Abstract
Gout is an inflammatory joint disease associated with deposition of monosodium urate crystals in the bones forming the joints, in periarticular tissues and in other organs. The disease is one of the most frequent causes of disability.
This paper presents the case of a 57-year-old male patient treated for generalised gout. A “clinical mask” suggesting another disease was the cause of making the correct diagnosis only six years after the occurrence of the first manifestations.
The patient, with high values of inflammatory markers, severe pain and advanced joint destruction, was given an aggressive anti-inflammatory treatment. The unsatisfactory effect of the conservative treatment forced the authors to perform surgical resection of the gouty nodules in the hands. After several operations the function of the hand joints operated on, appearance of the hands and the quality of the patient’s life improved significantly.
Keywords: surgery, tophi, diagnostic difficulties
Introduction
Gout is an inflammatory disease of the joints caused by crystallisation and phagocytosis of monosodium urate crystals (MSU) in the synovial fluid and their deposition in the joint-forming bones, periarticular tissues and other organs.
Gout is therefore a metabolic disease associated with increased synthesis or reduced excretion of uric acid. In its aetiology and pathogenesis genetic predispositions (among other things SLC2A9 gene polymorphism), environmental factors (effect of alcohol, an excess of purines, fructose, use of diuretics), and frequently coexisting diseases such as metabolic syndrome and diabetes mellitus or arterial hypertension itself are important. Also renal failure and early menopause are recognized risk factors for developing gout [1–3].
In recent years the number of new cases of gout and the incidence of its complications have been increasing worldwide.
Also this disease is one of the most frequent causes of disability [4].
Gout affects about 1–2% of the population. The male-to-female ratio is 6 : 1 on average.
The increasing number of patients with gout is associated with prosperity and economic development, but the price to pay for improving the quality of life is to increase the number of people suffering from obesity and metabolic disorders.
Case report
In our clinic in the years 2002–2015 there were 24 hospitalized patients who were referred for surgical treatment of tophi.
Thirteen patients were not qualified for surgery due to contraindications (non-stabilised diabetes mellitus, unstable coronary artery disease, trophic crural lesions with ulcerations, extensive dental caries), or lack of indications for the operation (small defects or conservative treatment still possible).
Twelve patients (11 male, 1 female) were operated on and a total of 19 procedures were performed (one patient – five operations, one patient – three operations, two patients – two operations each).
The following were performed:
Nine tophectomy procedures in the region of proximal and distal interphalangeal joints of the fingers and joints of the thumb combined with debridement of the joints of gouty deposits.
Four tophectomy procedures in the region of metatarsophalangeal joints combined with debridement of the joints of gouty deposits and correction of the toes with temporary stabilisation with Kirschner wires.
Four tophectomy procedures in the region of the calcaneal tuber.
Two knee arthroscopy procedures with joint debridement.
Here we describe a 57-year-old man who was referred to our clinic for surgical removal of tophi. In the patient history he was previously hospitalized at the age of 42 in a regional hospital with the diagnosis of septicaemia, which was a complication of untreated whitlow of the middle finger of the left hand. Than he received antibiotic therapy. Two months after this hospitalisation the patient complained of pain and oedema in the knee, wrist, and elbow joint and the proximal interphalangeal joints of the index and middle fingers of the left hand. Laboratory tests revealed the following abnormalities: accelerated ESR – 48 mm/h, granulocyte percentage 70%. On X-ray examination geodes were visualised in the carpal bones. Non-steroidal anti-inflammatory drug (NSAID) treatment resulted in the improvement and reduction of complaints. The complaints described above were recurring with varying intensity for the next four years.
The patient was hospitalized again in another hospital at the age of 46. Due to periodically observed sub-febrile conditions and presence of antibodies against antigens of Salmonella enteritidis and Chlamydia trachomatis in IgG class, reactive arthritis was diagnosed. Sulfasalazine (SF) treatment was introduced. SF was withdrawn, however, after several months due to lack of any therapeutic effect.
Then the diagnosis was changed to unclassified arthritis (seronegative) and treatment with oral methylprednisolone was started in a 6 mg daily dose, with a very good therapeutic effect. All complaints resolved.
Methylprednisolone was withdrawn after several months and the arthralgia and joint oedema rapidly recurred. Contractures developed in the knee, hip, elbow, shoulder, hand and foot joints. Nodules were rapidly enlarging, deforming the middle and fifth fingers of the left hand, the index and ring fingers of the right hand, the olecranon region and toes of the right foot. The skin over the nodules periodically cracked and serous contents were oozing with uric acid crystal deposits. On X-ray and magnetic resonance imaging degenerative-proliferative lesions and geodes, articular space narrowing in almost all peripheral joints and vertebral joints, with multilevel discopathy in the lumbar segment and multilevel disc herniations with right-sided spinal nerve compression were found. In laboratory test results the markers of an acute inflammatory process were detected: elevated erythrocyte sedimentation rate (ESR) 28/42 mm, C-reactive protein (CRP) 8 mg/dl, hyperleucocytosis with granulocytosis – 12 000 (72%) and increased serum uric acid (UA) concentration to 9 mg/dl.
During puncture of the right knee joint, 35 ml fluid of inflammatory morphology, with confirmation of presence of uric acid crystals, was obtained.
Gout was diagnosed and treatment with a xanthine oxidase inhibitor (allopurinol) was started with doses increasing to 500 mg daily, and a diet with limitation of purines, fructose and alcohol was recommended.
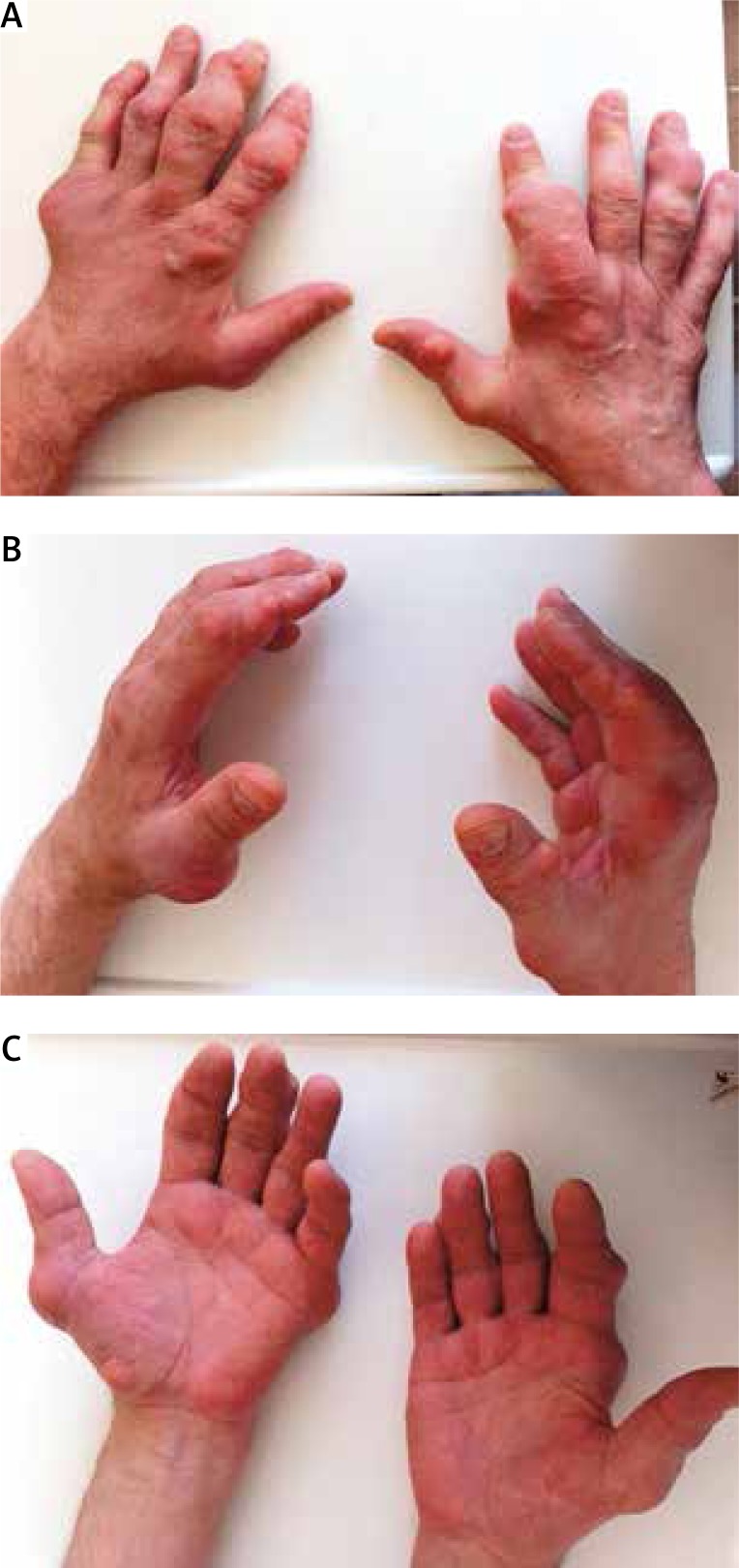
Despite that, arthralgia and joint oedema increased, articular contractures became more pronounced, the tophi reached significant dimensions and serous contents with deposits of uric acid crystals were oozing from them. The uric acid concentration was 7–8 mg/dl. Methylprednisolone treatment was restarted in a 6 mg daily dose and colchicine was added, initially in a 5 mg daily dose and then a 2 mg daily dose. In view of significant limitation of hand functions and difficulties in walking, disability to work was adjudicated. The patient was granted a disability pension (Fig. 1).
Fig. 1.
Preoperative photos of hands.
At the age of 52, after 10 years of disease duration, the tophi were so large that a decision about their surgical removal was taken in order to improve hand functioning and to improve the cosmetic defect (Fig. 2).
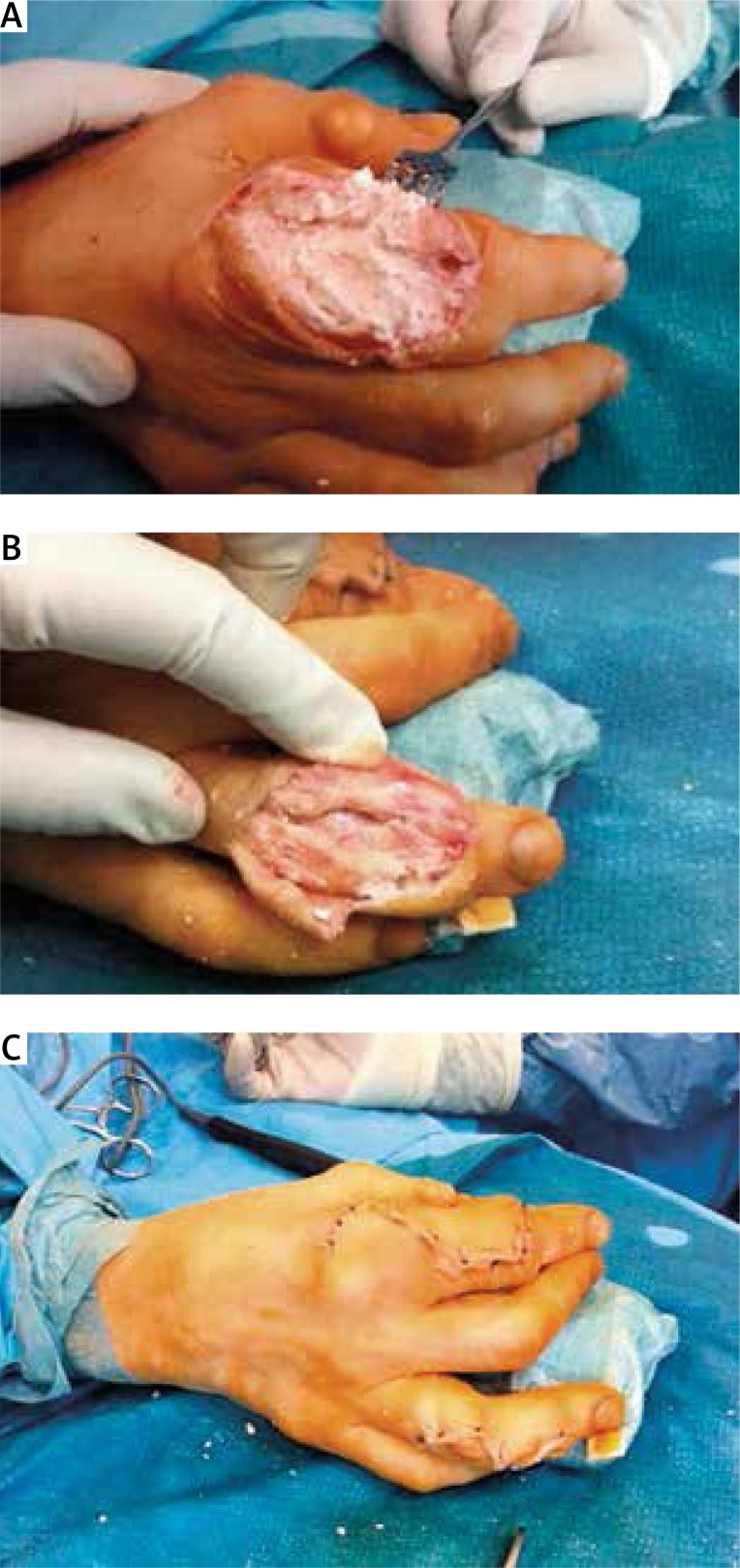
Fig. 2.
Intraoperative photos of hands.
In the five subsequent years, on continuous pharmacotherapy with allopurinol and colchicine and periodically with methylprednisolone, five open surgical procedures were performed in the majority of phalangeal, metacarpal and carpal joints and adjacent tendons of the extensor digitorum muscles, including removal of massive gouty deposits incrusting those regions and resection of gouty deposits forming large nodules. They were removed only to the available extent, since in view of the degree of tissue penetration by the deposits, their complete removal was impossible. The deposits involved the articular capsules, tendons, and neurovascular bundles. It was possible to avoid resection of articular surfaces and the necessity of arthrodesis, but not all deposits could be removed from the displaced, thinned and inefficient extensor of the index finger of the right hand and the extensor of the fifth finger of the left hand (Fig. 2).
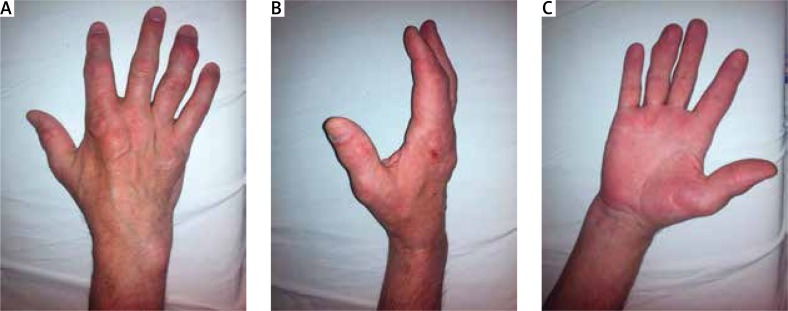
The surgical procedures were uncomplicated with infections, and the healing process was normal (Fig. 3). After the procedures, several-week physiotherapy courses were conducted.
Fig. 3.
Postoperative photos of hands.
As a result of the surgical operations the hand joint function significantly improved, the pain in the joints operated on decreased, the cosmetic appearance of the hands improved and serum UA concentration and serum markers of acute inflammation became normal. Now the patient is waiting for knee joint endoprosthesis implantation after previous elimination of dental caries and explanation of the asymptomatic changes, which were found on control preoperative chest X-ray (round shadow in the mediastinum for further urgent imaging diagnostic procedures) (Fig. 4).
Fig. 4.
Changes in the knee joints in the X-ray images.
Discussion
Although the symptoms of gout have been described for centuries, and the causes of the disease have been known for a long time, the evaluation of clinical divisions and diagnostic criteria is still continuing. And thus in 2014 Dalbeth and Stamp [5] proposed a staging system of the clinical course of gout with division into the following stages:
asymptomatic hyperuricaemia without deposits of monosodium urate crystals in tissues on imaging examinations,
asymptomatic hyperuricaemia with deposits,
gout attacks,
tophaceous gout, chronic gouty arthritis, bone erosions on X-ray examinations.
Richette et al. [6] in 2015 distinguished five clinical forms of gout. That classification reflects various pathophysiological processes associated with gout:
gout with minor symptoms and signs of other diseases,
gout with obesity and arterial hypertension,
gout with type 2 diabetes mellitus,
gout with dyslipidaemia,
gout with cardiovascular diseases and renal failure in patients taking large doses of diuretics.
In 2015 rheumatologists, members of the American College of Rheumatology and the European League Against Rheumatism, developed highly sensitive (92%) and highly specific (89%) new classification criteria of gout based on a three-grade scale. Grade one determines for which patients with what type of complaints this scale can be used, grade two makes it possible to diagnose the disease in a patient if monosodium urate crystals or tophi have been found in a joint or bursa with inflammatory lesions, grade three enables application in patients without urate deposits of a scoring system taking into account the detailed clinical picture, history data and character of the complaints and results of imaging examinations.
Those criteria enable one to count a patient among individuals with a possible diagnosis of gout [7]. Tophi develop in 12–35% of gout patients. Initially they cause no significant complaints and lead to no function limitation of the nearby joints. However, if they become larger, joint instability and movement range limitation, joint function impairment and bone erosions at the sites of their penetration can develop.
An effective hypouricaemic treatment prevents the development of gouty nodules, and can lead to reduction of the already present ones and to repair of the damage they may have caused.
The treatment is, however, not always successful. The causes can include incorrect or late diagnosis, unsuitable therapy, comorbidities, failure to observe dietetic instructions by the patient or abandoning treatment.
In such cases indications are present for surgical removal of the nodules. Tophi not only can impair articular function but also can ulcerate, be a source of infections, and compress local nerves [8].
Gout is a disease known since ancient times. It was mentioned in the Indian Veda book dated to 1250 B.C. and in Persian texts and works of Hippocrates [9]. Surgical treatment of gout was frequent in ancient times. It was recommended to “disburden” the joints surrounded by monosodium urate crystals or for cosmetic reasons [10].
Hippocrates in the 5th century B.C. reported regression of strong gouty pain after cauterization of tophi with burning hemp. In the 16th century, A. Paré, a French surgeon, rubbed in the roots of the hermodactylus plant (genus Colchicum) into surgically opened tophi.
The first reports on surgical removal of tophi, and limb amputations sometimes related to it, can be found in the literature from the end of the 19th century and the beginning of the 20th century [11].
Together with increasing knowledge of the mechanism of tophi development, association with hyperuricaemia, and treatment possibilities, the indications for surgical interventions have changed. They were published in the 1960s. They included the following conditions caused by tophi:
impairment of the function of tendons and joints,
skin ulceration or necrosis over the tophi,
local infections or septicaemia caused by tophi,
nerve compression [12].
There have been no controlled clinical studies comparing the effectiveness of pharmacotherapy and surgical treatment in patients with persistent gouty nodules. Although a surgical procedure can potentially produce a more rapid effect, it is hard to balance the benefits against the risk of surgical complications, particularly a possibility of infection and poorer wound healing [13]. It is believed that the type of surgical intervention should depend on the consistency of tophi, possibly on the degree of destruction of the joint involved.
In the case of “soft” tophus, the procedure should only include its emptying. In the case of minor involvement of a joint, debridement should be performed. In the case of articular surface destruction, arthrectomy is required with possible endoprosthesis implantation, and in the case of reoperation, even arthrodesis [8].
This year a large review paper by Kasper et al. [8] was published, in which the authors performed a review of available literature on surgical interventions in the treatment of gout. They found 171 papers in PubMed and about 800 articles in Google Scholar, published in the years 1950–2015. Those papers included no retrospective or prospective clinical studies, only case reports. Kasper et al. selected seven papers published in the years 2002–2015 and presented in a table the total number of 317 patients described, operated on for gouty nodules, comparing the surgical techniques used in them. The most common techniques included arthroscopic shaver and open tophectomy. The most frequent adverse effect was delayed surgical wound healing, mostly in patients with accompanying diabetes mellitus or peripheral vasculopathies. The results of the operations were positive in respect of function restoration of the joint involved.
Based on the mentioned literature review, the authors maintained the indications to surgery accepted to date and extended them to include the following:
lack of improvement in spite of normally conducted conservative treatment and persisting uric acid concentration in serum > 5.0–5.5 mg/dl,
significant painfulness of the tophus and oozing contents,
joint instability,
limitation of everyday activities (wearing shoes, clothes) and impairment of the quality of life [8].
Taking into account the above information and knowledge about the course of gout, we analysed the cases of described patients.
A well-known fact is that gout may have a “clinical mask” imitating another disease, and another disease may mimic symptoms of gout [14]. In our patient the correct diagnosis was established after six years of disease duration.
The crystals accumulating in the tissues destroyed them and caused a chronic inflammatory process with release of inflammation mediators which resulted in the development of systemic symptoms (subfebrile states, elevated laboratory markers of acute inflammation).
The symmetry of the inflammatory signs, involvement of the proximal joints in the hands and feet, metacarpophalangeal joints, large joints of the lower limbs and vertebral joints caused diagnostic errors. The synovial fluid at the time of analysis contained no MSU crystals, which could have resulted from its incorrect sampling or preparation. The MSU deposits were present on articular surfaces and in periarticular nodules.
Such a picture of gout and such “clinical masks” have been described by many authors [15, 16]. The masks significantly delayed institution of adequate treatment. The late start of appropriate treatment was not sufficient to normalize serum uric acid concentration. That facilitated crystallisation of MSU in tissues and on articular surfaces.
The nodules of significant size, containing those deposits, compressed the adjacent tissues, making normal function of the hands, feet and practically all peripheral and vertebral joints impossible. The patient was unable to work.
During the surgical procedures the accumulated crystals could not be completely removed; however, the function of the hand joints operated on, appearance of the hands and patient’s quality of life improved significantly. The pain in the joints operated on was alleviated and the laboratory markers of acute inflammation and UA concentration decreased, which prognosticates a reduction of the remaining, not surgically treated tophi and discontinuation of formation of new ones.
Summary
According to the current guidelines for management of gout, treatment can be implemented only after diagnosis of gout, and asymptomatic hyperuricaemia is not an indication for treatment. In the light of the abundant literature on gout and our case, particularly interesting is an article published this year by Garber in The Rheumatologist journal which takes into account the desirability of treating asymptomatic hyperuricaemia [17].
Undoubtedly debate over when to start treatment in case of an increase in the serum concentration of UA and when to actually decide on the surgical treatment of tophi will continue.
The authors declare no conflict of interest.
References
- 1.Dalbeth N, House ME, Gamble GD, et al. Population-specific influence of SLC2A9 genotype on the acute hyperuricaemic response to fructose load. Ann Rheum Dis. 2013;72:1868–1873. doi: 10.1136/annrheumdis-2012-202732. [DOI] [PubMed] [Google Scholar]
- 2.McAdams-DeMarco M, Maynard JW, Baer AN, et al. A urate gene-by diuretic interaction and gout risk in participants with hypertension: results from the ARIC study. Ann Rheum Dis. 2013;72:701–706. doi: 10.1136/annrheumdis-2011-201186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singh JA, Reddy SG, Kundukulam J. Risk factors for gout and prevention: a systemic review of the literature. Curr Opin Rheumatol. 2001;23:192–202. doi: 10.1097/BOR.0b013e3283438e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smith E, Hoy D, Cross M, et al. The global burden of gout: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73:1470–1476. doi: 10.1136/annrheumdis-2013-204647. [DOI] [PubMed] [Google Scholar]
- 5.Dalbeth N, Stamp L. Hyperuricemia and gout: time for a new staging system? Ann Rheum Dis. 2014;73:1598–1600. doi: 10.1136/annrheumdis-2014-205304. [DOI] [PubMed] [Google Scholar]
- 6.Richette P, Clerson P, Perissin L, et al. Revisiting comorbidities in gout: a cluster analysis. Ann Rheum Dis. 2015;74:142–147. doi: 10.1136/annrheumdis-2013-203779. [DOI] [PubMed] [Google Scholar]
- 7.Neogi T, Jansen TLThA, Dalbeth N, et al. 2015 Gout classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborate initiative. Ann Rheum Dis. 2015;74:1789–1798. doi: 10.1136/annrheumdis-2015-208237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kasper IR, Juriga MD, Giurini JM, et al. Treatment of tophaceous gout: When medication is not enough. Semin Arthritis Rheum. 2016;45:669–674. doi: 10.1016/j.semarthrit.2016.01.005. [DOI] [PubMed] [Google Scholar]
- 9.Łaszczyca M, Kusz B, Kusz D. Występowanie licznych guzków dnowych w nietypowym przebiegu dny moczanowej – opis przypadku. Kwart Ortop. 2013;1:128–137. [Google Scholar]
- 10.Casangrade P. Surgery for tophaeceous gout. Semin Arthritis Rheum. 1971;1:262–273. doi: 10.1016/0049-0172(72)90005-4. [DOI] [PubMed] [Google Scholar]
- 11.Straub IR, Smith JW, Carpenter GK, et al. The surgery of gout in the upper extremity. J Bone Joint Surg. 1961;43:731–774. [Google Scholar]
- 12.Larmon WA, Kurtz JF. The surgical management of chronic tophaceous gout. J Bone Joint Surg Am. 1958;40A:743–772. [PubMed] [Google Scholar]
- 13.Kumar S, Gow P. A survey of indications, results and complications of surgery for tophaceous gout. J N Z Med Assoc. 2002;115:1158. [PubMed] [Google Scholar]
- 14.Zimmermann-Górska I. Kliniczne maski związane z chorobami reumatycznymi wywołanymi przez kryształy. Reumatologia. 2006;44:320–323. [Google Scholar]
- 15.Schapira D, Stahl S, Izhak OB, et al. Chronic tophaceous gouty arthritis mimicking rheumatoid arthritia. Semin Arthritis Rheum. 1999;29:56–63. doi: 10.1016/s0049-0172(99)80038-9. [DOI] [PubMed] [Google Scholar]
- 16.Hausch R, Wilkerson M, Singh E, et al. Tophaceous gout of the thoracic spine presenting as back pain and fever. J Clin Rheumatol. 1999;5:335–341. doi: 10.1097/00124743-199912000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Garber M. Treating asymptomatic hyperuricemia could lower risk of developing chronic conditions. The Rheumatologist. 2016 Aug 12; online ISSN 1931-3209. [Google Scholar]