Abstract
Background
To determine the cost-effectiveness of In-Home Cognitive Behavioral Therapy (IH-CBT) for low-income mothers enrolled in a home visiting program.
Methods
A cost-utility analysis was conducted using results from a clinical trial of IH-CBT and standard of care for depression derived from the literature. A probabilistic, patient-level Markov model was developed to determine Quality Adjusted Life Years (QALYs). Costs were determined using the Medical Expenditure Panel Survey. A three-year time horizon and payer perspective were used. Sensitivity analyses were employed to determine robustness of the model.
Results
IH-CBT was cost-effective relative to standard of care. IH-CBT was expected to be cost-effective at a three-year time horizon 99.5%, 99.7%, and 99.9% of the time for willingness-to-pay thresholds of US$25,000, US$50,000, and US$100,000, respectively. Patterns were upheld at one-year and five-year time horizons. Over the three-year time horizon, mothers receiving IH-CBT were expected to have 345.6 fewer days of depression relative to those receiving standard home visiting and treatment in the community.
Conclusions
IH-CBT is a more cost-effective treatment for low-income, depressed mothers than current standards of practice. These findings add to the growing literature demonstrating the cost-effectiveness of CBT for depression, and expand it to cover new mothers. From a payer perspective, IH-CBT is a sound option for treatment of depressed, low-income mothers. Limitations include a restricted time horizon and estimating of standard of care costs.
Keywords: major depression, mothers, cognitive-behavioral therapy, cost-effectiveness
1. Introduction
Major depressive disorder (MDD) is a disabling psychiatric condition, particularly in new mothers (O’Hara and Wisner, 2014). The symptoms of depression, including fatigue, anhedonia, and feelings of worthlessness, contribute to functional impairments in parenting and nurturing. These, in turn, increase the risk for maladjustment and poor developmental outcomes in offspring (Goodman et al., 2011). The onset of depression in new mothers often begins during pregnancy and extends episodically through the child rearing years. Banti et al. (2011) found that 12.4% of women met criteria for minor or major depression during pregnancy. Wisner et al. (2013) reported that 14.0% of mothers exceeded clinical cutoffs on a screen for depression administered during 4–6 weeks postpartum. Another study examined self-reported depression measured at 10 time points over the first 12 years, reporting that 20.7% exceeded clinical cutoffs on average at one or more time points (Campbell et al., 2009). Low-income mothers are especially at risk for developing depression and for experiencing the deleterious consequences of the condition (Goyal et al., 2010).
1.1 Costs of depression in low-income mothers
In addition to its human costs, depression in mothers has financial implications as well. In depressed adults, Greenberg et al. (2003) found that, in 2000, the economic burden of depression was US$83.1 billion. These reflect costs in health care, labor productivity, and mortality. Documented costs associated with maternal depression include increased utilization of health care services (Greenberg et al., 2003), increased rates of prematurity and low birthweight that require specialized care of children (Jarde et al., 2016), and additional health and related costs (Smith and Smith, 2010). Ammerman et al. (2016) examined health care and labor productivity costs in low-income, depressed mothers. They documented US$2.41 billion in added direct and indirect costs annually in depressed mothers relative to their non-depressed counterparts. Delivery of effective treatments to depressed mothers who are at highest risk is essential to facilitate recovery, mitigate impact on offspring, and reduce costs to payers and society.
1.2 Treatment of depression in low-income mothers in home visiting
Providing treatment to low-income mothers with depression is complicated by barriers to identification, engagement, and retention. Recently, there have been calls to identify, screen, and treat mothers in the context of other programs that provide services to low-income mothers as a way to overcome these barriers (O’Connor et al., 2016). Early childhood prevention programs, in particular home visiting (Ammerman, 2016), provide a promising opportunity for delivery of effective treatment. Home visiting programs, both targeted and universal, are widely available in many developed countries (Engle et al., 2007). Home visiting programs seek to support new mothers in their roles as parents. They strive to teach parenting skills and promote a safe and nurturing environment for children in order to optimize developmental outcomes. Home visiting services are voluntary, and many routinely screen for depression. Research suggests that up to 61% of mothers in home visiting experience clinically elevated levels of depression during the course of service (Ammerman et al., 2010). A subgroup of mothers experiences a persistently high level of symptoms throughout the first years of the child’s life (Teeters et al., 2016). Home visiting alone appears to have little to no impact on depressive symptoms in mothers participating in home visiting (Ammerman et al., 2010), thus warranting direct treatment as the most appropriate response in most cases.
Ammerman et al. (2011) adapted cognitive behavioral therapy to meet the needs of depressed, low-income mothers enrolled in home visiting. In-Home Cognitive Behavioral Therapy (IH-CBT) is implemented by therapists who provide treatment concurrently with ongoing home visiting. IH-CBT uses strategies that facilitate engagement, make content relevant to the needs of low-income mothers, allow delivery in the home, and promote a collaborative relationship between the therapist and home visitor in order to smoothly coordinate services. Empirical support for IH-CBT was established in a clinical trial comparing mothers who received IH-CBT and concurrent home visiting with those who received home visiting alone (Ammerman et al., 2013). In this study, 93 mothers were first identified using the Edinburgh Postnatal Depression Scale (Cox et al., 1987) administered at three months postpartum as part of a standardized screening schedule. This was followed by diagnosis of MDD using a semi-structured interview. Following random assignment to treatment and control groups, mothers were re-assessed at post-treatment and at three-month follow-up. Results indicated that mothers receiving IH-CBT experienced significant benefits in terms of depression reduction relative to controls. Compared to those receiving home visiting alone, mothers in the IH-CBT condition were less likely to meet diagnostic criteria for MDD at post-treatment, reported fewer depressive symptoms, and obtained lower scores on clinician ratings of depression severity.
Mothers receiving IH-CBT also reported increased social support, improved functioning in day-to-day activities, and decreased psychological distress. Gains were maintained at three-month follow-up. Findings remained when controlling for other psychiatric conditions, severity of MDD, therapist, home visiting model, and number of home visits. It is noteworthy that some mothers in the standard home visiting condition received treatment in the community, although as expected, this was often insufficient or ended prematurely. Mothers received a significantly larger dose of IH-CBT treatment than what is typically observed in center-based mental health settings (Hansen et al., 2002; 11.2 vs. 4.3 sessions). Mothers who completed all sessions of IH-CBT treatment did especially well, with 78.3% no longer meeting criteria for major depressive disorder at post-treatment and 90.5% recovered at follow-up. Mothers who recovered from depression reported increased ability to cope with stress related to the parenting role and more nurturing parenting of their children (Ammerman et al., 2014).
1.3 Study objectives
Although empirical testing documents the clinical impact of IH-CBT in depressed mothers in home visiting, there is a need to examine the cost-effectiveness of the treatment. The purpose of a cost-effectiveness analysis is to determine if a treatment confers greater benefits at a given level of cost or equivalent benefits for less cost (Byford and Bower, 2002). Cost-effectiveness analyses guide decision makers in selecting and paying for certain treatments over others given limited resources. Despite a broad consensus that such studies are important to clinical decision-making (Hill, 2012), relatively few such analyses have been undertaken in the treatment of depression generally (Barrett et al., 2005; Brettschneider et al., 2014) or for maternal depression in particular (Dennis, 2005). For cognitive behavioral therapy (CBT) as a treatment of depression in adults, findings have been mixed. Some studies have suggested that CBT is cost-effective relative to antidepressant medications, while others have reported the opposite finding (Barret et al., 2005). As such, determining the cost-effectiveness of IH-CBT is an important undertaking both in understanding its economic value for low-income, depressed mothers and for the field as a whole in order to guide selection of and payment for this treatment option.
The purpose of this study was to estimate the cost-effectiveness of IH-CBT delivered concurrently with home visiting compared to home visiting alone in low-income, depressed mothers. We hypothesized that IH-CBT would be more cost-effective than the home visiting in conjunction with the most commonly used treatment approach (antidepressant medications). Specifically, we reasoned that IH-CBT would result in decreased costs given its high degree of clinical effectiveness with low-income depressed mothers participating in home visiting. The study was performed using the perspective of the payer, Medicaid, for services to this population in the United States. Home visiting and access to antidepressant medications was assumed in the comparison cohort over a three-year time horizon. We performed a cost utility analysis, expressing benefits in terms of quality-adjusted life years gained (QALYs). An incremental cost effectiveness ratio was computed, which compared the change in costs divided by the change in QALYs under IH-CBT versus home visiting alone.
2. Methods
2.1 Study population
The study population consisted of 93 new, low-income mothers who were enrolled in a home visiting program and were diagnosed with MDD. [A full description of the sample and recruitment procedures is in Ammerman et al. (2013).] Mothers were enrolled in Every Child Succeeds, a community-based home visitation program serving Southwestern Ohio and Northern Kentucky (USA). The geographic area covered by the program included urban, suburban and rural areas. Two models of home visiting were utilized in this program: Nurse-Family Partnership (NFP; Olds, 2010) and Healthy Families America (HFA; Holton and Harding, 2007). Participating mothers had at least one of the following demographic risk characteristics needed for eligibility: unmarried, low-income, ≤18 years, inadequate prenatal care. Mothers were enrolled in home visiting prior to 28 weeks’ gestation in NFP as per model parameters and from 20 weeks’ gestation through the child reaching three months of age for HFA. Mothers were referred from prenatal clinics, hospitals, social service agencies, and community physicians. In the NFP home visits were provided by nurses, while in HFA home visits were provided by social workers, related professionals and paraprofessionals. The goals of the home visitation program were to (1) improve pregnancy outcomes through nutrition education and substance use reduction; (2) support parents in providing children with a safe, nurturing, and stimulating home environment; (3) optimize child health and development; (4) link families to healthcare and other needed services; and (5) promote economic self-sufficiency.
Mothers were young (range was 16 to 37 years, M=21.9, SD=4.8), predominantly Caucasian (62.4%) and African-American (32.2%), unmarried (87.1%), and low-income (76.3% <US$20,000 annual household income). The breakdown of MDD severity was Mild = 28.0%, Moderate = 48.4%, and Severe = 23.6%. Onset of the presenting episode during postpartum (within 6 weeks after birth) was found in 29.0% of participants. Recurrent depression was reported by 74.2% of mothers (mean number of episodes = 2.6 (SD = 1.6), mean age of first episode = 15.2 years (SD = 5.1)). Comorbidity was high, with 76.1% of participants meeting criteria for other psychiatric disorders. The five most represented diagnoses were: PTSD = 40.9%, Generalized Anxiety Disorder = 36.6%, Social Phobia = 30.1%, Obsessive-Compulsive Disorder= 26.9%, Panic Disorder = 25.8%.
As part of the clinical trial, mothers were randomized to receive IH-CBT treatment delivered concurrently with on going home visiting (IH-CBT) or standard home visiting (SHV) alone. Mothers in both study arms received home visits according to the two home visiting approaches. Those in the SHV condition had the opportunity to receive community-based care and/or medication for the treatment of their MDD although few obtained or received adequate treatment. Mothers in the IH-CBT condition received 15 weekly sessions of cognitive behavioral therapy delivered in their home provided by a master’s-level therapist.
2.2 Modeling strategies
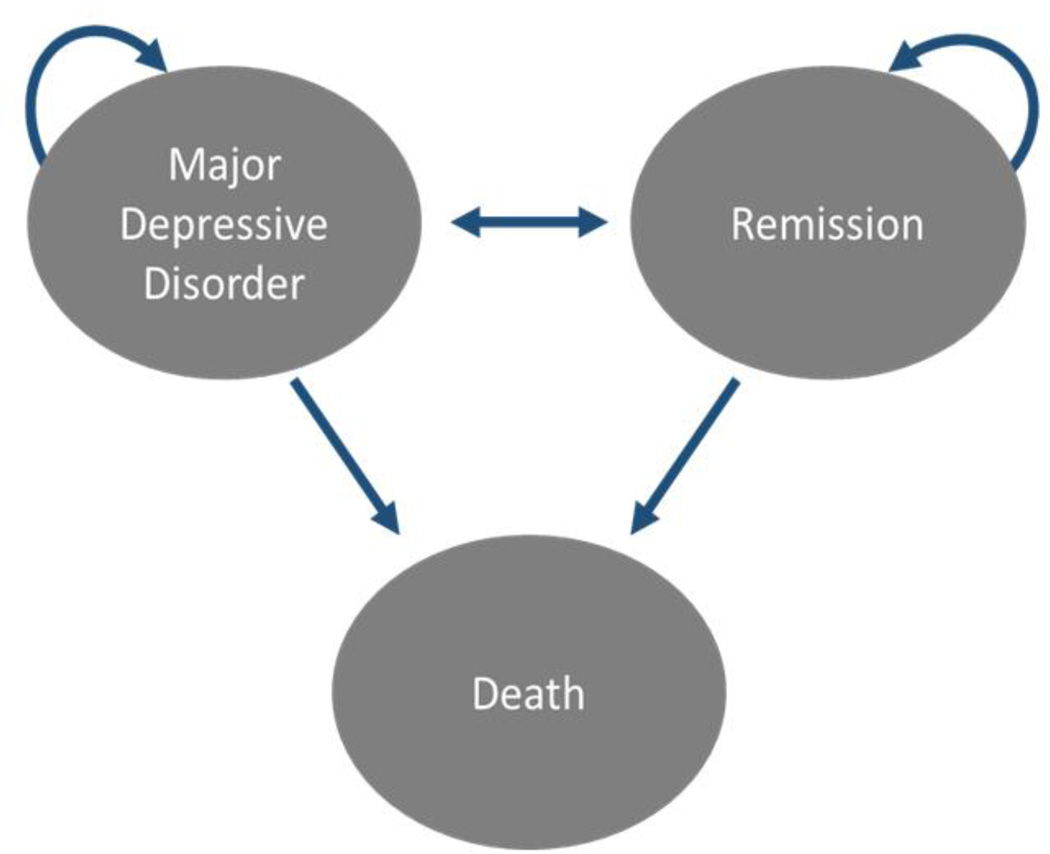
Effect sizes and results from the clinical trial were used in the economic models. The effectiveness measure used in the model was QALYs. QALYs represent both the quality and quantity of life. They are measured by a utility score where 1 represents perfect health and 0 represents death. The utility score is multiplied by each year the mother is alive to adjust for the fact that mother’s quality of life is impaired when in an MDD state. The mothers in the model were followed for three years. A probabilistic, patient-level Markov model was developed using TreeAge v2014 software (TreeAge, Williamstown MA, 2016) to conduct a cost-utility analysis (CUA) based on the findings of Ammerman et al. (2013). Figure 1 illustrates health state transitions in the model. Modeling strategies followed recommended practices by the International Society of Pharmacoeconomics and Outcomes Research and the Society of Medical Decision Making (Roberts et al., 2012; Siebert et al., 2012).
Fig. 1.
The diagram illustrates the health states (ovals) and possible transitions between health states (arrows) of a mother in the model. All patients begin in the Major Depressive Disorder health state and can transition to the next health state based on the arrows and transition probabilities. Each health state has a background mortality risk based on age and can transition to death.
2.3 Parameter estimates
Patient and clinical data for IH-CBT and SHV conditions were obtained from the clinical trial conducted by Ammerman et al. (2013). After the treatment interval, transition probabilities were obtained from the published literature to estimate the likelihood of remaining in an MDD health state, relapsing to an MDD health state, transitioning to a remission health state, and dying. At every time period and in each health state, subjects may transition to death. These transition probabilities were summarized from a best-evidence systematic literature review, described below, and applied to each cohort. Patients in MDD have a greater likelihood of transitioning to death to account for depression-related suicide. The probabilities of receiving medication and office-based treatment for MDD, hospitalization due to MDD, and suicide were also obtained from the published literature.
Cost data included costs of IH-CBT treatment and home visiting and costs related to medical care that were obtained from the Ohio Department of Medicaid (2014) where possible. It was augmented from the published literature when necessary from a public payer perspective. Health state utility information was obtained from the Medical Expenditure Panel Survey (MEPS) from the Agency for Healthcare Research and Quality (2015). The MEPS uses the EuroQoL EQ-5D, self-reported health status, and SF-12® survey instruments. This study employed the EQ-5D. The EQ-5D is well-suited for cost-utility analyses as it provides a utility score from 0 to 1, facilitating conversion of life years to QALYs. The utility values reflect an “at-risk” mother sample that was derived from a previous study delineating the health care and labor productivity costs associated with depression in demographically at-risk mothers (Ammerman et al., 2016).
Clinical data after the treatment intervention and cost data not available from the Ohio Department of Medicaid were obtained from a best-evidence systematic literature review. The best-evidence systematic literature review consisted of a literature search based on a-priori inclusion and ranking criteria. The criteria included studies published in the last ten years, written in English, and that were clinical studies or comparative in nature. All studies were assessed based on their relevance to informing study parameters, validity, quality of the source (i.e. randomized trial vs. observational study), and recentness. The studies meeting these criteria were summarized using the midpoint of the reported estimates as our base value and the full ranges in the sensitivity analysis. Table 1 contains the parameter values used in the analysis and their respective sources.
Table 1.
Parameter values and source.
| PARAMETER NAME |
BASE VALUE |
SD | LO Value |
HI Value |
Distribution | SOURCE |
|---|---|---|---|---|---|---|
| Probabilities | ||||||
| Number of SHV visits |
7 | 5 | 1 | Gamma | Ammerman et al., 2013 | |
| Number of IH-CBT visits |
12.36 | 5.8 | 1 | Gamma | Ammerman et al., 2013 | |
| Number of SHV visits for IH-CBT mothers |
8.7 | 5.4 | 1 | 15 | Gamma | Ammerman et al., 2013 |
| Prob. of office visit | 0.606 | 0.599 | 0.614 | Log-normal | Hasin et al., 2005 | |
| Prob. of office visit - SHV |
0.163 | * | * | * | Ammerman et al., 2013 | |
| Prob. of hospitalization |
0.096 | 0.091 | 0.101 | Log-normal | Hasin et al., 2005 | |
| Prob. of medication - SHV |
0.209 | * | * | * | Ammerman et al., 2013 | |
| Prob. of medication - MDD |
0.606 | 0.599 | 0.614 | Log-normal | Hasin et al., 2005 | |
| Prob. of medication Remission |
0.308 | 0.199 | 0.528 | Log-normal |
Piek et al., 2014 ten Doesschate et al., 2009, Bull et al., 2002 |
|
|
Transition Probabilities |
||||||
| MDD to Remission - SHV |
0.302 | * | * | * | Ammerman et al., 2013 | |
| MDD to Remission - IH-CBT |
0.707 | * | * | * | Ammerman et al., 2013 | |
| MDD to Remission w Tx |
0.157 | 0.120 | 0.191 | Beta | Miranda et al., 2006 | |
| MDD to Remission w/o Tx |
0.106 | 0.071 | 0.138 | Beta | Miranda et al., 2006 | |
| Remission to MDD w Tx |
0.058 | 0.035 | 0.080 | Beta | Dunner, 2007 | |
| Remission to MDD w/o Tx |
0.129 | 0.094 | 0.162 | Beta |
Dunner, 2007; Whiteford et al., 2013 |
|
| Suicide rate | 0.01 | 0.000 | 0.02 | Beta |
Coryell & Young, 2005; Holma, 2004 |
|
| Background mortality rate - 22 years |
0.000454 | ** | ** | ** | U.S. Social Security Administration, 2010 | |
| Background mortality rate - 23 years |
0.000476 | ** | ** | ** | U.S. Social Security Administration, 2010 | |
| Background mortality rate - 24 years |
0.000494 | ** | ** | ** | U.S Social Security Administration, 2010 | |
| Utility | ||||||
| Depressed | 0.69 | 0.29 | Beta | MEPS Data | ||
| Remission | 0.86 | 0.2 | Beta | MEPS Data | ||
| Cost | ||||||
| Initial home visit cost |
$88 | Fixed | Ohio Medicaid | |||
| SHV cost per visit | $46 | Fixed | Ohio Medicaid | |||
| IH-cost CBT per visit |
$88 | Fixed | Ohio Medicaid | |||
| Medications | $80 | $5 | $150 | Triangle | Consumer Reports, 2013 | |
| Hospitalization(s) due to depression |
$5,371 | $5,143 | $5,637 | Triangle | Stensland et al., 2012 | |
| Office Visits | $82 | $74 | $90 | Triangle | Ohio Medicaid | |
| General | ||||||
| Start Age | 22 | |||||
| End Age | 25 | |||||
| Discount Rate | 0.03 |
Parameter value fixed to reflect clinical study results reported in Ammerman et al., 2013
Parameter value fixed to reflect background mortality rates reported in US Life Tables
2.4 Analytic strategy
The CUA estimated the incremental costs and effects of SHV + IH-CBT compared to SHV alone. The model simulated the transitions between the health states throughout a three-year time frame for the mothers. The clinical and cost parameter estimates obtained from the best-evidence systematic literature review were extrapolated over the three-year time frame. A three-year time frame was chosen because payers typically do not consider beyond a three-year time horizon in their decision making. Scenario analyses evaluated the impact of time by examining a 1-year and 5-year horizons. The future costs and outcomes were discounted, which emphasizes the results seen in the clinical trial. The model was designed to examine outcomes following the treatment period of IH-CBT. Therefore, cycle times (the block of time after which outcomes were observed) were set at four months. The four-month cycle time approximated the treatment duration of IH-CBT. Monte Carlo Simulation was performed to estimate the results based on 1,000 model runs drawing parameter values based on the parameter’s range and distribution.
To illustrate this method, let Ci and Ei denote, respectively, the costs and effects (QALYs) of the IH-CBT treatment, and Co and Eo denote, respectively, the costs and effects of the SHV strategy. With that, the incremental cost-effectiveness ratio (ICER) for SHV + IH-CBT will be calculated as:
| (1) |
The CUA evaluated three different amounts that represent maximum thresholds an insurance company would be willing to pay (willingness-to-pay) for one additional QALY. These thresholds were US$25,000, US$50,000 and US$100,000 per QALY gained to assess the cost-effectiveness of SHV + IH-CBT compared to SHV. All model parameters were expressed as probabilities and listed as an annual rate. The model transformed the annual rates into four-month rates to correspond with the treatment duration of IH-CBT. The following formula was used to make this transformation.
| (2) |
where Prob is the annual probability of a given parameter to account for the four-month cycle.
The CUA model included costs and QALYs for both treatment arms, and used this information to calculate ICERs. A 3% discount rate was applied to all costs and QALYs in the model. The discount rate is used to determine the present value of future costs and clinical outcomes and is needed because costs and outcomes occur at different points in time. All costs were expressed in 2013 US dollars using the Medical Care Component of the Consumer Price Index. One- and five-year time horizons were also evaluated.
2.5 Sensitivity analysis
One-way and probabilistic sensitivity analyses were performed. One-way sensitivity analyses were performed to gauge the robustness and reliability of the results to changes in individual model input values. This sensitivity analysis thus entailed varying key model input values one-by-one and recalculating the ICER each time a change was made. Probabilistic sensitivity analysis used the model parameter ranges, distributions, and Monte Carlo simulation methods to recalculate the ICERs. This type of sensitivity analysis allows for scenarios that consider simultaneous variations in parameter values.
2.6 Model validation
The model results were validated against the published results in Ammerman et al. (2013). The rates of reduction in MDD for the IH-CBT and SHV conditions for the intervention and follow-up periods were compared at the conclusion of the first cycle and the second cycle of the model. The model was considered valid if the model results were within the standard deviation of the reported results in Ammerman et al. (2013). These time periods for validation corresponded with the intervention and follow-up time periods used by Ammerman et al. (2013).
3. Results
Table 2 reports the results for the CUA, which assumed a base case of three-year follow up, as well as, one-year and five-year time horizons. In the base case model assuming a three-year time horizon, IH-CBT was expected to be a dominant intervention compared to SHV alone. A dominant intervention is one that improves quality-of-life and decreases costs. In the three-year base case, IH-CBT was expected to improve QALYs by 0.07 QALYs (approximately 1 month) and reduce costs by US$2. IH-CBT was expected to be cost-effective 99.5%, 99.7%, and 99.9% of the time for willingness-to-pay thresholds of US$25,000, US$50,000, and US$100,000, respectively. Further, mothers receiving IH-CBT were expected to have 345.6 fewer days of depression relative to those receiving standard home visiting and treatment in the community over the three-year time horizon. Examining a one-year time horizon, IH-CBT was expected to have an ICER of US$9,862 and to be cost-effective 93.6%, 99.1%, and 99.7% at willingness-to-pay thresholds of US$25,000, US$50,000, and US$100,000, respectively. When a five-year time horizon was considered, SHV + IH-CBT was expected to be a dominant strategy 99.7% of the time for willingness-to-pay thresholds of US$25,000, US$50,000, and US$100,000, respectively. Alternative values for the discount rate were considered to account for different rates of time preference because a higher (lower) discount rate places less (more) weight on future costs and benefits. The results of this exercise indicated that varying the discount rate from 0% to 8% did not materially alter the results and IH-CBT remained a cost-effective strategy.
Table 2.
Cost-utility analysis for 3-year, 1-year, and 5-year time horizons.
| Strategy | Mean Costs |
Mean QALYs* |
ICER** | Probability of Cost Effectiveness at $25,000/QALY |
Probability of Cost Effectiveness at $50,000/QALY |
Probability of Cost Effectiveness at $100,000/QALY |
|
|---|---|---|---|---|---|---|---|
| 3- year |
IH-CBT | $4,588 | 2.10 | Dominant | 99.5% | 99.7% | 99.9% |
| SHV | $4,590 | 2.03 | |||||
| Difference | −$2 | 0.07 | |||||
| 1- year |
IH-CBT | $2,393 | 0.83 | $9,862 | 93.6% | 99.1% | 99.7% |
| SHV | $2,010 | 0.79 | |||||
| Difference | $929 | 0.04 | |||||
| 5- year |
IH-CBT | $6,882 | 3.35 | Dominant | 99.7% | 99.7% | 99.7% |
| SHV | $6,963 | 3.28 | |||||
| Difference | −$81 | 0.07 |
IH-CBT – In-Home Cognitive Behavioral Therapy; SHV – Standard Home Visiting
Difference was calculated as IH-CBT minus SHV
Dominant implies that the strategy decreases costs and increases QALYs
QALY is quality-adjusted life year
ICER is incremental cost-effectiveness ratio
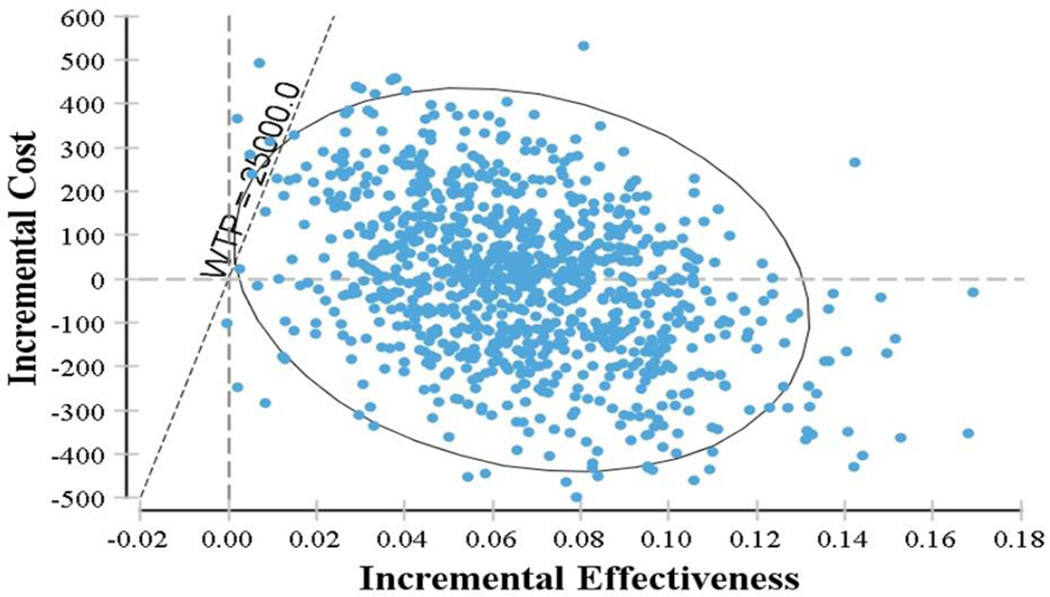
Probabilistic sensitivity analysis was performed using a Monte Carlo simulation. The parameter values were randomly chosen based on their range and distribution for 1,000 model iterations. IH-CBT was found to be a dominant strategy in 49% of the model iterations. Approximately 95% of the model iterations reported an ICER of less than US$10,000/QALY for the IH-CBT treatment strategy. Figure 2 is a plot of the incremental cost and effectiveness result for each model iteration. Based on a willingness-to-pay threshold of US$25,000/QALY, over 99% of the model iterations demonstrated IH-CBT to be a cost-effective strategy compared to SHV.
Fig. 2.
Plot of incremental cost-effectiveness, IH-CBT vs. SHV. This figure reports the incremental costs and effectiveness of each model iteration as a point on the graph. The incremental cost (x-axis) is the difference in costs incurred between IH-CBT and SHV treatment cohorts. The incremental effectiveness (y-axis) is the difference in QALYs achieved between IH-CBT and SHV treatment cohorts. A $25,000 willingness-to-pay (WTP) threshold limit line is plotted to illustrate the number of model iterations above this threshold. The ellipse represents 95% of all model iterations.
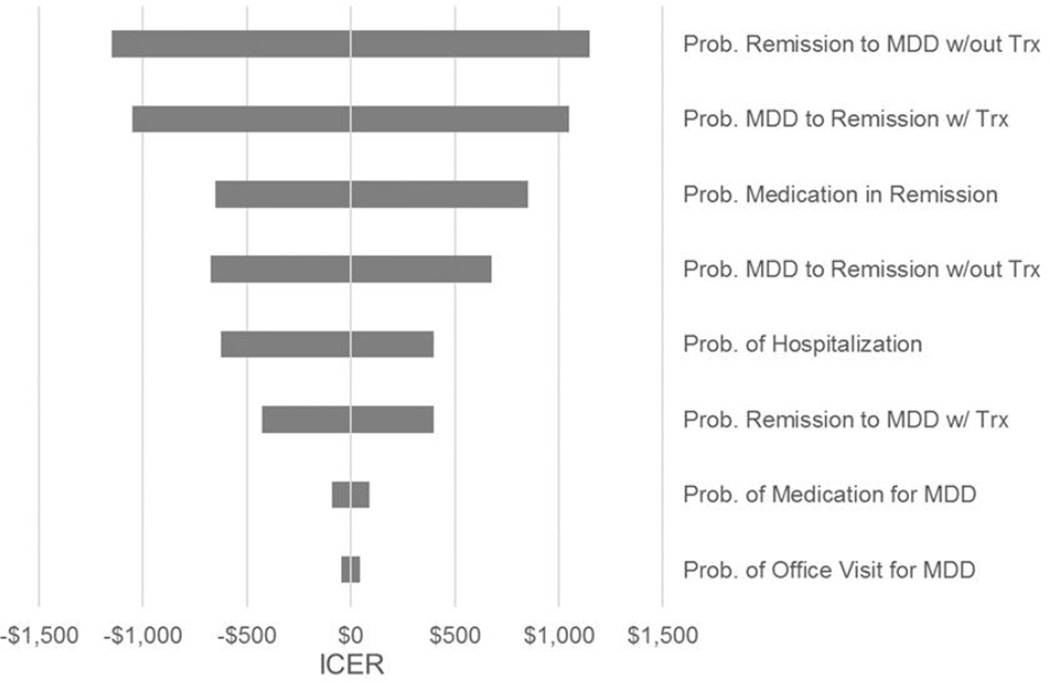
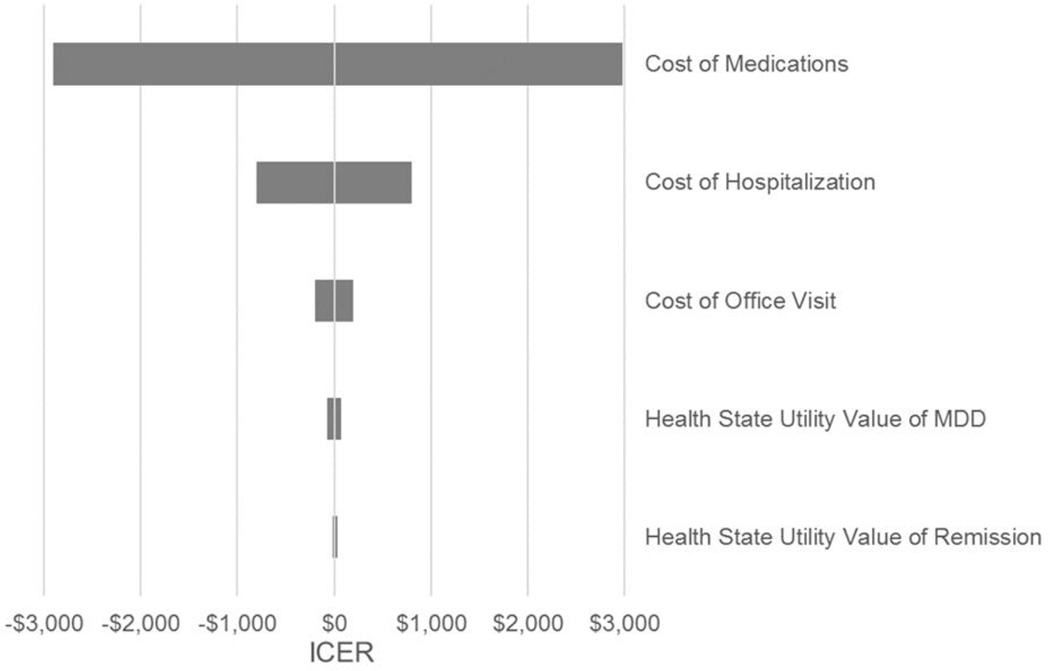
One-way sensitivity analysis was performed for key model parameters. Figure 3a summarizes the results for transition probabilities and healthcare utilization. Figure 3b summarizes the results for costs and health state utilities. As the figures reveal, IH-CBT remains a cost-effective strategy compared to SHV. The results were most sensitive to the following parameters: transition from remission to MDD, transition from MDD to remission, cost of MDD medications. However, the ICER for all of the parameters analyzed remained well below US$5,000. This finding indicated that despite uncertainty in the transition probabilities post treatment intervention, IH-CBT was expected to remain a highly cost-effective treatment.
Fig. 3.
a One-way sensitivity analysis tornado diagram for health state transition probabilities and frequency of healthcare utilization. The tornado diagram ranks the parameters listed on the right in order of influence on the incremental cost-effectiveness ratio (ICER). Each parameter was adjusted to the low value and high value and the ICER was calculated. The shaded bars represent the expected ICER range for the indicated parameter. The x-axis reports the expected ICER. b One-way sensitivity analysis tornado diagram for costs and health state utility values. The tornado diagram ranks the parameters listed on the right in order of influence on the incremental cost-effectiveness ratio (ICER). Each parameter was adjusted to the low value and high value and the ICER was calculated. The shaded bars represent the expected ICER range for the indicated parameter. The x-axis reports the expected ICER value.
The model was compared against the results of the clinical trial reported by Ammerman et al. (2013). The model matches the MDD reduction in the IH-CBT and SHV interventions. The model was also compared to the reported MDD diagnosis rate at the treatment follow-up period. The model results with respect to the diagnosis of MDD were within the reported standard deviation of the clinical study for both intervention strategies. The differences in MDD diagnosis rates were attributed to using the published literature to determine the transition probabilities post treatment intervention and the one-month difference between the follow-up period and the second cycle of the model. These differences were modest, indicating that the model calibrated well with the original clinical trial results.
4. Discussion
This study examined the cost-effectiveness of IH-CBT, an adapted version of CBT specifically designed for low-income mothers participating in home visiting programs. Results indicated that IH-CBT was cost-effective relative to SHV and antidepressant medications. Specifically, IH-CBT was expected to be cost-effective at a three-year time horizon 99.5%, 99.7%, and 99.9% of the time for willingness-to-pay thresholds of US$25,000, US$50,000, and US$100,000, respectively. At the three-year time horizon, IH-CBT was found to improve QALYs by one month. These patterns were upheld at one-year and five-year time horizons. Thus, even with lower willingness-to-pay thresholds, IH-CBT emerges as a cost-effective program from the perspective of payers. Probabilistic sensitivity analyses confirmed the robustness of findings and the stability of the ICER values. Taken together, these findings indicate that IH-CBT is a more cost-effective treatment for low-income, depressed mothers than current standards of practice. It is noteworthy that the added expense of home visiting did not offset the favorability of IH-CBT in these analyses.
The cost-effectiveness of IH-CBT was driven by the reduction in expected depression days resulting from treatment, nearly 346 days over the three-year time horizon. This was associated with decreased costs in medical care. Although home visiting by itself has limited impact on maternal depressive symptoms (Green et al., 2014), we have argued that the strong collaborative relationship between IH-CBT therapists and home visitors contributes to improved outcomes in depression (Ammerman et al., 2012). It is possible that this synergy in services is also a driver of improved cost-effectiveness. There are a number of additional human and financial costs (Goodman et al., 2011) associated with depression, including compromised maternal life course (lower educational achievement, unemployment) and poor child developmental outcomes (increased risk for psychiatric disorder, academic underachievement, use of special education services). These were not examined in our analyses, and future studies should seek to incorporate these into a broader examination of the potential cost-effectiveness and cost savings of IH-CBT and other treatments for depression in mothers.
Findings from this study add to the growing literature demonstrating the value of depression treatments specifically focused on the needs of low-income mothers. Beil et al. (2013) reported on a cost-effectiveness study interpersonal psychotherapy (IPT) administered to mothers in Early Head Start. They, too, found IPT to have favorable cost-effectiveness results. Our findings also add to the larger literature demonstrating the cost-effectiveness of CBT to adult depression in general (Barret et al., 2005; Brettschneider et al., 2014; Wiles et al., 2016). For example, in a systematic review of 22 studies of CBT in varied formats with different populations, Brettschnieder et al. concluded that most studies demonstrated acceptable incremental cost-utility ratios of <$50,000. Our findings compare very favorably with this willingness-to-pay threshold.
IH-CBT seeks to identify mothers with depression during their participation in early childhood prevention programs, provide effective treatment in the home setting to reduce barriers to obtaining care, and leverage ongoing home visiting to optimize outcomes. This novel delivery system is economically sustainable from a payer perspective given its cost-effectiveness, and adds further support for the cost utility of impactful depression treatments that are implemented in a focused and deliberate manner (Wang et al., 2006). Although many low-income mothers do not participate in home visiting programs, most receive some kind of social service support from other programs and organizations. Findings from this study suggest that using these settings to reach, screen, engage, and treat depressed mothers is a promising approach to make effective treatment more widely available and accessible.
The timeliness of this study is underscored by the increasing urgency to identify and effectively treat depressed mothers. The costs of maternal depression, to mothers and children, is staggering (Ammerman et al., 2016; Dagher et al., 2012). Recent research has confirmed the long-term deleterious outcomes of children exposed to maternal depression, particularly in the first years of life (Bagner et al., 2010). These consequences are amplified among mothers and children living in poverty (Heberle and Carter, 2015). Early identification and treatment of depressed mothers is an essential public health priority (Bauer et al., 2014). In the USA, the Affordable Care Act provides guidance and incentives to implement innovative outreach and treatment approaches, of which IH-CBT is a compelling option.
Future research should extend and expand our understanding of the economic utility of IH-CBT in particular, and treatments for low-income, depressed mothers in general. As noted, it is desirable to consider the multigenerational costs associated with maternal depression by incorporating child outcomes. Longer follow-up of depressed mothers receiving IH-CBT would provide a more precise documentation of risk for relapse and course of depression. The cost-effectiveness of different delivery strategies is also of interest. Shorter treatment duration, service delivery through the internet or other electronic sources, or use of different levels of training of care providers might yield lower cost but equally effective interventions. Establishing the clinical efficacy of treatments for depression is a well-recognized essential step, but in a service environment in which resources are limited it is also important that cost-effectiveness be considered (Byford and Bower, 2002).
4.1 Study limitations
This study has some important limitations that must be noted. First, the study results are based on a clinical study that enrolled a relatively small number of mothers all located in the same region. As such, the results may not be generalizable to other home visiting programs due to different program methods and/or geographical considerations. Second, while the model attempted to capture key features of treatments and costs encountered in managing these mothers, some simplifying assumptions had to be made, both to render the analysis manageable and in recognition of data limitations. For example, mothers were assumed to have a constant transition probability from remission to MDD regardless of how many times they relapsed. Third, the clinical study of the model had a limited window of follow-up to assess the duration of the treatment strategies. The transition probabilities after the initial treatment were obtained from the published literature. Therefore, they do not reflect the actual transition probabilities for the mothers in the clinical study. Thus, we had to make assumptions about these long-term effects and rely on sensitivity analysis to gauge the robustness of our findings. Future clinical studies should use a longer follow-up period to more precisely estimate these parameters.
4.2 Conclusion
Cost-effectiveness analyses are valuable in making decisions about which treatments to pay for when resources are limited. Low-income, depressed mothers are a high-risk patient population that incur significant costs to payers, health care providers, and employers (Ammerman et al., 2016). IH-CBT was developed to provide effective treatment to depressed mothers in home visiting programs, a population affected by poverty and adversity. Results from this study indicate that, in addition to its demonstrated clinical impact, IH-CBT is economically sound option for payers and warrants further dissemination and implementation.
Highlights.
We determine the cost-effectiveness of In-Home Cognitive Behavioral Therapy for low-income, depressed mothers enrolled in an early childhood prevention program
We use data from a the nationally-representative Medical Expenditure Panel Survey and the literature to determine standard of care costs
IH-CBT was a dominant strategy and expected to be cost-effective at a three-year time horizon 99.5%, 99.7%, and 99.9% of the time for willingness-to-pay thresholds of US$25,000, US$50,000, and US$100,000, respectively
Over the three-year time horizon, mothers receiving IH-CBT were expected to have 345.6 fewer days of depression relative to those receiving standard home visiting and treatment in the community
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Agency for Healthcare Research and Quality. [accessed 03.07.16];Medical Expenditure Panel Survey (MEPS) 2015 http://www.ahrq.gov/research/data/meps/index.html.
- Ammerman RT, Putnam FW, Bosse NR, Teeters AR, Van Ginkel JB. Maternal depression in home visitation: A systematic review. Aggress. Violent Beh. 2010;15:191–200. doi: 10.1016/j.avb.2009.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammerman RT, Putnam FW, Stevens J, Bosse NR, Short JA, Bodley AL, Van Ginkel JB. An open trial of In-Home CBT for depressed mothers in home visitation. Matern. Child Hlth. J. 2011;15:1333–1341. doi: 10.1007/s10995-010-0691-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammerman RT, Peugh JL, Putnam FW, Van Ginkel JB. Predictors of treatment response in depressed mothers receiving in-home cognitive-behavioral therapy and concurrent home visiting. Behav. Modif. 2012;36:462–481. doi: 10.1177/0145445512447120. [DOI] [PubMed] [Google Scholar]
- Ammerman RT, Putnam GW, Altaye M, Stevens J, Teeters AR, Van Ginkel JB. A clinical trial of In-Home CBT for depressed mothers in home visitation. Behav. Ther. 2013;44:359–372. doi: 10.1016/j.beth.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammerman RT, Altaye M, Putnam FW, Teeters AR, Zou Y, Van Ginkel JB. Depression improvement and parenting in low-income mothers in home visiting. Arch. Women. Ment. Hlth. 2014;18:555–563. doi: 10.1007/s00737-014-0479-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammerman RT. Toward the next generation of home visiting programs: New developments and promising directions. Curr. Probl. Pediatr. Adolesc. Health Care. Advanced online publication. 2016 doi: 10.1016/j.cppeds.2015.12.010. [DOI] [PubMed] [Google Scholar]
- Ammerman RT, Chen J, Mallow PJ, Rizzo JA, Folger AT, Van Ginkel JB. Annual direct health care expenditures and employee absenteeism costs in high-risk, low-income mothers with major depression. J. Affect. Disorders. 2016;190:386–394. doi: 10.1016/j.jad.2015.10.025. [DOI] [PubMed] [Google Scholar]
- Bagner DM, Pettit JW, Lewinsohn PM, Seeley JR. Effect of maternal depression on child behavior: A sensitive period? J. Am. Acad. Child Adolesc. Psychiat. 2010;49:699–707. doi: 10.1016/j.jaac.2010.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banti S, Mauri M, Oppo A, Borri C, Rambelli C, Ramacciotti D, Montagnani MS, Camilleri V, Cortopassi S, Rucci P, Cassano GB. From the third month of pregnancy to 1 year postpartum. Prevalence, incidence, recurrence, and new onset of depression. Results from the perinatal depression-research & screening unit study. Compr. Psychiat. 2011;52:343–351. doi: 10.1016/j.comppsych.2010.08.003. [DOI] [PubMed] [Google Scholar]
- Barrett B, Byford S, Knapp M. Evidence of cost-effective treatments for depression: A systematic review. J. Affect. Disorders. 2005;84:1–13. doi: 10.1016/j.jad.2004.10.003. [DOI] [PubMed] [Google Scholar]
- Bauer A, Pawlby S, Plant DT, King D, Pariante CM, Knapp M. Perinatal depression and child development: exploring the economic consequences from a South London cohort. Psychol. Med. 2014;45:51–61. doi: 10.1017/S0033291714001044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beil H, Beeber LS, Schwartz TA, Lewis G. Cost-effectiveness of alternative treatments for depression in low-income women. J. Ment. Health Policy. 2013;16:55–65. [PubMed] [Google Scholar]
- Brettschneider C, Djadran H, Härter M, Löwe B, Riedel-Heller S, König H-H. Cost-utility analyses of cognitive-behavioural therapy of depression: A systematic review. Psychother. Psychosom. 2014;84:6–21. doi: 10.1159/000365150. [DOI] [PubMed] [Google Scholar]
- Bull SA, Hu XH, Hunkeler EM, Lee JY, Ming EE, Markson LE, Fireman B. Discontinuation of use and switching of antidepressants. J. Amer. Med. Assoc. 2002;288:1403–1409. doi: 10.1001/jama.288.11.1403. [DOI] [PubMed] [Google Scholar]
- Byford S, Bower P. Cost-effectiveness of cognitive-behavioral therapy for depression: Current evidence and future research priorities. Exp. Rev. Pharmacoecon. Outcomes Res. 2002;2:89–97. doi: 10.1586/14737167.2.5.457. [DOI] [PubMed] [Google Scholar]
- Campbell SB, Morgan-Lopez AA, Cox MJ, McLoyd VC. A latent class analysis of maternal depressive symptoms over 12 years and offspring adjustment in adolescence. J. Abnorm. Psychol. 2009;118:479–493. doi: 10.1037/a0015923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Consumer Reports. [accessed 08.10.14];Best buy drugs: Using antidepressants to treat depression. 2013 http://www.consumerreports.org/health/resources/pdf/best-buy-drugs/Antidepressants_update.pdf.
- Coryell W, Young EA. Clinical predictors of suicide in primary major depressive disorder. J. Clin. Psychiat. 2005;66:412–417. doi: 10.4088/jcp.v66n0401. [DOI] [PubMed] [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Brit. J. Psychiat. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Dagher RK, McGovern PM, Dowd BE, Gjerdingen DK. Postpartum depression and health services expenditures among employed women. J. Occup. Environ. Med. 2012;54:210–215. doi: 10.1097/JOM.0b013e31823fdf85. [DOI] [PubMed] [Google Scholar]
- Dennis CL. Psychosocial and psychological interventions for prevention of postnatal depression: Systemic review. BMJ. 2005;331:15. doi: 10.1136/bmj.331.7507.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunner DL, Blier P, Keller MB, Pollack MH, Thase ME, Zajecka JM. Preventing recurrent depression: Long-term treatment for major depressive disorder. J. Clin. Psychiat. 2007;9:214–221. [PubMed] [Google Scholar]
- Engle PL, Black MM, Behrman JR, Cabral de Mello M, Gertler PJ, Kapiriri L, Martorell R, Young ME. Strategies to avoid the loss of developmental potential in more than 200 million children in the developing world. Lancet. 2007;369:229–242. doi: 10.1016/S0140-6736(07)60112-3. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: a meta-analytic review. Clin. Child Fam. Psych. 2011;14:1–27. doi: 10.1007/s10567-010-0080-1. [DOI] [PubMed] [Google Scholar]
- Goyal D, Gay C, Lee KA. How much does low socioeconomic status increase the risk of prenatal and postpartum depressive symptoms in first-time mothers? Women Health Iss. 2010;20:96–104. doi: 10.1016/j.whi.2009.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green BL, Tarte JM, Harrison PM, Nygren M, Sanders MB. Results from a randomized trial of the healthy families Oregon accredited statewide program: Early program impacts on parenting. Child. Youth Serv. Rev. 2014;44:288–298. [Google Scholar]
- Greenberg PE, Kessler RC, Birnbaum HG, Leong SA, Lowe SW, Berglund PA, Corey-Lisle PK. The economic burden of depression in the United States: how did it change between 1990 and 2000? J. Clin. Psychiat. 2003;64:1465–1475. doi: 10.4088/jcp.v64n1211. [DOI] [PubMed] [Google Scholar]
- Gross D. Implications of maternal depression for the development of young children. Image: J. Nurs. Scholarship. 1989;21:103–107. doi: 10.1111/j.1547-5069.1989.tb00108.x. [DOI] [PubMed] [Google Scholar]
- Hansen NB, Lambert MJ, Forman EM. The psychotherapy dose-response effect and its implications for treatment delivery services. Clin. Psychol.-Sci. Pr. 2002;9:329–343. [Google Scholar]
- Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: Results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch. Gen. Psychiat. 2005;62:1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- Heberle AE, Carter AS. Cognitive aspects of young children’s experience of economic disadvantage. Psychol. Bull. 2015;141:723–746. doi: 10.1037/bul0000010. [DOI] [PubMed] [Google Scholar]
- Hill SR. Cost-effectiveness analysis for clinicians. BMC Med. 2012;10:10. doi: 10.1186/1741-7015-10-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holma KM, Melartin TK, Haukka J, Holma IA, Sokero TP, Isometsä ET. Incidence and predictors of suicide attempts in DSM-IV major depressive disorder: A five-year prospective study. Am. J. Psychiat. 2010;167:801–808. doi: 10.1176/appi.ajp.2010.09050627. [DOI] [PubMed] [Google Scholar]
- Holton JK, Harding K. Healthy Families America: Ruminations on implementing a home visitation program to prevent child maltreatment. J. Prev. Interv. Community. 2007;34:13–38. doi: 10.1300/J005v34n01_02. [DOI] [PubMed] [Google Scholar]
- Jarde A, Morais M, Kingston D, Giallo R, MacQueen GM, Giglia L, Beyene J, Wang Y, McDonald SD. Neonatal outcomes in women with untreated antenatal depression compared with women without depression: A systematic review and meta-analysis. J. Amer. Med. Assoc. Psychiat. Advanced online publication. 2016 doi: 10.1001/jamapsychiatry.2016.0934. [DOI] [PubMed] [Google Scholar]
- Löthgren M. Economic evidence in affective disorders: A review. Eur. J. Health Econ. 2004;5:s12–s20. doi: 10.1007/s10198-005-0283-4. [DOI] [PubMed] [Google Scholar]
- Miranda J, Green BL, Krupnick JL, Chung J, Siddique J, Belin T, Revicki D. One-year outcomes of a randomized clinical trial treating depression in low-income minority women. J. Consult. Clin. Psych. 2006;74:99–111. doi: 10.1037/0022-006X.74.1.99. [DOI] [PubMed] [Google Scholar]
- O’Connor E, Rossom RC, Henninger M, Groom HC, Burda BU. Primary care screening for and treatment of depression in pregnant and postpartum women: Evidence report and systematic review for the US Preventive Services Task Force. J. Amer. Med. Assoc. 2016;315:388–406. doi: 10.1001/jama.2015.18948. [DOI] [PubMed] [Google Scholar]
- O’Hara MW, Wisner KL. Perinatal mental illness: definition, description and aetiology. Best Pract. Res. Cl. OB. 2014;28:3–12. doi: 10.1016/j.bpobgyn.2013.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohio Department of Medicaid. [accessed 09.10.14];Appendix DD to rule 5160-1-60. 2014 http://medicaid.ohio.gov/Portals/0/Providers/FeeScheduleRates/App-DD.pdf.
- Olds DL. The Nurse-Family Partnership: From trials to practice. In: Reynolds AJ, Rolnick AJ, Englund MM, Temple JA, editors. Childhood Programs and Practices in the First Decade of Life: A Human Capital Integration. New York: Cambridge University Press; 2010. pp. 49–75. [Google Scholar]
- Piek E, Kollen BJ, van der Meer K, Penninx BW, Nolen WA. Maintenance use of antidepressants in Dutch general practice: Non-guideline concordant. PLoS ONE. 2014;9:1–8. doi: 10.1371/journal.pone.0097463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts M, Russell LB, Paltiel AD, Chambers M, McEwan P, Krahn M ISPOR-SMDM Modeling Good Research Practices Task Force. Conceptualizing a model: A report of the ISPOR-SMDM modeling good research practices task force–2. Val. Health. 2012;15:804–811. doi: 10.1016/j.jval.2012.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siebert U, Alagoz O, Bayoumi AM, Jahn B, Owens DK, Cohen DJ, Kuntz KM ISPOR-SMDM Modeling Good Research Practices Task Force. State-transition modeling: A report of the ISPOR-SMDM modeling good research practices task force-3. Val. Health. 2012;15:812–820. doi: 10.1016/j.jval.2012.06.014. [DOI] [PubMed] [Google Scholar]
- Smith JP, Smith GC. Long-term economic costs of psychological problems during childhood. Soc. Sci. Med. 2010;71:110–115. doi: 10.1016/j.socscimed.2010.02.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stensland M, Watson PR, Grazier KL. An examination of costs, charges, and payments for inpatient psychiatric treatment in community hospitals. Psychiat. Serv. 2012;63:666–671. doi: 10.1176/appi.ps.201100402. [DOI] [PubMed] [Google Scholar]
- Teeters AR, Ammerman RT, Shenk CE, Goyal NK, Folger AT, Putnam FW, Van Ginkel JB. Trajectories in maternal depressive symptoms in home visiting. Am. J. Orthopsychiat. Advanced online publication. 2016 doi: 10.1037/ort0000159. [DOI] [PubMed] [Google Scholar]
- ten Doesschate MC, Bockting CLH, Schene AH. Adherence to continuation and maintenance antidepressant use in recurrent depression. J. Affect. Disorders. 2009;115:167–170. doi: 10.1016/j.jad.2008.07.011. [DOI] [PubMed] [Google Scholar]
- TreeAge Software, Inc. [accessed 18.12.14]; https://www.treeage.com.
- United States Social Security Administration. [accessed 15.10.14];Actuarial Life Table 2010. 2010 https://www.ssa.gov/oact/STATS/table4c6.html.
- Wang PS, Patrick A, Avorn J, Azocar F, Ludman E, McCulloch J, Simon G, Kessler R. The costs and benefits of enhanced depression care to employers. Arch. Gen. Psychiat. 2006;63:1345–1353. doi: 10.1001/archpsyc.63.12.1345. [DOI] [PubMed] [Google Scholar]
- Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, Charlson FJ, Norman RE, Flaxman AD, Johns N, Burstein R, Murray CJL, Vos T. Global burden of disease attributable to mental and substance use disorders: Findings from the Global Burden of Disease Study 2010. Lancet. 2013;382:1575–1586. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- Wisner KL, Sit DK, McShea MC, Rizzo DM, Zoretich RA, Hughes CL, Eng HF, Luther JF, Wisniewski SR, Costantino ML, Confer AL, Moses-Kolko EL, Famy CS, Hanusa BH. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. J. Amer. Med. Assoc. Psychiat. 2013;70:490–498. doi: 10.1001/jamapsychiatry.2013.87. [DOI] [PMC free article] [PubMed] [Google Scholar]