Abstract
Background/Aims
Subjective memory complaints (SMC) are strong predictors of mild cognitive impairment (MCI) and subsequent Alzheimer's disease. Our aims were to see if fully automated cerebral MR volume measurements could distinguish subjects with SMC and MCI from controls, and if probable parental late-onset Alzheimer's disease (LOAD), apolipoprotein E ε4 genotype, total plasma homocysteine, and cardiovascular risk factors were associated with MR volumetric findings.
Methods
198 stroke-free subjects comprised the control (n = 58), the SMC (n = 25) and the MCI (n = 115) groups. Analysis of covariance and receiver operating characteristic curve was used to see if MR volumetry distinguished subjects with SMC and MCI from controls.
Results
Subjects with SMC and MCI had significantly larger lateral ventricles and smaller hippocampal volumes than controls. The area under the curve in subjects with SMC and MCI compared to that of controls was less than 0.68 for all volumes of intracranial structures. There was an interaction between sex and probable parental LOAD for hippocampal volume, with a significant association between probable parental LOAD and hippocampal volume in women.
Conclusions
Fully automated MR volumetry can distinguish subjects with SMC and MCI from controls in a general population, but insufficiently to assume a clear clinical role. Research on sporadic LOAD might benefit from a sex-specific search for genetic risk factors.
Keywords: Alzheimer's disease, Apolipoprotein E4, Cardiovascular risk factors, Family history, Gender, Homocysteine, Magnetic resonance imaging, Mild cognitive impairment, Subjective memory complaints
Introduction
Alzheimer's disease (AD) usually has a long preclinical phase with a gradual cognitive decline, until eventually appearing as mild cognitive impairment (MCI) and Alzheimer's dementia [1]. Subjective memory complaints (SMC) may represent an early phase of cognitive decline, and may be an earlier harbinger of AD than MCI [2]. Persons with SMC score normally on standardized cognitive tests, and those with AD are interspersed among others with SMC due to various reasons [3, 4]. SMC can nevertheless predict dementia earlier than MCI [5, 6].
Cognitive tests have limited sensitivity and specificity in assessing cognitive impairment due to the wide span in normal cognitive function [7]. Self-reported and informant-reported memory complaints are more predictive of later cognitive decline than cognitive testing [8]. Since self-reported memory complaints have low diagnostic accuracy, it underlines the need for preclinical biomarkers of neurodegenerative diseases [9, 10]. For clinical utilization, they preferably have to be cost-effective and noninvasive.
Newer brain visualization methods are promising, and one of them is the application of fully automated brain MR volumetry [11, 12]. It is less expensive and time-consuming than manual or semiautomatic segmentation of brain structures, and more precise than qualitative visual assessment [13]. Volumetry of brain structures is a surrogate marker of AD, and many disorders can cause regional or global atrophy in the brain [14]. Earlier studies have shown that fully automated volumetry with the software package NeuroQuant cannot be used alone clinically, but that it can support other clinical investigations in diagnosing Alzheimer's dementia [15].
AD is the most prevalent cerebral degenerative disease and can be classified into early-onset AD (<5% AD cases), and familial (15–25%) and sporadic (75%) late-onset AD (LOAD) [16, 17, 18]. First-degree relatives have a three- to fourfold risk of developing AD, and for those with a parent with LOAD the risk is especially high [18, 19, 20]. The ε4 allele of the apolipoprotein E (APOE) gene is the best documented genetic risk factor for sporadic LOAD, but is only associated with half of the increased risk of AD in monozygotic twins, and other genes are clearly involved [17, 18, 21].
Coexisting cerebral small-vessel disease is often seen in AD, and there might be an overlap between vascular disease and AD [22, 23, 24]. Total plasma homocysteine (tHcy) and cardiovascular risk factors are therefore possible risk factors for AD [25, 26, 27].
Our objective was to see whether fully automated MR volumetry could distinguish persons with SMC and MCI from controls. Furthermore, we aimed to examine if MR volumetric findings were associated with probable LOAD in parent(s), ApoE ε4 genotype, tHcy and cardiovascular risk factors.
Materials and Methods
Study Design, Population, Cognitive Testing, Interviews and Biochemical Analyses
Details on the design of the Tromsø Dementia Study have previously been described [19]. The Tromsø Dementia Study is a nested case-control study carried out in the sixth survey of the Tromsø Study (Tromsø 6). The Tromsø Study, a prospective cohort study, addresses cardiovascular and other chronic diseases [28]. The first survey took place in 1974 and Tromsø 6 in 2007–2008. The cognitive tests in Tromsø 6 were the finger-tapping test, the digit symbol-coding test, the Mini-Mental State Examination and the 12-word test (a modification of the Californian Verbal Learning test) [7, 29, 30, 31]. The 12-word test measures verbal episodic memory using both immediate recall (word test part 1) and cued recall (word test part 2).
Subjects with a Mini-Mental State Examination score of <24 and/or a cognitive test score below the 2.5th percentile in Tromsø 5 on one of the cognitive tests in Tromsø 6 and who reported SMC were considered to have MCI. We applied the MCI construct as originally proposed by Petersen et al. [32]. Subjects who did not fulfill the criteria for MCI, but reported subjective memory problems by answering ‘yes’ to ‘Has your memory declined?’ on a questionnaire in Tromsø 6, were considered to have SMC. Subjects who answered ‘no’ to ‘Has your memory declined?’, and whose cognitive test scores in Tromsø 6 were above the cutoffs, were eligible as controls.
The Tromsø Dementia Study also applied the Trail Making Test A, the Trail Making Test B, the Informant Questionnaire on Cognitive Decline in the Elderly, the clock-drawing test, the Montgomery-Åsberg Depression Rating Scale and the Rapid Disability Rating Scale-2 [19]. In addition, the Norwegian revised version of Greene et al.'s Behavior and Mood Disturbance (BMD) scale was used [33]. It has 20 questions on behavior and 13 questions on cognition. All answers are scored from 0 to 4, and scores of ≤40 for behavior (BMD behavior) and ≥26 for cognition (BMD cognition) are considered normal.
Comprehensive interviews of subjects and informants on familial dispersion of probable LOAD identified subjects who had biological first-, second- and third-degree relatives with probable LOAD. We recorded age of onset of dementia and whether the onset was insidious or possibly caused by other diseases than LOAD, for instance Parkinson's disease or stroke. For the few subjects who were unaccompanied by a family member or a close friend, a family member or a close friend mailed the information afterwards. In the present study, we included subjects with information on the dispersion of probable LOAD in first-degree relatives. If subjects had a parent or parents with probable LOAD, it was termed as probable parental LOAD, and if not, it was termed as no parental LOAD.
All subjects were comprehensively interviewed regarding medication, earlier diseases and current health condition. None of the subjects had known neurodegenerative diseases or psychiatric disorders.
In addition to the 58 controls and 103 subjects with MCI described in our first paper on the Tromsø Dementia Study, 25 subjects who fulfilled the criteria for SMC and had no signs of cerebral stroke (not lacunar infarctions) on MRI were included. Further, 6 subjects with MCI who had not participated in our first study, due to incomplete information on probable LOAD in second- and third-degree relatives, and 6 subjects with MCI who reported earlier cerebral stroke, but whose MRI showed no signs thereof, were also included. The subjects thus constituted three groups: controls (n = 58), SMC (n = 25) and MCI (n = 115).
Standard Protocol Approvals, Registration and Patient Consents
The study was approved by the board of the Tromsø Study, the Regional Ethics Committee of Northern Norway and the Norwegian Social Science Data Services. All participants gave their informed consent.
Cerebral MRI
All examinations were performed using one of two identical Phillips 1.5T Intera scanners with a 6-channel head coil. A high-resolution 3D T1-weighted magnetization-prepared rapid-gradient echo (MPRAGE) scan and an axial T2-weighted FLAIR scan were obtained for each subject. The MPRAGE scans were used for volumetric measurements. Key parameters for the MPRAGE sequence were the following: TE = 4.0 ms, TR = 2,300 ms, TI = 1,000 ms, flip angle = 8°, FOV = 240 × 240 mm2, and voxel size = 0.94 × 0.94 × 1.20 mm3.
The NeuroQuant software package release 1.1.0.1123 (http://www.cortechs.net/) was used for fully automatic volume measurements of total intracranial volume (ICV), cerebral cortical gray matter, cerebral white matter and several subcortical structures including the amygdala and hippocampus. Except for ICV, volumes were reported for each hemisphere. NeuroQuant has been validated against manually traced volumes and semiautomatic methods [34, 35]. In order to adjust for differences in brain size, we used ICV-corrected volumes in the subsequent statistical analysis. These were obtained by summing the right and left hemisphere volumes for each structure and expressing this as a percentage of the ICV. Two neuroradiologists examined all scans together for pathology and made consensus-based judgments. White matter hyperintensities (WMH) were segmented using a semiautomatic procedure by one rater (T. Vangberg). The ‘paint grow-fuzzy connectedness’ tool in MIPAV v 5.1.1 (http://mipav.cit.nih.gov) was used for segmenting the WMH on FLAIR images. This was done by manually selecting WMH, and the segmentation algorithm would then segment the whole lesion. With a ‘fuzzy threshold’ of 0.8 this worked satisfactorily in most cases, but 25% of the cases required manual adjustment of the segmentation mask.
Statistical Analyses
The distributions of lateral ventricle and WMH volumes were skewed and therefore log transformed.
Analysis of covariance was used to see if sex- and age-adjusted volumes of cerebral structures were significantly different in SMC and MCI compared to controls. Receiver operating characteristic analysis was applied to test the validity of volumetric MR measurements.
Multivariate linear regression was used to test associations between volumes of cerebral structures and genetic risk factors, tHcy and cardiovascular risk factors. Associations were estimated in two models: adjusted for age and gender and in multivariate analysis.
In age-adjusted analysis, there was a borderline significant interaction (p = 0.070) be tween sex and probable parental LOAD for hippocampal volume. We therefore carried out additional analyses stratified by gender and probable parental LOAD.
All p values were two-tailed and considered significant when p < 0.05. SPSS version 22 was used to analyze the data.
Results
Participant characteristics are presented in table 1. Subjects with MCI were significantly older than controls and subjects with SMC, and had significantly higher tHcy than controls. The controls had a significantly longer education than subjects with SMC and MCI.
Table 1.
Characteristics of the participants
| Controls (n = 58) | SMC (n = 25) | MCI (n = 115) | |
|---|---|---|---|
| Age, years | 70.6 (6.7) | 70.0 (9.1) | 74.5 (7.5)* |
| Females, n (%) | 22 (38) | 11 (44) | 60 (52) |
| Education, years | 11.5 (8.0–14.0) | 7.0 (7.0–9.0)** | 7.0 (7.0–10.0)** |
| APOE ɛ4a, n (%) | 24 (41) | 13 (52) | 39 (34) |
| Females, n (%) | 10 (46) | 6 (55) | 21 (35) |
| Males, n (%) | 14 (39) | 7 (50) | 18 (33) |
| Probable parental LOAD, n (%) | 16 (28) | 9 (36) | 17 (15) |
| Females, n (%) | 5 (23) | 3 (27) | 10 (17) |
| Males, n (%) | 11 (31) | 6 (43) | 7 (13) |
| Probable LOAD in FD relative(s), n (%) | 20 (34) | 9 (36) | 29 (25) |
| Females, n (%) | 7 (32) | 3 (27) | 16 (27) |
| Males, n (%) | 13 (36) | 6 (43) | 13 (24) |
| Cobalamin, pm | 409.8 (160.3) | 365.0 (111.1) | 373.9 (159.7) |
| Folic acid, nmol | 17.0 (13.5–22.0) | 15.0 (12.5–18.0) | 16.0 (13.0–21.0) |
| tHcy, μmol | 14.7 (4.4) | 16.1 (5.1) | 18.3 (5.6)** |
| Risk factors for CVD | |||
| Smoking (ever), % | 72.4 | 80 | 68.7 |
| BMI | 27.4 (4.1) | 28.2 (5.4) | 26.7 (4.4) |
| Hypertension (ever), % | 32.8 | 40.0 | 33.0 |
| Systolic BPb, mm Hg | 144.9 (19.0) | 133.9 (24.6) | 144.8 (20.2) |
| BP medication (ever), % | 37.5 | 40.0 | 36.3 |
| Coronary disease (ever), % | 20.7 | 20.0 | 16.5 |
| Total cholesterol, mmol | 5.6 (1.2) | 5.5 (1.1) | 5.6 (1.2) |
| Lipid-lowering medication (ever), % | 35.1 | 44.0 | 32.4 |
| Diabetes (ever), % | 5.2 | 12.0 | 6.1 |
| HbA1c, % | 5.7 (5.5–5.9) | 5.8 (5.4–5.9) | 5.8 (5.5–6.1) |
| eGFR, ml/min/1.73 m2 | 83.3 (12.9) | 86.2 (14.2) | 82.4 (14.5) |
Values are expressed as means (standard deviations) for continuous normally distributed variables, and as medians (interquartile ranges) for continuous skewed variables unless indicated otherwise. FD = First degree; CVD = cardiovascular disease; BMI = body mass index; BP = blood pressure; ever = previous and/or current.
p < 0.05 (2-tailed) compared with controls and SMC.
p < 0.05 (2-tailed) compared with controls. Independent samples t test for continuous normally distributed variables and Mann-Whitney test for continuous skewed variables.
Presence of one or both APOE ɛ4 alleles.
Mean of the last two of three resting BP.
Table 2 shows the unadjusted differences between cases and controls on cognitive tests and MR volumetry, together with receiver operating characteristic curve analysis for the measured ICV. Apart from BMD cognition and BMD behavior, the cognitive test scores of subjects with SMC and MCI were significantly different from those of controls. The Montgomery-Åsberg Depression Rating Scale showed that none were more than mildly depressed. Hippocampal volume was significantly smaller in subjects with SMC and MCI compared to controls. In subjects with MCI, the volumes of the amygdala, lateral ventricles, cerebral cortex, cerebrum as well as WMH were significantly different from those of controls. The area under the curve in SMC and MCI compared to controls was less than 0.68 for all measured volumes of intracranial structures.
Table 2.
Results (unadjusted) of cognitive tests and MRI
| Controls (n = 58) | SMC (n = 25) | AUC (95% CI) SMC/controls | MCI (n = 115) | AUC (95% CI) MCI/controls | |
|---|---|---|---|---|---|
| MMSE | 29.0 (28.0–30.0) | 27.0 (27.0–29.0)a | 27.0 (26.0–28.0)b | ||
| Word test part 1 | 7.8 (1.6) | 6.9 (1.3)b | 5.4 (1.7)d | ||
| Word test part 2 | 22.0 (20.0–24.0) | 20.0 (16.0–22.0)b | 20.0 (16.0–22.0)a | ||
| DST | 39.6 (10.6) | 29.8 (11.1)ae | 25.7 (9.0)b | ||
| Trail A | 36.9 (11.4) | 48.6 (16.9)ce | 57.1 (23.2)b | ||
| Trail B | 92.4 (36.0) | 141.8 (61.2)a | 162.8 (64.2)b | ||
| Finger-tapping test | 51.6 (8.2) | 47.2 (8.7)b | 40.5 (11.7)d | ||
| IQCODE | 3.0 (3.0–3.0) | 3.2 (3.1–3.3)b | 3.1 (3.0–3.3)b | ||
| Clock-drawing test | 7.0 (6.8–7.0) | 6.0 (6.0–7.0)b | 6.0 (5.8–7.0)a | ||
| RDRS2 | 21.0 (21.0–22.0) | 23.5 (22.0–25.0)b | 23.0 (22.0–25.0)b | ||
| MADRS | 1.0 (1.0–2.0) | 3.0 (1.0–5.5)a | 2.0 (1.0–5.0)b | ||
| BMD cognitiong | 49.0 (47.0–52.0) | 50.0 (44.5–51.0) | 48.0 (44.0–52.0)b | ||
| BMD behaviorg | 2.0 (0.00–5.00) | 6.0 (2.5–10.0)ad | 3.0 (0.00–8.00) | ||
| Hippocampush | 0.50 (0.04) | 0.48 (0.06)b | 0.67 (0.52–0.81) | 0.48 (0.05)b | 0.60 (0.52–0.69) |
| Amygdalah | 0.22 (0.02) | 0.21 (0.02) | 0.53 (0.40–0.66) | 0.20 (0.03)b | 0.65 (0.56–0.73) |
| Lateral ventricleh | 2.00 (1.53–3.18) | 2.46 (1.87–3.18) | 0.61 (0.48–0.74) | 2.51 (2.03–3.84)b | 0.66 (0.57–0.75) |
| Cerebral cortexh | 30.88 (1.65) | 30.49 (1.86) | 0.53 (0.39–0.67) | 30.24 (1.80)b | 0.59 (0.51–0.68) |
| Cerebral white matterh | 27.96 (2.34) | 27.81 (2.54) | 0.52 (0.38–0.65) | 27.26 (2.33)f | 0.59 (0.50–0.68) |
| Cerebrumh | 72.55 (2.89) | 71.78 (3.20) | 0.57 (0.44–0.71) | 70.98 (3.36)b | 0.64 (0.56–0.73) |
| WMHh | 0.002 (0.001–0.007) | 0.005 (0.001–0.015) | 0.59 (0.44–0.73) | 0.006 (0.002–0.016)b | 0.66 (0.57–0.74) |
Values are expressed as means (standard deviations) for continuous normally distributed variables and medians (interquartile ranges) for continuous skewed variables. Independent samples t test for continuous normally distributed variables and Mann-Whitney test for continuous skewed variables. AUC = Area under the curve (component of receiver operating characteristic curve); DST = digit symbol-coding test; WMH = white matter hyperintensities.
p < 0.001 compared to controls.
p < 0.00001 compared to controls.
p < 0.05 (2-tailed) compared with controls.
p < 0.05 (2-tailed) compared with controls and SMC.
p < 0.05 (1-tailed) compared with MCI.
p < 0.05 (1-tailed) compared with controls.
Greene et al.'s Behavior and Mood Disturbance scale.
Total ICV-corrected volumes = (sum of bilateral volumes × 100) divided by ICV.
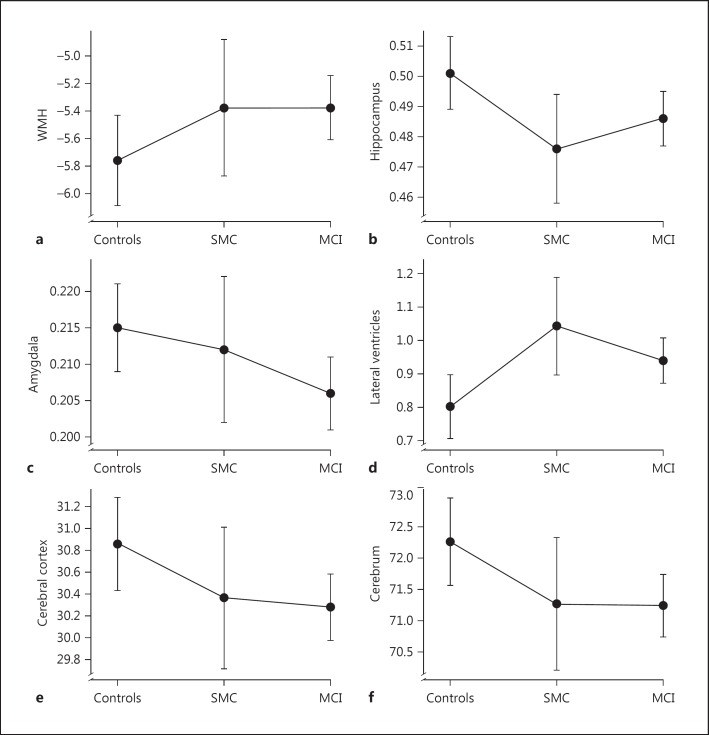
In age- and sex-adjusted analyses of covariance, the mean volume of the hippocampus was significantly smaller and the mean volume of the lateral ventricles was significantly larger in subjects with SMC and MCI compared to controls. In subjects with MCI, the mean volumes of the amygdala, cerebral cortex and cerebrum were significantly smaller than those in controls. The mean volume of WMH was larger in subjects with MCI than in controls (fig 1).
Fig. 1.
Mean age- and sex-adjusted ICV-corrected volumes of WMH (a), hippocampus (b), amygdala (c), lateral ventricles (d), cerebral cortex (e), and cerebrum (f) in the control, SMC and MCI groups. Lateral ventricles and WMH are log transformed. ICV-corrected volumes = (sum of bilateral volumes × 100) divided by total ICV. Error bars represent 95% confidence intervals.
Age- and sex-adjusted probable parental LOAD, ApoE ε4 and higher tHcy were associated with smaller hippocampal volume, as shown in table 3. In multivariate analysis, probable parental LOAD, ApoE ε4, higher estimated glomerular filtration rate (eGFR) and tHcy independently predicted a smaller hippocampus. In multivariate analyses, higher tHcy was associated with smaller hippocampal, amygdalar, cerebral cortical, and cerebral volumes, and larger lateral ventricles. Moreover, higher eGFR was associated with smaller hippocampal, cerebral cortical, and total cerebral volumes. Diabetes was associated with larger lateral ventricles. Adjusting for educational length did not alter the results.
Table 3.
Multivariate linear regression with volumes of cerebral structures as outcome variables.
| Adjusted for age and sex |
Multivariable analysis |
|||||||
|---|---|---|---|---|---|---|---|---|
| β | 95% CI | p | β | 95% CI | p | |||
| Hippocampus | ||||||||
| Age | −0.003 | −0.004 to–0.002 | <0.000001 | |||||
| Sexa | −0.021 | −0.035 to–0.007 | 0.003 | |||||
| Probable parental LOADb | −0.018 | −0.034 to–0.003 | 0.019 | −0.015 | −0.031 to 0.001 | 0.058 | ||
| ApoE ɛ4c | −0.021 | −0.033 to–0.008 | 0.001 | −0.016 | −0.029 to–0.003 | 0.015 | ||
| Smoking (ever) | 0.00004 | −0.150 to 0.150 | 1.00 | 0.002 | −0.012 to 0.016 | 0.83 | ||
| BMI | 0.002 | 0.000 to 0.003 | 0.036 | 0.001 | −0.001 to 0.002 | 0.27 | ||
| Hypertension (ever) | −0.005 | −0.018 to 0.008 | 0.46 | −0.003 | −0.017 to 0.011 | 0.69 | ||
| Systolic BP (mm Hg) | 0.0001 | 0.0002 to 0.0004 | 0.42 | 0.0002 | −0.0001 to 0.001 | 0.23 | ||
| Total cholesterol (mmol) | 0.006 | 0.000 to 0.011 | 0.049 | 0.007 | 0.001 to 0.013 | 0.015 | ||
| Diabetes (ever) | −0.0001 | −0.026 to 0.025 | 0.99 | −0.0003 | −0.033 to 0.033 | 0.99 | ||
| HbA1c (%) | 0.005 | −0.005 to 0.015 | 0.35 | 0.005 | −0.007 to 0.018 | 0.38 | ||
| eGFR (ml/min/1.73 m2) | −0.0004 | −0.001 to 0.0002 | 0.17 | −0.001 | −0.001 to–0.00002 | 0.045 | ||
| Cobalamin (pmol) | 0.00003 | −0.00001 to 0.00007 | 0.15 | 0.000006 | −0.00004 to 0.00005 | 0.78 | ||
| Folic acid (nmol) | 0.0004 | −0.0005 to 0.001 | 0.41 | −0.0004 | −0.001 to 0.001 | 0.39 | ||
| tHcy (μmol) | −0.002 | −0.003 to–0.004 | 0.010 | −0.002 | −0.004 to–0.001 | 0.004 | ||
| Amygdala* | ||||||||
| BMI | 0.001 | 0.0004 to 0.002 | 0.003 | 0.001 | 0.0003 to 0.002 | 0.008 | ||
| Total cholesterol (mmol) | 0.002 | −0.001 to 0.005 | 0.22 | 0.004 | 0.0004 to 0.007 | 0.029 | ||
| tHcy (μmol) | −0.001 | −0.001 to 0.0001 | 0.10 | −0.001 | −0.002 to–0.0001 | 0.028 | ||
| Cerebral cortex* | ||||||||
| eGFR (ml/min/1.73 m2) | −0.015 | −0.036 to 0.006 | 0.16 | −0.028 | −0.050 to–0.005 | 0.016 | ||
| Folic acid (nmol) | −0.021 | −0.052 to 0.010 | 0.19 | −0.047 | −0.084 to–0.010 | 0.013 | ||
| tHcy (µmol) | −0.022 | −0.067 to 0.023 | 0.34 | −0.080 | −0.137 to–0.024 | 0.006 | ||
| Cerebrum* | ||||||||
| Total cholesterol (mmol) | 0.004 | 0.00009 to 0.007 | 0.045 | 0.004 | 0.001 to 0.008 | 0.023 | ||
| eGFR (ml/min/1.73 m2) | −0.0001 | −0.0005 to 0.0002 | 0.46 | −0.0004 | −0.001 to–0.00004 | 0.030 | ||
| Folic acid (nmol) | −0.0003 | −0.001 to–0.0002 | 0.21 | −0.001 | −0.001 to–0.0002 | 0.013 | ||
| tHcy (μmol) | −0.0005 | −0.001 to 0.0003 | 0.19 | −0.001 | −0.002 to–0.0004 | 0.006 | ||
| LnLateral ventricle* | ||||||||
| Total cholesterol (mmol) | −0.024 | −0.044 to–0.003 | 0.25 | −0.030 | −0.052 to–0.008 | 0.007 | ||
| Diabetes (ever) | 0.093 | 0.001 to 0.184 | 0.047 | 0.135 | 0.012 to 0.257 | 0.031 | ||
| tHcy (μmol) | 0.005 | 0.0001 to 0.009 | 0.044 | 0.005 | −0.0002 to 0.011 | 0.061 | ||
Adjusted for age and sex and in multivariable analysis. With cerebral white matter and cerebral WMH as outcome variables, there were no significant/borderline significant associations. All cerebral volumes are bilateral. BMI = Body mass index; BP = mean of the last two of three resting blood pressures; Ln = natural logarithm; WMH = white matter hyperintensities. Bold font = Significant/borderline significant.
Only variables which were significant/borderline significant in multivariate analysis are displayed.
Female = 0 and male = 1.
No parental LOAD = 0 and probable parental LOAD = 1.
No ApoE ɛ4 alleles = 0 and presence of one or both ApoE ɛ4 alleles = 1.
With hippocampal volume as outcome variable in multivariate regression adjusted for age and sex, there was a borderline significant (p = 0.070) interaction between gender and probable parental LOAD. In our previous paper on the Tromsø Dementia Study in which there were 103 cases with MCI and 58 controls, this interaction was significant (p = 0.027). We therefore stratified by gender and probable parental LOAD, using the variables ApoE ε4, tHcy, cobalamin, eGFR, folic acid and age since these were the most relevant variables in table 3. Removing folic acid or adding total cholesterol to the analyses did not significantly alter the results.
In women, probable parental LOAD, presence of one or both ApoE ε4 alleles, higher eGFR and tHcy were independently associated with smaller hippocampal volume (table 4). In subjects with no parental LOAD, the presence of one or both ApoE ε4 alleles and higher tHcy were associated with smaller hippocampal volume. In subjects with probable parental LOAD, higher tHcy was associated with smaller hippocampal volume (p = 0.016). For higher eGFR, there was a borderline association with smaller hippocampal volume (p = 0.06).
Table 4.
Multivariate-adjusteda linear regression analysis with hippocampal volume as outcome variable, stratified by sex and probable parental LOAD
| Female (n = 93) |
Male (n = 105) |
||||||
|---|---|---|---|---|---|---|---|
| β | 95% CI | p | β | 95% CI | p | ||
| Age | −0.003 | −0.004 to–0.001 | 0.0002 | −0.003 | −0.004 to–0.001 | 0.0003 | |
| Probable parental LOADb | −0.032 | −0.054 to–0.010 | 0.005 | −0.005 | −0.028 to 0.017 | 0.64 | |
| ApoE ɛ4c | −0.021 | −0.038 to–0.003 | 0.024 | −0.012 | −0.031 to 0.007 | 0.22 | |
| eGFR (ml/min/1.73 m2) | −0.001 | −0.002 to–0.00002 | 0.044 | −0.0001 | −0.001 to 0.001 | 0.75 | |
| Cobalamin (pmol) | −0.000003 | −0.00006 to 0.00006 | 0.93 | 0.00001 | −0.00005 to 0.00007 | 0.78 | |
| Folic acid (nmol) | −0.001 | −0.002 to 0.001 | 0.28 | −0.001 | −0.002 to 0.001 | 0.47 | |
| tHcy (μmol) | −0.002 | −0.004 to–0.0003 | 0.021 | −0.002 | −0.004 to 0.001 | 0.15 | |
| No LOAD (n = 156) | Probable parental LOAD (n = 42) | ||||||
| β | 95% CI | p | β | 95% CI | p | ||
| Age | −0.003 | −0.004 to–0.002 | <0.000001 | −0.001 | −0.004 to 0.001 | 0.24 | |
| Sexd | −0.034 | −0.048 to–0.020 | <0.00001 | −0.008 | −0.036 to 0.020 | 0.55 | |
| ApoE ɛ4c | −0.019 | −0.033 to–0.004 | 0.012 | 0.002 | −0.026 to 0.030 | 0.89 | |
| eGFR (ml/min/1.73 m2) | −0.001 | −0.001 to 0.00001 | 0.06 | −0.0001 | −0.001 to 0.001 | 0.85 | |
| Cobalamin (pmol) | −0.00002 | −0.00008 to 0.00003 | 0.37 | 0.00006 | −0.00002 to 0.0001 | 0.14 | |
| Folic acid (nmol) | −0.0002 | −0.001 to 0.001 | 0.77 | −0.002 | −0.005 to–0.0001 | 0.039 | |
| tHcy (μmol) | −0.002 | −0.003 to–0.0001 | 0.035 | −0.005 | −0.009 to–0.001 | 0.016 | |
Bold font = Significant.
Adjusted for age, sex, probable parental LOAD, ApoE ɛ4, eGFR, cobalamin, folic acid, and tHcy.
No parental LOAD = 0 and probable parental LOAD = 1.
No ApoE ɛ4 alleles = 0 and presence of one or both ApoE ɛ4 alleles = 1.
Female = 0 and male = 1.
Discussion
In our study, fully automated MR volumetry distinguished subjects with SMC and MCI from controls. MR volumetry of the hippocampus and the lateral ventricles distinguished both subjects with SCM and MCI from controls, while MR volumetry of the amygdala, cerebral cortex and cerebrum distinguished subjects with MCI from controls. This might reflect that AD first affects the medial temporal lobe and thereafter the cerebral cortex and cerebral volume [10, 13]. Both hippocampus and amygdala atrophy occur early in AD, but in our study, the amygdala was significantly smaller only in subjects with MCI, possibly because it has less distinct boundaries and is harder to quantify than hippocampus [10]. The volume of WMH was larger in subjects with MCI than in controls and suggests that WMH might be a risk factor for AD [36].
Receiver operating curve analysis showed that MR volumetry did not distinguish well enough between controls and SMC/MCI. However, the challenge in clinical practice is often to assess whether a person with possible cognitive decline has a neurodegenerative disease. If the first examination is equivocal, fully automated MR volumetry can be repeated to assess whether the atrophy rate is abnormal [37]. This suggests that fully automated MR volumetry together with other biomarkers can be useful in diagnosing preclinical LOAD [9, 13, 38].
Probable parental LOAD, ApoE ε4 genotype, higher eGFR and tHcy were independently associated with smaller hippocampal volume. To our knowledge, this has not been shown earlier, and might imply that sporadic LOAD has several etiologies [39]. In women, but not in men, probable parental LOAD was strongly associated with smaller hippocampal volume, as were ApoE ε4 genotype, higher eGFR and tHcy. This is in line with earlier studies that suggest sex differences in the etiology and pathophysiology of sporadic LOAD [40, 41]. Apart from ApoE ε4 genotype, there are clearly additional genetic risk factors for sporadic LOAD, but these still remain obscure [42]. Our findings suggest a sex difference between men and women with probable parental LOAD in acquiring LOAD and underscore the need for sex-specific analyses in genetic studies of LOAD [21].
Although probable parental LOAD was associated with MR volumetry, we found no associations between the subjects having first-degree relatives with probable LOAD and findings on MR volumetry. This may reflect that even though the risk of acquiring AD is increased in subjects who have first-degree relatives with LOAD, it is especially high in those who have parents with LOAD [20].
Higher eGFR was associated with smaller hippocampal volume. Earlier trials have given equivocal results regarding the association between eGFR and cognitive impairment [43]. Our finding suggests that this should be studied further.
tHcy was associated with smaller volumes of the hippocampus, cerebral cortex, and cerebrum, as shown in earlier studies [19]. Also, tHcy was associated with smaller volumes of the amygdala and larger volumes of the lateral ventricles. Our study is cross-sectional, but our findings of strong associations between higher tHcy and cerebral structures affected by AD add weight to previous studies which showed that vitamin B treatment slowed the development of atrophy of gray matter regions affected by AD in elderly subjects with MCI and elevated tHcy [44, 45]. This suggests that homocysteine might be a risk factor for LOAD.
Higher total cholesterol was independently associated with larger volumes of the hippocampus, amygdala, and cerebrum and smaller volumes of the lateral ventricles. Genome-wide association studies have shown that the ApoE gene and some genetic risk loci for AD are associated with cholesterol and lipid processing, and other studies have shown that the impact of cholesterol might vary during the life span [46, 47, 48].
Higher folic acid was associated with smaller cerebral and cerebral cortical volumes in our study. It is known that folic acid deficiency might be a risk factor for AD [49]. Folic acid supplementation has been promoted in Norway during the last two decades, and some par ticipants may have used it.
ApoE ε4 genotype was present in 41, 52 and 34% of the controls, the subjects with SMC, and those with MCI, respectively. Approximately 40% of patients with AD have the ApoE ε4 genotype, as compared to approximately 15% in the general population [18]. The prevalence of the ApoE ε4 genotype in the Norwegian population is not well known. Studies suggest that 20% of control individuals and 60% of AD patients have the ApoE ε4 genotype [50]. The high prevalence of the ApoE ε4 genotype in our study suggests that subjects with LOAD in their families were more eager to participate, that ApoE ε4 is more prevalent in subjects with SMC and MCI, and that our subjects constituted a suitable sample.
Subjects with SMC scored significantly worse than controls on the informant-based questionnaires regarding cognitive function, anxiety, depression, and behavior. Earlier studies have shown that apart from cognitive decline, SMC also stems from anxiety and depression. Our findings are consistent with these studies [51].
The main limitations of our study are the cross-sectional design, rendering causative inferrals infeasible, and the small sample size, which increases the chance for spurious relationships and only enables detection of large effect sizes. Although atrophy of the hippocampus and other cerebral structures are widely used as surrogate endpoints for AD, other conditions also lead to atrophy [14].
Our results suggest that fully automated MR volumetry does not distinguish well enough between controls, subjects with SMC and subjects with MCI in a general population to assume a clear clinical role in assessing whether SMC and MCI are caused by AD. Our findings suggest that one might benefit from searching for genetic risk factors in men and women with probable parental LOAD, to find the cause of a probable sex difference in acquiring LOAD. tHcy, eGFR, and total cholesterol were associated with the volumes of cerebral structures central in the pathogenesis of AD, and further research is necessary to assess their roles in AD.
Disclosure Statement
Dr. Rogne, Torgil Vangberg and Dr. Wikran report no disclosures. Dr. Eldevik has received and receives research support from the Norwegian Research Council and the Northern Norway Health Authority. Dr. Mathiesen has received/receives research support from the Norwegian Research Council and the Northern Norway Health Authority. Dr. Schirmer has received/receives research support from the Norwegian Research Council, the Norwegian Council on Cardiovascular Diseases, the Odd Berg Research Foundation, and the Northern Norway Health Authority.
Acknowledgements
We are grateful for the invaluable contributions from research nurse Kristin Voie and IT consultant Inger Sperstad. The study received funding from the Northern Norway Regional Health Authority, Odd Berg Group Medical Research Fund, the National Association for Public Health, and the Norwegian Research Council.
References
- 1.Burns A, O'Brien J, Ames D, editors. Dementia. ed 4. London: Hodder Arnold; 2010. [Google Scholar]
- 2.Luck T, Luppa M, Matschinger H, Jessen F, Angermeyer MC, Riedel-Heller SG. Incident subjective memory complaints and the risk of subsequent dementia. Acta Psychiatr Scand. 2015;131:290–296. doi: 10.1111/acps.12328. [DOI] [PubMed] [Google Scholar]
- 3.Roberts JL, Clare L, Woods RT. Subjective memory complaints and awareness of memory functioning in mild cognitive impairment: a systematic review. Dement Geriatr Cogn Disord. 2009;28:95–109. doi: 10.1159/000234911. [DOI] [PubMed] [Google Scholar]
- 4.Bartley M, Bokde AL, Ewers M, Faluyi YO, Tobin WO, Snow A, Connolly J, Delaney C, Coughlan T, Collins DR, Hampel H, O'Neill D. Subjective memory complaints in community dwelling healthy older people: the influence of brain and psychopathology. Int J Geriatr Psychiatry. 2012;27:836–843. doi: 10.1002/gps.2794. [DOI] [PubMed] [Google Scholar]
- 5.Jonker C, Geerlings MI, Schmand B. Are memory complaints predictive for dementia? A review of clinical and population-based studies. Int J Geriatr Psychiatry. 2000;15:983–991. doi: 10.1002/1099-1166(200011)15:11<983::aid-gps238>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 6.Mitchell AJ. Is it time to separate subjective cognitive complaints from the diagnosis of mild cognitive impairment? Age Ageing. 2008;37:497–499. doi: 10.1093/ageing/afn147. [DOI] [PubMed] [Google Scholar]
- 7.Lezak MD, Howieson DB, Loring DW. Neuropsychological Assessment. ed 4. Oxford: Oxford University Press; 2004. [Google Scholar]
- 8.Gifford KA, Liu D, Lu Z, Tripodis Y, Cantwell NG, Palmisano J, Kowall N, Jefferson AL. The source of cognitive complaints predicts diagnostic conversion differentially among nondemented older adults. Alzheimers Dement. 2014;10:319–327. doi: 10.1016/j.jalz.2013.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fiandaca MS, Mapstone ME, Cheema AK, Federoff HJ. The critical need for defining preclinical biomarkers in Alzheimer's disease. Alzheimers Dement. 2014;10:S196–S212. doi: 10.1016/j.jalz.2014.04.015. [DOI] [PubMed] [Google Scholar]
- 10.Frisoni GB, Fox NC, Jack CR, Scheltens P, Thompson PM. The clinical use of structural MRI in Alzheimer disease. Nat Rev Neurol. 2010;6:67–77. doi: 10.1038/nrneurol.2009.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McEvoy LK, Brewer JB. Quantitative structural MRI for early detection of Alzheimer's disease. Expert Rev Neurother. 2010;10:1675–1688. doi: 10.1586/ern.10.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Desikan RS, Cabral HJ, Hess CP, Dillon WP, Glastonbury CM, Weiner MW, Schmansky NJ, Greve DN, Salat DH, Buckner RL, Fischl B. Automated MRI measures identify individuals with mild cognitive impairment and Alzheimer's disease. Brain. 2009;132:2048–2057. doi: 10.1093/brain/awp123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rathakrishnan BG, Doraiswamy PM, Petrella JR. Science to practice: translating automated brain MRI volumetry in Alzheimer's disease from research to routine diagnostic use in the workup of dementia. Front Neurol. 2014;4:216. doi: 10.3389/fneur.2013.00216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kantarci K, Jack CR. Quantitative magnetic resonance techniques as surrogate markers of Alzheimer's disease. NeuroRx. 2004;1:196–205. doi: 10.1602/neurorx.1.2.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Engedal K, Braekhus A, Andreassen OA, Nakstad PH. Diagnosis of dementia – automatic quantification of brain structures. Tidsskr Nor Laegeforen. 2012;132:1747–1751. doi: 10.4045/tidsskr.12.0148. [DOI] [PubMed] [Google Scholar]
- 16.Alagiakrishnan K, Gill SS, Fagarasanu A. Genetics and epigenetics of Alzheimer's disease. Postgrad Med J. 2012;88:522–529. doi: 10.1136/postgradmedj-2011-130363. [DOI] [PubMed] [Google Scholar]
- 17.Alonso Vilatela ME, Lopez-Lopez M, Yescas-Gomez P. Genetics of Alzheimer's disease. Arch Med Res. 2012;43:622–631. doi: 10.1016/j.arcmed.2012.10.017. [DOI] [PubMed] [Google Scholar]
- 18.Nussbaum R, McInnes R, Huntington FW. Thompson and Thompson Genetics in Medicine. ed 7. Philadelphia: Saunders; 2007. [Google Scholar]
- 19.Rogne S, Vangberg T, Eldevik P, Wikran G, Mathiesen EB, Schirmer H. Mild cognitive impairment, risk factors and magnetic resonance volumetry: role of probable Alzheimer's disease in the family. Dement Geriatr Cogn Disord. 2013;36:87–98. doi: 10.1159/000350408. [DOI] [PubMed] [Google Scholar]
- 20.Green RC, Cupples LA, Go R, Benke KS, Edeki T, Griffith PA, Williams M, Hipps Y, Graff-Radford N, Bachman D, Farrer LA, MIRAGE Study Group Risk of dementia among white and African American relatives of patients with Alzheimer disease. JAMA. 2002;287:329–336. doi: 10.1001/jama.287.3.329. [DOI] [PubMed] [Google Scholar]
- 21.Guerreiro R, Hardy J. Genetics of Alzheimer's disease. Neurotherapeutics. 2014;11:732–737. doi: 10.1007/s13311-014-0295-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Attems J, Jellinger KA. The overlap between vascular disease and Alzheimer's disease – lessons from pathology. BMC Med. 2014;12:206. doi: 10.1186/s12916-014-0206-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van Sloten TT, Protogerou AD, Henry RMA, Schram MT, Launer LJ, Stehouwer CDA. Association between ar<X00_Del_TrennDivis>- </X00_Del_TrennDivis>terial stiffness, cerebral small vessel disease and cognitive impairment: a systematic review and meta-analy<X00_Del_TrennDivis>- </X00_Del_TrennDivis>sis. Neurosci Biobehav Rev. 2015;53:121–130. doi: 10.1016/j.neubiorev.2015.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Snyder HM, Corriveau RA, Craft S, Faber JE, Greenberg SM, Knopman D, Lamb BT, Montine TJ, Nedergaard M, Schaffer CB, Schneider JA, Wellington C, Wilcock DM, Zipfel GJ, Zlokovic B, Bain LJ, Bosetti F, Galis ZS, Koroshetz W, Carrillo MC. Vascular contributions to cognitive impairment and dementia including Alzheimer's disease. Alzheimers Dement. 2015;11:710–717. doi: 10.1016/j.jalz.2014.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Daviglus ML, Plassman BL, Pirzada A, et al. Risk factors and preventive interventions for Alzheimer disease: state of the science. Arch Neurol. 2011;68:1185–1190. doi: 10.1001/archneurol.2011.100. [DOI] [PubMed] [Google Scholar]
- 26.Zhuo J-M, Wang H, Praticò D. Is hyperhomocysteinemia an Alzheimer's disease (AD) risk factor, an ad marker, or neither? Trends Pharmacol Sci. 2011;32:562–571. doi: 10.1016/j.tips.2011.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.de Bruijn RF, Ikram MA. Cardiovascular risk factors and future risk of Alzheimer's disease. BMC Med. 2014;12:130. doi: 10.1186/s12916-014-0130-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jacobsen BK, Eggen AE, Mathiesen EB, Wilsgaard T, Njølstad I. Cohort profile: the Tromsø Study. Int J Epidemiol. 2012;41:961–967. doi: 10.1093/ije/dyr049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bäckman L, Forsell Y. Episodic memory functioning in a community-based sample of old adults with major depression: utilization of cognitive support. J Abnorm Psychol. 1994;103:361–370. doi: 10.1037//0021-843x.103.2.361. [DOI] [PubMed] [Google Scholar]
- 30.Folstein MF, Folstein SE, McHugh PR. ‘Mini-mental state’: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 31.Arntzen KA, Schirmer H, Wilsgaard T, Mathiesen EB. Impact of cardiovascular risk factors on cognitive function: the Tromsø Study. Eur J Neurol. 2011;18:737–743. doi: 10.1111/j.1468-1331.2010.03263.x. [DOI] [PubMed] [Google Scholar]
- 32.Petersen RC, Roberts RO, Knopman DS, et al. Mild cognitive impairment: ten years later. Arch Neurol. 2009;66:1447–1455. doi: 10.1001/archneurol.2009.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Greene JG, Smith R, Gardiner M, Timbury GC. Measuring behavioural disturbance of elderly demented patients in the community and its effects on relatives: a factor analytic study. Age Ageing. 1982;11:121–126. doi: 10.1093/ageing/11.2.121. [DOI] [PubMed] [Google Scholar]
- 34.Brewer JB, Magda S, Airriess C, Smith ME. Fully-automated quantification of regional brain volumes for improved detection of focal atrophy in Alzheimer disease. AJNR Am J Neuroradiol. 2009;30:578–580. doi: 10.3174/ajnr.A1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kovacevic S, Rafii MS, Brewer JB. High-throughput, fully automated volumetry for prediction of MMSE and CDR decline in mild cognitive impairment. Alzheimer Dis Assoc Disord. 2009;23:139–145. doi: 10.1097/WAD.0b013e318192e745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brickman A. Contemplating Alzheimer's disease and the contribution of white matter hyperintensities. Curr Neurol Neurosci Rep. 2013;13:1–9. doi: 10.1007/s11910-013-0415-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Petrella JR. Neuroimaging and the search for a cure for Alzheimer disease. Radiology. 2013;269:671–691. doi: 10.1148/radiol.13122503. [DOI] [PubMed] [Google Scholar]
- 38.England HB, Gillis MM, Hampstead BM. RBANS memory indices are related to medial temporal lobe volumetrics in healthy older adults and those with mild cognitive impairment. Arch Clin Neuropsychol. 2014;29:322–328. doi: 10.1093/arclin/acu012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Korczyn AD. Why have we failed to cure Alzheimer's disease? J Alzheimers Dis. 2012;29:275–282. doi: 10.3233/JAD-2011-110359. [DOI] [PubMed] [Google Scholar]
- 40.Gao S, Hendrie HC, Hall KS, Hui S. The relationships between age, sex, and the incidence of dementia and Alzheimer disease: a meta-analysis. Arch Gen Psychiatry. 1998;55:809–815. doi: 10.1001/archpsyc.55.9.809. [DOI] [PubMed] [Google Scholar]
- 41.Mielke MM, Vemuri P, Rocca WA. Clinical epidemiology of Alzheimer's disease: assessing sex and gender differences. Clin Epidemiol. 2014;6:37–48. doi: 10.2147/CLEP.S37929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bettens K, Sleegers K, Van Broeckhoven C. Genetic insights in Alzheimer's disease. Lancet Neurol. 2013;12:92–104. doi: 10.1016/S1474-4422(12)70259-4. [DOI] [PubMed] [Google Scholar]
- 43.Rogne SO, Solbu MD, Arntzen KA, Herder M, Mathiesen EB, Schirmer H. Albuminuria and carotid atherosclerosis as predictors of cognitive function in a general population. Eur Neurol. 2013;70:340–348. doi: 10.1159/000353701. [DOI] [PubMed] [Google Scholar]
- 44.Smith AD, Smith SM, de Jager CA, Whitbread P, Johnston C, Agacinski G, Oulhaj A, Bradley KM, Jacoby R, Refsum H. Homocysteine-lowering by B vitamins slows the rate of accelerated brain atrophy in mild cognitive im pairment: a randomized controlled trial. PLoS One. 2010;5:e12244. doi: 10.1371/journal.pone.0012244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Douaud G, Refsum H, de Jager CA, Jacoby R, Nichols TE, Smith SM, Smith AD. Preventing Alzheimer's disease-related gray matter atrophy by B-vitamin treatment. Proc Natl Acad Sci USA. 2013;110:9523–9528. doi: 10.1073/pnas.1301816110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lim WLF, Martins IJ, Martins RN. The involvement of lipids in Alzheimer's disease. J Genet Genomics. 2014;41:261–274. doi: 10.1016/j.jgg.2014.04.003. [DOI] [PubMed] [Google Scholar]
- 47.Solomon A, Kivipelto M, Wolozin B, Zhou J, Whitmer RA. Midlife serum cholesterol and increased risk of Alzheimer's and vascular dementia three decades later. Dement Geriatr Cogn Disord. 2009;28:75–80. doi: 10.1159/000231980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Raskin J, Cummings J, Hardy J, Schuh K, Dean RA. Neurobiology of Alzheimer's disease: integrated molecular, physiological, anatomical, biomarker, and cognitive dimensions. Curr Alzheimer Res. 2015;12:712–722. doi: 10.2174/1567205012666150701103107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hinterberger M, Fischer P. Folate and Alzheimer: when time matters. J Neural Transm. 2013;120:211–224. doi: 10.1007/s00702-012-0822-y. [DOI] [PubMed] [Google Scholar]
- 50.Sando SB, Melquist S, Cannon A, Hutton ML, Sletvold O, Saltvedt I, White LR, Lydersen S, Aasly JO. Apoe ε4 lowers age at onset and is a high risk factor for Alzheimer's disease; a case control study from central Norway. BMC Neurol. 2008;8:1–7. doi: 10.1186/1471-2377-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Reid LM, MacLullich AMJ. Subjective memory complaints and cognitive impairment in older people. Dement Geriatr Cogn Disord. 2006;22:471–485. doi: 10.1159/000096295. [DOI] [PubMed] [Google Scholar]