Abstract
Platelets and circulating CD34-positive cells have been reported to contribute to vascular repair (endothelial repair and developing atherosclerosis). And because hypertension is known to be a strong vascular impairment factors, it should also influence the respective numbers of these factors. To clarify the clinical importance of platelets on vascular repair, we conducted a cross-sectional study of 567 Japanese men aged 60-69 who underwent an annual health check-up between 2013 and 2015. Multiple linear regression analysis of non-hypertensive subjects adjusting for classical cardiovascular risk factors showed that although platelet count did not significantly correlate with carotid intima media thickness (β = −0.05, p = 0.356), it did positively correlate significantly with the natural log of the number of circulating CD34-positive cells (β = 0.26, p < 0.001). In hypertensive subjects, a significant positive correlation was seen between platelets and intima media thickness (β = 0.19, p = 0.008), whereas no significant correlation was seen between platelet count and the natural log of the number of circulating CD34-positive cells (β = 0.11, p = 0.119). Our results indicate that platelet count is an indicator of vascular repair activity (endothelial repair and developing atherosclerosis). Additionally, hypertension might mask the beneficial effects of circulating CD34-positive cells.
Keywords: platelets, vascular repair, atherosclerosis, hypertension, CD34-positive cell, elderly men, Gerotarget
INTRODUCTION
Recent experimental studies have revealed a correlation between platelets and circulating CD34-positive cells. These studies indicated that platelets promoted the mobilization of bone marrow-derived CD34-positive cells into the peripheral blood [1–8]. Furthermore, platelets are reported to induce differentiation of human CD34-positive cells into endothelial cells [9]. Since CD34-positive cells have been reported to contribute to endothelial repair [10], and platelet rich plasma could enhance the proliferation of bone marrow multi-potent stem cells [6], high levels of platelets in the plasma might have a beneficial effect on endothelial repair. However, platelets are also reported to play an important role in the development of atherosclerotic lesions as an initial actor [11]. A previous study reported that platelets induced the differentiation of human CD34-positive cells into foam cells [9], which are a well-known contributing factor in the development of atherosclerotic lesions. Therefore, high plasma platelet counts may also play a crucial role in the development of atherosclerosis.
On the other hand, hypertension is well-known as a strong endothelial impairment factor [12]. In our previous study, we reported that hypertension masks the beneficial effect of circulating CD34-positive cells as an endothelial repair factor [13]. Therefore, the presence of hypertension might act as a confounding factor in the correlation between platelet count and the number of circulating CD34-positive cells.
To investigate the correlation between platelets and circulating CD34-positive cells as a marker of vascular repair (endothelial repair and atherosclerosis development), we conducted a cross-sectional study of 567 men aged 60-69 who underwent an annual health check-up between 2013 and 2015.
RESULTS
Characteristics of the study population
Among 567 elderly men, 238 were diagnosed as hypertensive. Characteristics of the study population by hypertension status are shown in Table 1. In addition to systolic and diastolic blood pressure, hypertensive subjects showed significantly higher BMI and CIMT than non-hypertensive subjects.
Table 1. Characteristics of the study population based on hypertension status.
| Non-hypertension | Hypertension | p value | |
|---|---|---|---|
| No. of participants | 329 | 238 | |
| Age, years | 65.4 ± 2.5 | 65.6 ± 2.7 | |
| Systolic blood pressure, mmHg | 122 ± 10 | 150 ± 12 | <0.001 |
| Diastolic blood pressure, mmHg | 74 ± 8 | 90 ± 9 | <0.001 |
| Body mass index (BMI), kg/m2 | 23.0 ± 2.9 | 23.9 ± 2.9 | <0.001 |
| Serum HDL-cholesterol (HDL), mg/dL | 57 ± 14 | 57 ± 15 | 0.581 |
| Serum triglycerides (TG), mg/dL | 116 ± 80 | 121 ± 101 | 0.486 |
| Hemoglobin A1c (HbA1c), % | 5.7 ± 0.6 | 5.7 ± 0.7 | 0.596 |
| Serum aspartate aminotransferase (AST), IU/L | 24 ± 9 | 26 ± 9 | 0.083 |
| Serum γ-glutamyltranspeptidase (γ-GTP), IU/L | 48 ± 67 | 52 ± 54 | 0.446 |
| Serum uric acid (UA), mg/dL | 5.9 ± 1.2 | 5.9 ± 1.2 | 0.574 |
| Serum creatinine, mg/dL | 0.88 ± 0.60 | 0.84 ± 0.15 | 0.327 |
| Glomerular filtration rate (GFR), mL/min/1.73m2 | 73.0 ± 15.3 | 73.2 ± 13.7 | 0.877 |
| Mean carotid intima-media thickness (CIMT), mm2 | 0.67 ± 0.10 | 0.70 ± 0.12 | 0.005 |
| Circulating CD34-positive cells, cells/μL | 1.29 ± 1.19 | 1.36 ± 1.54 | 0.516 |
| White blood cells (WBC), cells/μL | 5538 ± 1388 | 5655 ± 1432 | 0.328 |
| Platelets (Plt), ×104/μL | 21.7 ± 5.2 | 22.3 ± 5.1 | 0.204 |
values: mean ± standard deviation. p values are age-adjusted value.
Platelets and other variables in relation to hypertension
From simple correlation analysis (simple correlation coefficient), for subjects without hypertension, platelets showed a significant positive correlation with circulating CD34-positive cells and an inverse correlation with AST, but not with CIMT; and for subjects with hypertension, platelets showed a significant positive correlation with CIMT (Table 2).
Table 2. Simple correlation coefficient of platelets and other variables.
| Platelets | ||||
|---|---|---|---|---|
| Non-hypertension | Hypertension | |||
| r | p | r | p | |
| No. of participants | 329 | 238 | ||
| Age | −0.11 | 0.053 | −0.08 | 0.237 |
| Systolic blood pressure | 0.001 | 0.982 | 0.03 | 0.685 |
| Diastolic blood pressure | −0.03 | 0.549 | 0.003 | 0.959 |
| Body mass index (BMI) | −0.04 | 0.526 | −0.06 | 0.331 |
| Serum HDL-cholesterol (HDL) | −0.02 | 0.673 | −0.05 | 0.412 |
| Serum triglycerides (TG) | 0.05 | 0.392 | 0.07 | 0.251 |
| Hemoglobin A1c (HbA1c) | 0.002 | 0.978 | 0.09 | 0.148 |
| Serum aspartate aminotransferase (AST) | −0.22 | <0.001 | −0.13 | 0.054 |
| Serum γ-glutamyltranspeptidase (γ-GTP) | −0.003 | 0.961 | −0.11 | 0.100 |
| Serum uric acid (UA) | 0.04 | 0.460 | −0.06 | 0.326 |
| Glomerular filtration rate (GFR) | 0.09 | 0.086 | 0.07 | 0.313 |
| Circulating CD34-positive cells | 0.25 | <0.001 | 0.12 | 0.075 |
| Mean carotid intima-media thickness (CIMT) | −0.05 | 0.388 | 0.17 | 0.010 |
r: Correlation coefficient. Circulating CD34-positive cells, TG, and γ-GTP are calculated in logarithm values.
Platelets and circulating CD34-positive cells, mean CIMT in relation to hypertension
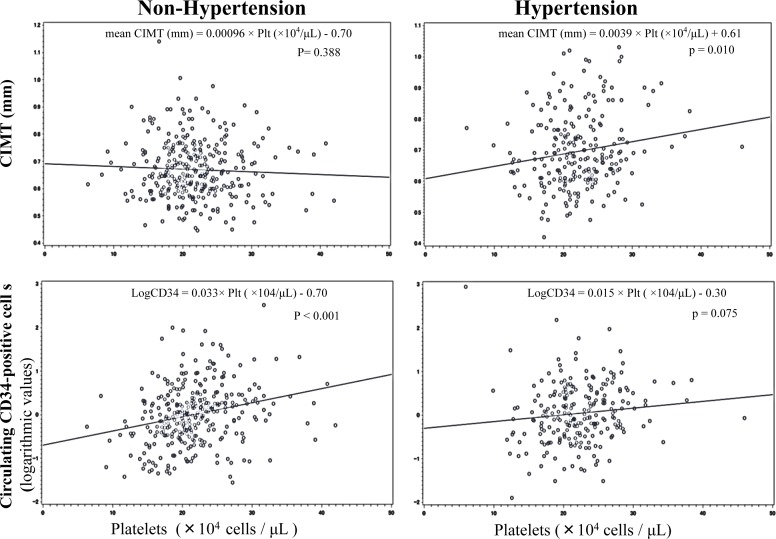
From simple linear regression analysis, for subjects without hypertension, platelets showed a significant positive correlation with circulating CD34-positive cells, whereas for subjects with hypertension, no significant correlation was observed. We also found that even though there was no significant correlation between platelets and CIMT in non-hypertensive subjects, a significant positive correlation was seen in hypertension men (Figure 1).
Figure 1. Simple linear regression analyses of platelets and mean CIMT, and circulating CD34-positive cells.
These correlations remained unchanged even after further adjustment for known cardiovascular risk factors (Tables 3, 4).
Table 3. Multiple linear regression analysis of mean CIMT with relevant factors adjusted for confounding factors.
| mean carotid intima-media thickness (CIMT) | ||||||
|---|---|---|---|---|---|---|
| Non-Hypertension | Hypertension | |||||
| β | 95%CI | p | β | 95%CI | p | |
| No. of participants | 329 | 238 | ||||
| Age | 0.14 | (0.03, 0,25) | 0.010 | 0.20 | (0.06, 0.33) | 0.004 |
| Systolic blood pressure | 0.29 | (0.05, 0.52) | 0.017 | 0.10 | (−0.11, 0.32) | 0.347 |
| Diastolic blood pressure | −0.10 | (−0.30, 0.10) | 0.337 | −0.09 | (−0.27, 0.09) | 0.317 |
| Body mass index (BMI) | −0.01 | (−0.13, 0.10) | 0.819 | 0.03 | (−0.12, 0.18) | 0.688 |
| Serum HDL-cholesterol (HDL) | −0.14 | (−0.26, −0.01) | 0.032 | −0.02 | (−0.18, 0.13) | 0.752 |
| Serum triglycerides (TG) | −0.15 | (−0.28, −0.02) | 0.022 | 0.01 | (−0.15, 0.17) | 0.927 |
| Hemoglobin A1c (HbA1c) | 0.05 | (−0.06, 0.17) | 0.346 | 0.03 | (−0.10, 0.16) | 0.606 |
| Serum aspartate aminotransferase (AST) | −0.07 | (−0.19, 0.04) | 0.217 | 0.07 | (−0.09, 0.22) | 0.389 |
| Serum γ-glutamyltranspeptidase (γ-GTP) | 0.09 | (−0.03, 0.22) | 0.151 | −0.10 | (−0.27, 0.07) | 0.267 |
| Serum uric acid (UA) | 0.07 | (−0.04, 0.17) | 0.230 | −0.09 | (−0.13, 0.06) | 0.232 |
| Glomerular Filtration Rate (GFR) | 0.01 | (−0.09, 0.11) | 0.839 | −0.07 | (−0.23, 0.08) | 0.352 |
| Platelets (Plt) | −0.05 | (−0.15, 0.05) | 0.356 | 0.19 | (0.05, 0.33) | 0.008 |
β: Standardized parameter estimate. TG and γ-GTP are calculated in logarithm values.
Table 4. Multiple Linear Regression Analysis of Circulating CD34-positive cells with Relevant Factors adjusted for Confounding Factors.
| Circulating CD34-positive cells | ||||||
|---|---|---|---|---|---|---|
| Non-hypertension | Hypertension | |||||
| β | 95%CI | p | β | 95%CI | P | |
| No. of participants | 329 | 238 | ||||
| Age | −0.08 | (−0.19, 0.02) | 0.129 | −0.03 | (−0.16, 0.10) | 0.620 |
| Systolic blood pressure | −0.02 | (−0.26, 0.21) | 0.857 | −0.02 | (−0.22, 0.19) | 0.872 |
| Diastolic blood pressure | 0.06 | (−0.14, 0.26) | 0.567 | −0.01 | (−0.19, −0.16) | 0.867 |
| Body mass index (BMI) | 0.20 | (0.08, 0.31) | 0.001 | 0.16 | (0.02, 0.30) | 0.025 |
| Serum HDL-cholesterol (HDL) | −0.04 | (−0.16, 0.09) | 0.563 | 0.02 | (−0.13, 0.17) | 0.817 |
| Serum triglycerides (TG) | 0.19 | (0.06, 0.32) | 0.004 | 0.01 | (−0.15, 0.16) | 0.933 |
| Hemoglobin A1c (HbA1c) | 0.05 | (−0.06, 0.16) | 0.389 | 0.02 | (−0.10, 0.15) | 0.733 |
| Serum aspartate aminotransferase (AST) | 0.06 | (−0.06, 0.18) | 0.342 | −0.15 | (−0.19, −0.00002) | 0.050 |
| Serum γ-glutamyltranspeptidase (γ-GTP) | −0.02 | (−0.14, 0.11) | 0.800 | −0.06 | (−022, 0.11) | 0.509 |
| Serum uric acid (UA) | −0.01 | (−0.12, 0.09) | 0.802 | 0.07 | (−0.06, 0.21) | 0.291 |
| Glomerular Filtration Rate (GFR) | −0.06 | (−0.16, 0.04) | 0.271 | −0.02 | (−0.17, 012) | 0.741 |
| Platelets (Plt) | 0.26 | (0.15, 0.36) | <0.001 | 0.11 | (−0.03, 0.24) | 0.119 |
β: Standardized parameter estimate. Circulating CD34-positive cells, TG, and γ-GTP are calculated in logarithm values.
DISCUSSION
The main findings of present study showed platelet count to be significantly positively correlated with circulating CD34-postive cells, but not with CIMT in non-hypertensive men, and not significantly correlated with circulating CD34-positive cells, but significantly positively correlated with CIMT in hypertensive men. These results demonstrate that platelet count is an indicator of vascular repair activity, and that hypertension might mask the beneficial effects of circulating CD34-positive cells.
This is the first epidemiological study clarifying the correlation between platelet count and the number of circulating CD34-positive cells and CIMT. It is also the first study to clarify the influence of hypertension on these correlations. Even though platelet count indicates endothelial repair activity, a high platelet count contributes to high CIMT in hypertensive men. These findings might indicate an efficient tool to clarify the mechanism of vascular repair in elderly men.
Platelets play an important role in vascular inflammation and vessel wall remodeling [14,15]. Injury to the arterial endothelial cells causes exposure of sub-endothelial components, notably collagen [16,17] and von Willebrand factor [18], resulting in the adherence of platelets to damaged vessel walls and their subsequent activation. Activated platelets (P-selectin-positive platelets) express or release stromal cell-derived factor 1α (SDF-1α) [1], leading to mobilization of bone marrow-derived CD34-positive cells into the peripheral blood in human acute coronary syndrome [2]. Furthermore, platelets secrete vascular endothelial growth factor (VEGF) and sphingosine-1-phosphate (S1P) [3] upon their activation. A previous study also reported that myocardial necrosis with simultaneous elevation of VEGF and SDF-1α caused significant CD34-positive cell elevation in patients with cardiovascular disease [4]. Additionally, plasma levels of S1P have been shown to lead to the trafficking of stem cells from the bone marrow to the peripheral blood [5]. Platelets are a rich source of VEGF, SDF-1α, and S1P [3], and platelet-rich plasma could enhance the proliferation of bone marrow mesenchymal stem cells, which are known to be multi-potent stem cells [6]. On the other hand, stem cells are also known to differentiate into megakaryocytes and to subsequently produce platelets [7]. Therefore, platelet count might positively correlate with the number of circulating CD34-positive cells.
Moreover, CD34-positive cells have been reported to contribute to endothelial repair [10]. Since platelets induce differentiation of human CD34-positive cells into endothelial cells [9], and SDF-1α promotes differentiation of CD34-positive cells to endothelial progenitor cells [1], the positive correlation between platelets and circulating CD34-positive cells might indicate endothelial repair activity.
However, in subjects with hypertension, we found no significant correlation between platelets and circulating CD34-positive cells. Furthermore, in subjects with hypertension, a significant positive correlation was seen between platelets and CIMT.
Since hypertension is a well-known endothelial impairment factor [12], the necessity of endothelial repair in hypertensive subjects is much higher than in subjects without hypertension. Therefore, hypertension has been reported to increase the number of activated platelets in peripheral blood [19]. However, in hypertensive subjects, maximum CD34-positive cell productivity by the bone marrow might easily be attained, followed by a consumptive reduction in circulating CD34-positive cells. Since CD34-positive cells are immature cells, aggressive endothelial repair might cause consumptive reduction in circulating CD34-positive cells because many of them become mature cells (CD34-negative cells) such as endothelial cells, mural cells, and foam cells. Even though the presence of CD34-positive cells in human atherosclerotic lesions was previously observed [20,21], that fact that increased circulating CD34-positive cell count was associated with a decrease in the extent of subclinical atherosclerosis in asymptomatic men [22] might be explained by the influence of this consumptive reduction. Under such conditions, the positive correlation between platelet count and number of circulating CD34-positive cells disappears.
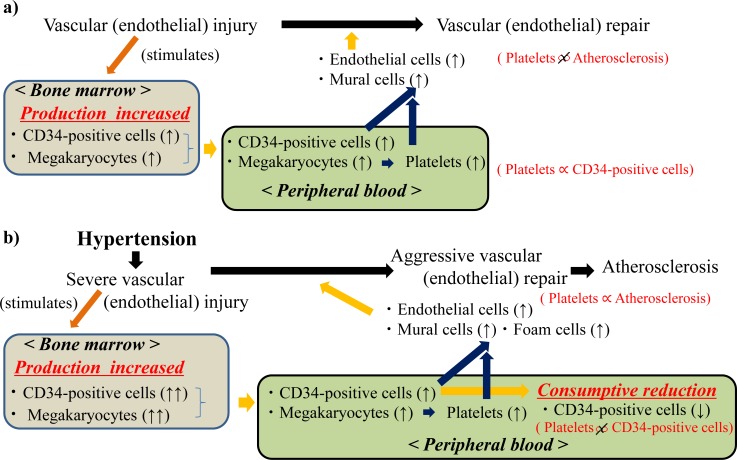
On the other hand, platelets are reported to play an important role in the development of atherosclerotic lesions as an initial actor [11]. Additionally, platelets not only induce differentiation of human CD34-positive cells into endothelial cells, but also into foam cells, which are a contributing factor in the development of atherosclerosis [9]. The existence of circulating CD34-positive cells in hypertensive men with high plasma platelet levels might no longer reduce the risk of atherosclerosis despite CD34-positive cells playing important role in endothelial repair [10]. Therefore, in our study, the significant positive correlation between platelets and mean CIMT is limited to subjects with hypertension. The possible mechanisms underlying the correlation between platelet and CD34-positive cell on vascular repair are summarized in Figure 2. The number of circulating CD34-positive cell is determined by production and consuming.
Figure 2.
Possible mechanisms underlying the platelet and CD34-positive cell on vascular repair among a) subjects without hypertension and b) subjects with hypertension
Potential limitations of this study warrant consideration. Since we have no data regarding activated platelets (P-selectin-positive platelets), the exact influence of active platelets on the circulating CD34-positive cells is unknown. However, a previous study reported that platelet rich plasma enhances the proliferation of bone marrow multi-potent stem cells [6]. Therefore, we believe that the number of platelets correlates with the number of active platelets. Further studies that include data on active platelets are necessary. Additionally, as this was a cross-sectional study, we were not able to establish causal relationships.
In conclusion, our findings demonstrate that platelet count indicates vascular repair activity, and that hypertension might mask the beneficial effects of circulating CD34-positive cells.
MATERIALS AND METHODS
Subjects and methods
This study was approved by the Ethics Committee for Human Use of Nagasaki University (project registration number 14051404). Written consent forms were available in Japanese to ensure comprehensive understanding of the study objectives, and informed consent was provided by the participants. The study population comprised 617 male residents aged 60-69 years from the western rural communities of the Goto city and Saza town, who undertook an annual medical check-up from 2013 to 2015 as recommended by the Japanese government.
To avoid the influence of inflammatory disease and hematological disease, subjects with high and low white blood cell counts (≥10,000 cells/μL (n = 8) and 1,000 cells/μL< (n = 2), respectively) were excluded. Additionally, to avoid the influence of bone marrow- activating medications, subjects taking medicines for anemia (n = 3) were also excluded from the analysis, as were persons with missing data (n = 37). The remaining patients, comprising 567 men with a mean age of 65.5 years (standard deviation (SD): 2.6; range: 60-69), were enrolled in the study.
Data collection and laboratory measurements
Body weight and height were measured with an automatic body composition analyzer (BF-220; Tanita, Tokyo, Japan) and body mass index (BMI; kg/m2) was calculated. Systolic and diastolic blood pressure was recorded at rest. Hypertension was diagnosed as a systolic blood pressure ≥ 140mmHg and/or a diastolic blood pressure ≥ 90mmHg.
Fasting blood samples were collected in an EDTA-2K tube, a heparin sodium tube and a siliconized tube. The levels of platelets (Plt) and white blood cells (WBC) in samples from the EDTA-2K tube were measured at SRL, Inc. (Tokyo, Japan) using flow cytometry.
Fresh samples (within 24 hours of collection) from a heparin sodium tube were used to determine the number of CD34-positive cells. BD (Beckton Dickinson Biosciences) TrucountTM technology, an accurate and reproducible single platform assay conforming to the International Society of Hematotherapy and Graft Engineering (ISHAGE) guidelines [23, 24] and supported by automated software on the BD FACSCantoTM II system, was used to measure circulating CD34-positive cells. Serum samples were separated to measure the concentration of aspartate aminotransferase (AST) and γ-glutamyltranspeptidase (γ-GTP) using the Japanese Society of Clinical Chemistry (JSCC) standardization method. Triglycerides (TG), uric acid (UA) and creatinine were measured enzymatically. HDL-cholesterol (HDL) was measured using the direct method, while hemoglobin A1c (HbA1c) was measured using the latex coagulation method. Glomerular filtration rate (GFR) was estimated by means of an established method using three variations that had recently been proposed by the working group of the Japanese Chronic Kidney Disease initiative [25]. According to this adapted version, GFR (mL/min/1.73 m2) = 194 × (serum creatinine (enzyme method))−1.094× (age)−0.287.
Measurement of carotid intima media thickness (CIMT) was determined by ultrasonography of the left and right carotid arteries by an experienced vascular technician using a LOGIQ Book XP with a 10-MHz transducer, GE Healthcare, Milwaukee, WI, USA). Mean values for the left and right CIMT were calculated using automated digital edge-detection software (Intimascope; MediaCross, Tokyo, Japan) and a protocol that has been described in detail elsewhere [26].
Statistical analysis
Distribution of circulating CD34 cells, plasma platelet concentration, and mean CIMT were analyzed. Clinical characteristics of hypertensive and non-hypertensive subjects were compared. Simple correlation analysis (correlation coefficient) of circulating CD34-positive cells, platelets and other variables stratified by hypertension status were performed. In order to determine the correlation between the number of circulating CD34-positive cells and platelets, simple and multiple linear regression analysis accounting for hypertension status was performed, along with simple and multiple linear regression analysis of the mean CIMT and other variables.
Adjustments were made for classical cardiovascular risk factors such as age, systolic blood pressure (mmHg), diastolic blood pressure (mmHg), body mass index, HbA1c (%), HDL (mg/dL), TG(mg/dL), AST (IU/L), γ-GTP(IU/L), UA(mg/dL), and GFR (mL/min/1.73m2). Because CD34-positive cells, TG, and γ-GTP had a skewed distribution, logarithmic transformation was performed for simple and partial correlation analysis, and linear regression analysis.
All statistical analyses were performed with the SAS system for Windows (version 9.3; SAS Inc., Cary, NC). Probability values less than 0.05 were considered to be statistically significant.
Acknowledgments
We are grateful to the staff of Goto City Hall and Saza Town Hall for their outstanding support.
Footnotes
CONFLICTS OF INTEREST
The authors of this manuscript declare no conflict of interests.
FUNDING
This work was supported financially by a Grant-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (No.15K07243, No.25440255).
REFERENCES
- 1.Stellos K, Langer H, Daub K, Schoenberger T, Gauss A, Geisler T, Bigalke B, Mueller I, Schumm M, Schaefer I, Seizer P, Kraemer BF, Siegel-Axel D, May AE, Lindemann S, Gawaz M. Platelet-derived stromal cell-derived factor-1 regulates adhesion and promotes differentiation of human CD34+ cells to endothelial progenitor cells. Circulation. 2008;117:206–215. doi: 10.1161/CIRCULATIONAHA.107.714691. [DOI] [PubMed] [Google Scholar]
- 2.Stellos K, Bigalke B, Langer H, Geisler T, Schad A, Kögel A, Pfaff F, Stakos D, Seizer P, Müller I, Htun P, Lindemann S, Gawaz M. Expression of stromal-cell-derived factor-1 on circulating platelets is increased in patients with acute coronary syndrome and correlates with the number of CD34+ progenitor cells. Eur Heart J. 2009;30:584–593. doi: 10.1093/eurheartj/ehn566. [DOI] [PubMed] [Google Scholar]
- 3.Seitz G, Boehmler AM, Kanz L, Möhle R. The role of sphingosine 1-phosphate receptors in the trafficking of hematopoietic progenitor cells. Ann N Y Acad Sci. 2005;1044:84–89. doi: 10.1196/annals.1349.011. [DOI] [PubMed] [Google Scholar]
- 4.Cangiano E, Cavazza C, Campo G, Valgimigli M, Francolini G, Malagutti P, Pratola C, Ferrari R. Different clinical models of CD34+ cells mobilization in patients with cardiovascular disease. J Thromb Thrombolysis. 2011;32:1–8. doi: 10.1007/s11239-010-0543-8. [DOI] [PubMed] [Google Scholar]
- 5.Golan K, Vagima Y, Ludin A, Itkin T, Cohen-Gur S, Kalinkovich A, Kollet O, Kim C, Schajnovitz A, Ovadya Y, Lapid K, Shivtiel S, Morris AJ, Ratajczak MZ, Lapidot T. S1P promotes murine progenitor cell egress and mobilization via S1P1-mediated ROS signaling and SDF-1 release. Blood. 2012;119:2478–2488. doi: 10.1182/blood-2011-06-358614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zou J, Yuan C, Wu C, Cao C, Yang H. The effects of platelet-rich plasma on the osteogenic induction of bone marrow mesenchymal stem cells. Connect Tissue Res. 2014;55:304–309. doi: 10.3109/03008207.2014.930140. [DOI] [PubMed] [Google Scholar]
- 7.Matsubara Y, Ono Y, Suzuki H, Arai F, Suda T, Murata M, Ikeda Y. OP9 bone marrow stroma cells differentiate into megakaryocytes and platelets. PLos One. 2013;8:e58123. doi: 10.1371/journal.pone.0058123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gunn N, Damon L, Varosy P, Navarro W, Martin T, Ries C, Linker C. High CD34+ cell dose promotes faster platelet recovery after autologous stem cell transplantation for acute myeloid leukemia. Biol Blood Marrow Transplant. 2003;9:643–648. doi: 10.1016/s1083-8791(03)00232-5. [DOI] [PubMed] [Google Scholar]
- 9.Daub K, Langer H, Seizer P, Stellos K, May AE, Goyal P, Bigalke B, Schönberger T, Geisler T, Siegel-Axel D, Oostendorp RA, Lindemann S, Gawaz M. Platelets induce differentiation of human CD34+ progenitor cells into foam cells and endothelial cells. FASEB J. 2006;20:2559–2561. doi: 10.1096/fj.06-6265fje. [DOI] [PubMed] [Google Scholar]
- 10.Majka M, Janowska-Wieczorek A, Ratajczak J, Ehrenman K, Pietrzkowski Z, Kowalska MA, Gewirtz AM, Emerson SG, Ratajczak MZ. Numerous growth factors, cytokines, and chemokines are secreted by human CD34(+) cells, myeloblasts, erythroblasts, and megakaryoblasts and regulate normal hematopoiesis in an autocrine/paracrine manner. Blood. 2001;97:3075–3085. doi: 10.1182/blood.v97.10.3075. [DOI] [PubMed] [Google Scholar]
- 11.Lindemann S, Krämer B, Seizer P, Gawaz M. Platelets, inflammation and atherosclerosis. J Thromb Haemost. 2007;5(S1):203–211. doi: 10.1111/j.1538-7836.2007.02517.x. [DOI] [PubMed] [Google Scholar]
- 12.Puddu P, Puddu GM, Zaca F, Muscari A. Endothelial dysfunction in hypertension. Acta Cardiol. 2000;55:221–232. doi: 10.2143/AC.55.4.2005744. [DOI] [PubMed] [Google Scholar]
- 13.Shimizu Y, Sato S, Koyamatsu J, Yamanashi H, Nagayoshi M, Kadota K, Maeda T. Circulating CD34-positive cells, glomerular filtration rate and triglycerides in relation to hypertension. Atherosclerosis. 2015;243:71–76. doi: 10.1016/j.atherosclerosis.2015.08.035. [DOI] [PubMed] [Google Scholar]
- 14.Shi G, Morrell CN. Platelets as initiators and mediators of inflammation at the vessel wall. Thromb Res. 2011;127:387–390. doi: 10.1016/j.thromres.2010.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ombrello C, Block RC, Morrell CN. Our expanding view of platelet functions and its clinical implications. J Cardiovasc Transl Res. 2010;3:538–546. doi: 10.1007/s12265-010-9213-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dsouza D, Wu KK, Hellums JD, Phillips MD. Platelet activation and arterial thrombosis. Lancet. 1994;334:991–995. [Google Scholar]
- 17.Nakamura T, Kambayashi J, Okuma M, Tandon NN. Activation of the GPIIb -IIIa complex induced by platelet adhesion to collagen is mediated by both alpha2beta1 integrin and GP VI. J Biol Chem. 1999;274:11897–11903. doi: 10.1074/jbc.274.17.11897. [DOI] [PubMed] [Google Scholar]
- 18.Zaffran Y, Meyer SC, Negrescu E, Reddy KB, Fox JE. Signaling across the platelet adhesion receptor glycoprotein Ib-IX induces alpha IIb beta 3 activation both in platelets and a transfected Chinese hamster ovary cell system. J Biol Chem. 2000;275:16779–16787. doi: 10.1074/jbc.275.22.16779. [DOI] [PubMed] [Google Scholar]
- 19.Nityanand S, Pande I, Bajpai VK, Singh L, Chandra M, Singh BN. Platelets in essential hypertension. Thromb Res. 1993;72:447–454. doi: 10.1016/0049-3848(93)90245-j. [DOI] [PubMed] [Google Scholar]
- 20.Torsney E, Mandal K, Halliday A, Jahangiri M, Xu Q. Characterisation of progenitor cells in human atherosclerotic vessels. Atherosclerosis. 2007;191:259–264. doi: 10.1016/j.atherosclerosis.2006.05.033. [DOI] [PubMed] [Google Scholar]
- 21.Moreno PR, Purushothaman KR, Fuster V, Echeverri D, Truszczynska H, Sharma SK, Badimon JJ, O'Connor WN. Plaque neovascularization is increased in raptured atherosclerotic lesions of human aorta: implications for plaque vulnerability. Circulation. 2004;110:2032–2038. doi: 10.1161/01.CIR.0000143233.87854.23. [DOI] [PubMed] [Google Scholar]
- 22.Bielak LF, Horenstein RB, Ryan KA, Sheedy PF, Rumberger JA, Tanner K, Post W, Mitchell BD, Shuldiner AR, Peyser PA. Circulating CD34+ Cell Count is Associated with Extent of Subclinical Atherosclerosis in Asymptomatic Amish Men, Independent of 10-Yaer Framingham Risk. Clin Med Cardiol. 2009;3:53–60. doi: 10.4137/cmc.s2111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sutherland DR, Anderson L, Keeney M, Nayar R, Chin-Yee I. The ISHAGE guidelines for CD34+ cell determination by flow cytometry. International Society of Hemototherapy and Graft Engineering. J Hematother. 1996;5:213–226. doi: 10.1089/scd.1.1996.5.213. [DOI] [PubMed] [Google Scholar]
- 24.Barnett D, Janossy G, Lubenko A, Matutes E, Newland A, Reilly JT. Guideline for the flow cytometric enumeration of CD34+ haematopoietic stem cells. Prepared by the CD34+ haematopoietic stem cell working party. General Haematology Task Force of the British Committee for Standards in Haematology. Clin Lab Haematol. 1999;21:301–308. doi: 10.1046/j.1365-2257.1999.00253.x. [DOI] [PubMed] [Google Scholar]
- 25.Imai E, Horio M, Watanabe T, Iseki K, Yamagata K, Hara S, Ura N, Kiyohara Y, Moriyama T, Ando Y, Fujimoto S, Konta T, Yokoyama H, Makino H, Hishida A, Matsuo S. Prevalence of chronic kidney disease in the Japanese general population. Clin Exp Nephrol. 2009;13:621–630. doi: 10.1007/s10157-009-0199-x. [DOI] [PubMed] [Google Scholar]
- 26.Hara T, Takamura N, Akashi S, Nakazato M, Maeda T, Wada M, Nakashima K, Abe Y, Kusano Y, Aoyagi K. Evaluation of clinical markers of atherosclerosis in young and elderly Japanese adults. Clin Chem Lab Med. 2006;44:824–829. doi: 10.1515/CCLM.2006.149. [DOI] [PubMed] [Google Scholar]