Abstract
Non-melanoma skin cancer (NMSC) is the most common cancer world-wide and the incidence continues to rise, in part due to increasing numbers in high-risk groups such as organ transplant recipients and those taking photosensitizing medications. The most significant risk factor for NMSC is ultraviolet radiation (UVR) from sunlight, specifically UVB, which is the leading cause of DNA damage, photoaging, and malignant transformation in the skin. Activation of apoptosis following UVR exposure allows the elimination of irreversibly damaged cells that may harbor oncogenic mutations. However, UVR also activates signaling cascades that promote the survival of these potentially cancerous cells, resulting in tumor initiation. Thus, the UVR-induced stress response in the skin is multi-faceted and requires coordinated activation of numerous pathways controlling DNA damage repair, inflammation, and kinase-mediated signal transduction that lead to either cell survival or cell death. This review focuses on the central signaling mechanisms that respond to UVR and the subsequent cellular changes. Given the prevalence of NMSC and the resulting health care burden, many of these pathways provide promising targets for continued study aimed at both chemoprevention and chemotherapy.
Keywords: non-melanoma skin cancer, ultraviolet radiation, DNA damage response, apoptosis, signal transduction
INTRODUCTION
There are an estimated 3.5 million people in the US who have been diagnosed with non-melanoma skin cancer (NMSC) making it the most common form of cancer in the country [1], with medical related costs reaching $650 million annually [2]. The incidence of NMSC is also high in the United Kingdom; it has been reported that 1 out of every 1000 individuals in the UK are diagnosed with the disease per year [3]. NMSC has become a major health concern in both countries as the incidence of NMSC in the US has increased a remarkable 300% since 1994 [4], while the rate of NMSC occurrence in the UK appears to be rising faster than any other European country [3]. NMSC is classified into two major forms: basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). BCCs, which arise from basal cell layer, constitute the majority of all diagnosed skin cancers (80%) and are rarely life threatening or metastatic. SCCs, which can arise from hair follicle stem cells [5], account for 16% of all skin cancers and are much more dangerous; these cancers are more likely to invade and metastasize [2, 6]. Incidence of NMSC, like many cancers, is much higher in older adults, and individuals who are over 60 years of age account for nearly 80% of all NSMC cases [6, 7]. More alarmingly however, the rate of NMSC occurrence is steadily increasing in patients younger than 35 years [8]. Taken together, these facts demonstrate the importance of understanding the molecular pathways behind NMSC development in order to increase our ability to diagnose, prevent and treat NMSC.
Ultraviolet radiation (UVR) from the sun is the greatest environmental risk factor for developing NMSC [9]. There are three distinct energetic forms of UV light that are emitted from the sun: UVA (320–400 nm), UVB (280–320 nm), and UVC (200–280 nm). However, only UVA and UVB pierce the atmosphere and reach the general populace [10]. Although UVA can penetrate deeper into the skin, UVB is the more energetic and accounts for the majority of the biologically damaging effects from sun exposure; these effects include direct DNA damage, activation of receptor-mediated signaling pathways, and formation of reactive oxygen species (ROS) [11]. Heightened exposure to UVR, both in intensity and in duration, directly increases the risk of NMSC. Therefore, individuals who are fair-skinned (Fitzpatrick Scale- Type I and II) spend large amounts of time in the sun or on tanning beds, and/or live near the equator are more susceptible to UVB-induced skin carcinogenesis [2, 6, 7, 9, 12]. Currently, according to American Cancer Society (ACS), the best methods for protecting against the harmful effects of UVR when outdoors are to wear protective clothing, seek shade when possible, apply copious amounts of sunblock, and protect the eyes with sunglasses. However, previous medical conditions can also dramatically increase an individual’s vulnerability to NMSC in response to UVR exposure, even when following these guidelines. Patients who have had SCCs or related diseases in the past have an increased chance to acquire additional SCCs, as well as melanoma [13]. Similarly, it has been shown that patients who take immunosuppressive drugs following an organ transplant are 60–100x more likely to develop SCC than the general population [14, 15].
The molecular mechanisms behind UVR-induced skin carcinogenesis are complex. UVR, specifically UVB, is considered a complete carcinogen as it can both initiate and promote cancer. UVR is able to penetrate through the skin to affect the keratinocyte stem cells, located in the basal layer of the epidermis. DNA damage can result from UVR-irradiation, which primarily generates cyclobutane pyrimidine dimers and (6–4) photoproducts [16]. These damaged cells will undergo DNA repair, most commonly through nucleotide excision repair (NER) to correct the UVR-induced damage [17]. The importance of the DNA repair response following UVR exposure cannot be underestimated. Individuals who are born with Xeroderma pigmentosum (XP), an autosomal recessive genetic disease resulting in mutations in NER, have an extraordinary 2000-fold increased incidence of NMSC and melanoma [18–20]. If the irradiated keratinocyte cannot repair the UVR-induced DNA damage, it will either undergo cell cycle arrest or initiate apoptosis as a regulatory defense mechanism [21]. Importantly, UVR-irradiation can also initiate tumorigenesis by inducing pro-survival pathways in keratinocytes that oppose and counteract apoptosis, thereby allowing damaged cells to survive. UVR can activate these pathways through direct DNA damage of critical target genes [22], activation of cell surface receptors [22], and/or increased inflammation and immunosuppression [23]. Many of these pathways can promote tumorigenesis through increased cell cycle progression and proliferation [2, 24]. Thus, it is important to understand how these pathways are regulated in order to develop novel drugs and therapeutic strategies to both treat NMSC, as well as act as chemopreventive agents in high-risk individuals. This review will highlight key signaling pathways that are activated in response to UVR and describe the downstream pathophysiological responses each pathway elicits.
DNA DAMAGE
DNA damage from direct UVR exposure results in the formation of cyclobutane pyrimidine dimers, (6–4) photoproducts, DNA cross-links, single strand breaks (SSB) and double strand breaks (DSB) [2]. If the DNA damage caused by the resulting adducts is not repaired, a UVR-specific permanent mutation is introduced into the genome. Specifically, a cytosine that is adjacent to a thymine or another cytosine is mutated to a thymine [25]. This mutation is commonly found in the tumor suppressor p53 gene of SCCs and historically was considered the the primary driver of NMSC initiation [26]. However, more recent studies have begun to show that, in addition to direct DNA damage, UVR-induced signal transduction can also play a central role in NMSC initiation. Due to the large number of molecular pathways that are activated in response to UVR, UVR exposure can elicit a response in keratinocytes that is simultaneously both oncogenic/pro-survival and tumor suppressive/apoptotic [27]. Alterations in any of these pathways in damaged cells can shift the balance in favor of survival or death. Among the first of these signaling mechanisms to be studied were the pathways controlled by the phosphatidylinositol 3-kinase-related kinases (PIKK kinases) ataxia telangiectasia mutated (ATM) and Rad3-related (ATR) proteins.
ATM/ATR signaling
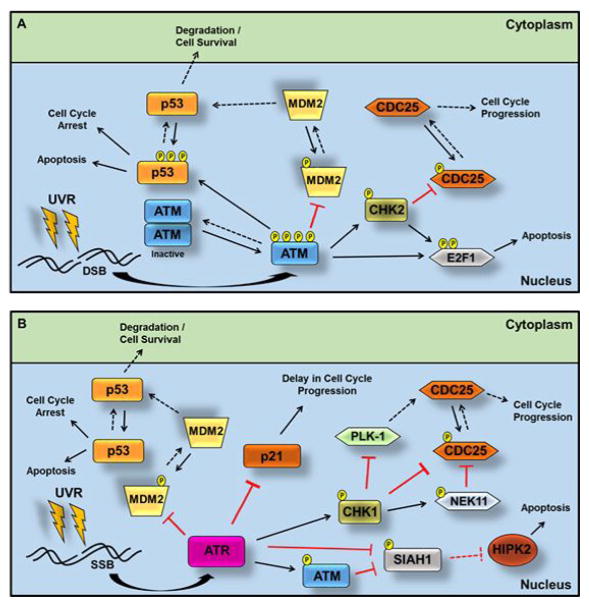
The PIKK family of proteins are critical in maintaining and regulating DNA damage checkpoints [28]. Specifically, ATM and ATR are essential proteins activated in response to UVR-induced DNA damage [29, 30]. In addition to their role in recruiting [31] or being recruited by [32] the DNA repair machinery to the site of damage, ATM and ATR activate a downstream signaling cascade that results in either repair or apoptosis, depending on the extent of DNA damage (Figure 1A,B). In the absence of stimulation, ATM resides as an inactive dimer. Upon UVR-induced DSB, ATM undergoes autophosphorylation (at Ser367, Ser1893, Ser1981 [33], and Ser2996 [34]) and becomes an active monomer [35], which subsequently phosphorylates checkpoint kinase 2 (CHK2) at Thr68 [36]. Activated CHK2 inhibits the CDC25 phosphatases through phosphorylation at Ser216, which promotes their degradation. This reduction in CDC25 activity prevents the cell from entering mitosis [37]. Additionally, ATM has been shown to phosphorylate p53 (at Ser9, Ser15, and Ser46), resulting in increased p53 stability and accumulation [38, 39], which leads to cell cycle arrest in G1 [40]. More recent studies have shown that in addition to direct p53 phosphorylation, ATM also phosphorylates the E3 ubiquitin-protein ligase mouse double minute 2 homolog (MDM2) at Ser394. MDM2 normally targets p53 for degradation; however, phosphorylation by ATM inhibits this action, further increasing the stability of p53 [41]. By halting the cell cycle through either CDC25 degradation or p53 accumulation, ATM provides the damaged cell both time to repair the DSB and also prevents its replication [28, 42]. The presence of DSB that cannot be repaired can trigger apoptosis as a result of prolonged activation of ATM. Both ATM and subsequent CHK2 activation can phosphorylate and activate the pro-apoptotic transcription factor E2F1 at Ser31 and Ser364 respectively [43, 44]. Therefore, ATM-dependent apoptosis can occur through increased activity of both p53 and E2F1 (Figure 1A).
Figure 1. ATM/ATR-dependent cell cycle arrest or apoptosis in response to UVR.
(A.) UVR-induced DSB trigger autophosphorylation of ATM at Ser367, Ser1893, Ser1981 and Ser2996. The active ATM monomer phosphorylates CHK2 at Thr68, which leads to inhibition of cell cycle progression through an inhibitory phosphorylation of CDC25 at Ser216. ATM can either directly phosphorylates p53 at Ser9, Ser15, and Ser46 or indirectly regulate p53 through phosphorylation (at Ser394) and inhibition of MDM2. Both of these events lead to cell cycle arrest or, with prolonged ATM activation, apoptosis. ATM can also phosphorylate CHK2 (at Ser364) and the transcription factor E2F1 (at Ser31), both of which ultimately lead to apoptosis. (B.) UVR-induced SSB lead to ATR activation and increased p53 stability through an inhibitory phosphorylation of MDM2 at Ser407. Direct phosphorylation (at Ser19) of the E3 ubiquitin ligase SIAH1 by ATR results in SIAH1 inhibition, which allows HIPK2 to activate p53. SIAH1 inhibition can also occur through ATR-dependent phosphorylation of ATM at Ser1981. Phosphorylation of CHK1 at Ser345 by ATR can lead to cell cycle arrest by several routes: CHK1 can directly phosphorylate CDC25 or indirectly inhibit CDC25 through NEK11 or PLK-1. Excessive DNA damage caused by high-dose UVB can also lead to promotion of apoptosis through p21 inhibition (see text for details). Solid lines indicate UVR-induced events, while dotted lines represent outcomes in the absence of UVR.
In contrast, ATR is activated by generation of SSB due to UV-induced damage and replication stress/stalling [28, 45]. Similar to ATM, ATR halts the cell cycle to allow sufficient time for DNA repair or, if the resulting DNA damage is too excessive, induce apoptosis. Interestingly, direct signaling cross-talk exists between the two kinases as activated ATR can directly phosphorylate ATM at Ser1981 in response to UV exposure, resulting in the activation of ATM [46]. UV-induced activation of ATR leads to the phosphorylation of checkpoint kinase 1 (CHK1) at Ser345 [47], which subsequently phosphorylates and inhibits CDC25 activity, halting the cell cycle in a manner similar to CHK2 [48]. CHK1 can also inhibit CDC25 activity by either the activation of Never In Mitosis A (NIMA)-Related Kinase 11 (NEK11), which phosphorylates and inhibits CDC25 [49, 50], or via direct inhibition of the polo-like kinase 1 (PLK-1), a known activator of CDC25 [51]. Analogous to the action of ATM, ATR increases p53 stability through phosphorylation of MDM2 at Ser407. This phosphorylation reduces the MDM2-dependent nuclear export of p53, thereby increasing p53 activity [52]. Both ATM and ATR can also directly phosphorylate (at Ser19) and inhibit the E3 ubiquitin ligase seven in absentia homologue 1 (SIAH1), resulting in activation of p53. In the absence of stimulation, SIAH1 promotes the degradation of the homeodomain-interacting protein kinase 2 (HIPK2) [53], thus preventing HIPK2 from activating p53 [54] (Figure 1B).
UVR-induced activation of ATR has also been linked to the cyclin-dependent kinase inhibitor p21WAF1/Cip1 (p21) pathway, which interacts with numerous cyclins/CDKs to halt the cell cycle [55]. Reports show that ATR has UVR dosage dependent, paradoxical effects on the p21 pathway. At high doses, ATR inhibits p21, which appears counter-intuitive; however, this inhibition has been shown to promote apoptosis [56], which may be the result of excessive DNA damage. Interestingly, low dose UVR protects p21 from s-phase kinase-associated protein 2 (SKP2)-mediated degradation, leading to a delay in cell cycle progression to allow DNA repair [57]. Furthering the complexity, a recent report shows that high energy UVC exposure can lead to increased p21 mRNA stability in a CHK1-dependent fashion via cytoplasmic localization of the RNA binding protein HuR. In the absence of ATR activation, HuR is localized to the nucleus due to cyclin-dependent kinase 1 (CDK1)-dependent phosphorylation of HuR at Ser202. Activation of ATR/CHK1 inhibits CDK1, which allows HuR to translocate to the cytoplasm and stabilize p21 mRNA [58]. While several reports show that complete inhibition of ATR can increase both tumor development and aging [59, 60], another study found that the diminished expression/function of ATR in UVR-sensitive mice resulted in protection from UVR-induced skin carcinogenesis [61]. Therefore, when developing therapeutics that target DNA repair proteins for the treatment of NMSC, it is important to consider how different levels of activity of these proteins may affect skin tumorigenesis.
INFLAMMATION
Multiple studies have shown an association between inflammation and the promotion of various cancer types, and inflammation has been referred to as the “seventh hallmark of cancer” [62–64]. In fact, the correlation between cancer and inflammation dates back to 1863, when Rudolf Virchow discovered leukocytes associated with tumor cells [65]. Inflammatory pathways are classically activated upon skin injury via UVR-induced sunburn, which stimulates the dilation of blood vessels to increase blood supply to the injury site, changes in the microvascular structure that help plasma proteins enter from the blood stream, and increased migration of white blood cells to the site through the endothelium [66]. These responses create a microenvironment that aids in wound healing. However, this environment can be hijacked to help stimulate tumorigenesis [62]. Inflammation has been shown to increase keratinocyte survival, proliferation, and transformation in NMSC development and progression, as well as promoting invasion and metastasis [66]. Clinical studies have demonstrated that inflammation is involved in the progression from actinic keratosis (AK) to SCC. Additionally, chronic inflammation is consistently observed in the invasive periphery of tumor cells in patients with SCC [66]. Since inflammation is a hallmark response of sunburned skin [67], it is of obvious importance to understand the molecular pathways involved and their effect on NMSC progression. Here we will highlight two key inflammatory pathways involved in UVR-induced inflammation: the nuclear factor kappa-light-chain-enhancer of activated B cells (NFκB) pathway and the signal transducer and activator of transcription 3 (STAT3) pathway.
The NFκB pathway
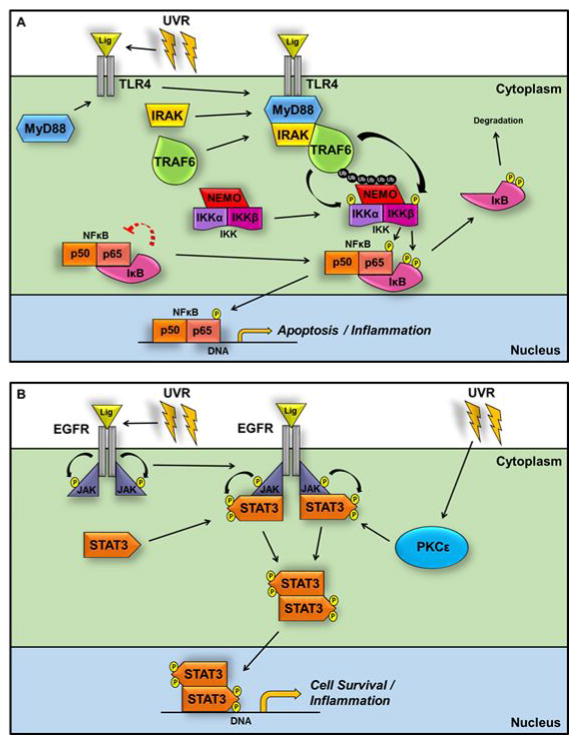
The NFκB pathway has been extensively studied and revealed to be crucial in mediating inflammation of the skin (reviewed in [68]). Inactive NFκB exists primarily as a cytoplasmic heterodimer of the p65 and p50 subunits, which are bound to the inhibitory protein IκB. Induction of the canonical NFκB pathway can occur either via direct UVR activation or by the binding of UV-induced cytokines to plasma membrane receptors. The most commonly associated receptors with NFκB activation in NMSC are Receptor Tyrosine Kinases (RTK, discussed elsewhere in this review), Tumor Necrosis Factor receptors (TNFR1, reviewed in [69]), and Toll-like receptors (TLRs), specifically TLR2, 3, & 4 [70] (Figure 2A). In general, TLR activation occurs following UVR-induced ligand binding, which recruits the I kappa B kinase (IKK) complex, consisting of IKKα and β, as well as the NFκB essential modulator (NEMO/IKKγ), to the TLR receptor, resulting in activation of IKK and subsequently, NFκB. Specifically, activation of the TLR4 induces a conformational change, which allows binding of the Myeloid Differentiation Primary Response 88 (MyD88) protein to the TLR. The IL-1 receptor-associated kinase (IRAK) family of kinases then bind to MyD88, inducing autophosphorylation and activation of IRAK [71] and recruitment of TNF receptor associated factor 6 (TRAF6) proteins. TRAF6 proteins are E3 ubiquitin ligases that interact with ubiquitin conjugating enzymes to promote the creation of polyubiquitin chains [72]. The recruitment of the IKK complex to the newly formed ubiquitin chains at the receptor is driven by the ubiquitin-binding protein NEMO. This NEMO-dependent binding of the IKK complex to TRAF6 allows for the proximal phosphorylation and activation of IKK (at Ser177&181 for IKKβ and at Ser176&180 for IKKα) [73–75]. The activated IKK proteins in turn phosphorylate IκB at Ser32 and Ser36, inducing ubiquitination and proteasomal degradation of the protein and releasing the inhibition of NFκB [76]. The active NFκB heterodimer translocates to the nucleus to promote the transcription of pro-inflammatory genes [77], specifically genes that control apoptosis, as well as genes that lead to the production of cytokines and interferons that regulate the immune/inflammatory response. Among these targets are TNFα, IL-1, IL-6 and IL-8 [78]. IKK can also phosphorylate the p65/50 dimer directly at Ser536 of p65. This phosphorylation site has been shown to further increase NFκB nuclear transcriptional activity [79, 80]. Recent reports show that the p65 subunit of NFκB is essential for skin carcinogenesis in mice. Loss of p65 prevented both SCC tumor initiation and tumor promotion [77]. Other reports show that dsRNA released from UVB-induced necrotic keratinocytes can activate TLR3, which results in the archetypal sunburned skin inflammatory response [81]. In addition, there are numerous studies that link activation of NFκB to a variety of other skin diseases (reviewed in [82]).
Figure 2. The inflammatory response to UVR acts through TLR4-dependent NFκB signaling and EGFR-dependent activation of STAT3.
UVR-induced sunburn activates an inflammatory response that includes pathways dependent on NFκB and STAT3. (A.) Ligand binding recruits MyD88 to TLR4. IRAK binding to MyD88 causes autophosphorylation and activation of IRAK and recruits the TRAF6 E3 ubiquitin ligases. NEMO-dependent binding of the IKK complex to TRAF6 allows phosphorylation and activation of IKK (at Ser177&181 for IKKβ and at Ser176&180 for IKKα). Activated IKK phosphorylates IκB at Ser32 and Ser36 to induce ubiquitination and proteasomal degradation of IκB and release of the active NFκB heterodimer, which translocates to the nucleus to promote the transcription of pro-inflammatory genes. IKK can also phosphorylate the p65/50 dimer directly at Ser536 of p65. (B.) Activation of EGFR in response to UVR leads to the phosphorylation of Jak, which allows the recruitment of STAT3 to the receptor complex through binding of its SH2 domain to Jak. STAT3 is subsequently phosphorylated at Tyr705, allowing dimerization and increased transcription of pro-inflammatory genes. Activation of PKCε by ROS results in direct phosphorylation of STAT3 at Ser727, further increasing STAT3-dependent transcription.
The STAT3 pathway
The STAT family of transcription factors are induced in response to growth factors and cytokines. This family of proteins regulates factors that can affect both tumorigenesis and the tumor microenvironment [83]. STAT3 has been shown to play an important role in survival and proliferation of keratinocytes exposed to UVB. Targeted overexpression of STAT3 in the basal epidermis (K14-STAT3) accelerates skin tumor formation in mice exposed to UVB, while targeted deletion of STAT3 in the same cells confers resistance [84]. Interestingly, altering STAT3 activity within basal keratinocytes has profound effects on hair follicle stem cells and skin progenitor cells [85], which are implicated as the origin cells in NMSCs. Constitutively active STAT3 has been found in both mouse and human SCCs, and plays a role in promoting skin inflammation during tumor development [86]. In the canonical STAT3 pathway (Figure 2B), UVR exposure activates the epidermal growth factor receptor (EGFR), a cell surface RTK, which phosphorylates the Janus-associated-kinase (Jak). This allows the recruitment of STAT3 to the receptor complex through binding of the Src Homology 2 (SH2) domain of STAT3 to phosphorylated Jak [87]. Following recruitment, STAT3 is phosphorylated at Tyr705, which induces dimerization of STAT3 and allows it to bind to DNA and increase transcription of pro-inflammatory genes [88]. Specifically, STAT3 promotes the transcription of numerous genes that are related to inflammation (ie. interleukins), tumor promotion (c-Myc and c-Fos), cell survival (Bcl-2, Cyclin D1 and Survivin), and metastasis (Twist and Zeb1) [89, 90]. Additionally, studies in mice have shown that UVR-induced reactive oxygen species (ROS) activates protein kinase c epsilon (PKCε), which directly phosphorylates STAT3 at Ser727 [91, 92]. While phosphorylation of STAT3 at Tyr705 is required to activate STAT3 transcriptional activity, studies show that dual phosphorylation of STAT3 at Tyr705 and Ser727 further increases the activity of STAT3-dependent transcription [91, 93]. Non-canonical STAT3 pathways have also been linked to tumorigenesis of various cancers. It is important to note that while little is currently known of the non-canonical STAT3 pathways in UVR-induced skin carcinogenesis, these pathways are being actively investigated [94, 95].
OXIDATIVE STRESS
UVR exposure activates multiple stress response pathways in keratinocytes. Oxidative stress, defined as unbalanced ROS production and antioxidant defenses, has been linked to the initiation of numerous cancers, including NMSC [96]. Antioxidants have shown clinical efficacy to both prevent and treat cancer [97]. However, recent studies show that prolonged increases in ROS production within cancer cells have tumor suppressive roles and initiate apoptotic pathways; therefore, administering antioxidative therapies may actually harm a patient depending on the stage of their cancer [98]. Importantly, UVR exposure transiently increases ROS production within the skin both immediately following UVR-irritation, as well as in a second response up to 3 hours later [99]. Depending on the activated molecular pathway, UVR-induced oxidative stress has been linked to multiple skin conditions including aging, inflammation and skin cancer. There is an inherent defense network present in keratinocytes to combat ROS accumulation; however, following UVB exposure, ROS production can be increased to such high levels that these antioxidative defenses are overwhelmed [100]. Tumor development can result from a combination of increased ROS production and reduced antioxidant defense mechanisms in the skin, which leads to DNA damage and activating mutations [101, 102]. Interestingly, differences in the accumulation of antioxidant enzymes such as the superoxide dismutases and catalase were observed in patient biopsies of both non-melanoma and melanoma tumors. NMSC had strikingly lower levels of these enzymes than their melanoma counterparts, suggesting that chronic UVR exposure associated with NMSC development leads to weakened antioxidant defense response during tumorigenesis [103]. This review describes two critical pathways that are activated in response to UVR-induced oxidative stress NMSC development: the p38 mitogen-activated protein kinases (p38) pathway and c-Jun N-terminal kinases (JNK) pathway.
p38 signaling
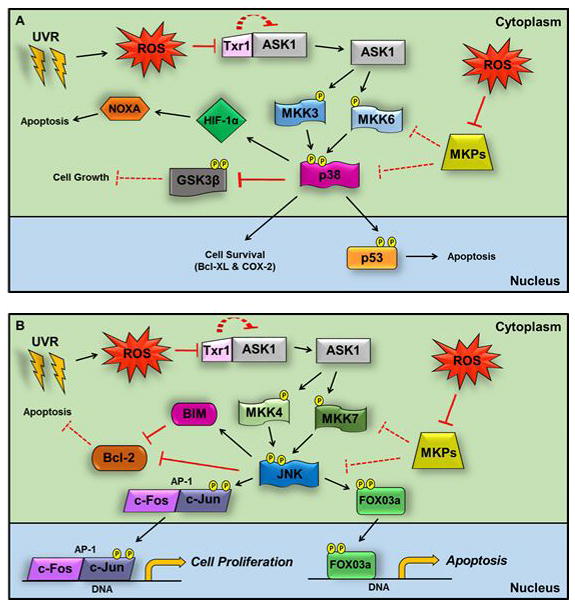
The pathophysiological effect of UVR-induced activation of both p38 and JNK in keratinocytes is controversial, as reports show that these stress response proteins can elicit both pro- and anti-survival mechanisms [104]. However, given the bimodal role that oxidative stress plays in cancer, this seemingly contradictory response is not surprising. p38 is a member of the mitogen-activated protein kinase (MAPK) family of proteins and responds to a variety of cellular stress stimuli, including oxidative stress (Figure 3A). The dual specificity mitogen-activated protein kinase kinase (MKK) 3 and 6 phosphorylate p38 at Thr180 and Tyr182 within the activation loop of the protein. Once active, p38 phosphorylates both cytoplasmic and nuclear targets [105]. ROS-dependent activation of p38 in keratinocytes has also been linked with activation of apoptosis signal-regulating kinase 1 (ASK1), a member of the MAP Kinase Kinase Kinase (MAP3K) family of proteins that is upstream of both p38 and MKK3/6. Under oxidative stress, activation of ASK1 occurs following disassociation from the inhibitory thiol-disulphide oxidoreductase thioredoxin-1 (Trx1) protein [106]. Other studies reveal that cells lacking specific mitogen-activated protein kinase phosphatases (MKP), phosphatases that target MAPKs, have increased p38 activation following UVR exposure. Importantly, increased ROS production has been shown to inhibit MKPs, which triggers increased p38 activation in response to elevated oxidative stress [107, 108]. It is also important to note that UVR can activate the p38 pathway independent of oxidative stress. Specifically, UVR-induced DNA damage can elicit a p38 response and can regulate the cell cycle through activation of MAPKAPK-2 (MK2) [109, 110].
Figure 3. UVR-induced reactive oxygen species activate p38- and JNK-dependent signaling.
UVR-induced activation of p38 and JNK in keratinocytes can elicit both pro- and anti-survival mechanisms. (A.) In the presence of ROS, ASK1 is activated by dissociation from Trx1. ASK1 phosphorylates MKK 3 and 6, which activate p38 by phosphorylation at Thr180 and Tyr182. ROS production also inhibits MKPs, which results in increased p38 activation. Once activated, p38 can act on multiple targets. It can promote apoptosis by phosphorylating p53 at Ser33 and Ser46 or induce NOXA-dependent apoptosis through increased protein expression of HIF-1α. Conversely, p38 can increase cell survival by upregulating Bcl-XL and COX-2 or direct phosphorylation of GSK3β at Thr43 and Thr 390. (B.) Analogous to p38, after phosphorylation by ASK1, MKK4 and 7 activate JNK by phosphorylating Thr183 and Tyr185. Reduced MKP activity can also activate JNK. JNK targets include the AP1 transcription factor, which stimulates cell proliferation in the presence of UVB as a result of JNK phosphorylation of c-Jun at Ser63 and Ser73. Conversely, JNK can respond to excessive damage by activating apoptosis. High dose UVB can induce JNK-dependent nuclear localization of the pro-apoptotic factor FOXO3a, and JNK can inhibit the pro-survival Bcl-2 either directly or indirectly though activation of BIM.
Recent studies have demonstrated that inhibition of p38 increases cell survival in murine SCC in vivo [111, 112]. In agreement with this, activation of p38 in response to UVR promotes apoptosis in keratinocytes by phosphorylating p53 at Ser33 and Ser46, which increases the apoptotic activity of p53 [113]. Other reports indicate that UVR-induced p38 activation induces NOXA-dependent apoptosis through increased protein expression of hypoxia-inducible factor 1-alpha (HIF-1α) in a p53-independent manner [114]. In contrast, it has been shown that p38 activation increases UVR-induced survival of keratinocytes though upregulation of the cancer associated genes Bcl-XL and COX-2 [104]. Activation of p38 can also directly phosphorylate glycogen synthase kinase 3 beta (GSK3β) at Thr43 and Thr 390 (Ser389 in mice), which promotes β-catenin dependent growth and proliferation [115]. Moreover, transgenic mice expressing a dominant negative p38 protein are resistant to skin carcinogenesis upon exposure to chronic UVR-irradiation, perhaps due to a reduction in p38-dependent hyperproliferation [116].
JNK signaling
JNK, like p38, is a member of the MAPK family that is activated upon phosphorylation following oxidative stress by upstream MKKs (MKK4 and 7) at Thr183 and Tyr185 (Figure 3B). MKK4 and 7, like MKK3 and 6, are activated in response to ROS production through either increased ASK-1 activity or reduced MKP activity [117]. JNK activation occurs in human keratinocytes as quickly as 5 minutes following UVR exposure, with maximal activity peaking at 30 min post-UVR. This correlates perfectly with UVR-induced p38 kinase activity [118]. A major target of JNK is the transcription factor activator protein-1 (AP-1). AP-1 exists as either a homodimer containing two c-Jun or c-Fos proteins, or a heterodimer containing one of each. AP-1 is known primarily as an oncogenic transcription factor as it is involved in promoting cell proliferation, specifically through transcription of cell cycle regulator genes (such as cyclin D1, cyclin A, cyclin E, p53, p21, p16Ink4a and p19ARF). Additionally, AP-1 can elicit a cell survival response through crosstalk with NFκB [119]. Once activated, JNK can phosphorylate c-Jun at Ser63 and Ser73 [120] and this phosphorylation increases AP-1 activity in response to UVR exposure [121]. Bowden and colleagues showed that pharmacological inhibition of JNK in human keratinocytes sensitizes cells to UVR-induced apoptosis in vitro [122], which correlates with a study by the same group showing that in vivo inhibition of AP-1 protected transgenic mice expressing a dominant negative c-jun from UVB-induced SCC [123]. Additionally, pharmacological inhibition of JNK inhibited the growth of xenograft studies using human head and neck SCCs in mice [124]. However, similar to p38, JNK activation can induce a pro-apoptotic response. Exposure of lung adenocarcinoma ASTC-a-1 cells to high dose UVB results in JNK-dependent nuclear localization of the pro-apoptotic factor FOXO3a (discussed elsewhere in this review) [125], but this localization does not occur with lower doses of UVB. This low vs high dosage effect may be similar to the response described above for ATR. Specifically, UVR-dependent JNK activation is initially protective; however, when the damage induced by UVR-irradiation reaches a threshold level, the JNK-mediated signaling mechanisms within the cell activate apoptosis. It has also been shown in HEK293T cells that UVR-induced JNK activation can induce mitochondrial-derived intrinsic apoptosis through inhibition of Bcl-2 directly, or indirectly though activation of BIM (Bcl-2-like protein 11) [126]. However, this effect has not yet been studied in keratinocytes.
RTK ACTIVATION
As mentioned above, activation of various signaling pathways in the skin can occur as quickly as 5 minutes following exposure to UVR with peak activity occurring between 30 minutes to 1 hour on average [127–129]. The RTKs belong to an important family of receptors that are rapidly activated in response to UVR and have been linked to NMSC [24, 130, 131]. Key RTKs that are induced in response to UVR include the insulin receptor (IR), the insulin like growth factor 1 receptor (IGF-1-R), and EGFR [132]. Activation occurs when two transmembrane RTK subunits dimerize, typically in response to ligand binding, which induces autophosphorylation of their cytosolic kinase domains. While UVR-induced autocrine activation of RTKs has been previously described [133–135], the near immediate activation of RTKs upon exposure to UVR may be independent of ligand binding. Studies have shown that RTK activation can be propagated through UVR-induced ROS production [136, 137], while other reports suggest the possibility that activation occurs through cell surface clustering of RTKs in response to UVR to promote autophosphorylation and subsequent activation [137, 138]. RTK activation in keratinocytes predominantly initiates an anti-apoptotic and cell proliferative response, which are critical processes for both wound repair and growth of new skin [139]. However, aberrant UVB-induced activation of RTK pathways can lead to both NMSC initiation and promotion [7]. It is for this reason that a variety of drugs are being developed to target and inhibit RTKs directly, as well as inhibiting the downstream components of the RTK signaling cascade (see for example [140, 141]). This review discusses the two best-studied NMSC-related RTK pathways: the phosphoinositide 3-kinase (PI3K)/mechanistic (mammalian) target of rapamycin (mTOR) pathway and the rapidly accelerated fibrosarcoma kinase (RAF)/mitogen-activated protein kinase kinase (MEK)/extracellular signal-regulated kinases (ERK) pathway.
PI3K/mTOR signaling
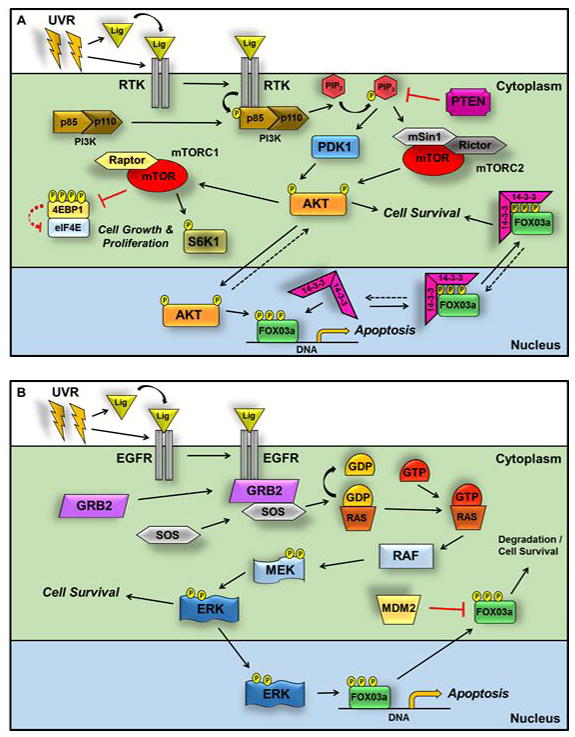
The serine/threonine kinase mTOR is a PIKK kinase that is part of an incompletely defined signaling network that responds to diverse nutrients, growth factors and cellular stressors [142–144], including UVR [129, 145, 146]. mTOR exists in two distinct signaling complexes: the rapamycin-sensitive mTOR complex 1 (mTORC1) and the rapamycin-resistant mTORC2 [143], both of which are important in NMSC development in response to UVB exposure. mTOR was identified as a therapeutic target in several cancer types, as upregulated mTOR signaling is frequently found in cancers [142–144]. Additionally, mutations in two critical upstream proteins of the mTOR pathway, PI3K and phosphatase and tensin homolog (PTEN), are commonly found in NMSC [147, 148]. Reports show that increased levels of both mTORC1 and mTORC2 activity are present during progression from normal keratinocytes to pre-cancerous actinic keratosis, and culminating in NMSC development [149]. Activation of mTORC1-dependent pathways (Figure 4A) occurs following upstream activation of Protein Kinase B (AKT/PKB) via the PI3K pathway. Following autophosphorylation of the UVR-inducible RTKs (EGFR, IGF-R-1, and IR), PI3K, a heterodimer that consists of the p85 regulator subunit and the p110 kinase subunit, is recruited to the receptor through binding of the SH2 domain on p85 to the phosphorylated RTK. The p85 subunit is subsequently phosphorylated at Tyr458, activating the heterodimer. This allows PI3K to phosphorylate the phospholipid phosphatidylinositol 4,5-bisphosphate (PIP2) to generate phosphatidylinositol (3,4,5)- trisphosphate (PIP3) on the plasma membrane. PIP3 recruits both phosphoinositide-dependent kinase-1 (PDK1) and AKT to the receptor complex, where PDK1 can activate and phosphorylate AKT at Thr308. AKT is a central regulator of numerous cellular processes including cell survival, metabolism, protein translation, and angiogenesis [150]. Three AKT isoforms have been described, of which AKT1 and 2 have been strongly implicated in tumorigenesis; however, studies suggest that melanoma development may depended on AKT3 [151]. The tumor suppressor PTEN negatively regulates PI3K-dependent signaling though PIP3 dephosphorylation and conversion to PIP2. Phosphorylation by PDK1 activates AKT, which subsequently phosphorylates and inhibits the mTORC1 negative regulator Tuberous Sclerosis Complex 1/2 (TSC1/2). This inhibition allows the ras homolog enriched in brain (RHEB) GTPase to bind to and activate mTORC1 [152]. mTORC1 activation leads to cell growth and proliferation primarily through the downstream phosphorylation (at Thr389) and activation of ribosomal protein S6 kinase beta-1 (S6K1), which controls ribosome biogenesis, as well as activation of cap-dependent translation via the phosphorylation (at Thr37, Thr46, Ser65, and Thr70) and subsequent degradation of the eukaryotic translation initiation factor 4E (eIF4E) inhibitory 4E-binding protein 1 (4E-BP1) [153]. This mTORC1-dependent signaling cascade has been described in detail in multiple reviews [142–144, 154–156].
Figure 4. RTK activation by UVR results in an anti-apoptotic and cell proliferative response through PI3K/mTOR and Raf/MEK/ERK-dependent pathways.
(A.) Autophosphorylation of multiple UVR-inducible RTKs activates the PI3K heterodimer by recruitment to the receptor and binding of the p85 subunit SH2 domain. Phosphorylation of p85 at Tyr458 activates the heterodimer, and PI3K phosphorylates PIP2 to generate PIP3. PIP3 recruits PDK1 and AKT to the receptor complex, where PDK1 activates AKT by phosphorylation of Thr308. Once phosphorylated, AKT leads to mTORC1 activation (see text for details), which regulates proliferation and ribosome biogenesis by phosphorylation of S6K1 at Thr389 and cap-dependent translation by phosphorylation (at Thr37, Thr46, Ser65, and Thr70) and degradation of 4EBP1. PTEN negatively regulates PI3K-dependent signaling though PIP3 dephosphorylation and conversion to PIP2. To activate mTORC2, the PH domain of SIN1 binds to PIP3 to uncover the active kinase site of mTOR. PIP3 recruits AKT to mTORC2, and mTORC2 phosphorylates AKT at the hydrophobic motif site Ser473. Dual phosphorylation of AKT at Thr308 and Ser473 controls cell survival pathways by inhibition of pro-apoptotic proteins such as the FOXO3a transcription factor. AKT-dependent phosphorylation of FOXO3a at Thr32, Ser256 and Ser319 causes association of the 14-3-3ζ chaperone, which binds to this motif and sequesters FOXO3a in the cytoplasm. (B.) When Raf/MEK/ERK signaling is stimulated, GRB2 and SOS are recruited to the activated EGFR. Following exchange of GDP for GTP, the Ras GTPase induces RAF activation, which phosphorylates MEK1 and 2 at Ser217 and Ser221, respectively. ERK is activated by MEK-dependent phosphorylation at Thr202 and Tyr204 and regulates numerous downstream targets (see text for details), including FOXO3a. Phosphorylation of FOXO3a at Ser294, Ser344, and Ser425 triggers exit of FOXO3a into the cytoplasm in a 14-3-3-independent manner. In the absence of its association with 14-3-3, FOXO3a is targeted for MDM2-mediated cytoplasmic degradation.
Activation of mTORC1 plays a causal role in tumor promotion [157], and the mTORC1 specific inhibitor rapamycin (Sirolimus) is approved as a therapeutic in multiple cancer types [141, 158–160]. Rapamycin allosterically inhibits mTORC1 by binding to the FK-binding protein 12 (FKBP12) in the cytosol, which can then directly bind to the mTOR kinase subunit of mTORC1 and block its function [161]. Notably, rapamycin has no direct inhibitory effect on the activity of mTORC2 and, depending on length of exposure and tissue type, the indirect effects of rapamycin treatment on mTORC2 can vary [162]. DiGiovanni and colleagues showed that mTORC1 inhibition with topical rapamycin blocks dermal inflammation that is linked with the hyperproliferative response to tumor promotion in mice [163]. In addition, organ-transplant patients who took rapamycin as an immunosuppressive drug had a significant reduction in acquired NMSC when compared to patients taking cyclosporine A [164]. Our lab and others have demonstrated that mTORC1 is required for keratinocyte hyperproliferation in response to tumor promotion in murine skin carcinogenesis models [129, 165]. There is controversy regarding the role of mTORC1 in NMSC tumor initiation. Studies in other cancer models demonstrate that treatment with rapamycin can either increase or decrease cell survival [166–170]. Studies from our lab showed that treatment with rapamycin or genetic knockdown of the essential mTORC1 scaffolding protein Raptor does not affect cell viability or apoptosis following exposure to UVB in spontaneously immortalized human keratinocytes (HaCaT cells) or mouse primary keratinocytes [129, 145]. In contrast, a recent report by Bowden and colleagues showed that rapamycin treatment did increase UVR-induced keratinocyte cell death in mice [165]. The differing results seen in these studies are likely due to the differences in both model systems and UVR-dosages used. For example, our in vitro studies used UVB dosages between 20–35 mJ/cm2, whereas the Bowden group used 640 mJ/cm2 UVB for acute in vivo exposure experiments.
Studies linking mTORC2 to tumor initiation have suggested that this less studied of the mTOR complexes is also a viable target for therapeutic intervention [171]. Using mouse models with stage-specific deletion of Rictor in the basal layer of the epidermis, our recent work has established an essential role for mTORC2-controlled pathways in both skin tumor development and maintenance [145]. These results suggest that inhibition of mTORC2 signaling may be an effective strategy for both treatment and prevention of NMSC. Though the mechanism of mTORC2 signaling is only partially defined (Figure 4A), recent reports show that the activation of mTORC2 occurs following PIP3 phosphorylation by PI3K [172]. The pleckstrin homology (PH) domain of the mTORC2 scaffolding/inhibitory protein SIN1 is recruited to the plasma membrane, where it binds to PIP3. Binding of SIN1 to PIP3 induces a conformational change in mTORC2 and uncovers the active kinase site of mTOR [173]. The first role described for mTORC2 was the control of actin cytoskeleton rearrangement [174]; however, induction of mTORC2 also activates both the serum-and glucocorticoid-induced protein kinase SGK and AKT, both of which are involved in controlling apoptosis in response to various cellular stresses and have been implicated as potential therapeutic targets in cancer [171]. Following its initial binding of mTORC2, PIP3 recruits the PH domain of AKT to mTORC2, which permits the phosphorylation of AKT at the hydrophobic motif site Ser473 by mTORC2 [173]. Recent studies have revealed that the DNA-dependent protein kinase catalytic subunit (DNA-PKcs) can also regulate mTORC2 activation. In response to UVR-induced DNA damage, DNA-PKcs exits the nucleus and binds to SIN1. This interaction promotes mTORC2-mediated phosphorylation of AKT at Ser473 [175]. This phosphorylation, in addition to the PDK1-dependent Thr308 phosphorylation, increases the substrate specificity of AKT for downstream targets. While phosphorylation of AKT at Thr308 is sufficient to induce mTORC1-specific activation [154], studies suggest that AKT must be phosphorylated at both Thr308 and Ser473 in order to control downstream cell survival pathways, including regulation and inhibition of pro-apoptotic proteins including BAD (Bcl-2-associated death promoter), BAX (Bcl-2-associated X), GSK-3β, ASK1, Caspase-9, and FOXO3a [150, 176].
The transcription factor FOXO3a has been identified as a critical component in the apoptotic pathway of several cancer types [177–185]. FOXO3a is a member of the FOX (Forkhead Box) superfamily of transcription factors that control diverse cellular functions [182]. The subclass FOX”O” proteins chiefly regulate oxidative stress, cell cycle progression, and apoptosis [183, 184, 186]. FOXO3a directly targets and increases transcription of both extrinsic (Trail and FasL) and intrinsic (BIM and PUMA) apoptotic genes [183], which are implicated in UVR-induced apoptosis [187–189]. While there are a variety of cellular elements that post-translationally modify FOXO3a, AKT and ERK are considered two of its primary negative regulators [186, 190, 191]. Upon phosphorylation of AKT at Thr308 and Ser473, AKT translocates into the nucleus and phosphorylates FOXO3a at three sites: Thr32, Ser256 and Ser319 [192] (Figure 4A). Previous studies show that AKT-mediated phosphorylation of FOXO3a alone does not reduce its activity. Instead, the 14-3-3ζ chaperone binds to this evolutionally conserved motif and reduces the affinity of FOXO3a for DNA by masking the DNA binding domain [193]. In addition, 14-3-3ζ binding masks two nuclear localization sequences on the FOXO3a [194], which along with two already exposed nuclear export signals, induces FOXO3a cytoplasmic localization and sequestration [195]. Our lab has recently demonstrated that knockdown of either rictor or mSIN1, two key structural components of mTORC2, sensitizes keratinocytes to UVB-induced apoptosis, and that this effect is dependent on AKT-mediated FOXO3a regulation [127]. Upon exposure to UVR, FOXO3a is shuttled out of the nucleus and sequestered into the cytoplasm. However, disruption of mTORC2/AKT signaling inhibits this process and an increased accumulation of FOXO3a is observed in the nucleus. The increased sensitivity to UVR-induced apoptosis following inhibition of mTORC2 signaling is rescued with simultaneous knockdown of FOXO3a, suggesting this process is dependent on the activity of FOXO3a [127].
Raf/MEK/ERK signaling
Activation of RAF/MEK/ERK signaling also occurs downstream of EGFR in response to UVR exposure [196, 197], and this pathway has been identified as a chemoprevention target in NMSC [2, 198]. Following EGFR activation (Figure 4B), the growth factor receptor-bound protein 2 (GRB2) is recruited to the receptor, resulting in binding to the guanine nucleotide exchange factor Son of Sevenless (SOS). This enables SOS to liberate the bound GDP on the RAS GTPase. Once GDP is released, RAS quickly binds a free GTP and induces RAF activation [199]. There are three isoforms of RAF that are involved in signaling to the MEK/ERK pathway: A-RAF, B-RAF, and C-RAF (RAF1). Mutations in B-RAF in particular are linked with development of melanoma and are reviewed in [200]. All three RAF isoforms can bind to and phosphorylate MEK1 and 2 (at Ser217 and Ser221). This phosphorylation activates MEK, which in turn phosphorylates (at Thr202 and Tyr204) and activates ERK (p44/42 MAPK) 1 and 2 [201]. Once activated, ERK regulates numerous downstream targets involved in cancer that control cell growth and survival including c-Jun, c-Myc, IKK, and FOXO3a [202]. Interestingly, studies show that certain patients who were successfully treated for BCCs through the use of smoothened (Smo) inhibitors, inhibitors that block sonic hedgehog (SHH) signaling, later develop SCCs at the same site. It was determined that following Smo inhibition, the regressed BCC cells switch from aberrant SHH activation to increased RAS/MEK/ERK signaling, which promotes the development of SCC [203].
Similar to AKT, ERK can phosphorylate FOXO3a (at Ser294, Ser344, and Ser425) in the nucleus, which triggers its exit into the cytoplasm (Figure 4B). However, contrary to mTORC2/AKT/14-3-3ζ regulation, FOXO3a is targeted for MDM2-mediated cytoplasmic degradation in response to the ERK-specific phosphorylation [204]. In our recent study, we noticed a UVR-induced increase in total FOXO3a abundance in HaCaT cells with intact mTORC2 signaling that was not present following inhibition of mTORC2 [127], suggesting a possible degradation of FOXO3a. Several studies suggest that 14-3-3ζ binding acts as a “protective barrier” for FOXO3a, which guards FOXO3a from PP2A-mediated dephosphorylation and subsequent degradation triggered by other signaling pathways, including the RAF/MEK/ERK pathway [195, 205]. Therefore, we simultaneously inhibited both of these pathways in HaCaT cells and showed an increase in nuclear FOXO3a protein both before and immediately after exposure to UVR. These results correlated with a further increased sensitivity to UVR-induced apoptosis compared to inhibition of either pathway alone, which was also dependent on FOXO3a [127]. It has been demonstrated that dual-targeting of the mTORC2/AKT and RAF/MEK/ERK pathways in advanced cancers produces better efficacy in patients than inhibition of either pathway alone [206]. In addition, studies in colon and pancreatic cancer models also show that dual inhibition of these pathways specifically increases the tumor suppressor activity of FOXO3a [185, 207, 208]. These results reflect the extensive cross-talk that occurs between the PI3K/mTOR and the RAF/MEK/ERK pathways (see [209] for review). Given these results, combination therapy with a TOR kinase inhibitor and MEK inhibitor for NMSC prevention warrants further investigation.
APOPTOSIS
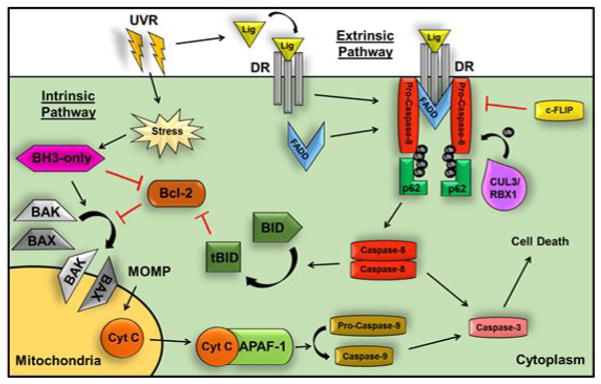
A common denominator relevant to each reviewed signaling pathway is the ability to inhibit and/or induce caspase-dependent apoptosis upon exposure to UVR. As discussed above, increased cell survival due to inhibition of apoptosis is a key contributor to UVR-induced initiation of NMSC; therefore, an understanding of the signaling cascades that result in apoptosis initiation will provide insight into NMSC development. Caspase-dependent apoptosis is described as either extrinsic, death receptor (DR)-dependent apoptosis or intrinsic apoptosis initiated at the mitochondria [210]. Initiation of extrinsic apoptosis (Figure 5) requires ligand binding and activation of plasma membrane DRs, which are members of the tumor necrosis factor super family of receptors (TNFR) [84]. Three examples of DRs that have been linked to in skin carcinogenesis are TNF-R1, the Fas/APO1/CD95 receptor (FasR), and the TNF-related apoptosis-inducing ligand receptors 1 and 2 (TRAIL-R1/DR4 and TRAIL-R2/DR5) [89, 203], each with a specific extracellular ligand reflected in the receptor name (i.e. TRAIL binds to TRAIL-R). Negative regulators of DRs, referred to as decoy death receptors (DcR), have parallel extracellular domains that allow them to act as ligand sinks; however, only the active DRs have the fully functional intracellular death domain (DD) needed to induce apoptosis [81]. TNFR1 signaling is reviewed in detail in [69]. Briefly, FasR and TRAIL-R1/2 trimerize upon ligand binding, which allows the recruitment and homotypic binding of fas-associated protein with death domain (FADD) to the death domain binding sites on the intracellular domain of the DR. This binding allows FADD to recruit the pro-apoptotic proteins procaspase-8 and -10 into a complex referred to as the death-inducing signaling complex (DISC) [211]. Following recruitment by FADD, pro-caspase 8 is ubiquitinated via a complex consisting of the cullin3 ubiquitin E3 ligase (CUL3) and RING-box protein 1 (RBX1). The resulting ubiquitination permits the binding of pro-caspase 8 to ubiquitin-binding protein p62/sequestosome-1 (p62), which promotes aggregation and homodimerization of pro-caspase 8 allowing auto-proteolytic cleavage of pro-caspase 8 into its active form [212]. This process is inhibited by the cellular FLICE-like inhibitory protein (c-FLIP), which binds to FADD and prevents the dimerization and subsequent activation of caspase-8.
Figure 5. UVR can activate both intrinsic and extrinsic apoptosis.
Extrinsic apoptosis is initiated by ligand binding to DRs such as FasR and TRAIL-R1/2, which trimerize and recruit FADD to intracellular death domain binding sites. FADD then recruits the pro-caspase-8 dimer to form the DISC. Ubiquitination of pro-caspase-8 by CUL3/RBX1 allows binding of p62 and cleavage of pro-caspase-8 into its active form. The caspase-8 dimer causes the downstream activation of pro-caspase-3 to induce cell death. This process is inhibited by c-FLIP binding to FADD, which prevents caspase-8 dimerization and activation. Intrinsic apoptosis is activated by UVR in response to both DNA damage and hypoxia. In the absence of UVR, the activities of BAX and BAK are inhibited by Bcl-2 family proteins, whereas UVR exposure causes the BH3-only proteins to bind to and inhibit Bcl-2, allowing BAX and BAK to generate mitochondrial outer membrane permeabilization (MOMP) and subsequent release of cytochrome C into the cytosol. In the cytosol, cytochrome C binds APAF-1 to recruit and activate pro-caspase-9, which initiates caspase-3-dependent cell death. Caspase-8 can also cleave BID to generate tBID, which promotes mitochondrial-mediated cell death, thus linking the intrinsic and extrinsic pathways.
Once cleaved, the caspase-8 dimer causes the downstream activation of pro-caspase-3, -6, and -7. Activation of these caspases, primarily caspase-3, induces cell death through the cleavage of DNA, as well as various proteins involved in cell maintenance and survival. In this context, cleavage of poly (ADP-ribose) polymerase (PARP) is often considered an endpoint marker of caspase-dependent apoptosis [213]. Therapeutics that target DR activation may be an effective treatment for NMSC, as in vivo studies have shown that activation of these receptors prevent skin tumor development in a mouse model [214]. In addition, targeting of either TRAIL-R or FasR has been shown to be an effective therapy against several types of cancers [215], although data on NMSC are not currently available.
Classically, intrinsic apoptosis (Figure 5) is activated in response to cellular stressors such as DNA damage or hypoxia, resulting in mitochondrial outer membrane (MOM) permeabilization (MOMP) and subsequent release of cytochrome C into the cytosol [176, 216]. Specifically, MOMP is generated following the formation of pores in the MOM by the proteins BAX and BAK (Bcl-2 homologous antagonist) though the specific mechanism is still the subject of investigation [217]. In the absence of UVR-induced cellular stress, the activities of BAX and BAK are inhibited by the anti-apoptotic Bcl-2 (B-cell lymphoma 2) proteins, including Bcl-2, Bcl-xL (Bcl-extra-large), and Bcl-w (Bcl-2-like protein 2) [218]. Following UVR-irradiation, the BH3-only family of proteins, which include BID (BH3 interacting-domain death agonist), BIM, BAD, PUMA (p53 up regulator of apoptosis), and NOXA, bind to and inhibit the anti-apoptotic Bcl-2 proteins [219]. BID and BIM can also directly activate BAX and BAK, resulting in pore formation on the MOM [220]. UVR-induced activation of the BH3-family of proteins results from increased activity of pro-apoptotic transcription factors such as FOXO3a, HIF-1α, and p53 [218, 221]. In contrast, UVR-inducible signal transduction pathways can also reduce the activity of the BH3-only proteins through direct protein inhibition (i.e. AKT phosphorylation of BAD), as well as indirect inhibition of upstream pro-apoptotic transcription factors (i.e. inhibition of p53) [24, 27].
Following its release into the cytosol, cytochrome C and the apoptotic protease activating factor 1 (APAF-1) form a complex referred to as the ‘apoptosome’. This complex recruits and activates caspase 9, which in turn activates caspase-3 and -7 to induce cell death [222]. Cross-talk between the extrinsic and intrinsic pathway exists in keratinocytes primarily through caspase-8 [223, 224]. In addition to activating caspase-3, -6, and -7, caspase-8 can cleave BID to generate a truncated form (tBID), which is able to both inhibit the Bcl-2 proteins and promote BAX/BAM activation and subsequent mitochondrial mediated cell death [216] (Figure 5). Thus, because UVR-irradiation can initiate intrinsic apoptosis through DR activation as well as through direct mechanisms such as DNA damage, oxidative stress and TLR/RTK activation, this apoptotic pathway is viewed as a more viable therapeutic target in the prevention and treatment of NMSC. Therapies designed to either inhibit the anti-apoptotic Bcl-2 proteins or mimic the pro-apoptotic BH3-only family are currently being tested as a means of treating both melanoma and NMSC [219, 225].
CONCLUSIONS
Recognizing the complexity of UVR-induced signal transduction is critical to our understanding of NMSC tumorigenesis. Depending on the intensity and duration of UVR irradiation, as well as the level of cellular damage (i.e. DNA/oxidative damage) that results from exposure to UVR, each activated signaling pathway can elicit varying responses that can be either tumor suppressive, oncogenic, or a mixture of both. As with most physiological mechanisms, there is a great deal of redundancy that exists within the cell, which allows extensive regulation and cross-talk between pathways. As a result, UVR exposure does not activate unique pathways in isolation, but rather elicits an intricate stress response that may become pathologic. Furthermore, genetic variation between individuals, in addition to genetic heterogeneity in tumors that develop, can play an important role in evaluating whether a targeted treatment will be beneficial, ineffective, or possibly even harmful. Thus, continued intensive study of the signaling pathways that respond to UVR will help lead to the development of more effective novel therapeutics in both the prevention and treatment of NMSC.
Summary Statement.
The intracellular signaling response that leads to non-melanoma skin cancer (NMSC) is remarkably complex. This review summarizes key pathways activated by exposure to UV irradiation, the most important risk factor for NMSC, and describes their deregulation in NMSC development.
Acknowledgments
We would like to thank Dr. Amanda Nelson for critical reading of the manuscript.
FUNDING
Work described in this manuscript from the authors’ laboratory was supported by grants from the National Institute of Environmental Health Sciences, NIH (ES019242 to LMS and ES026471 to RPF).
Abbreviations used
- NMSC
non-melanoma skin cancer
- BCC
basal cell carcinoma
- SCC
squamous cell carcinoma
- UVR
Ultraviolet radiation
- ROS
reactive oxygen species
- XP
Xeroderma pigmentosum
- SSB
single strand breaks
- DSB
double strand breaks
- PIKK
phosphatidylinositol 3-kinase-related kinases
- ATM
ataxia telangiectasia mutated protein
- ATR
ataxia telangiectasia and Rad3-related protein
- CHK
checkpoint kinase
- MDM2
mouse double minute 2 homolog
- NIMA
Never In Mitosis A
- NEK11
NIMA-Related Kinase 11
- PLK-1
polo-like kinase 1
- SIAH1
seven in absentia homologue 1
- HIPK2
homeodomain-interacting protein kinase 2
- SKP2
s-phase kinase-associated protein 2
- CDK1
cyclin-dependent kinase 1
- AK
actinic keratosis
- NFκB
nuclear factor kappa-light-chain-enhancer of activated B cells
- STAT3
signal transducer and activator of transcription 3
- RTK
Receptor Tyrosine Kinase
- TNFR1
Tumor Necrosis Factor receptors
- TLR
Toll-like receptors
- IKK
I kappa B kinase
- NEMO
NFκB essential modulator
- MyD88
Myeloid Differentiation Primary Response 88
- IRAK
IL-1 receptor-associated kinase
- TRAF6
TNF receptor associated factor 6
- EGFR
epidermal growth factor receptor
- Jak
Janus-associated-kinase
- SH2
Src Homology 2
- PKCε
protein kinase c epsilon
- JNK
c-Jun N-terminal kinases
- MAPK
mitogen-activated protein kinase
- MKK
mitogen-activated protein kinase kinase
- ASK1
apoptosis signal-regulating kinase 1
- MAP3K
MAP kinase kinase kinase
- Trx1
thiol-disulphide oxidoreductase thioredoxin-1
- MKP
mitogen-activated protein kinase phosphatase
- HIF-1α
hypoxia-inducible factor 1-alpha
- GSK3β
glycogen synthase kinase 3 beta
- AP-1
activator protein-1
- FOXO3a
Forkhead box O3a
- Bcl-2
B-cell lymphoma 2
- BIM
Bcl-2-like protein 11
- IR
insulin receptor
- IGF-1-R
insulin like growth factor 1 receptor
- PI3K
phosphoinositide 3-kinase
- mTOR
mechanistic (mammalian) target of rapamycin
- RAF
rapidly accelerated fibrosarcoma kinase
- MEK
mitogen-activated protein kinase kinase
- ERK
extracellular signal-regulated kinases
- PTEN
phosphatase and tensin homolog
- AKT/PKB
Protein Kinase B
- PIP2
phospholipid phosphatidylinositol 4,5-bisphosphate
- PIP3
phosphatidylinositol (3,4,5)-trisphosphate
- PDK1
phosphoinositide-dependent kinase-1
- TSC
Tuberous Sclerosis Complex
- RHEB
ras homolog enriched in brain
- S6K1
S6 kinase beta-1
- eIF4E
eukaryotic translation initiation factor 4E
- 4E-BP1
4E-binding protein 1
- FKBP12
FK-binding protein 12
- PH
pleckstrin homology
- DNA-PKcs
DNA-dependent protein kinase catalytic subunit
- BAD
Bcl-2-associated death promoter
- BAX
Bcl-2-associated X
- GRB2
growth factor receptor-bound protein 2
- SOS
Son of Sevenless
- Smo
smoothened
- SHH
sonic hedgehog
- DR
death receptor
- TNFR
tumor necrosis factor receptor
- FasR
Fas/APO1/CD95 receptor
- TRAIL
TNF-related apoptosis-inducing ligand receptor
- DcR
decoy death receptors
- DD
death domain
- FADD
fas-associated protein with death domain
- DISC
death-inducing signaling complex
- CUL3
cullin3 ubiquitin E3 ligase
- RBX1
RING-box protein 1
- c-FLIP
cellular FLICE-like inhibitory protein
- PARP
poly (ADP-ribose) polymerase
- MOMP
mitochondrial outer membrane permeabilization
- BAK
Bcl-2 homologous antagonist
- Bcl-xL
Bcl-extra-large
- Bcl-w
Bcl-2-like protein 2
- BID
BH3 interacting-domain death agonist
- PUMA
p53 up regulator of apoptosis
- APAF-1
apoptotic protease activating factor 1
- tBID
truncated BID
Footnotes
DECLARATIONS OF INTEREST
The authors declare no financial interests.
AUTHOR CONTRIBUTIONS
RPF wrote the first draft of the manuscript, which was edited by LMS. Both authors approved the final version of the manuscript.
References
- 1.American Cancer Society. Cancer Facts and Figures. 2015. [Google Scholar]
- 2.Bowden GT. Prevention of non-melanoma skin cancer by targeting ultraviolet-Blight signalling. Nat Rev Cancer. 2004;4:23–35. doi: 10.1038/nrc1253. [DOI] [PubMed] [Google Scholar]
- 3.Lomas A, Leonardi-Bee J, Bath-Hextall F. A systematic review of worldwide incidence of nonmelanoma skin cancer. Br J Dermatol. 2012;166:1069–1080. doi: 10.1111/j.1365-2133.2012.10830.x. [DOI] [PubMed] [Google Scholar]
- 4.Xiang F, Lucas R, Hales S, Neale R. Incidence of nonmelanoma skin cancer in relation to ambient UV radiation in white populations, 1978–2012: empirical relationships. JAMA Dermatol. 2014;150:1063–1071. doi: 10.1001/jamadermatol.2014.762. [DOI] [PubMed] [Google Scholar]
- 5.Croft M, Benedict CA, Ware CF. Clinical targeting of the TNF and TNFR superfamilies. Nat Rev Drug Discov. 2013;12:147–168. doi: 10.1038/nrd3930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Madan V, Lear JT, Szeimies RM. Non-melanoma skin cancer. Lancet. 2010;375:673–685. doi: 10.1016/S0140-6736(09)61196-X. [DOI] [PubMed] [Google Scholar]
- 7.Kim RH, Armstrong AW. Nonmelanoma skin cancer. Dermatologic clinics. 2012;30:125–139. ix. doi: 10.1016/j.det.2011.08.008. [DOI] [PubMed] [Google Scholar]
- 8.Christenson LJ, Borrowman TA, Vachon CM, Tollefson MM, Otley CC, Weaver AL, Roenigk RK. Incidence of basal cell and squamous cell carcinomas in a population younger than 40 years. JAMA. 2005;294:681–690. doi: 10.1001/jama.294.6.681. [DOI] [PubMed] [Google Scholar]
- 9.Ley RD. Photoreactivation in humans. Proc Natl Acad Sci USA. 1993;90:4337. doi: 10.1073/pnas.90.10.4337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Matsumura Y, Ananthaswamy HN. Toxic effects of ultraviolet radiation on the skin. Toxicol Appl Pharmacol. 2004;195:298–308. doi: 10.1016/j.taap.2003.08.019. [DOI] [PubMed] [Google Scholar]
- 11.Bruls WA, Slaper H, van der Leun JC, Berrens L. Transmission of human epidermis and stratum corneum as a function of thickness in the ultraviolet and visible wavelengths. Photochem Photobiol. 1984;40:485–494. doi: 10.1111/j.1751-1097.1984.tb04622.x. [DOI] [PubMed] [Google Scholar]
- 12.Armstrong BK, Kricker A. The epidemiology of UV induced skin cancer. J Photochem Photobiol B. 2001;63:8–18. doi: 10.1016/s1011-1344(01)00198-1. [DOI] [PubMed] [Google Scholar]
- 13.Marcil I, Stern RS. Risk of developing a subsequent nonmelanoma skin cancer in patients with a history of nonmelanoma skin cancer: a critical review of the literature and meta-analysis. Arch Dermatol. 2000;136:1524–1530. doi: 10.1001/archderm.136.12.1524. [DOI] [PubMed] [Google Scholar]
- 14.Athar M, Walsh SB, Kopelovich L, Elmets CA. Pathogenesis of nonmelanoma skin cancers in organ transplant recipients. Arch Biochem Biophys. 2011;508:159–163. doi: 10.1016/j.abb.2011.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berg D, Otley CC. Skin cancer in organ transplant recipients: Epidemiology, pathogenesis, and management. J Amer Acad Dermatol. 2002;47:1–17. doi: 10.1067/mjd.2002.125579. [DOI] [PubMed] [Google Scholar]
- 16.Patrick MH. Studies on thymine-derived UV photoproducts in DNA--I. Formation and biological role of pyrimidine adducts in DNA. Photochem Photobiol. 1977;25:357–372. doi: 10.1111/j.1751-1097.1977.tb07355.x. [DOI] [PubMed] [Google Scholar]
- 17.Sinha RP, Hader DP. UV-induced DNA damage and repair: a review. Photochem Photobiol Sci. 2002;1:225–236. doi: 10.1039/b201230h. [DOI] [PubMed] [Google Scholar]
- 18.Friedberg EC, Aguilera A, Gellert M, Hanawalt PC, Hays JB, Lehmann AR, Lindahl T, Lowndes N, Sarasin A, Wood RD. DNA repair: from molecular mechanism to human disease. DNA Repair. 2006;5:986–996. doi: 10.1016/j.dnarep.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 19.Friedberg EC, Henning KA. The conundrum of xeroderma pigmentosum--a rare disease with frequent complexities. Mut Res. 1993;289:47–53. doi: 10.1016/0027-5107(93)90129-4. [DOI] [PubMed] [Google Scholar]
- 20.Nishigori C, Moriwaki S, Takebe H, Tanaka T, Imamura S. Gene alterations and clinical characteristics of xeroderma pigmentosum group A patients in Japan. Arch Dermatol. 1994;130:191–197. [PubMed] [Google Scholar]
- 21.Tian H, Gao Z, Li H, Zhang B, Wang G, Zhang Q, Pei D, Zheng J. DNA damage response--a double-edged sword in cancer prevention and cancer therapy. Cancer Lett. 2015;358:8–16. doi: 10.1016/j.canlet.2014.12.038. [DOI] [PubMed] [Google Scholar]
- 22.Ananthaswamy HN, Pierceall WE. Molecular mechanisms of ultraviolet radiation carcinogenesis. Photochem Photobiol. 1990;52:1119–1136. doi: 10.1111/j.1751-1097.1990.tb08452.x. [DOI] [PubMed] [Google Scholar]
- 23.Nishisgori C. Current concept of photocarcinogenesis. Photochem Photobiol Sci. 2015;14:1713–1721. doi: 10.1039/c5pp00185d. [DOI] [PubMed] [Google Scholar]
- 24.Strozyk E, Kulms D. The role of AKT/mTOR pathway in stress response to UV-irradiation: implication in skin carcinogenesis by regulation of apoptosis, autophagy and senescence. Int J Mol Sci. 2013;14:15260–15285. doi: 10.3390/ijms140815260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ziegler A, Jonason AS, Leffell DJ, Simon JA, Sharma HW, Kimmelman J, Remington L, Jacks T, Brash DE. Sunburn and p53 in the onset of skin cancer. Nature. 1994;372:773–776. doi: 10.1038/372773a0. [DOI] [PubMed] [Google Scholar]
- 26.Leffell DJ. The scientific basis of skin cancer. J Amer Acad Dermatol. 2000;42:18–22. doi: 10.1067/mjd.2000.103340. [DOI] [PubMed] [Google Scholar]
- 27.Van Laethem A, Garmyn M, Agostinis P. Starting and propagating apoptotic signals in UVB irradiated keratinocytes. Photochem Photobiol Sci. 2009;8:299–308. doi: 10.1039/b813346h. [DOI] [PubMed] [Google Scholar]
- 28.Abraham RT. Cell cycle checkpoint signaling through the ATM and ATR kinases. Genes Dev. 2001;15:2177–2196. doi: 10.1101/gad.914401. [DOI] [PubMed] [Google Scholar]
- 29.Abraham RT. PI 3-kinase related kinases: ‘big’ players in stress-induced signaling pathways. DNA Repair. 2004;3:883–887. doi: 10.1016/j.dnarep.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 30.Stokes MP, Rush J, Macneill J, Ren JM, Sprott K, Nardone J, Yang V, Beausoleil SA, Gygi SP, Livingstone M, Zhang H, Polakiewicz RD, Comb MJ. Profiling of UV-induced ATM/ATR signaling pathways. Proc Natl Acad Sci USA. 2007;104:19855–19860. doi: 10.1073/pnas.0707579104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jarrett SG, Wolf Horrell EM, Christian PA, Vanover JC, Boulanger MC, Zou Y, D’Orazio JA. PKA-mediated phosphorylation of ATR promotes recruitment of XPA to UV-induced DNA damage. Mol Cell. 2014;54:999–1011. doi: 10.1016/j.molcel.2014.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 32.Ray A, Milum K, Battu A, Wani G, Wani AA. NER initiation factors, DDB2 and XPC, regulate UV radiation response by recruiting ATR and ATM kinases to DNA damage sites. DNA Repair. 2013;12:273–283. doi: 10.1016/j.dnarep.2013.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kozlov SV, Graham ME, Peng C, Chen P, Robinson PJ, Lavin MF. Involvement of novel autophosphorylation sites in ATM activation. EMBO J. 2006;25:3504–3514. doi: 10.1038/sj.emboj.7601231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kozlov SV, Graham ME, Jakob B, Tobias F, Kijas AW, Tanuji M, Chen P, Robinson PJ, Taucher-Scholz G, Suzuki K, So S, Chen D, Lavin MF. Autophosphorylation and ATM activation: additional sites add to the complexity. J Biol Chem. 2011;286:9107–9119. doi: 10.1074/jbc.M110.204065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bakkenist CJ, Kastan MB. DNA damage activates ATM through intermolecular autophosphorylation and dimer dissociation. Nature. 2003;421:499–506. doi: 10.1038/nature01368. [DOI] [PubMed] [Google Scholar]
- 36.Jazayeri A, Falck J, Lukas C, Bartek J, Smith GC, Lukas J, Jackson SP. ATM- and cell cycle-dependent regulation of ATR in response to DNA double-strand breaks. Nat Cell Biol. 2006;8:37–45. doi: 10.1038/ncb1337. [DOI] [PubMed] [Google Scholar]
- 37.Falck J, Mailand N, Syljuasen RG, Bartek J, Lukas J. The ATM-Chk2-Cdc25A checkpoint pathway guards against radioresistant DNA synthesis. Nature. 2001;410:842–847. doi: 10.1038/35071124. [DOI] [PubMed] [Google Scholar]
- 38.Saito S, Goodarzi AA, Higashimoto Y, Noda Y, Lees-Miller SP, Appella E, Anderson CW. ATM mediates phosphorylation at multiple p53 sites, including Ser(46), in response to ionizing radiation. J Biol Chem. 2002;277:12491–12494. doi: 10.1074/jbc.C200093200. [DOI] [PubMed] [Google Scholar]
- 39.Banin S, Moyal L, Shieh S, Taya Y, Anderson CW, Chessa L, Smorodinsky NI, Prives C, Reiss Y, Shiloh Y, Ziv Y. Enhanced phosphorylation of p53 by ATM in response to DNA damage. Science. 1998;281:1674–1677. doi: 10.1126/science.281.5383.1674. [DOI] [PubMed] [Google Scholar]
- 40.Decraene D, Agostinis P, Pupe A, de Haes P, Garmyn M. Acute response of human skin to solar radiation: regulation and function of the p53 protein. J Photochem Photobiol B. 2001;63:78–83. doi: 10.1016/s1011-1344(01)00204-4. [DOI] [PubMed] [Google Scholar]
- 41.Gannon HS, Woda BA, Jones SN. ATM phosphorylation of Mdm2 Ser394 regulates the amplitude and duration of the DNA damage response in mice. Cancer Cell. 2012;21:668–679. doi: 10.1016/j.ccr.2012.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shiloh Y. ATM and related protein kinases: safeguarding genome integrity. Nature reviews Cancer. 2003;3:155–168. doi: 10.1038/nrc1011. [DOI] [PubMed] [Google Scholar]
- 43.Stevens C, Smith L, La Thangue NB. Chk2 activates E2F-1 in response to DNA damage. Nat Cell Biol. 2003;5:401–409. doi: 10.1038/ncb974. [DOI] [PubMed] [Google Scholar]
- 44.Lin WC, Lin FT, Nevins JR. Selective induction of E2F1 in response to DNA damage, mediated by ATM-dependent phosphorylation. Genes Dev. 2001;15:1833–1844. [PMC free article] [PubMed] [Google Scholar]
- 45.Shiotani B, Nguyen HD, Hakansson P, Marechal A, Tse A, Tahara H, Zou L. Two distinct modes of ATR activation orchestrated by Rad17 and Nbs1. Cell Reports. 2013;3:1651–1662. doi: 10.1016/j.celrep.2013.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stiff T, Walker SA, Cerosaletti K, Goodarzi AA, Petermann E, Concannon P, O’Driscoll M, Jeggo PA. ATR-dependent phosphorylation and activation of ATM in response to UV treatment or replication fork stalling. EMBO J. 2006;25:5775–5782. doi: 10.1038/sj.emboj.7601446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liu Q, Guntuku S, Cui XS, Matsuoka S, Cortez D, Tamai K, Luo G, Carattini-Rivera S, DeMayo F, Bradley A, Donehower LA, Elledge SJ. Chk1 is an essential kinase that is regulated by Atr and required for the G(2)/M DNA damage checkpoint. Genes Dev. 2000;14:1448–1459. [PMC free article] [PubMed] [Google Scholar]
- 48.Zhang Y, Hunter T. Roles of Chk1 in cell biology and cancer therapy. International journal of cancer. Int J Cancer. 2014;134:1013–1023. doi: 10.1002/ijc.28226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Melixetian M, Klein DK, Sorensen CS, Helin K. NEK11 regulates CDC25A degradation and the IR-induced G2/M checkpoint. Nat Cell Biol. 2009;11:1247–1253. doi: 10.1038/ncb1969. [DOI] [PubMed] [Google Scholar]
- 50.Sorensen CS, Melixetian M, Klein DK, Helin K. NEK11: linking CHK1 and CDC25A in DNA damage checkpoint signaling. Cell Cycle. 2010;9:450–455. doi: 10.4161/cc.9.3.10513. [DOI] [PubMed] [Google Scholar]
- 51.Tang J, Erikson RL, Liu X. Checkpoint kinase 1 (Chk1) is required for mitotic progression through negative regulation of polo-like kinase 1 (Plk1) Proc Natl Acad Sci USA. 2006;103:11964–11969. doi: 10.1073/pnas.0604987103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shinozaki T, Nota A, Taya Y, Okamoto K. Functional role of Mdm2 phosphorylation by ATR in attenuation of p53 nuclear export. Oncogene. 2003;22:8870–8880. doi: 10.1038/sj.onc.1207176. [DOI] [PubMed] [Google Scholar]
- 53.Winter M, Sombroek D, Dauth I, Moehlenbrink J, Scheuermann K, Crone J, Hofmann TG. Control of HIPK2 stability by ubiquitin ligase Siah-1 and checkpoint kinases ATM and ATR. Nat Cell Biol. 2008;10:812–824. doi: 10.1038/ncb1743. [DOI] [PubMed] [Google Scholar]
- 54.Hofmann TG, Moller A, Sirma H, Zentgraf H, Taya Y, Droge W, Will H, Schmitz ML. Regulation of p53 activity by its interaction with homeodomain-interacting protein kinase-2. Nat Cell Biol. 2002;4:1–10. doi: 10.1038/ncb715. [DOI] [PubMed] [Google Scholar]
- 55.Xiong Y, Hannon GJ, Zhang H, Casso D, Kobayashi R, Beach D. p21 is a universal inhibitor of cyclin kinases. Nature. 1993;366:701–704. doi: 10.1038/366701a0. [DOI] [PubMed] [Google Scholar]
- 56.Lee H, Zeng SX, Lu H. UV Induces p21 rapid turnover independently of ubiquitin and Skp2. J Biol Chem. 2006;281:26876–26883. doi: 10.1074/jbc.M605366200. [DOI] [PubMed] [Google Scholar]
- 57.Al-Khalaf HH, Hendrayani SF, Aboussekhra A. ATR controls the p21(WAF1/Cip1) protein up-regulation and apoptosis in response to low UV fluences. Mol Carcinog. 2012;51:930–938. doi: 10.1002/mc.20864. [DOI] [PubMed] [Google Scholar]
- 58.Al-Khalaf HH, Aboussekhra A. ATR controls the UV-related upregulation of the CDKN1A mRNA in a Cdk1/HuR-dependent manner. Mol Carcinog. 2014;53:979–987. doi: 10.1002/mc.22066. [DOI] [PubMed] [Google Scholar]
- 59.Brown EJ, Baltimore D. ATR disruption leads to chromosomal fragmentation and early embryonic lethality. Genes Dev. 2000;14:397–402. [PMC free article] [PubMed] [Google Scholar]
- 60.Murga M, Bunting S, Montana MF, Soria R, Mulero F, Canamero M, Lee Y, McKinnon PJ, Nussenzweig A, Fernandez-Capetillo O. A mouse model of ATR-Seckel shows embryonic replicative stress and accelerated aging. Nat Genet. 2009;41:891–898. doi: 10.1038/ng.420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kawasumi M, Lemos B, Bradner JE, Thibodeau R, Kim YS, Schmidt M, Higgins E, Koo SW, Angle-Zahn A, Chen A, Levine D, Nguyen L, Heffernan TP, Longo I, Mandinova A, Lu YP, Conney AH, Nghiem P. Protection from UV-induced skin carcinogenesis by genetic inhibition of the ataxia telangiectasia and Rad3-related (ATR) kinase. Proc Natl Acad Sci USA. 2011;108:13716–13721. doi: 10.1073/pnas.1111378108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454:436–444. doi: 10.1038/nature07205. [DOI] [PubMed] [Google Scholar]
- 63.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 64.Ernst P. Review article: the role of inflammation in the pathogenesis of gastric cancer. Aliment Pharmacol Ther. 1999;13(Suppl 1):13–18. doi: 10.1046/j.1365-2036.1999.00003.x. [DOI] [PubMed] [Google Scholar]
- 65.Kundu JK, Surh YJ. Inflammation: gearing the journey to cancer. Mut Res. 2008;659:15–30. doi: 10.1016/j.mrrev.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 66.Maru GB, Gandhi K, Ramchandani A, Kumar G. The role of inflammation in skin cancer. Adv Exp Med Biol. 2014;816:437–469. doi: 10.1007/978-3-0348-0837-8_17. [DOI] [PubMed] [Google Scholar]
- 67.Driscoll MS, Wagner RF., Jr Clinical management of the acute sunburn reaction. Cutis. 2000;66:53–58. [PubMed] [Google Scholar]
- 68.Sur I, Ulvmar M, Toftgard R. The two-faced NF-kappaB in the skin. Int Rev Immunol. 2008;27:205–223. doi: 10.1080/08830180802130319. [DOI] [PubMed] [Google Scholar]
- 69.Andera L. Signaling activated by the death receptors of the TNFR family. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2009;153:173–180. doi: 10.5507/bp.2009.029. [DOI] [PubMed] [Google Scholar]
- 70.Kim Y, He YY. Ultraviolet radiation-induced non-melanoma skin cancer: Regulation of DNA damage repair and inflammation. Genes Dis. 2014;1:188–198. doi: 10.1016/j.gendis.2014.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kobayashi K, Hernandez LD, Galan JE, Janeway CA, Jr, Medzhitov R, Flavell RA. IRAK-M is a negative regulator of Toll-like receptor signaling. Cell. 2002;110:191–202. doi: 10.1016/s0092-8674(02)00827-9. [DOI] [PubMed] [Google Scholar]
- 72.Adhikari A, Xu M, Chen ZJ. Ubiquitin-mediated activation of TAK1 and IKK. Oncogene. 2007;26:3214–3226. doi: 10.1038/sj.onc.1210413. [DOI] [PubMed] [Google Scholar]
- 73.Mercurio F, Zhu H, Murray BW, Shevchenko A, Bennett BL, Li J, Young DB, Barbosa M, Mann M, Manning A, Rao A. IKK-1 and IKK-2: cytokine-activated IkappaB kinases essential for NF-kappaB activation. Science. 1997;278:860–866. doi: 10.1126/science.278.5339.860. [DOI] [PubMed] [Google Scholar]
- 74.Clark K, Nanda S, Cohen P. Molecular control of the NEMO family of ubiquitin-binding proteins. Nature reviews Mol Cell Biol. 2013;14:673–685. doi: 10.1038/nrm3644. [DOI] [PubMed] [Google Scholar]
- 75.Delhase M, Hayakawa M, Chen Y, Karin M. Positive and negative regulation of IkappaB kinase activity through IKKbeta subunit phosphorylation. Science. 1999;284:309–313. doi: 10.1126/science.284.5412.309. [DOI] [PubMed] [Google Scholar]
- 76.Zandi E, Rothwarf DM, Delhase M, Hayakawa M, Karin M. The IkappaB kinase complex (IKK) contains two kinase subunits, IKKalpha and IKKbeta, necessary for IkappaB phosphorylation and NF-kappaB activation. Cell. 1997;91:243–252. doi: 10.1016/s0092-8674(00)80406-7. [DOI] [PubMed] [Google Scholar]
- 77.Kim C, Pasparakis M. Epidermal p65/NF-kappaB signalling is essential for skin carcinogenesis. EMBO Mol Med. 2014;6:970–983. doi: 10.15252/emmm.201303541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hoesel B, Schmid JA. The complexity of NF-kappaB signaling in inflammation and cancer. Mol Cancer. 2013;12:86. doi: 10.1186/1476-4598-12-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Yang F, Tang E, Guan K, Wang CY. IKK beta plays an essential role in the phosphorylation of RelA/p65 on serine 536 induced by lipopolysaccharide. J Immunol. 2003;170:5630–5635. doi: 10.4049/jimmunol.170.11.5630. [DOI] [PubMed] [Google Scholar]
- 80.Afaq F, Malik A, Syed D, Maes D, Matsui MS, Mukhtar H. Pomegranate fruit extract modulates UV-B-mediated phosphorylation of mitogen-activated protein kinases and activation of nuclear factor kappa B in normal human epidermal keratinocytes paragraph sign. Photochem Photobiol. 2005;81:38–45. doi: 10.1562/2004-08-06-RA-264. [DOI] [PubMed] [Google Scholar]
- 81.Sheikh MS, Fornace AJ., Jr Death and decoy receptors and p53-mediated apoptosis. Leukemia. 2000;14:1509–1513. doi: 10.1038/sj.leu.2401865. [DOI] [PubMed] [Google Scholar]
- 82.Bell S, Degitz K, Quirling M, Jilg N, Page S, Brand K. Involvement of NF-kappaB signalling in skin physiology and disease. Cell Signal. 2003;15:1–7. doi: 10.1016/s0898-6568(02)00080-3. [DOI] [PubMed] [Google Scholar]
- 83.Yu H, Pardoll D, Jove R. STATs in cancer inflammation and immunity: a leading role for STAT3. Nat Rev Cancer. 2009;9:798–809. doi: 10.1038/nrc2734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wilson NS, Dixit V, Ashkenazi A. Death receptor signal transducers: nodes of coordination in immune signaling networks. Nat Immunol. 2009;10:348–355. doi: 10.1038/ni.1714. [DOI] [PubMed] [Google Scholar]
- 85.Chuang YC, Lin TK, Huang HY, Chang WN, Liou CW, Chen SD, Chang AY, Chan SH. Peroxisome proliferator-activated receptors gamma/mitochondrial uncoupling protein 2 signaling protects against seizure-induced neuronal cell death in the hippocampus following experimental status epilepticus. J Neuroinflammation. 2012;9:184. doi: 10.1186/1742-2094-9-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sano S, Chan KS, Kira M, Kataoka K, Takagi S, Tarutani M, Itami S, Kiguchi K, Yokoi M, Sugasawa K, Mori T, Hanaoka F, Takeda J, DiGiovanni J. Signal transducer and activator of transcription 3 is a key regulator of keratinocyte survival and proliferation following UV irradiation. Cancer Res. 2005;65:5720–5729. doi: 10.1158/0008-5472.CAN-04-4359. [DOI] [PubMed] [Google Scholar]
- 87.Zhang T, Kee WH, Seow KT, Fung W, Cao X. The coiled-coil domain of Stat3 is essential for its SH2 domain-mediated receptor binding and subsequent activation induced by epidermal growth factor and interleukin-6. Mol Cell Biol. 2000;20:7132–7139. doi: 10.1128/mcb.20.19.7132-7139.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Bromberg JF, Wrzeszczynska MH, Devgan G, Zhao Y, Pestell RG, Albanese C, Darnell JE., Jr Stat3 as an oncogene. Cell. 1999;98:295–303. doi: 10.1016/s0092-8674(00)81959-5. [DOI] [PubMed] [Google Scholar]
- 89.Leverkus M, Diessenbacher P, Geserick P. FLIP ing the coin? Death receptor-mediated signals during skin tumorigenesis. Exp Dermatol. 2008;17:614–622. doi: 10.1111/j.1600-0625.2008.00728.x. [DOI] [PubMed] [Google Scholar]
- 90.Carpenter RL, Lo HW. STAT3 Target Genes Relevant to Human Cancers. Cancers. 2014;6:897–925. doi: 10.3390/cancers6020897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Shen Y, Schlessinger K, Zhu X, Meffre E, Quimby F, Levy DE, Darnell JE., Jr Essential role of STAT3 in postnatal survival and growth revealed by mice lacking STAT3 serine 727 phosphorylation. Mol Cell Biol. 2004;24:407–419. doi: 10.1128/MCB.24.1.407-419.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Aziz MH, Manoharan HT, Verma AK. Protein kinase C epsilon, which sensitizes skin to sun’s UV radiation-induced cutaneous damage and development of squamous cell carcinomas, associates with Stat3. Cancer Res. 2007;67:1385–1394. doi: 10.1158/0008-5472.CAN-06-3350. [DOI] [PubMed] [Google Scholar]
- 93.Wen Z, Zhong Z, Darnell JE., Jr Maximal activation of transcription by Stat1 and Stat3 requires both tyrosine and serine phosphorylation. Cell. 1995;82:241–250. doi: 10.1016/0092-8674(95)90311-9. [DOI] [PubMed] [Google Scholar]
- 94.Srivastava J, DiGiovanni J. Non-canonical Stat3 signaling in cancer. Mol Carcinog. 2015 doi: 10.1002/mc.22438. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 95.Macias E, Rao D, Digiovanni J. Role of stat3 in skin carcinogenesis: insights gained from relevant mouse models. J Skin Cancer. 2013;2013:684050. doi: 10.1155/2013/684050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Sabharwal SS, Schumacker PT. Mitochondrial ROS in cancer: initiators, amplifiers or an Achilles’ heel? Nature reviews. Cancer. 2014;14:709–721. doi: 10.1038/nrc3803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Fuchs-Tarlovsky V. Role of antioxidants in cancer therapy. Nutrition. 2013;29:15–21. doi: 10.1016/j.nut.2012.02.014. [DOI] [PubMed] [Google Scholar]
- 98.Sayin VI, Ibrahim MX, Larsson E, Nilsson JA, Lindahl P, Bergo MO. Antioxidants accelerate lung cancer progression in mice. Sci Trans Med. 2014;6:221ra215. doi: 10.1126/scitranslmed.3007653. [DOI] [PubMed] [Google Scholar]
- 99.Rezvani HR, Mazurier F, Cario-Andre M, Pain C, Ged C, Taieb A, de Verneuil H. Protective effects of catalase overexpression on UVB-induced apoptosis in normal human keratinocytes. J Biol Chem. 2006;281:17999–18007. doi: 10.1074/jbc.M600536200. [DOI] [PubMed] [Google Scholar]
- 100.Narendhirakannan RT, Hannah MA. Oxidative stress and skin cancer: an overview. Indian J Clin Biochem. 2013;28:110–115. doi: 10.1007/s12291-012-0278-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Loft S, Poulsen HE. Cancer risk and oxidative DNA damage in man. J Mol Med. 1996;74:297–312. doi: 10.1007/BF00207507. [DOI] [PubMed] [Google Scholar]
- 102.de Gruijl FR, van Kranen HJ, Mullenders LH. UV-induced DNA damage, repair, mutations and oncogenic pathways in skin cancer. J Photochem Photobiol B. 2001;63:19–27. doi: 10.1016/s1011-1344(01)00199-3. [DOI] [PubMed] [Google Scholar]
- 103.Sander CS, Hamm F, Elsner P, Thiele JJ. Oxidative stress in malignant melanoma and non-melanoma skin cancer. British J Dermatol. 2003;148:913–922. doi: 10.1046/j.1365-2133.2003.05303.x. [DOI] [PubMed] [Google Scholar]
- 104.Zhang J, Bowden GT. Activation of p38 MAP kinase and JNK pathways by UVA irradiation. Photochem Photobiol Sci. 2012;11:54–61. doi: 10.1039/c1pp05133d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Cuadrado A, Nebreda AR. Mechanisms and functions of p38 MAPK signalling. Biochem J. 2010;429:403–417. doi: 10.1042/BJ20100323. [DOI] [PubMed] [Google Scholar]
- 106.Nadeau PJ, Charette SJ, Toledano MB, Landry J. Disulfide Bond-mediated multimerization of Ask1 and its reduction by thioredoxin-1 regulate H(2)O(2)-induced c-Jun NH(2)-terminal kinase activation and apoptosis. Mol Biol Cell. 2007;18:3903–3913. doi: 10.1091/mbc.E07-05-0491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Owens DM, Keyse SM. Differential regulation of MAP kinase signalling by dual-specificity protein phosphatases. Oncogene. 2007;26:3203–3213. doi: 10.1038/sj.onc.1210412. [DOI] [PubMed] [Google Scholar]
- 108.Gross S, Knebel A, Tenev T, Neininger A, Gaestel M, Herrlich P, Bohmer FD. Inactivation of protein-tyrosine phosphatases as mechanism of UV-induced signal transduction. J Biol Chem. 1999;274:26378–26386. doi: 10.1074/jbc.274.37.26378. [DOI] [PubMed] [Google Scholar]
- 109.Reinhardt HC, Yaffe MB. Kinases that control the cell cycle in response to DNA damage: Chk1, Chk2, and MK2. Curr Opin Cell Biol. 2009;21:245–255. doi: 10.1016/j.ceb.2009.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Reinhardt HC, Aslanian AS, Lees JA, Yaffe MB. p53-deficient cells rely on ATM- and ATR-mediated checkpoint signaling through the p38MAPK/MK2 pathway for survival after DNA damage. Cancer Cell. 2007;11:175–189. doi: 10.1016/j.ccr.2006.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Qiang L, Wu C, Ming M, Viollet B, He YY. Autophagy controls p38 activation to promote cell survival under genotoxic stress. J Biol Chem. 2013;288:1603–1611. doi: 10.1074/jbc.M112.415224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Liu L, Rezvani HR, Back JH, Hosseini M, Tang X, Zhu Y, Mahfouf W, Raad H, Raji G, Athar M, Kim AL, Bickers DR. Inhibition of p38 MAPK signaling augments skin tumorigenesis via NOX2 driven ROS generation. PloS one. 2014;9:e97245. doi: 10.1371/journal.pone.0097245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Bulavin DV, Saito S, Hollander MC, Sakaguchi K, Anderson CW, Appella E, Fornace AJ., Jr Phosphorylation of human p53 by p38 kinase coordinates N-terminal phosphorylation and apoptosis in response to UV radiation. EMBO J. 1999;18:6845–6854. doi: 10.1093/emboj/18.23.6845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Nys K, Van Laethem A, Michiels C, Rubio N, Piette JG, Garmyn M, Agostinis P. A p38(MAPK)/HIF-1 pathway initiated by UVB irradiation is required to induce Noxa and apoptosis of human keratinocytes. J Invest Dermatol. 2010;130:2269–2276. doi: 10.1038/jid.2010.93. [DOI] [PubMed] [Google Scholar]
- 115.Thornton TM, Pedraza-Alva G, Deng B, Wood CD, Aronshtam A, Clements JL, Sabio G, Davis RJ, Matthews DE, Doble B, Rincon M. Phosphorylation by p38 MAPK as an alternative pathway for GSK3beta inactivation. Science. 2008;320:667–670. doi: 10.1126/science.1156037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Dickinson SE, Olson ER, Zhang J, Cooper SJ, Melton T, Criswell PJ, Casanova A, Dong Z, Hu C, Saboda K, Jacobs ET, Alberts DS, Bowden GT. p38 MAP kinase plays a functional role in UVB-induced mouse skin carcinogenesis. Mol Carcinog. 2011;50:469–478. doi: 10.1002/mc.20734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Kyriakis JM, Avruch J. Mammalian mitogen-activated protein kinase signal transduction pathways activated by stress and inflammation. Physiol Rev. 2001;81:807–869. doi: 10.1152/physrev.2001.81.2.807. [DOI] [PubMed] [Google Scholar]
- 118.Silvers AL, Bachelor MA, Bowden GT. The role of JNK and p38 MAPK activities in UVA-induced signaling pathways leading to AP-1 activation and c-Fos expression. Neoplasia. 2003;5:319–329. doi: 10.1016/S1476-5586(03)80025-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Hess J, Angel P, Schorpp-Kistner M. AP-1 subunits: quarrel and harmony among siblings. J Cell Sci. 2004;117:5965–5973. doi: 10.1242/jcs.01589. [DOI] [PubMed] [Google Scholar]
- 120.Hilberg F, Aguzzi A, Howells N, Wagner EF. c-jun is essential for normal mouse development and hepatogenesis. Nature. 1993;365:179–181. doi: 10.1038/365179a0. [DOI] [PubMed] [Google Scholar]
- 121.Chen W, Borchers AH, Dong Z, Powell MB, Bowden GT. UVB irradiation-induced activator protein-1 activation correlates with increased c-fos gene expression in a human keratinocyte cell line. J Biol Chem. 1998;273:32176–32181. doi: 10.1074/jbc.273.48.32176. [DOI] [PubMed] [Google Scholar]
- 122.Silvers AL, Finch JS, Bowden GT. Inhibition of UVA-induced c-Jun N-terminal kinase activity results in caspase-dependent apoptosis in human keratinocytes. Photochem Photobiol. 2006;82:423–431. doi: 10.1562/2005-08-26-RA-659. [DOI] [PubMed] [Google Scholar]
- 123.Cooper SJ, MacGowan J, Ranger-Moore J, Young MR, Colburn NH, Bowden GT. Expression of dominant negative c-jun inhibits ultraviolet B-induced squamous cell carcinoma number and size in an SKH-1 hairless mouse model. Mol Cancer Res. 2003;1:848–854. [PubMed] [Google Scholar]
- 124.Gross ND, Boyle JO, Du B, Kekatpure VD, Lantowski A, Thaler HT, Weksler BB, Subbaramaiah K, Dannenberg AJ. Inhibition of Jun NH2-terminal kinases suppresses the growth of experimental head and neck squamous cell carcinoma. Clin Cancer Res. 2007;13:5910–5917. doi: 10.1158/1078-0432.CCR-07-0352. [DOI] [PubMed] [Google Scholar]
- 125.Wang X, Chen WR, Xing D. A pathway from JNK through decreased ERK and Akt activities for FOXO3a nuclear translocation in response to UV irradiation. J Cell Physiol. 2012;227:1168–1178. doi: 10.1002/jcp.22839. [DOI] [PubMed] [Google Scholar]
- 126.Dhanasekaran DN, Reddy EP. JNK signaling in apoptosis. Oncogene. 2008;27:6245–6251. doi: 10.1038/onc.2008.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Feehan RP, Shantz LM. Negative regulation of the FOXO3a transcription factor by mTORC2 induces a pro-survival response following exposure to ultraviolet-B irradiation. Cell Signal. 2016;28:798–809. doi: 10.1016/j.cellsig.2016.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Syed DN, Afaq F, Mukhtar H. Differential activation of signaling pathways by UVA and UVB radiation in normal human epidermal keratinocytes. Photochem Photobiol. 2012;88:1184–1190. doi: 10.1111/j.1751-1097.2012.01115.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Carr TD, DiGiovanni J, Lynch CJ, Shantz LM. Inhibition of mTOR suppresses UVB-induced keratinocyte proliferation and survival. Cancer Prev Res. 2012;5:1394–1404. doi: 10.1158/1940-6207.CAPR-12-0272-T. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Gaffney DC, Soyer HP, Simpson F. The epidermal growth factor receptor in squamous cell carcinoma: An emerging drug target. Australas J Dermatol. 2014;55:24–34. doi: 10.1111/ajd.12025. [DOI] [PubMed] [Google Scholar]
- 131.Rodust PM, Stockfleth E, Ulrich C, Leverkus M, Eberle J. UV-induced squamous cell carcinoma--a role for antiapoptotic signalling pathways. British J Dermatol. 2009;161(Suppl 3):107–115. doi: 10.1111/j.1365-2133.2009.09458.x. [DOI] [PubMed] [Google Scholar]
- 132.Coffer PJ, Burgering BM, Peppelenbosch MP, Bos JL, Kruijer W. UV activation of receptor tyrosine kinase activity. Oncogene. 1995;11:561–569. [PubMed] [Google Scholar]
- 133.Falus A, Hegyesi H, Lazar-Molnar E, Pos Z, Laszlo V, Darvas Z. Paracrine and autocrine interactions in melanoma: histamine is a relevant player in local regulation. Trends Immunol. 2001;22:648–652. doi: 10.1016/s1471-4906(01)02050-6. [DOI] [PubMed] [Google Scholar]
- 134.He YY, Council SE, Feng L, Chignell CF. UVA-induced cell cycle progression is mediated by a disintegrin and metalloprotease/epidermal growth factor receptor/AKT/Cyclin D1 pathways in keratinocytes. Cancer Res. 2008;68:3752–3758. doi: 10.1158/0008-5472.CAN-07-6138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Ley KD, Ellem KA. UVC modulation of epidermal growth factor receptor number in HeLa S3 cells. Carcinogenesis. 1992;13:183–187. doi: 10.1093/carcin/13.2.183. [DOI] [PubMed] [Google Scholar]
- 136.Cao C, Lu S, Kivlin R, Wallin B, Card E, Bagdasarian A, Tamakloe T, Chu WM, Guan KL, Wan Y. AMP-activated protein kinase contributes to UV- and H2O2-induced apoptosis in human skin keratinocytes. J Biol Chem. 2008;283:28897–28908. doi: 10.1074/jbc.M804144200. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 137.Zhang Y, Dong Z, Bode AM, Ma WY, Chen N, Dong Z. Induction of EGFR-dependent and EGFR-independent signaling pathways by ultraviolet A irradiation. DNA Cell Biol. 2001;20:769–779. doi: 10.1089/104454901753438589. [DOI] [PubMed] [Google Scholar]
- 138.Nakamura S, Takahashi H, Kinouchi M, Manabe A, Ishida-Yamamoto A, Hashimoto Y, Iizuka H. Differential phosphorylation of mitogen-activated protein kinase families by epidermal growth factor and ultraviolet B irradiation in SV40-transformed human keratinocytes. J Dermatol Sci. 2001;25:139–149. doi: 10.1016/s0923-1811(00)00123-7. [DOI] [PubMed] [Google Scholar]
- 139.Fuchs E, Raghavan S. Getting under the skin of epidermal morphogenesis. Nature reviews Genetics. 2002;3:199–209. doi: 10.1038/nrg758. [DOI] [PubMed] [Google Scholar]
- 140.Arora A, Scholar EM. Role of tyrosine kinase inhibitors in cancer therapy. JPharmacol Exper Ther. 2005;315:971–979. doi: 10.1124/jpet.105.084145. [DOI] [PubMed] [Google Scholar]
- 141.Spallone G, Botti E, Costanzo A. Targeted therapy in nonmelanoma skin cancers. Cancers. 2011;3:2255–2273. doi: 10.3390/cancers3022255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Alayev A, Holz MK. mTOR signaling for biological control and cancer. J Cell Physiol. 2013;228:1658–1664. doi: 10.1002/jcp.24351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Laplante M, Sabatini DM. mTOR signaling in growth control and disease. Cell. 2012;149:274–293. doi: 10.1016/j.cell.2012.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Albanell J, Dalmases A, Rovira A, Rojo F. mTOR signalling in human cancer. Clin Trans Oncol. 2007;9:484–493. doi: 10.1007/s12094-007-0092-6. [DOI] [PubMed] [Google Scholar]
- 145.Carr TD, Feehan RP, Hall MN, Ruegg MA, Shantz LM. Conditional disruption of rictor demonstrates a direct requirement for mTORC2 in skin tumor development and continued growth of established tumors. Carcinogenesis. 2015;36:487–497. doi: 10.1093/carcin/bgv012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Wan YS, Wang ZQ, Shao Y, Voorhees JJ, Fisher GJ. Ultraviolet irradiation activates PI 3-kinase/AKT survival pathway via EGF receptors in human skin in vivo. Int J Oncol. 2001;18:461–466. doi: 10.3892/ijo.18.3.461. [DOI] [PubMed] [Google Scholar]
- 147.Ming M, He YY. PTEN: new insights into its regulation and function in skin cancer. J Invest Dermatol. 2009;129:2109–2112. doi: 10.1038/jid.2009.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Hafner C, Landthaler M, Vogt T. Activation of the PI3K/AKT signalling pathway in non-melanoma skin cancer is not mediated by oncogenic PIK3CA and AKT1 hotspot mutations. Exp Dermatol. 2010;19:e222–227. doi: 10.1111/j.1600-0625.2009.01056.x. [DOI] [PubMed] [Google Scholar]
- 149.Einspahr JG, Calvert V, Alberts DS, Curiel-Lewandrowski C, Warneke J, Krouse R, Stratton SP, Liotta L, Longo C, Pellacani G, Prasad A, Sagerman P, Bermudez Y, Deng J, Bowden GT, Petricoin EF., 3rd Functional protein pathway activation mapping of the progression of normal skin to squamous cell carcinoma. Cancer Prev Res. 2012;5:403–413. doi: 10.1158/1940-6207.CAPR-11-0427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Manning BD, Cantley LC. AKT/PKB signaling: navigating downstream. Cell. 2007;129:1261–1274. doi: 10.1016/j.cell.2007.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Davies MA. Regulation, role, and targeting of Akt in cancer. J Clin Oncol. 2011;29:4715–4717. doi: 10.1200/JCO.2011.37.4751. [DOI] [PubMed] [Google Scholar]
- 152.Vanhaesebroeck B, Stephens L, Hawkins P. PI3K signalling: the path to discovery and understanding. Nat Rev Mol Cell Biol. 2012;13:195–203. doi: 10.1038/nrm3290. [DOI] [PubMed] [Google Scholar]
- 153.Showkat M, Beigh MA, Andrabi KI. mTOR Signaling in Protein Translation Regulation: Implications in Cancer Genesis and Therapeutic Interventions. Mol Biol Int. 2014;2014:686984. doi: 10.1155/2014/686984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Hemmings BA, Restuccia DF. PI3K-PKB/Akt pathway. Cold Spring Harb Perspect Biol. 2012;4:a011189. doi: 10.1101/cshperspect.a011189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Laplante M, Sabatini DM. Regulation of mTORC1 and its impact on gene expression at a glance. J Cell Sci. 2013;126:1713–1719. doi: 10.1242/jcs.125773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Shimobayashi M, Hall MN. Making new contacts: the mTOR network in metabolism and signalling crosstalk. Nat Rev Mol Cell Biol. 2014;15:155–162. doi: 10.1038/nrm3757. [DOI] [PubMed] [Google Scholar]
- 157.Populo H, Lopes JM, Soares P. The mTOR signalling pathway in human cancer. Int J Mol Sci. 2012;13:1886–1918. doi: 10.3390/ijms13021886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Seto B. Rapamycin and mTOR: a serendipitous discovery and implications for breast cancer. Clin Transl Med. 2012;1:29. doi: 10.1186/2001-1326-1-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Dufour M, Dormond-Meuwly A, Demartines N, Dormond O. Targeting the Mammalian Target of Rapamycin (mTOR) in Cancer Therapy: Lessons from Past and Future Perspectives. Cancers. 2011;3:2478–2500. doi: 10.3390/cancers3022478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Cloughesy TF, Yoshimoto K, Nghiemphu P, Brown K, Dang J, Zhu S, Hsueh T, Chen Y, Wang W, Youngkin D, Liau L, Martin N, Becker D, Bergsneider M, Lai A, Green R, Oglesby T, Koleto M, Trent J, Horvath S, Mischel PS, Mellinghoff IK, Sawyers CL. Antitumor activity of rapamycin in a Phase I trial for patients with recurrent PTEN-deficient glioblastoma. PLoS Med. 2008;5:e8. doi: 10.1371/journal.pmed.0050008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Sehgal SN. Sirolimus: its discovery, biological properties, and mechanism of action. Transplant Proc. 2003;35:7S–14S. doi: 10.1016/s0041-1345(03)00211-2. [DOI] [PubMed] [Google Scholar]
- 162.Schreiber KH, Ortiz D, Academia EC, Anies AC, Liao CY, Kennedy BK. Rapamycin-mediated mTORC2 inhibition is determined by the relative expression of FK506-binding proteins. Aging Cell. 2015;14:265–273. doi: 10.1111/acel.12313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Checkley LA, Rho O, Moore T, Hursting S, DiGiovanni J. Rapamycin is a potent inhibitor of skin tumor promotion by 12-O-tetradecanoylphorbol-13-acetate. Cancer Prev Res. 2011;4:1011–1020. doi: 10.1158/1940-6207.CAPR-10-0375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Campbell SB, Walker R, Tai SS, Jiang Q, Russ GR. Randomized controlled trial of sirolimus for renal transplant recipients at high risk for nonmelanoma skin cancer. Am J Transplant. 2012;12:1146–1156. doi: 10.1111/j.1600-6143.2012.04004.x. [DOI] [PubMed] [Google Scholar]
- 165.Dickinson SE, Janda J, Criswell J, Blohm-Mangone K, Olson ER, Liu Z, Barber C, Petricoin EF, 3rd, Calvert VS, Einspahr J, Dickinson JE, Stratton SP, Curiel-Lewandrowski C, Saboda K, Hu C, Bode AM, Dong Z, Alberts DS, Timothy Bowden G. Inhibition of Akt Enhances the Chemopreventive Effects of Topical Rapamycin in Mouse Skin. Cancer Prev Res. 2016;9:215–224. doi: 10.1158/1940-6207.CAPR-15-0419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Wang YD, Su YJ, Li JY, Yao XC, Liang GJ. Rapamycin, an mTOR inhibitor, induced apoptosis via independent mitochondrial and death receptor pathway in retinoblastoma Y79 cell. Int J Clin Exp Med. 2015;8:10723–10730. [PMC free article] [PubMed] [Google Scholar]
- 167.Chen S, Ren Q, Zhang J, Ye Y, Zhang Z, Xu Y, Guo M, Ji H, Xu C, Gu C, Gao W, Huang S, Chen L. N-acetyl-L-cysteine protects against cadmium-induced neuronal apoptosis by inhibiting ROS-dependent activation of Akt/mTOR pathway in mouse brain. Neuropathol Appl Neurobiol. 2014;40:759–777. doi: 10.1111/nan.12103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Samkari A, Cooper ZA, Holloway MP, Liu J, Altura RA. Rapamycin induces the anti-apoptotic protein survivin in neuroblastoma. Int J Biochem Mol Biol. 2012;3:28–35. [PMC free article] [PubMed] [Google Scholar]
- 169.Chen L, Xu B, Liu L, Luo Y, Zhou H, Chen W, Shen T, Han X, Kontos CD, Huang S. Cadmium induction of reactive oxygen species activates the mTOR pathway, leading to neuronal cell death. Free Radic Biol Med. 2011;50:624–632. doi: 10.1016/j.freeradbiomed.2010.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Zhang JF, Liu JJ, Lu MQ, Cai CJ, Yang Y, Li H, Xu C, Chen GH. Rapamycin inhibits cell growth by induction of apoptosis on hepatocellular carcinoma cells in vitro. Transpl Immunol. 2007;17:162–168. doi: 10.1016/j.trim.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 171.Zou Z, Chen J, Yang J, Bai X. Targeted Inhibition of Rictor/mTORC2 in Cancer Treatment: A New Era after Rapamycin. Curr Cancer Drug Targets. 2016;16:288–304. doi: 10.2174/1568009616666151113120830. [DOI] [PubMed] [Google Scholar]
- 172.Gan X, Wang J, Su B, Wu D. Evidence for direct activation of mTORC2 kinase activity by phosphatidylinositol 3,4,5-trisphosphate. J Biol Chem. 2011;286:10998–11002. doi: 10.1074/jbc.M110.195016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Liu P, Gan W, Chin YR, Ogura K, Guo J, Zhang J, Wang B, Blenis J, Cantley LC, Toker A, Su B, Wei W. PtdIns(3,4,5)P3-Dependent Activation of the mTORC2 Kinase Complex. Cancer Discov. 2015;5:1194–1209. doi: 10.1158/2159-8290.CD-15-0460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Sarbassov DD, Ali SM, Kim DH, Guertin DA, Latek RR, Erdjument-Bromage H, Tempst P, Sabatini DM. Rictor, a novel binding partner of mTOR, defines a rapamycin-insensitive and raptor-independent pathway that regulates the cytoskeleton. Curr Biol. 2004;14:1296–1302. doi: 10.1016/j.cub.2004.06.054. [DOI] [PubMed] [Google Scholar]
- 175.Tu Y, Ji C, Yang B, Yang Z, Gu H, Lu CC, Wang R, Su ZL, Chen B, Sun WL, Xia JP, Bi ZG, He L. DNA-dependent protein kinase catalytic subunit (DNA-PKcs)-SIN1 association mediates ultraviolet B (UVB)-induced Akt Ser-473 phosphorylation and skin cell survival. Mol Cancer. 2013;12:172. doi: 10.1186/1476-4598-12-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Roos WP, Thomas AD, Kaina B. DNA damage and the balance between survival and death in cancer biology. Nat Rev Cancer. 2016;16:20–33. doi: 10.1038/nrc.2015.2. [DOI] [PubMed] [Google Scholar]
- 177.Yu T, Ji J, Guo YL. MST1 activation by curcumin mediates JNK activation, Foxo3a nuclear translocation and apoptosis in melanoma cells. Bioch Biophys Res Commun. 2013;441:53–58. doi: 10.1016/j.bbrc.2013.10.008. [DOI] [PubMed] [Google Scholar]
- 178.Shukla S, Shukla M, Maclennan GT, Fu P, Gupta S. Deregulation of FOXO3A during prostate cancer progression. Int J Oncol. 2009;34:1613–1620. doi: 10.3892/ijo_00000291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Masui K, Tanaka K, Akhavan D, Babic I, Gini B, Matsutani T, Iwanami A, Liu F, Villa GR, Gu Y, Campos C, Zhu S, Yang H, Yong WH, Cloughesy TF, Mellinghoff IK, Cavenee WK, Shaw RJ, Mischel PS. mTOR complex 2 controls glycolytic metabolism in glioblastoma through FoxO acetylation and upregulation of c-Myc. Cell Metab. 2013;18:726–739. doi: 10.1016/j.cmet.2013.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Maiese K, Chong ZZ, Shang YC. OutFOXOing disease and disability: the therapeutic potential of targeting FoxO proteins. Trends Mol Med. 2008;14:219–227. doi: 10.1016/j.molmed.2008.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Maiese K, Chong ZZ, Shang YC. “Sly as a FOXO”: new paths with Forkhead signaling in the brain. Curr Neurovasc Res. 2007;4:295–302. doi: 10.2174/156720207782446306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Katoh M, Igarashi M, Fukuda H, Nakagama H, Katoh M. Cancer genetics and genomics of human FOX family genes. Cancer Lett. 2013;328:198–206. doi: 10.1016/j.canlet.2012.09.017. [DOI] [PubMed] [Google Scholar]
- 183.Greer EL, Brunet A. FOXO transcription factors at the interface between longevity and tumor suppression. Oncogene. 2005;24:7410–7425. doi: 10.1038/sj.onc.1209086. [DOI] [PubMed] [Google Scholar]
- 184.Daitoku H, Fukamizu A. FOXO transcription factors in the regulatory networks of longevity. J Biochem. 2007;141:769–774. doi: 10.1093/jb/mvm104. [DOI] [PubMed] [Google Scholar]
- 185.Allen JE, Krigsfeld G, Mayes PA, Patel L, Dicker DT, Patel AS, Dolloff NG, Messaris E, Scata KA, Wang W, Zhou JY, Wu GS, El-Deiry WS. Dual inactivation of Akt and ERK by TIC10 signals Foxo3a nuclear translocation, TRAIL gene induction, and potent antitumor effects. Sci Transl Med. 2013;5:171ra117. doi: 10.1126/scitranslmed.3004828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Zhang X, Tang N, Hadden TJ, Rishi AK. Akt, FoxO and regulation of apoptosis. Biochim Biophys Acta. 2011;1813:1978–1986. doi: 10.1016/j.bbamcr.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 187.Bivik C, Ollinger K. JNK mediates UVB-induced apoptosis upstream lysosomal membrane permeabilization and Bcl-2 family proteins. Apoptosis. 2008;13:1111–1120. doi: 10.1007/s10495-008-0240-7. [DOI] [PubMed] [Google Scholar]
- 188.Kim DJ, Kataoka K, Sano S, Connolly K, Kiguchi K, DiGiovanni J. Targeted disruption of Bcl-xL in mouse keratinocytes inhibits both UVB- and chemically induced skin carcinogenesis. Mol Carcinog. 2009;48:873–885. doi: 10.1002/mc.20527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Qin JZ, Bacon P, Panella J, Sitailo LA, Denning MF, Nickoloff BJ. Low-dose UV-radiation sensitizes keratinocytes to TRAIL-induced apoptosis. J Cell Physiol. 2004;200:155–166. doi: 10.1002/jcp.20017. [DOI] [PubMed] [Google Scholar]
- 190.Engelman JA. Targeting PI3K signalling in cancer: opportunities, challenges and limitations. Nat Rev Cancer. 2009;9:550–562. doi: 10.1038/nrc2664. [DOI] [PubMed] [Google Scholar]
- 191.Xie Q, Chen J, Yuan Z. Post-translational regulation of FOXO. Acta Biochim Biophys Sin. 2012;44:897–901. doi: 10.1093/abbs/gms067. [DOI] [PubMed] [Google Scholar]
- 192.Brunet A, Bonni A, Zigmond MJ, Lin MZ, Juo P, Hu LS, Anderson MJ, Arden KC, Blenis J, Greenberg ME. Akt promotes cell survival by phosphorylating and inhibiting a Forkhead transcription factor. Cell. 1999;96:857–868. doi: 10.1016/s0092-8674(00)80595-4. [DOI] [PubMed] [Google Scholar]
- 193.Obsil T, Ghirlando R, Anderson DE, Hickman AB, Dyda F. Two 14-3-3 binding motifs are required for stable association of Forkhead transcription factor FOXO4 with 14-3-3 proteins and inhibition of DNA binding. Biochemistry. 2003;42:15264–15272. doi: 10.1021/bi0352724. [DOI] [PubMed] [Google Scholar]
- 194.Brunet A, Kanai F, Stehn J, Xu J, Sarbassova D, Frangioni JV, Dalal SN, DeCaprio JA, Greenberg ME, Yaffe MB. 14-3-3 transits to the nucleus and participates in dynamic nucleocytoplasmic transport. J Cell Biol. 2002;156:817–828. doi: 10.1083/jcb.200112059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Tzivion G, Dobson M, Ramakrishnan G. FoxO transcription factors; Regulation by AKT and 14-3-3 proteins. Biochim Biophys Acta. 2011;1813:1938–1945. doi: 10.1016/j.bbamcr.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 196.Engelberg D, Klein C, Martinetto H, Struhl K, Karin M. The UV response involving the Ras signaling pathway and AP-1 transcription factors is conserved between yeast and mammals. Cell. 1994;77:381–390. doi: 10.1016/0092-8674(94)90153-8. [DOI] [PubMed] [Google Scholar]
- 197.Bermudez Y, Stratton SP, Curiel-Lewandrowski C, Warneke J, Hu C, Bowden GT, Dickinson SE, Dong Z, Bode AM, Saboda K, Brooks CA, Petricoin EF, 3rd, Hurst CA, Alberts DS, Einspahr JG. Activation of the PI3K/Akt/mTOR and MAPK Signaling Pathways in Response to Acute Solar-Simulated Light Exposure of Human Skin. Cancer Prev Res. 2015;8:720–728. doi: 10.1158/1940-6207.CAPR-14-0407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Cheepala SB, Yin W, Syed Z, Gill JN, McMillian A, Kleiner HE, Lynch M, Loganantharaj R, Trutschl M, Cvek U, Clifford JL. Identification of the B-Raf/Mek/Erk MAP kinase pathway as a target for all-trans retinoic acid during skin cancer promotion. Molecular cancer. 2009;8:27. doi: 10.1186/1476-4598-8-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.van Hattum H, Waldmann H. Chemical biology tools for regulating RAS signaling complexity in space and time. Chemistry & biology. 2014;21:1185–1195. doi: 10.1016/j.chembiol.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 200.Holderfield M, Deuker MM, McCormick F, McMahon M. Targeting RAF kinases for cancer therapy: BRAF-mutated melanoma and beyond. Nat Rev Cancer. 2014;14:455–467. doi: 10.1038/nrc3760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Wellbrock C, Karasarides M, Marais R. The RAF proteins take centre stage. Nature reviews Mol Cell Biol. 2004;5:875–885. doi: 10.1038/nrm1498. [DOI] [PubMed] [Google Scholar]
- 202.McCubrey JA, Steelman LS, Chappell WH, Abrams SL, Wong EW, Chang F, Lehmann B, Terrian DM, Milella M, Tafuri A, Stivala F, Libra M, Basecke J, Evangelisti C, Martelli AM, Franklin RA. Roles of the Raf/MEK/ERK pathway in cell growth, malignant transformation and drug resistance. Biochim Biophys Acta. 2007;1773:1263–1284. doi: 10.1016/j.bbamcr.2006.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Omran OM, Ata HS. Expression of tumor necrosis factor-related apoptosis-inducing ligand death receptors DR4 and DR5 in human nonmelanoma skin cancer. Amer J Dermatopathol. 2014;36:710–717. doi: 10.1097/DAD.0b013e3182a3d31d. [DOI] [PubMed] [Google Scholar]
- 204.Yang JY, Zong CS, Xia W, Yamaguchi H, Ding Q, Xie X, Lang JY, Lai CC, Chang CJ, Huang WC, Huang H, Kuo HP, Lee DF, Li LY, Lien HC, Cheng X, Chang KJ, Hsiao CD, Tsai FJ, Tsai CH, Sahin AA, Muller WJ, Mills GB, Yu D, Hortobagyi GN, Hung MC. ERK promotes tumorigenesis by inhibiting FOXO3a via MDM2-mediated degradation. Nat Cell Biol. 2008;10:138–148. doi: 10.1038/ncb1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Dobson M, Ramakrishnan G, Ma S, Kaplun L, Balan V, Fridman R, Tzivion G. Bimodal regulation of FoxO3 by AKT and 14-3-3. Biochim Biophys Acta. 2011;1813:1453–1464. doi: 10.1016/j.bbamcr.2011.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Shimizu T, Tolcher AW, Papadopoulos KP, Beeram M, Rasco DW, Smith LS, Gunn S, Smetzer L, Mays TA, Kaiser B, Wick MJ, Alvarez C, Cavazos A, Mangold GL, Patnaik A. The clinical effect of the dual-targeting strategy involving PI3K/AKT/mTOR and RAS/MEK/ERK pathways in patients with advanced cancer. Clin Cancer Res. 2012;18:2316–2325. doi: 10.1158/1078-0432.CCR-11-2381. [DOI] [PubMed] [Google Scholar]
- 207.Prabhu VV, Allen JE, Dicker DT, El-Deiry WS. Small-Molecule ONC201/TIC10 Targets Chemotherapy-Resistant Colorectal Cancer Stem-like Cells in an Akt/Foxo3a/TRAIL-Dependent Manner. Cancer Res. 2015;75:1423–1432. doi: 10.1158/0008-5472.CAN-13-3451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Roy SK, Srivastava RK, Shankar S. Inhibition of PI3K/AKT and MAPK/ERK pathways causes activation of FOXO transcription factor, leading to cell cycle arrest and apoptosis in pancreatic cancer. J Mol Signal. 2010;5:10. doi: 10.1186/1750-2187-5-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Dent P. Crosstalk between ERK, AKT, and cell survival. Cancer Biol Ther. 2014;15:245–246. doi: 10.4161/cbt.27541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.McIlwain DR, Berger T, Mak TW. Caspase functions in cell death and disease. Cold Spring Harb Perspect Biol. 2015:7. doi: 10.1101/cshperspect.a026716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Dickens LS, Boyd RS, Jukes-Jones R, Hughes MA, Robinson GL, Fairall L, Schwabe JW, Cain K, Macfarlane M. A death effector domain chain DISC model reveals a crucial role for caspase-8 chain assembly in mediating apoptotic cell death. Mol Cell. 2012;47:291–305. doi: 10.1016/j.molcel.2012.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Bekes M, Salvesen GS. The CULt of caspase-8 ubiquitination. Cell. 2009;137:604–606. doi: 10.1016/j.cell.2009.04.052. [DOI] [PubMed] [Google Scholar]
- 213.Elmore S. Apoptosis: a review of programmed cell death. Toxicol Pathol. 2007;35:495–516. doi: 10.1080/01926230701320337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Kedinger V, Muller S, Gronemeyer H. Targeted expression of tumor necrosis factor-related apoptosis-inducing ligand TRAIL in skin protects mice against chemical carcinogenesis. Mol Cancer. 2011;10:34. doi: 10.1186/1476-4598-10-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Takeda K, Stagg J, Yagita H, Okumura K, Smyth MJ. Targeting death-inducing receptors in cancer therapy. Oncogene. 2007;26:3745–3757. doi: 10.1038/sj.onc.1210374. [DOI] [PubMed] [Google Scholar]
- 216.Tait SW, Green DR. Mitochondria and cell death: outer membrane permeabilization and beyond. Nat Rev Mol Cell Biol. 2010;11:621–632. doi: 10.1038/nrm2952. [DOI] [PubMed] [Google Scholar]
- 217.Westphal D, Dewson G, Czabotar PE, Kluck RM. Molecular biology of Bax and Bak activation and action. Biochim Biophys Acta. 2011;1813:521–531. doi: 10.1016/j.bbamcr.2010.12.019. [DOI] [PubMed] [Google Scholar]
- 218.Hardwick JM, Soane L. Multiple functions of BCL-2 family proteins. Cold Spring Harb Perspect Biol. 2013:5. doi: 10.1101/cshperspect.a008722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Nys K, Agostinis P. Bcl-2 family members: essential players in skin cancer. Cancer Lett. 2012;320:1–13. doi: 10.1016/j.canlet.2012.01.031. [DOI] [PubMed] [Google Scholar]
- 220.Ren D, Tu HC, Kim H, Wang GX, Bean GR, Takeuchi O, Jeffers JR, Zambetti GP, Hsieh JJ, Cheng EH. BID, BIM, and PUMA are essential for activation of the BAX- and BAK-dependent cell death program. Science. 2010;330:1390–1393. doi: 10.1126/science.1190217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Kim JY, Ahn HJ, Ryu JH, Such K, Park JH. BH3-only protein Noxa is a mediator of hypoxic cell death induced by hypoxia-inducible factor 1alpha. J Exp Med. 2004;199:113–124. doi: 10.1084/jem.20030613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Riled SJ, Salvesen GS. The apoptosome: signalling platform of cell death. Nature reviews Mol Cell Biol. 2007;8:405–413. doi: 10.1038/nrm2153. [DOI] [PubMed] [Google Scholar]
- 223.Wu CS, Chen GS, Lin PY, Pan IH, Wang ST, Lin SH, Yu HS, Lin CC. Tazarotene induces apoptosis in human basal cell carcinoma via activation of caspase-8/t-Bid and the reactive oxygen species-dependent mitochondrial pathway. DNA Cell Biol. 2014;33:652–666. doi: 10.1089/dna.2014.2366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Lee da H, Nam YJ, Kim YJ, Lee MW, Lee CS. Rotundarpene prevents TRAIL-induced apoptosis in human keratinocytes by suppressing the caspase-8- and Bid-pathways and the mitochondrial pathway. Naunyn Schmiedebergs Arch Pharmacol. 2014;387:1209–1219. doi: 10.1007/s00210-014-1051-8. [DOI] [PubMed] [Google Scholar]
- 225.Eberle J, Fecker LF, Forschner T, Ulrich C, Rowert-Huber J, Stockfleth E. Apoptosis pathways as promising targets for skin cancer therapy. Br J Dermatol. 2007;156(Suppl 3):18–24. doi: 10.1111/j.1365-2133.2007.07855.x. [DOI] [PubMed] [Google Scholar]