Abstract
Importance
A binocular approach to treating anisometropic and strabismic amblyopia has recently been advocated. Initial studies have yielded promising results, suggesting that a larger randomized clinical trial is warranted.
Objective
To compare visual acuity (VA) improvement in children with amblyopia treated with a binocular iPad® game versus part-time patching.
Design
Randomized, non-inferiority clinical trial.
Setting
Multicenter, community and institutional practices
Participants
385 participants 5 to <13 years of age (mean 8.5 years) with amblyopia (20/40 to 20/200, mean 20/63) resulting from strabismus, anisometropia, or both.
Interventions
Participants were randomly assigned to either 16 weeks of a binocular iPad game, prescribed for 1 hour a day (n=190, binocular group) or patching of the fellow eye prescribed for 2 hours a day (n=195, patching group). Study follow-up visits were scheduled at 4, 8, 12, and 16 weeks.
Main outcome measure
Change in amblyopic-eye VA from baseline to 16 weeks.
Results
At 16 weeks, mean amblyopic-eye VA improved 1.05 lines (2-sided 95% confidence interval (CI): 0.85 to 1.24 lines) in the binocular group and 1.35 lines (2-sided 95% CI: 1.17 to 1.54 lines) in the patching group, with an adjusted treatment group difference of 0.31 lines favoring patching (upper limit of the 1-sided 95% CI 0.53 lines). This upper limit exceeded the pre-specified non-inferiority limit of 0.5 lines. Only 22% of participants randomized to the binocular game performed >75% of the prescribed treatment (median 46%, interquartile range 20% to 72%). In younger participants age 5 to <7 years old, without prior amblyopia treatment, amblyopic-eye VA improved 2.5 ± 1.5 lines in the binocular group and 2.8 ± 0.8 in the patching group. Adverse effects (including diplopia) were uncommon and of similar frequency between groups.
Conclusions and Relevance
In children 5 to <13 years of age, amblyopic-eye VA improved with binocular game play and with patching, particularly in younger children age 5 to <7 years without prior amblyopia treatment. Although the primary non-inferiority analysis was indeterminate, a post-hoc analysis suggested VA improvement with this particular binocular iPad treatment was not as good as with 2 hours of prescribed daily patching.
Introduction
A binocular approach to treating anisometropic and strabismic amblyopia has recently been advocated,1–6 without patching,7, 8 atropine drops,9 or Bangerter filters10 applied to the fellow eye. In such binocular therapy, images are presented dichoptically, with high-contrast images presented to the amblyopic eye and low-contrast images to the fellow eye, to achieve a binocular percept.11 Recently, this binocular treatment has been adapted to an iPad® device as a “falling blocks” game, which uses red-green anaglyphic glasses. Initial studies have yielded promising results,3–5 suggesting that a larger randomized clinical trial is warranted.
The purpose of the present randomized clinical trial was to establish whether treatment of amblyopia with a binocular iPad game (prescribed 1 hour per day for 16 weeks) was not substantially worse (non-inferior) than treatment with patching of the fellow eye (prescribed 2 hours per day) in children age 5 to <13 years, with 20/40 to 20/200 amblyopic-eye VA
Methods
The study was conducted at 78 institution- or community-based clinical sites and approved by the respective institutional review boards (IRB). A parent or guardian (referred to subsequently as “parent”) of each study participant gave written informed consent, and each participant assented to participation as required. The study is listed on www.clinicaltrials.gov, under identifier NCT02200211, accessed 5/27/16. The complete study protocol is available on the PEDIG website (www.pedig.net, accessed 5/27/16). Eligibility criteria are listed in Table 1.
Table 1.
Study Inclusion and Exclusion Criteria
|
ELIGIBILITY CRITERIA The following criteria must be met for the patient to be enrolled in the study: |
|
EXCLUSION CRITERIA
|
Study Visits and Testing Procedures
Visual acuity was measured in each eye with optimal refractive correction (if applicable), and without cycloplegia by a study-certified examiner (masked at follow up). We used a consistent method throughout the study for each participant; either the Amblyopia Treatment Study single-surround HOTV protocol (ATS-HOTV©)12 for participants age 5 to <7 years or the Electronic Early Treatment Diabetic Retinopathy Study (E-ETDRS©) protocol13 for participants age 7 to <13 years. Visual acuity was converted to the logarithm of the minimum angle of resolution (logMAR) scale. Additional testing at all study visits included measurement of ocular alignment with a simultaneous prism and cover test (SPCT), and a prism and alternate cover test (PACT), and stereoacuity (masked at follow-up) using the Randot Butterfly and Randot Preschool stereoacuity tests (Stereo Optical Co., Chicago IL).
Follow-up visits occurred at 4, 8, 12, and 16 weeks (± 1 week) after randomization (± 1 week), with the primary outcome visit at 16 weeks. At each visit, a standardized questionnaire was administered to participants and their parents to assess the presence and frequency of diplopia.
Randomization and Treatment
Participants were randomly assigned via the PEDIG website with equal probability, using a permutated block design stratified by age group (5 to <7 years, 7 to <13 years) and site, to receive either binocular treatment or patching (subsequently referred to as the “binocular” and “patching” groups, respectively), administered via the PEDIG website.
The patching group was prescribed 2 hours of daily patching (allowing division into shorter sessions) with an adhesive style patch (Coverlet/3M Opticlude/Ortopad), 7 days a week for 16 weeks. The binocular group was prescribed the binocular falling blocks iPad game for 1 hour a day (allowing division into shorter sessions), 7 days a week for 16 weeks, with instructions to perform therapy a minimum of 4 days a week if unable to play for 7 days per week. The differing durations per day (2 hours versus 1 hour) were chosen to reflect commonly used regimes with each treatment. Compliance was calculated based on an intended treatment of 7 days a week for 16 weeks.
The game was played on a study-supplied iPad device at the participants’ habitual reading distance while wearing red/green anaglyphic glasses (over the spectacles if applicable) with the green filter placed over the amblyopic eye. Participants played the game by moving the falling blocks to form solid lines, with the level of difficulty (easy, medium, hard) set at the participant’s discretion. While the contrast of the falling blocks for the amblyopic eye was always 100%, the contrast for the fellow eye was initially set to 20% and automatically increased/decreased by 10% increments (with a lowest level of 10%), or left unchanged from the last contrast level, based on previous day game play duration and performance. The contrast only changed if ≥ 30 minutes of game play occurred the previous day, increasing if ≥1000 points were scored or decreasing otherwise.
Parents recorded the number of hours the participant played the game or wore the patch each day using calendars. The iPad device automatically recorded the duration of game play, contrast and performance.
Statistical Analyses
The trial was designed as a non-inferiority study. The sample size of 346 participants was computed to have 90% power with a type I error of 5% for a non-inferiority limit of 0.05 logMAR (0.5 lines), assuming a standard deviation of change of 0.15 logMAR (1.5 lines) based on prior PEDIG studies,10, 14–17 and no more than 10% loss to follow-up. This non-inferiority margin represents a conservative estimate of the treatment benefit of part-time patching compared with optical correction alone (based on previous studies14, 15), chosen so the effect of binocular treatment, if found non-inferior to patching, would very likely be greater than that of optical correction alone.
The primary outcome measure was change in amblyopic-eye VA from baseline to 16 weeks (14 to <20 week window). The upper limit of a 1-sided 95% confidence interval (CI) was computed on the treatment group difference, using an analysis of covariance (ANCOVA) model, adjusted for baseline age and VA, including only participants completing the 16-week outcome in a modified intent-to-treat analysis. Alternative approaches to the primary analysis are specified in eTable 1. The primary analysis was repeated with computation of a 2-sided 95% CI for the adjusted treatment group difference as a post-hoc analysis to estimate the range of plausible values of the treatment group difference.
In a post-hoc analysis, we compared the 16-week outcomes in those who were compliant (completing >50% prescribed treatment) and successfully played the game (fellow-eye contrast increased to >95%) with those who were not.
Statistical methods for additional analyses are described in the relevant tables and figures (including online tables and figures). Analyses were conducted using SAS version 9.4 (SAS Inc., Cary, NC).
Results
Baseline Characteristics
Between September 2014 and August 2015, 385 participants were randomly assigned to the binocular group (n=190) or to the patching group (n=195). Baseline characteristics were similar in the two groups (Table 2). Seven patients were subsequently found to be ineligible (reasons listed in Table 2).
Table 2.
Baseline Characteristics of Randomized Participants by Treatment Group a
| Binocular (N=190) |
Patching (N=195) |
|||
|---|---|---|---|---|
| N | % | N | % | |
| Gender | ||||
| Female | 98 | 52 | 89 | 46 |
| Race/Ethnicity | ||||
| White | 134 | 71 | 145 | 74 |
| Black/African American | 11 | 6 | 12 | 6 |
| Hispanic | 33 | 17 | 24 | 12 |
| Asian/American Indian/Alaskan Native | 9 | 5 | 6 | 3 |
| More than one race | 2 | 1 | 5 | 3 |
| Unknown/not reported | 1 | <1 | 3 | 2 |
| Age at enrollment (Years) | ||||
| 5 to <7 | 43 | 23 | 50 | 26 |
| 7 to <9 | 78 | 41 | 62 | 32 |
| 9 to <13 | 69 | 36 | 83 | 43 |
| Mean (SD) Years | 8.4 (1.8) | 8.6 (2.0) | ||
| Prior Amblyopia Treatment | ||||
| None | 45 | 24 | 40 | 21 |
| Patching | 89 | 47 | 89 | 46 |
| Other (Not Patching) b | 5 | 3 | 7 | 4 |
| Patching Plus Other Treatment b | 51 | 27 | 59 | 30 |
| Distance Amblyopic-Eye Visual Acuity | ||||
| 20/200 (33–37 Letters) | 5 | 3 | 4 | 2 |
| 20/160 (38–42 Letters) | 6 | 3 | 7 | 4 |
| 20/125 (43–47 Letters) | 8 | 4 | 4 | 2 |
| 20/100 (48–52 Letters) | 16 | 8 | 12 | 6 |
| 20/80 (53–57 Letters) | 30 | 16 | 24 | 12 |
| 20/63 (58–62 Letters) | 37 | 19 | 46 | 24 |
| 20/50 (63–67 Letters) | 61 | 32 | 52 | 27 |
| 20/40 (68–72 Letters) | 27 | 14 | 46 | 24 |
| Mean (SD) LogMAR | 0.51 (0.17) | 0.48 (0.17) | ||
| Mean Snellen Equivalent | 20/63−1 | 20/63+1 | ||
| Distance Fellow-Eye Visual Acuity | ||||
| Mean (SD) LogMAR | −0.03 (0.09) | −0.03 (0.08) | ||
| Mean Snellen Equivalent | 20/20+2 | 20/20+2 | ||
| Interocular Difference | ||||
| Mean (SD) (Lines) | 5.5 (1.8) | 5.1 (1.8) | ||
| Baseline Stereoacuity (Seconds of Arc)c | ||||
| Nil | 69 | 36 | 57 | 29 |
| 2000 | 28 | 15 | 37 | 19 |
| 800 | 18 | 9 | 26 | 13 |
| 400 | 17 | 9 | 19 | 10 |
| 200 | 23 | 12 | 18 | 9 |
| 100 | 23 | 12 | 23 | 12 |
| 60 | 10 | 5 | 9 | 5 |
| 40 | 2 | 1 | 6 | 3 |
| Median (Seconds of Arc) | 2000 | 800 | ||
| Amblyopia Cause | ||||
| Strabismus | 22 | 12% | 44 | 23% |
| Anisometropia | 107 | 56 | 92 | 47 |
| Strabismus/Anisometropia combined | 61 | 32 | 59 | 30 |
| Maximum Magnitude of Tropia Deviation at Distance Measured by SPCT (pd) | ||||
| Orthotropic | 140 | 74 | 123 | 63 |
| 1 to 9 | 44 | 23 | 66 | 34 |
| ≥ 10 | 6 | 3 | 6 | 3 |
| Maximum Magnitude of Tropia Deviation at Near Measured by SPCT (pd) | ||||
| Orthotropic | 132 | 69 | 125 | 64 |
| 1 to 9 | 54 | 28 | 63 | 32 |
| ≥ 10 | 4 | 2 | 7 | 4 |
| Amblyopic-Eye Spherical Equivalent (Diopters) | ||||
| Mean (SD) Diopters | +4.74 (2.41) | +4.20 (2.65) | ||
| Fellow-Eye Spherical Equivalent (Diopters) | ||||
| Mean (SD) Diopters | +2.39 (2.04) | +2.31 (2.21) | ||
| Spherical Equivalent Anisometropia (Diopters) | ||||
| Mean (SD) Diopters | +2.52 (1.74) | +2.11 (1.76) | ||
logMAR = logarithm of the minimum angle of resolution; SD = standard deviation, SPCT = simultaneous prism and cover test
Of the 12 participants who wore contact lens(s) during the study, an over-refraction was not performed for 7 participants and the contact lens over-refraction did not meet eligibility criteria for 1 participant. An over-refraction was not initially required for study eligibility but later added as an amendment to the protocol.
Seven participants (3 in the binocular group and 4 in the patching group) were later found to be ineligible for the study based on the following pre-enrollment criteria: spectacles did not meet refractive correction guidelines (n=1), no over-refraction performed when required (n=1) or over-refraction was outside of the pre-specified tolerance limits (n=1) for contact lens wear, failure to meet visual acuity stability criteria for corrective wear (n=3), and the most recent cycloplegic refraction was performed more than 7 months prior to enrollment (n=1). These 7 participants were included in the primary analysis, but were excluded in a separate analysis as an additional approach to the primary analysis (eTable 1).
Other treatment includes atropine, plano (or reduced plus) lens wear, fogging (Bangerter filter, tape, optical), vision therapy (home or office) or levodopa treatment for amblyopia.
Results of the Randot Butterfly stereoacuity test were analyzed as 2000 seconds of arc (if correct response). Nil was defined as an incorrect response on the butterfly (n=67 and n=56 in binocular and patching groups, respectively), or on the 800 seconds of arc level of the Randot Preschool stereoacuity test if the butterfly was not attempted (n=2 and n=1 in binocular and patching groups, respectively)
Visit Completion and Treatment Adherence
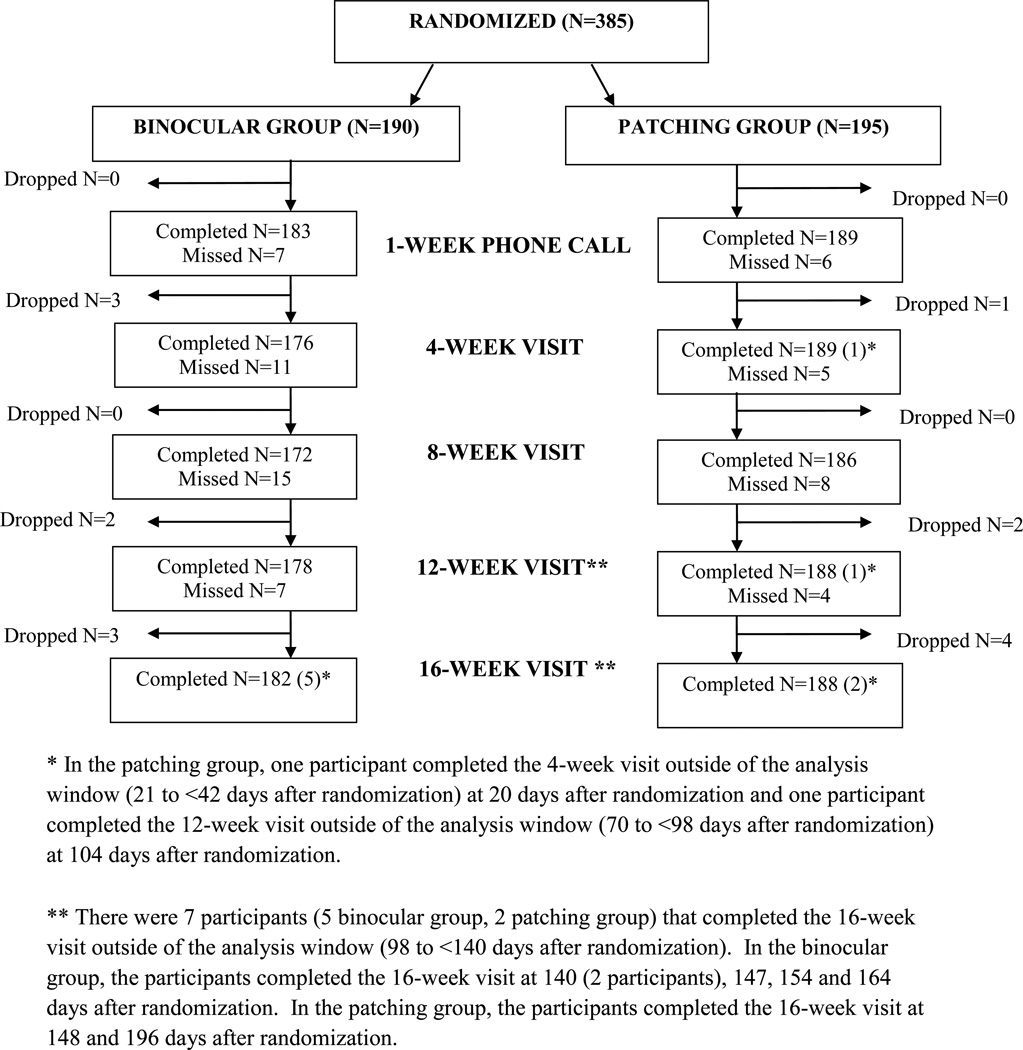
The 16-week primary outcome was completed by 182 (96%) in the binocular group and 188 (96%) in the patching group (Figure 1), with masking maintained at 99% of visits.
Figure 1. Visit completion by treatment group.
Flowchart showing study completion in each treatment group.
During the 16-week follow-up period, 118 (67%) in the binocular group and 172 (92%) in the patching group reported completing >75% of prescribed treatment based on calendars. However, for the binocular group, the iPad device indicated only 22% of participants achieved >75% (median 46%, interquartile range 20% to 72%) of prescribed treatment. Only two participants in the binocular group had been prescribed less than the 1 hour/d 7 days/week intended dose during follow-up. In the binocular group, 100% contrast in the fellow eye was achieved for 35 participants (20%) at 4 weeks and for 86 participants (49%) at 16 weeks. Thirty-one (18%) participants had 20% contrast or worse, to the fellow eye, at 16 weeks. Non-protocol alternative treatment was received by no participants in the patching group and 4 participants in the binocular group (1 atropine, 3 patching, one of whom received patching in addition to protocol binocular therapy).
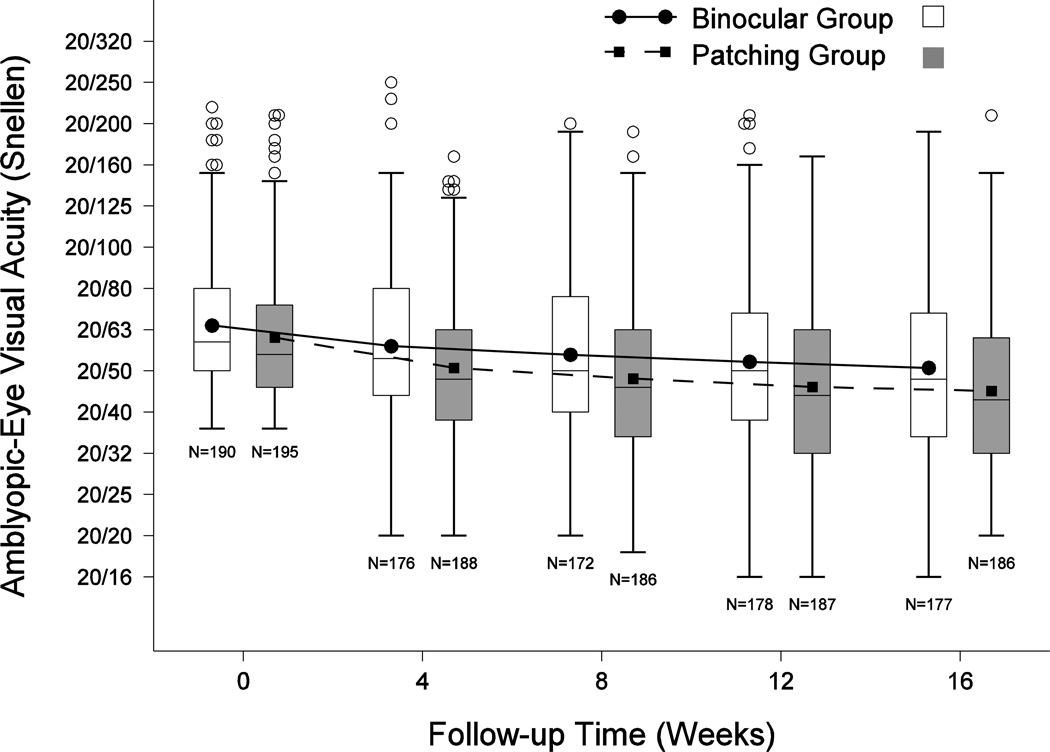
Amblyopic-Eye Visual Acuity
At 16 weeks, mean amblyopic-eye VA improved from baseline by 1.08 lines (2-sided 95% confidence interval (CI): 0.86 to 1.29 lines) in the binocular group and by 1.32 lines (2-sided 95% CI: 1.14 to 1.51 lines) in the patching group (Figure 2, eFigure 1, eTable 2, Table 3). After adjusting for baseline covariates of age and VA, mean amblyopic eye VA improved from baseline by 1.05 lines (95% CI: 0.85 to 1.24 lines) and 1.35 lines (95% CI: 1.17 to 1.54 lines) in the patching and binocular groups respectively, resulting in a treatment group difference of 0.31 lines favoring the patching group. The upper limit of the 1-sided 95% CI of the treatment difference was 0.53 lines, which exceeded the pre-specified non-inferiority limit of 0.5 lines. Because we were unable to reject the null hypothesis (that binocular treatment was inferior to patching), our primary analysis was indeterminate. In a post-hoc analysis, the 2-sided 95% CI for the adjusted treatment group difference was 0.04 to 0.58 lines, favoring the patching group. Results of alternative analyses were consistent with the primary analysis (eTable 1).
Figure 2. Visual acuity (VA) in amblyopic eyes from baseline to 16 weeks.
At each time point, the left box represents the binocular group (joined by solid line) and the right represents the patching group (joined by dashed line). Bottom and top of each box represents the 25th and 75th percentiles. Line in the box is the median and dot the mean. Bars above and below extend to the closest observed data point inside 1.5 times the interquartile range and open circles represent near statistical outliers and the asterisks indicate far outliers.
Table 3.
Amblyopic-eye Visual Acuity Outcomes at 16 Weeks by Treatment Group a
| Binocular Group (N=177) |
Patching Group (N=186) |
|||
|---|---|---|---|---|
| N | % | N | % | |
| Distribution of Amblyopic-eye Visual Acuity | ||||
| 20/200 (33–37 Letters) | 2 | 1 | 1 | <1 |
| 20/160 (38–42 Letters) | 2 | 1 | 3 | 2 |
| 20/125 (43–47 Letters) | 10 | 6 | 2 | 1 |
| 20/100 (48–52 Letters) | 12 | 7 | 7 | 4 |
| 20/80 (53–57 Letters) | 18 | 10 | 17 | 9 |
| 20/63 (58–62 Letters) | 25 | 14 | 22 | 12 |
| 20/50 (63–67 Letters) | 30 | 17 | 38 | 20 |
| 20/40 (68–72 Letters) | 32 | 18 | 37 | 20 |
| 20/32 (73–77 Letters) | 33 | 19 | 27 | 15 |
| 20/25 (78–82 Letters) | 8 | 5 | 22 | 12 |
| 20/20 (83–87 Letters) | 3 | 2 | 10 | 5 |
| 20/16 (88–92 Letters) | 2 | 1 | 0 | 0 |
| Mean (SD) LogMAR | 0.41 (0.21) | 0.35 (0.20) | ||
| Snellen Equivalent | 20/50−1 | 20/50+2 | ||
| Distribution of Amblyopic-eye Visual Acuity Change | ||||
| ≥ 3 lines (≥ 15 letters) better | 19 | 11 | 29 | 16 |
| 2 lines (10–14 letters) better | 32 | 18 | 36 | 19 |
| 1 line (5–9 letters) better | 47 | 27 | 46 | 25 |
| 0 line (within 4 letters) | 64 | 36 | 69 | 37 |
| 1 line (5–9 letters) worse | 12 | 7 | 6 | 3 |
| 2 lines (10–14 letters) worse | 1 | <1 | 0 | 0 |
| ≥ 3 lines (≥ 15 letters) worse | 2 | 1 | 0 | 0 |
| Unadjusted Mean (95% CI) Lines | 1.08 (0.86 to 1.29) | 1.32 (1.14 to 1.51) | ||
| Adjusted Mean (95% CI) Lines | 1.05 (0.85 to 1.24) | 1.35 (1.17 to 1.54) | ||
|
Participants with Amblyopic-eye Improvement of ≥ 2 Lines (≥ 10 Letters) from Baseline |
51 | 29 | 65 | 35 |
| Treatment Group Difference (95% CI) c | 5% (−4% to 13%) | |||
| Participants with Amblyopia Resolutionb | 8 | 5 | 18 | 10 |
| Treatment Group Difference (95% CI) c | 2% (−1% to 5%) | |||
SD = standard deviation, CI = confidence interval
Visual acuity analyses only included data from participants who completed the 16-week visit within the pre-defined analysis window (14 to <20 weeks after randomization).
Amblyopia resolution was defined as having an amblyopic-eye visual acuity of 20/25 or better (≥ 78 letters) and an interocular difference within 1 line (≤ 5 letters).
Binomial regression was used to compute the treatment group difference, which was adjusted for baseline age group (5 to <7, 7 to <13 years) and baseline visual acuity. For the treatment group comparison of amblyopic-eye visual acuity of ≥ 2 lines, the baseline amblyopic-eye visual acuity was treated as a continuous covariate in the model whereas this variable was included as a categorical factor (20/40, 20/50 or worse) for the treatment group comparison of amblyopia resolution. Due to model convergence issues, age was included as a categorical factor in the model (and baseline visual acuity for amblyopia resolution). Positive values favor the patching group.
At 16-weeks, amblyopic-eye VA improved ≥ 2 lines from baseline for 65 (35%) and 51 (29%) participants in the patching and binocular groups, respectively (adjusted difference: 5%, 2-sided 95% CI: −4% to 13%), and amblyopia resolved (VA of 20/25 or better and within 1 logMAR line of fellow eye) for 18 (10%) and 8 (5%) participants in the patching and binocular groups, respectively (adjusted difference: 2%, 2-sided 95% CI: −1% to 5%). The rate of amblyopic-eye VA improvement was not statistically different between treatment groups (P = 0.83, Figure 2).
Treatment effect by baseline characteristics
The overall reduced effect of binocular treatment compared with patching on improvement of amblyopic-eye VA was paralleled in baseline subgroups (eTable 3). For both treatment groups, there was a particularly noticeable improvement in younger participants (5 to <7 years) with no prior treatment (2.5 ± 1.5 lines in the binocular group and 2.8 ± 0.8 lines in the patching group) (eTable 3).
VA improvement in binocular group by compliance
At both 4 and 16 weeks, improvement in amblyopic-eye VA was not associated with objective measures of total hours of treatment or change in fellow-eye contrast for the binocular group, overall (eFigure 2, eFigure 3), or within baseline subgroups of age (5 to <7 years, 7 to <13 years) with or without previous treatment (eFigure 4, eFigure 5). In addition, mean improvement in 16-week amblyopic-eye VA for participants who completed >50% of prescribed treatment and achieved >95% fellow-eye contrast was 0.9 ± 1.4 line (n=51) compared with 1.2 ± 1.5 lines (n=125) in those who did not fulfill these criteria.
Stereoacuity
Change in stereoacuity did not differ significantly between treatment groups for the overall cohort (P = 0.66) or for participants with no history of strabismus at baseline (P = 0.19) (eTable 4). The median change in stereoacuity from baseline to 16 weeks was 0 in both groups, and there was a similar lack of an effect of binocular treatment and patching on change in stereoacuity in baseline subgroups (eTable 5).
At both 4 and 16 weeks, improvement in stereoacuity was not associated with either total hours of completed binocular treatment or change in fellow-eye contrast, either overall (eFigure 2, eFigure 3) or within baseline subgroups of age (5 to <7 years, 7 to <13 years) with or without previous treatment (eFigure 6, eFigure 7). At 16 weeks, median stereoacuity improvement was 0 for participants who completed >50% prescribed binocular treatment and achieved >95% fellow-eye contrast (n=51) and 0 for those who did not fulfill these criteria (n=124).
VA of Fellow Eye at 16 weeks
Mean improvement in fellow-eye VA, adjusted for baseline VA, differed by 0.16 lines (95% CI: 0.02 to 0.30 lines) favoring the binocular group (eTable 6).
Adverse Events at 16 weeks
The number of participants with a new tropia and/or worsening of a pre-existing deviation of ≥ 10 Δ was 16 (9%) and 11 (6%) in the binocular and patching groups, respectively (Fisher exact test: P = 0.32). Diplopia was rare in both groups (eTable 7).
Three participants (2%) in the patching group reported moderate/severe skin irritation with patching during follow-up.
Discussion
In children 5 to 12 years of age, amblyopic-eye VA improved in both the binocular and patching groups, particularly in younger participants (5 to 6 years) without prior amblyopia treatment. VA improvement in the binocular group did not meet the pre-specified definition for non-inferiority compared with 2 hours of prescribed daily patching, and therefore our primary analysis was indeterminate. Nevertheless, a post-hoc analysis suggested VA improvement with this particular binocular iPad treatment was not as good as with 2 hours of prescribed daily patching.
Mean improvement in amblyopic-eye VA with binocular treatment over our 16-week study was similar in magnitude (approximately 1 logMAR line) to that previously reported in non-randomized studies prescribing 4 hours/week of binocular treatment for 4 weeks in 4 to 12 year-olds,3, 5 and in 3 to 6 year-olds.4 These previous studies3–5 of binocular iPad treatment included 4 different games, one of which was the falling blocks game, and allowed concurrent patching at a different time of day at the eye care provider’s discretion, although a sub-analysis of those only treated with binocular games yielded a similar magnitude of effect.4 Knox et al2 also found a similar magnitude of improvement in children (mean age 8.5 years) treated with an analogous game, using a head-mounted display in a supervised setting for 1 hour/day for 5 sessions over one week. The rate of improvement in amblyopic-eye VA was slower in the present study than in these previous studies,3–5 which may have been due to a larger proportion of older participants in the present study.
When treating adults with amblyopia using binocular therapy in a supervised setting for 1 hour/day over 2 weeks, Li et al6 reported a mean improvement of approximately 2 logMAR lines, greater than that found in the present study of children. Nevertheless, this treatment in adults was in a laboratory setting using a head-mounted display, so results cannot be directly compared.
In our study, investigators noted participants often lost interest in the game after a number of days or weeks, well before the prescribed 16-week course was completed. Only 22% of our children achieved greater than 75% compliance, suggesting that compliance should be reviewed more frequently and games need to be more appealing such as more engrossing children’s games, binocular first person action games,18 and binocular movie viewing.19
Another reason why we may not have found a greater effect of binocular treatment was the timing of the initial and final assessments. Previous studies of binocular therapy have evaluated patients after a shorter duration of treatment. It is unclear whether active progression through contrast levels is necessary for treatment to be ongoing, or whether treatment is ongoing even when equal contrast has been achieved. If active progression is needed, many of our children who achieved 100% contrast to the fellow eye would have completed treatment well before our primary outcome (49%) and even before 4 weeks (20%). We also found that 18% of participants failed to progress in contrast to the fellow eye, suggesting that the contrast starting point was not optimally set for each participant, and that the initial contrast should be based on an individual measurement of suppression rather than the arbitrary 20% used here.
Regarding improvement of stereoacuity, it has been suggested that the mechanism of binocular treatment of amblyopia is by reducing suppression and increasing binocularity. Stereoacuity outcomes differ between studies, with some reporting improvement1, 2 and others (like ours) reporting no improvement for most subjects.3, 4 It is possible that these differences may be due to the type of stereoacuity test used. Improvements might be more easily detected using the Frisby test or contour tests, rather than random dot tests.20, 21
It remains unclear that the binocular iPad treatment used in our study was actually better than optical treatment alone (if needed) and, as such, whether binocular iPad treatment is actually better than sham therapy. Nevertheless, the large magnitude of the VA improvement in the younger participants (5 to <7 years old) in the binocular group, who had not received previous treatment, (2.5 ± 1.5 lines) suggests that binocular treatment produced a real effect, greater than would be expected with continued optical treatment alone after achieving stable VA in spectacles.15 Regarding the effect of patching in our study, our overall mean improvement (1.3 logMAR lines) was less than we expected, but this was most likely due to a large proportion (63%) of participants who were both older (7 to <13 years) and who had received previous treatment.
There has been some concern that binocular treatment might be associated with new-onset diplopia because its mechanism of action may be via anti-suppression. Nevertheless, In our study, and in previous studies of this particular form of binocular treatment,3–5 diplopia was rare.
Our study has a number of limitations regarding assessing compliance. For patching, we did not use occlusion dose monitors. Our compliance data relied on parental report (for patching and, in part, for binocular treatment) which may have been inaccurate. The electronic recording of compliance by the binocular game may have also included time when the game was not actually being played, but this would be expected to be minimal because the game sessions automatically ended after about 1 minute of inactivity. For binocular treatment, we allowed participants to play a minimum of 4 days per week, if they could not play 7 days per week, but reduced game play was only prescribed in 2 subjects. Finally, we did not monitor compliance with wearing the red-green glasses required to play the game.
In summary, in children 5 to 12 years of age, amblyopic-eye VA improved with binocular game play and with patching, but VA improvement with this particular binocular iPad treatment, when prescribed 1 hour a day, failed to meet our study’s pre-specified definition for non-inferiority compared with 2 hours of prescribed daily patching, and therefore our primary analysis was indeterminate. Nevertheless, a post-hoc analysis suggested VA improvement with this particular binocular iPad treatment was not as good as with 2 hours of prescribed daily patching.
Supplementary Material
Acknowledgments
Funding/Support: This study was supported by the National Eye Institute of National Institutes of Health, Department of Health and Human Services EY011751, EY023198, and EY018810.
One clinical site denoted with an † in the list of clinical sites received support from NIH grant EY010572 to fund shared departmental resources for research purposes. Five clinical sites denoted with an * in the list of clinical sites received support utilized for this project from an unrestricted grant from Research to Prevent Blindness (RPB) Inc., New York, New York.
No funding organization had any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Appendix
Clinical Sites
Sites are listed in order by number of participants enrolled. Personnel are listed as (I) for Investigator, (C) for Coordinator or (E) for Examiner.
Norfolk, VA - Virginia Pediatric Eye Center (31)
Earl R. Crouch, Jr. (I); Earl R. Crouch III (I); Stacy R. Martinson (I); Gaylord G. Ventura (C); Candice C. Brown (E); Cynthea M. Carlton (E); Carolina A. Escala (E)
Miami, FL - Bascom Palmer Eye Institute (19)
Susanna M. Tamkins (I); Carolina Manchola-Orozco (C); Kara M. Cavuoto (E); Isaura Gomez Tamayo (E); Maria D. Martinez (E); Eva M. Olivares (E); Oriel Spierer (E); Erin Yanowitch (E)
Gainesville, FL - Accent Physicians (17)
Nausheen Khuddus (I); Kathy Bryan (C); Tammy Toskes Price (E)
Rockville, MD - Stephen R. Glaser (17)
Stephen R. Glaser (I); Tara G. Missoi (I); Nancy A. Morrison (I); Kasey L. Yost (C); Deandra B. Andrade (E); Odalis R. Flores (E)
Poland, OH - Eye Care Associates, Inc. (15)
S. Ayse Erzurum (I); Beth J. Colon (C); Diana C. McOwen (C); Guy C. Barrett (E); Zainab Dinani (E)
Cranberry TWP, PA - Everett and Hurite Ophthalmic Association (14)
Darren L. Hoover (I); Pamela A. Huston (C); Christine J. Deifel (E); Jody L. Desiderio (E); Pamela M. Racan (E); Kari E. Soros (E)
Chattanooga, TN - Pediatric Eye Specialists (11)
Edward A. Peterson (I); Zachary S. McCarty (I); Charla H. Peterson (C); Amie Jenkins (E)
Fullerton, CA - Southern California College of Optometry (11)
Susan A. Cotter (I); Angela M. Chen (I); Raymond H. Chu (I); Silvia Han (I); Catherine L. Heyman (I); Kristine Huang (I); Sue M. Parker (C); Reena A. Patel (I); Maureen D. Plaumann (I); Carlee Y. Young (I); Carmen N. Barnhardt (E)
Houston, TX - University of Houston College of Optometry (11)
Karen D. Fern (I); Heather A. Anderson (I); Debra C. Currie (I); Dashaini V. Retnasothie (I); Sylvia Landa (C); Fawn M. Candelari (C)
Portland, OR - Casey Eye Institute (11)*, †
Allison I. Summers (I); Paula K. Rauch (C); Yelena M. Bubnov (E); Grant A. Casey (E); Rhea N. Nelson (E); Kevin M. Woodruff (E)
The Woodlands, TX - Houston Eye Associates (11)
Aaron M. Miller (I); Jorie Jackson (C); Angela C. Dillon (C); Kathleen M. Curtin (E); Maria N. Olvera (E); Starla J. Skaggs (E)
Birmingham, AL - University of Alabama at Birmingham School of Optometry (10)
Marcela Frazier (I); Kristine T. Hopkins (I); Sarah D. Lee (I); Katherine K. Weise (I); Paul Christian Spain (C); Michelle B. Bowen (C)
Baltimore, MD - Wilmer Institute (9)*
Michael X. Repka (I); Courtney Kraus (I); Anya A. Trumler (I); Xiaonong Liu (C); Alex X. Christoff (E); Kyle Pearce Harrold (E); Colin Patrick Kane (E)
Cincinnati, OH - Cincinnati Children’s Hospital (9)
Michael E. Gray (I); Melissa L. Rice (I); Daniele P. Saltarelli (I); Corey S. Bowman (C); Shemeka R. Forte (E); Amanda R. Johnson (E); Erica M. Setser (E); Miqua LThomas (E); Felicia J. Timmermann (E)
Boise, ID - St Luke’s Hospital (7)
Katherine A. Lee (I); Daniel R. Brooks (I); Bonita R. Schweinler (C); Lori Lynne McDaniel (E); Larry W. Plum (E)
Grand Rapids, MI - Helen DeVos Children’s Hospital Pediatric Ophth. (7)
Brooke E. Geddie (I); Elisabeth T. Wolinski (C); Kimberly J. Hubbard (E); Michael N. Patton (E)
Rochester, MN - Mayo Clinic (7)*
Jonathan M. Holmes (I); Suzanne M. Wernimont (C); Matthew W. Heiderscheit (E); Anita R. Hermanson (E); Julie A. Holmquist (E); Jordan J. Huisman (E); Melissa J. Hunemuller (E); Lindsay D. Klaehn (E); Marna L. Levisen (E); Laura Liebermann (E); Rebecca A. Nielsen (E); Debbie M. Priebe (E); Casandra M. Turri (E)
Spokane, WA - Northwest Pediatric Ophthalmology, P.S. (7)
George F. Whitehead (I); Christina N. Nye (I); Caroline J. Shea (I); SueAnn M. Stillman (C)
Atlanta, GA - The Emory Eye Center (6)
Scott R. Lambert (I); Amy K. Hutchinson (I); Phoebe D. Lenhart (I); Judy L. Brower (C); Jayne M. Brown (E); Linda T. Curtis (E); Melanie K. Fowler (E); Marla J. Shainberg (E)
Lancaster, PA - Conestoga Eye (6)
David I. Silbert (I); Noelle S. Matta (C); Karen L. Delgado (E); Prucilla R. Shady (E)
Waterbury, CT - Eye Care Group, PC (6)
Tara H. Cronin (I); Andrew J. Levada (I); Susan H. Heaton (C); Cheryl Capobianco (E); Lindsay Gill (E)
Big Rapids, MI - Michigan College of Optometry at Ferris State Univ (5)
Paula S. McDowell (I); Alison M. Jenerou (I); Kerrie Rachelle Currie (C); Emily Jean Aslakson (E); Sarah B. Hinkley (E)
Chicago, IL - Illinois College of Optometry (ICO) (5)
Yi Pang (I); Huizi Yin (I); Elyse Nylin (C)
Erie, PA - Pediatric Ophthalmology of Erie (5)
Nicholas A. Sala (I); Allyson Sala (C); Catherine Johnson (E); V. Lori Zeto (E)
Grand Rapids, MI - Pediatric Ophthalmology, P.C. (5)
Patrick J. Droste (I); Robert J. Peters (I); Jan Hilbrands (C); Leslie J. Bileth (E); Andrew P. Droste (E); Jennifer L. Mooney (E)
Rochester, NY - University of Rochester Eye Institute (5)
Benjamin P. Hammond (I); Matthew D. Gearinger (I); Andrea Czubinski (C); Rebecca K. Gerhart (E)
Silverdale, WA - Jason C. Cheung, M.D., PS (5)
Jason C. Cheung (I); Tiffany M. Parypa (C); Jacque J. Ferro (E)
West Des Moines, IA - Wolfe Clinic (5)
Myra N. Mendoza (I); Sara D. Khan (I); Jill J. Frohwein (C); Lisa M. Fergus (E); Susan K. Hayes (E); Rhonda J. Countryman (E)
Chicago Ridge, IL - The Eye Specialists Center, L.L.C. (4)
Benjamin H. Ticho (I); Megan Allen (I); Birva K. Shah (I); Deborah A. Clausius (C); Sharon L. Giers (E); Micaela N. Quebbemann (E)
Cleveland, OH - Cole Eye Institute (4)
Fatema F. Ghasia (I); Diana C. McOwen (C); Susan W. Crowe (C); Angela M. Borer (E); Rachael Briggs (E)
Fall River, MA - Center for Eye Health, Inc. (4)
John P. Donahue (I); Samantha J. Pape (C); Danielle K. Berry (E); Linda M. Cabeceiras (E); Mary E. Silvia (E); Samantha Teixeira (E)
Houston, TX - University of Texas- Robert Cizik Eye Clinic (4)
Kartik S. Kumar (I); Ephrem K. Melese (C); Laura A. Baker (E)
Marlton, NJ - Michael F. Gallaway, O.D., P.C. (4)
Michael F. Gallaway (I); Debbie L. Killion (C); Tammy Lynn Thomas (E); Beth Zlock (E)
Portland, OR - Pacific University College of Optometry (4)
Richard London (I); Ryan C. Bulson (I); Jayne L. Silver (C); James J. Kundart (E)
Rio Rancho, NM - City of Vision Eye Care (4)
Lisa M. Edwards (I); Carolyn Sue Marquez (C); Jessica Noel Marquez (E); Tristan Lee Martinez (E)
Wilmette, IL - Pediatric Eye Associates (4)
Lisa C. Verderber (I); Deborah R. Fishman (I); Roberta A. Forde (C); Sarah Ahn (E); Adam J. Julian (E)
Aberdeen, NC - Family Eye Care of the Carolinas (3)
Michael J. Bartiss (I); Tennille F. McGaw (C); Leah M. Kelly (E); Lauren E. Simmons (E)
Arnold, MD - Ophthalmology Associates of Greater Annapolis (3)
John M. Avallone (I); Charlene R. Bryant (C); Wanda E. Peyton (E)
Chicago, IL - Ann & Robert H. Lurie Children’s Hospital of Chicago (3)
Bahram Rahmani (I); Sudhi P. Kurup (I); Magdalena Stec (I); Hawke H. Yoon (I); Janice B. Zeid (I); Hantamalala Ralay Ranaivo (C); Kristyn M. Magwire (E); Erika A. Talip (E); Vivian Tzanetakos (E)
Durham, NC - Duke University Eye Center (3)
Laura B. Enyedi (I); David K. Wallace (I); Sarah K. Jones (C); Courtney E. Fuller (E); Namita Kashyap (E)
Houston, TX - Texas Children's Hospital - Dept. Of Ophthalmology (3)
Evelyn A. Paysse (I); Amit R. Bhatt (I); Kimberly G. Yen (I); Lingkun Kong (C); Melynda T. Homann (E)
Kansas City, MO – Children’s Mercy Hospitals and Clinics (3)
Amy L. Waters (I); Christina M. Twardowski (I); Rebecca J. Dent (C); Lori L. Soske (C); Lezlie L. Bond (E); Cindy J. Cline (E)
Kingston, Canada - Children’s Eye Research Center (3)
Brian W. Arthur (I); Lesley E. MacSween (E)
Mayfield Hts, OH - Rainbow Babies and Children’s Hospital Dept of Ophth (3)*
Faruk H. Orge (I); Alicia Marie Baird (C); Veronica Marie Bontempo (E)
Munster, IN - The Eye Specialist Center, LLC (3)
Birva K. Shah (I); Micaela N. Quebbemann (C); Deborah Ann Clausius (E)
Omaha, NE - University of Nebraska Medical Center (3)
Donny W. Suh (I); Carolyn Chamberlain (C); Whitney R. Brown (E); Joel O. Rivas (E); Dimitra M. Triantafilou (E)
Pittsburgh, PA - UPMC Children’s Eye Center of Children’s Hospital of Pittsburgh (3)
Ken K. Nischal (I); Ellen B. Mitchell (I); Lauren Bolling (C); Bianca Blaha (E); Whitney Churchfield (E); Christina Fulwylie (E)
Aurora, CO - Univ. Of Colorado HSC (2)
Emily A. McCourt (I); Daniel E. Smith (I); Nanastasia Welnick (C); Susan James (E); Sarah E. Peck (E)
Bloomington, IN - Indiana University School Of Optometry (2)
Don W. Lyon (I); Kristy M. Dunlap (C); Vidhyapriya Sreenivasan (E); Yifei Wu (E)
Charleston, SC - Medical Univ of South Carolina, Storm Eye Instit. (2)
Edward W. Cheeseman (I); Carol U. Bradham (C); Paige P. Edwards (E); Carole M. Lemieux (E)
Columbus, OH - Pediatric Ophthalmology Associates (2)
Don L. Bremer (I); Richard P. Golden (I); Mary Lou McGregor (I); Meghan C. McMillin (C); Sara Ann Oravec (C); Andrea Nicole Gearhart (E); Benita Nechell Mansperger (E)
Dubuque, IA - Medical Associates Clinic P.C. (2)
Timothy J. Daley (I); Shannon R. Walsh (C); Cheyanne M. Hoeger (E)
Ft. Lauderdale, FL - Nova Southeastern University College of Optometry, The Eye Institute (2)
Michael Au (I); Jacqueline Rodena (I); Yin C. Tea (I); Nadine Girgis Hanna (I); Erin Jenewein (I); Surbhi Bansal (C)
Little Rock, AR - Arkansas Childrens Hospital/University of Arkansas Medical Sciences (2)
Robert Scott Lowery (I); Paul H. Phillips (I); Brita S. Deacon (I); Kelly D. To (C); Shawn L. Cupit (E)
Minneapolis, MN - University of Minnesota (2)*
Raymond G. Areaux (I); Sara J. Downes (I); Ann M. Holleschau (C); Kathy M. Hogue (E); Andrea M. Kramer (E); Kim S. Merrill (E)
Montreal, Canada - CHU - Sainte-Justine (2)
Rosanne Superstein (I); Maryse Thibeault (C); Emma Chilliet (E); Charlotte Riguidel (E)
Philadelphia, PA - Salus University/Pennsylvania College of Optometry (2)
Erin C. Jenewein (I); Mitchell M. Scheiman (I); Karen E. Pollack (C); Michael F. Gallaway (E); Jenny Myung (E); Ruth Y. Shoge (E)
Seattle, WA - Seattle Children's Hospital (2)
Vivian Manh (I); Lyndsey A. Tews (C); Amy Gladstone (E); Jennifer Vincent (E)
Spokane, WA - Spokane Eye Clinic (2)
Jeffrey D. Colburn (I); Eileen Dittman (C); Dylan C. Waidelich (E); Marilyn M. Westerman (E)
Wheaton, IL - Wheaton Eye Clinic (2)
Noha S. Ekdawi (I); Darin L. Strako (C); Brittany Freese (E); Maria T. Jimenez (E)
Baltimore, MD - Greater Baltimore Medical Center (1)
Mary Louise Z. Collins (I); Allison A. Jensen (I); Maureen A. Flanagan (C); Saman Bhatti (E); Cheryl L. McCarus (E); Srianna Narain (E)
Boston, MA - Boston Medical Center (1)
Jenna R. Titelbaum (I); Jean E. Ramsey (I); Stephen P. Christiansen (I); Kate Hutton McConnell (C); Kelly M. Castle (E); Jennifer E. Lambert (E)
Boston, MA - Harvard Vanguard Medical Associates (1)
Mei L. Mellott (I); Troy L. Kieser (C); Linette Miranda (E)
Calgary, Canada - Alberta Children's Hospital (1)
William F. Astle (I); Emi N. Sanders (C); Zuzana Ecerova (E); Charlene D. Gillis (E); Catriona I. Kerr (E); Shannon L. Steeves (E); Heather N. Sandusky (E)
Concord, NH - Concord Ophthalmologic Associates (1)
Christie L. Morse (I); Melanie L. Christian (C); Caroline C. Fang (E)
Glendale, AZ - Midwestern University Eye Institute (1)
Paula A. Handford (I); Alicia E. Feis (I); Christina A. Esposito (I); Tracy A. Bland (C)
Hurricane, WV - Marshall University (1)
Deborah L. Klimek (I); Ginger Peters (C); Amanda C. Conley (E); Sara E. Miramontes (E); Sonya G. Walls (E)
Indianapolis, IN - Riley Hospital for Children (1)
Kathryn M. Haider (I); Michele E. Whitaker (C); Adam J. Harshbarger (E); Jingyun Wang (E)
Iowa City, IA - University of Iowa Hospitals and Clinics (1)
Scott A. Larson (I); Xiaoyan Shan (C); Tara L. Bragg (E); Miriam Di Menna (E)
Jacksonville, FL - Nemours Children’s Specialty Care (1)
John W. Erickson (I); Charlotte Ann Louise Reaser (C); Gracie Sylvester (E)
Lincoln, NE - Eye Surgical Associates (1)
Donald P. Sauberan (I); Jody C. Hemberger (C); Gail Walker (E)
Nashville, TN - Vanderbilt Eye Center (1)
Sean P. Donahue (I); Lori Ann F. Kehler (I); Scott T. Ruark (C); Lisa A. Fraine (E); Ronald J. Biernacki (E)
New Haven, CT - Yale Univ. Med. School, Dept. of Ophthal. & Visual Science (1)
Jennifer A. Galvin (I); Margaret B. Therriault (C); Jaime Harrison (E); Christine C. Medina (E)
New York, NY - State University of New York, College of Optometry (1)
Marilyn Vricella (I); Erica L. Schulman-Ellis (I); Valerie Leung (C); Rochelle Mozlin (E)
Oklahoma City, OK - Dean McGee Eye Institute (1)
Tammy L. Yanovitch (I); Keven W. Lunsford (C); Lauren Ukleya (C); Shannon Almeida (E); Vanessa K. Drummond (E); Sonny William Icks (E); Lauren Pendarvis (E)
Saint Paul, MN - Associated Eye Care (1)
Susan Schloff (I); Kristi D. Neuenfeldt (E); Cheera M. Sundgaard (E)
Schaumburg, IL - Advanced Vision Center (1)
Ingryd J. Lorenzana (I); Beata Wajs (C); Angelyque L. Lorenzana (E); Yesenia Meza (E)
Toms River, NJ - Ocean Eye Institute (1)
Michael J. Spedick (I); Katelyn Karausky (C); Emily Guyer (E); Mary A. Lizardo (E); Dena Mitchell (E); Pamela Stokes (E)
PEDIG Coordinating Center - Tampa, FL
Raymond T. Kraker, Roy W. Beck, Darrell S. Austin, Nicole M. Boyle, Courtney L. Conner, Danielle L. Chandler, Trevano W. Dean, Quayleen Donahue, Brooke P. Fimbel, Graham M. Hardt, James E. Hoepner, Joseph D. Kaplon, Elizabeth L. Lazar, B. Michele Melia, Gillaine Ortiz, Diana E. Rojas, Jennifer A. Shah, Rui Wu.
ATS18 Planning Committee
Jonathan M. Holmes (Co-Chair), Vivian Manh (Co-Chair), Eileen B. Birch, Susan A. Cotter, Robert F. Hess (Consultant), Kristine B. Hopkins, Raymond T. Kraker, Elizabeth L. Lazar, David A. Leske, Donald W. Lyon, B. Michele Melia, Michael X. Repka, David K. Wallace.
National Eye Institute - Bethesda, MD
Donald F. Everett
PEDIG Executive Committee
David K. Wallace (chair), William F. Astle (2013–2015), Roy W. Beck, Eileen E. Birch, Susan A. Cotter (2011–2014, 2015-present), Eric R. Crouch (2014–2015), Laura B. Enyedi (2014-present), Donald F. Everett, Jonathan M. Holmes, Raymond T. Kraker, Scott R. Lambert (2013–2015), Katherine A. Lee (2014-present), Ruth E. Manny, Michael X. Repka, Jayne L. Silver (2014-present), Katherine K. Weise (2014-present), Lisa C. Verderber (2015-present).
Amblyopia Treatment Study Steering Committee
Eileen E. Birch, Trevano W. Dean, Donald F. Everett, Michael E. Gray (2016-present), Jonathan M. Holmes, Raymond T. Kraker, Marjean T. Kulp, Sylvia Landa, Elizabeth L. Lazar, Vivian Manh, Diana McOwen (2014–2015), B. Michele Melia, Evelyn A. Paysse, Donny W. Suh, Allison I. Summers (2016-present), Rosanne Superstein (2014–2015), David K. Wallace.
Data and Safety Monitoring Committee
Marie Diener-West (chair), John D. Baker, Barry Davis, Donald F. Everett, Dale L. Phelps, Stephen W. Poff, Richard A. Saunders, Lawrence Tychsen.
Footnotes
Trial Registration: Listed on www.clinicaltrials.gov, identifier NCT02200211.
Access to Data: Elizabeth Lazar had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Conflict of Interest: No conflicting relationships exist for any of the authors.
References
- 1.Hess RF, Mansouri B, Thompson B. A new binocular approach to the treatment of amblyopia in adults well beyond the critical period of visual development. Restor Neurol Neurosci. 2010;28(6):793–802. doi: 10.3233/RNN-2010-0550. [DOI] [PubMed] [Google Scholar]
- 2.Knox PJ, Simmers AJ, Gray LS, Cleary M. An exploratory study: prolonged periods of binocular stimulation can provide an effective treatment for childhood amblyopia. Invest Ophthalmol & Vis Sci. 2012;53(2):817–824. doi: 10.1167/iovs.11-8219. [DOI] [PubMed] [Google Scholar]
- 3.Li SL, Jost RM, Morale SE, et al. A binocular iPad treatment for amblyopic children. Eye (Lond) 2014;28(10):1246–1253. doi: 10.1038/eye.2014.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Birch EE, Li SL, Jost RM, et al. Binocular iPad treatment for amblyopia in preschool children. J AAPOS. 2015;19(1):6–11. doi: 10.1016/j.jaapos.2014.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li SL, Jost RM, Morale SE, et al. Binocular iPad treatment of amblyopia for lasting improvement of visual acuity. JAMA Ophthalmol. 2015;133(4):479–480. doi: 10.1001/jamaophthalmol.2014.5515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li J, Thompson B, Deng D, Chan LY, Yu M, Hess RF. Dichoptic training enables the adult amblyopic brain to learn. Curr Biol. 2013;23(8):R308–R309. doi: 10.1016/j.cub.2013.01.059. [DOI] [PubMed] [Google Scholar]
- 7.Pediatric Eye Disease Investigator Group. A randomized trial of patching regimens for treatment of moderate amblyopia in children. Arch Ophthalmol. 2003;121(5):603–611. doi: 10.1001/archopht.121.5.603. [DOI] [PubMed] [Google Scholar]
- 8.Pediatric Eye Disease Investigator Group. A randomized trial of prescribed patching regimens for treatment of severe amblyopia in children. Ophthalmology. 2003;110(11):2075–2087. doi: 10.1016/j.ophtha.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 9.Pediatric Eye Disease Investigator Group. A randomized trial of atropine vs patching for treatment of moderate amblyopia in children. Arch Ophthalmol. 2002;120(3):268–278. doi: 10.1001/archopht.120.3.268. [DOI] [PubMed] [Google Scholar]
- 10.Pediatric Eye Disease Investigator Group. A randomized trial comparing Bangerter filters and patching for the treatment of moderate amblyopia in children. Ophthalmology. 2010;117(5):998–1004. doi: 10.1016/j.ophtha.2009.10.014. 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.To L, Thompson B, Blum JR, Maehara G, Hess RF, Cooperstock JR. A game platform for treatment of amblyopia. IEEE Trans Neural Syst Rehabil Eng. 2011;19(3):280–289. doi: 10.1109/TNSRE.2011.2115255. [DOI] [PubMed] [Google Scholar]
- 12.Holmes JM, Beck RW, Repka MX, et al. The Amblyopia Treatment Study visual acuity testing protocol. Arch Ophthalmol. 2001;119(9):1345–1353. doi: 10.1001/archopht.119.9.1345. [DOI] [PubMed] [Google Scholar]
- 13.Beck RW, Moke PS, Turpin AH, et al. A computerized method of visual acuity testing: adaptation of the Early Treatment of Diabetic Retinopathy Study testing protocol. Am J Ophthalmol. 2003;135(2):194–205. doi: 10.1016/s0002-9394(02)01825-1. [DOI] [PubMed] [Google Scholar]
- 14.Pediatric Eye Disease Investigator Group. Randomized trial of treatment of amblyopia in children aged 7 to 17 years. Arch Ophthalmol. 2005;123(4):437–447. doi: 10.1001/archopht.123.4.437. [DOI] [PubMed] [Google Scholar]
- 15.Pediatric Eye Disease Investigator Group. A randomized trial to evaluate 2 hours of daily patching for strabismic and anisometropic amblyopia in children. Ophthalmology. 2006;113(6):904–912. doi: 10.1016/j.ophtha.2006.01.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pediatric Eye Disease Investigator Group. A randomized trial of near versus distance activities while patching for amblyopia in children aged 3 to less than 7 years. Ophthalmology. 2008;115(11):2071–2078. doi: 10.1016/j.ophtha.2008.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pediatric Eye Disease Investigator Group. Patching vs atropine to treat amblyopia in children aged 7 to 12 years: a randomized trial. Arch Ophthalmol. 2008;126(12):1634–1642. doi: 10.1001/archophthalmol.2008.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vedamurthy I, Nahum M, Huang SJ, et al. A dichoptic custom-made action video game as a treatment for adult amblyopia. Vision Res. 2015;114:173–187. doi: 10.1016/j.visres.2015.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li SL, Reynaud A, Hess RF, et al. Dichoptic movie viewing treats childhood amblyopia. J AAPOS. 2015;19(5):401–405. doi: 10.1016/j.jaapos.2015.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leske DA, Birch EE, Holmes JM. Real depth vs randot stereotests. Am J Ophthalmol. 2006;142(4):699–701. doi: 10.1016/j.ajo.2006.04.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Levi DM, Knill DC, Bavelier D. Stereopsis and amblyopia: A mini-review. Vision Res. 2015;114:17–30. doi: 10.1016/j.visres.2015.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.