A review of 59 articles published between 2006 and July 2014 on the effect of occupational therapy interventions on functional outcomes for adults with musculoskeletal disorders of the forearm, wrist, and hand found that the strongest evidence supports postsurgical early active motion protocols and splinting for various conditions.
Abstract
Occupational therapy practitioners are key health care providers for people with musculoskeletal disorders of the distal upper extremity. It is imperative that practitioners understand the most effective and efficient means for remediating impairments and supporting clients in progressing to independence in purposeful occupations. This systematic review provides an update to a previous review by summarizing articles published between 2006 and July 2014 related to the focused question, What is the evidence for the effect of occupational therapy interventions on functional outcomes for adults with musculoskeletal disorders of the forearm, wrist, and hand? A total of 59 articles were reviewed. Evidence for interventions was synthesized by condition within bone, joint, and general hand disorders; peripheral nerve disorders; and tendon disorders. The strongest evidence supports postsurgical early active motion protocols and splinting for various conditions. Very few studies have examined occupation-based interventions. Implications for occupational therapy practice and research are provided.
Musculoskeletal disorders (MSDs) are 1 of 10 diagnostic groups that increased in size by more than 30% from 1990 to 2010 (Murray et al., 2013). By 2013, people with MSDs had incurred a global burden of approximately 150,000 disability-adjusted life years, an increase in burden of 17% since 2005 (Murray et al., 2015). Moreover, in the United States, MSDs account for three of the top four diagnoses with the most total pooled years lived with a disability across the population (Murray et al., 2013). Functional hand use is a large component of the human identity, because hands are a person’s interface with the world (Kielhofner, 2014). As such, MSDs of the forearm, wrist, and hand present an especially difficult challenge to functioning in everyday life. Moreover, serious hand injury and chronic pain and discomfort are correlated with low quality of life, anxiety, and depression (Calfee, Chu, Sorensen, Martens, & Elfar, 2015; Kovacs et al., 2011).
Occupational therapy practitioners frequently work with people who have MSDs of the distal upper extremity (UE). Working collaboratively with the client to identify areas of importance, the occupational therapy practitioner’s primary role in UE rehabilitation is to evaluate and intervene to improve a client’s ability to independently perform functional tasks. Although the target of the occupational therapy plan of care is ultimately participation in purposeful activities, treating clients in this setting often requires the completion of a variety of preparatory activities and other techniques that target impairments in body structures and functions (American Occupational Therapy Association [AOTA], 2014). It is imperative that practitioners know the most effective and efficient means to remediate these impairments so that they can support clients’ progression to independence in purposeful occupations. Thus, it is necessary to consider the evidence for all means of intervention, including preparatory methods and tasks, advocacy, education and training, activities, and occupations (AOTA, 2014).
Since 1998, AOTA has instituted a series of evidence-based practice (EBP) projects to assist members with meeting the challenge of finding and reviewing literature to identify evidence and, in turn, use that evidence to inform practice (Lieberman & Scheer, 2002). A major focus of AOTA’s EBP projects is an ongoing program of systematic reviews of the multidisciplinary scientific literature to identify occupational therapy–relevant evidence and discuss its implications for practice, education, and research.
A previous review was completed to evaluate the evidence published through 2005 for occupational therapy interventions for work-related MSDs of the forearm, wrist, and hand (Amini, 2011). This article provides an update to the review by summarizing articles published between 2006 and July 2014. In addition, the scope for this review was expanded to include all MSDs of the distal UE regardless of etiology. The review was conducted to answer the following focused question: What is the evidence for the effect of occupational therapy interventions on functional outcomes for adults with MSDs of the forearm, wrist, and hand?
Method
The question guiding this review and all search terms were reviewed by the authors, an advisory group of experts in the field, AOTA staff, and the methodology consultant to the AOTA EBP Project. The search strategy from the previous review was used (Arbesman, Lieberman, & Thomas, 2011), and additional search terms were added to ensure maximum coverage of the question on the basis of diagnoses and interventions of interest beyond only work-related injuries (i.e., the focus of the previous review). See Table 1 for a full list of the search terms.
Table 1.
Search Terms for Musculoskeletal Disorders and Arthritis
| Category | Key Search Terms |
| Diagnoses/injuries/clinical conditions—hand/wrist/forearm, elbow, shoulder | adhesive capsulitis, amputation—above elbow, amputations (below elbow, transradial, thumb, finger, with wrist disarticulation), arthritis, arthrogryposis, athletic injuries, axilla, biceps tendon rupture, bicipital tendonitis, brachial plexus injury, burn, calcific shoulder, camptodactly, carpal instability, carpal tunnel syndrome, collateral ligament, collateral strain, Colles’ fracture (closed and open), complex regional pain syndrome, crushing injury—upper arm, crushing injury (wrist, hand, and finger), cubital tunnel syndrome, cumulative trauma, degenerative joint disease, DeQuervain’s tenosynovitis, digital injuries, digits, dislocated finger, dislocation, dislocation—glenohumeral, Dupuytren’s contracture, elbow, elbow joint, extensor tendon rupture, finger, finger injuries, flexor tendon rupture, forearm, fracture anatomical head humerus, fracture greater tuberosity humerus—open, fracture humerus shaft—closed, glenohumeral, hand, hand injuries, joint, Kienbocks disease, lacerating tendon, lateral epicondylitis, mallet finger, medial epicondylitis, multiple fractures hand (closed and open), open wound (finger and hand), pronator teres syndrome, radial and ulnar fractures, radial head fracture, radial tunnel syndrome, reflex sympathetic dystrophy, repetitive strain injury, rotator cuff syndrome shoulder, rotator cuff tear, scapulothoracic articulation, shoulder impingement, shoulder joint, shoulder pain, shoulder strain, shoulder tendonitis, sprain elbow, sprain radiohumeral joint, sprains and strains—rotator cuff, subacromial bursitis, tennis elbow, tenosynovitis elbow, tenosynovitis—hand and wrist, thumb, thumb injuries, triangular fibrocartilage complex (TFCC), trigger finger, ulnar, ulnar nerve syndrome, wounds and injuries—elbow, shoulder, wrist, wrist injuries |
| Intervention | AAROM, activities of daily living, adaptation, adaptive equipment, AROM, arthrokinematics, assistive technology, athletic training, back school, biofeedback, body awareness, body mechanics, cognitive behavior therapy, compensation, create, driving adaptations, durable medical equipment, edema control, education, energy conservation, ergonomics, establish, exercise, functional training, hand therapy, home modification, industrial rehabilitation, interventions, job coaching, job modification, job retraining, joint protection, limb reshaping, modify, occupational medicine, occupational therapy, orthotics, physical agent modalities, physical therapy, postural training, preprosthetic and prosthetic training, prevention, problem solving, PROM, promotion, rehabilitation, relaxation techniques, restore, scapulohumeral rhythm, splint, sports medicine, stretching, therapeutic management, therapy, training, treatment, work hardening, work/occupational rehabilitation, work reconditioning/conditioning |
| Outcomes | absenteeism, anxiety, circumferential measurement for edema, coordination, coping patterns, depression, disability, dynamometry, dysfunction/function, EMG, endurance, fatigue, fear, fine motor coordination, functional/work capacity evaluation, grip strength, hand function, level of independence (ADLs, IADLs), manual muscle testing (MMT), mobility, NCV, occupational engagement (rest, sleep, education, social participation, leisure), occupational performance, occupational stress, pain, physical mobility, pinch strength, productivity, prosthetic use, psychological distress, quality of life, range of motion (ROM), return to work, sensation, sickness, strength, symptom magnification, tolerance to activity, volumetric measurement for edema, weakness, work/employment status |
| Study and trial designs | appraisal, best practices, case control, case report, case series, clinical guidelines, clinical trial, cohort, comparative study, consensus development conferences, controlled clinical trial, critique, cross over, cross-sectional, double-blind, epidemiology, evaluation study, evidence-based, evidence synthesis, feasibility study, follow-up, health technology assessment, intervention, longitudinal, main outcome measure, meta-analysis, multicenter study, observational study, outcome and process assessment, pilot, practice guidelines, prospective, random allocation, randomized controlled trials, retrospective, sampling, scientific integrity review, single subject design, standard of care, systematic literature review, systematic review, treatment outcome, validation study |
Note. AAROM = active assistive range of motion; ADLs = activities of daily living; AROM = active range of motion; EMG = electromyography; IADLs = instrumental activities of daily living; NCV = nerve conduction velocity; PROM = passive range of motion.
A medical research librarian with experience in completing systematic review searches conducted all searches. Databases and sites searched included MEDLINE, PsycINFO, CINAHL, Ergonomics Abstracts, and OTseeker. In addition, consolidated information sources, such as the Cochrane Database of Systematic Reviews, were included in the search. Moreover, reference lists from included articles were examined for potential articles, and selected journals (e.g., American Journal of Occupational Therapy, Journal of Hand Therapy) were hand searched. References with relevance to the distal UE identified in the search results of the other reviews being conducted as part of the EBP Project were evaluated to ensure that all appropriate articles were included. Searches were restricted to peer-reviewed scientific literature published in English between 2006 and July 2014; lower level data from the gray literature such as presentations, conference proceedings, non–peer-reviewed literature, dissertations, and theses were excluded.
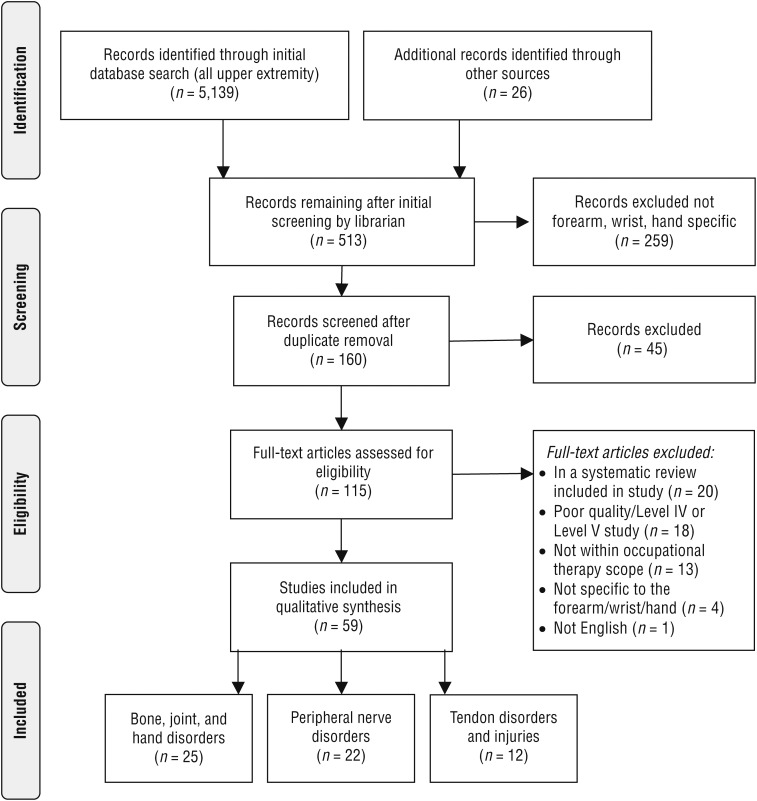
Figure 1 details the flow of all records through the review process. The search resulted in a total of 5,139 records. The consultant to the EBP Project completed initial screening of all citations and abstracts to eliminate articles with no relevance to the question (e.g., diagnosis not of the distal UE), resulting in 513 records, of which 409 were unique. The review authors for all upper-extremity questions coded and divided the abstracts into proximal (i.e., shoulder, elbow) and distal (i.e., forearm, wrist, hand) segments. Two reviewers screened the 160 abstracts related to the forearm, wrist, and hand, identifying 115 articles potentially meeting the primary inclusion criteria. The full text of each article was retrieved and individually read by the two reviewers.
Figure 1.
Flow of search results and studies through the review process.
Note. Format from “Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement,” by D. Moher, A. Liberati, J. Tetzlaff, & D. G. Altman; The PRISMA Group, 2009, PLoS Medicine, 6(6), e1000097. https:/doi.org/10.1371/journal.pmed1000097
Consensus was required between the two reviewers to determine final eligibility, which was based on the following criteria: The study (1) targeted an MSD of the forearm, wrist, or hand; (2) included an intervention within the occupational therapy scope of practice; (3) measured functional outcomes, including measures of body structures with functional implications (e.g., pain, grip, pinch, motion); and (4) met minimum quality standards, which were based on level of evidence and risk of bias. Because intervention for UE MSDs falls within the scopes of practice of multiple professions, involvement of an occupational therapist within a study was not required, provided the study met all other inclusion criteria.
AOTA uses a standard-of-evidence model that ranks the value of scientific evidence for biomedical practice. In this model, the highest level of evidence, Level I, includes systematic reviews of the literature, meta-analyses, and randomized controlled trials (RCTs). Level II evidence includes studies in which assignment to a treatment or a control group is not randomized. Lower levels of evidence are ranked as follows: Level III, which includes cohort studies that do not have a control group; Level IV, single- or multiple-case experimental designs; and Level V, case reports and expert opinions. Studies in this review were limited to Levels I and II. Given the preponderance of studies, Level III evidence was included only when limited or no higher level evidence for the intervention was found. Level IV and V evidence was automatically excluded. Guided by definitions of the U.S. Preventive Services Task Force (2016), determination of the overall strength of evidence for individual topics was classified as insufficient, mixed, limited, moderate, or strong on the basis of the number of studies at each level of evidence and the quality of the individual studies (i.e., analysis of bias).
Results
A total of 59 articles met all inclusion criteria, including 51 Level I studies, 5 Level II studies, and 3 Level III studies (Table 2). For ease of interpretation and reporting, the included studies were grouped into three categories: (1) bone, joint, and general hand disorders, including arthritic conditions specific to the hand (n = 25); (2) peripheral nerve disorders, including carpal tunnel syndrome (CTS; n = 22); and (3) tendon disorders (n = 12). Each article was abstracted in an evidence table to provide readers with detailed descriptions of the study sample, techniques included in the interventions, and results (see Supplemental Table 1, available online at http://otjournal.net; navigate to this article, and click on “Supplemental”).
Table 2.
Studies Included at Each Level of Evidence (N = 59)
| Disorder | Level I (SR/RCT) | Level II | Level III |
| Bone, joint, and hand disorders | |||
| Distal radius fracture | 7 (2/5) | 1 | 0 |
| Boxer’s fracture | 1 (1/0) | 0 | 0 |
| Rheumatoid arthritis | 3 (0/3) | 1 | 0 |
| Osteoarthritis | 4 (1/3) | 0 | 0 |
| Joint contracture | 4 (1/3) | 0 | 1 |
| General hand disorders | 2 (0/2) | 1 | 0 |
| Peripheral nerve disorders | |||
| Carpal tunnel syndrome | 19 (9/10) | 0 | 1 |
| Sensory dysfunction | 1 (1/0) | 0 | 1 |
| Tendon disorders | |||
| Extensor tendon injury | 2 (1/1) | 2 | 0 |
| Flexor tendon injury | 1 (1/0) | 0 | 0 |
| Dupuytren’s contracture | 2 (0/2) | 0 | 0 |
| Trigger finger | 1 (0/1) | 0 | 0 |
| Mallet finger | 3 (0/3) | 0 | 0 |
| Tendon transfer | 1 (1/0) | 0 | 0 |
Note. RCT = randomized controlled trial or randomized comparative trial; SR = systematic review.
Risk of bias was assessed for all studies using published criteria for intervention studies (Higgins & Altman, 2008) and systematic reviews (Shea et al., 2007). The quality of included RCTs varied, with common problems being a lack of participant blinding, poorly described randomization methods, study dropout, and lack of long-term follow-up (Supplemental Table 2, online). Methodological quality of the systematic reviews was primarily good to excellent, with multiple reviews having been conducted using the highly standardized Cochrane system (Supplemental Table 3, online).
Bone, Joint, and General Hand Disorders
Distal Radius and Boxer’s Fractures.
Other than short-term effects on pain, no evidence supported long-term effects on functional outcomes for exercise or modalities that begin postimmobilization compared with no intervention after distal radial fracture (Bruder, Taylor, Dodd, & Shields, 2011; Handoll, Madhok, & Howe, 2006). An RCT (Kuo et al., 2013) found that, compared with postimmobilization therapy, early therapy during immobilization led to greater thumb and finger work space range of motion (ROM) at 12 wk, and a retrospective Level II study (Valdes, 2009) found that patients receiving early ROM attended significantly fewer therapy visits and attained functional ROM of wrist and forearm significantly faster. Similarly, a Cochrane systematic review (Handoll et al., 2006) found that even though there was no evidence for greater effects at long-term follow-up, occupational therapy during immobilization led to better short-term improvements in grip, pinch, and ROM.
Two systematic reviews indicated that early exercises via either supervised therapy or instruction in a home exercise program (HEP) have equivocal benefits (Bruder et al., 2011; Handoll et al., 2006). In contrast, 2 RCTs found that, compared with guided physical or occupational therapy, patients receiving postsurgical HEP instruction had significantly greater improvement in functional outcomes at 6 wk (Krischak et al., 2009), as well as at 3 and 6 mo (Souer, Buijze, & Ring, 2011). A moderate-quality RCT (Magnus et al., 2013) found that patients receiving contralateral strengthening that began during immobilization had faster recovery of grip in the affected hand. For treatment of boxer’s fractures, a Cochrane review (Poolman et al., 2005) determined that the evidence supported short-term effects of numerous different immobilization techniques, with no specific technique being better than another.
Rheumatoid Arthritis.
A moderate-quality RCT found that an HEP that included strengthening led to better function at 6-mo follow-up than either an HEP focused only on stretching or no HEP (O’Brien, Jones, Mullis, Mulherin, & Dziedzic, 2006). A low-quality Level II study suggested that the addition of kinesiotaping to traditional therapy may lead to greater increases in hand function (Szczegielniak, Łuniewski, Bogacz, & Sliwiński, 2012). For people with boutonniere deformity of the thumb secondary to rheumatoid arthritis (RA), use of a custom-made thermoplastic thumb splint during functional activities resulted in a significant reduction in pain compared with no splint but had no effect on strength, dexterity, or general hand function (Silva, Lombardi, Breitschwerdt, Poli Araújo, & Natour, 2008). (Although professional nomenclature has changed from splint to orthosis [Coverdale, 2012], we use the terms splint and splinting throughout this review to avoid confusion because they are the most common terms used in the reviewed studies.) Patients with RA who had swan neck deformities equally preferred silver ring splints and prefabricated thermoplastic splints, and both contributed to improvements in dexterity after 4 wk of wear (van der Giesen et al., 2009). A detailed review of the evidence for occupational therapy interventions for people with RA can be found in a separate systematic review in this issue (Siegel, Watson, Apodaca, & Poole, 2017).
Osteoarthritis.
A high-quality systematic review concluded that for people with osteoarthritis (OA) of the hand, limited evidence supports use of education and exercise, mixed evidence supports a beneficial effect of splinting on pain, and no evidence supports one splinting design over another (Moe, Kjeken, Uhlig, & Hagen, 2009). Three RCTs evaluated interventions for carpometacarpal OA (CMC OA). A low-quality RCT (with significant dropout) found no difference in outcomes between a prefabricated neoprene and a custom-made thermoplastic thumb splint, but patients found the neoprene splint more comfortable (Becker, Bot, Curley, Jupiter, & Ring, 2013).
Hermann et al. (2014) found no effects for either a hand-exercise HEP combined with a prefabricated soft thumb spica splint or the HEP alone, although pain was lower during activities while wearing the splint. Finally, a high-quality RCT found that a comprehensive radial nerve mobilization technique led to a significantly higher pain threshold to pressure over the carpal bones and improved pinch strength immediately after treatment, but no long-term effects compared with a placebo treatment were found (Villafañe, Silva, Bishop, & Fernandez-Carnero, 2012).
Joint Contracture and Decreased ROM.
A moderate-quality systematic review concluded that moderate evidence supports the use of joint mobilization techniques at the wrist for patients with decreased ROM after distal radius fracture (Heiser, O’Brien, & Schwartz, 2013). A moderate- to high-quality RCT found no evidence to support dynamic splinting for contracture resulting from distal radial fracture as superior to standard care in improving passive or active wrist ROM or occupational performance (Jongs, Harvey, Gwinn, & Lucas, 2012).
A Level III cohort study found that dynamic splinting improved active and passive ROM in participants with contracture in finger joints (Glasgow, Tooth, Fleming, & Peters, 2011). A low-quality RCT by the same investigators found no differential effect of wearing protocols with different end-range times on outcomes, potentially because the average time ended up being similar between the two groups (Glasgow, Fleming, Tooth, & Peters, 2012). A moderate-quality RCT found that the use of mirror therapy as part of a conventional therapy program and a mirror-based HEP for people with decreased finger ROM resulted in significantly larger increases in posttherapy total active ROM and functional scores than conventional therapy alone (Rostami, Arefi, & Tabatabaei, 2013).
General Hand Disorders.
A moderate-quality RCT found that a custom-made leather wrist splint and a commercially available fabric splint with a palmar metal bar were equally effective at reducing pain and improving function in adults with chronic wrist pain; patients were more satisfied with the custom-made splint (Thiele, Nimmo, Rowell, Quinn, & Jones, 2009). A moderate-quality RCT found no benefit to hand-related outcomes with the addition of core-strengthening activities to the rehabilitation of people with wrist injuries (Ayhan, Unal, & Yakut, 2014).
Compared with a standard inpatient care model for patients with hand-related diagnoses, a Level II nonrandomized comparative study found greater functional improvement and decreased pain among patients in a patient-oriented rehabilitation program based on a biopsychosocial model. Patients were screened and treated for anxiety and depression, met jointly on a weekly basis with a multidisciplinary treatment team, had a rehabilitation manager, and participated in targeted work-related activities as part of the occupational therapy intervention (Harth, Germann, & Jester, 2008).
Peripheral Nerve Disorders
Physical Agent Modalities for Carpal Tunnel Syndrome.
Five systematic reviews and 5 RCTs evaluated the effects of various physical agent modalities in the treatment of CTS; the majority evaluated low-level laser therapy (LLLT) or ultrasound (US). Three systematic reviews of LLLT’s effect on CTS symptoms found no evidence that LLLT was better than sham or placebo treatments (Huisstede et al., 2010; Peters, Page, Coppieters, Ross, & Johnston, 2013; Piazzini et al., 2007). Although 1 low-quality RCT found posttreatment effects (i.e., at 2 wk) of LLLT versus a sham treatment (Chang, Wu, Jiang, Yeh, & Tsai, 2008), a higher quality RCT found that all participants had improved outcomes regardless of whether they received any dose of LLLT or a placebo treatment (Tascioglu, Degirmenci, Ozkan, & Mehmetoglu, 2012).
Two low-quality studies found that LLLT was as effective as magnetic field therapy (Dakowicz, Kuryliszyn-Moskal, Kosztyła-Hojna, Moskal, & Latosiewicz, 2011) and US (Sawan, Sayed Mahmoud, & Hussien, 2013). As for US, two high-quality systematic reviews found limited evidence to support the use of US over placebo and no evidence for a specific US protocol or for US as better than other conservative treatments (Huisstede et al., 2010; Page, O’Connor, Pitt, & Massy-Westropp, 2013). No evidence supported the use of other thermal modalities.
Regarding other modalities, a 3-day heat wrap intervention led to immediate reduction in symptoms, but no sustained effects were found at 5-day follow-up (Huisstede et al., 2010), and contrast baths showed no benefit for patients after surgical release (Peters et al., 2013). An RCT found that 10 wk of phonophoresis was more effective than iontophoresis in reducing symptoms for up to 4 wk (Bakhtiary, Fatemi, Emami, & Malek, 2013); a 2nd RCT found no difference between these modalities and no evidence of any effect on strength or dexterity outcomes (Gurcay, Unlu, Gurcay, Tuncay, & Cakci, 2012).
Exercise and Manual Therapies for Carpal Tunnel Syndrome.
Three systematic reviews examined various exercise and manual therapy interventions for CTS. A Cochrane review (Page, O’Connor, Pitt, & Massy-Westropp, 2012) found moderate evidence for short-term effects of mobilization on symptoms and function compared with no treatment; however, the evidence was inconclusive regarding the benefit of mobilization over other conservative treatments or for one specific type of mobilization over another. Two additional systematic reviews found limited evidence for neural gliding exercises as an alternative to other interventions and recommended neural gliding as part of a comprehensive intervention for CTS because of its low cost (Medina McKeon & Yancosek, 2008; Peters et al., 2013).
In addition to these systematic reviews, 2 RCTs and 1 Level III cohort study each provided suggestive evidence for positive benefits of manual therapies. Myofascial release on trigger points in the pronator teres, axilla, and biceps resulted in significantly greater improvements in symptoms and functional status than release on nonrelevant trigger points; effects were sustained at 6-mo follow-up (Hains, Descarreaux, Lamy, & Hains, 2010). Completion of a daily self-massage protocol added to splinting led to greater, although nonsignificant, increases in strength and function, improved nerve conduction, and decreases in pain compared with splinting alone (Madenci, Altindag, Koca, Yilmaz, & Gur, 2012). Similarly, a small Level III cohort study indicated that integrated transverse massage and progressive joint mobilization led to significantly improved symptoms and function (Maddali Bongi et al., 2013).
Splinting for Carpal Tunnel Syndrome.
Four systematic reviews and 2 RCTs evaluated effects of splint use for CTS. Although 1 Cochrane review (Peters et al., 2013) found no supporting evidence for the use of splinting after carpal tunnel release, a 2nd Cochrane review of 19 RCTs (Page, Massy-Westropp, O’Connor, & Pitt, 2012) found limited evidence for night splinting versus no treatment or other conservative treatments. Two additional systematic reviews (Huisstede et al., 2010; Piazzini et al., 2007) found moderate evidence to support full-time and night-time splinting, as did an RCT not included in either of these systematic reviews (Hall et al., 2013).
Despite evidence supporting splinting, none of the reviews identified one type of splint as the most effective. However, results of an RCT by Baker et al. (2012) indicated that the combination of a general splint (i.e., cock-up splint) with lumbrical stretching exercises or a custom-made lumbrical splint with general wrist-stretching exercises was more effective at improving function and reducing symptoms than general splinting–general stretching or lumbrical splinting–lumbrical stretching combinations. Moreover, participants using the general splint–lumbrical stretch combination were more likely to present with clinically important changes in function at 24 wk than those using the other combinations.
Ergonomic Interventions for Carpal Tunnel Syndrome.
Two systematic reviews found mixed evidence for the use of ergonomic interventions as a means to treat CTS (Huisstede et al., 2010; O’Connor, Page, Marshall, & Massy-Westropp, 2012). A Cochrane review on ergonomic keyboards for CTS found low-quality evidence that ergonomic keyboards reduced pain more than placebo (O’Connor et al., 2012), whereas Huisstede et al. (2010) found moderate evidence for short-term improvement in hand function with use of ergonomic keyboards compared with normal keyboards.
Interventions for Sensory Dysfunction.
A moderate- to high-quality systematic review of 7 comparative trials found limited evidence for short-term benefits and inconsistent evidence for long-term benefits of both classical and early-phase sensory reeducation for ulnar and median nerve injuries (Miller, Chester, & Jerosch-Herold, 2012). A small Level III cohort study found that self-massage 3 times a day with progressive graded texturing over hypersensitive areas after surgery resulted in significant improvement in pain, sensitivity, and occupational performance (Goransson & Cederlund, 2011).
Tendon Disorders
Extensor Tendon Injuries.
A moderate-quality systematic review of 17 studies found evidence for the equivalent benefit of early active motion and dynamic splinting protocols and found that both outperformed static splinting protocols after repair of extensor Zones V–VIII (Sameem, Wood, Ignacy, Thoma, & Strumas, 2011). Two additional studies that compared early active motion with static splinting after repair in Zones V and VI had similar findings. One low-quality RCT (small sample, large dropout) found that patients who completed active finger motions within 5 days of surgery, and during the first 3 wk after surgery, had the least extension lag and the greatest improvement in functional reports at 12 wk compared with patients receiving early passive motion or whose hand was fully immobilized for the first 3 wk postsurgery (Hall, Lee, Page, Rosenwax, & Lee, 2010).
Similarly, a Level II study found that early motion during the first 4 wk after surgery, using a modified relative motion splint to keep the proximal phalanges of affected fingers in 15°–20° of relative extension to the other fingers (i.e., allowing for performance of functional tasks), resulted in significantly improved total active motion at 6 wk and significantly quicker return to work (3.3 wk vs. 9.4 wk; Hirth et al., 2011). One additional low-quality Level II study (poorly described methods) found that patients who had surgery for tendon injury in extensor Zones I and II followed by therapy fared similarly to patients receiving therapy only, but the duration of therapy was shorter for surgically treated patients (Wańczyk, Pieniazek, & Pelczar-Pieniazek, 2008).
Flexor Tendon Injuries.
A moderate-quality meta-analysis found that studies using early active motion protocols yielded excellent or good results in 94% of cases, which was significantly better than any other protocol (Chesney, Chauhan, Kattan, Farrokhyar, & Thoma, 2011). Although the differences were not significant, studies in which a combined Kleinert and Duran protocol was used showed the lowest tendon rupture rate (2.3%) compared with an early active motion protocol (4.1%), a Duran protocol (3.8%), or a Kleinert protocol (7.1%).
Dupuytren’s Contracture.
Two moderate-quality RCTs found no difference in ROM or reported functional outcomes when comparing the addition of a custom-made night splint to hand therapy alone either at 6-wk or 3-mo follow-up (Collis, Collocott, Hing, & Kelly, 2013) or at 3-, 6-, or 12-mo follow-up (Jerosch-Herold et al., 2011).
Trigger Finger.
One moderate-quality RCT comparing therapy with corticosteroid injection for trigger finger found that, at 3 mo, both groups had improved grip strength, decreased pain, and fewer triggering events and that patient satisfaction was better in the injection group. At 6 mo, the therapy group had no recurrence, compared with 15.8% symptom return and 10.5% triggering return in the injection group (Salim, Abdullah, Sapuan, & Haflah, 2012).
Mallet Finger.
A high-quality RCT comparing cast immobilization with removable orthotic immobilization of the affected distal interphalangeal (DIP) joint found that those wearing the cast had significantly greater reduction in edema and greater active DIP extension at 12 wk and that those wearing the removable orthotic had lower pain and higher ratings of the splint’s aesthetic quality (Tocco et al., 2013). A moderate-quality RCT found no significant differences in outcomes at 12 or 20 wk when comparing stack splints, dorsal aluminum splints, and custom-made thermoplastic splints but noted significant rates of treatment failure and complications with the stack and dorsal aluminum splints (O’Brien & Bailey, 2011). A low-quality RCT found no outcome differences at 12 wk when comparing full-time extension splinting with volar aluminum, dorsal aluminum, and custom-made thermoplastic splints (Pike et al., 2010).
Tendon Transfer.
One moderate-quality systematic review assessed 6 studies that evaluated interventions after tendon transfer in the hand (Sultana, MacDermid, Grewal, & Rath, 2013). Participants receiving early active motion showed better strength and ROM at 3–4 mo than did participants in immobilization conditions. Although no significant differences were found at long-term follow-up, patients receiving early active motion protocols returned to work sooner. Evidence for early active and early controlled motion protocols was mostly equivocal for patient outcomes, adverse events, and time of rehabilitation.
Discussion
This review summarizes the recent literature to determine the effectiveness of occupational therapy interventions for MSDs of the distal UE. CTS and distal radius fracture were the most frequently treated conditions in the studies in this review. Across all diagnoses, the most frequently studied interventions were early active motion after surgical intervention, exercise, and splinting. Intervention protocols had significant heterogeneity across the studies, which led to difficulty identifying the clinical effects of any one specific intervention or intervention protocol. Across all conditions, the evidence suggests that interventions for short-term improvement in functional outcomes are effective, but few studies showed significant differences in long-term outcomes among the compared interventions.
Evidence for the treatment of CTS points primarily to the wearing of splints either full time or at night combined with exercise, which may include stretching, strengthening, or nerve or tendon gliding activities. Specifically, a combination of general splinting and lumbrical stretching holds the most promise for both short-term and long-term benefits (Baker et al., 2012). Mixed evidence exists for mobilization techniques and manual therapy for the treatment of CTS. The evidence for use of any physical agent modality for treatment of CTS is limited; this evidence partially supports the use of US for short-term improvements, but the effectiveness of LLLT and other modalities is not supported.
For people with distal radius fractures, moderate evidence shows that early intervention during immobilization leads to quicker recovery and that exercise of any type results in a positive effect on symptoms and functional outcomes. As such, the evidence suggests that instruction in an HEP may be just as effective as supervised activities with a therapist. However, none of the studies comparing HEPs with guided therapy evaluated moderating factors (e.g., impairment severity at initiation of care, comorbid conditions) to identify which patients would benefit the most from a directed holistic intervention by an occupational therapy practitioner versus an HEP. For patients with loss of wrist ROM, moderate evidence supports the use of joint mobilization, but no evidence supports the use of dynamic splinting.
Similar to findings for treatment of distal radius fracture, moderate evidence supports early active motion after extensor tendon repair, flexor tendon repair, and tendon transfer. For each of these conditions, early active motion leads to quicker recovery and earlier return to functional activities. Moreover, the evidence suggests that early motion among these patients also results in greater long-term outcomes than immobilization. Various protocols for early active motion all show beneficial results, but no protocol is clearly superior to another.
Exercise and splinting were frequently used interventions across the various diagnostic groups and were the primary interventions evaluated for RA and OA. Moderate evidence suggests that strengthening as part of an exercise program may be appropriate for patients with RA. Evidence also supports the use of splints to improve dexterity for RA patients with swan neck deformities and to improve functional outcomes for patients with mallet finger. However, no evidence supports one specific type of splint over another for treatment of these conditions, and no evidence supports the use of splints for RA-related boutonniere deformities. For patients with hand OA, the evidence for the use of exercise is limited, and the evidence for the use of spica splints for CMC OA is mixed.
In addition to common treatments, this systematic review identified multiple novel interventions for which the evidence suggests that additional higher level or higher quality studies are required: contralateral strengthening for patients with distal radius fracture during immobilization, targeted myofascial release and massage for treatment of CTS, kinesiotaping for people with RA, radial nerve mobilization for pain reduction in patients with CMC OA, and mirror therapy for patients with limited ROM.
Along with the need to examine these novel interventions, a gap in the literature exists regarding the evaluation of occupation-based interventions and outcomes. Although many of the studies involved occupational therapy practitioners who may have used occupation-based activities as part of their interventions, only 1 study described an intervention, other than patient education for energy conservation and joint protection, that would be considered occupation based (Harth et al., 2008). Moreover, although all the studies in this review used a measure associated with function (e.g., ROM, grip strength, subjective reports) as the primary outcome, very few studies directly measured occupation-based, functional outcomes. The paucity of evidence for occupation-based interventions and outcomes points to an opportunity and need to expand the scope of UE rehabilitation research.
Limitations of the Review
This systematic review has several limitations. First, given the broad scope of the research question and the amount of literature within each diagnostic category, it was possible to provide only a general synthesis of the overall effect of intervention types. We were not able to include detailed descriptions of each study for direct comparison; however, descriptions of the interventions and sample characteristics are provided in Supplemental Table 1 for reference and comparison. Second, because of the significant heterogeneity across studies, we were unable to tease out the effects of variations in dosage, provider experience, patient demographics, etiology of the condition, and specific characteristics of individual interventions (e.g., type of exercise, settings for modalities). The issue with heterogeneity of interventions was frequently noted in the other systematic reviews included in this synthesis, indicating a need for more thought in the design of future rehabilitation research studies.
Implications for Occupational Therapy Practice and Research
This systematic review summarizes the available evidence for the effectiveness of interventions used by occupational therapy practitioners in treating patients with MSDs of the forearm, wrist, and hand. The primary implications for occupational therapy practice and research are as follows:
For treatment of patients with CTS, the strongest evidence exists for use of night or full-time splinting combined with stretching or tendon or nerve gliding activities.
Whether directed by a therapist or completed as an HEP, exercise is a vital component of recovery after distal radius fracture.
Early activity motion is recommended for patients after fixation of distal radius fracture, surgical repair of flexor or extensor tendon injuries, and surgical tendon transfer.
Although no evidence strongly supports any one type of splinting, splinting is recommended for improvement in functional activities for patients with swan neck deformities and mallet finger; no evidence supports the use of splints for boutonniere deformity or Dupuytren’s contracture.
There is a paucity of studies evaluating the use of occupation-based interventions and outcomes for MSDs of the distal UE, indicating a need for research in this area to support the distinct value of occupational therapy.
Supplementary Material
Acknowledgments
We thank Deborah Lieberman and Marian Arbesman for their guidance and methodological support and Naoya Ogura and Justina Wong for their assistance with data management. A preliminary overview of the data included in this article was presented at the 2015 AOTA Annual Conference & Expo in Nashville, TN. Shawn C. Roll was funded by National Institutes of Health (NIH) Rehabilitation Research Career Development Program Grant K12 HD055929 at the time this article was prepared. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Footnotes
*Indicates studies that were included in the systematic review.
Contributor Information
Shawn C. Roll, Shawn C. Roll, PhD, OTR/L, RMSKS, FAOTA, is Assistant Professor, Mrs. T. H. Chan Division of Occupational Science and Occupational Therapy, University of Southern California, Los Angeles; sroll@usc.edu
Mark E. Hardison, Mark E. Hardison, MS, OTR/L, is PhD Student, Mrs. T. H. Chan Division of Occupational Science and Occupational Therapy, University of Southern California, Los Angeles
References
- American Occupational Therapy Association. (2014). Occupational therapy practice framework: Domain and process (3rd ed.). American Journal of Occupational Therapy, 68(Suppl. 1), S1–S48. https:/doi.org/10.5014/ajot.2014.682006 [PubMed] [Google Scholar]
- Amini D. (2011). Occupational therapy interventions for work-related injuries and conditions of the forearm, wrist, and hand: A systematic review. American Journal of Occupational Therapy, 65, 29–36. https:/doi.org/10.5014/ajot.2011.09186 [DOI] [PubMed] [Google Scholar]
- Arbesman M., Lieberman D., & Thomas V. J. (2011). Methodology for the systematic reviews on occupational therapy for individuals with work-related injuries and illnesses. American Journal of Occupational Therapy, 65, 10–15. https:/doi.org/10.5014/ajot.2011.09183 [DOI] [PubMed] [Google Scholar]
- *Ayhan C., Unal E., & Yakut Y. (2014). Core stabilisation reduces compensatory movement patterns in patients with injury to the arm: A randomized controlled trial. Clinical Rehabilitation, 28, 36–47. https:/doi.org/10.1177/0269215513492443 [DOI] [PubMed] [Google Scholar]
- *Baker N. A., Moehling K. K., Rubinstein E. N., Wollstein R., Gustafson N. P., & Baratz M. (2012). The comparative effectiveness of combined lumbrical muscle splints and stretches on symptoms and function in carpal tunnel syndrome. Archives of Physical Medicine and Rehabilitation, 93, 1–10. https:/doi.org/10.1016/j.apmr.2011.08.013 [DOI] [PubMed] [Google Scholar]
- *Bakhtiary A. H., Fatemi E., Emami M., & Malek M. (2013). Phonophoresis of dexamethasone sodium phosphate may manage pain and symptoms of patients with carpal tunnel syndrome. Clinical Journal of Pain, 29, 348–353. https:/doi.org/10.1097/AJP.0b013e318255c090 [DOI] [PubMed] [Google Scholar]
- *Becker S. J., Bot A. G., Curley S. E., Jupiter J. B., & Ring D. (2013). A prospective randomized comparison of neoprene vs thermoplast hand-based thumb spica splinting for trapeziometacarpal arthrosis. Osteoarthritis and Cartilage, 21, 668–675. https:/doi.org/10.1016/j.joca.2013.02.006 [DOI] [PubMed] [Google Scholar]
- *Bruder A., Taylor N. F., Dodd K. J., & Shields N. (2011). Exercise reduces impairment and improves activity in people after some upper limb fractures: A systematic review. Journal of Physiotherapy, 57, 71–82. https:/doi.org/10.1016/S1836-9553(11)70017-0 [DOI] [PubMed] [Google Scholar]
- Calfee R., Chu J., Sorensen A., Martens E., & Elfar J. (2015). What is the impact of comorbidities on self-rated hand function in patients with symptomatic trapeziometacarpal arthritis? Clinical Orthopaedics and Related Research, 473, 3477–3483. https:/doi.org/10.1007/s11999-015-4507-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Chang W. D., Wu J. H., Jiang J. A., Yeh C. Y., & Tsai C. T. (2008). Carpal tunnel syndrome treated with a diode laser: A controlled treatment of the transverse carpal ligament. Photomedicine and Laser Surgery, 26, 551–557. https:/doi.org/10.1089/pho.2007.2234 [DOI] [PubMed] [Google Scholar]
- *Chesney A., Chauhan A., Kattan A., Farrokhyar F., & Thoma A. (2011). Systematic review of flexor tendon rehabilitation protocols in Zone II of the hand. Plastic and Reconstructive Surgery, 127, 1583–1592. https:/doi.org/10.1097/PRS.0b013e318208d28e [DOI] [PubMed] [Google Scholar]
- *Collis J., Collocott S., Hing W., & Kelly E. (2013). The effect of night extension orthoses following surgical release of Dupuytren contracture: A single-center, randomized, controlled trial. Journal of Hand Surgery, 38, 1285–1294.e2. https:/doi.org/10.1016/j.jhsa.2013.04.012 [DOI] [PubMed] [Google Scholar]
- Coverdale J. J. (2012). An editorial note on nomenclature: Orthosis versus splint. Journal of Hand Therapy, 25, 3–4. https:/doi.org/10.1016/j.jht.2011.10.002 [Google Scholar]
- *Dakowicz A., Kuryliszyn-Moskal A., Kosztyła-Hojna B., Moskal D., & Latosiewicz R. (2011). Comparison of the long-term effectiveness of physiotherapy programs with low-level laser therapy and pulsed magnetic field in patients with carpal tunnel syndrome. Advances in Medical Sciences, 56, 270–274. https:/doi.org/10.2478/v10039-011-0041-z [DOI] [PubMed] [Google Scholar]
- *Glasgow C., Fleming J., Tooth L. R., & Peters S. (2012). Randomized controlled trial of daily total end range time (TERT) for Capener splinting of the stiff proximal interphalangeal joint. American Journal of Occupational Therapy, 66, 243–248. https:/doi.org/10.5014/ajot.2012.002816 [DOI] [PubMed] [Google Scholar]
- *Glasgow C., Tooth L. R., Fleming J., & Peters S. (2011). Dynamic splinting for the stiff hand after trauma: Predictors of contracture resolution. Journal of Hand Therapy, 24, 195–206. https:/doi.org/10.1016/j.jht.2011.03.001 [DOI] [PubMed] [Google Scholar]
- *Goransson I., & Cederlund R. (2011). A study of the effect of desensitization on hyperaesthesia in the hand and upper extremity after injury or surgery. Hand Therapy, 16, 12–18. https:/doi.org/10.1258/ht.2010.010023 [Google Scholar]
- *Gurcay E., Unlu E., Gurcay A. G., Tuncay R., & Cakci A. (2012). Assessment of phonophoresis and iontophoresis in the treatment of carpal tunnel syndrome: A randomized controlled trial. Rheumatology International, 32, 717–722. https:/doi.org/10.1007/s00296-010-1706-9 [DOI] [PubMed] [Google Scholar]
- *Hains G., Descarreaux M., Lamy A. M., & Hains F. (2010). A randomized controlled (intervention) trial of ischemic compression therapy for chronic carpal tunnel syndrome. Journal of the Canadian Chiropractic Association, 54, 155–163. [PMC free article] [PubMed] [Google Scholar]
- *Hall B., Lee H. C., Fitzgerald H., Byrne B., Barton A., & Lee A. H. (2013). Investigating the effectiveness of full-time wrist splinting and education in the treatment of carpal tunnel syndrome: A randomized controlled trial. American Journal of Occupational Therapy, 67, 448–459. https:/doi.org/10.5014/ajot.2013.006031 [DOI] [PubMed] [Google Scholar]
- *Hall B., Lee H., Page R., Rosenwax L., & Lee A. H. (2010). Comparing three postoperative treatment protocols for extensor tendon repair in Zones V and VI of the hand. American Journal of Occupational Therapy, 64, 682–688. https:/doi.org/10.5014/ajot.2010.09091 [DOI] [PubMed] [Google Scholar]
- *Handoll H. H., Madhok R., & Howe T. E. (2006). Rehabilitation for distal radial fractures in adults. Cochrane Database of Systematic Reviews, 2006, CD003324 https://doi.org/10.1002/14651858.CD003324 [DOI] [PubMed] [Google Scholar]
- *Harth A., Germann G., & Jester A. (2008). Evaluating the effectiveness of a patient-oriented hand rehabilitation programme. Journal of Hand Surgery (European Volume), 33, 771–778. https:/doi.org/10.1177/1753193408091602 [DOI] [PubMed] [Google Scholar]
- *Heiser R., O’Brien V. H., & Schwartz D. A. (2013). The use of joint mobilization to improve clinical outcomes in hand therapy: A systematic review of the literature. Journal of Hand Therapy, 26, 297–311. https:/doi.org/10.1016/j.jht.2013.07.004 [DOI] [PubMed] [Google Scholar]
- *Hermann M., Nilsen T., Eriksen C. S., Slatkowsky-Christensen B., Haugen I. K., & Kjeken I. (2014). Effects of a soft prefabricated thumb orthosis in carpometacarpal osteoarthritis. Scandinavian Journal of Occupational Therapy, 21, 31–39. https:/doi.org/10.3109/11038128.2013.851735 [DOI] [PubMed] [Google Scholar]
- Higgins J., & Altman D. G. (2008). Assessing risk of bias in included studies. In Higgins J. P. T., Altman D. G., & Sterne J. A. C. (Eds.), Cochrane handbook for systematic reviews of interventions (pp. 187–241). London: Cochrane Collection. Retrieved from http://handbook.cochrane.org/chapter_8/8_assessing_risk_of_bias_in_included_studies.htm
- *Hirth M. J., Bennett K., Mah E., Farrow H. C., Cavallo A. V., Ritz, M., & Findlay, M. W. (2011). Early return to work and improved range of motion with modified relative motion splinting: A retrospective comparison with immobilization splinting for Zones V and VI extensor tendon repairs. Hand Therapy, 16, 86–94. https:/doi.org/10.1258/ht.2011.011012 [Google Scholar]
- *Huisstede B. M., Hoogvliet P., Randsdorp M. S., Glerum S., van Middelkoop M., & Koes B. W. (2010). Carpal tunnel syndrome. Part I: Effectiveness of nonsurgical treatments—A systematic review. Archives of Physical Medicine and Rehabilitation, 91, 981–1004. https:/doi.org/10.1016/j.apmr.2010.03.022 [DOI] [PubMed] [Google Scholar]
- *Jerosch-Herold C., Shepstone L., Chojnowski A. J., Larson D., Barrett E., & Vaughan S. P. (2011). Night-time splinting after fasciectomy or dermo-fasciectomy for Dupuytren’s contracture: A pragmatic, multi-centre, randomised controlled trial. BMC Musculoskeletal Disorders, 12, 136 https:/doi.org/10.1186/1471-2474-12-136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Jongs R. A., Harvey L. A., Gwinn T., & Lucas B. R. (2012). Dynamic splints do not reduce contracture following distal radial fracture: A randomised controlled trial. Journal of Physiotherapy, 58, 173–180. https:/doi.org/10.1016/S1836-9553(12)70108-X [DOI] [PubMed] [Google Scholar]
- Kielhofner G. (2014). A meditation on the use of hands. Scandinavian Journal of Occupational Therapy, 21(Suppl. 1), 34–47. https:/doi.org/10.3109/11038128.2014.952901 [DOI] [PubMed] [Google Scholar]
- *Knygsand-Roenhoej K., & Maribo T. (2011). A randomized clinical controlled study comparing the effect of modified manual edema mobilization treatment with traditional edema technique in patients with a fracture of the distal radius. Journal of Hand Therapy, 24, 184–194. https:/doi.org/10.1016/j.jht.2010.10.009 [DOI] [PubMed] [Google Scholar]
- Kovacs L., Grob M., Zimmermann A., Eder M., Herschbach P., Henrich G., . . . Papadopulos N. A. (2011). Quality of life after severe hand injury. Journal of Plastic, Reconstructive and Aesthetic Surgery, 64, 1495–1502. https:/doi.org/10.1016/j.bjps.2011.05.022 [DOI] [PubMed] [Google Scholar]
- *Krischak G. D., Krasteva A., Schneider F., Gulkin D., Gebhard F., & Kramer M. (2009). Physiotherapy after volar plating of wrist fractures is effective using a home exercise program. Archives of Physical Medicine and Rehabilitation, 90, 537–544. https:/doi.org/10.1016/j.apmr.2008.09.575 [DOI] [PubMed] [Google Scholar]
- *Kuo L. C., Yang T. H., Hsu Y. Y., Wu P. T., Lin C. L., Hsu H. Y., & Jou I. M. (2013). Is progressive early digit mobilization intervention beneficial for patients with external fixation of distal radius fracture? A pilot randomized controlled trial. Clinical Rehabilitation, 27, 983–993. https:/doi.org/10.1177/0269215513487391 [DOI] [PubMed] [Google Scholar]
- Lieberman D., & Scheer J. (2002). AOTA’s Evidence-Based Literature Review Project: An overview. American Journal of Occupational Therapy, 56, 344–349. https:/doi.org/10.5014/ajot.56.3.344 [DOI] [PubMed] [Google Scholar]
- *Maddali Bongi S., Signorini M., Bassetti M., Del Rosso A., Orlandi M., & De Scisciolo G. (2013). A manual therapy intervention improves symptoms in patients with carpal tunnel syndrome: A pilot study. Rheumatology International, 33, 1233–1241. https:/doi.org/10.1007/s00296-012-2507-0 [DOI] [PubMed] [Google Scholar]
- *Madenci E., Altindag O., Koca I., Yilmaz M., & Gur A. (2012). Reliability and efficacy of the new massage technique on the treatment in the patients with carpal tunnel syndrome. Rheumatology International, 32, 3171–3179. https:/doi.org/10.1007/s00296-011-2149-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Magnus C. R., Arnold C. M., Johnston G., Dal-Bello Haas V., Basran J., Krentz J. R., & Farthing J. P. (2013). Cross-education for improving strength and mobility after distal radius fractures: A randomized controlled trial. Archives of Physical Medicine and Rehabilitation, 94, 1247–1255. https:/doi.org/10.1016/j.apmr.2013.03.005 [DOI] [PubMed] [Google Scholar]
- *Medina McKeon J. M., & Yancosek K. E. (2008). Neural gliding techniques for the treatment of carpal tunnel syndrome: A systematic review. Journal of Sport Rehabilitation, 17, 324–341. [DOI] [PubMed] [Google Scholar]
- *Miller L. K., Chester R., & Jerosch-Herold C. (2012). Effects of sensory reeducation programs on functional hand sensibility after median and ulnar repair: A systematic review. Journal of Hand Therapy, 25, 297–307. https:/doi.org/10.1016/j.jht.2012.04.001 [DOI] [PubMed] [Google Scholar]
- *Moe R. H., Kjeken I., Uhlig T., & Hagen K. B. (2009). There is inadequate evidence to determine the effectiveness of nonpharmacological and nonsurgical interventions for hand osteoarthritis: An overview of high-quality systematic reviews. Physical Therapy, 89, 1363–1370. https:/doi.org/10.2522/ptj.20080398 [DOI] [PubMed] [Google Scholar]
- Murray C. J., Atkinson C., Bhalla K., Birbeck G., Burstein R., Chou D., . . . Murray; U.S. Burden of Disease Collaborators. (2013). The state of US health, 1990–2010: Burden of diseases, injuries, and risk factors. JAMA, 310, 591–608. https:/doi.org/10.1001/jama.2013.13805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray C. J., Barber R. M., Foreman K. J., Abbasoglu Ozgoren A., Abd-Allah F., Abera S. F., . . . Vos T.; GBD 2013 DALYs and HALE Collaborators. (2015). Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: Quantifying the epidemiological transition. Lancet, 386, 2145–2191. https:/doi.org/10.1016/S0140-6736(15)61340-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- *O’Brien A. V., Jones P., Mullis R., Mulherin D., & Dziedzic K. (2006). Conservative hand therapy treatments in rheumatoid arthritis—A randomized controlled trial. Rheumatology, 45, 577–583. https:/doi.org/10.1093/rheumatology/kei215 [DOI] [PubMed] [Google Scholar]
- *O’Brien L. J., & Bailey M. J. (2011). Single blind, prospective, randomized controlled trial comparing dorsal aluminum and custom thermoplastic splints to stack splint for acute mallet finger. Archives of Physical Medicine and Rehabilitation, 92, 191–198. https:/doi.org/10.1016/j.apmr.2010.10.035 [DOI] [PubMed] [Google Scholar]
- *O’Connor D., Page M. J., Marshall S. C., & Massy-Westropp N. (2012). Ergonomic positioning or equipment for treating carpal tunnel syndrome. Cochrane Database of Systematic Reviews, 2012, CD009600 https:/doi.org/10.1002/14651858.CD009600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Page M. J., Massy-Westropp N., O’Connor D., & Pitt V. (2012). Splinting for carpal tunnel syndrome. Cochrane Database of Systematic Reviews, 2012, CD010003 https:/doi.org/10.1002/14651858.CD010003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Page M. J., O’Connor D., Pitt V., & Massy-Westropp N. (2012). Exercise and mobilisation interventions for carpal tunnel syndrome. Cochrane Database of Systematic Reviews, 2012, CD009899 http://dx.doi.org/10.1002/14651858.CD009899%20PubMedhttps:/doi.org/10.1002/14651858.CD009899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Page M. J., O’Connor D., Pitt V., & Massy-Westropp N. (2013). Therapeutic ultrasound for carpal tunnel syndrome. Cochrane Database of Systematic Reviews, 201 3, CD009601.https:/doi.org/10.1002/14651858.CD009601.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Peters S., Page M. J., Coppieters M. W., Ross M., & Johnston V. (2013). Rehabilitation following carpal tunnel release. Cochrane Database of Systematic Reviews, 2013, CD004158 https:/doi.org/10.1002/14651858.CD004158.pub2 [DOI] [PubMed] [Google Scholar]
- *Piazzini D. B., Aprile I., Ferrara P. E., Bertolini C., Tonali P., Maggi L., . . . Padua L. (2007). A systematic review of conservative treatment of carpal tunnel syndrome. Clinical Rehabilitation, 21, 299–314. https:/doi.org/10.1177/0269215507077294 [DOI] [PubMed] [Google Scholar]
- *Pike J., Mulpuri K., Metzger M., Ng G., Wells N., & Goetz T. (2010). Blinded, prospective, randomized clinical trial comparing volar, dorsal, and custom thermoplastic splinting in treatment of acute mallet finger. Journal of Hand Surgery, 35, 580–588. https:/doi.org/10.1016/j.jhsa.2010.01.005 [DOI] [PubMed] [Google Scholar]
- *Poolman R. W., Goslings J. C., Lee J. B., Statius Muller M., Steller E. P., & Struijs P. A. (2005). Conservative treatment for closed fifth (small finger) metacarpal neck fractures. Cochrane Database of Systematic Reviews , 2005, CD003210 https:/doi.org/10.1002/14651858.CD003210.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Rostami H. R., Arefi A., & Tabatabaei S. (2013). Effect of mirror therapy on hand function in patients with hand orthopaedic injuries: A randomized controlled trial. Disability and Rehabilitation, 35, 1647–1651. https:/doi.org/10.3109/09638288.2012.751132 [DOI] [PubMed] [Google Scholar]
- *Salim N., Abdullah S., Sapuan J., & Haflah N. H. (2012). Outcome of corticosteroid injection versus physiotherapy in the treatment of mild trigger fingers. Journal of Hand Surgery (European Volume), 37, 27–34. https:/doi.org/10.1177/1753193411415343 [DOI] [PubMed] [Google Scholar]
- *Sameem M., Wood T., Ignacy T., Thoma A., & Strumas N. (2011). A systematic review of rehabilitation protocols after surgical repair of the extensor tendons in Zones V–VIII of the hand. Journal of Hand Therapy, 24, 365–373. https:/doi.org/10.1016/j.jht.2011.06.005 [DOI] [PubMed] [Google Scholar]
- *Sawan S. A., Sayed Mahmoud H. M., & Hussien M. M. (2013). Effect of different physical therapy modalities on post-operative recovery following transverse carpal ligament release: A randomized controlled trial. Physiotherapy Practice and Research, 34, 75–82. https:/doi.org/10.3233/PPR-130024 [Google Scholar]
- Shea B. J., Grimshaw J. M., Wells G. A., Boers M., Andersson N., Hamel C., . . . Bouter L. M. (2007). Development of AMSTAR: A measurement tool to assess the methodological quality of systematic reviews. BMC Medical Research Methodology, 7, 10 https:/doi.org/10.1186/1471-2288-7-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Shi Q., & MacDermid J. C. (2011). Is surgical intervention more effective than non-surgical treatment for carpal tunnel syndrome? A systematic review. Journal of Orthopaedic Surgery and Research, 6, 17 https:/doi.org/10.1186/1749-799X-6-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel P., Watson M., Apodaca B., & Poole J. L. (2017). Evidence for occupational therapy interventions for adults with rheumatoid arthritis: A systematic review. American Journal of Occupational Therapy, 71, 7101180050. https:/doi.org/10.5014/ajot.2017.023176 [Google Scholar]
- *Silva P. G., Lombardi I. Jr., Breitschwerdt C., Poli Araújo P. M., & Natour J. (2008). Functional thumb orthosis for Type I and II boutonniere deformity on the dominant hand in patients with rheumatoid arthritis: A randomized controlled study. Clinical Rehabilitation, 22, 684–689. https:/doi.org/10.1177/0269215508088989 [DOI] [PubMed] [Google Scholar]
- *Souer J. S., Buijze G., & Ring D. (2011). A prospective randomized controlled trial comparing occupational therapy with independent exercises after volar plate fixation of a fracture of the distal part of the radius. Journal of Bone and Joint Surgery, 93, 1761–1766. https:/doi.org/10.2106/JBJS.J.01452 [DOI] [PubMed] [Google Scholar]
- *Sultana S. S., MacDermid J. C., Grewal R., & Rath S. (2013). The effectiveness of early mobilization after tendon transfers in the hand: A systematic review. Journal of Hand Therapy, 26, 1–21. https:/doi.org/10.1016/j.jht.2012.06.006 [DOI] [PubMed] [Google Scholar]
- *Szczegielniak J., Łuniewski J., Bogacz K., & Sliwiński Z. (2012). The use of kinesiology taping method in patients with rheumatoid hand—Pilot study. Ortopedia, Traumatologia, Rehabilitacja, 14, 23–30. https:/doi.org/10.5604/15093492.976896 [DOI] [PubMed] [Google Scholar]
- *Tascioglu F., Degirmenci N. A., Ozkan S., & Mehmetoglu O. (2012). Low-level laser in the treatment of carpal tunnel syndrome: Clinical, electrophysiological, and ultrasonographical evaluation. Rheumatology International, 32, 409–415. https:/doi.org/10.1007/s00296-010-1652-6 [DOI] [PubMed] [Google Scholar]
- *Thiele J., Nimmo R., Rowell W., Quinn S., & Jones G. (2009). A randomized single blind crossover trial comparing leather and commercial wrist splints for treating chronic wrist pain in adults. BMC Musculoskeletal Disorders, 10, 129 https:/doi.org/10.1186/1471-2474-10-129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Tocco S., Boccolari P., Landi A., Leonelli C., Mercanti C., Pogliacomi F., . . . Nedelec B. (2013). Effectiveness of cast immobilization in comparison to the gold-standard self-removal orthotic intervention for closed mallet fingers: A randomized clinical trial. Journal of Hand Therapy, 26, 191–201. https:/doi.org/10.1016/j.jht.2013.01.004 [DOI] [PubMed] [Google Scholar]
- U.S. Preventive Services Task Force. (2016). Grade definitions Retrieved from http://www.uspreventiveservicestaskforce.org/Page/Name/grade-definitions
- *Valdes K. (2009). A retrospective pilot study comparing the number of therapy visits required to regain functional wrist and forearm range of motion following volar plating of a distal radius fracture. Journal of Hand Therapy, 22, 312–319. https:/doi.org/10.1016/j.jht.2009.06.003 [DOI] [PubMed] [Google Scholar]
- *van der Giesen F. J., van Lankveld W. J., Kremers-Selten C., Peeters A. J., Stern E. B., Le Cessie S., . . . Vliet Vlieland T. P. (2009). Effectiveness of two finger splints for swan neck deformity in patients with rheumatoid arthritis: A randomized, crossover trial. Arthritis and Rheumatism, 61, 1025–1031. https:/doi.org/10.1002/art.24866 [DOI] [PubMed] [Google Scholar]
- *Villafañe J. H., Silva G. B., Bishop M. D., & Fernandez-Carnero J. (2012). Radial nerve mobilization decreases pain sensitivity and improves motor performance in patients with thumb carpometacarpal osteoarthritis: A randomized controlled trial. Archives of Physical Medicine and Rehabilitation, 93, 396–403. https:/doi.org/10.1016/j.apmr.2011.08.045 [DOI] [PubMed] [Google Scholar]
- *Wańczyk A., Pieniazek M., & Pelczar-Pieniazek M. (2008). Method and results of rehabilitation for extensor tendon injury of fingers II–V in Zone I and II. Ortopedia, Traumatologia, Rehabilitacja, 10, 218–225. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.