Abstract
Childhood trauma (CT) has been identified as a potential risk factor for the onset of psychotic disorders. However, to date, there is limited consensus with respect to which symptoms may ensue after exposure to trauma in early life, and whether specific pathways may account for these associations. The aim of the present study was to use the novel network approach to investigate how different types of traumatic childhood experiences relate to specific symptoms of psychotic disorders and to identify pathways that may be involved in the relationship between CT and psychosis. We used data of patients diagnosed with a psychotic disorder (n = 552) from the longitudinal observational study Genetic Risk and Outcome of Psychosis Project and included the 5 scales of the Childhood Trauma Questionnaire-Short Form and all original symptom dimensions of the Positive and Negative Syndrome Scale. Our results show that all 5 types of CT and positive and negative symptoms of psychosis are connected through symptoms of general psychopathology. These findings are in line with the theory of an affective pathway to psychosis after exposure to CT, with anxiety as a main connective component, but they also point to several additional connective paths between trauma and psychosis: eg, through poor impulse control (connecting abuse to grandiosity, excitement, and hostility) and motor retardation (connecting neglect to most negative symptoms). The results of the current study suggest that multiple paths may exist between trauma and psychosis and may also be useful in mapping potential transdiagnostic processes.
Key words: early trauma, psychotic disorders, affective pathway to psychosis, schizophrenia, network analysis
Introduction
Childhood trauma (CT) has been extensively investigated as a potential risk factor for the onset and course of psychosis, and found to relate to some of the most severe forms of symptomatology in adulthood, including hallucinations, delusions, and paranoia (here used with the meaning “suspiciousness”).1–4 However, in spite of intense research into the topic, the nature of the relationship between CT and psychosis is yet to be fully understood.
Current psychometric practices in psychopathology research conceptualize psychotic disorders—and mental disorders in general—as common causes of symptoms.5 In other words, symptoms are taken to be indicators of an underlying disease entity and correlations between symptoms can be fully explained by the common influence of the latent variable. Despite decades of research, however, finding such underlying causes for symptoms has been very rare6; instead, the causes appear to be multifactorial, thus, challenging the likelihood of a common cause explanation for associations between symptoms.7–10 As a result, in recent years, the common cause approach to mental disorders has been called into question and the dynamical systems conceptualization of psychopathology gained ground, leading to the development of “network models”.11 In network models, correlations between symptoms are no longer explained by the common latent factor (ie, mental disorder), but mental disorders are conceptualized as complex systems, in which symptoms and psychological, biological, and sociological components have autonomous causal power to influence each other.11–13 Within this framework, the associations among symptoms are conceptualized to constitute the disorder—an external trigger could produce a certain symptom (eg, anxiety), which could in turn activate other symptoms (eg, paranoia). In addition, in contrast to the common cause model and in line with clinicians’ viewpoints,14 network models allow for the notion of mutually reinforcing symptom cycles (eg, social withdrawal leading to poor rapport and poor rapport leading in turn to social withdrawal). To date, the network approach contributed to several advancements in psychopathology research7,15,16 and personality research.17 For instance, it was found that losing a partner (ie, bereavement) mainly impacted on the symptom “loneliness,” which in turn activated other depression symptoms.15 In addition, non-DSM18 symptoms, such as sympathetic arousal, were identified to be as central in a network (ie, as important) as DSM depression symptoms.19 Finally, at least in depression, symptom network structures appear to be associated with the prospective course of the disorder: The symptom network is more strongly connected in the subgroup of individuals with a worse prognosis.20
The current article used the network framework to address 2 issues in psychosis research that have yet to be solved. First, there is limited consensus whether CT only evokes specific psychotic symptoms or all symptoms to the same degree. For instance, several studies have specifically linked CT to hallucinations,21 to both hallucinations and delusions,2,22–24 and found no significant link between CT and negative symptoms.1 More recent research, however, highlighted the heterogeneity in the relationship between CT and psychotic symptoms. In a large sample of patients with psychosis, childhood abuse and neglect resulted in a vulnerability to develop both (subthreshold) positive and negative symptoms25; all positive symptoms were more pronounced in the context of abuse.26 Furthermore, in a large recent epidemiological study, no evidence for specificity of any of the CT variables (emotional neglect, physical abuse, psychological abuse, or sexual abuse) to any of the psychotic experiences was identified and CT was associated with a wide range of psychotic symptoms.27
Second, the exploration of potential mechanistic pathways that account for the association between CT and psychosis is at very best in its infancy. It has been hypothesized that traumatic experiences may result in structural and neurochemical abnormalities in the brain and nervous system, thereby affecting the function of the hypothalamus-pituitary-adrenal axis, which plays a role in stress response.28–30 It is thus possible that CT may lead to psychosis due to increased emotional reactivity to daily life stress, supporting the construct of an affective pathway to psychosis.31 Alternatively, cognitive models of psychosis argue that trauma may lead to negative beliefs about the self, world, and others. These beliefs may in turn lead to distressing interpretations of everyday events, eventually resulting in psychotic experiences.32
One limitation of many existing studies is that these investigated the relationship between CT and positive psychotic symptoms (primarily hallucinations and delusions), but less attention was given to other symptom scales in patient populations. This may be an important omission, as the psychosis spectrum is composed of multiple symptom domains, covering in addition to positive psychotic symptoms, also negative psychotic symptoms as well as affective and cognitive symptoms.33 In the present study, all these symptom dimensions are considered. To this end, we used the most widely accepted questionnaire to assess symptom severity in psychotic disorders: the Positive and Negative Syndrome Scale (PANSS).34 The PANSS consists of 3 subscales: the positive scale, the negative scale, and the general psychopathology scale. The aim of the present study is to contribute to the efforts of revealing the nature of the relationship between CT and psychosis, by analyzing the network structure of all underlying symptoms of psychotic disorders and their relationship to CT. This may give insights into both the relationship between CT and psychotic symptoms, and the potential pathways that may account for this association.
Method
Participants
We analyzed data (database version 3.2) from the longitudinal observational cohort study “Genetic Risk and Outcome of Psychosis Project” (GROUP),35 which was designed to study vulnerability and protective factors for variation in expression and course of nonaffective psychotic disorders. The full GROUP sample consists of patients with psychotic disorders (n = 1120), their siblings (n = 1057), their parents (n = 919), and a control group (n = 590). In the present study, we used data from the patient sample only. The patients were recruited from 36 mental health care institutions in The Netherlands and Belgium including 4 academic medical centers (Amsterdam, Groningen, Maastricht, and Utrecht). Inclusion criteria for participating patients were the age between 16 and 50 years, meeting full DSM18 criteria for a nonaffective psychotic disorder, maximum duration of illness of 10 years, and estimated level of intelligence quotient above 70. More detailed information of sample characteristics and recruitment methods has been previously published.35
Symptomatology
We used the first wave of data from the PANSS34 as an interview-rated measure of symptom severity in the patient population. The PANSS consists of 30 items divided in 3 subscales: the positive scale (eg, hallucinations, paranoia), the negative scale (eg, social withdrawal, blunted affect), and the general psychopathology scale (eg, anxiety and poor impulse control). It is scored by a trained interviewer on a 7-point Likert-type scale, ranging from 1 (absent) to 7 (very severe).
Childhood Trauma
CT was measured with the Dutch version of the Childhood Trauma Questionnaire-Short Form (CTQ-SF).36 First wave data were collected at the Maastricht site, whereas follow-up measurements were collected at the other sites. The CTQ-SF is a self-report questionnaire, consisting of 24 items, which were scored on a 5-point Likert-type scale, ranging from 1 (never true) to 5 (always true). The CTQ measured 5 types of childhood maltreatment (before the age of 17 years): physical neglect (failure of caretaker to provide basic necessities for a child such as food, clothing, shelter); physical abuse (bodily assault on a child posing a risk of or resulting in injury); emotional neglect (failure of caretaker basic emotional and psychological needs for a child, such as love and nurturance); emotional abuse (verbal assaults on a child, such as humiliation); and sexual abuse (unwanted sexual contact or conduct between a child and an adult). Each scale encompassed 5 items, with the exception of the sexual abuse scale, from which the item “Molestation” was removed in the current study due to improper translation into Dutch.37 A sum-score was calculated for each scale and used when computing the networks—the sum of the sexual abuse scale was multiplied by 5/4 to have approximately the same mean levels as the other scales.38
Network Construction
We constructed networks in which each of the PANSS symptoms and each of the 5 scales of the CTQ-SF questionnaire are represented as “nodes,” and an “edge” between 2 nodes indicates a partial correlation between the 2 variables, after conditioning on all other variables in the dataset. Green edges illustrate positive partial correlations, red edges negative partial correlations, and the wider and more saturated the edge, the stronger the correlation.39 State of the art methodology from the field of statistical learning was utilized to select which edges should be included in the network. These edges can be interpreted as predictive effects. Thus, the networks lie in-between correlation networks (in which connections represent zero-order correlations) and fully directed causal networks (in which all connections are oriented): They represents the part of the pairwise association structure that cannot be explained by other variables in the model.
More technically, we fitted a Gaussian graphical model (GGM)40 to the data. A GGM is an undirected network, in which a missing edge indicates that 2 variables are independent after conditioning on the set of remaining variables. To control for spurious connections that may result from sampling error, as well as to estimate a more interpretable and sparse model, recent literature41 suggests to employ L1 regularization.42 L1 regularization corrects for Type 1 errors and reduces the overall strength of parameter estimates, for model simplification (ie, the small values will thus become exactly 0, whereas the others values will be shrunken)43; in addition, we used a minimum absolute value of 0.03 for visualization. L1 regularization utilizes a tuning parameter that controls the sparsity of the model, which can be selected by minimizing the extended Bayesian information criterion.44 The EBIC itself utilizes a tuning hyperparameter γ, typically set to 0.5, which was shown to yield accurate network estimations.45–47 This method converges to the true network, assuming that a set of sparse pairwise interactions indeed underlie the data.48 For more details, we refer the reader to the cited tutorial article.41
Network Analysis
The resulting network was further analyzed by investigating the importance (centrality) of each node in the network. This can be captured in centrality measures of which three were investigated here: node strength, betweenness, and closeness.46–48 In weighted networks, node strength is a measure of the number and strength of connections. “Betweenness” measures how often a node lies on the shortest path between every combination of 2 other nodes, indicating to what extent the node facilitates the flow of information through the network. The “closeness” of a node measures the average distance from that node to all other nodes in the network, with high closeness indicating a short average distance between a given node and the remaining nodes in the network.
Next, networks illustrating the shortest paths between each trauma scale and the positive and negative symptoms of the PANSS were computed. In comparison to the first network, these networks allow clear identification of possible pathways and mediating items between trauma and psychotic symptoms. The shortest path between 2 nodes represents the minimum number of steps needed to go from one node to the other,49 and it is computed using Dijkstra’s algorithm.50 This can be seen as a roadmap including all possible routes from destination A to destination B, but only one of these routes being quicker—this would then be the route highlighted in the shortest path network. Our networks illustrate what the shortest routes are from each CT scale to the different clusters of positive and negative psychotic symptoms. Given that the partial correlations between one node and all other nodes in the network are directly related to the regression coefficients obtained in a multiple regression model, these can thus be interpreted as predictive effects51: Two connected nodes predict each other, and any node that connects the 2 nodes (eg, node B in the pathway A-B-C) can be seen to mediate the predictive quality between the 2 nodes. As such, a partial correlation network can be viewed as a causal skeleton encompassing the existence of putative causal relationships.
All analyses were performed using the “R”-statistical software.52 The networks were constructed and visualized using the R-package “qgraph.”39 The layout used when computing the networks was the Fruchterman and Reingold layout,53 which places the nodes with stronger connections into the center of the network, and the nodes with weaker connections closer to the periphery of the network.
Results
In total, after removing all missing data, 552 patients were included in the analyses. The participating patients, of whom 75% were male, had a mean age of 30.8 years (SD = 7.27). On the basis of a cutoff score of low to moderate severity,38 approximately 25% of the patients reported being physically neglected, 79% emotionally neglected, 25% sexually abused, 26% emotionally abused, and 16% physically abused. A significant gender difference (P = .01) was identified on the sexual abuse scale, with females reporting higher scores than males.
All missing data were removed using the listwise deletion method. Comparison of participating patients with excluded patients revealed a significant difference (P = .008) in gender, with the number of male patients being higher in the sample excluded due to missing data. We have carried out a missing completely at random test using the R-package “MissMech,”54 which confirmed that the PANSS and CT data were missing at random. No significant differences were identified between the omitted participants and participants who were included in the analytic sample on age, diagnosis, scores on the PANSS interview, and CT reports (all P > .05), with the exception of the score on the physical neglect scale of the CTQ (P = .048). In addition, no significant differences were found (all comparison > .05) in the PANSS scores between participants who completed the PANSS and the CTQ at baseline and participants who completed the PANSS but were not available for CT assessment.
Table 1 presents the demographic and clinical characteristics of the sample, the mean sum-scores on the 3 PANSS dimensions and the 5 dimensions of the CTQ-SF. Table 2 presents the item distribution and the item labels for all following networks. The current data were not univariate normally distributed, and as such, a nonparanormal transformation55 to relax the normality assumption was applied prior to constructing the networks.
Table 1.
Demographic and Clinical Characteristics of Participating Patients: Means (SD)
| Variable | Men (n = 418) | Women (n = 134) | Total (n = 552) |
|---|---|---|---|
| Age (years) | 30.35 (6.59) | 32.01 (8.99) | 30.76 (7.27) |
| Diagnostic | |||
| Schizophrenia | 294 (53.3%) | 86 (15.6%) | 380 (68.9%) |
| Schizophreniform | 12 (2.2%) | 7 (1.2%) | 19 (3.4%) |
| Schizoaffective | 63 (11.4%) | 28 (5.1%) | 91 (16.5%) |
| Delusional | 7 (1.2%) | 0 | 7 (1.2%) |
| Psychotic NOS | 42 (7.6%) | 13 (2.4%) | 55 (10%) |
| PANSS (sum) | |||
| Positive symptoms | 12.93 (5.42) | 11.16 (4.64) | 12.50 (5.29) |
| Negative symptoms | 13.65 (5.69) | 12.04 (5.15) | 13.26 (5.60) |
| General psychopathology | 27.67 (8.26) | 25.18 (7.72) | 27.06 (8.20) |
| CTQ-SF (sum) | |||
| Emotional neglect | 18.80 (4.25) | 18.25 (4.75) | 18.69 (4.38) |
| Physical neglect | 12.18 (1.82) | 11.90 (1.83) | 12.11 (1.83) |
| Emotional abuse | 8.83 (3.85) | 9.96 (4.77) | 9.11 (4.19) |
| Physical abuse | 6.25 (2.65) | 6.28 (2.71) | 6.26 (2.66) |
| Sexual abuse | 10.30 (3.04) | 9.75 (2.86) | 10.17 (3.00) |
Note: CTQ-SF, Childhood Trauma Questionnaire-Short Form; PANSS, Positive and Negative Syndrome Scale; Psychotic NOS, Psychotic not otherwise specified.
Table 2.
Items of the Positive and Negative Syndrome Scale and the Childhood Trauma Questionnaire-Short Form and Their Assigned Colors and Labels
| Item Label | Domain Color | Item Description |
|---|---|---|
| P1 | Purple | Delusions |
| P2 | Purple | Conceptual disorganization |
| P3 | Purple | Hallucinations |
| P4 | Purple | Excitement |
| P5 | Purple | Grandiosity |
| P6 | Purple | Paranoia/suspiciousness |
| P7 | Purple | Hostility |
| N1 | Blue | Blunted affect |
| N2 | Blue | Emotional withdrawal |
| N3 | Blue | Poor rapport |
| N4 | Blue | Social withdrawal |
| N5 | Blue | Difficulty in abstract thinking |
| N6 | Blue | Lack of spontaneity |
| N7 | Blue | Stereotyped thinking |
| GP1 | Yellow | Somatic concern |
| GP2 | Yellow | Anxiety |
| GP3 | Yellow | Guilt |
| GP4 | Yellow | Tension |
| GP5 | Yellow | Mannerism and posturing |
| GP6 | Yellow | Depression |
| GP7 | Yellow | Motor retardation |
| GP8 | Yellow | Uncooperativeness |
| GP9 | Yellow | Unusual thought content |
| GP10 | Yellow | Disorientation |
| GP11 | Yellow | Poor attention |
| GP12 | Yellow | Poor judgment and insight |
| GP13 | Yellow | Disturbed willpower |
| GP14 | Yellow | Poor impulse control |
| GP15 | Yellow | Preoccupation |
| GP16 | Yellow | Active social avoidance |
| CT1 | Maroon | Physical neglect |
| CT2 | Maroon | Emotional neglect |
| CT3 | Maroon | Sexual abuse |
| CT4 | Maroon | Emotional abuse |
| CT5 | Maroon | Physical abuse |
CT and PANSS
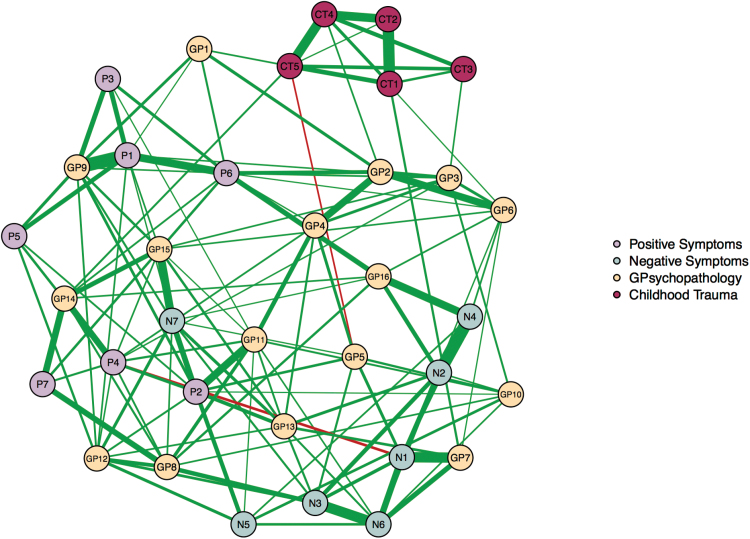
The first network we constructed illustrates the relationship between CT and all 3 scales of the PANSS (ie, positive symptoms, negative symptoms, and general psychopathology symptoms; figure 1). When evaluating the network, strikingly, there is no connectivity between the CT scales and positive or negative psychotic symptoms; CT only connects to the general psychopathology scale of the PANSS. Node CT5 (physical abuse) is positively associated with GP1 (somatic concern) and GP14 (poor impulse control) and negatively associated with GP5 (mannerism and posturing). Node CT4 (emotional abuse) is positively associated with item GP2 (anxiety), node CT3 (sexual abuse) is positively associated with item GP3 (guilt), and node CT1 (physical neglect) is positively associated with item GP7 (motor retardation). Centrality measures of the network (see supplementary figure 1) show that item GP9 (unusual thought content) has the highest betweenness, closeness, and strength measures, suggesting this is as an influential node within the network. In addition, all CT items are highly interconnected within their given scale, implying that correlations among this subscale are much larger than correlations across scales.
Fig. 1.
Network depicting the 3 dimensions (positive, negative, and general psychopathology symptoms) of the Positive and Negative Syndrome Scale and the 5 dimensions of the Childhood Trauma Questionnaire-Short Form. Symptom groups are differentiated by colors. Each edge within the network corresponds to a partial correlation between 2 individual items. The thickness of an edge represents the absolute magnitude of the correlation (the thicker the edge, the stronger the connection), whereas the color of the edge indicates the size of the correlation (green for positive connections; red for negative connections). For a color version, see this figure online.
Shortest Paths: CT—Positive and Negative Psychotic Symptoms
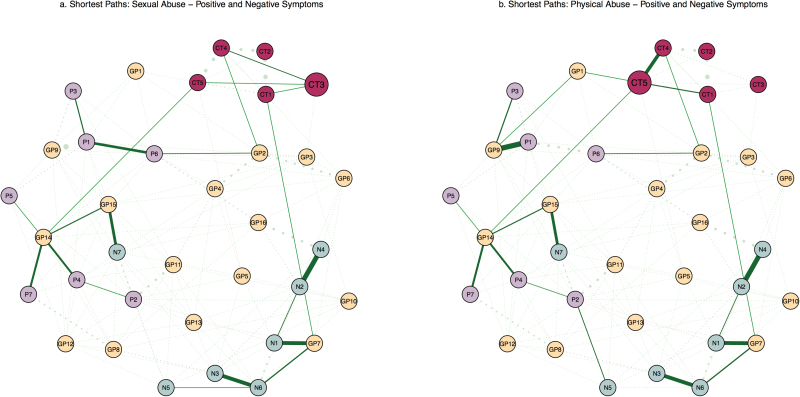
Following the symptoms network, we constructed 5 networks that depict shortest paths between each of the 5 CT scales and all individual symptoms of the PANSS. Due to high similarities between these networks and space constraints, only 2 such networks will be described in this section and the other networks are included as online supplementary material. These 2 specific CT scales were chosen because they highlight nearly all possible routes from other trauma scales to the psychotic symptoms as well.
The shortest path networks illustrate pathways between the node CT3 (sexual abuse) and the positive and negative symptoms (figure 2a), and the node CT5 (physical abuse) and the positive and negative symptoms (figure 2b). In other words, the networks display the shortest routes that connect the nodes CT3 (sexual abuse) and CT5 (physical abuse) to each individual positive and negative symptom of the PANSS.
Fig. 2.
a. Network depicting shortest paths between the Sexual Abuse scale (ie, node CT3) of the Childhood Trauma Questionnaire-Short Form (CTQ-SF) and the 2 main dimensions of the Positive and Negative Syndrome Scale (PANSS): positive symptoms and negative symptoms; b. Network depicting shortest paths between the Physical Abuse scale (ie, node CT5) of the CTQ-SF and the 2 main dimensions of the PANSS: positive symptoms and negative symptoms. Dashed lines represent background connections existent within the network that are less relevant when investigating shortest paths; thicker dashed lines represent stronger connections. For a color version, see this figure online.
In figure 2a, the shortest route to reach most negative psychotic symptoms from node CT3 (sexual abuse) is via node CT1 (physical neglect) and GP7 (motor retardation). The shortest route from CT3 (sexual abuse) to P1 (delusions), P3 (hallucinations), and P6 (paranoia) is via CT4 (emotional abuse) and GP2 (anxiety), whereas the connectivity to the remaining positive nodes P2 (conceptual disorganization), P4 (excitement), P5 (grandiosity), and P7 (hostility) runs through CT5 (physical abuse) and GP14 (poor impulse control). Lastly, to reach node N7 (stereotyped thinking) from CT3 (sexual abuse), the shortest route is via node CT5 (physical abuse), GP14 (poor impulse control), and GP15 (preoccupation).
Similarly, in figure 2b, node CT1 (physical neglect) is connected to node GP7 (motor retardation), which is in turn connected to the negative symptoms N1 (blunted affect), N2 (emotional withdrawal), N3 (poor rapport), N4 (social withdrawal), and N6 (lack of spontaneity and flow of conversation). Node CT5 (physical abuse) appears to be associated with positive symptoms through 3 pathways: (1) CT5 connects to nodes GP1 (somatic concern) and GP9 (unusual thought concern), which is in turn connected to nodes P1 (delusions) and P3 (hallucinations); (2) CT5 (physical abuse) connects to node GP14 (poor impulse control), which is in turn connected to the nodes P2 (conceptual disorganization), P4 (excitement), P5 (grandiosity), and P7 (hostility); (3) CT5 (physical abuse) connects to the trauma node CT4 (emotional abuse), which is in turn connected to item GP2 (anxiety), followed by item P6 (paranoia). The networks depicting the shortest paths between the remaining 3 CT scales—CT1 (physical neglect), CT2 (emotional neglect), and CT4 (emotional abuse)—and the positive, negative, and general psychopathology symptoms can be accessed in supplementary figures 2–4.
In addition, taking into account previous literature that focused mainly on positive and negative psychotic symptoms, we constructed a network that illustrates the relationship between CT and only these 2 scales of the PANSS (supplementary figure 5). This additional step highlights that in the absence of the general psychopathology scale, there is direct connectivity between CT and positive psychotic symptoms, via the nodes P6 (paranoia) and P7 (hostility). When including the general psychopathology scale, however, this connectivity is no longer present.
Discussion
The current article provides the first network-based analysis of the relationship between CT and psychosis. In sum, we constructed a network that included the 3 original symptom dimensions of the PANSS interview (ie, positive symptoms, negative symptoms, and general psychopathology symptoms). Our results show that the CT subscales are not directly associated with any of the positive or negative symptoms—they are connected to the 2 scales only via general psychopathology symptoms. In other words, general psychopathology symptoms appear to mediate the relationship between trauma and psychosis. By computing shortest path networks, we illustrated which general psychopathology symptoms are activating different positive and negative symptoms (eg, anxiety activating paranoia, delusions, and hallucinations; poor impulse control activating grandiosity, hostility, and excitement; motor retardation activating the cluster of negative symptoms). In certain cases, a CT node is identified on the shortest pathway between another CT node and psychotic symptoms (eg, physical neglect, emotional abuse, and physical abuse are identified on the shortest path from sexual abuse to psychotic symptoms). In line with findings from previous research,24,56 this indicates that the effects of trauma to symptoms can propagate through other types of trauma as well.
Research Implications
Even though research has so far been successful in establishing a connection between CT and psychotic symptoms, there is limited consensus with regard to potential pathways that may account for this relationship. Supporting the idea of an affective pathway to psychosis, previous research found that subjects with a history of CT reported increased negative affect, which moderated the emotional reactivity to small daily stressors.57 Likewise, higher levels of daily life stress sensitivity were associated with higher levels of positive symptoms,58 and a history of life events was found to increase the emotional reaction to daily life stressors.23 Additionally, the relationship between sexual abuse and psychosis was found to be mediated by anxiety and depression.59 Our results are in line with the existence of an affective pathway to psychosis23—trauma may lead to psychosis through a pathway of heightened emotional distress (eg, anxiety, tension, and depression). In the present article, anxiety was the main link between emotional abuse and the positive symptoms cluster paranoia, delusions, and hallucinations. Recent studies using the experience sampling method also found that an increase in anxiety predicts the onset of paranoid episodes.60,61 Furthermore, unusual thought concern was the most central item in the network, indicating that it is essential in facilitating the flow of information.
However, the current findings also suggest the existence of a connective role of other symptoms of general psychopathology (eg, poor impulse control, motor retardation, and somatic concern). First, even though not often investigated in relation to psychotic disorders, one previous study identified impulsivity as a predictor of psychotic experiences.62 Our results support these findings and suggest that poor impulse control should receive more attention as a potential risk factor in psychosis because it is the linking item between physical abuse and the positive symptoms cluster grandiosity, hostility, and excitement.
Second, motor retardation (ie, delayed or reduced movements, speech, and decreased responsiveness to stimuli) has long been acknowledged as a central component in major depression and bipolar disorder.63 In a recent network article investigating the centrality of depression symptoms, motor retardation displayed high centrality indices and was associated with energy loss, concentration problems, sympathetic arousal, and suicidal ideation.19 It is thus not surprising that in the present analysis motor retardation is strongly connected to blunted affect and lack of spontaneity and flow of conversation, setting up the main pathway between physical neglect and other negative symptoms.
Third, somatic concern and unusual thought concern were identified on the pathway from physical abuse to delusions and hallucinations, suggesting that overattention toward somatic symptoms may also act as a trigger of psychotic symptoms. Other potential pathways from CT to psychosis through symptoms of general psychopathology may exist, given that our symptom network shows further links (eg, sexual abuse associated with guilt). Nonetheless, these are not apparent in the shortest path networks and as such we argue that the 3 pathways described above may be most influential in the association of CT to psychosis—clinical practice and future interventions may benefit from taking these into consideration.
In addition, such findings re-emphasize the idea that CT is connected to a wide array of symptoms that are present in several mental conditions,64,65 and thus are not only specific to psychotic symptoms. Indeed, CT has been found to increase the risk of anxiety disorders, major depressive disorder, bipolar disorder, and personality disorders.66–68 In our sample, comorbidity rates with depression and bipolar disorder were low,35 but not fulfilling the diagnostic criteria does not imply the absence of subthreshold symptoms (eg, motor retardation is a central symptom in depression, but also a symptom measured by the general psychopathology scale of the PANSS).
Several limitations of the current study should be taken into consideration. First, the majority of the sample studied in this report was male, and males often report lower levels of early trauma compared to females.69 In our analysis, a higher number of male patients were excluded due to missing data. In addition, males and females display different psychosis symptom profiles70 and as such a different pattern of results may be observed for a more gender-balanced sample. Unfortunately, because of unequal sample sizes and power issues, separate analyses in the current dataset were not feasible. Follow-up studies may investigate gender differences in relation to early trauma and psychosis within a network framework. Second, the CTQ-SF is a self-report, retrospective measure of CT and may thus be prone to bias (eg, social desirability, memory bias, and demand characteristics). Third, CT data collection points were not identical, thus making it possible that more severe symptoms could have influenced the trauma reports. Nonetheless, recent research showed that reports on childhood abuse in patients with psychotic disorders are reasonably stable over a 7-year period and are not associated with current severity of psychotic symptoms.71 Fourth, the current analyses were based on cross sectional data; the resulting networks may be exemplary for individuals, but research on generalizability to the individual level is warranted. Moreover, due to the between-subject design, conclusions regarding direction of effects or causality should be drawn with caution. Further research could extend on this analysis by using Bayesian techniques for the application of causal modeling—such as those based on the theory of Directed Acyclic Graphs—that may help elucidate further structure in the network.72,73 Lastly, given the novelty of network models in psychopathology, rigorous methods for assessing the reliability of the estimated graph are required (eg, a more clear identification of potential errors resulting from sampling, validity of underlying assumptions)74 and still in the process of being developed. We trust future studies will be able to overcome these current shortcomings.
Conclusions
To our knowledge, the present study is the first study to investigate the relationship between CT and psychotic experiences in patients diagnosed with a psychotic disorder by using the network framework. This novel alternative approach to psychopathology conceptualizes mental disorders as causal systems of interacting symptoms. Our results suggest that several symptoms of general psychopathology may mediate the relationship between trauma and psychosis, providing evidence for multiple paths between trauma and psychosis, and re-emphasizing questions regarding the specificity of trauma to psychosis.
Supplementary Material
Supplementary material is available at http://schizophreniabulletin.oxfordjournals.org.
Funding
Geestkracht Program of the Dutch Health Research Council (ZonMw, 10-000-1002 to GROUP project); The Netherlands Organisation for Scientific Research (NWO) Veni Grant (016.156.019 to J.T.W.W.); European Research Council (ERC) Consolidator Grant (647209 to D.B.).
Supplementary Material
Acknowledgments
We thank the participants of the GROUP, the research staff involved in this project, and the mental health care organizations that made the GROUP project possible (Amsterdam: Academic Medical Center and the mental health institutions: Ingeest, Arkin, Dijk en Duin, Rivierduinen, Erasmus Medical Center, GGZ Noord Holland Noord. Maastricht: Maastricht University Medical Center and the mental health institutions: GGZ Eindhoven, GGZ Midden-Brabant, GGZ Oost-Brabant, GGZ Noord-Midden Limburg, Mondriaan Zorggroep, Prins Clauscentrum Sittard, RIAGG Roermond, Universitair Centrum Sint-Jozef Kortenberg, CAPRI University of Antwerp, PC Ziekeren Sint-Truiden, PZ Sancta Maria Sint-Truiden, GGZ Overpelt, OPZ Rekem. Groningen: University Medical Center Groningen and the mental health institutions: Lentis, GGZ Friesland, GGZ Drenthe, Dimence, Mediant, GGZ De Grote Rivieren and Parnassia psycho-medical center (The Hague). Utrecht: University Medical Center Utrecht and the mental health institutions Altrecht, Symfora, Meerkanten, Riagg Amersfoort en Delta). The authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1. Read J, Van Os J, Morrison AP, Ross CA. Childhood trauma, psychosis and schizophrenia: a literature review with theoretical and clinical implications. Acta Psychiatr Scand. 2005;112:330–350. [DOI] [PubMed] [Google Scholar]
- 2. Larkin W, Read J. Childhood trauma and psychosis: evidence, pathways, and implications. J Postgrad Med. 2003;54:287–293. [DOI] [PubMed] [Google Scholar]
- 3. Read J, Agar K, Argyle N, Aderhold V. Sexual and physical abuse during childhood and adulthood as predictors of hallucinations, delusions and thought disorder. Psychol Psychother Theory Res Pract. 2003;76:1–22. [DOI] [PubMed] [Google Scholar]
- 4. Longden E, Sampson M, Read J, Longden E, Sampson M, Sciences P. Childhood adversity and psychosis: generalised or specific effects? [published online ahead of print July 9, 2015]. Epidemiol Psychiatr Sci. 2015;1–11. doi: 10.1017/S204579601500044X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Schmittmann VD, Cramer AOJ, Waldorp LJ, Epskamp S, Kievit RA, Borsboom D. Deconstructing the construct: a network perspective on psychological phenomena. New Ideas Psychol. 2013;31:43–53. [Google Scholar]
- 6. Fried EI. Problematic assumptions have slowed down depression research: why symptoms, not syndromes are the way forward. Front Psychol. 2015;6:309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. McNally RJ, Robinaugh DJ, Wu GWY, Wang L, Deserno M, Borsboom D. Mental disorders as causal systems: a network approach to posttraumatic stress disorder [published online ahead of print December 5, 2014]. Clin Psychol Sci. 2015;3:836–849. doi: 10.1177/2167702614553230. [Google Scholar]
- 8. Fried EI, Nesse RM. The impact of individual depressive symptoms on impairment of psychosocial functioning. PLoS One. 2014;9:e90311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wichers M. The dynamic nature of depression: a new micro-level perspective of mental disorder that meets current challenges. Psychol Med. 2013;616:1–12. [DOI] [PubMed] [Google Scholar]
- 10. Cramer AOJ, Borsboom D, Aggen SH, Kendler KS. The pathoplasticity of dysphoric episodes: differential impact of stressful life events on the pattern of depressive symptom inter-correlations. Psychol Med. 2012;42:957–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Borsboom D, Cramer AOJ. Network analysis: an integrative approach to the structure of psychopathology. Annu Rev Clin Psychol. 2013;9:91–121. [DOI] [PubMed] [Google Scholar]
- 12. Cramer AOJ, Waldorp LJ, van der Maas HLJ, Borsboom D. Comorbidity: a network perspective. Behav Brain Sci. 2010;33:137–150; discussion 150–193. [DOI] [PubMed] [Google Scholar]
- 13. Kendler KS, Zachar P, Craver C. What kinds of things are psychiatric disorders? Psychol Med. 2011;41:1143–1150. [DOI] [PubMed] [Google Scholar]
- 14. Ma SH, Teasdale JD. Mindfulness-based cognitive therapy for depression: replication and exploration of differential relapse prevention effects. J Consult Clin Psychol. 2004;72:31–40. [DOI] [PubMed] [Google Scholar]
- 15. Fried EI, Bockting C, Arjadi R, et al. From loss to loneliness: the relationship between bereavement and depressive symptoms. J Abnorm Psychol. 2015;124:256–265. [DOI] [PubMed] [Google Scholar]
- 16. Ruzzano L, Borsboom D, Geurts HM. Repetitive behaviors in autism and obsessive-compulsive disorder: new perspectives from a network analysis. J Autism Dev Disord. 2015;45:192–202. [DOI] [PubMed] [Google Scholar]
- 17. Cramer AOJ, van der Sluis S, Noordhof A, et al. Dimensions of normal personality as networks in search of equilibrium: you can’t like parties if you don’t like people. Eur J Pers. 2012;26:414–431. [Google Scholar]
- 18. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 19. Fried EI, Epskamp S, Nesse RM, Tuerlinckx F, Borsboom D. What are “good” depression symptoms? Comparing the centrality of DSM and non-DSM symptoms of depression in a network analysis. J Affect Disord. 2015;189:314–320. [DOI] [PubMed] [Google Scholar]
- 20. van Borkulo CD, Boschloo L, Borsboom D, Brenda WJHP, Waldorp LJ, Schoevers RA. Association of symptom network structure with the course of depression. JAMA Psychiatry. 2016;72:1219–1226. [DOI] [PubMed] [Google Scholar]
- 21. Whitfield CL, Dube SR, Felitti VJ, Anda RF. Adverse childhood experiences and hallucinations. Child Abuse Negl. 2005;29:797–810. [DOI] [PubMed] [Google Scholar]
- 22. Read J, Argyle N. Hallucinations, delusions, and thought disorder among adult psychiatric inpatients with a history of child abuse. Psychiatr Serv. 1999;50:1467–1472. [DOI] [PubMed] [Google Scholar]
- 23. Janssen I, Krabbendam L, Bak M, et al. Childhood abuse as a risk factor for psychotic experiences. Acta Psychiatr Scand. 2004;109:38–45. [DOI] [PubMed] [Google Scholar]
- 24. Bentall RP, Wickham S, Shevlin M, Varese F. Do specific early-life adversities lead to specific symptoms of psychosis? A study from the 2007 the Adult Psychiatric Morbidity Survey. Schizophr Bull. 2012;38:734–740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Vinkers CH, Van Gastel WA, Schubart CD, et al. The effect of childhood maltreatment and cannabis use on adult psychotic symptoms is modified by the COMT Val158Met polymorphism. Schizophr Res. 2013;150:303–311. [DOI] [PubMed] [Google Scholar]
- 26. van Dam DS, van Nierop M, Viechtbauer W, et al. Childhood abuse and neglect in relation to the presence and persistence of psychotic and depressive symptomatology. Psychol Med. 2015;45:1363–1377. [DOI] [PubMed] [Google Scholar]
- 27. Van Nierop M, Lataster T, Smeets F, et al. Psychopathological mechanisms linking childhood traumatic experiences to risk of psychotic symptoms: analysis of a large, representative population-based sample. Schizophr Bull. 2014;40(suppl 2):123–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Carpenter LL, Tyrka AR, Ross NS, Khoury L, Anderson GM, Price LH. Effect of childhood emotional abuse and age on cortisol responsivity in adulthood. Biol Psychiatry. 2009;66:69–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Dannlowski U, Stuhrmann A, Beutelmann V, et al. Limbic scars: long-term consequences of childhood maltreatment revealed by functional and structural magnetic resonance imaging. Biol Psychiatry. 2012;71:286–293. [DOI] [PubMed] [Google Scholar]
- 30. Read J, Fosse R, Moskowitz A, Perry B, Moskowitz A, Perry B. The traumagenic neurodevelopmental model of psychosis revisited. Neuropsychiatry. 2014:65–79. [Google Scholar]
- 31. Myin-Germeys I, van Os J. Stress-reactivity in psychosis: evidence for an affective pathway to psychosis. Clin Psychol Rev. 2007;27:409–424. [DOI] [PubMed] [Google Scholar]
- 32. Birchwood M, Meaden A, Trower P, Gilbert P, Plaistow J. The power and omnipotence of voices: subordination and entrapment by voices and significant others. Psychol Med. 2000;30:337–344. [DOI] [PubMed] [Google Scholar]
- 33. van Os J, Kapur S. Schizophrenia. Lancet. 2009;374:635–645. [DOI] [PubMed] [Google Scholar]
- 34. Kay SR, Fiszbein A, Opler LA. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–276. [DOI] [PubMed] [Google Scholar]
- 35. Korver N, Quee PJ, Boos HB, Simons CJ, de Haan L. Genetic Risk and Outcome of Psychosis (GROUP), a multi-site longitudinal cohort study focused on gene-environment interaction: objectives, sample characteristics, recruitment and assessment methods. Int J Methods Psychiatr Res. 2012;21:205–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bernstein DP, Stein JA, Newcomb MD, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abus Negl. 2003;27:169–190. [DOI] [PubMed] [Google Scholar]
- 37. Thombs BD, Bernstein DP, Lobbestael J, Arntz A. A validation study of the Dutch Childhood Trauma Questionnaire-Short Form: factor structure, reliability, and known-groups validity. Child Abus Negl. 2009;33:518–523. [DOI] [PubMed] [Google Scholar]
- 38. Bernstein DP, Fink L. Childhood Trauma Questionnaire: A Retrospective Self-Report: Manual. San Antoinio, TX: Psychological Corporation; 1998. [Google Scholar]
- 39. Epskamp S, Cramer AOJ, Waldorp LJ, Schmittmann VD, Borsboom D. qgraph : network visualizations of relationships in psychometric data. J Stat Softw. 2012;48:1–18. [Google Scholar]
- 40. Lauritzen SL, Wermuth N. Graphical models for associations between variables, some of which are qualitative and some quantitative. Ann Stat. 1989;17:1916–1916. [Google Scholar]
- 41. Costantini G, Epskamp S, Borsboom D, et al. State of the {aRt} personality research: {A} tutorial on network analysis of personality data in {R}. J Res Pers. 2015;54:13–29. [Google Scholar]
- 42. Tibshirani R. Regression selection and shrinkage via the lasso. J R Stat Soc B. 1994;58:267–288. [Google Scholar]
- 43. Friedman J, Hastie T, Tibshirani R. Sparse inverse covariance estimation with the graphical lasso. Biostatistics. 2008;9:432–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Chen J, Chen Z. Extended Bayesian information criteria for model selection with large model spaces. Biometrika. 2008;95:759–771. [Google Scholar]
- 45. van Borkulo CD, Borsboom D, Epskamp S, et al. A new method for constructing networks from binary data. Sci Rep. 2014;4:5918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Opsahl T, Agneessens F, Skvoretz J. Node centrality in weighted networks: generalizing degree and shortest paths. Soc Netw. 2010;32:245–251. [Google Scholar]
- 47. Boccaletti S, Latora V, Moreno Y, Chavez M, Hwang D-U. Complex networks: structure and dynamics. Phys Rep. 2006;424:175–308. [Google Scholar]
- 48. Barrat A, Barthélemy M, Pastor-Satorras R, Vespignani A. The architecture of complex weighted networks. Proc Natl Acad Sci USA. 2004;101:3747–3752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Brandes U. On variants of shortest-path betweenness centrality and their generic computation. Soc Netw. 2008;30:136–145. [Google Scholar]
- 50. Dijkstra EW. A note on two problems in connexion with graphs. Numer Math. 1959;1:269–271. [Google Scholar]
- 51.Langley DJ, Wijn R, Epskamp S, van Bork R. Should I get that jab? Exploring influence to encourage vaccination via online social media. ECIS 2015 Research-in-Progress Papers. 2015. Paper 64.
- 52. R Development Core Team R. R: a language and environment for statistical computing. R Found Stat Comput. 2014;1:409. [Google Scholar]
- 53. Fruchterman TMJ, Reingold EM. Graph drawing by force-directed placement. Softw Pract Exp. 1991;21:1129–1164. [Google Scholar]
- 54. Jamshidian M, Jalal S, Jansen C. MissMech: an R package for testing homoscedasticity, multivariate normality, and missing completely at random (MCAR). J Stat Softw. 2014;56:1–31. [Google Scholar]
- 55. Liu H, Lafferty J, Wasserman L. The nonparanormal: semiparametric estimation of high dimensional undirected graphs. J Mach Learn Res. 2009;10:2295–2328. [PMC free article] [PubMed] [Google Scholar]
- 56. Shevlin M, Houston JE, Dorahy MJ, Adamson G. Cumulative traumas and psychosis: an analysis of the national comorbidity survey and the British Psychiatric Morbidity Survey. Schizophr Bull. 2008;34:193–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Glaser JP, van Os J, Portegijs PJM, Myin-Germeys I. Childhood trauma and emotional reactivity to daily life stress in adult frequent attenders of general practitioners. J Psychosom Res. 2006;61:229–236. [DOI] [PubMed] [Google Scholar]
- 58. Lataster T, Dina C, Lardinois M, Valmaggia L, Van Os J, Myin-Germeys I. On the pathway from stress to psychosis. Schizophr Res. 2010;117:182. [Google Scholar]
- 59. Bebbington P, Jonas S, Kuipers E, et al. Childhood sexual abuse and psychosis: data from a cross-sectional national psychiatric survey in England. Br J Psychiatry. 2011;199:29–37. [DOI] [PubMed] [Google Scholar]
- 60. Thewissen V, Bentall RP, Oorschot M, et al. Emotions, self-esteem, and paranoid episodes: an experience sampling study. Br J Clin Psychol. 2011;50:178–195. [DOI] [PubMed] [Google Scholar]
- 61. Ben-Zeev D, Ellington K, Swendsen J, Granholm E. Examining a cognitive model of persecutory ideation in the daily life of people with schizophrenia: a computerized experience sampling study. Schizophr Bull. 2011;37:1248–1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Chapman LJ, Chapman JP, Numbers JS, Edell WS, Carpenter BN, Beckfield D. Impulsive nonconformity as a trait contributing to the prediction of psychotic-like and schizotypal symptoms. J Nerv Ment Dis. 1984;172:681–691. [DOI] [PubMed] [Google Scholar]
- 63. Buyukdura JS, McClintock SM, Croarkin PE. Psychomotor retardation in depression: biological underpinnings, measurement, and treatment. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35:395–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Nanni V, Uher R, Danese A. Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: a meta-analysis. Am J Psychiatry. 2012;169:141–151. [DOI] [PubMed] [Google Scholar]
- 65. Hovens JGFM, Giltay EJ, Wiersma JE, Spinhoven P, Penninx BWJH, Zitman FG. Impact of childhood life events and trauma on the course of depressive and anxiety disorders. Acta Psychiatr Scand. 2012;126:198–207. [DOI] [PubMed] [Google Scholar]
- 66. Leverich GS, McElroy SL, Suppes T, et al. Early physical and sexual abuse associated with an adverse course of bipolar illness. Biol Psychiatry. 2002;51:288–297. [DOI] [PubMed] [Google Scholar]
- 67. Young EA, Abelson JL, Curtis GC, Nesse RM. Childhood adversity and vulnerability to mood and anxiety disorders. Depress Anxiety. 1997;5:66–72. [PubMed] [Google Scholar]
- 68. Herman JL, Perry JC, van der Kolk BA. Childhood trauma in borderline personality disorder. Am J Psychiatry. 1989;146:490–495. [DOI] [PubMed] [Google Scholar]
- 69. Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: a quantitative review of 25 years of research. Psychol Bull. 2006;132:959–992. [DOI] [PubMed] [Google Scholar]
- 70. Read J, Beavan V. Gender and psychosis. In: Read J, Bentall R, Dillon J, eds. Models of Madness: Psychological, Social and Biological Approaches to Psychosis. 2nd ed. London, UK: Routledge; 2013:210–219. [Google Scholar]
- 71. Fisher HL, Craig TK, Fearon P, et al. Reliability and comparability of psychosis patients’ retrospective reports of childhood abuse. Schizophr Bull. 2011;37:546–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Scutari M. Learning Bayesian Networks with the bnlearn R Package. J Stat Softw. 2010;35:1–22.21603108 [Google Scholar]
- 73. Nagarajan R, Scutari M, Lè̀bre S. Bayesian Networks in R : With Applications in Systems Biology. New York, NY: Springer; 2013. [Google Scholar]
- 74. Kalisch M, Fellinghauer BAG, Grill E, Maathuis MH, Mansmann U, Bühlmann P. Understanding human functioning using graphical models. 2010;10:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.