Abstract
Purpose
The current investigation sought to illustrate the etiology of adverse alcohol consequences in young adult veterans using a path analytic framework.
Methods
A total of 312 veterans aged 19–34 were enrolled in a larger intervention study on alcohol use. At baseline, participants completed measures of combat severity, PTSD symptom severity, and drinking motives to cope. At one month follow-up, participants completed measures of perceived stigma of behavioral health treatment seeking and past 30-day alcohol consequences.
Results
After entering the covariates of age, gender, race/ethnicity, and past year behavioral health treatment utilization, a path analytic model demonstrated a good fit to the data predicting alcohol consequences in this population. Further, a separate exploratory analysis confirmed that both drinking motives to cope and perceived stigma of behavioral health treatment seeking mediated the link between PTSD symptom severity and alcohol consequences.
Conclusions
The current model expands upon prior research showing the relationship between combat severity and alcohol use behavior in young adult veterans. Results support the notion that veterans with PTSD symptoms may drink to cope and that perceived stigma surrounding help seeking may further contribute to alcohol related problems.
Keywords: Veterans, PTSD, Coping Motives, Alcohol Consequences, Path Analysis, Mediation
1. Introduction
1.1 Problem Drinking Among Young Adult Veterans
American veterans returning home after service face a number of challenges as they attempt to reintegrate into civilian life, not the least of which involves coping with any combat related trauma they may have endured. The literature on returning veterans suggests that between 5% and 22% of returning veterans report symptoms that would effectually screen them positive for posttraumatic stress disorder (PTSD) (Bray et al., 2010; Schumm & Chard, 2012; Wisco et al., 2014). Further, there is a growing body of evidence that links PTSD with heavy drinking and related alcohol use disorder (AUD) in younger veterans of the conflicts in Iraq and Afghanistan (Jacobson et al., 2008; Larson, Wooten, Adams, & Merrick, 2012; Seal et al., 2011). Several environmental and psychosocial variables in addition to PTSD have been posited to explain the prevalence of heavy drinking in young adult veterans including (but not limited to): combat exposure, drinking motives, and perceived stigma (Dixon, Leen-Feldner, Ham, Feldner, & Lewis, 2009; Wright, Foran, Wood, Eckford, & McGurk, 2012). The current investigation begins with an overview of common factors linked to heavy alcohol use in veterans then expands on the existing literature by illustrating how the link between combat exposure and PTSD symptoms can lead to alcohol problems via the dual pathways of coping drinking motives and perceived stigma of treatment seeking.
1.2 Combat Exposure and PTSD
A nationally representative survey of recent US veterans found that combat related trauma was linked to PTSD in this population (Wisco et al., 2014). A meta-analytic review of risk factors for combat-related PTSD found that increased combat exposure and other severity indicators (e.g. witnessing a death) led to a greater likelihood of developing PTSD (Xue et al., 2015). Although some studies have found that potential genetic factors combine with the level of combat exposure to predict PTSD manifestation in veterans (e.g. Kimbrel et al., 2015), a longitudinal twin study of Vietnam era veterans found that the majority of PTSD related symptoms reported by combat veterans are most likely attributable solely to their combat experience (Gilbertson et al., 2010). In addition to the evidence linking combat exposure to PTSD, there is also strong evidence to suggest that combat exposure and PTSD are both linked to higher rates of alcohol use and problems in veterans (e.g., Godfrey et al., 2015; Hahn, Tirabassi, Simons, & Simons, 2015). Moreover, although US female veterans are not typically assigned combat roles, some are nonetheless exposed to combat and therefore are just as likely to evince the same link between heavy alcohol use and PTSD (Creech, Swift, Zlotnick, Taft, & Street, 2016).
1.3 Coping Drinking Motives
The connection between PTSD and drinking behavior has been explained in part by research on drinking motives, specifically “drinking to cope” (Lehavot, Stappenbeck, Luterek, Kaysen, & Simpson, 2014). Research on drinking motives has shown that individuals use alcohol as a means to regulate their emotions (Cooper, Frone, Russell, & Mudar, 1995) and that for some, drinking to regulate negative affect serves as a means to cope in lieu of more adaptive emotional strategies, such as engaging in goal-directed behavior (Veilleux, Skinner, Reese, & Shaver, 2014). Research, particularly in college students, supports the assertion that some young adults drink to regulate their mood. For example, researchers found that daytime negative affect predicted subsequent drinking later that night (Dvorak, Pearson, & Day, 2014), while others found that more frequent changes in mood, specifically negative moods, predicted higher general levels of drinking to cope (Gottfredson & Hussong, 2013). Drinking to cope may reinforce the belief that alcohol is effective for regulating negative affect which can further contribute to the development of an AUD (Rousseau, Irons, & Correia, 2011).
Coping motives for drinking (e.g., drinking to reduce tension, drinking to deal with problems) appear to be qualitatively different from other drinking motives, such as social motives related to drinking with friends or during celebrations, or conformity motives related to wanting to fit in with others who are drinking. Specifically, drinking to cope has been consistently linked to alcohol related problems among young people (Carey & Correia, 1997; Merrill & Read, 2010; Rafnsson, Jonsson, & Windle, 2006). Further, longitudinal work has linked drinking to cope with the subsequent development of an AUD (Carpenter & Hasin, 1998). Evidence for the complete pathway between negative affect, coping drinking motives, and alcohol related problems is strong for college students (Martens et al.,2008), adults in the community (Carpenter & Hasin, 1999), and heavy drinking veterans with and without diagnosed PTSD (McDevitt-Murphy, Fields, Monahan, & Bracken, 2015).
1.4 Help Seeking Stigma
Concurrently with the relationship between PTSD symptomatology and drinking motives to cope, there is the added concern of stigmatization of help seeking which is particularly prevalent in military populations (Gorman, Blow, Ames, & Reed; 2011; Kulesza, Pedersen, Corrigan, & Marshall, 2015). Exacerbating this problem is the evidence which shows that those combat veterans suffering from PTSD (i.e. those likely in need of treatment) are the most likely to perceive stigma for seeking help, such as the belief others would view them as weak if they sought care (Hoge et al., 2004), and are therefore less likely to seek help (Kim, Thomas, Wilk, Castro, & Hoge, 2010). Further, there is recent evidence to suggest that not only is the presence of a mental health or substance use disorder predictive of stigmatizing beliefs, but that such beliefs are in turn related to alcohol problems (Jones, Keeling, Thandi, & Greenberg, 2015). This corresponds with research showing that people with comorbid AUD and mood disorders (e.g., depression) perceived greater stigma towards people who have an AUD (Glass, Williams, Bucholz, 2014). Further, in a sample of active duty military personnel, researchers found a dynamic interplay between PTSD, perceived stress, AUD, and help seeking stigma such that perceived stigma moderated the relationship between stress (strongly correlated with PTSD) and AUD (De La Rosa, Delaney, Webb-Murphy, & Johnston, 2015). Perceived stigma of help seeking is particularly complicated for young military populations; for example, by choosing to seek help, Army soldiers reported this could not only be seen by peers as a sign of weakness, but there is a perception that by choosing care, one is voluntarily leaving their unit, which could harm the unit in terms of readiness and productivity (Gibbs, Rae Olmsted, Brown, & Clinton-Sherrod, 2011).
1.6 Current Study
The current investigation builds off of previous research on the relationship between PTSD and problem drinking in military veterans. The primary aim of the current study is to test the hypothesis that adverse alcohol consequences in young adult veterans can be predicted using a path analytic framework incorporating combat exposure, PTSD symptomatology, drinking motives to cope, and perceived stigma of treatment seeking. A secondary aim is to test the dual hypotheses that both drinking motives to cope and perceived stigma of treatment seeking mediate the relationship between evinced PTSD symptoms and adverse alcohol consequences.
2. Methods
2.1 Participants and Procedures
Participants were recruited as part of a larger longitudinal study to test an online alcohol intervention for young adult veterans (Pedersen, Marshall, Schell, & Neighbors, 2016; Pedersen, Parast, Marshall, Schell, & Neighbors, 2016). The intervention group received feedback to correct their misperceptions of veteran peers’ drinking behavior. An attention control group received feedback about the video game playing behavior of their veteran peers. Participants were recruited using a novel framework employing Facebook to reach veterans that might otherwise be missed by traditional outreach efforts. Initially, 2312 individuals clicked on Facebook links advertising the study, of which 1177 completed a screening questionnaire and signed a consent form. Participants were eligible if they were aged 18–34, a veteran from the Air Force, Army, Marine Corps, or Navy, and screened on the AUDIT (Saunders, Aasland, Babor, de la Fuente, & Grant, 1993) a minimum threshold score of “4” or greater for men and “3” or greater for women. The study utilized a screening protocol designed to validate participants’ status as a veteran, such as use of validation checks to ensure items on time of service, rank, pay grade, and branch of service matched for consistency (see Pedersen, Naranjo, & Marshall, 2016). After screening, the total sample for the larger study was 783. The analytic sample for the current investigation only included the participants who did not receive the intervention in the larger study (N =312).
2.2 Measures
Time 1 Measurement
Combat Exposure Scale
Combat exposure was assessed using an 11-item scale (Schell & Marshall, 2008) with items on whether or not participants experienced combat events (Yes/No). Example items included, “Having a friend who was seriously wounded or killed,” and “Being injured, requiring hospitalization.” Scores ranged from 0 to 11, with higher scores indicated a greater degree of combat severity. Scores of “0” on the scale were imputed for 35 participants who indicated they were not deployed during their service.
Posttraumatic Stress Disorder (PCL-5)
PTSD symptoms were assessed using the 20-item PCL-5 checklist (PCL-5; Botvin et al., 2015; Weathers et al., 2013). The PCL-5 asks participants to indicate the degree to which they were bothered by each of the DSM-5 PTSD symptoms in the past month using a 5-point scale ranging from “Not at all” to “Extremely.”
Drinking Motives Questionnaire
Coping drinking motives were assessed using 5-item coping subscale from the Drinking Motives Questionnaire (DMQ; Cooper, 1994). Asked to think of all the times they drink, participants indicate the frequency with which they drink for the coping reasons (e.g. “To forget about your problems”) on a 5-point scale from 1-”Almost never/never” to 5-”Almost always/always.” The “coping” subscale has been shown to be a statistically valid and reliable component of the DMQ (Kuntsche, Knibbe, Gmel, Engels, 2006).
Covariates: Demographics and Treatment Receipt
We assessed each participant with regard to their age, gender, and race/ethnicity. In addition, we asked participants to indicate whether or not they had received behavioral health treatment in the past year (i.e., attended an appointment for a mental health concern, an alcohol use concern, or a substance use concern). A “yes” answer to care for any of the three concerns constituted having received behavioral health services in the past year.
Time 2 One Month Follow-Up Measurement
Perceived Stigma of Behavioral Health Treatment Seeking
Perceived public stigma of seeking behavioral health treatment was assessed using a 6-item scale developed by Britt and colleagues (Britt, 2000; Britt et al., 2008). The scale asks participants to indicate the extent to which various stigma concerns might influence their decision to seek treatment for a psychological problem (i.e., a stress or emotional problem such as depression, anxiety attacks, or substance use concerns). Answers were provided on a 4-point scale ranging from “strongly disagree” to “strongly agree” (e.g., “I would be seen as weak”). This scale has been used in active duty military and veteran samples and has shown a high degree of reliability and validity (e.g. Hoge et al., 2004; Kulesza et al., 2015).
Brief Young Adult Alcohol Consequences Questionnaire (B-YAACQ)
The B-YAACQ (Kahler, Strong, & Read, 2005) was used to assess past month drinking consequences. The B-YAACQ is a 24-item measure that asks (Yes/No) how many adverse consequences participants attributed to their drinking in the past 30 days, e.g., “I often have ended up drinking on nights when I had planned not to drink.” The B-YAACQ has shown good psychometric validity as a measure of problem drinking (Kahler, Hustad, Barnett, Strong, & Borsari, 2008), a behavior of particular concern among young adult veterans.
2.3 Data Analysis
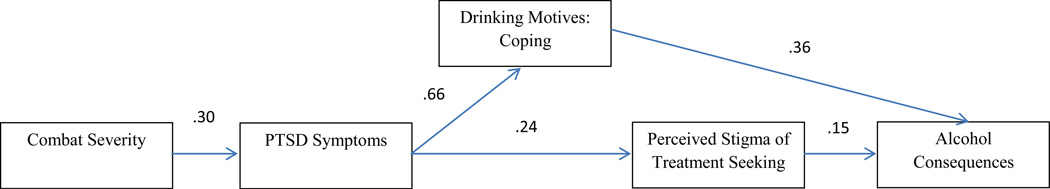
Data were analyzed using SPSS v.24. Descriptive statistics were calculated for the covariates of age, gender, race/ethnicity, and behavioral health treatment seeking in the past year. Descriptive statistics were also calculated for the five core variables of the path analysis model: Combat severity, PTSD symptom severity, coping drinking motives, perceived public stigma of treatment seeking, and alcohol consequences. Bivariate correlations were also calculated for all of the variables (including covariates). The path analysis model was tested using AMOS v.24. In addition to the unidirectional paths seen in Figure 1, all covariates were regressed onto all of the endogenous variables and correlated with combat severity and each other as was coping drinking motives with perceived public stigma. A maximum likelihood model estimating means and intercepts was used to test model fit. Standardized estimates for all paths were calculated and are reported with fit indices for the default model. Finally, an exploratory mediation analysis was conducted using the PROCESS package for SPSS v.2.15 (Hayes, 2013).
Figure 1.
Path analysis with standardized estimates of the hypothesized link between combat severity and alcohol consequences.
3. Results
3.1 Demographics and Bivariate Correlations
Table 1 contains demographic information about the sample. Each of the measures used to assess combat severity (α =.78), PTSD (α =.97), drinking motives: coping (α =.90), perceived treatment seeking stigma (α =.91), and alcohol consequences (α =.95) demonstrated good to excellent internal consistency. Preliminary analyses revealed significant correlations among all five of the proposed model variables. In addition, significant correlations were observed for some of the proposed covariates (see Table 1). In the subsequent test of the proposed model, all of the covariates were included in the final analysis.
Table 1.
Bivariate correlations among model variables and covariates.
| Mean | S.D. | Age | Gender | Ethnicity | Past Year Behavioral Health Treatment |
Combat Severity |
PTSD Symptoms |
DMQ: Coping |
Perceived Stigma of Treatment Seeking |
Alcohol Consequences | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | 28.87 | 3.42 | - | .00 | −.11* | .06 | .23** | .05 | −.03 | .00 | −.05 |
| Gender | Male (80%) Female (20%) |
- | .22** | .04 | −.29** | .04 | −.01 | .08 | −.09 | ||
| Race/ethnicity | White (84%) Non-White (16%) |
- | .01 | −.03 | −.01 | −.02 | .04 | .04 | |||
| Past Year Behavioral Health Treatment |
Yes (43%) No (57%) |
- | .19** | .43** | .25** | .02 | .14* | ||||
| Combat Severity | 15.01 | 3.12 | - | .32** | .20** | .19** | .16** | ||||
| PTSD Symptoms | 29.68 | 23.17 | - | .64** | .19** | .26** | |||||
| DMQ: Coping | 2.56 | 1.20 | - | .21** | .41** | ||||||
| Perceived Stigma of Treatment Seeking |
2.29 | 1.14 | - | .22** | |||||||
| Alcohol Consequences |
5.28 | 6.31 | - |
Note: All variables were measured at T1, except for Perceived Stigma of Treatment Seeking and Alcohol Consequences which were measured at T2. Gender was coded 0 = “Male” and 1 = “Female.” Race was coded 0 = “White”, 1 = “Non-White.” Past Year Behavioral Health Treatment was coded 0 = “No treatment” and 1 = “Any treatment.” DMQ=Drinking Motives Questionnaire, PTSD=Posttraumatic Stress Disorder.
p < .01
3.2 Path Analysis
A path analysis was conducted to test the hypothesized linkages between combat severity, PTSD symptom severity, coping drinking motives, perceived public stigma of treatment seeking, and alcohol consequences. The hypothesized measurement model fit the data well in accordance with recommended fit indices in the literature (Barrett, 2007; Hu & Bentler, 1999). Fit indices for the default model were as follows: χ2 =11.952, df =4; p = 018; CMIN/df =2.988; CFI = 981; RMSEA = 080, C.I. [.03 −.13]; SRMR = .025. The standardized estimates for each path in the model are reported in Figure 1. Further, this model controlled for the covariates of age, gender, ethnicity, and any use of behavioral health treatment services in the past year. Standardized estimates for use of any behavioral health treatment services in the past year were significant for PTSD symptoms (β =.37, p <001) and perceived public stigma (β = −.12, p = .046), such that those who had received any treatment reported both greater PTSD symptom severity and less stigma about seeking care. In addition, standardized estimates for gender were significant for PTSD symptom severity (β = .12, p < .05) and alcohol consequences (β = −.11, p < .05), such that men reported greater PTSD symptom severity at Time 1 but fewer alcohol consequences at Time 2. Neither age nor ethnicity yielded significant standardized estimates for any of the endogenous variables. Of note in the model was the relatively strong relationship between PTSD and drinking to cope at baseline. Also, PTSD symptom severity at baseline was predictive of perceived stigma one month later, while drinking to cope was also significantly predictive of alcohol consequences at follow-up.
3.3 Mediation
Mediation analyses tested the hypotheses that drinking motives coping and perceived stigma of treatment seeking mediate the relationship between PTSD symptoms and alcohol consequences. A multiple mediation model with a 1,000 iteration bootstrap procedure, provided support for both hypotheses. That is, both drinking to cope (Point Estimate = .0677, S.E. = .0145, C.I. [.0412−.0989]) and perceived public stigma (Point Estimate = .0105, S.E. = .0050, C.I. [.0030−.0241]) mediated the relationship between PTSD symptoms and alcohol consequences. This finding indicates that veterans with greater PTSD symptom severity were both more likely to drink alcohol to cope with negative affect and to view stigma as interfering with the likelihood of seeking treatment. Further, both perceived stigma and drinking to cope were predictive of experiencing a higher number of alcohol consequences for veterans with greater PTSD symptom severity.
4. Discussion
This study examined the associations of combat severity and PTSD symptoms with adverse alcohol consequences, and tested hypotheses regarding the roles of drinking to cope and perceived stigma regarding help-seeking as mediators of said relationship. Overall, this model provided a good explanation of the data. Specifically, main effects were found for the relationship between combat severity and PTSD symptom severity, between PTSD symptom severity and both drinking motives to cope and perceived stigma of treatment seeking, and for drinking motives to cope and perceived stigma of treatment seeking on adverse alcohol consequences. Additionally, indirect effects via mediating pathways were found from PTSD symptom severity to alcohol consequences through drinking motives to cope and perceived stigma of treatment seeking. Taken as a whole, these findings suggest that both drinking to cope and perceived stigma serve to explain the well-established link (see Larson et al., 2012) between PTSD and alcohol consequences in this population.
Although various studies have established a connection between combat severity, PTSD, and alcohol use (e.g. Ramchand et al., 2011; Seal et al., 2011), few have explored the mediating role of coping motives to deal with PTSD symptoms (e.g. McDevitt-Murphy et al., 2015). The results of the current study reveal that the link between PTSD symptoms and coping motives for drinking was by far the strongest relationship, suggesting that veterans suffering from PTSD may use alcohol to cope with their PTSD symptoms. Coping motives, therefore, are a likely candidate for explaining why some young adult veterans are more likely than others to experience adverse alcohol consequences from their heavy drinking. Future studies could continue to examine the role of drinking motives in problem drinking behavior in young adult veterans. Although there is ample research on this construct in college students, the unique nature of military service warrants additional studies in young veterans. These results highlight the important role that perceived stigma may play in the etiology of alcohol use behavior among young adult veterans. A robust pattern of findings in the literature suggest that veterans who experience PTSD symptoms are more likely to perceive stigma associated with treatment seeking (Hoge et al., 2004; Jones et al., 2015), and although other studies have examined how stigma influences treatment seeking (Kim et al., 2010), the current study took a different approach informed by the literature linking stigma to alcohol use (De La Rosa et al., 2015; Glass et al., 2013). As perceived stigma itself can be conceptualized as a negative drive state (Livingston & Boyd, 2010), it could serve to exacerbate the effects of PTSD on drinking behavior as shown in the present model. In sum, perceived stigma is a very real phenomenon that most likely contributes to the frequency with which young adult veterans with PTSD symptoms experience adverse alcohol consequences.
The mediators examined within the context of the hypothesized model under investigation are perhaps two of the most likely reasons why so many young adult veterans with PTSD develop an AUD. It is reasonable to assume that anyone experiencing strong negative drive states such as PTSD and stigma are going to deal with them one way or another. Unfortunately for some this may mean eschewing healthier treatment options and instead managing their symptoms with alcohol. As discussed in previous research (Rousseau et al., 2011), this becomes problematic when this reinforcing pattern of alcohol use leads to adverse alcohol consequences and possibly an AUD. This can be compounded by the perceived stigma that one who seeks care is weak or that one’s peers would view them differently if they were to seek care (Fox, Meyer, & Vogt, 2015; Hoge et al., 2004). Thus, the individual now uses alcohol heavily, which can exacerbate PTSD symptoms (Brady, Back, & Coffey, 2004; Jakupcak et al., 2010; Kehle et al., 2012), and is unwilling to go to care for either problem due to perceived stigma. This makes stigma-reduction programs and outreach efforts in the military context (Acosta et al., 2014) so important in the effort to bring veterans into behavioral care settings.
4.1 Limitations
Limitations should be noted. While the current investigation was longitudinal in nature, the study design only allowed for a one-month follow-up of outcome measures. Future studies should expand the timeframe of measurement points to allow for a more comprehensive assessment of the hypothesized model. The coping and stigma measures related generally to negative affect and behavioral health respectively and not to PTSD specifically. Finally, although the self-report measure of PTSD conformed to the DSM-V criteria for a diagnosis, a clinically administered measure could prove more informative for future studies.
4.2 Conclusion
Our model helped to identify two areas that should be targeted to help veterans suffering from PTSD symptoms. The first concerns coping with PTSD and how veterans understand their symptoms and treatment options. Resources should be provided that help develop coping skills, identify support groups, and present relevant information on the nature of PTSD (DoD, 2010; Veilleux et al., 2014) to help veterans manage PTSD symptoms without the use of alcohol to cope. Given the current stigma associated with mental health disorders and the culture of the military that seeking help may be a sign of weakness, young adult veterans suffering from PTSD will often not seek help from a professional counselor. Thus, the second area for targeting should focus on combating the stigma associated with behavioral health treatment seeking among the military population. Mental health professionals in conjunction with military personnel should work to combat the notion that seeking help for a mental condition is somehow incompatible with the “Warrior Ethos” of service and duty. On the contrary, the military should communicate loudly and clearly that the credo “Leave no one behind” applies long after service has ended and that they will do whatever it takes for as long as it takes to ensure their veterans thrive in civilian life.
Highlights.
We proposed a path model of the relationship between combat severity, PTSD, and alcohol consequences.
Greater combat severity and PTSD placed young adult veterans at increased risk of alcohol consequences.
Coping motives and treatment seeking stigma mediate the link between PTSD and alcohol consequences.
Acknowledgments
This work was funded by a grant from the National Institute on Alcohol Abuse and Alcoholism (R34AA022400, “Brief Online Intervention to Reduce Heavy Alcohol Use among Young Adult Veterans”) awarded to Eric R. Pedersen. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIAAA or the National Institutes of Health.
Role of Funding Sources
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
SM conceptualized the model, conducted the statistical analysis, and wrote the first draft of the manuscript. EP and GM designed the original study, obtained funding, and directed data collection procedures. All authors provided edits to the paper and approved of the final manuscript.
Declaration of Interest
All authors declare they have no conflicts of interest to report.
References
- Acosta J, Becker A, Cerully JL, Fisher MP, Martin LT, Vardavas R, Slaughter ME, Schell TL. Mental Health Stigma in the Military. Santa Monica, CA: RAND Corporation; 2014. Retrieved from: http://www.rand.org/pubs/research_reports/RR426.html. [Google Scholar]
- Barrett P. Structural equation modelling: adjudging model fit. Personality and Individual Differences. 2007;42:815–824. [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, Keane TM. Psychometric Properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (PCL-5) in Veterans. Psychological Assessment. 2015 doi: 10.1037/pas0000254. [DOI] [PubMed] [Google Scholar]
- Brady KT, Back SE, Coffey SF. Substance abuse and posttraumatic stress disorder. Current Directions In Psychological Science. 2004;13(5):206–209. [Google Scholar]
- Bray RM, Pemberton MR, Lane ME, Hourani LL, Mattiko MJ, Babeu LA. Substance use and mental health trends among U.S. Military active duty personnel: Key findings from the 2008 DoD. Health Behavior Survey Military Medicine. 2010;175(6):390–399. doi: 10.7205/milmed-d-09-00132. [DOI] [PubMed] [Google Scholar]
- Britt TW. The stigma of psychological problems in a work environment: Evidence from the screening of service members returning from Bosnia. Journal Of Applied Social Psychology. 2000;30(8):1599–1618. [Google Scholar]
- Britt TW, Greene-Shortridge TM, Brink S, Nguyen QB, Rath J, Cox AL, Castro CA. Perceived stigma and barriers to care for psychological treatment: Implications for reactions to stressors in different contexts. Journal Of Social And Clinical Psychology. 2008;27(4):317–335. [Google Scholar]
- Carey KB, Correia CJ. Drinking motives predict alcohol-related problems in college students. Journal of Studies on Alcohol. 1997;58(1):100–105. doi: 10.15288/jsa.1997.58.100. [DOI] [PubMed] [Google Scholar]
- Carpenter KM, Hasin D. A prospective evaluation of the relationship between reasons for drinking and DSM-IV alcohol-use disorders. Addictive Behaviors. 1998;23(1):41–46. doi: 10.1016/s0306-4603(97)00015-4. [DOI] [PubMed] [Google Scholar]
- Carpenter KM, Hasin DS. Drinking to cope with negative affect and DSM-IV alcohol use disorders: A test of three alternative explanations. Journal Of Studies On Alcohol. 1999;60(5):694–704. doi: 10.15288/jsa.1999.60.694. [DOI] [PubMed] [Google Scholar]
- Colder CR. Life stress, physiological and subjective indexes of negative emotionality, and coping reasons for drinking: Is there evidence for a self-medication model of alcohol use? Psychology Of Addictive Behaviors. 2001;15(3):237–245. [PubMed] [Google Scholar]
- Cooper ML. Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychological Assessment. 1994;6(2):117–128. [Google Scholar]
- Cooper ML, Frone MR, Russell M, Mudar P. Drinking to regulate positive and negative emotions: a motivational model of alcohol use. Journal of personality and social psychology. 1995;69(5):990–1005. doi: 10.1037//0022-3514.69.5.990. [DOI] [PubMed] [Google Scholar]
- Creech SK, Swift R, Zlotnick C, Taft C, Street AE. Combat exposure, mental health, and relationship functioning among women veterans of the Afghanistan and Iraq wars. Journal Of Family Psychology. 2016;30(1):43–51. doi: 10.1037/fam0000145. [DOI] [PubMed] [Google Scholar]
- De La Rosa GM, Delaney EM, Webb-Murphy JA, Johnston SL. Interactive effects of stress and individual differences on alcohol use and posttraumatic stress disorder among personnel deployed to Guantanamo Bay. Addictive Behaviors. 2015;50:128–134. doi: 10.1016/j.addbeh.2015.06.016. [DOI] [PubMed] [Google Scholar]
- Department of Defense. VA/DoD Clinical Practice Guideline for Management of Post-Traumatic Stress. 2010 Retrieved from: http://www.healthquality.va.gov/guidelines/MH/ptsd/cpgPTSDFULL201011612c.pdf.
- Dixon LJ, Leen-Feldner EW, Ham LS, Feldner MT, Lewis SF. Alcohol use motives among traumatic event-exposed, treatment-seeking adolescents: Associations with posttraumatic stress. Addictive Behaviors. 2009;34(12):1065–1068. doi: 10.1016/j.addbeh.2009.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dvorak RD, Pearson MR, Day AM. Ecological momentary assessment of acute alcohol use disorder symptoms: Associations with mood, motives, and use on planned drinking days. Experimental And Clinical Psychopharmacology. 2014;22(4):285–297. doi: 10.1037/a0037157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox AB, Meyer EC, Vogt D. Attitudes about the VA health-care setting, mental illness, and mental health treatment and their relationship with VA mental health service use among female and male OEF/OIF veterans. Psychological Services. 2015;12(1):49–58. doi: 10.1037/a0038269. [DOI] [PubMed] [Google Scholar]
- Gibbs DA, Rae Olmsted KL, Brown JM, Clinton-Sherrod AM. Dynamics of stigma for alcohol and mental health treatment among army soldiers. Military Psychology. 2011;23(1):36–51. [Google Scholar]
- Gilbertson MW, McFarlane AC, Weathers FW, Keane TM, Yehuda R, Shalev AY, Pitman RK. Is trauma a causal agent of psychopathologic symptoms in posttraumatic stress disorder? Findings from identical twins discordant for combat exposure. Journal Of Clinical Psychiatry. 2010;71(10):1324–1330. doi: 10.4088/JCP.10m06121blu. [DOI] [PubMed] [Google Scholar]
- Glass JE, Mowbray OP, Link BG, Kristjansson SD, Bucholz KK. Alcohol stigma and persistence of alcohol and other psychiatric disorders: A modified labeling theory approach. Drug And Alcohol Dependence. 2013;133(2):685–692. doi: 10.1016/j.drugalcdep.2013.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glass JE, Williams EC, Bucholz KK. Psychiatric comorbidity and perceived alcohol stigma in a nationally representative sample of individuals with DSM-5 alcohol use disorder. Alcoholism: Clinical And Experimental Research. 2014;38(6):1697–1705. doi: 10.1111/acer.12422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godfrey KM, Mostoufi S, Rodgers C, Backhaus A, Floto E, Pittman J, Afari N. Associations of military sexual trauma, combat exposure, and number of deployments with physical and mental health indicators in Iraq and Afghanistan veterans. Psychological Services. 2015;12(4):366–377. doi: 10.1037/ser0000059. [DOI] [PubMed] [Google Scholar]
- Gorman LA, Blow AJ, Ames BD, Reed PL. National Guard families after combat: mental health, use of mental health services, and perceived treatment barriers. Psychiatric Services. 2011;62:28–34. doi: 10.1176/ps.62.1.pss6201_0028. [DOI] [PubMed] [Google Scholar]
- Gottfredson NC, Hussong AM. Drinking to dampen affect variability: Findings from a college student sample. Journal Of Studies On Alcohol And Drugs. 2013;74(4):576–583. doi: 10.15288/jsad.2013.74.576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn AM, Tirabassi CK, Simons RM, Simons JS. Military sexual trauma, combat exposure, and negative urgency as independent predictors of PTSD and subsequent alcohol problems among OEF/OIF veterans. Psychological Services. 2015;12(4):378–383. doi: 10.1037/ser0000060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasking P, Lyvers M, Carlopio C, Raber A. The relationship between coping strategies, alcohol expectancies, drinking motives and drinking behaviour. Addictive Behaviors. 2011;36(5):479–487. doi: 10.1016/j.addbeh.2011.01.014. [DOI] [PubMed] [Google Scholar]
- Hassija CM, Jakupcak M, Maguen S, Shipherd JC. The influence of combat and interpersonal trauma on PTSD, depression, and alcohol misuse in U.S. Gulf War and OEF/OIF women veterans. Journal Of Traumatic Stress. 2012;25(2):216–219. doi: 10.1002/jts.21686. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY, US: Guilford Press; 2013. [Google Scholar]
- Hides L, Lubman DI, Cosgrave EM, Buckby JA, Killackey E, Yung AR. Motives for substance use among young people seeking mental health treatment. Early Intervention In Psychiatry. 2008;2(3):188–194. doi: 10.1111/j.1751-7893.2008.00076.x. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat Duty in Iraq and Afghanistan, Mental Health Problems, and Barriers to Care. The New England Journal Of Medicine. 2004;351(1):13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Jacobson IG, Ryan MK, Hooper TJ, Smith TC, Amoroso PJ, Boyko EJ, Bell NS. Alcohol use and alcohol-related problems before and after military combat deployment. JAMA: Journal Of The American Medical Association. 2008;300(6):663–675. doi: 10.1001/jama.300.6.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakupcak M, Tull MT, McDermott MJ, Kaysen D, Hunt S, Simpson T. PTSD symptom clusters in relationship to alcohol misuse among Iraq and Afghanistan war veterans seeking post-deployment VA health care. Addictive Behaviors. 2010;35(9):840–843. doi: 10.1016/j.addbeh.2010.03.023. [DOI] [PubMed] [Google Scholar]
- Jones N, Keeling M, Thandi G, Greenberg N. Stigmatisation, perceived barriers to care, help seeking and the mental health of british military personnel. Social Psychiatry And Psychiatric Epidemiology. 2015 doi: 10.1007/s00127-015-1118-y. [DOI] [PubMed] [Google Scholar]
- Kahler CW, Hustad J, Barnett NP, Strong DR, Borsari B. Validation of the 30-day version of the Brief Young Adult Alcohol Consequences Questionnaire for use in longitudinal studies. Journal Of Studies On Alcohol And Drugs. 2008;69(4):611–615. doi: 10.15288/jsad.2008.69.611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahler CW, Strong DR, Read JP. Toward Efficient and Comprehensive Measurement of the Alcohol Problems Continuum in College Students: The Brief Young Adult Alcohol Consequences Questionnaire. Alcoholism: Clinical And Experimental Research. 2005;29(7):1180–1189. doi: 10.1097/01.alc.0000171940.95813.a5. [DOI] [PubMed] [Google Scholar]
- Kaikkonen NM, Laukkala T. International military operations and mental health— A review. Nordic Journal Of Psychiatry. 2016;70(1):10–15. doi: 10.3109/08039488.2015.1048718. [DOI] [PubMed] [Google Scholar]
- Kehle SM, Ferrier-Auerbach AG, Meis LA, Arbisi PA, Erbes CR, Polusny MA. Predictors of postdeployment alcohol use disorders in National Guard soldiers deployed to Operation Iraqi Freedom. Psychology Of Addictive Behaviors. 2012;26(1):42–50. doi: 10.1037/a0024663. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ. The Self-Medication Hypothesis Revisited: The Dually Diagnosed Patient. Primary Psychiatry. 2003;10(9):47–48. [Google Scholar]
- Kulesza M, Pedersen ER, Corrigan PW, Marshall GN. Help seeking stigma and mental health treatment seeking among young adult veterans. Military Behavioral Health. 2015;3:230–239. doi: 10.1080/21635781.2015.1055866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim PY, Thomas JL, Wilk JE, Castro CA, Hoge CW. Stigma, barriers to care, and use of mental health services among active duty and National Guard soldiers after combat. Psychiatric Services. 2010;61(6):572–588. doi: 10.1176/ps.2010.61.6.582. [DOI] [PubMed] [Google Scholar]
- Kimbrel NA, Hauser MA, Garrett M, Ashley-Koch A, Liu Y, Dennis MF, Beckham JC. Effect of the APOE ε4 allele and combat exposure on PTSD among Iraq/Afghanistan-era veterans. Depression And Anxiety. 2015;32(5):307–315. doi: 10.1002/da.22348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulesza M, Pedersen ER, Corrigan PW, Marshall GN. Help-Seeking Stigma and Mental Health Treatment Seeking Among Young Adult Veterans. Military Behavioral Health. 2015;3:230–239. doi: 10.1080/21635781.2015.1055866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, Engels R. Why do young people drink? A review of drinking motives. Clinical psychology review. 2005;25(7):841–861. doi: 10.1016/j.cpr.2005.06.002. [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, Engels R. Replication and Validation of the Drinking Motive Questionnaire Revised (DMQ-R, Cooper, 1994) among Adolescents in Switzerland. European Addiction Research. 2006;12:161–168. doi: 10.1159/000092118. [DOI] [PubMed] [Google Scholar]
- Larson MJ, Wooten NR, Adams RS, Merrick EL. Military combat deployments and substance use: Review and future directions. Journal Of Social Work Practice In The Addictions. 2012;12(1):6–27. doi: 10.1080/1533256X.2012.647586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehavot K, Stappenbeck CA, Luterek JA, Kaysen D, Simpson TL. Gender differences in relationships among PTSD severity, drinking motives, and alcohol use in a comorbid alcohol dependence and PTSD sample. Psychology Of Addictive Behaviors. 2014;28(1):42–52. doi: 10.1037/a0032266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levant RF, Rankin TJ, Williams CM, Hasan NT, Smalley KB. Evaluation of the factor structure and construct validity of scores on the Male Role Norms Inventory—Revised (MRNI-R) Psychology Of Men & Masculinity. 2010;11(1):25–37. [Google Scholar]
- Livingston JD, Boyd JE. Correlates and consequences of internalized stigma for people living with mental illness: A systematic review and meta-analysis. Social Science & Medicine. 2010;71(12):2150–2161. doi: 10.1016/j.socscimed.2010.09.030. [DOI] [PubMed] [Google Scholar]
- Martens MP, Neighbors C, Lewis MA, Lee CM, Oster-Aaland L, Larimer ME. The roles of negative affect and coping motives in the relationship between alcohol use and alcohol-related problems among college students. Journal of Studies on Alcohol and drugs. 2008;69(3):412–419. doi: 10.15288/jsad.2008.69.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDevitt-Murphy ME, Fields JA, Monahan CJ, Bracken KL. Drinking motives among heavy-drinking veterans with and without posttraumatic stress disorder. Addiction Research & Theory. 2015;23(2):148–155. doi: 10.3109/16066359.2014.949696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarling L, D’Angelo M, Drain M, Gibbs DA, Rae Olmsted KL. Stigma as a barrier to substance abuse and mental health treatment. Military Psychology. 2011;23(1):1–5. [Google Scholar]
- Merrill JE, Read JP. Motivational pathways to unique types of alcohol consequences. Psychology Of Addictive Behaviors. 2010;24(4):705–711. doi: 10.1037/a0020135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen ER, Marshall GN, Schell TL. Study protocol for a web-based personalized normative feedback alcohol intervention for young adult veterans. Addiciton Science & Clinical Practice. 2016;11 doi: 10.1186/s13722-016-0055-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen ER, Marshall GN, Schell TL, Neighbors C. Young adult veteran perceptions of peers’ drinking behavior and attitudes. Psychology Of Addictive Behaviors. 2016;30(1):39–51. doi: 10.1037/adb0000120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen ER, Parast L, Marshall GN, Schell TL, Neighbors C. A randomized controlled trial for a web-based personalized normative feedback alcohol intervention for young adult veterans. Manuscript submitted for publication. 2016 doi: 10.1037/ccp0000187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrzak RH, Johnson DC, Goldstein MB, Malley JC, Southwick SM. Perceived stigma and barriers to mental health care utilization among OEF-OIF veterans. Psychiatric Services. 2009;60:1118–1122. doi: 10.1176/ps.2009.60.8.1118. [DOI] [PubMed] [Google Scholar]
- Rafnsson FD, Jonsson FH, Windle M. Coping strategies, stressful life events, problem behaviors, and depressed affect. Anxiety, Stress & Coping: An International Journal. 2006;19(3):241–257. [Google Scholar]
- Ramchand R, Miles J, Schell T, Jaycox L, Marshall GN, Tanielian T. Prevalence and correlates of drinking behaviors among previously deployed military and matched civilian populations. Military Psychology. 2011;23(1):6–21. doi: 10.1080/08995605.2011.534407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rousseau GS, Irons JG, Correia CJ. The reinforcing value of alcohol in a drinking to cope paradigm. Drug And Alcohol Dependence. 2011;118(1):1–4. doi: 10.1016/j.drugalcdep.2011.02.010. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption: II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Schell TL, Marshall GN. Survey of individuals previously deployed for OEF/OIF. In: Tanielian T, Jaycox LH, editors. Invisible wounds of war: Psychological and cognitive injuries, their consequences, and services to assist recovery. Santa Monica, CA: RAND MG-720; 2008. [Google Scholar]
- Schumm JA, Chard KM. Alcohol and stress in the military. Alcohol Research: Current Reviews. 2012;34(4):401–407. doi: 10.35946/arcr.v34.4.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seal KH, Cohen G, Waldrop A, Cohen BE, Maguen S, Ren L. Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001–2010: Implications for screening, diagnosis and treatment. Drug And Alcohol Dependence. 2011;116(1–3):93–101. doi: 10.1016/j.drugalcdep.2010.11.027. [DOI] [PubMed] [Google Scholar]
- Veilleux JC, Skinner KD, Reese ED, Shaver JA. Negative affect intensity influences drinking to cope through facets of emotion dysregulation. Personality And Individual Differences. 2014;59:96–101. [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD Checklist for DSM-5 (PCL-5) Boston, MA: National Center for PTSD; 2013. [Google Scholar]
- Wisco BE, Marx BP, Wolf EJ, Miller MW, Southwick SM, Pietrzak RH. Posttraumatic stress disorder in the US veteran population: Results from the National Health and Resilience in Veterans Study. Journal Of Clinical Psychiatry. 2014;75(12):1338–1346. doi: 10.4088/JCP.14m09328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright KM, Foran HM, Wood MD, Eckford RD, McGurk D. Alcohol problems, aggression, and other externalizing behaviors after return from deployment: Understanding the role of combat exposure, internalizing symptoms, and social environment. Journal Of Clinical Psychology. 2012;68(7):782–800. doi: 10.1002/jclp.21864. [DOI] [PubMed] [Google Scholar]
- Xue C, Ge Y, Tang B, Liu Y, Kang P, Wang M, Zhang L. A meta-analysis of risk factors for combat-related PTSD among military personnel and veterans. Plos ONE. 2015;10(3) doi: 10.1371/journal.pone.0120270. [DOI] [PMC free article] [PubMed] [Google Scholar]