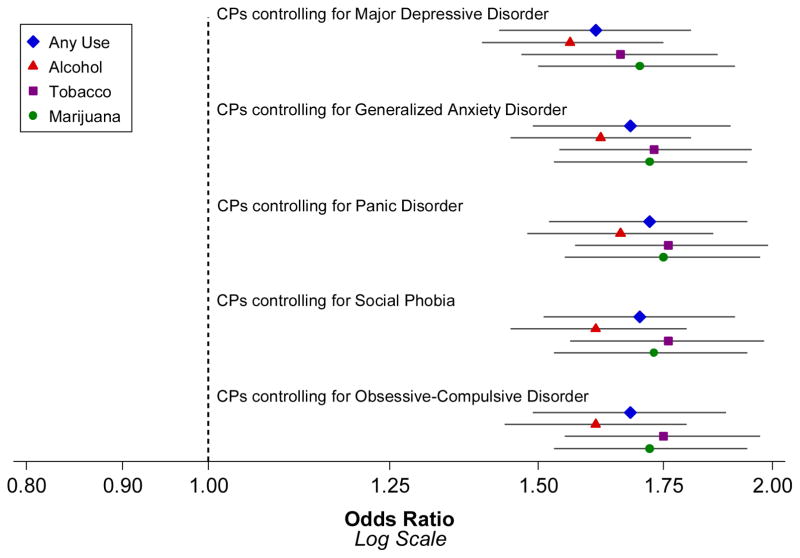
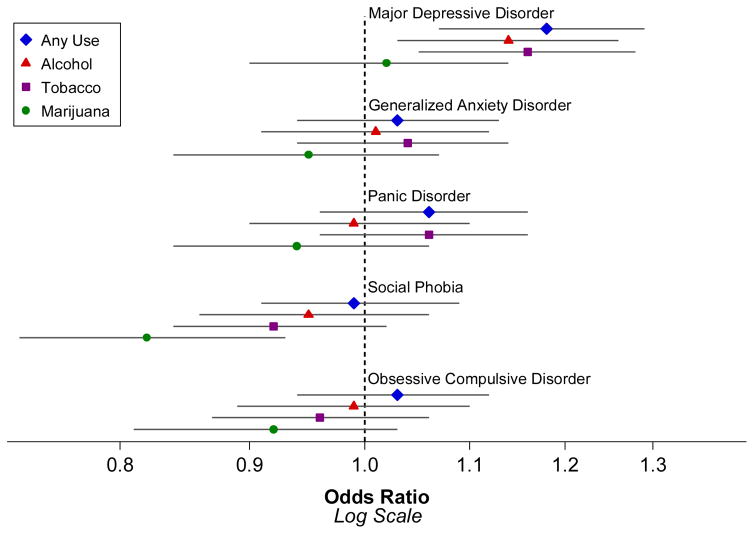
Unadjusted and adjusted ORs for associations of CP and IntSx with substance use outcomes were similar across analyses. Thus, for parsimony, adjusted ORs are reported in Figures 1–4.
Figure 1.
Independent associations of baseline Conduct Problems and Internalizing Symptom indexes in the prediction of past 6-month substance use at follow-up.
Note: All models adjusted for past six-month substance use at baseline, highest parental education, ethnicity, and gender.
Figure 4.
Interaction Betwen Baseline Conduct Problems and Internalizing Symptom Indexes in the Prediction of Past 6-month Any Substance Use at Follow-Up.
Note: MDD = Major Depressive Disorder. GAD = Generalized Anxiety Disorder. PD = Panic Disorder. OCD = Obsessive Compulsive Disorder.
3.1.1 Independent associations
Figure 1 depicts the independent association of each form of psychopathology to substance use alone without accounting for the covariance between CP and the internalizing measures.
For the any substance use status outcome measured at follow-up, baseline CPs had a strong positive association with substance use with results indicating that for each one standard deviation increase, the likelihood of an adolescent reporting substance use at follow-up was 72% greater after adjusting for baseline use and other covariates. The independent association of each IntSx measure on any substance use varied by the specific form of IntSx. Each IntSx domain was significantly associated with risk of any use at follow-up (ORs range = 1.04 – 1.28, p < .05), with the exception of social phobia (OR = 1.04 [0.96, 1.13], p = .35).
For substance-specific analyses, CPs were positively association with alcohol (OR = 1.62[1.46, 1.80], p < .0001), tobacco (OR = 1.72[1.53, 1.92], p < .0001), and marijuana use (OR = 1.75[1.56, 1.96], p < .0001). Major Depressive Disorder symptoms also had a positive independent association with each measure of substance use, whereas the association of other IntSx domains with individual drug outcomes varied across IntSx domains and were not consistently significant. Social Phobia was only associated with marijuana use (OR = 0.87[0.77, 0.97], p < .05), with the OR < 1 indicating social phobia may be a protective factor against marijuana use.
In each case, the 95% CI for associations involving CPs and associations involving IntSx did not overlap with one another, providing evidence that CPs were significantly more robust risk factors for substance use than IntSx (Figure 1).
3.1.2 Incremental associations
Figure 2 depicts the ORs of CPs on substance use when accounting for the comorbidity of each type of IntSx. CPs were significantly associated with substance use over and above each internalizing syndrome (p < .0001) and the inclusion of internalizing problems in the models did not meaningfully reduce the ORs for risk carried by CPs.
Figure 2.
Incremental associations of baseline Conduct Problems when comorbid with each Internalizing Symptom index in the prediction of past 6-month substance use at follow-up.
Note: All models adjusted for past six-month substance use at baseline, highest parental education, ethnicity, and gender.
Figure 3 depicts the ORs of each IntSx on substance use when adjusting for comorbid CPs. Depressive symptoms (OR = 1.19[1.09, 1.30], p < .001) were the only form of IntSx that had a significant incremental relationship with increased likelihood of alcohol, tobacco, and any substance use over and above CPs. Social Phobia was incrementally associated with lower marijuana use (OR = .84[0.74, 0.94]; p < .01) when accounting for co-occurring CPs.
Figure 3.
Incremental associations of each Internalizing Symptom Index when comorbid with Conduct Problems in the prediction of past 6-month substance use at follow-up.
Note: All models adjusted for past six-month substance use at baseline, highest parental education, ethnicity, and gender
3.1.3 Interactive associations
Figure 4 depicts the interaction between IntSx and CP symptoms. There were significant interactions between each internalizing measure (except Social Phobia) and CPs in predicting past six-month any substance use at follow-up (ORs range = .87 – .91, p < .05), with the ORs < 1 indicating antagonistic interactions. Adolescents endorsing less CPs reported higher rates of substance use at follow-up as the number of internalizing symptoms they endorsed increased, whereas, the likelihood of reporting substance use at follow-up was less pronounced among those with higher levels of CPs.
Only one substance-specific interactive association was found. There was an antagonistic interaction between Panic Disorder and CPs on tobacco use (OR = .92[.84, .99]; p < .05). However, this interaction was no longer significant after adjusting for demographic covariates.
4. DISCUSSION
This study provides novel evidence regarding how several forms of IntSx operate as risk factors for adolescent substance use in the context of CPs during the noteworthy transitional period of the first year of high school. First, the robust relationships between CPs and substance use regardless of IntSx levels point to the importance of drug use prevention efforts that effectively target high-risk teens with externalizing behaviors. Second, the incremental relationships between CPs and depressive symptomology highlight the additive risk that both CPs and depression carry above and beyond the association of each disorder independently. Lastly, the current study found evidence for several interactive relationships between CPs and IntSx; however, these associations were not synergistic as expected and displayed antagonistic interplay of CPs and IntSx in substance use risk.
4.1 Conduct Problems as a robust risk factor for substance use
Prior studies examining CPs independently (Hayatbakhsh et al., 2008; Mayzer et al., 2009) as well as in relation to IntSx (Ingoldsby et al., 2006; King et al., 2004; Lansford et al., 2008; Maslowsky and Schulenberg, 2013) have noted the robustness of CP-related risk of drug use. There are many possible reasons that could be underlying this phenomenon, including social explanations that suggest delinquent peer groups may encourage substance involvement or may simply use substances as part of their delinquency (Duncan et al., 2006; Hawkins et al., 1992). It could also be that substance use and CPs are manifestations a shared underlying externalizing construct (Krueger et al., 2002) with common genetic influences (Krueger et al., 2002; Slutske et al., 1998; Young et al., 2000, 2009). Current findings reinforce and extend a solid evidence base that CPs are a robust risk factors for substance use.
4.2 Incremental relationships between Conduct Problems and Internalizing Symptomatology
Depressive symptomatology was the only IntSx to have an incremental relationship with substance use, such that, the relation of depressive symptomatology with substance use risk went above and beyond the risks it shares with CPs. This is consistent with prior developmental psychopathology literature that has found that the comorbidity between Conduct Disorder and Major Depressive Disorder is associated with subsequent substance use (Brook et al., 2015; Lansford et al., 2008; Maslowsky et al., 2013; Pardini et al., 2007). The current study also extends these prior findings by examining incremental associations with multiple facets of IntSx. No other significant incremental associations were found with other forms of IntSx. The null finding raises the possibility that the risk marked by anxiety disorder symptoms may be a weak proxy for CP-related increases in substance use risk.
Additionally, given that only depressive symptoms, and not anxiety symptomatology, was significantly and incrementally associated with substance use over and above conduct problems, it may suggest that there are unique facets to depressive symptomatology that confer some degree of risk that does not overlap with anxiety symptoms. Depression’s core elements, like anhedonia, sadness, psychomotor retardation may play a unique role in substance use, whereas depressive features shared with anxiety (e.g., agitation, insomnia, concentration problems) may have less relevance to substance use risk. Some literature provides evidence that melancholic subtypes of depression, which are characterized by anhedonia and psychomotor changes, may be more strongly associated with nicotine and drug dependence than non-melancholic subtypes (Leventhal et al., 2008). Further disentanglement of how the different symptoms of Major Depressive Disorder are related to subsequent substance use in adolescents may be beneficial.
4.3 Antagonistic interactions between Conduct Problems and Internalizing Symptomatology
The present study found an antagonistic interaction, whereby, the combination of high IntSx and high CPs was associated with a disproportionately smaller increase in risk than what would be expected based on additive incremental effects of risk carried by the combination of IntSx alone and CPs alone. One possible explanation of this relationship is that some IntSx may offset some risk carried by comorbid CPs. For example, symptoms related to fearfulness and high arousal may suppress some of the behavioral disinhibition associated with CPs and substance use (Young et al., 2009). It could also be that the association of CPs and substance use is so robust that the etiological role of IntSx on substance use may have less of an impact on substance use. Figure 4 provides some support for this hypothesis given that adolescents at the highest levels of CPs appear to be less impacted by the presence of IntSx compared to those with lower levels of IntSx.
4.4 Generalizability of findings to specific substances
Although there were few significant substance-specific findings, results suggest that Social Phobia may be protective against marijuana use, over and above the negative impact of CPs. Prior literature has also corroborated this finding in adolescent community samples (Kellam et al., 1982; Myers et al., 2003; Shedler and Block, 1990). Socially anxious teens may not surround themselves with many peers, and thus, limit their access to negative modeling behaviors. Consistent with this theory, research shows that children at age 10 with higher levels of anxiety symptoms re less likely to associate with deviant peers who use drugs (Fergusson and Horwood, 1999). The current study extends on this by elucidating the relative impact of different measures of anxiety. Specifically, social anxiety may be protective against marijuana use, but other measures, including Generalized Anxiety Disorder symptoms and Panic Disorder symptoms confer some risk on overall substance use.
4.5 Limitations
First, participants were sampled from a restricted geographic region, which raises limitations on generalizability. Second, the IntSx and CP measures were based on self-report data and not structured clinical interviews. Thus, response styles could have impacted results. However, one would not expect that a reporting bias would confound the extent to which a measure has an incremental or interactive association with substance use. Third, although the CP measure examines several types of CPs, it is not a diagnostic tool used to examine individuals at clinical levels for Conduct Disorder. However, this study may be relevant to many teens who engage in sub-clinical levels of CPs who further progress to substance use. Fourth, a binary any substance use outcome variable was used, which has high sensitivity but low specificity for identifying problematic patterns of use. Finally, the brief follow-up period between waves makes it difficult to discern the longitudinal impact of the IntSx-CP comorbidity as well as potential substance-specific differences that may emerge later on in adolescence.
4.6 Conclusions
Current study results highlight the robustness of CPs as a risk factor for substance use as well as nuanced interplay of internalizing-externalizing problems in the developmental psychopathology of adolescent drug use vulnerability. Because of the risk associated with each internalizing disorder individually as well as in combination with CPs, it is critical that school administrators and mental health professionals assess for symptoms along the internalizing-externalizing spectrum to identify and prevent future substance use. Furthermore, adolescence who have high levels of CPs and depressive symptoms may benefit most from early drug use prevention.
Supplementary Material
Highlights.
Conduct problems were a consistent and robust risk factor for substance use.
Depression posed a risk for substance use above that of conduct problems.
Social Phobia symptoms appear to be protective against marijuana use.
Am antagonistic interaction was found between conduct and internalizing problems.
Footnotes
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Contributors
Rubin Khoddam conducted literature searches, wrote the initial complete draft of the manuscript, and maintained contact between authors to bring the manuscript to fruition. Nicholas Jackson conducted statistical analyses, made the figures, and edited drafts of the manuscript. Dr. Adam Leventhal edited drafts of the manuscript, designed the study, and wrote the protocol. All authors contributed to and have approved the final manuscript.
Conflict of Interest
None of the authors declare that they have no conflicts of interest.
Role of Funding Source
Funding for this study was provided by NIDA Grants R01-DA033296 and F31-DA039708; NIDA had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. Diagnostic And Statistical Manual Of Mental Disorders. 5. APA; Washington, DC: 2013. [Google Scholar]
- Anthony JC, Warner LA, Kessler RC. Comparative epidemiology of dependence on tobacco, alcohol, controlled substances, and inhalants: basic findings from the National Comorbidity Survey. Exp Clin Psychopharmacol. 1994;2:244–268. [Google Scholar]
- Brook JS, Lee JY, Finch SJ, Brook DW. Conjoint trajectories of depressive symptoms and delinquent behavior predicting substance use disorders. Addict Behav. 2015;42:14–19. doi: 10.1016/j.addbeh.2014.10.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Schmidt NB, Lang AR, Small JW, Schlauch RC, Lewinsohn PM. Specificity of social anxiety disorder as a risk factor for alcohol and cannabis dependence. J Psychiatr Res. 2008;42:230–239. doi: 10.1016/j.jpsychires.2007.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chavira DA, Stein MB. childhood social anxiety disorder: from understanding to treatment. Child Adolesc Psychiatr Clin N Am. 2005;14:797–818. doi: 10.1016/j.chc.2005.05.003. [DOI] [PubMed] [Google Scholar]
- Couwenbergh C, van den Brink W, Zwart K, Vreugdenhil C, van Wijngaarden-Cremers, van der Gaag RJ. Comorbid psychopathology in adolescents and young adults treated for substance use disorders. Eur Child Adolesc Psychiatry. 2006;15:319–328. doi: 10.1007/s00787-006-0535-6. [DOI] [PubMed] [Google Scholar]
- Crum RM, Green KM, Storr CL, Chan Y, Ialongo N, Stuart EA, Anthony JC. Depressed mood in childhood and subsequent alcohol use through adolescence and young adulthood. Arch Gen Psychiatry. 2008;65:702–712. doi: 10.1001/archpsyc.65.6.702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cukrowicz KC, Schlegel EF, Smith PN, Jacobs MP, Van Orden KA, Paukert AL, Pettit JW, Joiner TE. Suicide ideation among college students evidencing subclinical depression. J Am Coll Health. 2011;59:575–581. doi: 10.1080/07448481.2010.483710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dierker LC, Vesel F, Sledjeski EM, Costello D, Perrine N. Testing the dual pathway hypothesis to substance use in adolescence and young adulthood. Drug Alcohol Depend. 2007;87:83–93. doi: 10.1016/j.drugalcdep.2006.08.001. [DOI] [PubMed] [Google Scholar]
- Duncan SC, Duncan TE, Strycker LA. Alcohol use from ages 9 to 16: a cohort-sequential latent growth model. Drug Alcohol Depend. 2006;81:71–81. doi: 10.1016/j.drugalcdep.2005.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J, Harris WA, Lowry R, McManus T, CHyen D, Lim C, Whittle L, Brener ND, Wechsler H CDC. Youth risk behavior surveillance - United States, 2009. MMWR Surveill Summ. 2010;59:1–142. [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Ridder EM. Conduct and attentional problems in childhood and adolescence and later substance use, abuse and dependence: results of a 25-year longitudinal study. Drug Alcohol Depend. 2007;88:S14–S26. doi: 10.1016/j.drugalcdep.2006.12.011. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Haberstick BC, Young SE, Zeiger JS, Lessem JM, Hewitt JK, Hopfer CJ. Prevalence and correlates of alcohol and cannabis use disorders in the United States: results from the national longitudinal study of adolescent health. Drug Alcohol Depend. 2014;136:158–161. doi: 10.1016/j.drugalcdep.2013.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins JD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: implications for substance abuse prevention. Psychol Bull. 1992;112:64–105. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- Henry B, Feehan M, McGee R, Stanton W, Moffitt TE, Silva P. The importance of conduct problems and depressive symptoms in predicting adolescent substance use. J Abnorm Child Psychol. 1993;21:469–480. doi: 10.1007/BF00916314. [DOI] [PubMed] [Google Scholar]
- Hussong AM, Jones DJ, Stein GL, Baucom DH, Boeding S. An internalizing pathway to alcohol use and disorder. Psychol Addict Behav. 2011;25:390–404. doi: 10.1037/a0024519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson KM, Sher KJ, Cooper ML, Wood PK. Adolescent alcohol and tobacco use: onset, persistence and trajectories of use across two samples. Addiction. 2002;97:517–531. doi: 10.1046/j.1360-0443.2002.00082.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplow JB, Curran PJ, Angold A, Costello EJ. The prospective relation between dimensions of anxiety and the initiation of adolescent alcohol use. J Clin Child Psychol. 2001;30:316–326. doi: 10.1207/S15374424JCCP3003_4. [DOI] [PubMed] [Google Scholar]
- Kellam SG, Stevenson DL, Rubin BR. How specific are the early predictors of teenage drug use? NIDA Res Monograph Ser. 1982;43:329–334. [PubMed] [Google Scholar]
- Kilbey MM, Downey K, Breslau N. Predicting the emergence and persistence of alcohol dependence in young adults: the role of expectancy and other risk factors. Exp Clin Psychopharmacology. 1998;6:149–156. doi: 10.1037//1064-1297.6.2.149. [DOI] [PubMed] [Google Scholar]
- King SM, Iacono WG, McGue M. Childhood externalizing and internalizing psychopathology in the prediction of early substance use. Addiction. 2004;99:1548–1559. doi: 10.1111/j.1360-0443.2004.00893.x. [DOI] [PubMed] [Google Scholar]
- Koopmans JR, Slutske WS, Heath AC, Neale MC, Boomsma DI. The genetics of smoking initiation and quantity smoked in Dutch adolescent and young adult twins. Behav Genet. 1999;29:383–393. doi: 10.1023/a:1021618719735. [DOI] [PubMed] [Google Scholar]
- Kovacs M, Paulauskas S, Gatsonis C, Richards C. Depressive disorders in childhood III. A longitudinal study of comorbidity with and risk for conduct disorders. J Affect Disord. 1988;15:205–217. doi: 10.1016/0165-0327(88)90018-3. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Hicks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M. Etiologic connections among substance dependence, antisocial behavior, and personality: modeling the externalizing spectrum. J Abnorm Psychol. 2002;111:411–424. [PubMed] [Google Scholar]
- Lansford JE, Erath S, Yu T, Pettit GS, Dodge KA, Bates JE. The developmental course of illicit substance use from age 12 to 22: links with depressive, anxiety, and behavior disorders at age 18. J Child Psychol Psychiatry. 2008;49:877–885. doi: 10.1111/j.1469-7610.2008.01915.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III—R disorders in high school students. J Abnorm Psychol. 1993;102:133–144. doi: 10.1037//0021-843x.102.1.133. [DOI] [PubMed] [Google Scholar]
- Leventhal AM, Kahler CW, Ray LA, Stone K, Young D, Chelminski I, Zimmerman M. Anhedonia and amotivation in psychiatric outpatients with fully remitted stimulant use disorder. Am J Addict. 2008;17:218–223. doi: 10.1080/10550490802019774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal AM, Waters AJ, Kahler CW, Ray LA, Sussman S. Relations between anhedonia and smoking motivation. Nicotine Tob Res. 2009;11:1047–1054. doi: 10.1093/ntr/ntp098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal AM, Brightman M, Ameringer KJ, Greenberg J, Mickens L, Ray LA, Sun P, Sussman S. Anhedonia associated with stimulant use and dependence in a population-based sample of American adults. Exp ClinPsychopharmacol. 2010;18:562–569. doi: 10.1037/a0021964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lilienfeld SO. Comorbidity between and within childhood externalizing and internalizing disorders: reflections and directions. J Abnorm Child Psychol. 2003;31:285–291. doi: 10.1023/a:1023229529866. [DOI] [PubMed] [Google Scholar]
- Lloyd-Richardson EE, Papandonatos G, Kazura A, Stanton C, Niaura R. Differentiating stages of smoking intensity among adolescents: stage-specific psychological and social influences. J Consult Clin Psychol. 2002;70:998–1009. doi: 10.1037//0022-006x.70.4.998. [DOI] [PubMed] [Google Scholar]
- MacLatchy-Gaudet HA, Stewart SH. The context-specific positive alcohol outcome expectancies of university women. Addict Behav. 2001;26:31–49. doi: 10.1016/s0306-4603(00)00080-0. [DOI] [PubMed] [Google Scholar]
- Marmorstein NR, Iacono WG. An investigation of female adolescent twins with both major depression and conduct disorder. J Am Acad Child Adolesc Psychiatry. 2001;40:299–306. doi: 10.1097/00004583-200103000-00009. [DOI] [PubMed] [Google Scholar]
- Maslowsky J, Schulenberg JE. Interaction matters: Quantifying conduct problem x depressive symptoms interaction and its association with adolescent alcohol, cigarette, and marijuana use in a national sample. Dev Psychopathol. 2013;25:1029–1043. doi: 10.1017/S0954579413000357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maslowsky J, Schulenberg JE, O’Malley PM, Kloska DD. Depressive symptoms, conduct problems, and risk for polysubstance use among adolescents: results form US national surveys. Ment Health Subst Use. 2013;7:157–169. doi: 10.1080/17523281.2013.786750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maslowsky J, Schulenberg JE, Zucker RA. Influence of conduct problems and depressive symptomatology on adolescent substance use: developmentally proximal versus distal effects. Dev Psychol. 2013;50:1179–1189. doi: 10.1037/a0035085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masse LC, Tremblay RE. Behavior of boys in kindergarten and the onset of substance use during adolescence. Arch Gen Psychiatry. 1997;54:62–68. doi: 10.1001/archpsyc.1997.01830130068014. [DOI] [PubMed] [Google Scholar]
- Mayzer R, Fitzgerald HE, Zucker RA. Anticipating problem drinking risk from preschoolers’ antisocial behavior: evidence for a common delinquency-related diathesis model. J Am Acad Child Adolesc Psychiatry. 2009;48:820–827. doi: 10.1097/CHI.0b013e3181aa0383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGue M, Iacono WG. The association of early adolescent problem behavior with adult psychopathology. Am J Psychiatry. 2005;162:1118–1124. doi: 10.1176/appi.ajp.162.6.1118. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Mehta RL, Molnar BE, Walters EE, Swendsen JD, Aguilar-Gaziola S, Bijl R, Borges G, Caraveo-Anduaga JJ, DeWit DJ, Kolody B, Vega WA, Wittchen HU, Kessler RC. Comorbidity of substance use disorders with mood and anxiety disorders: results of the International Consortium in Psychiatric Epidemiology. Addict Behav. 1998;23:893–907. doi: 10.1016/s0306-4603(98)00076-8. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, Georgiades K, Swendsen J. Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, McClair VL. Epidemiology of substance use disorders. Hum Genet. 2012;131:779–789. doi: 10.1007/s00439-012-1168-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller-Johnson S, Lochman JE, Coie JD, Terry R, Hyman C. Comorbidity of conduct and depressive problems at sixth grade: substance use outcomes across adolescence. J Abnorm Child Psychol. 1998;26I:221–232. doi: 10.1023/a:1022676302865. [DOI] [PubMed] [Google Scholar]
- Myers MG, Aarons GA, Tomlinson K, Stein MB. Social anxiety, negative affectivity, and substance use among high school students. Psychol Addict Behav. 2003;17:277–283. doi: 10.1037/0893-164X.17.4.277. [DOI] [PubMed] [Google Scholar]
- Pardini D, Lochman J, Wells K. Negative emotions and alcohol use initiation in high-risk boys: the moderating effect of good inhibitory control. J Abnorm Child Psychol. 2004;32:505–518. doi: 10.1023/b:jacp.0000037780.22849.23. [DOI] [PubMed] [Google Scholar]
- Pardini D, White HE, Stouthamer-Loeber M. Early adolescent psychopathology as a predictor alcohol use disorders by young adulthood. Drug Alcohol Depend. 2007;88S:S38–S49. doi: 10.1016/j.drugalcdep.2006.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick MD, Bearman PS, Blum RW, Bauman KE, Harris KM, Jones J, Tabor J, Beuhring T, Sieving RE, Shew M, Ireland M, Bearinger LH, Udry JR. Protecting adolescents from harm: findings from the National Longitudinal Study on Adolescent Health. JAMA. 1997;278:823–832. doi: 10.1001/jama.278.10.823. [DOI] [PubMed] [Google Scholar]
- Rhee SH, Hewitt JK, Young SE, Corley RP, Crowley TJ, Stallings MC. Genetic and environmental influences on substance initiation, use, and problem use in adolescents. Arch Gen Psychiatry. 2003;60:1256–1264. doi: 10.1001/archpsyc.60.12.1256. [DOI] [PubMed] [Google Scholar]
- Sartor CE, Lynskey MT, Heath AC, Jacob T, True W. The role of childhood risk factors in initiation of alcohol use and progression to alcohol dependence. Addiction. 2007;102:216–225. doi: 10.1111/j.1360-0443.2006.01661.x. [DOI] [PubMed] [Google Scholar]
- Shedler J, Block J. Adolescent drug use and psychological health: a longitudinal inquiry. Am Psychol. 1990;45:612–630. doi: 10.1037//0003-066x.45.5.612. [DOI] [PubMed] [Google Scholar]
- Slutske WS, Heath AC, Dinwiddie SH, Madden PA, Bucholz KK, Dunne MP, … Martin NG. Common genetic risk factors for conduct disorder and alcohol dependence. J Abnorm Psychol. 1998;107:363–374. doi: 10.1037//0021-843x.107.3.363. [DOI] [PubMed] [Google Scholar]
- Smith GT, Goldman MS, Greenbaum PE, Christiansen BA. Expectancy for social facilitation from drinking: the divergent paths of high-expectancy and low-expectancy adolescents. J Abnorm Psychol. 1995;104:32–40. doi: 10.1037//0021-843x.104.1.32. [DOI] [PubMed] [Google Scholar]
- Squeglia LM, Jacobus J, Tapert SF. The influence of substance use on adolescent brain development. Clin EEG Neurosci. 2009;40:31–38. doi: 10.1177/155005940904000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2008 National Survey on Drug Use and Health: National Findings. Rockville, MD: 2009. (Office of Applied Studies, NSDUH Series H-36, HHS Publication No. SMA 09–4434) [Google Scholar]
- Thompson MP, Ho CH, Kingree JB. Prospective associations between delinquency and suicidal behaviors in a nationally representative sample. J Adolesc Health. 2007;40:232–237. doi: 10.1016/j.jadohealth.2006.10.016. [DOI] [PubMed] [Google Scholar]
- Young SE, Stallings MC, Corley RP, Krauter KS, Hewitt JK. Genetic and environmental influences on behavioral disinhibition. Am J Med Genet. 2000;96:684–695. [PubMed] [Google Scholar]
- Young SE, Friedman NP, Miyake A, Willcutt EG, Corley RP, Haberstick BC, Hewitt JK. Behavioral disinhibition: liability for externalizing spectrum disorders and its genetic and environmental relation to response inhibition across adolescence. J Abnorm Psychol. 2009;118:117–130. doi: 10.1037/a0014657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinbarg RE, Barlow DH. Structure of anxiety and the anxiety disorders: a hierarchical model. J Abnorm Psychol. 1996;106:181–193. doi: 10.1037//0021-843x.105.2.181. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.