Abstract
Objective
Supportive behaviors (both instrumental and emotional) from spouses and close family members can impact the trajectory of older adults’ depressive symptoms. Interventions that target both the patient and support person may be more effective than interventions that target the patient only, in terms of alleviating mood symptoms in the identified patient. The purpose of this paper was to review the characteristics and findings of dyadic and family-oriented interventions for late-life mood disorders to determine if they are effective and beneficial.
Methods
Following PRISMA guidelines, we conducted a systematic review of reports in the literature on dyadic or family-oriented interventions for late-life mood disorders. We searched PubMed, OVID PsycINFO, and EMBASE for peer-reviewed journal articles in English through October 2014.
Results
We identified 13 articles, representing a total of 10 independent investigations. Identified studies focused on spouses and close family members as support persons. Effect sizes for dyadic interventions that treated major depressive disorder were, on average, moderately strong, while effect sizes for dyadic interventions that reduced depressive symptoms were generally small. We did not identify any dyadic studies that treated bipolar disorder.
Conclusions
This review showed that dyadic interventions are feasible and that these interventions can decrease symptomatology in individuals who have major depressive disorder. Research is needed to understand the relative efficacy of a dyadic approach over a single-target approach in treating depression.
Keywords: older adults, couples, mood disorders, interventions, systematic review
Late-life depression is relatively common, yet difficult to treat given the range of physical, emotional, and cognitive symptoms (Fiske et al., 2009). While the 12-month prevalence for depression in the general late-life community is 5% (Byers, Yaffe, Covinsky, Friedman, & Bruce, 2010), an estimated 6–9% of older adults in the primary-care setting meet criteria for major depressive disorder (MDD) (Gum et al., 2009). An estimated 19% of older adults suffer from clinically significant depressive symptoms (Cole and Dendukuri, 2004). Treatment of late-life depression often includes pharmacotherapy, psychotherapy (e.-g., cognitive-behavioral therapy, problem-solving therapy, interpersonal therapy, or supportive psychotherapy), or a combination of psychotherapy with pharmacological medications. While considered effective, these approaches have been shown to alleviate symptoms in about only two-thirds of older adults who receive protocolized treatment (Lavretsky et al., 2013). Treatment of depression may be improved by integrating spouses and family members into psychotherapy and pharmacotherapy treatment. Correlational research suggests that family members—particularly spouses/intimate partners—can impact the incidence, trajectory, and recurrence of older adults’ depressive symptoms (Miklowitz et al., 2003; Martire et al., 2008; Bolka et al., 2013; Teo et al., 2013). This effect is likely because older adults typically rely upon their spouse/intimate partner as their most important source of support when faced with a chronic medical condition (Fiske, 2006).
Late-life relationships and mental health
Theoretical models of interpersonal relationships suggest that one partner’s beliefs and behaviors will affect those of the other partner (Kelley and Thibaut, 1978; Meyler et al., 2007). Models of dyadic coping are prevalent in the fields of chronic disease and illness. They suggest that spouses share health stressors and actively engage in joint coping efforts (Berg and Upchurch, 2007). In the context of one partner experiencing depression, we might expect that a patient’s ability to adhere to a prescribed treatment plan would be influenced by their partner’s support, or lack thereof. Partner support could be informational, tangible, and/or emotional (Berg and Upchurch, 2007). Unfortunately, mood disorders like MDD and bipolar disorder may not be viewed as chronic diseases that require care or involvement from a support person. Correlational research shows that increased partner and/or family support may decrease the risks for depression (Teo et al., 2013), increase adherence to depression medication treatment (Bolka et al., 2013), improve treatment response (Martire et al., 2008), and decrease relapse (Miklowitz et al., 2003). Alternatively, lack of partner support—in the form of criticism and controlling behaviors (Thompson and Sobolew-Shubin, 1993; Martire et al., 2003) frequent couple conflict (Park and Unützer, 2014), burden associated with providing assistance (Martire et al., 2008) and poor family functioning (Keitner et al., 1995)—can independently increase older patients’ depressive symptomatology. Depression is also reciprocal in late life, meaning that depression in one partner increases the risk for depression in the other (Townsend et al., 2001).
Current study
Close relationships become increasingly salient to adults as they age (Socioemotional Selectivity Theory; Carstensen et al., 1999); therefore, dyadic treatment approaches may have an advantage over patient-focused approaches in treating mood disorders in the long term by considering not only the patient’s symptomatology but promoting effective support behaviors of the spouse or close family member. Numerous reviews have focused on the effects of antidepressants, psychotherapy, and alternative therapies (and moderators of these effects) for mood disorders. A recent review noted the importance of patients’ social support and social networks, and demonstrated that psychotherapy treatment for depression has a positive effect on patients’ perceived level of social support (Park et al., 2014). As these authors note, patient-level treatment outcomes may be able to be enhanced by improving patients’ social support and network. Yet no systematic review has focused on whether dyadic treatment approaches to late-life depression (and other mood disorders) are effective and beneficial. Dyadic and family-oriented approaches encompass psychotherapy interventions where both the patient and a spouse or close family member(s) are included in treatment.
The goal of this paper is to systematically review the findings of randomized controlled trials (RCTs) evaluating dyadic or family-oriented interventions for late-life mood disorders. We review studies that focused specifically on engaging both patients and spouses/family members in the treatment of depressive symptoms. Given both the prevalence of depression and the increased salience of close relationships during late life, we focus on interventions that included spouses, intimate partners, or close family members as support persons. We refer to individuals who were the main focus of the intervention as “patients” and their spouses, intimate partners, or close family members who were included in the intervention as “support persons.” For each study included in the review, we characterize the intervention groups and summarize the findings for both patients and their support persons.
Method
We followed Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Liberati et al., 2009).
Search strategy
We conducted literature searches in PubMed, Ovid PsycINFO, and EMBASE for English language RCTs evaluating dyadic or family-oriented psychological, psychosocial, or behavioral interventions for MDD, dysthymic disorder, BD, or depressive symptoms. The searches focused on peer-reviewed papers through October 2014 and on older adult populations where all patients were at least 60 years of age. The search strategy incorporated terms representing the three main concepts in this review: dyads; interventions; and depression/bipolar disorders. We tested and refined the initial search strategy in PubMed with subsequent translations into PsycINFO and EMBASE search languages. We used a combination of controlled vocabulary specific to each database supplemented by free-text searching in keywords and titles. Search techniques such as mapping, use of multiple search fields, sub-headings, and filters customized the strategy for implementation in each individual database. Searching the literature for dyadic relationships proved challenging. The relationship is not always expressed by the term “dyad,” but rather in the context of varied permutations of patient-family member or patient-partner relationship. Therefore, in order to express the concept of “dyads,” we included combinations of as many relevant keywords as possible to capture studies with reference to dyadic relationships. Subsequent to the electronic searches, we hand searched references listed in the selected articles.
Screening of articles
Inclusion criteria for this review were studies that (i) examined adults aged 60 years and older; (ii) used a randomized, controlled design; (iii) are psychologically, psychosocially, or behaviorally oriented in intervention content; (iv) focus on treating MDD, dysthymic disorder, bipolar disorder (BD), or depressive symptoms as their main outcome; and (v) include both the patient and support person in at least one arm of the intervention. Multicomponent interventions for which depression is not the prime focus, but one of several outcomes, were not included.
Data extraction and analysis
Data extracted included the study population, mean age of the patient and support person in each intervention group, content of the intervention, patient and support person outcomes assessed, and results including intervention effects on patients and intervention effects on support persons. We include both significant and non-significant findings in order to determine what did and did not appear to work. Because of the small number of studies and the heterogeneity of interventions, a meta-analysis was not considered informative. Results are presented descriptively, including risk-of-bias assessment and a measure of effect size to indicate the degree of association between intervention group exposure (versus control) and the depression outcome. Thus, we extracted or calculated r, the Pearson correlation coefficient. This effect size was chosen because it is a more multi-purpose measure than, for example, Cohen’s d, which assesses the association between a dichotomous (grouping factor) and a continuous outcome. The effect size, r, is mathematically interchangeable with d and can be used to indicate the association between intervention exposure and continuous, dichotomous, or ranked variables. This allows for greater ability to compare effect sizes across studies.
Results
Study characteristics
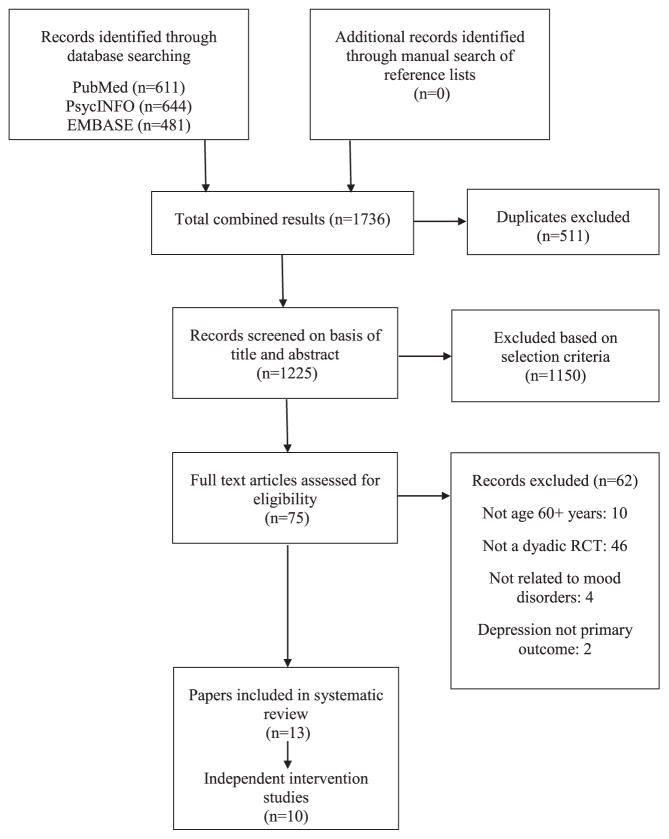
The literature searches yielded 1736 potentially relevant publications. After screening the title and abstracts of these publications, 1723 were excluded. Hand searches did not yield any new reports addressing our research question. Reasons for exclusion are shown in Figure 1. Most were excluded because they were not RCTs, did not report results related to mood disorders, or did not include both the patient and support person in an intervention arm.
Figure 1.
Summary of literature search process.
A total of 13 articles met inclusion criteria. These articles were based on 10 independent studies; three studies had two publications each, using the same sample but reporting different outcomes (Mittelman et al., 1995 & 2000; Joling et al., 2008 & 2012; Shimazu et al., 2011 & Shimodera et al., 2012). All studies were RCTs published in peer-reviewed journals; one study was a preliminary study of efficacy (Alexopoulos et al., 2012). All studies focused on treating MDD and/or alleviating depressive symptom burden. Our search did not locate any studies that focused on treating BD. Two studies focused on treating MDD only (Shimazu et al., 2011 & Shimodera et al., 2012; Teri et al. 1997); six studies focused on alleviating symptoms of depression only (Mittelman et al., 2000; 2004 & 2008; Eisdorfer et al., 2003; Wilz and Barskova, 2007; Gaugler et al., 2008), and two studies focused on both MDD and depressive symptoms (Joling et al., 2008, 2012; Alexopoulos et al., 2012). Studies were conducted in the USA (n = 8), Germany (Wilz and Barskova, 2007), Japan (Shimazu et al., 2011 & Shimodera et al., 2012), and the Netherlands (Joling et al., 2008, 2012). Table 1 shows a summary of study characteristics. All eligible articles are marked with an asterisk in the reference section.
Table 1.
Study characteristics
| No. of studies | |
|---|---|
| Mood disorder population | |
| Depressive symptoms | 6 |
| Major depressive disorder | 2 |
| Both of the above | 2 |
| Dyadic intervention contenta | |
| Psycho-education | 6 |
| Family counseling | 3 |
| Ecosystems therapy | 2 |
| Problem-solving therapy | 3 |
| Behavioral therapies | 2 |
| Marital therapy/partner support | 2 |
| Group(s) compared with dyadic intervention | |
| Treatment as usual | 10 |
| Patient only intervention | 0 |
| Support person included in intervention | |
| Close family member | 8 |
| Spouse | 2 |
| Patient outcomes assessed | |
| Disability | 4 |
| Incident mood disorder | 4 |
| Cognitive health | 4 |
| Physical health | 1 |
| Social support | 2 |
| Quality of life | 2 |
| Expressed emotion | 1 |
| Relapse-free days | 1 |
| Support person outcomes assessed | |
| Family/marital functioning | 3 |
| Mental health | 2 |
| Physical health | 2 |
| Cognitive health | 2 |
| Behavioral functioning | 2 |
| Disability | 1 |
Some studies included multiple areas of content.
All studies compared their dyadic intervention with usual medical care only. None of the studies compared a dyadic intervention with a single-target (i.e., patient-only) intervention. While depression was the main focus of all studies, a variety of secondary outcomes were assessed. They included disability (n = 4 studies), cognitive health (n = 4), and social support (n = 2), among others. Half of all studies assessed outcomes for support persons. The most common outcome assessed among support persons was marital or family functioning (n = 3 studies). Only one study assessed support persons’ mental health (Teri et al., 1997).
Participant characteristics
Sample sizes ranged from 24 to 406 participants. Patients were 70 years of age on average. Support persons’ age was only reported in five studies; their mean age was 69 years. More patients were women than men, and they were mostly White participants.
Participants were recruited primarily from general medical practices, psychiatry departments, rehabilitation centers, and memory clinics (i.e., individuals accompanying dementia patients to appointments). It is noteworthy that studies differed in how they identified potential study participants. In some investigations, any individual within a given setting was eligible. In others, individuals were identified because they held a specific social role (e.g., caregiver). For example, some studies included in this review focused on a class of individuals like caregivers to someone with dementia and then among that eligible population identified the depressed individuals for their intervention. These depressed individuals were cognitively intact, and their support persons were other, cognitively intact family members (i.e., the support persons were not the individuals with dementia). Our rationale for including all studies, no matter the mechanism by which study participants were identified, lies in the fact that all patients, across all of the studies, were reporting symptoms of depression for some reason. The reason may have both biologic and psychosocial components, the latter of which include social role responsibilities (e.g., spouse, friend, care-giver, and grandparent). We judged it critical to include all studies of patients and not selectively exclude a segment of those studies that more clearly recruited study participants based on risk or potential cause of depression (stemming from caregiver status, for example) compared with other studies that did not seek to characterize any such risk factors.
Patients’ depressive symptomatology varied greatly at baseline. In the six studies that focused on alleviating symptoms of depression, participants did not have to meet a certain level of symptomatology to enroll. Studies measured depression at baseline with the 20-item Center for Epidemiologic Studies Depression Scale (CES-D), Geriatric Depression Scale (GDS), or Beck Depression Inventory (BDI). In one study, 50% of patients had CES-D scores above 16 (indicating possible clinical depression) (Eisdorfer et al., 2003). Forty-three percent (Mittelman et al., 2004) and 68% (Mittelman et al., 1995; Mittelman, 2000) of patients had GDS scores above 11 (indicating possible clinical depression). In another study, a GDS mean of 9.7 (SD = 6.5) was reported (Gaugler et al., 2008). Nineteen percent of patients had BDI scores above 14 (indicating mild depression) (Mittelman et al., 2008), and a BDI mean of 10.3 (SD = 5.9) was reported in another study (Wilz and Barskova, 2007). In the four studies that focused on treating MDD, a clinical diagnosis of MDD was required at baseline.
Close family members were the most common type of dyads (e.g., patient + sibling [eight studies]) followed by married couples (e.g., patient + spouse [two studies]). A description of each paper including study sample, mean age of patients, main study outcome, and results for both patients and support persons is presented in Table 2.
Table 2.
Summary of dyadic and family-oriented RCTs to treat depression in older adults
| First author (year) country | Sample | Source(s) of recruitment | Mean age, in years | Intervention groups | Intervention duration | Main outcome | Between-group findings for patients | Between-group findings for support persons | Effect size (r)^ |
|---|---|---|---|---|---|---|---|---|---|
| Alexopoulos et al. (2012)a USA | 24 post-stroke depression patients and a close family member | rehabilitation hospital | patients: 70.8 ± 8.5 support persons: NR |
1) ecosystem focused therapy (EFT) 2) education on stroke and depression (ESD) |
3 months | remission of depression (Hamilton Depression Rating Scale <10) | EFT was more efficacious than ESD in reducing patients depressive symptoms, disability, and improving remission rates. EFT: pre HRSD = 20.4 (9.19); post HRSD = 8.2 (6.63) | No outcomes were reported. | 0.39 |
| Eisdorfer et al. (2003) USA | 225 patients and their spouses/family members | memory disorder clinics, primary care clinics, social service agencies, and physician offices. | patients: 68.5 ± 11.3 support persons: NR |
1) structural (family) ecosystems therapy (SET) 2) SET + Computer-telephone integrated system (CTIS) 3) minimal support control (MSC) |
12 months | depressive symptoms (Center for Epidemiological Studies Depression Scale) | Patients in the SET + CTIS experienced a decrease in depression relative to SET and MSC. | No outcomes were reported. | - |
| Gaugler et al. (2008) USA | 406 patients and an additional family member | NYU Aging and Dementia Research Center, local Alzheimer’s chapters | patients: 71.3 ± 9.1 support persons: NR |
1) individual and family counseling 2) usual care |
4 months | depressive symptoms (Geriatric Depression Scale) | Patients in the intervention group experienced significantly lower depression than those in usual care. | No outcomes were reported. | 0.06 |
| Joling et al. (2008, 2012) Netherlands | 192 depressed patients and an additional family member or friend | memory clinics, specialized mental health care clinics | patients: 69.5 ± 10.3 support persons: NR |
1) family meetings intervention 2) treatment as usual (TAU) |
12 months | 12-month incident depressive disorder (Mini International Neuropsychiatric Interview) | Compared with TAU, the family meetings intervention did not significantly reduce patients risk of developing a depressive disorder and did not reduce symptom burden (CESD change = 1.51). | No outcomes were reported. | 0.02 |
| Mittelman (1995, 2000) USA | 206 patients and an additional family member | ADRC, Alzheimer’s Association of NY, elderly day care centers | patients: 86% ≥60 support persons: NR |
1) individual and family counseling 2) treatment as usual (TAU) |
4 months | depressive symptoms (Geriatric Depression Scale) | Individual and family counseling significantly decreased patients depression, but not until 8 months post-treatment (GDS change = 0.03, SD = 4.56) | No outcomes were reported. | 0.19 |
| Mittelman et al. (2004) USA | 406 patients and an additional family member | ADRC, Alzheimer’s Association of NY, media announcements, referrals from physicians and social workers | patients: 71.3 ± 9.0 support persons: NR |
1) enhanced counseling and family support 2) usual care |
4 months | depressive symptoms (Geriatric Depression Scale) | Patients in the treatment group had fewer depressive symptoms (GDS change = −1.1, SD + 5.0) than control persons. These effects sustained for 3.1 years post-baseline. | No mental health outcomes were reported. | 0.15, 0.05 |
| Mittelman et al. (2008) USA, UK, and Australia | 158 patients and an additional family member | outpatient research clinics | patients: NR support persons: NR |
1) individual and family counseling + patient pharmacotherapy 2) patient pharmacotherapy |
4 months | depressive symptoms (Beck Depression Inventory) | Compared with the control group, individual and family counseling significantly decreased patients depression across 2 years. | No outcomes were reported. | 0.11 |
| Shimodera et al. (2012); Shimazu et al. (2011) | 57 depressed patients and their primary family member | Department of Psychiatry, affiliated hospital in Japan | patients: 60 ± 13.8 support persons: 60.4 ± 11.1 |
1) family psychoeducation (FS) 2) treatment as usual (TAU) |
2 months | time to relapse (in days) | The FS group experienced more relapse free days (272; SD = 7.1) compared with the TAU group (214; SD = 90.8). | No mental health outcomes were reported. | 0.41 |
| Teri (1997) USA | 72 depressed patients and their spouses | geriatric & family services clinic, the ADRC | patients: 76.4 ± 8.2 support persons: NR |
1) behavior therapy-pleasant events (BT-PE) 2) behavior therapy-problem solving (BT-PT) 3) typical care control (TCC) 4) waitlist control (WLC) |
9 weeks | depressive symptoms (Hamilton Depression Rating Scale; Cornell Scale for Depression in Dementia) | Patients in both BT-PE and BT-PT showed significant improvements in depressive symptoms compared with a control condition. BT-PE: HDRS change = −5.3 (4.0); BT-PT: HDRS change = 3.8 (2.3) | Support persons in both behavioral treatments showed significant improvements in depressive symptoms compared with those in a control condition. | 0.41 |
| Wilz and Barskova (2007) Germany | 124 patients and their spouses | rehabilitation centers | patients: 64.7 ± 9.6 support persons: 62.7 ± 10.0 |
1) cognitive behavioral group intervention 2) informational control 3) standard care control |
8 months | depressive symptoms (Beck Depression Inventory) | Patients in the intervention groups showed significant declines in depression (BDI compared to controls, but not until 6 months post-intervention. | No mental health outcomes were reported. | 0.33 |
MDD, major depressive disorder; ADRC, Alzheimer’s Disease Research Center; NR, not reported.
Pilot study and/or preliminary feasibility study.
Intervention characteristics
Dyadic interventions included a combination of psycho-education for both the patient and support person regarding depression symptom management and some form of psychotherapy where both members of the dyad were included, including problem solving therapy, behavioral activation therapy, ecosystems therapy (a specialized psychotherapy that helps patients learn problem-solving skills and make adjustments in their environment; Alexopoulos et al., 2012), family meetings (aimed to offer psycho-education teach problem solving techniques, and mobilize naturally existing family networks; Joling et al., 2008, 2012), and enhanced counseling (a strategy where counselors were continuously available over the course of the study; Mittelman et al., 2004). Another included the primary goal of the dyadic (family) psychotherapy sessions was to activate existing networks of support persons in order to increase the patient’s emotional and instrumental support. In addition to dyadic psychotherapy, many interventions also provided individual counseling/psychotherapy to the patient and support person separately. Intervention protocols ranged from 2 to 12 months in duration. None of the studies employed pharmacotherapy, either alone or in combination with psychotherapy. Intervention groups are presented in Table 2.
Intervention effects
Patients
Seven studies found a significant dyadic intervention effect on depression symptom levels post treatment (Alexopoulos et al., 2012; Eisdorfer et al., 2003; Gaugler et al., 2008; Mittelman et al., 2004; Mittelman et al., 2008; Shimodera et al., 2012; Teri et al., 1997); two studies found a significant dyadic intervention effect but not until 6–8 months post-treatment (Mittelman et al., 1995; Mittelman, 2000; Wilz and Barskova, 2007), and one study did not find a significant effect (Joling et al., 2008, 2012). The most common outcome variable was depressive symptom burden measured by the CES-D, BDI, GDS, or the Hamilton Rating Scale for Depression.
Compared with a control group, two studies that tested an ecosystems therapy decreased patients’ symptomatology (Eisdorfer et al., 2003) and improved remission rates in persons with MDD (Alexopoulos et al., 2012). In addition, a family psycho-educational intervention (Shimodera et al., 2012; Shimazu et al., 2011) increased the number of relapse free days in persons with MDD. Two studies that tested an individual + family counseling intervention decreased patients’ symptomatology (Gaugler et al., 2008), but one did not see an effect until 8 months post-intervention (Mittelman, 2000). One study of behavioral therapy did find a significant intervention effect on patients’ symptomatology (Teri, 1997), and another study of cognitive behavioral group therapy significantly improved patients’ symptomatology, but not until 6 months post-intervention (Wilz and Barskova, 2007). Two studies showed long-term intervention effects. Compared with treatment as usual, individual + family counseling significantly decreased patients’ symptomatology across 2 years (Mittelman et al., 2008) and 3 years post-baseline (Mittelman et al., 2004). The one study that did not find an intervention effect tested a family meetings intervention (Joling et al., 2008, 2012). Overall, small (r = 0.02) to medium (r = 0.41) effect sizes were calculated. Small effect sizes (r = 0.06–0.15) were calculated for studies that aimed to reduce depressive symptom burden. In treatment studies of MDD, medium effects were calculated (r = 0.39–0.41).
Support persons
Few studies collected health information on support persons’ outcomes. In the studies that did collect support person information, intervention effects on depression were not reported. Instead, support person variables were entered into regression models to examine their impact on patients’ symptomatology. One study reported the effects of their dyadic intervention on support persons’ depression and found a significant intervention effect (Teri et al., 1997). Studies did not provide enough data to calculate effect sizes for impact on support persons.
Potential sources of bias
It is important to report potential sources of bias in systematic reviews, as they may account for heterogeneity in intervention results (Cochrane Bias methods Group; Higgins et al., 2011). For this review, there was low risk of selection, performance, attrition, and reporting bias; it was unclear if there was risk of detection bias. There were no systematic differences in baseline characteristics between intervention groups and controls (selection bias). Participants and personnel were blinded to which intervention participants received (performance bias). Studies described reasons for attrition, cases excluded from analyses, and the total number of participants in each intervention group (attrition bias). The outcomes that were measured were reported in the results section; no outcomes were added, and no subgroup-only analyses were reported (reporting bias). It was unclear if interventionists/assessors were blinded to the outcomes measured (detection bias).
Discussion
We reviewed RCTs that evaluated a dyadic or family-oriented approach to the treatment of MDD or reduction of depressive symptom burden. We identified 13 papers, derived from 10 different studies. All studies examined the effects of a dyadic intervention on MDD or depressive symptomatology. We did not identify any papers that focused on dysthymia or BD. Seven of the 12 identified studies were published since 2005, highlighting the increased attention to this area. While this review shows that dyadic interventions are certainly feasible (attrition was low), we identified a small number of studies. There might not be many dyadic studies in older depressed populations because it is likely difficult to recruit and retain multiple members of a family unit, especially if additional personnel and resources are required. Older adults are also more likely to be widowed and are at greater risk of being socially isolated compared with other age groups, which makes identifying older adults and a close family member difficult. It would be useful for researchers to share effective and ineffective recruitment strategies in order to better identify and retain these dyads moving forward.
There is consistent evidence that a dyadic intervention is superior to a control arm in decreasing depressive symptoms among patients. Effect sizes were variable; however, several studies demonstrated significant effects (small to moderately strong) on depressive symptomatology despite differences in intervention content (problem solving therapy, behavioral activation, family therapy, among others). With respect to evidence-based treatments of MDD, pharmacotherapy and psychological therapy (that include a behavioral component) often report moderate to large effect sizes (Fiske et al., 2009). We calculated medium-effect sizes for dyadic interventions that targeted MDD and small effect sizes for dyadic interventions that reduced depressive symptom burden. Differences in effect sizes may be due to the large baseline differences in severity of depression scores. The studies that focused on MDD required a diagnosis at baseline, whereas studies that focused on depressive symptomatology included smaller proportions of patients with clinically significant levels of symptoms. More research is needed to determine whether support persons are better at facilitating treatment outcomes in individuals with MDD than individuals with subsyndromal depressive symptoms.
Suggestions for future research
Based upon our findings, we provide several suggestions for researchers to consider when testing the effects of a dyadic intervention on late-life depression.
Methodological considerations
Several design and measurement issues are noteworthy. First, the majority of studies compared their dyadic intervention with usual medical care only. A large body of correlational and survey research shows that support from spouses/family members can positively impact patients’ depressive symptomatology. Therefore, it is important to include an individual only condition to determine whether a dyadic intervention is more efficacious than a single-target intervention in terms of depression treatment. Other chronic illness fields have implemented this design feature and shown that dyadic interventions significantly impact patient functioning over patient-only interventions (for review, see Martire et al., 2010). These interventions have benefits beyond single-target interventions because they enhance spousal functioning including support behaviors. Another methodological consideration that needs to be addressed concerns the lack of support person assessments. Depression is reciprocal, so it is important to address whether there were any psychological benefits for the support person. Lack of patient progress may be explained by unexamined support person effects on the patient such as negative or controlling support behaviors (Martire et al., 2010). Similarly, few studies described possible mechanisms of change. It is possible that partner variables like emotional support or relationship quality are important moderators of treatment effects (Park et al., 2014). Finally, studies included patients with a range of depressive symptoms, possibly including those with low depression scores. All patients reported some level of depressive symptomatology, but not everyone met criteria (e.g., CES-D score >16) for clinically significant depressive symptoms. It is possible that authors believed any depression score was meaningful to reduce. However, the lack of an intervention effect could be attributed to including patients with low depression scores. Future studies should describe their reasons for inclusion and specify a desired range of depression scores at baseline.
Implications for treatment
There are several ways in which this review could inform dyadic depression intervention studies during late life. First, dyadic interventions need to be further developed in the mental health field and could first be explored as adjunctive therapy to proven methods. For example, cognitive behavioral therapy or problem-solving therapy could be adapted to include the patient’s support person. The support person could act as a “coach” who helps the patient initiate behavioral changes or solve problems. The components of the dyadic arm should be described in detail so that others know the steps for adapting a therapy for a patient-support person dyad. Second, investigators should reference a theoretical model that they used when developing their dyadic intervention. Ideally, a conceptually driven intervention would describe why a dyadic model of depression was chosen and would identify the target of change. Theoretical models could include social control models, marital and family systems frameworks, and stress and coping models. Finally, comparative effectiveness studies will be necessary as the field moves forward to determine which intervention is best for both the patient and support person.
Limitations of the review
Our findings should be considered in light of its limitations. First, we only reviewed published studies. It is possible that dyadic interventions that did not find significant treatment effects were never published. Second, we only focused on English-language reports. Third, we did not perform a quantitative analysis or assess the quality of the results reviewed. We believe that systematically describing the results of each study is informative as it allows researchers to become familiar with a range of relevant findings on late-life dyadic depression treatment.
Conclusions
Remarkably few dyadic intervention studies have been attempted to treat depression in older adults. This review showed that dyadic interventions are feasible and that including support persons significantly decreased patients’ depressive symptomatology. A dyadic effect was stronger in treatment studies of MDD than in studies that aimed to reduce depressive symptomatology. Additional research is needed to understand the relative efficacy of a dyadic approach over a single-target approach in treating depression. Given the profound physical, cognitive, and emotional effects of MDD, understanding the mechanisms by which inclusion of support persons leads to greater intervention effectiveness should be a high priority.
Acknowledgments
Preparation of this manuscript was supported in part by grants from NIH P30 MH090333, P60 MD000207, MHO19986, K01MH103467, KL2TR000146, K01NR 015101, and UL1 TR000005.
Footnotes
Conflicts of interest
Drs. Stahl, Rodakowski, Park, and Dew report no competing interests. Ms Saghafi also reports no competing interests. Dr. Reynolds reports receiving pharmaceutical support for NIH-sponsored research studies from Bristol-Myers Squibb, Forest, Pfizer, and Lilly; and serving on the American Association for Geriatric Psychiatry editorial review board. He has received an honorarium as a speaker from MedScape/WEB MD. He is the co-inventor (Licensed Intellectual Property) of Psychometric analysis of the Pittsburgh Sleep Quality Index (PSQI) PRO10050447 (PI: Buysse).
References
- *.Alexopoulos GS, Wilkins V, Marino P, et al. Ecosystem focused therapy in post-stroke depression: a preliminary study. Int J Geriatr Psychiatry. 2012;27:1053–1060. doi: 10.1002/gps.2822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg CA, Upchurch R. A developmental-contextual model of couples coping with chronic illness across the adult life span. Psych Bulletin. 2007;133:920–954. doi: 10.1037/0033-2909.133.6.920. [DOI] [PubMed] [Google Scholar]
- Bolka CR, Bonner LM, Campbell DG, et al. Family involvement, medication adherence, and depression outcomes among patients in veterans affairs primary care. Psychiatric Serv. 2013;64:472–478. doi: 10.1176/appi.ps.201200160. [DOI] [PubMed] [Google Scholar]
- Byers AL, Yaffee K, Covinsky KE, Friedman MB, Bruce High cooccurance of mood and anxiety disorders among older adults: the national comorbidity study replication. Arch Gen Psychiatry. 2010;67:489–496. doi: 10.1001/archgenpsychiatry.2010.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carstensen LL, Isaacowitz D, Charles ST. Taking time seriously: a theory of socioemotional selectivity. Am Psychologist. 1999;54:165–181. doi: 10.1037//0003-066x.54.3.165. [DOI] [PubMed] [Google Scholar]
- *.Eisdorfer C, Czaja SJ, Loewenstein DA, et al. The effect of a family therapy and technology-based intervention on caregiver depression. Gerontologist. 2003;43:521–531. doi: 10.1093/geront/43.4.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiske A. The nature of depression in later life. In: Qualls S, Knight B, editors. Psychotherapy for Depression in Older Adults. John Wiley & Sons; Hoboken, NJ: 2006. pp. 29–44. [Google Scholar]
- Fiske A, Wetherell JL, Gatz M. Depression in older adults. Ann Review Clin Psych. 2009;5:363–389. doi: 10.1146/annurev.clinpsy.032408.153621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Gaugler JE, Roth D, Haley WE, Mittelman MS. Can counseling and support reduce Alzheimer’s caregivers’ burden and depressive symptoms during the transition to institutionalization? Results from the NYU caregiver intervention study. J Am Geriatric Soc. 2008;56:421–428. doi: 10.1111/j.1532-5415.2007.01593.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gum AM, King-Kallimanis B, Kohn R. Prevalence of mood, anxiety, and substance-abuse disorders for older Americans in the National Comorbidity Survey-Replication. Am J Geriatr Psychiatry. 2009;17:769–781. doi: 10.1097/JGP.0b013e3181ad4f5a. [DOI] [PubMed] [Google Scholar]
- Higgins JPT, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeksm L, Sterne JAC the Cochran Bias Methods Group. The Cochrane Collaboration’s tool for assessing risk of bias in randomized trials. Brit Med J. 2011;11:343–351. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Joling KJ, van Hout HPJ, Scheltens P, et al. Cost-effectiveness of family meetings on indicated prevention of anxiety and depressive symptoms and disorders of primary family caregivers of patients with dementia: design of a randomized controlled trial. BMC Geriatr. 2008;8 doi: 10.1186/1471-2318-8-2. open access. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Joling KJ, van Marwijk HWJ, Smit F, et al. Does a family meetings intervention prevent depression and anxiety in family caregivers of dementia patients? A randomized trial. PLoS One. 2012;7(1):e30936. doi: 10.1371/journal.pone.0030936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keitner GI, Ryan CE, Miller IW, et al. Role of the family in recovery and major depression. Am J Psychiatry. 1995;152:1002–1008. doi: 10.1176/ajp.152.7.1002. [DOI] [PubMed] [Google Scholar]
- Kelley HH, Thibaut JW. Interpersonal Relations: A Theory of Interdependence. Wiley-Interscience; New York: 1978. [Google Scholar]
- Lavretsky H, Sajatovic M, Reynolds CF. Late-life Mood Disorders. Oxford University Press; New York, New York: 2013. [Google Scholar]
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Int Med. 2009;151:65–94. doi: 10.7326/0003-4819-151-4-200908180-00136. [DOI] [PubMed] [Google Scholar]
- Martire LM, Schulz R, Helgeson VS, Small BJ, Saghafi EM. Review and meta-analysis of couple-oriented interventions for chronic illness. Ann Beh Med. 2010;40:325–342. doi: 10.1007/s12160-010-9216-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martire LM, Schulz R, Reynolds CF, et al. Impact of close family members on older adults’ early response to depression treatment. Psyc Aging. 2008;23:447–452. doi: 10.1037/0882-7974.23.2.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martire LM, Schulz R, Wrosch C, Newsom JT. Perceptions and implications of received spousal care: evidence from the Caregiver Health Effects Study. Psyc Aging. 2003;18:593–601. doi: 10.1037/0882-7974.18.3.593. [DOI] [PubMed] [Google Scholar]
- Meyler D, Stimpson JP, Peek MK. Health concordance within couples: a systematic review. Soc Sci Med. 2007;64:2297–2310. doi: 10.1016/j.socscimed.2007.02.007. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, George EL, Richards JA, Simoneau TL, Suddath RL. A randomized study of family-focused psychoeducation and pharmacotherapy in the outpatient management of bipolar disorder. Archiv Gen Psychiatry. 2003;60:904–912. doi: 10.1001/archpsyc.60.9.904. [DOI] [PubMed] [Google Scholar]
- *.Mittelman MS, Ferris SH, Shulman E, et al. A comprehensive support program: effect on depression in spouse-caregivers of AD patients. Gerontologist. 1995;35:792–802. doi: 10.1093/geront/35.6.792. [DOI] [PubMed] [Google Scholar]
- *.Mittelman MS. Effect of support and counseling on caregivers of patients with Alzheimer’s disease. Intrnl Psychogeriatr. 2000;23:341–346. [Google Scholar]
- *.Mittelman MS, Roth DL, Coon DW, Haley WE. Sustained benefit of supportive intervention for depressive symptoms in caregivers of patients with Alzheimer’s disease. Am J Psychiatry. 2004;161:850–856. doi: 10.1176/appi.ajp.161.5.850. [DOI] [PubMed] [Google Scholar]
- *.Mittelman MS, Brodaty H, Wallen AS, Burns A. A three-country randomized controlled trial of a psychosocial intervention for caregivers combined with pharmacological treatment for patients with Alzheimer disease: effects on caregiver depression. Am J Geriatr Psychiatry. 2008;16:893–903. doi: 10.1097/JGP.0b013e3181898095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park M, Cuijpers P, van Straten A, Reynolds CF. The effects of psychotherapy for adult depression on social support: a meta-analysis. Cog Ther Res. 2014 doi: 10.1007/s10608-014-9630-z. ePub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park M, Unützer J. Hundred forty eight more days with depression: the association between marital conflict and depression-free days. Internat J of Geriatr Psychiatry. 2014;29:1271–1277. doi: 10.1002/gps.4107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Shimazu K, Shumodera S, Mino Y, et al. Family psychoeducation for major depression: randomised controlled trial. Brit J Psychiatry. 2011;198:385–390. doi: 10.1192/bjp.bp.110.078626. [DOI] [PubMed] [Google Scholar]
- *.Shimodera S, Furukawa TA, Mino Y, et al. Cost-effectiveness of family psychoeducation to prevent relapse in major depression: results from a randomized controlled trial. BMC Psychiatry. 2012;12:40–46. doi: 10.1186/1471-244X-12-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teo A, Choi H, Valenstein M. Social relationships and depression: ten-year follow-up from a nationally representative study. PLoS One. 2013:30. doi: 10.1371/journal.pone.0062396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teri L, Logsdon RG, Uomoto J, Mcurry SM. Behavioral treatment of depression in dementia patients: a controlled clinical trial. J Gerontol B Psychol Sci Soc Sci. 1997;52:159–166. doi: 10.1093/geronb/52b.4.p159. [DOI] [PubMed] [Google Scholar]
- Thompson SC, Sobolew-Shubin A. Overprotective relationships: a nonsupportive side of social networks. Basic Appl Soc Psych. 1993;14:363–383. [Google Scholar]
- Townsend AL, Miller B, Guo S. Depressive symptomatology in middle-aged and older married couples a dyadic analysis. J Gerontology: Psych Sci Soc Sci. 2001;56:352–S364. doi: 10.1093/geronb/56.6.s352. [DOI] [PubMed] [Google Scholar]
- *.Wilz G, Barskova T. Evaluation of a cognitive behavioral group intervention program for spouses of stroke patients. Behav Res Ther. 2007;45:2508–2517. doi: 10.1016/j.brat.2007.04.010. [DOI] [PubMed] [Google Scholar]