Abstract
Geographic disparities in life expectancy are substantial and not fully explained by differences in race and socioeconomic status. To develop policies that address these inequalities, it is essential to identify other factors that account for this variation. In this study we investigated whether population well-being—a comprehensive measure of physical, mental, and social health—helps explain geographic variation in life expectancy. At the county level, we found that for every 1-standarddeviation (4.2-point) increase in the well-being score, life expectancy was 1.9 years higher for females and 2.6 years higher for males. Life expectancy and well-being remained positively associated, even after race, poverty, and education were controlled for. In addition, well-being partially mediated the established associations of race, poverty, and education with life expectancy. These findings highlight well-being as an important metric of a population’s health and longevity and as a promising focus for intervention.
Life expectancy varies considerably across counties in the United States. A 2013 study found that a male born in Fairfax County, Virginia, was expected to live almost eighteen years longer than a male born 350 miles away in McDowell County, West Virginia.1,2 Several studies have demonstrated that demographic and socioeconomic factors such as race, poverty, and education partly explain these geographic disparities.1,3–11 However, as these health inequalities persist and worsen, there is a growing need to identify other factors that account for this variation and that could guide efforts to reduce disparities.1,5–8
Population well-being—a measure that incorporates physical, emotional, and social health— may help explain variation in life expectancy.12–16 Well-being includes not only the absence of disease but also a sense of opportunity, happiness, and lack of stress. It reflects the ability to afford food, housing, and health care; to live in a safe neighborhood; and to work in a trusting, respectful environment.12,17–19 In other words, well-being comprehensively assesses both individual- and neighborhood-level characteristics that may influence the health and longevity of an entire community.17,20,21 Compared with residents of a community with low well-being, residents of a community with high well-being may be more likely to engage in healthy behaviors, develop social connections, and build strong support systems.12,20,22 Living in a community with high well-being may also promote resilience, buffer the negative impact of stressful events, and improve health throughout the life course.16,19,21 Therefore, population well-being may be an important community characteristic that explains geographic disparities in life expectancy.
Inequalities in life expectancy across demographic groups defined by race, poverty, and education level have been attributed to several factors, including differences in workplace exposures, burden of disease, and health behaviors.3–5 Population well-being, which considers these factors along with others, such as life satisfaction and access to housing, may therefore mediate the relations of race, poverty, and education with life expectancy and provide deeper insight into these established associations. Well-being may also express aspects of health that are not solely influenced by race, poverty, and education, and it may explain variation in life expectancy beyond these demographic characteristics.
Accordingly, we tested the hypothesis that population well-being is associated with life expectancy independent of, and as a mediator of, race, poverty, and education. We conducted this analysis using county-level estimates of wellbeing from a nationally representative survey, the Gallup-Healthways Well-being Index.17 County-level life expectancy estimates were adopted from a 2013 study that demonstrated geographic disparities in life expectancy.1,23 This article reports the findings of our analysis and discusses the implications of those findings for policy makers at all levels of government.
Study Data And Methods
Data
Our sample included 3,092 counties or county equivalents (in some states, parishes or boroughs) in the United States.
Our dependent variable was county-level life expectancy in 2010, measured in years and stratified by sex. These estimates were derived using models that incorporated five years of historic data and geographic patterns to improve accuracy and precision.1 The data were obtained from the Global Health Data Exchange.1,23
Our independent variables were the composite county-level well-being score and the six domain scores from the 2010–2012 Gallup-Healthways Well-being Index (GHWBI).17 The GHWBI is a national telephone survey of individuals age eighteen and older from all fifty states and the District of Columbia; approximately 1,000 telephone (landline and cell) surveys were conducted each day during the fielding period. The survey was influenced by the work of Daniel Kahneman and Ed Diener, experts in the field of well-being.24,25 The survey was designed to measure dimensions of overall well-being, such as standard of living, satisfaction with community, work relationships, and personal health. Factor analyses at the individual, state, and congressional district levels were conducted to refine item selection. As some factors were highly correlated with each other, the most statistically and conceptually redundant factors were combined into single indices, representing six well-being domains: physical health, emotional health, healthy behaviors, life evaluation, basic access, and work environment.
These six domains, as well as population demographics, are evaluated with fifty-five survey questions. Physical health assesses the burden of chronic disease and recent illness. Emotional health measures daily emotions and the presence or absence of depression. Healthy behaviors assesses the prevalence of smoking, exercising, and eating fruit and vegetables. Life evaluation measures life satisfaction and optimism about the future. Basic access includes perception of safety and access to housing and health care. Work environment assesses job satisfaction and trust and respect in the workplace. Each domain is represented by an index, measured on a scale of 0 to 100. The composite well-being score is an unweighted mean of all six domains.17 Additional details about the survey items in each of the domains can be found in online Appendix Exhibit A1.26 The GHWBI has been validated as a measure of population well-being, and prior studies have linked it with employee productivity and health care utilization.17,27,28
Data on race and ethnicity in 2010 were obtained from the Area Health Resources Files of the Health Resources and Services Administration. These data included the percentage of residents identifying as black, the percentage of Hispanic origin, and the percentage identifying as another minority.29 Educational attainment was based on five-year aggregated data from the Census Bureau’s American Community Survey for the years 2009–13 and was represented by the percentage of high school graduates, measured separately by sex.30 County-level poverty prevalence was measured by 2010 county-level percentages of individuals below the federal poverty level, from the Small Area Income and Poverty Estimates (SAIPE) project.31
Analysis
All analyses were performed at the county level and were stratified by sex. We first plotted county-level life expectancy against county-level well-being. We then estimated a series of linear regression models, with the standardized composite well-being score and each of the six domain scores as the independent variables and male and female life expectancy as the dependent variables. The regression coefficients can be interpreted as the change in life expectancy in years associated with a change of one standard deviation (SD) in the composite well-being or domain score. To account for differing precision of the estimates, each observation was weighted by the number of survey respondents. We first assessed unadjusted associations of wellbeing with life expectancy, stratified by sex. To evaluate whether race, poverty, and education attenuated these associations, we added these factors to the initial models.
We then used structural equation modeling to explore whether the composite well-being score mediated the associations of race, poverty, and education with life expectancy.32 Specifically, a structural equation model was estimated for each covariate. These models evaluated ten pathways connecting the five covariates (percentage black, percentage of Hispanic origin, percentage identifying as another minority, percentage living in poverty, and percentage of high school graduates), the mediator (well-being), and the outcome (life expectancy). The goal of this analysis was to determine if well-being was an important driver in the relations between these population characteristics and life expectancy. Additional details can be found in the Appendix.26
Limitations
Our study had several limitations. First, as this was an ecologic study, with a county population rather than an individual as the unit of analysis, we were unable to interpret our findings at the individual level. Nevertheless, our focus was on communities.
Second, life expectancy may be influenced by cumulative exposures over a lifetime, but we assessed well-being during a three-year period only. In addition, a portion of the well-being data was collected after the life expectancy estimates. To increase the reliability of the well-being estimates, we aggregated survey responses from 2010 to 2012. However, the most recently available county-level life expectancy estimates were from 2010. Given the timing of our data and the fact that this was a cross-sectional study, we were unable to make causal inferences between wellbeing and life expectancy. Future work should use additional years of data to explore how changes in well-being over time affect changes in life expectancy.
Third, in counties with small populations, life expectancy estimates were influenced heavily by patterns in nearby counties and structured relationships with covariates. Therefore, these estimates had substantial uncertainty intervals.1
Fourth, prior work has shown that the mortality rate within a certain county is associated with the characteristics of its neighboring counties such as race, ethnicity, and income inequality.9 We did not adjust for characteristics of neighboring counties; we also did not account for the heterogeneity in life expectancy within counties.
Fifth, although many socioeconomic and demographic factors have been associated with population life expectancy, we chose to adjust for race, poverty, and education because these are consistently recognized as strong predictors.1,3–9 County attributes such as rurality and social capital have previously been linked with longevity but were not included in this study.33,34
Finally, the well-being index sampling method has been designed to be representative at the state and congressional district levels but not the county level. To assess whether inclusion of counties with a small sample size influenced our results, we replicated analyses using only geographic areas with at least 100 respondents (n = 1,606).
Study Results
Among 3,092 counties, well-being scores for males and females ranged from 35.6 to 87.1 (mean: 66.4; SD: 4.2). County life expectancies ranged from 72.6 years to 85.0 years for women and 63.9 years to 81.7 years for men. Counties with lower life expectancies were located in the South and had a higher percentage of blacks, lower education levels, and higher poverty rates compared with counties with higher life expectancies (Appendix Exhibit A2).26
Well-being was significantly associated with female and male life expectancy at the county level (Appendix Exhibit A3).26 For every 1-standard-deviation higher composite well-being score, life expectancy was 1.9 years higher for females and 2.6 years higher for males (Exhibit 1). When race, education, and poverty were introduced into the model, the associations between composite well-being and life expectancy were attenuated but remained significant. In the adjusted regression, every 1-standard-deviation higher composite well-being score was associated with 0.9 year higher female life expectancy and 1.1 years higher male life expectancy (Exhibit 1).
Exhibit 1.
Unadjusted and adjusted associations of standardized well-being and domain scores with life expectancy
| Unadjusted | Adjusted for race, poverty, and education |
|||
|---|---|---|---|---|
| Well-being/domain | Female life expectancy (years) |
Male life expectancy (years) |
Female life expectancy (years) |
Male life expectancy (years) |
| Composite well-being | 1.91 | 2.56 | 0.86 | 1.13 |
| Physical health | 1.97 | 2.52 | 1.18 | 1.35 |
| Emotional health | 1.30 | 1.75 | 0.34 | 0.48 |
| Life evaluation | 1.33 | 1.76 | 0.51 | 0.76 |
| Healthy behaviors | 1.77 | 2.21 | 0.81 | 0.90 |
| Basic access | 1.59 | 2.22 | 1.06 | 1.35 |
| Work environment | 0.55 | 0.89 | 0.04 | 0.19 |
SOURCE Authors’ analysis using data from the Gallup-Healthways Well-being Index, life expectancy estimates, Area Health Resources Files, the American Community Survey 5-year estimates for the years 2009–2013, and data from the SAIPE project.
NOTES Composite well-being and domain scores are standardized—that is, in units of 1 standard deviation. Coefficients represent a change in life expectancy associated with a 1-standard-deviation increase in composite well-being or domain scores. All coefficients are significant at p < 0.002, except for the coefficient representing the adjusted association of the work environment domain with female life expectancy (p = 0.441).
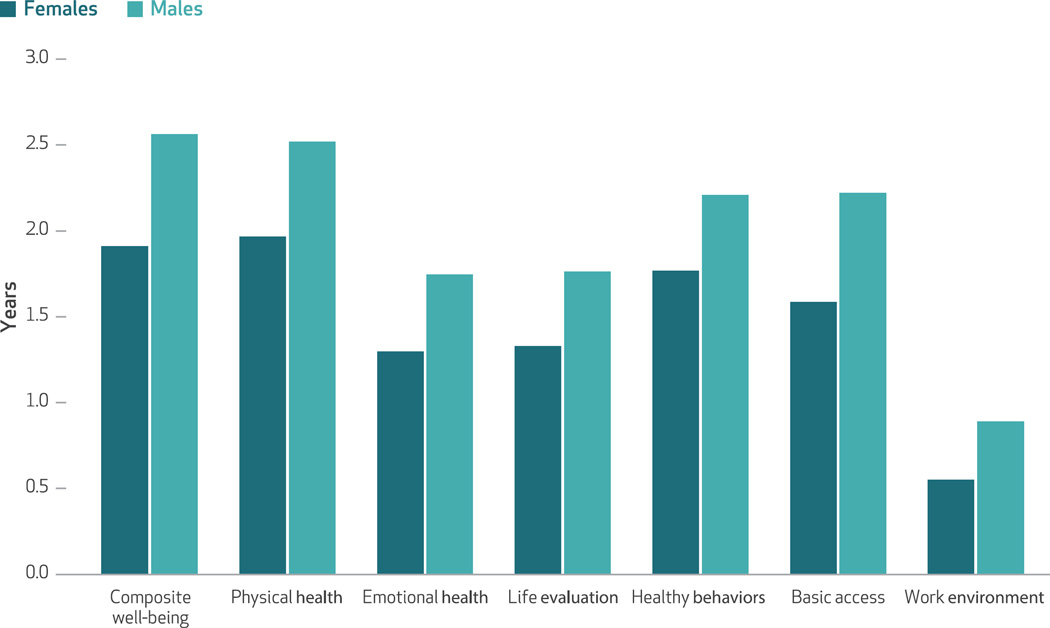
The six domains of well-being were also associated with female and male life expectancy (Exhibit 2). The physical health index was most strongly associated with life expectancy: A 1-standard-deviation increase in physical health was associated with 2.0 years higher female life expectancy and 2.5 years higher male life expectancy. The associations of healthy behaviors and basic access with life expectancy followed closely behind. Every 1-standard-deviation increase in healthy behaviors was associated with 1.8 years higher female life expectancy and 2.2 years higher male life expectancy, while a 1-standard-deviation increase in the basic access index was associated with 1.6 years higher female life expectancy and 2.2 years higher male life expectancy. After race, poverty, and education were controlled for, all six components of well-being remained positively associated with life expectancy, but the effects were attenuated. The only association that became insignificant described the relationship between work environment and female life expectancy (Exhibit 1).
Exhibit 2. Increase in life expectancy associated with a 1-standard-deviation increase in composite well-being or domain scores.
SOURCE Authors’ analysis using data from the Gallup-Healthways Well-being Index and life expectancy estimates. NOTES Composite well-being and domain scores are standardized—that is, in units of 1 standard deviation. Coefficients represent a change in life expectancy associated with a 1-standard-deviation increase in composite well-being or domain scores.
Results from structural equation modeling analyses indicated that well-being partially mediated the associations of race, poverty, and education with life expectancy; all effects were significant (p < 0.001). The total effects represent the overall associations of race, poverty, and education with life expectancy, while the indirect effects represent the parts of these associations that were mediated by well-being. For example, the total effect of poverty on male life expectancy was −0.279, indicating that for every one-unit increase in the poverty rate, male life expectancy decreased 0.279 years. The indirect effect of −0.044 represented the decrease in life expectancy associated with poverty that was mediated by well-being. Therefore, the lower life expectancy in low-income areas was partly explained by low well-being in these counties. The indirect effects from the structural equation models for race and education also indicated that well-being mediated a substantial portion of the relationships between these population characteristics and life expectancy (Exhibit 3).
Exhibit 3.
Effects of population characteristics on life expectancy, mediated by well-being
| Exogenous variable | Direct effect | Indirect effect (effect mediated by well-being) |
Total effect |
|---|---|---|---|
| Female life expectancy | |||
| Percent black | −0.055 | −0.008 | −0.062 |
| Percent Hispanic | 0.012 | 0.005 | 0.017 |
| Percent other minority | 0.013 | 0.007 | 0.020 |
| Percent in poverty | −0.165 | −0.036 | −0.201 |
| Percent high school education | 0.141 | 0.035 | 0.176 |
| Male life expectancy | |||
| Percent black | −0.076 | −0.010 | −0.085 |
| Percent Hispanic | 0.016 | 0.006 | 0.022 |
| Percent other minority | 0.017 | 0.009 | 0.025 |
| Percent in poverty | −0.236 | −0.044 | −0.279 |
| Percent high school education | 0.169 | 0.037 | 0.206 |
SOURCE Authors’ analysis using data from the Gallup-Healthways Well-being Index, life expectancy estimates, Area Health Resources Files, the American Community Survey 5-year estimates for the years 2009–2013, and data from the SAIPE project.
NOTES Each coefficient represents a change in years of life expectancy associated with a one-unit change in the exogenous variable. All coefficients are significant (p < 0.001). The direct effect represents the pathway from the exogenous variable to life expectancy, while controlling for well-being. The indirect effect represents the part of the pathway from the exogenous variable to life expectancy that is mediated by well-being. The total effect is the sum of the direct and indirect effects and represents the association of the exogenous variable with life expectancy.
In sensitivity analyses, excluding counties with fewer than 100 participants did not substantially change our results. The results from these analyses are in the Appendix.26
Discussion
Variation in life expectancy across US counties is substantial. Although differences in race, poverty, and education partly explain these disparities, there is a need to identify other drivers of this variation.1,3–7 In our study we found that population well-being was associated with life expectancy, even after race, poverty, and education were controlled for. Well-being also mediated the relationships of these socioeconomic and demographic factors with life expectancy. Our results highlight well-being as an important population health measure that explains geographic disparities in life expectancy.
Our primary finding was that population wellbeing and life expectancy were positively associated. Several aspects of population well-being have previously been linked with life expectancy or other physical and emotional health outcomes. These components include the prevalence of healthy behaviors, neighborhood safety, access to healthy food, and a place to exercise.4,6,20,35–38 However, to our knowledge, this is the first study to establish a relation between a summary measure of population well-being and life expectancy in a national sample of communities. We also found that all six components of this summary measure—physical health, emotional health, life evaluation, healthy behaviors, basic access, and work environment—were significantly associated with life expectancy. It is not surprising that physical health and healthy behaviors were associated with life expectancy, as these relationships are well established in the literature.3,4 However, other domains, such as life evaluation, which measures life satisfaction and optimism about the future, and basic access, which includes perception of safety and access to housing and health care, were also significantly associated with life expectancy. These results demonstrate that life expectancy is linked with the individual- and community-level factors captured by well-being, ranging from the disease burden of individuals to the safety of neighborhoods.
These findings have several policy implications. By linking well-being with life expectancy, a well-established population health measure, we demonstrate that well-being may be a useful indicator of a community’s health and longevity. Organizations in the United States and abroad already employ well-being metrics to examine population health and to influence and analyze interventions. The Centers for Disease Control and Prevention, the Office for National Statistics in the United Kingdom, and the Organization for Economic Cooperation and Development track various measures of well-being within and across countries.19,39–41 Aspects of well-being, including healthy behaviors and mental health, have also been used to evaluate the impact of Well London, a multiyear, government-supported, and community-engaged program focused on improving health and well-being in disadvantaged neighborhoods of London, England. Program interventions have included mental health awareness training, happiness workshops to increase psychological resilience, healthy cooking classes, development of community gardens, and sports tournaments to encourage physical activity.42–44 The findings of our study suggest the possibility that these types of local investments in wellbeing may reduce health disparities and increase life expectancy, which is an idea worth testing.22
Finally, many aspects of communities with high collective well-being, such as employment opportunities, affordable housing, and public spaces where residents can exercise and build social ties, are determined not by the health care system, but by social and economic policies.20,21,45 Collaboration across sectors to address these community-level characteristics may improve well-being and, potentially, life expectancy.15,22
Although our study uniquely linked population well-being and life expectancy, many prior studies performed at the individual level have shown similar results. These studies have found that happier individuals with higher life satisfaction tend to live longer.12–14,46 This relationship may exist because happier individuals make better life choices, engage in healthier behaviors, and have stronger immune system function, while stress and negative emotions increase inflammation and result in telomere shortening, a known determinant of decreased longevity.12,47,48 At the population level, the mechanisms of the relation between well-being and life expectancy are likely similar but may also reflect the spread of happiness and healthy behaviors through social connections within a community.21,45 The persistence of the association between well-being and life expectancy at the population level underscores the opportunity to design local interventions to improve these outcomes.
Consistent with prior studies, we found that counties with higher percentages of blacks, higher poverty rates, and lower education levels had lower life expectancies.1,3–7,10 Importantly, we also found that the composite well-being score remained significantly associated with life expectancy even after race, poverty, and education were controlled for. These results suggest that well-being expresses aspects of health that are not merely reflecting differences in demographic characteristics. A recent study by Raj Chetty and colleagues is consistent with our findings.6 Although the authors confirmed that income is a powerful predictor of life expectancy, they also discovered significant geographic variation in life expectancy among low-income populations. This variation was partly explained by differences in community characteristics such as the prevalence of unhealthy behaviors, government expenditure levels, and the percentages of college graduates and immigrants.6,49 As in our study, poverty was not the only determinant of life expectancy and community characteristics also predicted health. The findings of Chetty and colleagues’ study and ours highlight a potential opportunity to improve life expectancy among socioeconomically disadvantaged groups by targeting community characteristics that support population well-being.
After race, poverty, and education were controlled for, the six components of well-being also remained positively associated with life expectancy, but the association between work environment and female life expectancy became insignificant. In other words, work environment significantly predicted life expectancy beyond race, poverty and education, but only for males. Similarly, all associations between the components of population well-being and life expectancy were stronger for males than for females. A deeper exploration of why the associations between well-being and life expectancy vary by sex was beyond the scope of this paper but would be an important focus for future work.
Through structural equation modeling, we showed that well-being mediated the relationships between race, poverty, and education with life expectancy. These results are consistent with findings from previous studies that explored health inequalities across demographic groups. Lower life expectancies among populations with higher percentages of blacks, higher poverty rates, and lower education levels may be caused by higher levels of stress, less effective chronic disease management, worse health behaviors, decreased access to community resources, and increased exposure to harmful workplace practices within these populations.5,7,10,50–52 We found that well-being, which includes these predictors of health, explained between 10 percent and 35 percent of the associations of race, poverty, and education with life expectancy. Not surprisingly, among the demographic characteristics we tested, poverty was most strongly associated with life expectancy. However, almost one-fifth of this effect was mediated by well-being. Therefore, a substantial portion of the negative effect of poverty on life expectancy is explained by the lower well-being experienced by low-income populations. Similarly, the lower life expectancy experienced by populations with higher percentages of blacks and lower percentages of high school graduates was partly explained by the lower well-being among these groups. These results emphasize the potential opportunity to reduce disparities in life expectancy by targeting population well-being.
Conclusion
Population well-being—a comprehensive evaluation of physical, mental, and social health—helps explain geographic disparities in life expectancy. Local initiatives aimed to enhance population well-being and its components may improve not only the quality of life in a community, but also the quantity of life among its inhabitants.
Acknowledgments
Anita Arora is supported by the Robert Wood Johnson Foundation (RWJF) and the Yale Center for Clinical Investigation through Clinical and Translational Science Award (CTSA) Grant No. TL1 TR001864 from the National Center for Advancing Translational Science (NCATS), a component of the National Institutes of Health (NIH). Erica Spatz and Brita Roy are supported by Grant No. K12HS023000 from the Agency for Healthcare Research and Quality (AHRQ) Patient Centered Outcomes Research (PCOR) Institutional Mentored Career Development Program. Roy is also supported by a grant from the RWJF. Spatz, Jeph Herrin, and Harlan Krumholz also report receiving support from the Centers for Medicare and Medicaid Services to develop and maintain performance measures that are used in public reporting programs. Kenneth Kell and Elizabeth Rula are employees and shareholders in Healthways, the company that developed the measure of well-being used in this article. Carter Coberley is also a shareholder in Healthways. Krumholz is a recipient of research agreements from Medtronic and from Johnson & Johnson (Janssen), through Yale University, to develop methods of clinical trial data sharing; is the recipient of a grant from the Food and Drug Administration (FDA) and Medtronic to develop methods for postmarket surveillance of medical devices; chairs a cardiac scientific advisory board for UnitedHealth; and is the founder of Hugo, a personal health information platform. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of NIH, RWJF, AHRQ, CMS, or the FDA.
Footnotes
This study was presented as a poster at the Society of General Internal Medicine 38th Annual Meeting in Toronto, Ontario, in April 2015.
Contributor Information
Anita Arora, Email: Anita.Arora@yale.edu, Robert Wood Johnson Foundation Clinical Scholar at Yale School of Medicine, in New Haven, Connecticut.
Erica Spatz, Department of Cardiovascular Medicine, Yale School of Medicine.
Jeph Herrin, Department of Cardiovascular Medicine, Yale School of Medicine.
Carley Riley, Cincinnati Children’s Hospital Medical Center, in Ohio.
Brita Roy, Yale School of Medicine.
Kenneth Kell, Healthways, in Franklin, Tennessee.
Elizabeth Rula, Healthways, in Franklin, Tennessee.
Harlan M. Krumholz, Harold H. Hines, Jr. Professor of Medicine at Yale School of Medicine and director of the Yale Center for Outcomes Research and Evaluation (CORE)
NOTES
- 1.Wang H, Schumacher AE, Levitz CE, Mokdad AH, Murray CJ. Left behind: widening disparities for males and females in US county life expectancy, 1985–2010. Popul Health Metr. 2013;11(1):8. doi: 10.1186/1478-7954-11-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lowrey A. Income gap, meet the longevity gap. [cited 2016 Sep 29];New York Times [serial on the Internet] 2014 Mar 15; Available from: http://www.nytimes.com/2014/03/16/business/income-gap-meet-the-longevity-gap.html. [Google Scholar]
- 3.Murray CJ, Kulkarni SC, Michaud C, Tomijima N, Bulzacchelli MT, Iandiorio TJ, et al. Eight Americas: investigating mortality disparities across races, counties, and race-counties in the United States. PLoS Med. 2006;3(9):e260. doi: 10.1371/journal.pmed.0030260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Danaei G, Rimm EB, Oza S, Kulkarni SC, Murray CJ, Ezzati M. The promise of prevention: the effects of four preventable risk factors on national life expectancy and life expectancy disparities by race and county in the United States. PLoS Med. 2010;7(3):e1000248. doi: 10.1371/journal.pmed.1000248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goh J, Pfeffer J, Zenios S. Exposure to harmful workplace practices could account for inequality in life spans across different demographic groups. Health Aff (Millwood) 2015;34(10):1761–1768. doi: 10.1377/hlthaff.2015.0022. [DOI] [PubMed] [Google Scholar]
- 6.Chetty R, Stepner M, Abraham S, Lin S, Scuderi B, Turner N, et al. The association between income and life expectancy in the United States, 2001–2014. JAMA. 2016;315(16):1750–1766. doi: 10.1001/jama.2016.4226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Olshansky SJ, Antonucci T, Berkman L, Binstock RH, Boersch-Supan A, Cacioppo JT, et al. Differences in life expectancy due to race and educational differences are widening, and many may not catch up. Health Aff (Millwood) 2012;31(8):1803–1813. doi: 10.1377/hlthaff.2011.0746. [DOI] [PubMed] [Google Scholar]
- 8.Singh GK, Siahpush M. Widening socioeconomic inequalities in US life expectancy, 1980–2000. Int J Epidemiol. 2006;35(4):969–979. doi: 10.1093/ije/dyl083. [DOI] [PubMed] [Google Scholar]
- 9.Yang TC, Noah A, Shoff C. Exploring geographic variation in US mortality rates using a spatial Durbin approach. Popul Space Place. 2015;21(1):18–37. doi: 10.1002/psp.1809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McLaughlin DK, Stokes CS. Income inequality and mortality in US counties: does minority racial concentration matter? Am J Public Health. 2002;92(1):99–104. doi: 10.2105/ajph.92.1.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sparks PJ, Sparks CS. An application of spatially autoregressive models to the study of US county mortality rates. Popul Space Place. 2010;16(6):465–481. [Google Scholar]
- 12.Diener E, Chan MY. Happy people live longer: subjective well-being contributes to health and longevity. Appl Psychol Health Well Being. 2011;3(1):1–43. [Google Scholar]
- 13.Chida Y, Steptoe A. Positive psychological well-being and mortality: a quantitative review of prospective observational studies. Psychosom Med. 2008;70(7):741–756. doi: 10.1097/PSY.0b013e31818105ba. [DOI] [PubMed] [Google Scholar]
- 14.Xu J, Roberts RE. The power of positive emotions: it’s a matter of life or death—subjective well-being and longevity over 28 years in a general population. Health Psychol. 2010;29(1):9–19. doi: 10.1037/a0016767. [DOI] [PubMed] [Google Scholar]
- 15.Woolf SH, Purnell JQ. The good life: working together to promote opportunity and improve population health and well-being. JAMA. 2016;315(16):1706–1708. doi: 10.1001/jama.2016.4263. [DOI] [PubMed] [Google Scholar]
- 16.Steptoe A, Deaton A, Stone AA. Subjective wellbeing, health, and ageing. Lancet. 2015;385(9968):640–648. doi: 10.1016/S0140-6736(13)61489-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gallup-Healthways. Gallup-Healthways Well-being Index: methodology report for indexes [Internet] Washington (DC): Gallup; c; 2009. [cited 2016 Sep 29]. Available for download from: http://www.gallup.com/poll/195539/gallup-healthways-index-methodology-report-indexes.aspx. [Google Scholar]
- 18.World Health Organization. Preamble to the Constitution of the World Health Organization as adopted by the International Health Conference; 19–22 June, 1946; New York. New York (NY): United Nations World Health Organization Interim Commission; 1948. Jun, signed on 22 July 1946 by the representatives of 61 States (Official Records of the World Health Organization, no. 2, p. 100) and entered into force on 7 April 1948. [Google Scholar]
- 19.Kobau R, Bann C, Lewis M, Zack MM, Boardman AM, Boyd R, et al. Mental, social, and physical wellbeing in New Hampshire, Oregon, and Washington, 2010 Behavioral Risk Factor Surveillance System: implications for public health research and practice related to Healthy People 2020 foundation health measures on well-being. Popul Health Metr. 2013;11(1):19. doi: 10.1186/1478-7954-11-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci. 2010;1186:125–145. doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- 21.Prilleltensky I. Promoting wellbeing: time for a paradigm shift in health and human services. Scand J Public Health Suppl. 2005;66:53–60. doi: 10.1080/14034950510033381. [DOI] [PubMed] [Google Scholar]
- 22.Erickson D, Andrews N. Partnerships among community development, public health, and health care could improve the well-being of low-income people. Health Aff (Millwood) 2011;30(11):2056–2063. doi: 10.1377/hlthaff.2011.0896. [DOI] [PubMed] [Google Scholar]
- 23.GHDx. United States life expectancy estimates by county 1985–2010 [Internet] Seattle (WA): Institute for Health Metrics and Evaluation; [cited 2016 Sep 28]. last modified 2014 Sep 3; Available from: http://ghdx.healthdata.org/record/united-states-life-expectancy-estimates-county-1985-2010. [Google Scholar]
- 24.Kahneman D, Riis J. Living, and thinking about it: two perspectives on life. In: Huppert FA, Baylis N, Keverne B, editors. The science of well-being. Oxford: Oxford University Press; 2005. pp. 285–304. [Google Scholar]
- 25.Diener E. Guidelines for national indicators of subjective well-being and ill-being. Appl Res Qual Life. 2006;1(2):151–157. [Google Scholar]
- 26.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 27.Gandy WM, Coberley C, Pope JE, Rula EY. Well-being and employee health—how employees’ well-being scores interact with demographic factors to influence risk of hospitalization or an emergency room visit. Popul Health Manag. 2014;17(1):13–20. doi: 10.1089/pop.2012.0120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sears LE, Shi Y, Coberley CR, Pope JE. Overall well-being as a predictor of health care, productivity, and retention outcomes in a large employer. Popul Health Manag. 2013;16(6):397–405. doi: 10.1089/pop.2012.0114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Health Resources and Services Administration. Rockville (MD): HRSA; 2010. [cited 2016 Sep 29]. Area Health Resources Files: population by race and ethnicity [Internet] Available for download from: http://ahrf.hrsa.gov/ALLVARs_list.asp. [Google Scholar]
- 30.Census Bureau. Washington (DC): Census Bureau; [cited 2016 Sep 29]. 2009–2013 American Community Survey 5-year estimates [Internet] Available for download from: http://factfinder.census.gov/faces/nav/jsf/pages/searchresults.xhtml. [Google Scholar]
- 31.Census Bureau. Washington (DC): Census Bureau; 2010. [cited 2016 Sep 29]. Small Area Income and Poverty Estimates (SAIPE) for school districts, counties, and states [Internet] Available for download from: https://www.census.gov/did/www/saipe/data/statecounty/data/2010.html. [Google Scholar]
- 32.Gunzler D, Chen T, Wu P, Zhang H. Introduction to mediation analysis with structural equation modeling. Shanghai Arch Psychiatry. 2013;25(6):390–394. doi: 10.3969/j.issn.1002-0829.2013.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yang TC, Jensen L, Haran M. Social capital and human mortality: explaining the rural paradox with county-level mortality data. Rural Sociol. 2011;76(3):347–374. doi: 10.1111/j.1549-0831.2011.00055.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Singh GK, Siahpush M. Widening rural-urban disparities in life expectancy, U.S., 1969–2009. Am J Prev Med. 2014;46(2):e19–e29. doi: 10.1016/j.amepre.2013.10.017. [DOI] [PubMed] [Google Scholar]
- 35.Mujahid MS, Diez Roux AV, Shen M, Gowda D, Sanchez B, Shea S, et al. Relation between neighborhood environments and obesity in the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2008;167(11):1349–1357. doi: 10.1093/aje/kwn047. [DOI] [PubMed] [Google Scholar]
- 36.Auchincloss AH, Diez Roux AV, Mujahid MS, Shen M, Bertoni AG, Carnethon MR. Neighborhood resources for physical activity and healthy foods and incidence of type 2 diabetes mellitus: the Multi-Ethnic Study of Atherosclerosis. Arch Internal Med. 2009;169(18):1698–1704. doi: 10.1001/archinternmed.2009.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Unger E, Diez-Roux AV, Lloyd-Jones DM, Mujahid MS, Nettleton JA, Bertoni A, et al. Association of neighborhood characteristics with cardiovascular health in the Multi-Ethnic Study of Atherosclerosis (MESA) Circ Cardiovasc Qual Outcomes. 2014;7(4):524–531. doi: 10.1161/CIRCOUTCOMES.113.000698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schule SA, Bolte G. Interactive and independent associations between the socioeconomic and objective built environment on the neighbourhood level and individual health: a systematic review of multilevel studies. PloS One. 2015;10(4):e0123456. doi: 10.1371/journal.pone.0123456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Organization for Economic Cooperation and Development. How’s life? 2015: measuring well-being. Paris: OECD Publishing; 2015. [Google Scholar]
- 40.Centers for Disease Control and Prevention. Atlanta (GA): CDC; [cited 2016 Sep 29]. Health-Related Quality of Life (HRQOL), well-being concepts [Internet] last updated 2016 May 31; Available from: http://www.cdc.gov/hrqol/wellbeing.htm. [Google Scholar]
- 41.Office for National Statistics. London: ONS; 2016. Jul 7, [cited 2016 Sep 29]. Personal well-being in the UK: 2015 to 2016 [Internet] Available from: http://www.ons.gov.uk/peoplepopulationandcommunity/wellbeing/bulletins/measuringnationalwellbeing/2015to2016. [Google Scholar]
- 42.Derges J, Clow A, Lynch R, Jain S, Phillips G, Petticrew M, et al. “Well London” and the benefits of participation: results of a qualitative study nested in a cluster randomised trial. BMJ Open. 2014;4(4):e003596. doi: 10.1136/bmjopen-2013-003596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Phillips G, Bottomley C, Schmidt E, Tobi P, Lais S, Yu G, et al. Well London Phase-1: results among adults of a cluster-randomised trial of a community engagement approach to improving health behaviours and mental well-being in deprived innercity neighbourhoods. J Epidemiol Community Health. 2014;68(7):606–614. doi: 10.1136/jech-2013-202505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Phillips G, Bottomley C, Schmidt E, Tobi P, Lais S, Yu G, et al. Measures of exposure to the Well London Phase-1 intervention and their association with health, well-being, and social outcomes. J Epidemiol Community Health. 2014;68(7):597–605. doi: 10.1136/jech-2013-202507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fowler JH, Christakis NA. Dynamic spread of happiness in a large social network: longitudinal analysis over 20 years in the Framingham Heart Study. BMJ. 2008;337:a2338. doi: 10.1136/bmj.a2338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lawrence EM, Rogers RG, Wadsworth T. Happiness and longevity in the United States. Soc Sci Med. 2015;145:115–119. doi: 10.1016/j.socscimed.2015.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Epel ES, Blackburn EH, Lin J, Dhabhar FS, Adler NE, Morrow JD, et al. Accelerated telomere shortening in response to life stress. Proc Natl Acad Sci U S A. 2004;101(49):17312–17315. doi: 10.1073/pnas.0407162101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Veenhoven R. Healthy happiness: effects of happiness on physical health and the consequences for preventive health care. J Happiness Stud. 2008;9(3):449–469. [Google Scholar]
- 49.McGinnis JM. Income, life expectancy, and community health: underscoring the opportunity. JAMA. 2016;315(16):1709–1710. doi: 10.1001/jama.2016.4729. [DOI] [PubMed] [Google Scholar]
- 50.Goldman DP, Smith JP. Can patient self-management help explain the SES health gradient? Proc Natl Acad Sci U S A. 2002;99(16):10929–10934. doi: 10.1073/pnas.162086599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.McEwen BS, Gianaros PJ. Central role of the brain in stress and adaptation: links to socioeconomic status, health, and disease. Ann N Y Acad Sci. 2010;1186:190–222. doi: 10.1111/j.1749-6632.2009.05331.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Seeman T, Epel E, Gruenewald T, Karlamangla A, McEwen BS. Socioeconomic differentials in peripheral biology: cumulative allostatic load. Ann N Y Acad Sci. 2010;1186:223–239. doi: 10.1111/j.1749-6632.2009.05341.x. [DOI] [PubMed] [Google Scholar]