Abstract
Background:
Men who have sex with men (MSM) and female sex workers (FSW) are consistently shown to have a higher burden of HIV compared with other adults in Senegal. This study, HIV Prevention 2.0, evaluates the impact of the 3-tiered integrated stigma mitigation interventions (ISMIs) approach to optimizing HIV service delivery for key populations in Senegal.
Methods:
Baseline assessment includes a questionnaire and biological testing for HIV. A proportion of participants enrolled into a 24-month longitudinal cohort with questionnaires and biological testing every 3 months. In these preliminary analyses, ISMIs are evaluated from participants in the cohort through uptake of HIV services and implementation outcomes.
Results:
Overall, 724 MSM and 758 FSW participated in the baseline assessment. HIV prevalence is 30.2% (n = 219/724) among MSM and 5.3% (n = 40/758) among FSW. Fear of seeking health services among MSM is 17.7% (n = 128/724) at baseline, 10.5% (n = 18/172) at month 3, and 9.8% (n = 10/102) at month 6 (P < 0.004); and among FSW is 21.9% (n = 166/758) at baseline, 8.1% (n = 15/185) at month 3, and 10.7% (n = 18/168) at month 6 (P < 0.001). Overall, 63.9% (n = 62/97) of MSM and 82.5% (n = 118/143) of FSW agreed that the intervention is effective in addressing stigma; however, loss to follow-up was 41.1% among MSM and 10% among FSW.
Conclusion:
Baseline data reinforce the need for stigma mitigation interventions, combined with enhanced linkage and retention to optimize HIV treatment. Preliminary results show high levels of HIV-related risk determinants and suggest the potential utility of the ISMI to decrease perceived stigma relating to engagement in HIV prevention, treatment, and care services among key populations in Senegal.
Key Words: stigma, HIV, interventions, key populations, Senegal
INTRODUCTION
The government of Senegal was among the first countries across Sub-Saharan Africa to endorse and support early and broad access to antiretroviral therapy (ART) for people living with HIV (PLHIV).1 The government's approach and focus on prevention and treatment is suggested to be associated with the relatively limited overall burden of HIV in Senegal.1 Specifically, the HIV prevalence among adults of reproductive age is estimated to be approximately 0.5% in Senegal.2 In the context of a moderate burden of HIV among reproductive age adults, the burden among specific key populations has been shown to be disproportionately high. Among men who have sex with men (MSM) in Senegal, HIV incidence has been estimated to be as high as 16% per year with at least one in 5 MSM estimated to be living with HIV.3–5 Similarly, among female sex workers (FSW), the HIV prevalence has traditionally been estimated to exceed 20%; consistent with studies from other countries in West and Central Africa.4
The higher burden of HIV among populations with specific acquisition and transmission risks, including condomless anal sex with serodiscordant men, selling sex, and injection drug use, collectively called key populations, has been found in most settings studied. This disproportionate burden has long been known in higher income settings, with low-to-moderate levels among reproductive aged adults with undefined HIV acquisition risks. More recently, there continues to be an increasing understanding of specific acquisition risks among key populations even in the context of more generalized HIV epidemic settings.6 In part, this understanding has emerged from data demonstrating decreasing overall HIV incidence rates related to improved prevention options and expanded treatment.6–8 However, when studied separately, there has been sustained HIV incidence and high HIV prevalence among key populations.9
Although individual-level biological and behavioral risks among key populations are the most proximal determinants of HIV acquisition and transmission, the HIV epidemic in key populations continues to also be driven by structural level risk determinants.9–11 Consistent data suggest that the mechanism by which structural determinants increase HIV risks is by limiting the provision and uptake of effective HIV prevention, treatment, and care services.11–14 Enacted stigma, including verbal, physical, and sexual harassment, as well as discrimination within health care settings have been documented as barriers to services for key populations.10,15–19 Moreover, stigma appears to be associated with HIV-related risk practices, including higher numbers of sexual partners, limited condom and condom compatible lubricant use, and partner concurrency.14
Despite the documented experience of stigma and its impact on HIV risks among key populations across Sub-Saharan Africa, there remains relatively limited intervention data on effective stigma mitigation approaches for these populations. A recent systematic review focused on interventions addressing stigma identified only 3 interventions addressing MSM or FSW.20 The identified interventions addressing stigma toward key populations focused on stigma reduction either through individual-level information or services, or through organizational level activities. However, none of the identified interventions aimed to address stigma at the community level. Although limited studies focused on stigma mitigation for key populations, there are lessons that can be leveraged from broader HIV-related stigma mitigation interventions. It appears that stigma interventions are more effective when multiple strategies are implemented together.20 Moreover, interventions addressing multiple stigma domains, such as drivers, facilitators, and manifestations of stigma, are shown to be more effective.20 Given the consistent data suggesting the importance of stigma in mediating HIV-related outcomes and the potential impact of stigma mitigation interventions, there is a need to characterize stigma interventions specifically for key populations across Sub-Saharan Africa.
The HIV Prevention 2.0 (HP2) study is currently implementing integrated stigma mitigation interventions (ISMIs) aimed at alleviating barriers to seeking and accessing care for key populations. The ISMI Framework for Key Populations (Figure 1) is based on the modified social ecological model for HIV risk including individual, network, community, public policy, and HIV prevalence levels, and facilitates the contextualization of individual-level behaviors with network and community-level determinants of risk among MSM and FSW.21 The underlying framework for the ISMI suggests that coverage and impact of services necessitates both the provision and uptake of services. As illustrated by the framework for health communication across the HIV treatment cascade, a combination of communication approaches should be implemented to best impact behaviors in the HIV care continuum.22 In this study, we hypothesize that stigma is acting as a barrier to the uptake of services, limiting coverage and effectiveness for key populations in Senegal. Moreover, the study posits that combination stigma interventions will improve effectiveness of existing HIV services, increase uptake of these services by key populations, decrease reported experienced and perceived stigma, increase consistent use of condoms and condom compatible lubricants, increase adherence to HIV treatment regimens, and ultimately decreased community HIV viral load.
FIGURE 1.
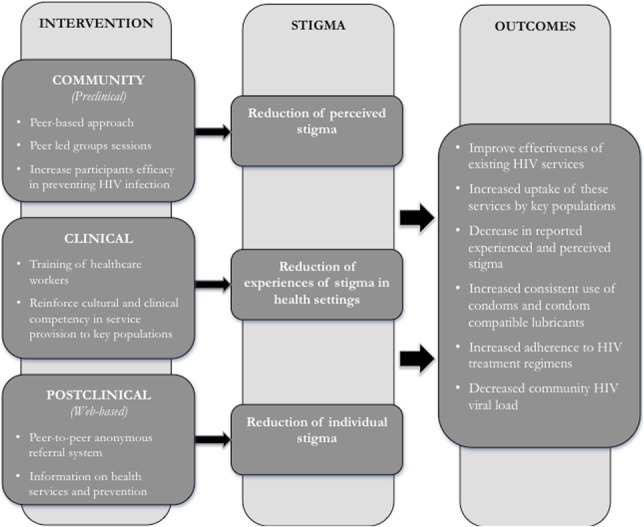
Integrated stigma mitigation intervention framework for key populations.
The overarching objective of the HP2 study is to leverage an implementation research framework to develop, implement, and comprehensively evaluate the impact of a multitiered ISMI approach to improving HIV/AIDS service delivery for key populations at risk for and living with HIV in Senegal. Given stigma's role in limiting the uptake of evidence-based services, including expanded ART for those living with HIV, we hypothesize that overcoming these barriers through comprehensive stigma mitigation will increase uptake of HIV prevention services and decrease community viral load among those living with HIV. Here, we report the preliminary findings including 6 months of follow-up for all participants.
METHODS
Study Setting and Population
This study is implemented across 3 sites in Dakar, Mbour, and Theis, Senegal and consists of 2 phases: phase 1 is a baseline assessment and phase 2 is a 24-month longitudinal cohort which includes a portion of those individuals who participated in phase 1. Participants for phase 1 were recruited through a combination of respondent driven sampling (RDS) and purposive sampling. Individuals were eligible to participate in the study if they reported to be 18 years or older, and either assigned female sex at birth and engaged in sex work as a primary source of income within the past year; or reported to be assigned male sex at birth, and engaged in anal sex with another man in the last year.
Individuals who participated in phase 1 were eligible for voluntary enrollment into the 24-month longitudinal cohort and participation in phase 2, which aimed to enroll a proportion of those who participated in phase 1. Methods for recruitment using RDS into the longitudinal cohort have been previously described.17 Phase 1 baseline assessment includes an interviewer-administered questionnaire and biological testing for HIV and syphilis as well as CD4, viral load, and phylogenetic testing for those living with HIV. HIV testing is conducted using a rapid test (Determine HIV Ag/Ab 1/2) and confirmatory testing (Biospot ImmunoComb II) for those who test positive. Phase 2 includes questionnaires and biological testing at 3, 6, 9, 12, 15, 18, and 24 months. All study visits take place in existing government health facilities.
Ethical review and approval were provided by the Johns Hopkins School of Public Health Institutional Review Board and the National Research Ethics Committee in Senegal.
Intervention Overview
The ISMIs are designed to be delivered in tiers: (1) a community intervention targeting perceived stigma; (2) a clinical intervention targeting enacted stigma in the health care setting; and (3) a postclinical, web-based referral system intervention aiming to increase diffusion of key population-friendly services and mitigate perceived stigma. Our team developed an ISMI Toolkit: Reducing Stigma and Increasing Health Among FSW and MSM in Senegal, which is used as a guide for peer educators to conduct the intervention for this study. This toolkit contains resources for both MSM and FSW, includes a series of parallel modules adapted for each population, and was developed from established interventions used globally.23–28
Community Intervention
The community intervention includes 5 modules: HIV prevention and transmission; human rights; stigma and discrimination; reproductive health; and living with HIV. Topics include HIV transmission and prevention, and risk-reduction techniques; definitions of human rights and rights issues in the MSM and FSW communities; and methods for identifying and responding to stigma and discrimination, stress management, and self-esteem. Additional topics include sexual health, nutrition specific information for PLHIV, disease progression, well-being, and life balance. The intervention is delivered by peer educators to the MSM and the FSW cohort participants, separately, and all modules are adapted to reflect MSM and FSW specifics needs.
The community intervention modules are designed to be delivered every 3 months. The intervention leverages social networks to increase social cohesion, social inclusion, and decrease social alienation. Each module of the community intervention is separated into several sections, which are delivered in intervals. This staggered delivery of modules is designed to reinforce topics covered in the modules and facilitate retention of the overarching module topics. Module activities include group discussions, role-play, question and answer sessions, and presentations. All modules are rooted in participatory learning, with the expectation that information and knowledge are better retained through combined individual and group learning.
Clinical Intervention
The clinical intervention aims at addressing enacted stigma and alleviating barriers to care for key populations on the part of the health care providers. The clinical intervention involves training health workers to improve the clinical and social competency of the providers in addressing the needs of MSM and FSW. The training is based on a curriculum by MSMGF and Johns Hopkins, and informed by Karnataka Health Promotion Trust.29 Each module includes facilitator's tips, group activities, case studies, pre- and post-assessment questions, prereading assignments, and additional readings. Topics include sex, sexuality, and sexual health; mental health promotion; overcoming barriers; creating a friendlier environment; health implications of sexual practices; assessing health status; evidence-based interventions; clinical care for HIV and other sexually transmitted infections; gender-based violence; and reproductive health.
Postclinical Intervention
The postclinical intervention involves a peer-to-peer referral system through a web-based platform, using the social media and communication interfaces. This intervention operationalizes a referral system designed to provide users anonymous and real-time feedback and recommendations for where friendly, nonstigmatizing health services may be accessed. This intervention aims to provide an anonymous reference system for health services and prevention information between peers of the cohort participants.
Intervention Evaluation
The primary form of evaluation of these interventions is through a longitudinal cohort. Through regularly administered questionnaires and biological testing, we assess changes in different components of stigma and uptake of services. Uptake of services are measured through self-reported service utilization, changes in reported sexual practices, and changes in viral load for those living with HIV in terms of higher achieved viral suppression and community (mean/total) viral load among all PLHIV in the study. The community intervention is evaluated throughout the 24-month period, from the perspective of the participant, through self-reported stigma, uptake of services, and implementation outcomes. Data from the clinical and postclinical interventions are not yet available for analysis.
Statistical Analyses
Demographic characteristics of participants from phase 1 baseline are presented as both crude numbers and proportions, as well as RDS adjusted estimates. HIV continuum of care indicators were analyzed as cross-sectional data and include all individuals in the phase 1 baseline assessment. HIV status was determined through biological testing, and plasma viral load was conducted for all HIV-positive participants. Viral suppression in this study is defined as viral load less than 1000 copies/milliliter.
Analysis of stigma indicators includes individuals from phase 1 as the baseline, and those enrolled in the longitudinal cohort for month 3 and month 6. Nonparametric test for trend across ordered groups30 was used to assess differences in responses between longitudinal waves. All analyses were conducted using STATA V.14.1(STATACorp, College Station, TX) statistical package. Nonparametric test for trend across ordered groups compared only those at baseline who enrolled into the longitudinal cohort to those in follow-up. Implementation outcomes are presented as crude numbers and proportions and were collected at 6 months of follow-up.
A total of 724 MSM and 758 FSW participated in the cross-sectional behavioral questionnaire and biological testing at baseline. Overall, 172 MSM and 185 FSW were enrolled and participated in the 3-month follow-up visit for the longitudinal cohort, of whom 102 MSM and 168 FSW had participated in the 6-month follow-up visit at the time of preliminary data analysis.
RESULTS
Demographic Characteristics
Demographic characteristics at baseline are presented in Table 1. Among MSM at baseline, 462 are living in Dakar, 159 in Mbour, and 103 in Thies. Within this sample, 62.7% (n = 454/724) are between 18 and 24 years old. The HIV prevalence among MSM in this study at baseline is 30.2% (n = 219/724), and the RDS adjusted population prevalence of HIV is 23.5% (95% CI: 18.6 to 28.4).
TABLE 1.
Demographic Characteristics of FSW and MSM in Senegal at Baseline
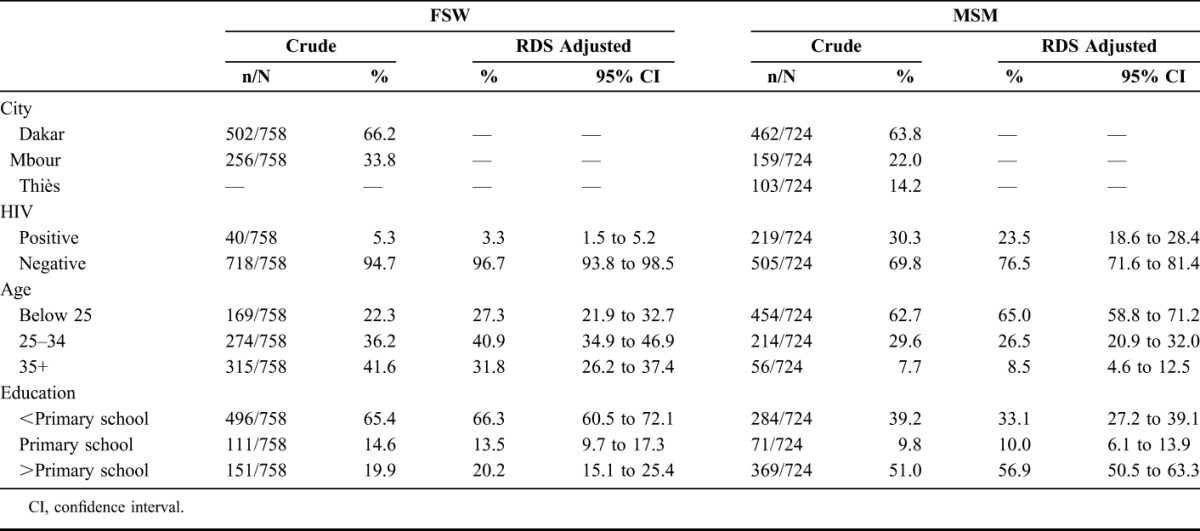
The baseline sample includes 502 FSW living in Dakar and 256 living in Mbour. Among FSW in this study, 41.6% (n = 315/758) are above 35 years old, and 65.4% (n = 496/758) have not completed primary education. The HIV prevalence among FSW participating in the baseline assessment is 5.3% (n = 40/758), and the RDS adjusted population prevalence of HIV is 3.3% (95% CI: 1.5 to 5.2).
HIV Treatment Cascade
The HIV treatment cascade data at baseline is presented in Table 2. Among MSM, 13.2% (n = 29/219) of those living with HIV self-reported knowledge of HIV positive status. Of those who reported knowing their HIV status, 58.6% (n = 17/29) reported to have ever had a CD4 test, and 82.8% (n = 24/29) reported to have initiated ART. Among those who reported ever initiating treatment, 91.7% (n = 22/24) are currently on ART, of whom 63.6% (n = 14/22) are virally suppressed.
TABLE 2.
HIV Continuum of Care at Baseline Among FSW and MSM in Senegal
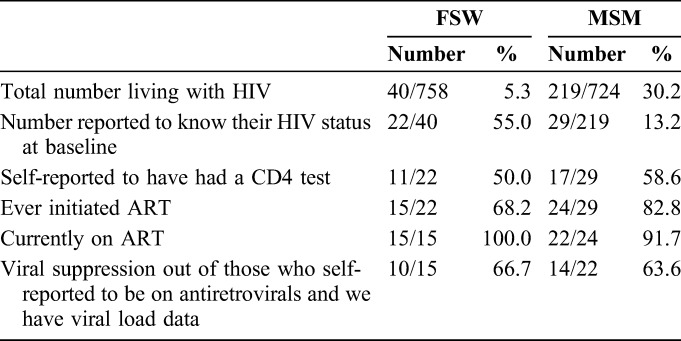
Among FSW, 55.0% (n = 22/40) of women living with HIV reported knowledge of their HIV-positive status. Of the women who reported knowledge of their HIV status, 50.0% (n = 11/22) self-reported ever receiving a CD4 test, and 68.2% (n = 15/22) reported ever having initiated ART. All women who reported ever initiating treatment also reported current enrollment in ART (n = 15/15) and among those who are currently on ART, 66.7% (n = 10/15) are virally suppressed.
Stigma in the Health Care Setting
Prevalence of perceived and enacted stigma outcomes across baseline and follow-up is presented in Table 3. Fear of seeking health services among MSM participants at baseline is 17.7% (n = 128/724) compared with 10.5% (n = 18/172) at month 3 and 9.8% (n = 10/102) at month 6 (P = 0.004). MSM participants avoiding health care services are 15.3% (n = 111/724) at baseline, compared with 11.0% (n = 19/172) at month 3 and 11.8% (n = 12/102) at month 6 (P = 0.062). MSM reporting health service denial or had someone keeping them from receiving health services because they have sex with men was 1.3% (n = 10/724) at baseline, followed by 1.7% (n = 3/172) at month 3, and 1.0% (n = 1/102) at month 6 (P < 0.755). Retention rate from the cohort was 58.9%, with 41.1% loss to follow-up.
TABLE 3.
Perceived and Enacted Stigma Among FSW and MSM
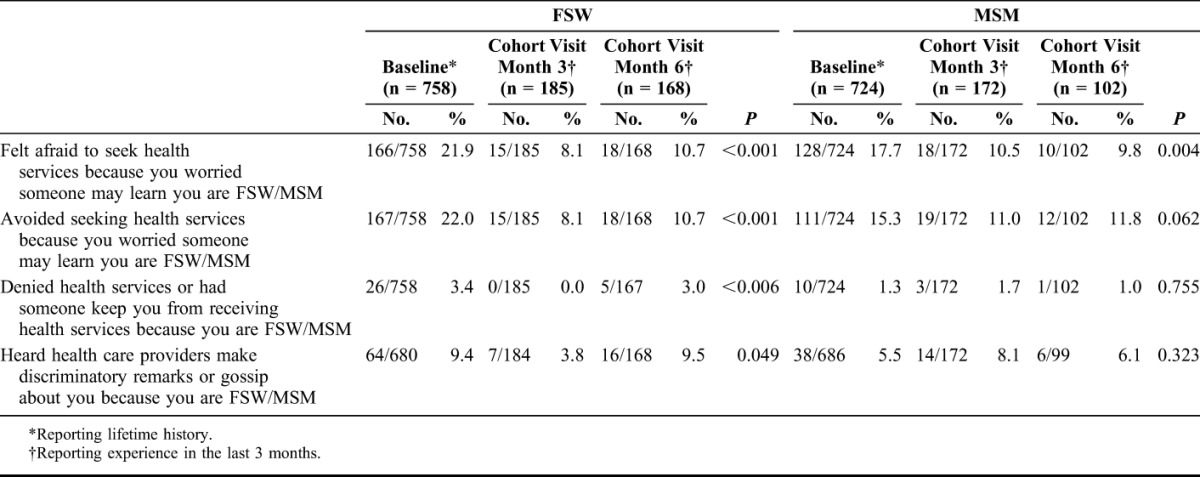
At baseline, 21.9% (n = 166/758) of FSW reported fear of seeking health services because of FSW status, and 8.1% (n = 15/185) at month 3, and 10.7% (n = 18/168) at month 6 (P < 0.001). At baseline, 22.0% (n = 167/758) reported avoiding seeking health services because of FSW status, 8.1% (n = 15/185) at month 3, and 10.7% (n = 18/168) at month 6 (P < 0.001). Overall, 9.4% (n = 64/680) of FSW at baseline, 3.8% (n = 7/184) and month 3, and 9.5% (n = 16/168) at month 6 reported hearing a health care providers make discriminatory remarks or gossip about them (P < 0.05). Retention rate from the FSW cohort was 90%, with 10% loss to follow-up.
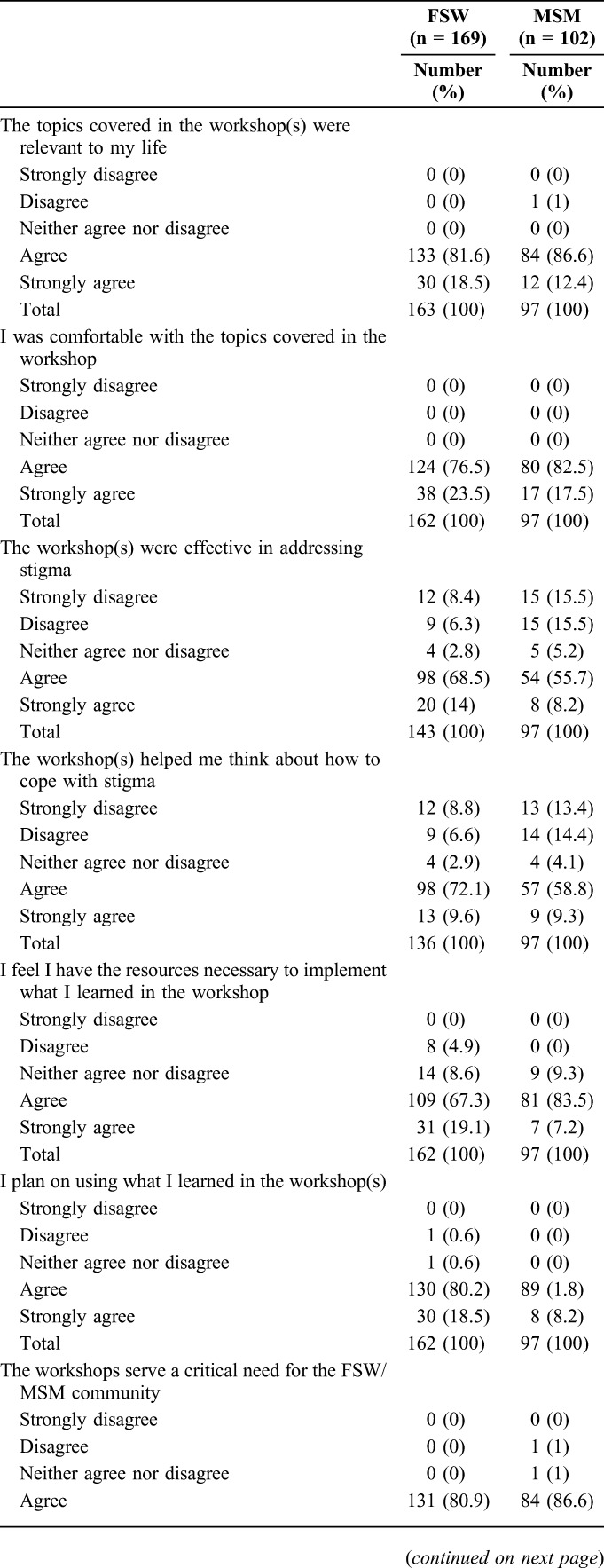
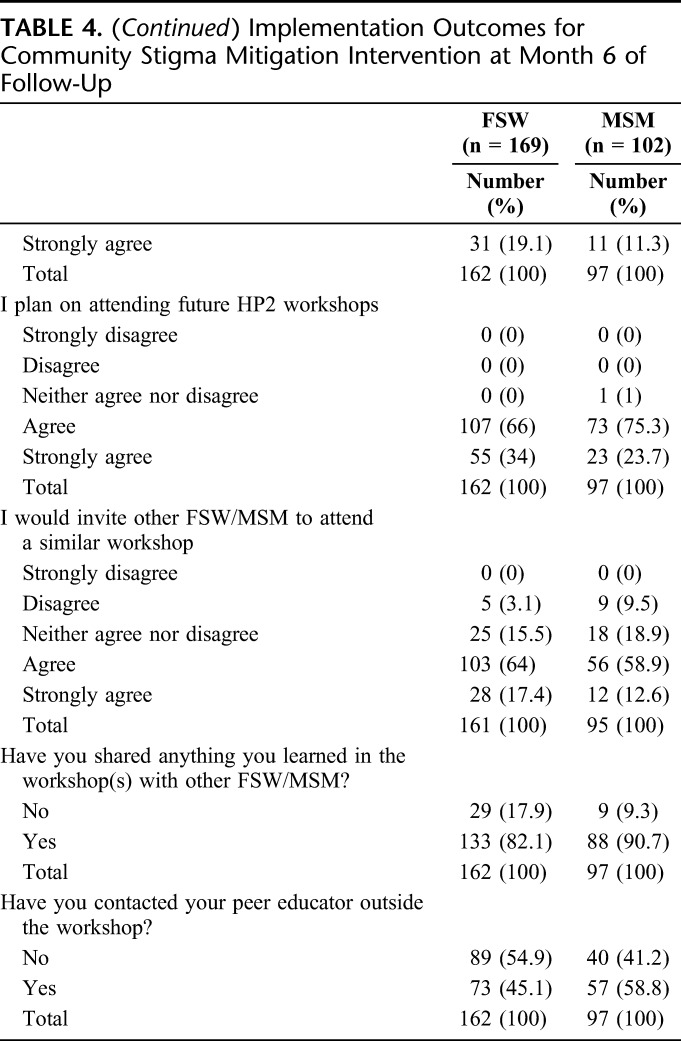
Implementation Outcomes
Table 4 presents implementation outcomes for the community intervention. Among participants of the longitudinal cohort at month 6 of follow-up, 63.9% (n = 62/97) of MSM and 82.5% (n = 118/143) of FSW agreed (or strongly agreed) that the workshops were effective in addressing stigma. Assessing feasibility, 68.0% (n = 66/97) of MSM and 81.6% (n = 111/136) of FSW self-reported that the workshops helped them think about how to cope with stigma.
TABLE 4.
Implementation Outcomes for Community Stigma Mitigation Intervention at Month 6 of Follow-Up
DISCUSSION
At baseline, there was limited uptake of HIV prevention, treatment, and care services among MSM and FSW in Senegal. Moreover, baseline data demonstrated high levels of enacted and perceived stigma in the health care setting for both FSW and MSM in Senegal. Taken together, these data suggest multiple levels of barriers to uptake of services due to care seeking behaviors and access to services. This is especially apparent considering the context of Senegal as a country that has shown success in providing HIV services and preventing HIV in the broader population of reproductive aged adults. Stigma in the health care setting was shown to be prevalent at baseline among FSW and MSM. Perceived stigma was also prevalent at baseline, however, showed to significantly decrease over 6 months of follow-up among participants in the longitudinal cohort. Finally, implementation outcomes related to the interventions suggested further utility of the ISMI.
Stigma in the health care setting was prevalent among participants in this study, which is consistent with findings among MSM and FSW in other settings.14,31 Stigma reduction, specifically among MSM and FSW has been shown in few settings. Reported perceived stigma, measured as fear of seeking health services, and avoiding health services, declined from baseline among participants in the longitudinal cohort. However, nearly one-third of MSM disagreed that the intervention effectively addressed stigma, which suggests there are areas to improve this aspect of the intervention. Although reduction was observed in perceived stigma, enacted stigma in the health care setting did not significantly decrease from baseline. Specifically, being denied access to health services for MSM, and hearing health care providers make discriminatory remarks or gossip did not significantly decrease. Therefore, despite sustained enacted stigma, participants demonstrated reductions in perceived stigma which highlights increased resiliency among participants in the cohort. Therefore, there is a need to continue perceived stigma reduction efforts with cohort participants to maintain progress despite continued experience of stigma. In addition, this highlights the need to continue to integrate stigma reduction interventions targeting the health care providers as to not limit the impact of the perceived stigma reduction interventions.32
Few interventions have been designed to improve HIV care among MSM and FSW.33 Implementation outcomes demonstrate that this intervention is relevant to participants and addresses a critical need among MSM and FSW. This reinforces previous data suggesting that the intervention targeted an appropriate barrier experienced by FSW and MSM in Senegal.
Furthermore, implementation results suggest that the intervention may be effective in addressing this need for stigma reduction and is well accepted by participants. Implementation outcomes suggest continued involvement among participants in the cohort, with high levels of participants reporting that they plan to attend future HP2 workshops. However, retention of cohort participants was low over the first 6 months, especially among MSM. Participants reported sharing information learned through the intervention with other FSW/MSM, and the willingness to invite other FSW/MSM to the interventions. Moreover, participants reported high levels of contacting their peer educator within the first 6 months of follow-up, suggesting uptake of the intervention. Despite limited data in the literature on effective interventions to reduce stigma among key populations, the implementation of this intervention suggests potential in reducing perceived stigma.34
Limitations
There are several limitations to this study's implementation and analyses. A combination of RDS and purposive sampling was used for recruitment of baseline participant, as finding eligible participants was difficult. This combined approach may introduce biases in the study sample. Recruitment from baseline into the longitudinal cohort was done using convenience sampling by HIV status, and therefore may have limitations regarding generalizability of the cohort to the broader target population. This study was statistically powered based on 24 months of follow-up necessitating additional follow-up for more conclusive evaluation of key impact indicators. With 6 months of follow-up data, we have limited ability to assess sustained improvements in knowledge and behavior change beyond the immediate dose response or the impact of the complete package of interventions. Missing data were observed in this study, with high levels in certain survey questions. High levels of loss to follow-up were also observed in longitudinal follow-up, especially among MSM. If loss to follow-up was not random, then biases may be present in the results. Retention among MSM not living with HIV was particularly low, with participants reporting low motivation for participation among this subpopulation. The study team has attempted messaging around the importance of HIV prevention to encourage retention among this subpopulation, however, continues to see low retention. Loss to follow-up presents limitations in the generalizability of the results. Biological data from the follow-up visits is not yet available for analysis, and therefore biological outcomes, such as viral suppression is not yet able to be assessed.
CONCLUSIONS
Data from this study reinforce the need for stigma mitigation interventions to be combined with enhanced linkage and retention to HIV care and treatment to optimize HIV outcomes among key populations in Senegal. Although stigma is understood to be an important determinant of HIV risks, less is known about effective interventions to reduce stigma among key populations especially in the Sub-Saharan African context.5,10,20 Baseline and follow-up data highlighted HIV-related determinants among key populations in Senegal, and suggested the potential utility of the multicomponent ISMI to be able to decrease fear of engaging in HIV prevention, treatment, and care services among key populations to support improved coverage of emerging ART-based prevention and treatment strategies. However, further analysis of longitudinal data across the 24 months of follow-up is needed to evaluate the impact and cost-effectiveness of the package of services.21 Taken together, the available data suggest an urgent need to address stigma to improve the health and human rights of key populations in Senegal and globally.
Footnotes
Funding HIV Prevention 2.0 (HP2): Achieving an AIDS-Free Generation in Senegal is supported by the United States Agency for International Development (USAID) under Cooperative Agreement No. AID‐OAA‐A‐13‐00089. HP2 is managed by Johns Hopkins University.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Méda N, Ndoye I, M'Boup S, et al. Low and stable HIV infection rates in Senegal: natural course of the epidemic or evidence for success of prevention? AIDS. 1999;13:1397–1405. [DOI] [PubMed] [Google Scholar]
- 2.UNAIDS. Senegal: 2014. Available at: http://www.unaids.org/en/regionscountries/countries/senegal. Accessed June 1, 2016. [Google Scholar]
- 3.Stahlman S, Lyons C, Sullivan PS, et al. HIV incidence among gay men and other men who have sex with men in 2020: where is the epidemic heading? Sex Health. 2016. [DOI] [PubMed] [Google Scholar]
- 4.Papworth E, Ceesay N, An L, et al. Epidemiology of HIV among female sex workers, their clients, men who have sex with men and people who inject drugs in West and Central Africa. J Int AIDS Soc. 2013;16(suppl 3):18751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beyrer C, Baral SD, van Griensven F, et al. Global epidemiology of HIV infection in men who have sex with men. Lancet. 2012;380:367–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baral SD, Grosso A, Holland C, et al. The epidemiology of HIV among men who have sex with men in countries with generalized HIV epidemics. Curr Opin HIV AIDS. 2014;9:156–167. [DOI] [PubMed] [Google Scholar]
- 7.Baral S, Beyrer C, Muessig K, et al. Burden of HIV among female sex workers in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12:538–549. [DOI] [PubMed] [Google Scholar]
- 8.Murray CJ, Ortblad KF, Guinovart C, et al. Global, regional, and national incidence and mortality for HIV, tuberculosis, and malaria during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:1005–1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beyrer C, Baral SD, Weir BW, et al. A call to action for concentrated HIV epidemics. Curr Opin HIV AIDS. 2014;9:95–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shannon K, Strathdee SA, Goldenberg SM, et al. Global epidemiology of HIV among female sex workers: influence of structural determinants. Lancet. 2015;385:55–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stahlman S, Beyrer C, Sullivan PS, et al. Engagement of gay men and other men who have sex with men (MSM) in the response to HIV: a critical step in achieving an AIDS-free generation. AIDS Behav. 2016. [DOI] [PubMed] [Google Scholar]
- 12.Poteat TC, Logie CH, Adams D, et al. Stigma, sexual health, and human rights among women who have sex with women in Lesotho. Reprod Health Matters. 2015;23:107–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baral SD, Ketende S, Mnisi Z, et al. A cross-sectional assessment of the burden of HIV and associated individual- and structural-level characteristics among men who have sex with men in Swaziland. J Int AIDS Soc. 2013;16(suppl 3):18768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stahlman S, Grosso A, Ketende S, et al. Depression and social stigma among MSM in Lesotho: implications for HIV and sexually transmitted infection prevention. AIDS Behav. 2015;19:1460–1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Risher K, Adams D, Sithole B, et al. Sexual stigma and discrimination as barriers to seeking appropriate healthcare among men who have sex with men in Swaziland. J Int AIDS Soc. 2013;16(3 suppl 2):18715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tucker A, Liht J, de Swardt G, et al. Homophobic stigma, depression, self-efficacy and unprotected anal intercourse for peri-urban township men who have sex with men in Cape Town, South Africa: a cross-sectional association model. AIDS Care. 2014;26:882–889. [DOI] [PubMed] [Google Scholar]
- 17.Schwartz SR, Nowak RG, Orazulike I, et al. The immediate eff ect of the Same-Sex Marriage Prohibition Act on stigma, discrimination, and engagement on HIV prevention and treatment services in men who have sex with men in Nigeria: analysis of prospective data from the TRUST cohort. Lancet HIV. 2015;2:e299–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fay H, Baral SD, Trapence G, et al. Stigma, health care access, and HIV knowledge among men who have sex with men in Malawi, Namibia, and Botswana. AIDS Behav. 2011;15:1088–1097. [DOI] [PubMed] [Google Scholar]
- 19.Decker MR, Wirtz AL, Baral SD, et al. Injection drug use, sexual risk, violence and STI/HIV among Moscow female sex workers. Sex Transm Infect. 2012;88:278–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stangl AL, Lloyd JK, Brady LM, et al. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come? J Int AIDS Soc. 2013;16(3 suppl 2):18734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baral S, Logie CH, Grosso A, et al. Modified social ecological model: a tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health. 2013;13:482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Babalola S, Van Lith LM, Mallalieu EC, et al. A framework for health communication across the HIV treatment continuum. J Acquir Immune Defic Syndr. 2017;74(suppl 1):S5–S14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Region WBEAaP. Curriculum for commercial sex workers. In: The Road to Good Health: HIV Prevention in Infrastructure Projects. Washington, DC: The World Bank; 2008. [Google Scholar]
- 24.Enda Sante Community Intervention Guide. 2006. [Google Scholar]
- 25.USAID and Population Council and PATH's Frontiers in Reproductive Health Program (FRPH) and USAID and Population Councils Tuko Pamoja Adolescent Reproductive Health and Life Skills Curriculum (TPC) Developed in Kenya. Program for Appropriate Technology in Health (PATH), Nairobi, Kenya, 2006. Available at: https://www.path.org/publications/files/CP_kenya_KARHP_curric_3-06.pdf.
- 26.Catalyst A. Trainer's Supplement: HIV/AIDS: The Rights Framework. In Know it: The Rights Framework: Asia Catalyst; Thailand, 2010. Available at: http://www.nswp.org/sites/nswp.org/files/Know%20It%20-%20The%20Rights%20Framework,%20Asia%20Catalyst%20-%202010.pdf. [Google Scholar]
- 27.Institute for Social development studies, & International Center for Research on Women, (2010), Understanding and Challenging HIV Stigma toward Sex Workers and HIV in Vietnam 28-33. Worker's Publishing House: Hanoi, Vietnam; 2010. [Google Scholar]
- 28.Anchoring Script and Directions from: Raudebaugh, C. (n.d.). Free Relaxation Script: Anchoring. Self-esteem Relaxation Script and Directions: Raudebaugh, C. (n.d.). Free Relaxation Script: Self-Esteem Relaxation; Inner Health Studio.
- 29.Beattie TS, Bhattacharjee P, Ramesh BM, et al. Violence against female sex workers in Karnataka state, South India: impact on health, and reductions in violence following an intervention program. BMC Public Health. 2010;10:476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cuzick J. A Wilcoxon-type test for trend. Stat Med. 1985;4:87–90. [DOI] [PubMed] [Google Scholar]
- 31.Decker MR, Lyons C, Billong SC, et al. Gender-based violence against female sex workers in Cameroon: prevalence and associations with sexual HIV risk and access to health services and justice. Sex Transm Infect. 2016. [DOI] [PubMed] [Google Scholar]
- 32.van der Elst EM, Smith AD, Gichuru E, et al. Men who have sex with men sensitivity training reduces homoprejudice and increases knowledge among Kenyan healthcare providers in coastal Kenya. J Int AIDS Soc. 2013;16(suppl 3):18748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Girault P, Green K, Clement NF, et al. Piloting a social networks strategy to increase HIV testing and counseling among men who have sex with men in greater Accra and Ashanti region, Ghana. AIDS Behav. 2015;19:1990–2000. [DOI] [PubMed] [Google Scholar]
- 34.Odeny TA, Padian N, Doherty MC, et al. Definitions of implementation science in HIV/AIDS. Lancet HIV. 2015;2:e178–180. [DOI] [PubMed] [Google Scholar]


