Abstract
Purpose: Sexual and gender minorities (SGMs) in medicine experience unique stressors in training. However, little is known about SGM specialty choice. This study examined predictors of SGM specialty choice, associations between specialty prestige and perceived SGM inclusion, and self-reported influences on specialty choice.
Methods: Medical trainees and practitioners (358 SGM, 1528 non-SGM) were surveyed online. We operationalized specialty choice at the individual level as respondents' specialty of practice; at the specialty level, as a percentage of SGM respondents in each specialty. We examined specialty prestige, perceived SGM inclusivity, and medical school climate as predictors of SGM specialty choice, and we compared additional influences on specialty choice between SGM and non-SGM.
Results: The percentage of SGM in each specialty was inversely related to specialty prestige (P = 0.001) and positively related to perceived SGM inclusivity (P = 0.01). Prestigious specialties were perceived as less SGM inclusive (P < 0.001). Medical school climate did not predict specialty prestige (P = 0.82). SGM were more likely than non-SGM to indicate that sexual and gender identity strongly influenced specialty choice (P < 0.01). SGM most frequently rated personality fit, specialty content, role models, and work–life balance as strong influences on specialty choice. Exposure as a medical student to SGM faculty did not predict specialty prestige among SGM.
Conclusion: Specialty prestige and perceived inclusivity predict SGM specialty choice. SGM diversity initiatives in prestigious specialties may be particularly effective by addressing SGM inclusion directly. Further research is needed to inform effective mentorship for SGM medical students. Exposure to SGM in medical training reduces anti-SGM bias among medical professionals, and SGM in medicine often assume leadership roles in clinical care, education, and research regarding SGM health. Supporting and promoting SGM diversity across the spectrum of medical specialties, therefore, represents a critical avenue to improve the care delivered to SGM populations and addresses the role of providers in the health disparities experienced by SGM.
Keywords: : gender identity, health education/training program, minority stress, sexual orientation, survey design or survey methodology
Introduction
Sexual and gender minority (SGM) individuals, including those who identify as lesbian, gay, bisexual, transgender, or queer, are subject to stigma-related stress, also known as minority stress.1 SGM stress is generated by stigmatizing social structures and institutions, which justify discriminatory treatment in interactions with family, friends, classmates, and coworkers. Chronic exposure to stigma yields anxious anticipation of future rejection, internalized heterosexism, and stress associated with identity concealment.1–4 A growing body of literature suggests that SGM medical students, residents, and physicians experience such stressors throughout medical training and practice.
Sexual minority (SM) medical students are more likely than non-SGM students to report stress, isolation, verbal insults, and harassment or threats5 and they are approximately twice as likely to experience depression and related mental health comorbidities.5,6 Almost one-fifth of lesbian-identified physicians report sexual orientation harassment during residency, and two-fifths report ever experiencing such harassment in a medical setting.7 Two-thirds of SGM physicians have heard disparaging remarks about SGM at work; one-third have witnessed discriminatory care of an SGM patient; approximately one-quarter have witnessed discrimination against an SGM employee; and approximately one-fifth report experiencing social ostracism because of their SGM identity.8
Although it is clear that SGM stress extends into the residency application process,9–11 little is known about the relationship between SGM identity and specialty choice. Furthermore, no research to date has examined the association between specialty prestige and SGM specialty choice. Anecdotal evidence and limited empirical data suggest that SGM in medicine perceive certain specialties as less inclusive, to the extent that SGM applicants may conceal their minority identity during the residency application process to protect their chances of matching in a given specialty.9–14 More prestigious specialties, including those with more competitive entry requirements and those with higher average incomes, may be less inclusive of SGM residents and practitioners.10,15 However, the association between specialty prestige, perceived inclusivity, and specialty choice among SGM has not been evaluated. Medical school climate for SM students has previously been associated with SM medical student comfort and with identity disclosure,6 but it has not previously been studied in relation to specialty choice. Additional predictors of specialty choice, such as income expectations or family plans, have also not been compared between SGM and non-SGM.
The Diversity in Medical Career Development Study was conducted among U.S. medical students, residents, and physicians to determine whether a specialty's prestige and perceived SGM inclusivity predict the proportion of SGM in that specialty, to evaluate the association between specialty prestige and perceived medical school support for SGM, and to compare factors influencing specialty choice between SGM and non-SGM.
Method
This study was deemed exempt from review by the Yale University Human Subjects Committee. Written informed consent was obtained before survey access. The survey (complete survey available as Supplementary Appendix A; Supplementary Data are available online at www.liebertpub.com/lgbt) was administered from May to August 2015. Recruitment messages were e-mailed to non-SGM-specific and SGM-specific medical organizations to oversample SGM respondents.
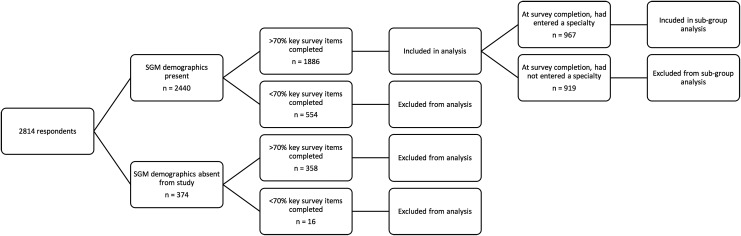
The survey was initiated by 2814 individuals. Respondents were able to skip any survey item. Respondents who did not complete (1) SGM-related demographics (n = 358), (2) at least 70% of the four items used to evaluate perceived SGM inclusion within specialties (n = 554), or (3) both (n = 16) were omitted (Fig. 1). To ensure that participants responded to the majority of specialty-specific items for the 26 specialties, we required that respondents complete at least 70% of these items to be retained in the final dataset. After application of the exclusion criteria, the percentage of missing data per item ranged from 0.0% to 9.6%, except for the item evaluating perceived support for LGBT professional activities in Internal Medicine-Pediatrics, for which 44.2% of respondents were missing data.
FIG. 1.
Determination of final analytic sample based on completion of SGM demographics and at least 70% of survey items evaluating perceived anti-SGM bias in medical specialties. SGM, sexual and gender minority.
The final analytic sample contained 358 SGM and 1528 non-SGM. We used this sample to examine the relationship between specialty prestige and perceived anti-SGM bias. Predictors of SGM specialty choice and self-reported influences on specialty choice were examined by using data from the subset of respondents who, at the time of survey completion, had entered or completed specialty training (n = 160 SGM; 807 non-SGM).
Survey design
Demographics included recruitment via SGM or non-SGM organization, age, race/ethnicity, natal sex, (anticipated) year of medical school graduation, allopathic versus osteopathic medical school, state of medical school, and specialty. States were categorized into census regions.16 SGM identity was evaluated by the questions: (1) “Which of the following best describes your sexual orientation identity?” (response options: lesbian; bisexual; gay; queer; heterosexual; other) and (2) “With which gender identity do you most identify currently?” (response options: female; male; transwoman; transman; genderqueer; other).
We calculated the proportion of SGM respondents in each specialty that contained at least 10 respondents, which excluded the following specialties, as they did not satisfy this threshold: Medical Genetics, Neurological Surgery, Plastic Surgery, Preventive Medicine, and Thoracic Surgery. SGM respondents ranked the 26 specialty options17 by using four 5-point Likert items evaluating perceived SGM inclusion and support (see Supplementary Appendix A for all items). For each specialty, principal component analysis uncovered a unitary factor structure accounting for more than 50% of the variance across items, ranging from 51.5% for Allergy and Immunology to 63.3% for Family Medicine. Perceived SGM inclusion for each specialty was calculated as the mean of SGM respondents' responses to these four items.
Specialty competitiveness and median income were measured by using publicly available data.18,19 Competitiveness was measured by using available residency positions per U.S. applicants, a metric of supply and demand that has been previously used to examine specialty competitiveness.20 We standardized income and competitiveness by calculating the z-scores for each item. Given their high correlation (r = 0.61, P = 0.004), we then combined these z-scores by calculating the mean of the z-score of income and the z-score of competitiveness, which served as our measure of specialty prestige. Prestige was dichotomized at the median of 0.02.
SGM respondents completed 18 previously used items describing medical school SGM support6; the mean of the items served as the medical school climate index. Medical school climate scores were dichotomized at the median of 0.61.
Factors influencing specialty choice were evaluated per the Association of American Medical Colleges' (AAMC) Medical School Graduation Questionnaire17 with the addition of “my race/ethnicity”; “my gender”; and “my sexual orientation or gender identity.” Likert items (1 = no influence; 2 = minor influence; 3 = moderate influence; 4 = strong influence) were dichotomized (strong influence = 1; not strong influence = 0). Exposure while a medical student to SGM faculty in medical school, in general, and to SGM faculty in the respondent's later specialty were evaluated with 4-point Likert items (1 = never, 2 = infrequently, 3 = sometimes, 4 = frequently). Responses were dichotomized (frequent exposure = 1; less than frequent exposure = 0).
Statistical analysis
We constructed specialty-level and person-level models (SPSS 23; IBM Corporation, Armonk, New York). In specialty-level models, linear regression was used to evaluate associations between (1) specialty prestige and proportion of SGM respondents in each specialty; (2) perceived SGM inclusion and proportion of SGM respondents; and (3) specialty prestige and perceived SGM inclusion. In person-level models, we first evaluated associations between SGM identity and other demographics by using chi-square tests of independence and independent-samples t-tests. We also used chi-square tests of independence and independent-samples t-tests to compare respondents included and excluded from the study based on the inclusion criteria. We conducted a post hoc analysis with a Bonferroni correction to identify the direction of difference for demographic data.21 Logistic regression was used to assess associations between medical school support and SGM respondents' entry into high prestige specialties by using region of medical school, type of medical school, and race/ethnicity as covariates. Using the same covariates, logistic regression was used to evaluate associations between SGM identity and predictors of specialty choice, and between frequency of exposure as a medical student to SGM faculty and specialty prestige. We also qualitatively describe the frequency with which each predictor of specialty choice was identified as strongly influential by SGM and by non-SGM respondents. Two-sided tests of significance were employed in all analyses. A P-value of 0.05 was used to evaluate statistical significance.
Results
The included respondents were younger (P = 0.006) and had graduated from medical school more recently (P = 0.004). Included and excluded respondents did not differ by specialty prestige (P = 0.083), SGM versus non-SGM identity (P = 0.10), reported natal sex (P = 0.911), gender identity (P = 0.141), sexual orientation identity (P = 0.350), race/ethnicity (P = 0.331), medical school region (P = 0.961), or allopathic versus osteopathic medical school (P = 0.054) (Supplementary Table S1). Post hoc analyses showed that included respondents were more likely to be recruited from a designated non-SGM organization (χ2 = 5.29, P = 0.02) and less likely to be recruited from an “unknown or other” organization (χ2 = 14.44, P < 0.001) compared with excluded respondents.
Among participants satisfying the inclusion criteria, SGM respondents were less likely to attend an osteopathic medical school (χ2 = 39.196, P < 0.001) and more likely to have entered a low prestige specialty (χ2 = 6.342, P = 0.01). Age and graduation year did not differ (Table 1). Post hoc analyses revealed that SGM were more likely than non-SGM to have been recruited via an SGM-specific organization (χ2 = 376.36, P < 0.001), and non-SGM were more likely than SGM to have been recruited via an non-SGM-specific organization (χ2 = 240.25, P < 0.001). SGM were more likely to identify as White (χ2 = 10.24, P < 0.005), and non-SGM were more likely to identify as Asian (χ2 = 6.76, P < 0.01) or Black/African American (χ2 = 9.00, P < 0.01). SGM were more likely to indicate natal sex as male (χ2 = 17.64, P < 0.001) or intersex (χ2 = 8.41, P < 0.01), and less likely to indicate natal sex as female (χ2 = 18.49, P < 0.001). SGM were more likely to be from the Western United States (χ2 = 11.56, P < 0.001), and less likely to be from the Midwestern United States (χ2 = 14.44, P < 0.001).
Table 1.
Demographic Characteristics of SGM and Non-SGM Medical Trainees and Practitioners Included in Analyses of the 2015 Online Diversity in Medical Career Development Study of Specialty Choice Among SGM in Medicine
| Demographic characteristics | SGM, n (%) | Non-SGM, n (%) | χ2 [Cramer's V] | Pa |
|---|---|---|---|---|
| Method of recruitment | 327 (100) | 1378 (100) | 379.239 [0.472] | <0.001* |
| SGM-specific medical organization | 120 (36.70) | 34 (2.47) | ||
| Non-SGM-specific medical organization | 187 (57.19) | 1259 (91.36) | ||
| Other (SGM specificity unknown) | 20 (6.12) | 85 (6.17) | ||
| Reported natal sexb | 356 (100) | 1521 (100) | 26.532 [0.119] | <0.001* |
| Female | 160 (44.94) | 877 (57.66) | ||
| Male | 194 (54.49) | 644 (42.34) | ||
| Intersex | 2 (0.56) | 0 (0.00) | ||
| Gender identity | 358 (100) | 1528 (100) | 114.653 [0.247] | <0.001* |
| Woman | 143 (39.94) | 877 (57.40) | ||
| Man | 194 (54.19) | 651 (42.60) | ||
| Transwoman | 1 (0.28) | 0 (0.00) | ||
| Transman | 3 (0.84) | 0 (0.00) | ||
| Genderqueer | 13 (3.63) | 0 (0.00) | ||
| Other | 4 (1.12) | 0 (0.00) | ||
| Sexual orientation identity | 358 (100) | 1528 (100) | 1866.531 [0.995] | <0.001* |
| Lesbian | 68 (18.99) | 0 (0.00) | ||
| Bisexual | 66 (18.44) | 0 (0.00) | ||
| Gay | 173 (48.32) | 0 (0.00) | ||
| Queer | 29 (8.10) | 0 (0.00) | ||
| Heterosexual | 3 (0.84) | 1528 (100) | ||
| Other | 19 (5.31) | 0 (0.00) | ||
| Race/ethnicity | 356 (100) | 1522 (100) | 18.553 [0.099] | 0.001* |
| Hispanic, Latino or of Spanish origin | 15 (4.21) | 68 (4.47) | ||
| Asian | 43 (12.08) | 271 (17.81) | ||
| Black or African American | 10 (2.81) | 108 (7.10) | ||
| White | 264 (74.16) | 994 (65.31) | ||
| Other | 24 (6.74) | 81 (5.32) | ||
| Type of medical school | 356 (100) | 1515 (100) | 39.196 [0.145] | <0.001* |
| Allopathic | 305 (85.67) | 1048 (69.17) | ||
| Osteopathic | 51 (14.37) | 467 (30.83) | ||
| Region of medical school | 356 (100) | 1508 (100) | 25.032 [0.116] | <0.001* |
| Northeast | 106 (29.78) | 377 (25.00) | ||
| Midwest | 82 (23.03) | 506 (33.55) | ||
| South | 93 (26.12) | 377 (25.00) | ||
| West | 61 (17.13) | 160 (10.61) | ||
| Outside of the United States | 14 (3.93) | 88 (5.84) | ||
| Prestige of medical specialty of practicec | 151 (100) | 758 (100) | 6.342 [0.084] | 0.01* |
| Low prestige | 127 (84.11) | 565 (74.54) | ||
| High prestige | 24 (15.89) | 193 (25.46) |
| Demographic characteristics | SGM mean [SD] | Non-SGM mean [SD] | Pa | |
|---|---|---|---|---|
| Age (years)d | 30.7535 [9.43671] | 31.4908 [10.89159] | 0.20 | |
| Year of medical school graduationd | 2012.45 [9.506] | 2011.32 [10.827] | 0.05 | |
Two-sided P-value less than 0.05 considered statistically significant, indicated by *.
Individuals born with an intersex condition, alternately referred to as a difference of sex development, have a congenital condition in which the development of chromosomal, gonadal, or anatomical sex is atypical relative to normatively developed males or females. “Intersex” was included as a response option for reported natal sex.
Non-graduating medical students (i.e., medical students who have not yet been accepted to train in a given medical specialty) were excluded from this analysis.
Relations between SGM identity and age, and between SGM identity and year graduated from medical school, were evaluated by using independent-samples t-tests. The Levine test of equality of variance indicated a threat to the assumption of homogeneity of variance for all t-tests, so t-tests were run without the assumption of equal variances.
SGM, sexual and gender minority.
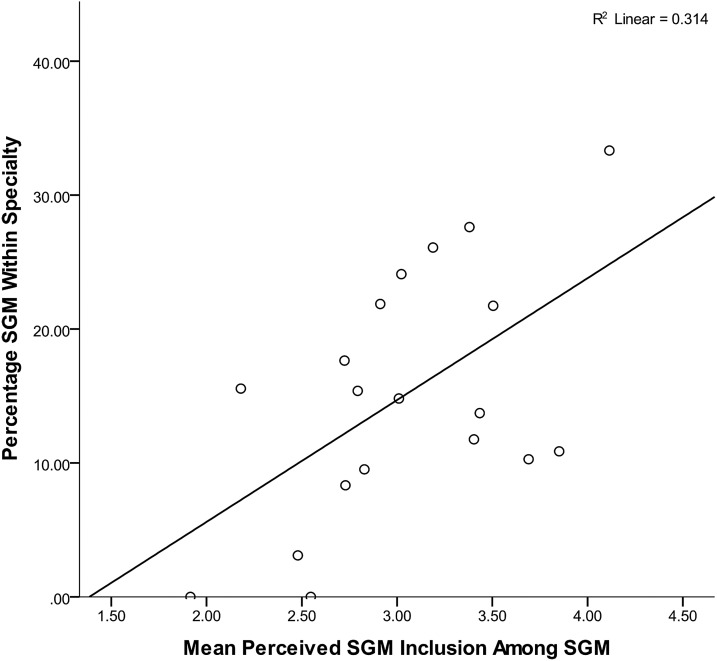
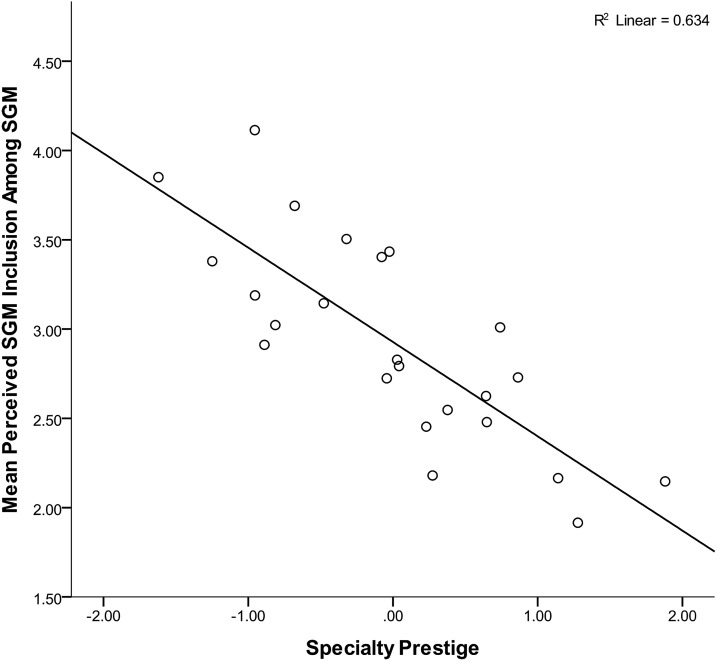
As shown in Figure 2, specialty prestige was inversely related to the percentage of SGM respondents within specialties (B = −0.679, P = 0.001), and, as shown in Figure 3, perceived SGM inclusion was positively related to the percentage of SGM respondents within specialties (B = 0.560, P = 0.01). Among SGM respondents, specialty prestige was strongly inversely related to perceived SGM inclusion (B = −0.796, P < 0.001) (Fig. 4). SGM respondents rated the following specialties, in order, as the most SGM inclusive: Psychiatry, Family Medicine, Pediatrics, Preventive Medicine, and Internal Medicine/Pediatrics. SGM respondents rated the following specialties, in order, as the least SGM inclusive: Orthopedics, Neurosurgery, Thoracic Surgery, General Surgery, and Colon and Rectal Surgery. Perceived medical school support did not predict SGM entry into high prestige specialties [Exp(B) = 1.106; 95% CI, 0.456, 2.681; P = 0.82].
FIG. 2.
Association between objective specialty prestige and proportion of SGMs in specialties in the 2015 Diversity in Medical Career Development Study of specialty choice among SGM in medicine.
FIG. 3.
Association between perceived specialty inclusion of SGMs among SGM respondents and proportion of SGM in specialties in the 2015 Diversity in Medical Career Development Study of specialty choice among SGM in medicine.
FIG. 4.
Association between objective specialty prestige and perceived inclusion of SGMs among SGM respondents in the 2015 Diversity in Medical Career Development Study of specialty choice among SGM in medicine.
Compared with non-SGM, SGM were more likely to rate sexual orientation or gender identity [Exp(B) = 56.505; 95% CI, 6.609, 483.132; P < 0.01] as a strong influence on specialty choice. SGM and non-SGM did not differ in the likelihood of rating the following factors as strongly influential on specialty choice: specialty competitiveness [Exp(B) = 1.377; 95% CI, 0.709, 2.675; P = 0.35], level of education debt [Exp(B) = 1.069; 95% CI, 0.496, 2.305; P = 0.87], role model influence [Exp(B) = 1.398; 95% CI, 0.979, 1.998; P = 0.07], income expectations [Exp(B) = 0.447; 95% CI, 0.199, 1.003; P = 0.05], length of residency training [Exp(B) = 1.109; 95% CI, 0.567, 2.169; P = 0.76], options for fellowship training [Exp(B) = 1.488; 95% CI, 0.941, 2.353; P = 0.09], family expectations [Exp(B) = 0.923; 95% CI, 0.370, 2.30; P = 0.86], future family plans [Exp(B) = 0.678; 95% CI, 0.411, 1.119; P = 0.13], work–life balance [Exp(B) = 1.211; 95% CI, 0.837, 1.751; P = 0.31], fit with personality, interests, and skills [Exp(B) = 1.215; 95% CI, 0.729, 2.024; P = 0.46], content of specialty [Exp(B) = 1.568; 95% CI, 0.991, 2.480; P = 0.06], gender [Exp(B) = 1.104; 95% CI, 0.400, 3.044; P = 0.85], or race/ethnicity [Exp(B) = 4.058; 95% CI, 0.964, 17.089; P = 0.06]. An alternative statistical model incorporating level of training did not show an interaction between level of training and SGM status for any factor influencing specialty choice, such that level of training did not affect the findings reported earlier (results not shown).
As shown in Table 2, the following factors (in order) were the most often rated as strong influences on specialty choice by SGM: fit with personality, interests and skills, specialty content, role model influences, and work–life balance. The following factors (in order) were the most often rated as strong influences by non-SGM: fit with personality, interests and skills, specialty content, role model influences, and work–life balance. Overall, SGM and non-SGM, thus, report a similar qualitative ranking of the factors strongly influencing specialty choice, as inferred by the frequency with which those factors are reported as strongly influential in each group.
Table 2.
Frequencies of Identification of Factors as Strong Influences on Specialty Choice Among SGM and Non-SGM Medical Practitioners Participating in the 2015 Online Diversity in Medical Career Development Study of Specialty Choice Among SGM in Medicine
| Factors influencing specialty choice | Number of SGM participants who rated the influence of factor | Percentage of SGM respondents identifying factor as a strong influence on specialty choice (n) | Number of non-SGM participants who rated the influence of factor | Percentage of non-SGM respondents identifying factor as a strong influence on specialty choice (n) |
|---|---|---|---|---|
| Specialty competitiveness | 159 | 8.8 (14) | 805 | 6.5 (52) |
| Level of education debt | 160 | 6.3 (10) | 805 | 5.5 (44) |
| Role model influences | 160 | 51.2 (82) | 806 | 41.6 (335) |
| Income expectations | 160 | 5.0 (8) | 805 | 9.2 (74) |
| Length of residency training | 160 | 8.1 (13) | 805 | 8.1 (65) |
| Options for fellowship training | 159 | 20.8 (33) | 805 | 14.8 (119) |
| Family expectations | 160 | 3.8 (6) | 806 | 4.2 (34) |
| Future family plans | 160 | 13.8 (22) | 805 | 18.6 (150) |
| Work–life balance | 160 | 38.1 (61) | 805 | 32.9 (265) |
| Fit with personality, interests, and skills | 160 | 86.9 (139) | 806 | 80.9 (652) |
| Content of specialty | 160 | 82.5 (132) | 806 | 72.8 (587) |
| My gender | 160 | 3.1 (5) | 805 | 3.0 (24) |
| My race/ethnicity | 159 | 2.5 (4) | 804 | 1.1 (9) |
| My sexual orientation or gender identity | 160 | 6.3 (10) | 805 | 0.1 (1) |
Among SGM, neither frequent exposure as a medical student to SGM faculty in general nor that to SGM faculty in the specialty of later practice predicted the prestige of respondents' specialties of practice [Exp(B) = 0.495; 95% CI, 0.153, 1.603; P = 0.24; Exp(B) = 0.361; 95% CI, 0.077, 1.689; P = 0.20].
Discussion
This study reveals that prestigious specialties, as measured by an objective index, are perceived by SGM to be less inclusive of SGM. This study also indicates that the proportion of SGM within a specialty is positively related to the perceived SGM inclusivity of that specialty, and inversely related to specialty prestige. SGM were significantly more likely than non-SGM to rate their sexual orientation or gender identity as a strong influence on specialty choice. Contrary to hypotheses, the associations between medical school climate and specialty prestige among SGM, and between exposure to SGM faculty as a medical student and specialty prestige among SGM, were not significant.
The findings of this study suggest that SGM may be systematically under-represented across a range of specialties. The specialties perceived as the most welcoming (Psychiatry, Family Medicine, Pediatrics, Preventive Medicine, and Internal Medicine/Pediatrics) and the least welcoming (Orthopedics, Neurosurgery, Thoracic Surgery, General Surgery, and Colon and Rectal Surgery) partially parallel those specialties identified in previous research from two decades ago to be perceived by sexual minorities (SM) as the most supportive (Psychiatry, Family Practice, Pediatrics, and Internal Medicine) and the most biased (Surgery, Obstetrics/Gynecology, Pediatrics, and Anesthesiology).11
Disproportionate distribution of SGM physicians may, thus, be a longstanding issue. This conclusion is supported by a previous study describing differences in the specialty of practice between SM and non-SM female physicians.22 Although SGM were more likely to attend an allopathic medical school than non-SGM in this study, it is unlikely that this demographic difference contributed substantially to the lower proportion of SGM in high prestige specialties, as type of medical school was controlled for as a covariate. Furthermore, under-representation of SGM within prestigious specialties may be a self-perpetuating phenomenon, as SGM identify SGM mentors as critical facilitators of professional success.23
Equitable representation of SGM across specialties has the potential to positively impact SGM-based health disparities in the general population, which include obesity, mental health, tobacco and other substance dependence, teenage pregnancy, asthma, infectious disease, and certain cancers.24–26 Deficits in cultural competency among physicians and overt anti-SGM bias and discrimination contribute to the creation and maintenance of disparities.27–33 Anti-SM bias has been well documented among medical trainees and providers,15,34,35 whereas contact with SGM (before or during medical education) consistently predicts reduced anti-SGM bias, greater comfort and willingness to serve SGM patients, and greater willingness to work with SGM colleagues.34,36–42
Conversely, medical trainees with less contact with SM are more likely to express anti-SM attitudes.38,39 The representation and visibility of SGM across medicine may, therefore, represent a powerful means to reduce bias among non-SGM physicians, since contact with SGM predicts reductions in explicit and implicit anti-SGM bias, and contact between equals has been experimentally shown to decrease bias.34 In addition, SGM in medicine often assume leadership roles in promoting educational reform, research, and clinical programs to address the health needs of SGM, and so may catalyze even greater downstream improvement in the health of SGM populations.23
Further research is needed on the factors contributing to perceptions of anti-SGM bias within specialties. Preliminary evidence suggests that perceptions of SGM inclusion may partially reflect extant professional environments. A 2007 study of practicing physicians found that (in order) surgery, family medicine, and orthopedic physicians expressed the most homophobic attitudes, whereas psychiatry, internal medicine, and pediatric physicians expressed the least homophobic attitudes.15 Similarly, a 1998 study reported that surgeons were particularly likely to discourage SM from entering their specialty.43 Further research is needed to evaluate the relationship between perceived and actual anti-SGM bias within specialties and the mechanisms by which perceptions of bias are acquired by SGM medical students.
The concurrent development and evaluation of programs to address anti-SGM bias and to promote SGM diversity across specialties is also needed. Although some specialty-specific organizations have published SGM health curricula guidelines44 and some independent groups have begun to develop specialty-level curricular materials on SGM topics,45 such efforts are disjointed and sporadic. Graduate medical education may benefit from adapting strategies to promote SGM diversity that have contributed to the recent, significant climate change around SGM issues in undergraduate medical education. For example, the American Osteopathic Association, the Joint Commission, the AAMC, and the American Medical Association46–49 have all publicly made statements supporting SGM diversity and promoting inclusion. Comparable specialty-level organizations could do the same, propelling further efforts to address SGM topics within specialties. The AAMC has also taken a leading role in developing and disseminating materials to support undergraduate SGM curriculum development and to instigate improvement of institutional climate change. In contrast, the Accreditation Council for Graduate Medical Education has not yet released comparable statements or resources, and, if it did so, could play a critical role by integrating the disparate programming already underway within specialty training, and instigating the development and adoption of SGM programming in graduate medical education. Similarly, individual scholars and institutions have contributed to a collaborative pool of SGM educational and student support materials within the AAMC's MedEdPORTAL. The development of a similar, easily accessible reservoir of specialty-specific educational and support materials might be an important step in facilitating SGM programming and, thus, supporting SGM diversity across medical specialties.
In the present study, no association was found between SGM respondents' medical school climate and specialty prestige. However, many SM medical students describe their institution as “noninclusive” or “homophobic.”6,50 Structural factors, such as institutional climate, have been shown to influence important decisions among SGM, including those regarding health behaviors and expenditures.51–56 Given the demonstrated influence of structural factors, our findings merit further study. In addition, the items used to evaluate climate were adapted for use with medical students from a scale originally designed and validated for use with undergraduate populations.6 A medical school-specific SGM climate assessment instrument would offer enhanced opportunities for future research in this area.
Perceptions of specialty and residency program inclusivity have previously been shown to influence SM specialty choice and ranking of residency programs.9–11 Our study confirms that SGM are more likely than non-SGM to consider their sexual orientation and gender identity as a strong influence on specialty choice. Thus, initiatives to encourage and sustain SGM diversity, particularly within prestigious specialties, may be particularly effective when specialty- or residency program-specific mentorship programs, publications, and other methods of medical student recruitment directly address nondiscrimination and SGM inclusion.
In our study, both SGM and non-SGM rated the following factors (in order) the most frequently as strong influences on specialty choice: fit with personality, interests, and skills; specialty content; role model influences; and work–life balance. These factors, in identical order, were also ranked the most frequently as strong influences on specialty choice by the ∼14,000 graduating medical students who completed the 2015 AAMC Medical School Graduation Questionnaire.17 Given the reported importance of SGM mentors to the professional development of SGM in healthcare23 and the consistency with which role models are identified as strong influences on specialty choice among medical students, it is surprising that exposure to SGM faculty as an SGM medical student did not predict specialty choice, operationalized as specialty prestige, in this study. In part, this finding may reflect the importance of the quality of exposure or interaction with SGM faculty, as opposed to the frequency of exposure to SGM faculty. This finding may also reflect the importance of other quantitative elements of interaction with SGM faculty, including the number of SGM faculty to whom a student is exposed and the duration of interaction.
Lack of recognition of SGM professional activities as “legitimate” and professional risks associated with visibility might discourage SGM in medicine from engaging with targeted SGM professional activities.23 Although medical students have called for more SGM role models and mentors,57 SGM in senior and leadership positions may continue to be discouraged from participating in SGM-related professional activities, particularly in light of their own training experiences during time periods in which anti-SGM bias and discrimination were explicit, and nonheterosexuality was considered a psychiatric disease.58,59 Further investigation is warranted to identify the qualitative aspects of interaction with SGM role models that may better promote and support SGM medical student entry into prestigious specialties.
The discrepancy between the prominence of role models as a strong influence on specialty choice among SGM and the lack of association between exposure to SGM role models and specialty choice may also reflect the importance of non-SGM professional role models for SGM medical students. By virtue of being a numeric minority in the general population and in medicine, considerably fewer SGM faculty compared with non-SGM faculty may be accessible to SGM medical students, particularly within specialties with disproportionately fewer SGM. Thus, effective support from non-SGM “allied” role models is likely critical to enhancing SGM diversity in prestigious specialties. Additional research on the best practices for non-SGM faculty working with SGM medical students is needed.
This study has several limitations. Its cross-sectional design does not allow causal inference. Longitudinal studies are needed to further evaluate associations between SGM identity, perceptions of SGM inclusion, and specialty prestige to establish temporal precedence of specialty perceptions when predicting ultimate specialty choice. As military, ophthalmology, and urology residency competitiveness are not included in the publicly available data that are used to develop the specialty prestige index, these residency options were excluded from analyses involving prestige. In addition, the small number of gender minority participants precluded SGM sub-group analyses. Lastly, despite our large, diverse sample representing more than 26 specialties, our survey method does not allow calculation of response rate. It is, therefore, possible that the survey response rate is low and that a biased subset of organizations disseminated the survey. The incorporation of SGM-specific assessments into representative surveys of medical students and practitioners may remedy these latter two problems. Such assessments will also provide critical, representative data about potential demographic differences between SGM and non-SGM that may also influence SGM entry into high prestige specialties, such as United States Medical Licensing Examination scores or research experiences.
Conclusion
This study provides the first evidence that objectively defined prestigious specialties are perceived as less inclusive by SGM and that SGM are less likely to train and practice in prestigious specialties. Further research is needed to enhance mentorship and other means of promoting SGM entry into prestigious specialties. Exposure to SGM reduces anti-SGM bias among non-SGM in medicine, such that supporting SGM diversity across medical specialties may constitute a powerful means by which to improve provider competency in serving SGM in the general population, thereby helping to ameliorate the substantial health disparities experienced by SGM.
Supplementary Material
Acknowledgments
The authors wish to thank the respondents of this study and the many organizations and individuals who disseminated the recruitment materials. In addition, the authors wish to thank the National Heart, Lung, and Blood Institute (NHLBI), which funded a stipend for NAS for the duration of this research project (T35HL007649-29).
Disclaimer
A preliminary subset of data described in this article was presented by NAS during a poster session at the 13th Annual American Medical Association Research Symposium at the 2015 Interim Meeting of the American Medical Association (November 13, 2015; Atlanta, GA).
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Meyer IH: Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychol Bull 2003;129:674–697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hatzenbuehler ML: How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychol Bull 2009;135:707–730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pachankis JE: The psychological implications of concealing a stigma: A cognitive-affective-behavioral model. Psychol Bull 2007;133:328–345 [DOI] [PubMed] [Google Scholar]
- 4.Pachankis JE, Goldfried MR, Ramrattan ME: Extension of the rejection sensitivity construct to the interpersonal functioning of gay men. J Consult Clin Psychol 2008;76:306–317 [DOI] [PubMed] [Google Scholar]
- 5.Przedworski JM, Dovidio JF, Hardeman RR, et al. : A comparison of the mental health and well-being of sexual minority and heterosexual first-year medical students: A report from the medical student CHANGE study. Acad Med 2015;90:652–659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lapinski J, Sexton P: Still in the closet: The invisible minority in medical education. BMC Med Educ 2014;14:171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brogan DJ, Frank E, Elon L, et al. : Harassment of lesbians as medical students and physicians. JAMA 1999;282:1290–1292 [DOI] [PubMed] [Google Scholar]
- 8.Eliason MJ, Dibble SL, Robertson PA: Lesbian, gay, bisexual, and transgender (LGBT) physicians' experiences in the workplace. J Homosex 2011;58:1355–1371 [DOI] [PubMed] [Google Scholar]
- 9.Merchant RC, Jongco AM, 3rd, Woodward L: Disclosure of sexual orientation by medical students and residency applicants. Acad Med 2005;80:786. [DOI] [PubMed] [Google Scholar]
- 10.Lee KP, Kelz RR, Dube B, Morris JB: Attitude and perceptions of the other underrepresented minority in surgery. J Surg Educ 2014;71:e47–e52 [DOI] [PubMed] [Google Scholar]
- 11.Oriel KA, Madlon-Kay DJ, Govaker D, Mersy DJ: Gay and lesbian physicians in training: Family practice program directors' attitudes and students' perceptions of bias. Fam Med 1996;28:720–725 [PubMed] [Google Scholar]
- 12.Peota C: Out: The climate has changed for gay and lesbian physicians. Minn Med 2013;96:10–13 [PubMed] [Google Scholar]
- 13.Tinmouth J, Hamwi G: The experience of gay and lesbian students in medical school. JAMA 1994;271:714–715 [DOI] [PubMed] [Google Scholar]
- 14.Risdon C, Cook D, Willms D: Gay and lesbian physicians in training: A qualitative study. CMAJ 2000;162:331–334 [PMC free article] [PubMed] [Google Scholar]
- 15.Smith DM, Mathews WC: Physicians' attitudes toward homosexuality and HIV: Survey of a California Medical Society-revisited (PATHH-II). J Homosex 2007;52:1–9 [DOI] [PubMed] [Google Scholar]
- 16.United States Census Bureau: Census Bureau regions and divisions with state FIPS codes. 2015. Available at www2.census.gov/geo/docs/maps-data/maps/reg_div.txt Accessed June18, 2015
- 17.Associaton of American Medical Colleges: Medical School Graduation Questionnaire: 2015 all schools summary report. 2015. Available at www.aamc.org/download/440552/data/2015gqallschoolssummaryreport.pdf Accessed August3, 2016
- 18.The National Resident Matching Program: Results and Data: 2015 main residency Match®. April, 2015. Washington, DC: National Resident Matching Program, 2015. Available at www.nrmp.org/wp-content/uploads/2015/05/Main-Match-Results-and-Data-2015_final.pdf Accessed August9, 2016 [Google Scholar]
- 19.Medical Group Management Association: MGMA physician compensation and production survey: 2013 report based on 2012 data. Englewood, CO: Medical Group Management Association, 2013. Available at www.mgma.com/industry-data/all-data-resources/survey-and-report-updates Accessed August9, 2016 [Google Scholar]
- 20.Chen JY, Heller MT: How competitive is the match for radiology residency? Present view and historical perspective. J Am Coll Radiol 2014;11:501–506 [DOI] [PubMed] [Google Scholar]
- 21.Beasley TM, Schumacker RE: Multiple regression approach to analyzing contingency tables: Post hoc and planned comparison procedures. J Experimental Educ 1995;64:79–93 [Google Scholar]
- 22.Brogan DJ, O'Hanlan KA, Elon L, Frank E: Health and professional characteristics of lesbian and heterosexual women physicians. J Am Med Womens Assoc 2003;58:10–19 [PubMed] [Google Scholar]
- 23.Sánchez NF, Rankin S, Callahan E, et al. : LGBT trainee and health professional perspectives on academic careers—Facilitators and challenges. LGBT Health 2015;2:346–356 [DOI] [PubMed] [Google Scholar]
- 24.Institute of Medicine (US) Committee on Lesbian, Gay, Bisexual, and Transgender Health Issues and Research Gaps and Opportunities: The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington (DC): National Academies Press (US), 2011 [PubMed] [Google Scholar]
- 25.Quinn GP, Sanchez JA, Sutton SK, et al. : Cancer and lesbian, gay, bisexual, transgender/transsexual, and queer/questioning (LGBTQ) populations. CA Cancer J Clin 2015;65:384–400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pinkerton KE, Harbaugh M, Han MK, et al. : Women and lung disease. Sex differences and global health disparities. Am J Respir Crit Care Med 2015;192:11–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.One Colorado Education Fund: Invisible: The state of LGBT health in Colorado. 2011. Available at www.one-colorado.org/wp-content/uploads/2012/01/OneColorado_HealthSurveyResults.pdf Accessed August3, 2016
- 28.Eliason MJ, Schope R: Does “don't ask don't tell” apply to health care? Lesbian, gay, and bisexual people's disclosure to health care providers. J Gay Lesbian Med Assoc 2001;5:125–134 [Google Scholar]
- 29.Lambda Legal: When health care isn't caring: Lambda legal's survey on discrimination against LGBT people and people living with HIV. New York: Lambda Legal, 2010. Available at www.lambdalegal.org/sites/default/files/publications/downloads/whcic-report_when-health-care-isnt-caring.pdf Accessed August3, 2016 [Google Scholar]
- 30.Grant JM, Mottet LA, Tanis J, et al. : Injustice at every turn: A report of the national transgender discrimination survey. Washington, DC: National Center for Transgender Equality and National Gay and Lesbian Task Force, 2011. Available at www.thetaskforce.org/static_html/downloads/reports/reports/ntds_full.pdf Accessed August3, 2016 [Google Scholar]
- 31.Klamen DL, Grossman LS, Kopacz DR: Medical student homophobia. J Homosex 1999;37:53–63 [DOI] [PubMed] [Google Scholar]
- 32.Li CC, Matthews AK, Aranda F, et al. : Predictors and consequences of negative patient-provider interactions among a sample of African American sexual minority women. LGBT Health 2015;2:140–146 [DOI] [PubMed] [Google Scholar]
- 33.Rankow EJ, Tessaro I: Cervical cancer risk and Papanicolaou screening in a sample of lesbian and bisexual women. J Fam Pract 1998;47:139–143 [PubMed] [Google Scholar]
- 34.Burke SE, Dovidio JF, Przedworski JM, et al. : Do contact and empathy mitigate bias against gay and lesbian people among heterosexual first-year medical students? A report from the medical student CHANGE study. Acad Med 2015;90:645–651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chaimowitz GA: Homophobia among psychiatric residents, family practice residents and psychiatric faculty. Can J Psychiatry 1991;36:206–209 [DOI] [PubMed] [Google Scholar]
- 36.Dunjic-Kostic B, Pantovic M, Vukovic V, et al. : Knowledge: A possible tool in shaping medical professionals' attitudes towards homosexuality. Psychiatria Danubina 2012;24:143–151 [PubMed] [Google Scholar]
- 37.Sanchez NF, Rabatin J, Sanchez JP, et al. : Medical students' ability to care for lesbian, gay, bisexual, and transgendered patients. Fam Med 2006;38:21–27 [PubMed] [Google Scholar]
- 38.Kopacz DR, Grossman LS, Klamen DL: Medical students and AIDS: Knowledge, attitudes and implications for education. Health Educ Res 1999;14:1–6 [DOI] [PubMed] [Google Scholar]
- 39.Ficarrotto TJ, Grade M, Bliwise N, Irish T: Predictors of medical and nursing students' levels of HIV-AIDS knowledge and their resistance to working with AIDS patients. Acad Med 1990;65:470–471 [DOI] [PubMed] [Google Scholar]
- 40.Kelley L, Chou CL, Dibble SL, Robertson PA: A critical intervention in lesbian, gay, bisexual, and transgender health: Knowledge and attitude outcomes among second-year medical students. Teach Learn Med 2008;20:248–253 [DOI] [PubMed] [Google Scholar]
- 41.Grabovac I, Abramovic M, Komlenovic G, et al. : Attitudes towards and knowledge about homosexuality among medical students in Zagreb. Collegium antropologicum 2014;38:39–45 [PubMed] [Google Scholar]
- 42.Sherman MD, Kauth MR, Shipherd JC, Street RL, Jr.: Provider beliefs and practices about assessing sexual orientation in two veterans health affairs hospitals. LGBT Health 2014;1:185–191 [DOI] [PubMed] [Google Scholar]
- 43.Ramos MM, Tellez CM, Palley, et al. : Attitudes of physicians practicing in New Mexico toward gay men and lesbians in the profession. Acad Med 1998;73:436–438 [DOI] [PubMed] [Google Scholar]
- 44.American Academy of Family Physicians: Family medicine residency curriculum guidelines. Available at www.aafp.org/medical-school-residency/program-directors/curriculum.html Accessed August3, 2016
- 45.Society of Teachers of Family Medicine: LGBT Health. Available at www.stfm.org/Groups/GroupPagesandDiscussionForums/LGBTHealth Accessed August3, 2016
- 46.American Osteopathic Association: American Osteopathic Association Urges Physicians to Improve the Quality of Care for LGBT Patients, End Fear of Health Care Discrimination. 2015. Available at www.osteopathic.org/inside-aoa/news-and-publications/media-center/2015-news-releases/Pages/5-13-aoa-urges-physicians-to-improve-the-quality-of-care-for-lgbt-patients-end-fear-of-health-care-discrimination.aspx Accessed August3, 2016
- 47.The Joint Commission: Advancing effective communication, cultural competence, and patient- and family-centered care for the lesbian, gay, bisexual, and transgender (LGBT) community: A field guide. Oak Brook, IL, 2011. Available at www.jointcommission.org/assets/1/18/LGBTFieldGuide.pdf Accessed August9, 2016 [Google Scholar]
- 48.Association of American Medical Colleges: Enhancing institutional diversity through inclusion of all sexual orientations and gender identities. May 2015. AAMC videos and resources. Washington, DC: Association of American Medical Colleges; Available at www.aamc.org/initiatives/diversity/431552/enhancinginstitutionaldiversitythroughinclusionofallsexualorien.html Accessed August9, 2016 [Google Scholar]
- 49.American Medical Association: AMA policies on LGBT issues. Available at www.ama-assn.org/ama/pub/about-ama/our-people/member-groups-sections/glbt-advisory-committee/ama-policy-regarding-sexual-orientation.page? Accessed August3, 2016
- 50.Dhaliwal JS, Crane LA, Valley MA, Lowenstein SR: Student perspectives on the diversity climate at a U.S. medical school: The need for a broader definition of diversity. BMC Res Notes 2013;6:154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hatzenbuehler ML, Pachankis JE, Wolff J: Religious climate and health risk behaviors in sexual minority youths: A population-based study. Am J Public Health 2012;102:657–663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pachankis JE, Hatzenbuehler ML, Starks TJ: The influence of structural stigma and rejection sensitivity on young sexual minority men's daily tobacco and alcohol use. Soc Sci Med 2014;103:67–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Coulter RW, Birkett M, Corliss HL, et al. : Associations between LGBTQ-affirmative school climate and adolescent drinking behaviors. Drug Alcohol Depend 2016;161:340–347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pachankis JE, Hatzenbuehler ML, Hickson F, et al. : Hidden from health: Structural stigma, sexual orientation concealment, and HIV across 38 countries in the European MSM Internet Survey. AIDS 2015;29:1239–1246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hatzenbuehler ML, Keyes KM, Hamilton A, Hasin DS: State-level tobacco environments and sexual orientation disparities in tobacco use and dependence in the USA. Tob Control 2014;23:e127–e132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hatzenbuehler ML, O'Cleirigh C, Grasso C, et al. : Effect of same-sex marriage laws on health care use and expenditures in sexual minority men: A quasi-natural experiment. Am J Public Health 2012;102:285–291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Townsend MH, Wallick MM, Cambre KM: Support services for homosexual students at U.S. medical schools. Acad Med 1991;66:361–363 [DOI] [PubMed] [Google Scholar]
- 58.Byne W: Forty years after the removal of homosexuality from the DSM: Well on the way but not there yet. LGBT Health 2014;1:67–69 [DOI] [PubMed] [Google Scholar]
- 59.Schuster MA: On being gay in medicine. Acad Pediatr 2012;12:75–78 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.