Abstract
Objective
To examine the extent to which poor sleep quality is associated with suicidal ideation among Ethiopian adults.
Methods
A cross-sectional study was conducted among 1,054 adults attending outpatient clinical facilities in Ethiopia. Standardized questionnaires were utilized to collect data on demographics, sleep quality, lifestyle, and depression status. Depression and suicidal ideation were assessed using the Patient Health Questionnaire-9 (PHQ-9), while the Pittsburgh Sleep Quality Index (PSQI) questionnaire was utilized to assess sleep quality. Multivariate logistic regression models were fit to estimate adjusted odds ratio (AOR) and 95% confidence intervals (95%CI).
Results
The prevalence of suicidal ideation was 24.3% while poor sleep quality (PSQI global score of > 5vs. ≤5) was endorsed by 60.2% of participants. After adjustment for confounders including depression, poor sleep quality was associated with more than 3-fold increased odds of suicidal ideation (AOR=3.46; 95%CI 2.27–5.26). When assessed as a continuous variable, each 1-unit increase in the global PSQI score resulted in a 20% increased odds for suicidal ideation, even after adjusting for depression (AOR=1.20; 95%CI 1.14–1.27). Participants with both poor sleep quality and depression had much higher odds (AOR=24.9, 95% CI 15.2–40.8) of suicidal ideation as compared with those who had good sleep quality and no depression although inferences from this analysis are limited due to the wide 95%CI.
Conclusion
Suicidal ideation and poor sleep quality are highly prevalent. Individuals with poor sleep quality have higher odds of suicidal ideation. If confirmed, mental health services need to address sleep disturbances seriously to prevent suicidal episodes.
Keywords: sleep quality, suicidal ideation, suicide, Ethiopia, Africa
Introduction
Suicide, a preventable public health problem and global disease burden, accounts for almost 1 million deaths annually and 57% of all violent deaths [1]. Approximately one life is lost every 40 seconds from suicide [2]. Globally, about 800,000 people die each year due to suicide; while 75% of global suicides occur in low- and middle-income countries (LAMICs). Suicide is one of the leading causes of death in LAMICs with profound personal, societal, and economic consequences [3]. Suicidal ideation is a harbinger of suicidal attempts and completed suicide [4].
Sleep disorders, affecting more than 45% of the world’s population, have emerged as important global public health problems [5]. Individuals experiencing sleep disorders have increased risks of chronic diseases such as cancer, hypertension, diabetes, and cognitive impairment, obesity, as well as increased all-cause mortality, [6–10]. Accumulating evidences show that sleep disorders have shared pathophysiologic mechanisms with many psychiatric disorders [11–14]. Sleep disorders such as insomnia, nightmares, and poor sleep quality symptoms may present elevated risks for suicidal ideation, suicide attempts, and death by suicide [12, 15]. However the geographical scope of evidences is limited, with the majority of researches being conducted in higher income countries, and disproportionately little evidence coming from LAMICs [14]. Recent studies conducted in Ethiopia have documented high prevalence estimates of poor sleep quality [5], [11] in adult populations similar to those reported in other occidental countries. To the best of our knowledge, however, no study has evaluated the link between sleep quality and suicidal ideation among Ethiopians or other sub-Saharan African adults. We therefore conducted this cross sectional study to evaluate the extent to which poor sleep quality is associated with suicidal ideation in Ethiopian adults.
Methods
This study consisted of 1,060 participants who attended the Saint Paul General Hospital outpatient facility in Addis Ababa, Ethiopia that provides all major specialized medical services. For this study, participants eligible for inclusion came from the internal medicine, general surgery, and gynecological outpatient departments. Data were collected between July and December 2011. Data were collected by research nurses who participated in a four-day training session that included training modules on the contents of the questionnaire, ethical conduct of research involving human subjects, and appropriate data collection techniques. Structured in-person interviews were used to collect information regarding demographics, sleep disturbances, and behavioral and lifestyle characteristics. The questionnaire was first written in English, then translated by linguistic experts into Amharic, which was then back translated into English. Research nurses approached and invited eligible patients to participate in the study. Interviews were conducted after completing the informed consent process. All study participants provided informed consent and the research protocol was approved by the Institutional Review Boards of Addis Continental Institute of Public Health, Addis Ababa, Ethiopia and the Human Subjects Division at the University of Washington, Seattle, USA.
Pittsburgh Sleep Quality Index (PSQI)
The PSQI is a self-rated questionnaire that assesses sleep quality and disturbances in the last 1-month preceding the interview [16]. The PSQI instrument has been widely used globally including in Ethiopia.[17] The PSQI consists of seven sleep components related to sleep habits including duration of sleep, sleep disturbance, sleep latency, habitual sleep efficiency, use of sleep medicine, daytime dysfunction and overall sleep quality [16]. The score for each sleep component ranges from 0 to 3, with 3 indicating the greatest dysfunctionality. The sum of scores for all seven components yields one global score ranging from 0 to 21, a higher global score indicating poor sleep quality. Participants with a global score greater than 5 were classified as having poor sleep quality. Those with a score of 5 or less were classified as having good sleep quality.
Major Depressive Disorder
The Patient Health Questionnaire-9 (PHQ-9) is a brief 9-item questionnaire designed to detect major depressive disorder according to the criteria from the Diagnostic and Statistical Manual for Mental Disorders (DSM-IV) [18]. The PHQ-9 has been previously validated in Ethiopia [19]. The score of each item ranges from 0 to 3, with 3 indicating most distress. The sum of all 9 items yields one overall score ranging from 0–27, a higher total score indicating depression. Those with a score of 9 or less were classified as not depressed. A meta-analysis of 14 studies support the use of a PHQ-9 score of ≥10 to classify subjects with major depressive disorder. [20] In the present study we utilized only the first 8 questions to calculate an overall depression score as the PHQ-8. Question number 9 that asks about suicidal ideation was not considered in the total score for depression. Participants with a total PHQ-8 score of 10 or greater were considered depressed.
Suicidal Ideation
Suicidal ideation was assessed on the basis of participants’ responses to item 9 of the PHQ-9; “thoughts that you would be better off dead, or of hurting yourself” in the 14 days prior to evaluation. If the response was “several days,” “more than half the days,” or “nearly every day,” suicidal ideation was coded as “yes.” Participants responding “not at all” were classified as “no” for suicidal ideation.
Covariates
Questions were also included regarding behavioral risk factors such as tobacco, alcohol, and khat consumption. Khat is an evergreen plant with amphetamine-like effects commonly used as a mild stimulant for social recreation and to improve work performance in Ethiopia [21, 22]. Participants were classified according to their alcohol consumption in the past year into; no alcoholic beverage, <1 alcoholic beverage a week, and ≥ 1 alcoholic beverages a week. Other variables were categorized as follows: age (years), sex (male, female), education (≤ primary (1–6), secondary (7–12), college graduate), smoking status (never, former, current), and khat consumption (none, former, current).
Statistical Analysis
Demographic and lifestyle characteristics of study participants were assessed using means (± standard deviation) for continuous variables and counts and percentages for categorical variables. Differences in categorical variables were evaluated using Chi-square test. For continuous variables Student’s t-tests were used to evaluate differences in mean values according to participants’ suicide ideation status (yes vs. no). Unadjusted, age and sex-adjusted, and multivariable models, were fit to estimate odd ratios (ORs) and 95% confidence intervals (95%CI) to assess the associations between sleep quality and suicidal ideation. Multivariable-adjusted logistic regression models controlled for age, sex, education, cigarette smoking, alcohol and khat consumption. Multivariate models were further adjusted for depression. We assessed the odds of suicidal ideation across tertiles of global PSQI score where tertiles were defined on the basis of the distribution of the scores for the entire cohort. We evaluated linear trends in the odds of suicidal ideation by treating the three tertiles as a continuous variable after assigning a score (i.e., 1, 2, 3) for successively higher tertiles. Further, to assess the joint and independent effects of poor sleep quality and depression on the odds of suicidal ideation, we grouped participants into four categories as follows: (1) good sleep quality and no depression, (2) poor sleep quality, no depression, (3) good sleep quality, depression, and (4) poor sleep quality and depression combined. Those with good sleep quality and no depression comprised the reference group, against which participants in each of the other three categories were compared. In multivariable analyses, we evaluated linear trend in odds of suicidal ideation by treating PSQI global score as a continuous variable. We also explored the possibility of a nonlinear relation between PSQI global score and odds of suicidal ideation using the generalized additive modeling (GAM) procedure; with a cubic spline function [23]. All analyses were performed using SPSS Version 22.0 (IBM SPSS Version 22, Chicago, IL). The GAM analyses were performed using “R” software version 3.1.2. All reported confidence intervals were calculated at the 95% level. All reported p-values are two-tailed and deemed statistically significant at α=0.05.
Results
Our study consisted of 1,054 participants. The majority of participants were women (60%), married (51%), and 78.4% had fewer than 12 years of formal education. Cigarette smoking was reported by 10% of participants, while 34% of participants reported consuming alcohol at least once a month. Approximately 60% of participants endorsed having poor sleep quality while 27% of participants reported suicidal ideation (Table 1).
Table 1.
Characteristics of the Study Population (N=1,060)
| Characteristic | All participants (N=1,060) | Suicidal Ideation
|
P valuec | ||||
|---|---|---|---|---|---|---|---|
| No (N = 829) | Yes (N = 261) | ||||||
|
| |||||||
| n | % | n | % | n | % | ||
| Mean age (years)a | 35.7±12.1 | 36.3±11.9 | 33.8 ± 12.7 | <0.001 | |||
| Sex | |||||||
| Women | 637 | 60.4 | 466 | 58.4 | 171 | 68.8 | 0.017 |
| Men | 417 | 39.6 | 332 | 41.6 | 85 | 33.2 | |
| Marital status | |||||||
| Married | 540 | 51.4 | 423 | 53.2 | 117 | 45.7 | 0.048 |
| Never married | 331 | 31.5 | 247 | 31.1 | 84 | 32.8 | |
| Otherb | 180 | 17.1 | 125 | 157 | 55 | 21.5 | |
| Education (years) | |||||||
| ≤ Primary (1–6) | 473 | 44.9 | 326 | 40.8 | 147 | 57.4 | <0.001 |
| Secondary (7–12) | 354 | 33.6 | 276 | 34.6 | 78 | 30.5 | |
| College graduate | 227 | 21.5 | 196 | 24.6 | 31 | 12.1 | |
| Smoking status | |||||||
| Never | 910 | 86.3 | 695 | 87.1 | 215 | 83.9 | 0.194 |
| Former | 102 | 9.7 | 76 | 9.5 | 26 | 10.2 | |
| Current | 42 | 4.0 | 27 | 3.4 | 15 | 5.9 | |
| Alcohol consumption past year | |||||||
| None | 599 | 56.8 | 446 | 55.9 | 153 | 59.8 | 0.552 |
| < once a month | 354 | 33.6 | 274 | 34.3 | 80 | 31.2 | |
| ≥ 1 day a week | 101 | 9.6 | 78 | 9.8 | 23 | 8.9 | |
| Khat consumption | |||||||
| None | 779 | 73.9 | 602 | 75.4 | 177 | 69.1 | 0.098 |
| Former | 58 | 5.5 | 39 | 4.9 | 19 | 7.4 | |
| Current | 217 | 20.6 | 157 | 19.7 | 60 | 23.4 | |
| Depressiond | |||||||
| No | 775 | 75.5 | 681 | 85.3 | 94 | 36.7 | <0.001 |
| Yes | 279 | 26.5 | 117 | 14.7 | 162 | 63.3 | |
Mean ± SD (standard deviation);
Other includes separated/divorced/widowed;
For continuous variables, P-value calculated using Wilcoxon Rank Sum Test; for categorical variables, P-value was calculated using Chi-square test;
Depression was defined as the Patient Health Questionnaire-8 score ≥ 10; Six participants were excluded due to missing information on PSQI and PHQ-9.
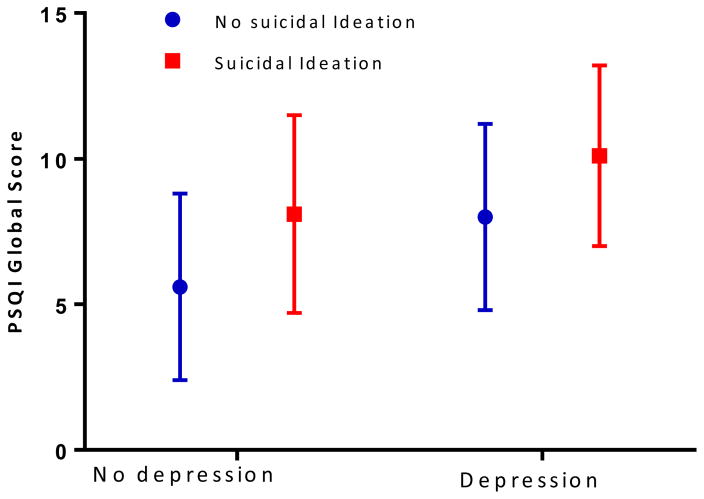
Depressed participants had higher mean PSQI global scores compared with non-depressed participants (Figure 1). As shown in Table 2, compared to those with good sleep quality (global PSQI score ≤ 5), participants with poor sleep quality (global PSQI score > 5) had more than 6-fold higher odds (OR=6.33; 95% CI 4.28–9.36) of suicidal ideation. The association remained essentially unchanged after adjusting for age, sex, education, cigarette smoking, alcohol and khat consumption (AOR=6.30; 95% CI 4.23–9.37). Further adjustment for depression, resulted in an attenuated association (AOR=3.46; 95% CI 2.27–5.26) (Table 2).
Figure 1. Self-reported Pittsburgh Sleep Quality Index (PSQI) Global Score according to Depression Status and Suicidal Ideation (N = 1054).
No depression was defined as the Patient Health Questionnare-8 (PHQ-8) score < 10; depression was defined as the PHQ- 8 score ≥ 10.
Table 2.
Model Statistic for Pittsburgh Sleep Quality Index (PSQI) Global Score Associated with Suicidal Ideation (N=1,054)
| PSQI global score | PHQ-9 Suicidal Ideation
|
Unadjusted a OR (95% CI) |
Adjusted b OR (95% CI) |
Adjusted c OR (95% CI) |
|||
|---|---|---|---|---|---|---|---|
| No (N = 829) | Yes (N = 261) | ||||||
|
| |||||||
| n | % | n | % | ||||
| Overall sleep quality | |||||||
| Good (PSQI global score ≤ 5) | 386 | 48.4 | 33 | 12.9 | Reference | Reference | Reference |
| Poor (PSQI global score > 5) | 412 | 51.6 | 223 | 87.1 | 6.33 (4.28–9.36) | 6.30 (4.23–9.37) | 3.59 (2.34–5.51) |
| PSQI global score | |||||||
| Lowest tertile (0–5) | 386 | 48.4 | 33 | 12.9 | Reference | Reference | Reference |
| Middle tertile (6–8) | 227 | 28.5 | 74 | 28.9 | 3.81 (2.45–5.95) | 3.81 (2.43–5.98) | 2.47 (1.71–4.41) |
| Highest tertile (≥ 9) | 185 | 23.2 | 149 | 58.2 | 9.42 (6.21–14.28) | 9.41 (6.14–14.40) | 4.66 (2.93–7.41) |
| P-value for trend | < 0.0001 | < 0.0001 | < 0.0001 | ||||
| PSQI global score (continuous) d | 6.1 ± 3.4 | 9.3 ± 3.4 | 1.32 (1.24–1.36) | 1.30 (1.24–1.37) | 1.20 (1.14–1.27) | ||
Abbreviations: OR, odds ratio; CI, confidence interval
Unadjusted model
Adjusted for age (years), sex, education, cigarette smoking, alcohol and khat consumption
Further adjusted for depression status (yes [PHQ-8 ≥ 10] vs. no [PHQ-8 < 10])
Mean ± SD (standard deviation)
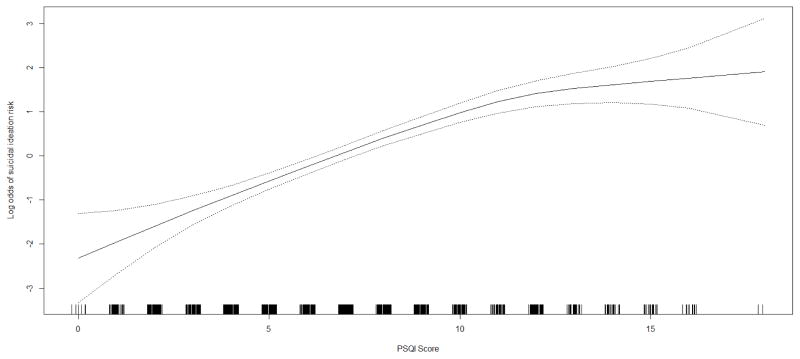
We next examined the odds of suicidal ideation according tertiles of global PSQI scores (Table 2). After adjusting for confounders including depression, the odds of suicidal ideation increased across increasing tertiles of global PSQI score (p for trend <0.001). Compared with those in the lowest PSQI global scores (PSQI global score <5), those with scores in the second tertile (PSQI global score=6–8) had a 2.5-fold increased odds of suicidal ideation (AOR=2.47; 95% CI 1.71–4.41). The odds of suicidal ideation was 4.7-fold higher for those with scores in the highest tertile (PSQI global score ≥9) (AOR=4.66; 95% CI 2.93–7.41) as compared with the referent group. When PSQI global score was modeled as a continuous variable, we noted that the odds of suicidal ideation increased by 20% for every 1-unit increase in the PSQI global score (AOR=1.20; 95% CI 1.14–1.27). The odds of suicidal ideation in relation to sleep quality expressed as a continuous variable using a generalized additive model (GAM), confirmed increasing odds of suicidal ideation with increasing global PSQI score (Figure 2)
Figure 2. Relation between Self-reported Pittsburgh Sleep Quality Index (PSQI) Global Score and Risk of Suicidal Ideation (solid line) with 95% Confidence Interval (dotted lines)a.
aVertical bars along PSQI axis indicate distribution of study subjects.
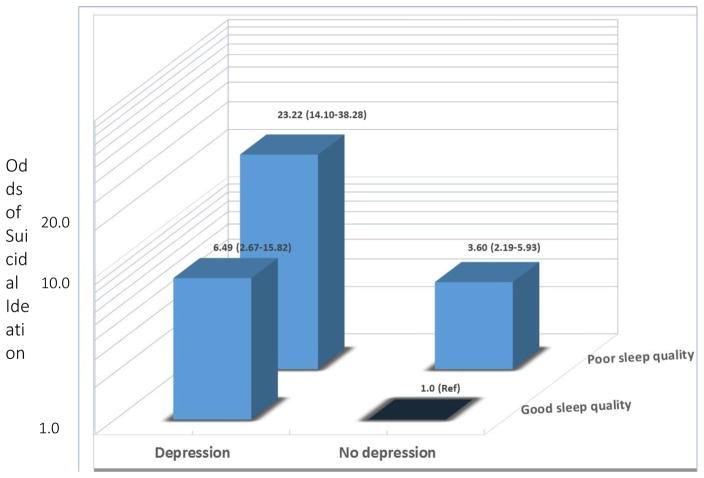
As shown in Figure 3, we observed some evidence of suggestive effect modification although the p-values for interaction terms were not significant. Individuals who were poor sleepers but who were not depressed had 7.96 fold increased odds (AOR = 7.96; 95% CI 3.34–18.96) of suicidal ideation as compared with those with individuals who had good sleep quality and who had no depression. Of note, individuals who were poor sleepers and who had depression had considerably elevated odds (AOR=24.9; 95% CI 15.2–40.8) of suicidal ideation as compared with the referent group. Inferences from these exploratory analyses, however, were limited by our relatively small sample size, as reflected by the wide 95% confidence intervals.
Figure 3. Associations between Sleep Quality, Depressive Symptoms, and Suicidal Ideation (N = 1,054).
a: Good sleep quality was defined as the PSQI global score ≤5; poor sleep quality was defined as the PSQI global score >5.
b: No depression was defined as the Patient Health Questionnare-8 (PHQ-8) score < 10; depression was defined as the PHQ - 8 score ≥ 10. Adjusted for age (years), sex, education, cigarette smoking, alcohol, and khat consumption
Discussion
The prevalence of suicidal ideation in this cohort of Ethiopian adults was 24.8%. We found that poor sleep quality was associated with a 3.46-fold increased odds of (AOR=3.46; 95% CI 2.27–5.26) suicidal ideation after adjusting for confounders including depression. When assessed as a continuous variable, every 1-unit increase in PSQI global score resulted in a 20% increased odds of suicidal ideation (AOR=1.20; 95% CI 1.14–1.27). The odds of suicidal ideation increased across successive tertiles of PSQI global scores, and this trend was confirmed when we modeled suicidal ideation using the generalized additive modeling (GAM) procedure with a cubic spline function. The data provides clear evidence that sleep quality and depressive symptoms have a strong association with suicidal ideation in Ethiopian adults.
Our findings are generally consistent with existing literature reporting strong associations between poor sleep quality and risk of suicidal ideation [24, 25]. For instance, Lapierre and colleagues, in their study among community living older adults, found that poor sleep quality (assessed using the PSQI) was significantly associated (p<0.001) with prevalent suicidal ideation (assessed using one item) [26]. Other investigators have reported similar associations. A recent meta-analysis of 39 studies has also indicated that sleep disturbances are associated with a 1.86-fold increased odds of suicidal ideation (OR=1.86; 95%CI 1.52–2.28) [27]. In sum, available evidence indicate that sleep disturbances, in addition to being a symptom of depressive disorders, is an important independent risk factor for suicidal ideation. On the basis of these epidemiological findings, authors have argued that sleep-focused intervention strategies should be developed and added to suicide prevention initiatives [15].
Biological mechanisms for the robustly observed association of sleep disturbances and poor sleep quality with suicidal ideation have not been fully elucidated. However, the associations are likely attributable to the fact that the two conditions share several neurobiological pathways including hypothalamic-pituitary-adrenal (HPA) axis alterations, elevations in pro-inflammatory cytokines, and decreased serotonergic tone [27]. Sleep disorders have been reported to lead to alterations in HPA axis hormones, such as adrenocorticotropic hormone (ACTH) and cortisol [27–29]. Alterations of the HPA axis, observed among individuals with suicidal ideation and depressive disorders, may well be one mechanism underlying the consistently observed statistical association of sleep disturbance and suicidal ideation. In a recent study, suicidal patients, as compared with their non-suicidal counterparts, were found to have chronic systemic inflammation, as evidenced by their higher plasma or serum concentrations of pro-inflammatory cytokines including interleukin-1β, interleukin-6, interleukin-10, C-reactive protein, and tumor necrosis factor-α [30]. In addition to these hypothesized neuroendocrine and proinflammatory mechanism, some investigators have posited that shared psychosocial and behavioral mechanisms, including adverse life events, psychiatric conditions and physical inactivity [26, 27] may explain the observed associations. More research is warranted to thoroughly explore hypotheses concerning mechanisms underlying observed sleep disturbance and suicidal ideation.
The strengths of our study include a large sample size and rigorous analytic approaches that included accounting for confounders. However, several limitations must be taken into consideration when interpreting our results. First, we used a cross-sectional study design, which hinders our capacity to make assertions pertaining to the directionality or temporal relations of sleep disorders and suicidal ideation. Second, our study population consists of patients who were attending outpatient clinics thereby limiting the generalizability of our study findings to a broader general population. Third, the potential of recall bias must be considered as participants were asked to report sleep habits over the past month and report distress over the past weeks to address PSQI and PHQ-9 instruments, respectively. Lastly, subjective sleep quality and sleep habits were measured using the self-administered assessment tool. Causal inferences will be enhanced in future prospective studies designed to allow interrogation of the directionality of sleep disturbances and suicidal ideation. Furthermore such studies should include both subjective and objective measurements of sleep quality and other sleep traits among to more fully characterize the associations.
This is the first reported study to assess the independent relationship between subjective sleep quality and suicidal ideation among sub-Saharan African adults. Future research with objective measures of sleep disorders and diagnostic assessments of suicidal ideation is needed to confirm and expand upon our findings. A recent WHO Mental Health Action Plan seeks to achieve a 10% reduction in suicide by 2020 in many LAMICS [3]. In light of this aspirational goal, and in light of our present findings, mental health services designed to identify, intervene, and prevent death by suicide should consider addressing sleep disturbances and poor sleep quality as an important components of care.
Acknowledgments
Funding: This research was supported by an award from the National Institutes of Health, National Institute of Minority Health and Health Disparities (T37-MD001449). The sponsor had no role in the design or conduct of this research
The authors wish to thank the staff of Addis Continental Institute of Public Health for their expert technical assistance. The authors would also like to thank Saint Paul Hospital for granting access to conduct the study.
Footnotes
Conflict of Interest: All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval: All procedures performed in the study were in accordance with the 1964 Helsinki declaration and its later amendments and were approved by the Institutional Review Boards of Addis Continental Institute of Public Health, Addis Ababa, Ethiopia and the Human Subjects Division at the University of Washington, Seattle, USA
Informed consent: Written informed consent was obtained from all individual participants included in the study.
References
- 1.Bernert RA, Turvey CL, Conwell Y, Joiner TE., Jr Association of poor subjective sleep quality with risk for death by suicide during a 10-year period: a longitudinal, population-based study of late life. JAMA Psychiatry. 2014;71(10):1129–1137. doi: 10.1001/jamapsychiatry.2014.1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bernert RA, Nadorff MR. Sleep Disturbances and Suicide Risk. Sleep Med Clin. 2015;10(1):35–39. doi: 10.1016/j.jsmc.2014.11.004. [DOI] [PubMed] [Google Scholar]
- 3.(WHO) WHO. [Accessed on 11/27/2015];Preventing suicide: A global imperative. 2015 Available at: http://apps.who.int/iris/bitstream/10665/131056/1/9789241564779_eng.pdf?ua=1&ua=1.
- 4.Nock MK, Hwang I, Sampson N, Kessler RC, Angermeyer M, Beautrais A, Borges G, Bromet E, Bruffaerts R, de Girolamo G, et al. Cross-national analysis of the associations among mental disorders and suicidal behavior: findings from the WHO World Mental Health Surveys. PLoS Med. 2009;6(8):11. doi: 10.1371/journal.pmed.1000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morgan I, Eguia F, Gelaye B, Peterlin BL, Tadesse MG, Lemma S, Berhane Y, Williams MA. Sleep disturbances and quality of life in Sub-Saharan African migraineurs. J Headache Pain. 2015;16:18. doi: 10.1186/s10194-015-0504-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gottlieb DJ, Redline S, Nieto FJ, Baldwin CM, Newman AB, Resnick HE, Punjabi NM. Association of usual sleep duration with hypertension: the Sleep Heart Health Study. Sleep. 2006;29(8):1009–1014. doi: 10.1093/sleep/29.8.1009. [DOI] [PubMed] [Google Scholar]
- 7.Gildner TE, Liebert MA, Kowal P, Chatterji S, Snodgrass JJ. Associations between sleep duration, sleep quality, and cognitive test performance among older adults from six middle income countries: results from the Study on Global Ageing and Adult Health (SAGE) J Clin Sleep Med. 2014;10(6):613–621. doi: 10.5664/jcsm.3782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sutter C, Zollig J, Allemand M, Martin M. Sleep quality and cognitive function in healthy old age: the moderating role of subclinical depression. Neuropsychology. 2012;26(6):768–775. doi: 10.1037/a0030033. [DOI] [PubMed] [Google Scholar]
- 9.Leblanc MF, Desjardins S, Desgagne A. Sleep problems in anxious and depressive older adults. Psychol Res Behav Manag. 2015;8:161–169. doi: 10.2147/PRBM.S80642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Al-Delaimy WK, Manson JE, Willett WC, Stampfer MJ, Hu FB. Snoring as a risk factor for type II diabetes mellitus: a prospective study. Am J Epidemiol. 2002;155(5):387–393. doi: 10.1093/aje/155.5.387. [DOI] [PubMed] [Google Scholar]
- 11.Lemma S, Patel SV, Tarekegn YA, Tadesse MG, Berhane Y, Gelaye B, Williams MA. The Epidemiology of Sleep Quality, Sleep Patterns, Consumption of Caffeinated Beverages, and Khat Use among Ethiopian College Students. Sleep Disord. 2012;2012:583510. doi: 10.1155/2012/583510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goodwin RD, Marusic A. Association between short sleep and suicidal ideation and suicide attempt among adults in the general population. Sleep. 2008;31(8):1097–1101. [PMC free article] [PubMed] [Google Scholar]
- 13.Byrd K, Gelaye B, Tadessea MG, Williams MA, Lemma S, Berhanec Y. Sleep Disturbances and Common Mental Disorders in College Students. Health Behav Policy Rev. 2014;1(3):229–237. doi: 10.14485/HBPR.1.3.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bernert RA, Hom MA, Roberts LW. A review of multidisciplinary clinical practice guidelines in suicide prevention: toward an emerging standard in suicide risk assessment and management, training and practice. Acad Psychiatry. 2014;38(5):585–592. doi: 10.1007/s40596-014-0180-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bernert RA, Kim JS, Iwata NG, Perlis ML. Sleep disturbances as an evidence-based suicide risk factor. Curr Psychiatry Rep. 2015;17(3):554. doi: 10.1007/s11920-015-0554-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 17.Gelaye B, Lohsoonthorn V, Lertmeharit S, Pensuksan WC, Sanchez SE, Lemma S, Berhane Y, Zhu X, Velez JC, Barbosa C, et al. Construct validity and factor structure of the pittsburgh sleep quality index and epworth sleepiness scale in a multi-national study of African, South East Asian and South American college students. PLoS One. 2014;9(12):e116383. doi: 10.1371/journal.pone.0116383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gelaye B, Williams MA, Lemma S, Deyessa N, Bahretibeb Y, Shibre T, Wondimagegn D, Lemenhe A, Fann JR, Vander Stoep A, et al. Validity of the Patient Health Questionnaire-9 for depression screening and diagnosis in East Africa. Psychiatry Res. 2013;210(2):653–661. doi: 10.1016/j.psychres.2013.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gilbody S, Richards D, Brealey S, Hewitt C. Screening for depression in medical settings with the Patient Health Questionnaire (PHQ): a diagnostic meta-analysis. J Gen Intern Med. 2007;22(11):1596–1602. doi: 10.1007/s11606-007-0333-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Belew M, Kebede D, Kassaye M, Enquoselassie F. The magnitude of khat use and its association with health, nutrition and socio-economic status. Ethiop Med J. 2000;38(1):11–26. [PubMed] [Google Scholar]
- 22.Kalix P. Khat: scientific knowledge and policy issues. Br J Addict. 1987;82(1):47–53. doi: 10.1111/j.1360-0443.1987.tb01436.x. [DOI] [PubMed] [Google Scholar]
- 23.Hastie T, Tibshirani R. Generalized Additive Models. Chapman-Hall; London: 1990. [DOI] [PubMed] [Google Scholar]
- 24.Agargun MY, Kara H, Solmaz M. Subjective sleep quality and suicidality in patients with major depression. J Psychiatr Res. 1997;31(3):377–381. doi: 10.1016/s0022-3956(96)00037-4. [DOI] [PubMed] [Google Scholar]
- 25.Turvey CL, Conwell Y, Jones MP, Phillips C, Simonsick E, Pearson JL, Wallace R. Risk factors for late-life suicide: a prospective, community-based study. Am J Geriatr Psychiatry. 2002;10(4):398–406. [PubMed] [Google Scholar]
- 26.Lapierre S, Boyer R, Desjardins S, Dube M, Lorrain D, Preville M, Brassard J. Daily hassles, physical illness, and sleep problems in older adults with wishes to die. Int Psychogeriatr. 2012;24(2):243–252. doi: 10.1017/S1041610211001591. [DOI] [PubMed] [Google Scholar]
- 27.Pigeon WR, Pinquart M, Conner K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J Clin Psychiatry. 2012;73(9):e1160–1167. doi: 10.4088/JCP.11r07586. [DOI] [PubMed] [Google Scholar]
- 28.Jacobs N, Myin-Germeys I, Derom C, Delespaul P, van Os J, Nicolson NA. A momentary assessment study of the relationship between affective and adrenocortical stress responses in daily life. Biol Psychol. 2007;74(1):60–66. doi: 10.1016/j.biopsycho.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 29.Mannie ZN, Harmer CJ, Cowen PJ. Increased waking salivary cortisol levels in young people at familial risk of depression. Am J Psychiatry. 2007;164(4):617–621. doi: 10.1176/ajp.2007.164.4.617. [DOI] [PubMed] [Google Scholar]
- 30.Gananca L, Oquendo MA, Tyrka AR, Cisneros-Trujillo S, Mann JJ, Sublette ME. The role of cytokines in the pathophysiology of suicidal behavior. Psychoneuroendocrinology. 2015;63:296–310. doi: 10.1016/j.psyneuen.2015.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]