Abstract
Tube-fed elderly patients are generally supplied with the same type of nutrition over long periods, resulting in an increased risk for micronutrient deficiencies. Dietary polyphenols promote immunity and have anti-inflammatory, anti-carcinogenic, and anti-oxidative properties. Carica papaya Linn. is rich in several polyphenols; however, these polyphenols are poorly absorbed from the digestive tract in their original polymerized form. Therefore, we determined the molecular components of a fermented Carica papaya Linn. preparation, as well as its effects on immunity and the composition of gut microbiota in tube-fed patients. Different doses of the fermented C. papaya L. preparation were administered to three groups of tube-fed patients for 30 days. Its effects on fecal microbiota composition and immunity were assessed by 16S rRNA gene sequencing and immune-marker analysis, respectively. The chemical composition of the fermented C. papaya L. preparation was analyzed by capillary electrophoresis- and liquid chromatography- time of flight mass spectrometry. The fermented C. papaya L. preparation restored peripheral blood mononuclear cell (PBMC) cytolytic activity; however, no other biomarkers of immunity were observed. Treatment with the preparation (9 g/day) significantly reduced the abundance of Firmicutes in the fecal microbiota. In particular, treatment reduced Clostridium scindens and Eggerthella lenta in most patients receiving 9 g/day. Chemical analysis identified low-molecular-weight phenolic acids as polyphenol metabolites; however, no polymerized, large-molecular-weight molecules were detected. Our study indicates that elderly patients who are tube-fed over the long-term have decreased PBMC cytolytic activity. In addition, low-molecular-weight polyphenol metabolites fermented from polymerized polyphenols restore PBMC cytolytic activity and modulate the composition of gut microbiota in tube-fed patients.
Introduction
Tube feeding is recommended for patients with swallowing dysfunction and dysphagia associated with conscious disturbances and neural dysfunction, such as cerebrovascular diseases, severe head trauma, and advanced stage neurodegenerative diseases (e.g., Alzheimer’s and Parkinson’s disease). Tube-fed patients are prone to various types of complications such as infectious diseases, particularly of the respiratory system [1–5].
Immunity is regulated by the thymus gland, and thymus gland function is known to gradually decrease with age [6–11]; therefore, the immune system is generally weaker in older patients than in younger patients. Large mononuclear lymphocytes, known as natural killer (NK) cells because of their spontaneous killing of cancer cells and antiviral properties [12–14], are a component of adaptive immunity; it is well known that they exhibit reduced function and altered composition with aging [12,15].
Patients requiring tube feeding are typically provided with a variety of nutrients such as milk proteins, glucose, minerals (Na, K, Mg, Fe, and Zn), vitamins (B1, B2, B12, and E), and polyunsaturated fatty acids. However, there is little or no information regarding the effects of supplementation nutrients on the maintenance and promotion of host immunity to prevent infections and malignancies. Polyphenols are well-known anti-inflammatory and immune-modulatory agents [16,17] that are easily consumed from vegetables, fruits, wheat, tea, and beverages. Elderly patients can maintain immunity by consuming polyphenol-rich fruits and vegetables [18–25].
Commercially available tube-feeding formulas are primarily designed to supply standardized calories, but there is little information on their role in promoting immunity. Tube-fed patients often receive the same nutrients over a long period without daily or seasonal changes. We suggest that altering the micronutrients supplied on a daily basis can improve the immunity of tube-fed patients and prevent infections or malignancies.
Carica papaya L. is traditional medicinal plant rich in many types of polyphenols [26–30]. For example, the papaya fruit exocarp is rich in ferulic acid, caffeic acid, caffeoyl-hexoside, rutin, and quercetin 3-O-rutinoside. Furthermore, the mesocarp contains caffeic acid, caffeoyl-hexoside gallic acid, gallic acid hexoside, protocatechuic acid, protocatechuic acid hexoside, quercetin, myricetin, isorhamnetin, and kaempferol [26].
Fermented papaya preparations (FPPs) have been reported to have anti-inflammatory and immune-modulatory properties in both in vivo and in vitro experiments [31–34].
FPPs are the products of wild unripe C. Papaya L. fermented by Enterococcus faecalis and Aspergillus oryzae. Therefore, FPPs can be considered symbiotic, including both prebiotics and probiotics. Several studies have indicated that live bacteria in probiotics activate human immunity by stimulating the immune system in the colon [35–38].
In the present study, we examined the effects of FPP supplementation for 30 days on immunological and metabolic functions and fecal flora in tube-fed patients; the composition of FPP was also determined by chemical analysis. The results show that FPP enhance NK cell cytotoxicity and decrease the number of Clostridium scindens and Eggerthella lenta in the gut flora of elderly tube-fed patients.
Materials and Methods
Materials
FPPs (SAIDO-PS501, Lot No. S-50330) were obtained from SAIDO Co., Ltd. (Fukuoka, Japan). The juice from wild, whole, unripe, ground, C. papaya L. (including fruit skins and seeds) was extracted in the Philippines and exported to Japan where it was fermented for approximately one year with E. faecalis, followed by approximately six months with A. oryzae, and then dried. Both fermentation processes were conducted at room temperature under aerobic conditions.
Chemical Analysis of FPP Components
The different FPP components were analyzed by capillary electrophoresis-time-of-flight mass spectrometry (CE-TOFMS) and liquid chromatography (LC-TOFMS) from 1 to 5 years after extraction at Human Metabolome Technologies, Inc. (Yamagata, Japan).
For CE-TOFMS measurements, approximately 100 mg of FPP was plunged into 500 μL of methanol containing an internal standard solution (50 μM; #H3304-1002; HMTI) at 0°C. FPPs were then homogenized thrice at 1,500 rpm for 120 sec using a tissue homogenizer (BMS-M10N21; Bio Medical Science Inc. BMS Tokyo, Japan). Then, 200 μL of Milli-Q water and 500 μL of chloroform were added to the samples, thoroughly mixed, and centrifuged for 5 min at 2,300 × g and 4°C. The upper aqueous layer (400 μL) was centrifugally filtered through a Millipore 5 kDa-cutoff filter to remove the proteins. The filtrate was then lyophilized and suspended in 50 μL of Milli-Q water and analyzed by CE-TOFMS.
For LC-TOFMS measurements, approximately 100 mg of FPP was plunged into 500 μL of methanol containing an internal standard solution (20 μM; #H3304-1002; HMTI) at 0°C to inactivate enzymes. The tissue was homogenized twice at 1,500 rpm for 120 sec using a tissue homogenizer (BMS·M10N21). The mixture was centrifuged at 2,300 × g at 4°C for 5 min. The supernatant was desiccated and then dissolved with 100 μL of 50% isopropanol /Milli-Q water for LC-TOFMS analysis at Human Metabolome Technologies, Inc.
The CE and -LC-TOFMS data were analyzed by Human Metabolome Technologies, Inc., using Master Hands automatic-integral analysis software (ver. 2.9.0.9, Keio University, Tsuruoka, Japan).
The mass-to-change ratio (m/z), migration time (MT), and relative peak area were obtained from the peak values. The relative peak area was computed with the following equation: Peak area ratio = targeted peak area/internal standard peak area.
Clinical Study
Patients
Study participants included 8 males (mean age 77 ± 10.6, range 67–96 years) and 12 females (mean age 89 ± 5.8, range 77–97) patients with cerebrovascular disease (n = 12, 4 males and 8 females), neurodegenerative disease (n = 7, 4 males and 3 females), and post-traumatic head injury (n = 1, male). Study participants had been tube-fed for 1–7 years. The study protocol was approved by the human ethics committees of Yuno Onsen Hospital, and written consent for the study was obtained from a family member of each patient.
FPP treatment
Study participants were divided into three groups, including a control group that did not receive FPP (n = 5); the remaining two groups were administered 3 g FPP/day (n = 7) or 9 g FPP/day (n = 8). Treatments were administered once (3 grams) per day or 3 times (3 grams each) per day for 30 consecutive days.
Laboratory examination
Blood samples were collected and sent in cooling boxes within 24 h to BioMedical Laboratory (BML, Tokyo, Japan) for analysis. Samples were analyzed for peripheral blood mononuclear cell (PBMC) count, total serum protein, serum albumin, serum globulin, and liver function (total bilirubin, glutamic oxaloacetic transaminase (GOT), guanosine triphosphatase (GPT), gamma glutamyl-transpeptidase (γGTP), alkaline phosphatase (ALP), cholinesterase, leucine aminopeptidase (LAP), and lactic acid dehydrogenase (LDH)). In addition, renal function (blood urea nitrogen (BUN), creatinine, and uric acid) and lipid metabolites (total cholesterol (T-ch), high density lipoprotein (HDL), low density lipoprotein (LDL), and triglycerides (TG)) were studied using Roche Reflotron system kits (Roche Diagnostics Co., Ltd.). Serum electrolytes, as well as cellular and humoral immunity were additionally analyzed. IgG, IgA, and IgM were assayed using immunoglobulin kits from NITTOBO Medical (Koriyama, Japan); interleukins (IL-2, IL-6, and IL-10) and chemokines (interferon γ (IFN-γ) and tissue necrosis factor α (TNF-α)) were assayed by a quantitative enzyme immunoassay technique using a MXL (Dynex Technologies, Chantilly, VA, USA).
Cell isolation
PBMCs were isolated from peripheral blood (diluted 1.6 times with 10% phosphate buffered saline) by density gradient centrifugation (800 × g for 25 min at room temperature) over Isolymph (specific gravity 1.077) (CT Scientific Supply Corp., Deer Park, NY, USA) in Leucosep tubes (Greiner Bio-One, Tokyo Japan) for use in the NK cell activity assay. The supernatant (isolated PBMCs) was washed twice with saline solution and the efficiency of cell separation was confirmed by flow-cytometry (Accuri C6, Becton Dickinson and -Company, Franklin Lakes, NJ, USA).
Cytotoxicity assay
A 51Cr release assay was used to measure PBMC cytolytic activity; target cells (K562) were labeled with 100 μCi 51CrO4 (Perkin Elmer, Japan) for 60 min at 37°C in atmosphere of 5% CO2 in air. Labeled K562 target cells were adjusted to 2 x 105 cells/mL in RPMI-1640 medium supplemented with 10% fetal bovine serum. K562 (1 x 105 cells/well) and effector cells (1 x 104 PBMC/well) at 1:10 and 1:20 effector/target (E: T) ratios were co-incubated in 200 μL of RPMI-1640 in 96-well U-bottomed plates in triplicate for 4 h at 37°C and 5% CO2 in air. Radioactivity was measured with a gamma scintillation counter (Perkin Elmer, Japan). The percentage of cytotoxic activity was calculated using the following formula:
specific lysis (%) = (sample cpm–spontaneous cpm)/(maximal cpm–spontaneous cpm) * 100 Large mononuclear lymphocytes have cytolytic activity against malignant tumor cells. The cytolytic activity of PBMCs against malignant cells such as K564 depends almost entirely on NK cell cytotoxicity [39]; therefore, we expressed NK cell cytotoxicity as cytolytic activity of PBMCs.
Fecal Flora Analysis
Fecal bacterial composition was analyzed before and after administration of FPP and in the control group by high-throughput sequencing of 16S rRNA gene fragments amplified from each stool sample [40]. Briefly, whole genomic DNA was extracted from the stool samples by the bead-beating method [41] and the V6–V8 variable region of the 16S rRNA gene was amplified by PCR with universal primers Q-968F and Q-1390R, each carrying a barcode label sequence. The amplified fragments were mixed and applied to the pyrotag sequence using Roche 454 GS FLX Titanium system. The obtained sequences were processed by the QIIME 1.7.0. pipeline [42] equipped with USEARCH ver. 5.2.236 [43,44] for barcode splitting, denoising, chimera removal, and construction of operational taxonomic units (OTUs). Consequently, 568 OTUs, comprising 182,834 reads (mean ds/sample 3975 ± 680, minimum = 2117), were considered to be a non-redundant set of OTUs. The reads were subsampled for adjustment to 2,000 reads/sample. The taxonomy of each OTU was assigned using the RDP classification in the QIIME pipeline based on the Greengenes taxonomy (97 OTU taxonomy) and the Greengenes reference database (97 OTUs, FASTA) [45]. To search for closest species, the representative sequence of each OTU was subjected to RDP Seqmatch [46] in the Ribosomal Database Project II (http://rdp.cme.msu.edu/seqmatch/seqmatch.intro.jsp), in which the lower threshold of the Sab score was set to 0.84. If more than two species showed the same highest scores, the one with the highest count among the top 20 matches was selected for annotating the species by using a Microsoft Excel macro file named Seqmatch Q400 [47]. The bacterial composition of each fecal sample was determined at each taxonomic rank according to the OTU table and the taxonomic information of each OTU.
Statistical Analysis
All data are expressed as the mean ± SD. Differences between groups were compared using the Student’s t-test or analysis of variance (ANOVA). Differences were considered significant when P < 0.05.
Results
FPP Stimulates NK Cell Activity
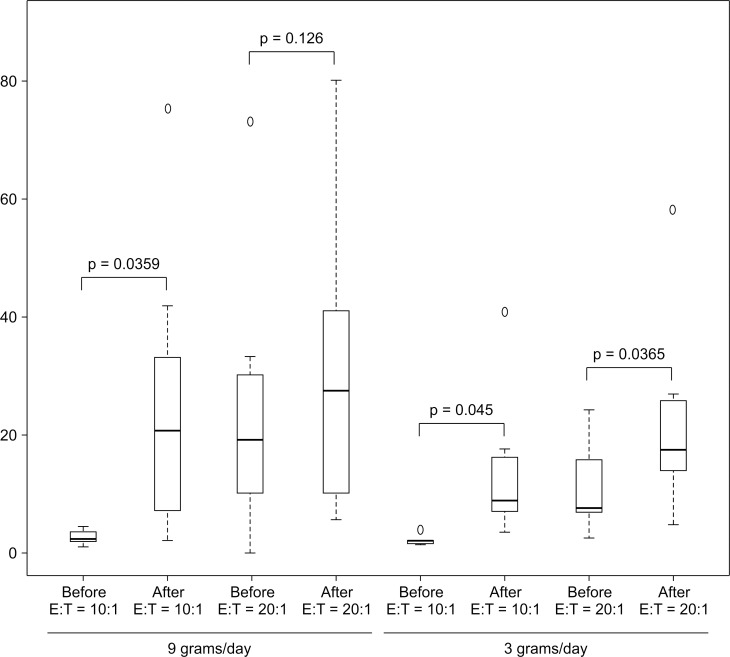
Administration of FPP at 3 and 9 g/day at an E: T ratio of 10:1 significantly increased NK cell cytotoxicity, whereas administration of FPP at an E: T ratio of 20:1 tended to increase the activity, although it did not reach significance. However, FPP administration at these doses did not affect IgG, IgA, and IgM levels (Table 1, Fig 1).
Table 1. PBMC cytolytic activity (NK cell activity) induced by FPP administration for 30 days*.
| PBMC cytolytic activity [10:1 (8.9–29.5), 20:1 (17.1–48.7)] | IgG (820–1740) | IgA (90–400) | IgM [♂(31–200), ♀(52–270)] | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| before | after | P value | before | After | P | before | after | P | before | After | P | |
| 9 g/day | 2017±682 | 2119±827 ±±827 | 0.19 | 360±82 | 364±103 | 0.73 | 123±100 | 120±86 | 0.69 | |||
| E:T = 10:1 | 2.9±1.1 | 25.0±16.6 | 0.035 | |||||||||
| E:T = 20:1 | 24.2±22.6 | 30.6±25.1 | 0.126 | |||||||||
| 3 g/day | 1731±506 | 1697±512 | 0.30 | 454±189 | 436±196 | 0.09 | 106±67 | 101±60 | 0.07 | |||
| E:T = 10:1 | 2.2±0.7 | 14.4±12.7 | 0.045 | |||||||||
| E:T = 20:1 | 11.6±8.3 | 23.0±17.3 | 0.036 | |||||||||
| Control | No FPP | for 30 days | 1551±198 | 1533±280 | 0.81 | 500±197 | 506±207 | 0.81 | 74±9 | 64±12 | 0.01 | |
| E:T = 10:1 | 2.7±0.9 | 7.4±4.9 | 0.088 | |||||||||
| E:T = 20:1 | 10.0±7.1 | 13.8±7.9 | 0.256 | |||||||||
*Data in parentheses are normal values for 20–65-year-old healthy subjects.
Fig 1. NK cell cytotoxicity induced by FPP administration for 30 days.
It has been reported that cytokines and chemokines released in response to lipopolysaccharide (LPS) from the cell membrane of gram-negative bacteria stimulate NK cell activity through dendritic cell (DC) toll-like receptors (TLRs) of intestinal epithelium [48–53]; however, administration of FPP did not affect the level of cytokines or chemokines analyzed in the present study (Table 2).
Table 2. Changes in cytokines and chemokines following FPP administration for 30 days*.
| IL-2 (<5) | IL-6 (<6) | IL-10 (<8) | INF-γ (<7.8) | TNF-α (<2.8) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| before | after | before | after | before | after | before | after | Before | after | |
| 9 g/day | all cases <5 | all cases <5 | all cases <6 | all cases <6 | all cases <8 | all cases <8 | all cases <7.8 | all cases <7.8 | 2.16±0.7 | 2.89±1.2 |
| P value | ns | ns | ns | ns | 0.98 | |||||
| 3 g/day | all cases <5 | all cases <5 | all cases <6 | all cases <6 | all cases <8 | all cases <8 | all cases <7.8 | all cases <7.8 | 2.17±0.7 | 2.17±0.8 |
| P value | ns | ns | ns | ns | 0.97 | |||||
*Data in parentheses are normal values for 20–65-year-old healthy subjects. ns: not significant
These results suggest that FPPs directly influence NK cells in the peripheral blood rather than through LPS-activated TLRs on the intestinal epithelium. FPP administration did not alter the levels of lipid metabolite biomarkers (T-Ch, LDL, and HDL) or markers of inflammation (leukocyte count, monocytes, and c-reactive protein (CRP)) (Tables 3 and 4). It is possible, however, that FPP-induced changes were too small to be detected by our methods.
Table 3. Changes in lymphocytes, monocytes, and CRP following FPP administration for 30 days*.
| Normal Value range | Before | After | P value | |
|---|---|---|---|---|
| Lymphocyte | (18.0–50.0) | |||
| 9 g/day | 31.9±5.6 | 32.9±7.3 | 0.64 | |
| 3 g/day | 42.8±6.3 | 38.4±7.0 | 0.040* | |
| control | 23.2±1.8 | 25.0±5.8 | 0.49 | |
| Monocyte | (1.0–8.0) | |||
| 9 g/day | 5.9±0.7 | 6.8±1.1 | 0.07 | |
| 3 g/day | 6.1±1.0 | 6.7±0.9 | 0.24 | |
| control | 5.5±1.3 | 5.0±1.3 | 0.80 | |
| CRP | (<0.3) | |||
| 9 g/day | 1.3±0.9 | 0.9±0.5 | 0.48 | |
| 3 g/day | 0.5±0.3 | 0.3±0.1 | 0.17 | |
| control | 0.7±0.7 | 2.1±4.0 | 0.41 |
*Data in parentheses are normal values for 20-65-year-old healthy subjects.
*P < 0.05.
Table 4. Changes in lipid metabolites following FPP administration for 30 days*.
| Lipid metabolites | Before | After | P value | |
|---|---|---|---|---|
| T-ch | (150–219) | |||
| 9 g/day | 178±25 | 181±26 | 0.49 | |
| 3 g/day | 174±29 | 178±26 | 0.12 | |
| HDL | (males 40–80) | |||
| (females 40–90) | ||||
| 9 g/day | 42±12 | 45±12 | 0.16 | |
| 3 g/day | 56±13 | 60±16 | 0.06 | |
| LDL | (70–139) | |||
| 9 g/day | 109±15 | 112±20 | 0.51 | |
| 3 g /day | 99±22 | 99±23 | 0.90 | |
| LDL/HDL ratio | (<2) | |||
| 9 g/day | 2.7±0.8 | 2.6±0.7 | 0.79 | |
| 3 g/day | 1.8±0.5 | 1.7±0.6 | 0.17 | |
| TG | (50–149) | |||
| 9 g/day | 154±82 | 127±51 | 0.12 | |
| 3 g/day | 74±18 | 78±20 | 0.11 |
*Data in parentheses are normal values for 20-65-year-old healthy subjects.
Chemical Analyses
CE-TOFMS and LC-TOFMS analyses identified seven low-molecular-weight phenolic acids in the FPP (Table 5); we did not detect significant levels of homovanillic and m-phenolic acid in FPP fermented for less than one year (Table 5). In addition to those listed in Table 5, we identified several other types of organic acids such as lactic acid, various amino acids, and nucleic acids.
Table 5. List of primary phenolic acids analyzed by CE- and LC-TOFMS.
| Phenolic acids | Lot No. | ||||||
|---|---|---|---|---|---|---|---|
| 060123 | 070122 | 080121 | 090119 | 100118 | 110124 | 120116 | |
| 2-Hydroxy-4-methylvaleric acid | 1.1E-05 | 9.9E-05 | 7.4E-05 | 9.1E-05 | 1.0E-05 | 6.7E-05 | 5.7E-05 |
| m-Hydroxybenzoic acid | 6.2E-05 | 3.7E-05 | 5.4 E-05 | 5.5E-05 | 6.2E-05 | 8.8E-05 | 2.7E-05 |
| 2,5-Dihydroxybenzoic acid | 5.7E-04 | 3.0E-04 | 4.8E-04 | 5.1E-04 | 6.6E-04 | 8.8E-04 | 2.6E-04 |
| Shikimic acid | 4.9E-06 | 5.2E-06 | 7.7E-06 | 6.3E-06 | 1.2E-05 | 8.6E-06 | 7.1E-06 |
| Hippuric acid | 1.4E-05 | 1.3E-05 | 1.3E-05 | 1.9E-05 | 1.5E-05 | 1.5E-05 | 1.1E-05 |
| Homovanillic acid | 4.7E-05 | 3.0E-05 | 3.9E-05 | 3.0E-05 | 4.2E-05 | 4.8E-05 | N.D. |
| Quinic acid | 1.0E-04 | 6.2E-05 | 6.4E-05 | 5.2E-05 | 7.5E-05 | 1.1E-04 | 1.6E-04 |
| m-Aminophenol | 6.1 E-05 | 3.7E-05 | 3.5E-05 | 3.2E-05 | 2.5E-05 | 2.5E-05 | N.D. |
The first two numbers included in the Lot No. indicate the production year (e.g., 060123 is January 23, 2006).
Numbers in the table indicate relative peak area of phenolic acids.
E: exponential, ND: not detected
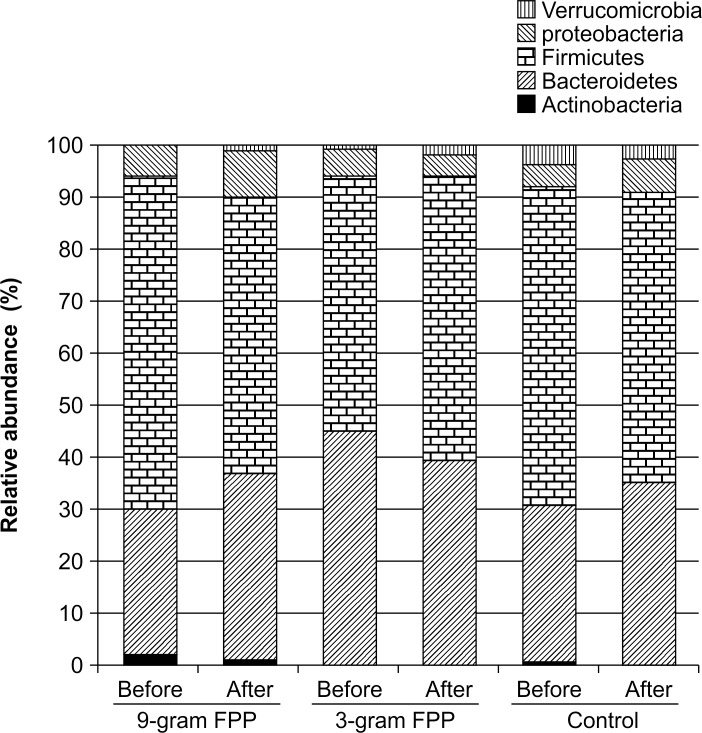
Composition of Fecal Microbiota
Analysis of fecal samples in the control group and at baseline in the FPP groups showed characteristic microbiota with a high proportion of phylum Firmicutes (mean = 57.9%, Fig 2) and genus Parabacteroides (mean = 21.2%), and with a low proportion of genus Bifidobacterium (mean = 0.97%). At baseline (before the administration of FPP), bifidobacteria were detected in only 3 out of the 21 tested subjects.
Fig 2. Change in bacterial composition at the phylum level following FPP administration for 30 days.
Stool samples were collected before and after the administration of FPP. Bacterial compositions were analyzed by pyrotag sequencing of 16S rRNA genes. The average relative abundance of OTUs for each phylum per treatment group is shown.
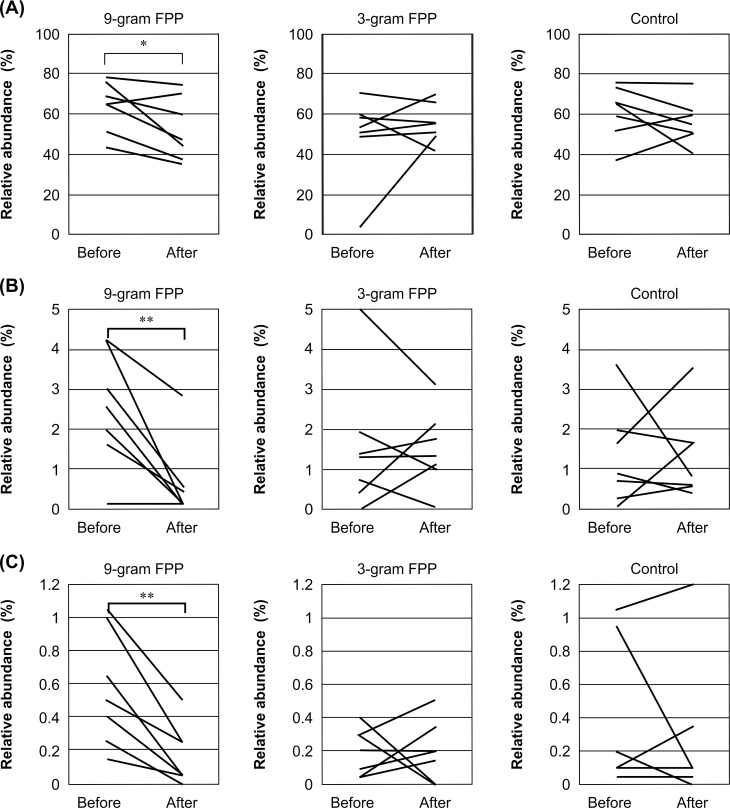
After administration of FPP, the abundance of Firmicutes was significantly decreased (P < 0.05, Student’s t-test) (Table 6, Figs 2 and 3A). In particular, administration of FPP at 9 g/day reduced the level of OTU308, which is closely related to C. scindens (Fig 3B), in all subjects but one. The levels of OTU58, which is closely related to E. lenta (Fig 3C), were also reduced after FPP administration. Interestingly, FPP administration decreased the offensive fecal odor.
Table 6. Effects of FPP on fecal microbiota.
| Taxonomy | Overall average | FPP at 9 g/day | FPP at 3 g/day | Control group | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| before | after | P value | before | after | P value | before | after | P value | ||
| Phylum | ||||||||||
| Firmicutes | 55.09 | 63.72 | 52.96 | 0.05 | 49.13 | 55.32 | 0.11 | 50.89 | 55.94 | 0.34 |
| Proteobacteria | 6.23 | 5.19 | 8.43 | 0.06 | 5.14 | 3.33 | 0.43 | 4.32 | 5.66 | 0.13 |
| Class | ||||||||||
| 4Cod-2 | 0.24 | 0.05 | 0.36 | 0.091 | 0.11 | 0.34 | 0.170 | 0.02 | 0.56 | 0.349 |
| Clostridia | 49.30 | 56.14 | 47.03 | 0.067 | 42.60 | 46.87 | 0.461 | 53.46 | 49.68 | 0.394 |
| Bacilli | 1.51 | 1.91 | 0.54 | 0.229 | 0.54 | 0.34 | 0.094 | 2.89 | 2.86 | 0.936 |
| Family | ||||||||||
| Coriobacteriaceae | 1.00 | 0.66 | 0.21 | 0.003* | 0.61 | 0.76 | 0.310 | 2.32 | 1.43 | 0.251 |
| Enterococcaceae | 1.08 | 1.89 | 0.16 | 0.096 | 0.34 | 0.26 | 0.245 | 1.44 | 2.41 | 0.356 |
| Porphyromonadaceae | 20.39 | 15.46 | 23.77 | 0.089 | 33.56 | 22.56 | 0.177 | 14.73 | 12.46 | 0.546 |
| Ruminococcaceae | 13.08 | 14.92 | 11.55 | 0.100 | 11.43 | 13.83 | 0.120 | 14.29 | 12.46 | 0.167 |
| Veillonellaceae | 1.95 | 1.15 | 1.14 | 0.095 | 2.02 | 2.66 | 0.240 | 1.63 | 2.10 | 0.338 |
| Genus | ||||||||||
| Anaerofustis | 0.01 | 0.02 | 0.00 | 0.078 | 0.00 | 0.01 | 0.356 | 0.04 | 0.00 | 0.172 |
| Anaerotruncus | 0.26 | 0.16 | 0.16 | 0.923 | 0.33 | 0.61 | 0.057 | 0.16 | 0.16 | 1.000 |
| Bilophila | 0.16 | 0.10 | 0.24 | 0.066 | 0.06 | 0.06 | 1.000 | 0.17 | 0.31 | 0.416 |
| Blautia | 7.16 | 8.74 | 3.82 | 0.015* | 7.41 | 6.17 | 0.205 | 11.87 | 4.96 | 0.102 |
| Eggerthella | 0.33 | 0.60 | 0.20 | 0.004* | 0.22 | 0.22 | 1.000 | 0.41 | 0.30 | 0.434 |
| Enterococcus | 1.08 | 1.89 | 0.16 | 0.096 | 0.34 | 0.26 | 0.245 | 1.44 | 2.41 | 0.356 |
| Parabacteroides | 20.34 | 15.46 | 23.77 | 0.089 | 33.35 | 22.54 | 0.177 | 14.67 | 12.04 | 0.518 |
Taxonomic groups showing significant (P < 0.1) population changes after 30-day administration of FPP are listed.
*P < 0.05.
Fig 3.
Change in abundance of Firmicutes (A), OTU308 (C. scindens) (B), and OTU58 (E. lenta) (C). The relative abundance in each sample is plotted. Stool samples were collected before and after the administration of FPP and their bacterial compositions were analyzed by pyrotag sequencing of 16S rRNA genes. Data from the same subject are connected by a line. *P < 0.05 and **P < 0.01 (paired Student’s t-test)
Bacteria in FPPs were analyzed by high-throughput sequencing of amplified 16S rRNA gene fragments. No living bacteria (e.g., E. faecalis and A. oryzae used for fermentation) were found in the FPP incubation medium.
Discussion
The tube fed patients included in this study have chronic inflammatory diseases in addition to their primary diagnoses, as indicated by laboratory inflammatory biomarkers such as elevated CRPs (Table 3).
Many reports have demonstrated the anti-inflammatory effects of several polyphenols [16,17]. Most studies analyzing polyphenols are in vitro studies, with limited research in animals and only a few studies in humans. Therefore, many questions about the clinical effects of polyphenols remain unanswered. In fact, there is no information regarding the in situ chemical structure, effective dosage, absorption, and metabolism of most FPPs. To our knowledge, the present study is the first to evaluate the clinical effects of FPPs in tube-fed patients.
Effect of FPP on Immunity
Clinical laboratory effects of FPP administration revealed changes in PBMC cytolytic activity only, which are primarily dependent on the function of NK cell cytotoxicity (as discussed in Materials and Methods) and on the microbiota in feces. Here, we consider PBMC cytolytic activity to be representative of the effects of FPP on NK cell cytotoxicity.
Our results indicate that before FPP administration, NK cell cytotoxicity (cytolytic activity) was lower (E: T = 10:1, 2.56 ± 9.0; 20:1, 24.95 ±15.3) in elderly patients (67–97 years of age) than healthy controls aged 20–60 years (E: T = 10:1, 8.9 ~ 29.5; 20:1, 171 ~ 47.8) (Table 1). NK cell cytotoxicity increased after administration of FPP in a dose-dependent manner, although the effect was not statistically significant because of differences between strong and poor responders.
It is reported that the number of NK cells increases and their components change (e.g., CD56 increases) in the elderly; however, NK cell cytotoxicity decreases [54–56]. Decreased NK cell cytotoxicity in the elderly is not dependent on NK cells, but rather on the host environment [57]; however, the decrease observed in this study was not restored by IL-15/IL-15R mediated by IL-2 [57,58]. These experiments suggest that the decrease in NK cell cytotoxicity may be caused by the environment surrounding the aged NK cells and/or intracellular events such as energy production and signal trafficking, rather than by the NK cells themselves. NK cells are activated in the presence of LPS released from probiotics, which is accompanied by changing cytokines and chemokines. LPS stimulates TLR-4 in colon membrane DCs and enhances the expression of interferon-γ (INF-γ) and tumor necrosis factor-α (TNF-α), which in turn stimulates NK cell surface receptors [59–61]. In our study, however, NK cell activity was enhanced by FPPs without upregulation of IL-2, IL-6, IL-10, INF-γ, or TNF-α (Tables 1–3) (Fig 1). In addition, there were no observed increases in gram-negative bacteria (Lactococcus and Bifidobacteroides), which are found in probiotics and reported to be stimulators of TLR-4, or living bacteria (E. faecalis and A. oryzae used for fermentation) in FPP, as determined by 16S rRNA analysis of the incubation media.
These results suggest that FPP do not increase NK cell cytotoxicity by activating cytokines. Studies have shown that polyphenols (epigalocatechin gallate, oenothelin B, ellagitanin, and resveratrol) augment NK cell cytotoxicity [62–65]; however, a study of hesperidin showed no effects in healthy, well-nourished humans [62]. In an in vitro study, INF-γ concentrations were increased after treatment with resveratrol; however, because the study was done in a cell culture system, release of INF-γ was likely the result of NK cell activation [66]. While treatment with FPP augmented NK cell cytotoxicity in elderly patients, it is possible that it has no effect on NK cell cytotoxicity in healthy young people, as observed for hesperidin [62].
Further studies are needed to determine which low-molecular-weight phenolic acids, phenolic acid combinations, or ratios are most effective for activating NK cells without activating cytokines and chemokines or increasing the frequency of NK cells.
Molecular Structure/function Relationship, Absorption, and Effective Dosage
Bioactive polyphenols are polymerized large molecules and not easily absorbed from digestive tracts as their original large molecules; therefore, FPP bioactivity, molecular structure/function relationship, and absorption are important considerations. There are many reports of in vivo and in vitro experiments showing that low-molecular-weight phenolic acids have various bioactivities, including antioxidant activity [25–29]; however, these studies do not indicate the bioactive molecular structure/functional relationships.
FPP contains single phenolic acids and many kinds of low-molecular-weight substances, but no polymerized structures; however, these low-molecular-weight substances behave similar to polymerized polyphenols in vivo.
There are relatively few reports that studied the relationship between the molecular structure and biological activity of polyphenols as whole a molecule [66–68]. Park et al. [67] reported differences between monomeric, dimeric, and trimeric flavonoids in nitric oxide (NO) production, TNF-α secretion, and NF-κB-dependent gene expression in RAW 254.7 macrophages. These responses were repressed by monomers and dimers, but enhanced by trimers. However, these experiments were conducted in vitro, and further in vivo studies are needed to confirm these findings in animals and humans.
Williamson et al. [68] suggested that colonic catabolites of orally administered polyphenols are the “missing” compounds, and that they are potentially important compounds that mediate some of the biological activities and health benefits of polyphenol-rich foods.
The chemical structure and effective dosage of functional candidate compounds are different in vivo from that in vitro. The majority of polyphenols are broken down and absorbed in the intestines by intestinal microflora, suggesting that the original structures of polyphenols do not necessarily mediate their functions in vivo.
The level of polyphenols such as procyanidins, chlorogenic acids, and anthocyanins are lower in peripheral blood than that of other flavonoids, even after administration of high doses or consumption of large amounts of foods rich in these compounds [69]. In this regard, several studies have investigated the absorption and metabolism of certain flavonoids such as quercetin and (-)-epicatechin [62]. Intervention studies involving consumption of procyanidin-, chlorogenic acid-, or anthocyanidin-rich foods have shown that these foods do not change the levels of certain biomarkers [70,71]. However, these results could be explained by the low blood concentrations of parent compounds and their failure to affect the levels of these biomarkers [72,73]. Based on the effective doses in vivo, these reports also indicated that the effects of polymerized polyphenols do not necessarily resemble those of the original chemical structure.
Polyphenols are primarily absorbed from the large intestine (90–95%), although some are absorbed from the small intestine (5–10%) [74–87]. Interestingly, the concentration of excreted polyphenols in urine and feces is less than the amount ingested [72]. This fact indicates that a large percentage of consumed polyphenols is metabolized to small molecules and absorbed; the metabolites are then consumed in biological reactions.
These studies suggest that the low-molecular-weight phenolic acids in FPP have the same bioactivities as the original polymerized polyphenols in C. papaya L.
Fermentation of Polyphenols
C. papaya L. is fermented under aerobic conditions; aerobic metabolites are different from those formed under anaerobic conditions, such as in the colon. The polyphenol catabolites of aerobic fermentation exert better biological effects than the polyphenols in grapes [85]. Several studies have demonstrated that fermentation enhances polyphenol bioactivity [86–88], suggesting that fermentation results in the conversion of polyphenols with large molecular weights to compounds of low molecular weight, which have more biological activity. Under aerobic conditions where fermentation is influenced by oxygen, oxidized structures are generated, giving rise to lower-molecular-weight compounds that are converted into mono-aromatic acids and CO2 [89].
Prebiotic Effects of FPP on Colonic Flora
The type and amount of food consumed daily, such as volume of fiber, may explain the profile of fecal microflora of FPP. Daily recommendations in Japan (version 2010) include consumption of more than 17 g/day of dietary fiber. Our tube-fed patients receiving FPP were supplied with approximately 17 g/day of fiber. Commercially available tube nutrition includes an average of 1.5 g fiber/100 kcal/100 g and provide from 800 to 1,000 kcal. Therefore, dietary fiber deficiencies are not likely to be the reason for the characteristic features of fecal microflora described in this study. FPP did not increase Bifidobacterium or decrease Bacteroidetes, but significantly reduced the abundance of Firmicutes, particularly the class Clostridia, including E. lenta and C. scindens (Table 6). These results suggest that bile acids are decreased, as supported by a previous study showing the outgrowth of Clostridia in rats fed high concentrations of bile acids [90].
Polyphenols and/or their catabolites could alter the composition of gut microflora by reducing the colonic pH value, suppressing Bacteroidetes and pathogenic Clostridium perfringens and Clostridium difficile, and increasing the proportion of Bifidobacteria and eubacteria without inhibiting lactic acid bacteria [91,92]. Gallic acid and caffeic acid have been reported to repress Clostridium and Bacteroides species [93]. These effects were also observed in our study, although the exact mechanisms are not yet clear. Our results indicate that low-molecular-weight phenolic acids in FPP affect the composition of colon microflora similarly to polymerized polyphenols.
The (C6-C1) low-molecular-weight polyphenol catabolites (e.g., protocatechuic acid) reduce serum levels of total cholesterol, LDL, and HDL in overloaded rats [94,95]. Data from animal and in vitro studies suggest that (C6-C2) and especially (C6-C3) [96,97] catabolites interfere with various enzymes in the mevalonate pathway. For example, 3-hydroxy-3-methylglutaryl-CoA reductase reduced glucose levels in an experimental type II diabetes animal model [98,99]. These experiments were performed in overloaded animals and rats with genetically induced diabetes. Our study, however, showed no changes in lipid metabolism after administration of FPP. Elderly tube-fed patients are often discouraged from consuming cholesterol-rich and fat-rich nutrients or excessive calories. Fig 2 indicates that tube-fed patients are typically supplied with the same kind of artificial nutrition over long periods without supplementary natural probiotic foods or are treated frequently with antibiotics against repeated infections. Our results suggest that FPP and probiotic supplementation is useful for tube-fed patients to maintain a healthy immune status.
Conclusions
Our results show that older patients who are tube-fed over the long term have decreased NK cell toxicity, and that low-molecular-weight phenolic acids produced by the fermentation of polymerized large molecular weight polyphenols are bioactive. In addition, these low-molecular-weight phenolic acids exert their effects, such as increasing NK cell activity, without causing hypercytokinemia, hyperchemokinemia, or changing the components of the gut microbiota.
The present study does have limitations. For example, we did not classify NK cell frequency, which may further explain our results showing enhanced NK cell cytotoxicity. C. papaya L. is not the only source of polyphenols, with many polymerized large molecular weight polyphenols existing in the plant world; however, most of them are difficult to digest or absorb. Consequently, development of fermentation biotechnology of polymerized large molecular weight polyphenols may introduce useful low-molecular-weight phenolic acids with improved absorption and human health benefits.
Acknowledgments
We had a significant amount of help from the Nutrition Support Team at Yuno Onsen Hospital. We also thank Science Technology Interact Co., Ltd. for management of this collaboration and Dr. Tomoko Hidaka and Mrs. Megumi Iwata from Kyushu University for 16S rRNA sequencing. We would like to thank Editage (http://www.editage.jp) for English language editing.
Data Availability
All relevant data are within the paper.
Funding Statement
The authors received financial support from SAIDO Co., Ltd. for this work. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Marik PE, Kaplan D. Aspiration pneumonia and dysphagia in the elderly. Chest. 2003;124: 328–336. [DOI] [PubMed] [Google Scholar]
- 2.Nakajoh K, Nakagawa T, Sekizawa K, Matsui T, Arai H, Sasaki H. Relation between incidence of pneumonia and protective reflexes in post-stroke patients with oral or tube feeding. J Intern Med. 2000;247: 39–42. [DOI] [PubMed] [Google Scholar]
- 3.Park RH, Allison MC, Lang J, Spence E, Morris AJ, Danesh BJ, et al. Randomised comparison of percutaneous endoscopic gastrostomy and nasogastric tube feeding in patients with persisting neurological dysphagia. BMJ. 1992;304: 1406–1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baeten C, Hoefnagels J. Feeding via nasogastric tube or percutaneous endoscopic gastrostomy: a comparison. Scand J Gastroenterol. 1992;194: s95–s98. [DOI] [PubMed] [Google Scholar]
- 5.Amadori A, Zanovello P, Cozzi E, Ciminale V, Borghesan F, Fagiolo U, et al. Study of some early immunological parameters in aging humans. Gerontology. 1988;34: 277–283. [DOI] [PubMed] [Google Scholar]
- 6.Miller RA. Aging and immune function: cellular and biochemical analyses. Exp Gerontol. 1994;29: 21–35. [DOI] [PubMed] [Google Scholar]
- 7.Patel HR, Miller RA. Age-associated changes in mitogen-induced protein phosphorylation in murine T lymphocytes. Eur J Immunol. 1992;22: 253–260. 10.1002/eji.1830220137 [DOI] [PubMed] [Google Scholar]
- 8.Hirokawa K, Utsuyama M, Katsura Y, Sado T. Influence of age on the proliferation and peripheralization of thymic T cells. Arch Pathol Lab Med. 1988;112: 13–21. [PubMed] [Google Scholar]
- 9.Goodwin JS, Searles RP, Tung KS. Immunological responses of healthy elderly population. Clin Exp Immunol. 1982;48: 403–410. [PMC free article] [PubMed] [Google Scholar]
- 10.Meydani SN, Wu D, Santos MS, Hayek MG. Antioxidants and immune response in aged persons: overview of present evidence. Am J Clin Nutr. 1995;62: 1462S–1476S. [DOI] [PubMed] [Google Scholar]
- 11.Qureshi AA, Khan DA, Mahjabeen W, Papasian CJ, Qureshi N. Suppression of nitric oxide production and cardiovascular risk factors in healthy seniors and hypercholesterolemic subjects by a combination of polyphenols and vitamins. J Clin Exp Cardiol. 2012;7: s5–s8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Itoh K, Suzuki R, Umezu Y, Hanaumi K, Kumagai K. Studies of murine large granular lymphocytes. II. Tissue, strain, and age distributions of LGL and LAL. J Immunol. 1982;129: 395–405. [PubMed] [Google Scholar]
- 13.Pross HF, Jondal M. Cytotoxic lymphocytes from normal donors. A functional marker of human non-T lymphocytes. Clin Exp Immunol. 1975;21: 226–235. [PMC free article] [PubMed] [Google Scholar]
- 14.Kumagai K, Itoh K, Suzuki R, Hinuma S, Saitoh F. Studies of murine large granular lymphocytes. I. Identification as effector cells in NK and K cytotoxicities. J Immunol. 1982;129: 388–394. [PubMed] [Google Scholar]
- 15.Facchini A, Mariani AR, Papa S, Vitale M, Manzoli FA. Increased number of circulating Leu 11+ (CD16) large granular lymphocytes and decreased NK activity during human ageing. Clin Exp Immunol. 1987;68: 340–347. [PMC free article] [PubMed] [Google Scholar]
- 16.González-Gallego J, García-Mediavilla MV, Sánche-Campos S, Tuñón MJ. Fruits polyphenol, immunity and inflammation. Br J Nutr. 2010;104: S15–S27. 10.1017/S0007114510003910 [DOI] [PubMed] [Google Scholar]
- 17.González-Gallego J, Sánche-Campos S, Tuñón MJ. Anti-inflammatory properties of dietary flavonoids. Nutr Hosp. 2007;22: 287–293. [PubMed] [Google Scholar]
- 18.Magrone T, Jirillo E. Disorders of innate immunity in human ageing and effects of nutraceutical administration. Endocr Metab Immune Disord Drug Targets. 2014;14: 272–282. [DOI] [PubMed] [Google Scholar]
- 19.Cases J, Romain C, Dallas C, Gerbi A, Cloarec M. Regular consumption of Fiit-ns, a polyphenol extract from fruit and vegetables frequently consumed within the Mediterranean diet, improves metabolic ageing of obese volunteers: a randomized, double-blind, parallel trial. Int J Food Sci Nutr. 2015;66: 120–125. 10.3109/09637486.2014.971229 [DOI] [PubMed] [Google Scholar]
- 20.Tapsell LC. Foods and food components in the Mediterranean diet: supporting overall effects. BMC Med. 2014;12: 100 10.1186/1741-7015-12-100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Biasi E, Deiana M, Guina P, Gamba P, Leonarduzzi G, Poli G. Wine consumption and intestinal redox homeostasis. Redox Biol. 2014;2: 795–802. 10.1016/j.redox.2014.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Williamson G, Manach C. Bioavailability and bioefficacy of polyphenols in humans. II. Review of 93 intervention studies. Am J Clin Nutr. 2005;81: 243S–255S. [DOI] [PubMed] [Google Scholar]
- 23.Rivera-Pastrana DM, Yahia EM, González-Aguilar GA. Phenolic and carotenoid profiles of papaya fruit (Carica papaya L.) and their contents under low temperature storage. J Sci Food Agric. 2010;90: 2358–2365. 10.1002/jsfa.4092 [DOI] [PubMed] [Google Scholar]
- 24.Lans CA. Ethno medicines used in Trinidad and Tobago on urinary problems and diabetes mellitus. J Ethnobiol Enthroned. 2006;2: 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chávez-Quintal P, González-Flores T, Rodríguez-Baneful I, Gallegos-Tin tore S. Antifungal activity in ethanol extracts of Carica papaya L. cv. Marisol leaves and seeds. Indian J Microbiol. 2011;51: 54–61. 10.1007/s12088-011-0086-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Juárez-Roop IE, Díaz-Zagoya JC, Ble-Castillo JL, Miranda-Osorio PH, Castell-Rodríguez AE, Tovilla-Zárate CA, et al. Hypoglycemic effect of Carica papaya leaves in streptozotocin-induced diabetic rats. BMC Complement Altern Med. 2012;12: 236 10.1186/1472-6882-12-236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Olagunjo JA, Adeneye AA, Fagbohunka BS, Bisuga NA, Ketiku AO, Benebo AS, et al. Nephroprotective activities of aqueous seed extract of Carica papaya Linn. in carbon tetrachloride induced renal injured rats: a dose- and time-dependent study. Biol Med 2009;1: 11–119. [Google Scholar]
- 28.Onako LO, Harna AA, Okure VC, Tijani AY, Ngene AA, Esimone CO. Antagonistic antimalarial properties of pawpaw leaf aqueous extract in combination with artesunic acid in Plasmodium berghei-infected mice. J Vector Borne Dis. 2011;48: 96–100. [PubMed] [Google Scholar]
- 29.Noda Y, Murakami S, Mankura M, Mori A. Inhibitory effect of fermented papaya preparation on hydroxyl radical generation from methylguanidine. J Clin Biochem Nutr. 2008;41: 185–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Roberfroid M, Gibson GR. McCartney AL, Rastall R, Rowland I, Wolvers D, et al. Probiotic effects: metabolic and health benefits. Br J Nutr. 2010;104: s1–s63. [DOI] [PubMed] [Google Scholar]
- 31.Soares JB, Pimentel-Nunes P, Roncon-Albuquerque R Jr., Leite-Moreira A. The role of lipopolysaccharide/toll-like receptor 4 signaling in chronic liver diseases. Hepatol Int. 2010;4: 659–672. 10.1007/s12072-010-9219-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nakamura YK, Omaye ST. Metabolic diseases and pro- and prebiotics: mechanistic insights. Nutr Metab (Lond). 2012;9: 60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schuster M, Anneman M, Plaza-Sirvent C, Schmitz I. Atypical IκB proteins-nuclear modulators of NF-κB signaling. Cell Commun Signal. 2013;11: 23 10.1186/1478-811X-11-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hiramoto K, Imao M, Sato EF, Inoue M, Mori A. Effect of fermented papaya preparation on dermal and intestinal mucosal immunity and allergic inflammations. J Sci Food Agric. 2008;88: 1151–1157. [Google Scholar]
- 35.Zhang J, Mori A, Chen Q, Zhao B. Fermented papaya preparation attenuated β-amyloid precursor protein: β-amyloid-mediated copper neurotoxicity in β-amyloid precursor protein and β-amyloid precursor protein Swedish mutation overexpressing SH-SY5Y cells. Neuroscience. 2006;13: 63–72. [DOI] [PubMed] [Google Scholar]
- 36.Imao K, Komatsu M, Wang H, Hiramatsu M. Inhibitory effect of fermented papaya preparation on oxidative damage and tissue injury in the brain formed during iron-induced epileptogenesis in rats. J Brain Sci. 1999;25: 71–76. [Google Scholar]
- 37.Colland E, Roy S. Improved function of diabetic wound site macrophages and accelerated wound closure in response to oral supplementation of fermented papaya preparation. Antioxid Redox Signal. 2010;13: 599–606. 10.1089/ars.2009.3039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Makkar HPS, Blummel M, Borowy NK, Becker K. Gravimetric determination of tannins and their correlations with chemical and protein precipitation methods. J Sci Food Agric. 1993;61: 161–165. [Google Scholar]
- 39.Wahlberg BJ, Burholt DR, Kornblith P, Richards TJ, Bruffsky A, Herberman RB, Vujanovic NL. Measurement of NK activity by the microcytotoxicity assay (MCA): a new application for an old assay. J Immunol Methods. 2001;253: 69–81. [DOI] [PubMed] [Google Scholar]
- 40.Nakayama J, Watanabe K, Jiang J, Matsuda K, Chao SH, Haryono P, et al. Diversity in gut bacterial community of school-age children in Asia. Sci Rep. 2015;5: 8397 10.1038/srep08397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Matsuki T, Watanabe K, Fujimoto J, Takada T, Tanaka R. Use of 16S rRNA gene-targeted group-specific primers for real-time PCR analysis of predominant bacteria in human feces. Appl Environ Microbiol. 2004; 70: 7220–7228. 10.1128/AEM.70.12.7220-7228.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Caporaso JG, Kucxynski J, Stombaugh J, Bittinger K, Bushman FD, Costello EK, et al. QIIME allows analysis of high-throughput community sequencing data. Nat Methods. 2010;7: 335–336. 10.1038/nmeth.f.303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Edgar RC. Search and clustering orders of magnitude faster than BLAST. Bioinformatics. 2010;26: 2460–2461. 10.1093/bioinformatics/btq461 [DOI] [PubMed] [Google Scholar]
- 44.Edgar RC, Haas BJ, Clemente JC, Quince C, Knight R. UCHIME improves sensitivity and speed of chimera detection. Bioinformatics. 2011;27: 2194–2200. 10.1093/bioinformatics/btr381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.DeSantis TZ, Hugenholtz P, Larsen N, Rojas M, Brodie EL, Keller K, et al. Greengenes, a chimera-checked 16S rRNA gene database and workbench compatible with ARB. Appl Environ Microbiol. 2006;72: 5069–5072. 10.1128/AEM.03006-05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cole JR, Chai B, Farris RJ, Wang Q, Kulam SA, McGarrell DM, et al. The Ribosomal Database Project (RDP-II): sequences and tools for high-throughput rRNA analysis. Nucleic Acids Res. 2005;33: D294–296. 10.1093/nar/gki038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nakayama J. Pyrosequence-based 16S rRNA profiling of gastro-intestinal microbiota. Biosci Microflora. 2010;29: 83–96. [Google Scholar]
- 48.Stephen AM, Cummings JH. The microbial contribution to human faecal mass. J Med Microbiol. 1980;13: 45–56. 10.1099/00222615-13-1-45 [DOI] [PubMed] [Google Scholar]
- 49.Rizzello V, Bonaccorsi I, Dongarrà ML, Fink LN, Ferlazzo G. Role of natural killer and dendritic cell crosstalk in immunomodulation by commensal bacteria probiotics. J Biomed Biotechnol. 2011;2011: 473097 10.1155/2011/473097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fink LN, Zeuthen LH, Christensen HR, Morandi B, Frøkiaer H, Ferlazzo G. Distinct gut-derived lactic acid bacteria elicit divergent dendritic cell-mediated NK cell responses. Int Immunol. 2007;19: 1319–1327. 10.1093/intimm/dxm103 [DOI] [PubMed] [Google Scholar]
- 51.Ferlazzo G, Pack M, Thomas D, Paludan C, Schmid D, Strowig T, et al. Distinct roles of IL-12 and IL-15 in human natural killer cell activation by dendritic cells from secondary lymphoid organs. Proc Natl Acad Sci U S A. 2004;101: 16606–16611 10.1073/pnas.0407522101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gerosa F, Gobbi A, Zorzi P, Burg S, Briere F, Carra G, et al. The reciprocal interaction of NK cells with plasmacytoid or myeloid dendritic cells profoundly affects innate resistance functions. J Immunol. 2005;74: 727–734. [DOI] [PubMed] [Google Scholar]
- 53.Fernandez NC, Lozier A, Flament C, Ricciardi-Castagnoli P, Bellet D, Suter M, et al. Dendritic cells directly trigger NK cell functions: cross-talk relevant in innate anti-tumor immune responses in vivo. Nat med. 1999;5: 405–411. 10.1038/7403 [DOI] [PubMed] [Google Scholar]
- 54.Panda A, Arjona A, Sapey E, Bai F, Fikrig E, Montogomery RR, et al. Human innate immunosenesence: causes and consequences for immunity in old age. Trends Immunol. 2009;30: 325–333. 10.1016/j.it.2009.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shaw AC, Joshi S, Greenwood H, Panda A, Lord JM. Aging of the innate immune system. Curr Opin Immunol. 2010;20: 507–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mariani E, Mariani AR, Meneghenetti A, Tarozzil A. Cocco L, Facchini A. Aged-dependent decreases of NK cell phosphoinositide turnover during spontaneous but not Fc-mediated cytolytic activity. Int Immun. 1997;10: 981–989. [DOI] [PubMed] [Google Scholar]
- 57.Porrata LF, Inwards DJ, Lacy MQ, Markovic SN. Immunomodulation of early engrafted natural killer cells with interleukin-2 and interferon-α in autologous stem cell transplantation. Bone Marrow Transplant. 2001;28: 673–680. 10.1038/sj.bmt.1703203 [DOI] [PubMed] [Google Scholar]
- 58.Ozdemir O, Savasan S. Combinational IL-2/IL-15 induction does not further enhance IL-15-induced lymphokine-activated killer cell cytotoxicity against human leukemia/lymphoma cells. Clin Immunol. 2005;115: 240–249. 10.1016/j.clim.2005.01.008 [DOI] [PubMed] [Google Scholar]
- 59.Camous X, Pera A, Solana R, Larbi A. NK cells in healthy aging and age-associated diseases. J Biomed Biotechnol. 2012;2012: 195956 10.1155/2012/195956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Micucci F, Capuano C, Marchetti E, Piccoli M, Frati L, Santoni A, et al. PI5KI-dependent signals are critical regulators of the cytolytic secretory pathway. Blood. 2008;111: 4165–4172. 10.1182/blood-2007-08-108886 [DOI] [PubMed] [Google Scholar]
- 61.Huag AC, Cheng HY, Lin TS, Chen WH, Lin JH, Lin JJ, et al. Epigallocatechin gallate (EGCG), influences a murine WEHI-3 leukemia model in vivo through enhancing phagocytosis of macrophages and populations of T- and B-cells. In Vivo. 2013;27: 627–634. [PubMed] [Google Scholar]
- 62.Perche O, Vergnaud-Gauduchon J, Morand C. Dubray C, Mazur A, Vasson MP. Orange juice and its major polyphenol hesperidin consumption do not induce immunomodulation in healthy well-nourished humans. Clin Nutr. 2014;33: 130–135. 10.1016/j.clnu.2013.03.012 [DOI] [PubMed] [Google Scholar]
- 63.Warner EF, Zhang Q, Raheem KS, O’Hagan D, O’Connell MA, Kay CD. Common phenolic metabolites of flavonoids, but not their unmetabolized precursors, reduce the secretion of vascular cellular adhesion molecules by human endothelial cells. J Nutr 2016;146: 465–473. 10.3945/jn.115.217943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Killian PH, Kronski E, Michalik KM, Barbieri O, Astigiano S, Sommerhoff CP, et al. Curcumin inhibits prostate cancer metastasis in vivo by targeting the inflammatory cytokines CXCL1 and -2. Carcinogenesis. 2012;33: 2507–2519. 10.1093/carcin/bgs312 [DOI] [PubMed] [Google Scholar]
- 65.Banerjee N, Talcott S, Safe S, Mertens-Talcott SU. Cytotoxicity of pomegranate polyphenolics in breast cancer cells in vitro and in vivo: potential role of miRNA-27a and miRNA-155 in cell survival and inflammation. Breast Cancer Res Treat. 2012;136: 21–34. 10.1007/s10549-012-2224-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Warner EF, Zhang Q, Raheem KS, O’Hagan D, O’Connell MA, Kay CD. Common phenolic metabolites of flavonoids, but not their unmetabolized precursors, reduce the secretion of vascular cellular adhesion molecules by human endothelial cells. J Nutr. 2016;146: 465–473. 10.3945/jn.115.217943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Park YC, Rimbach G, Salio C, Valacchi G, Packer L. Activity of monomeric, dimeric, and trimeric flavonoids on NO production, TNF-alpha secretion, and NF-kappaB-dependent gene expression in RAW 264.7 macrophages. FEBS Lett. 2000;465: 93–97. [DOI] [PubMed] [Google Scholar]
- 68.Williamson G, Clifford MN. Colonic metabolites of polyphenols: the missing link to biological activity? Br J Nutr. 2010;104: S48–S66. 10.1017/S0007114510003946 [DOI] [PubMed] [Google Scholar]
- 69.Nurmi T, Mursu J, Heinonen M, Nurmi A, Hiltunen R, Voutilainen S. Metabolism of berry anthocyanins to phenolic acids in humans. J Agric Food Chem. 2009;57: 2274–2281. 10.1021/jf8035116 [DOI] [PubMed] [Google Scholar]
- 70.Jensen GS, Wu X, Patterson KM, Barnes J, Carter SG, Scherwitz L, et al. In vitro and in vivo antioxidant and anti-inflammatory capacities of an antioxidant-rich fruit and berry juice blend. Results of a pilot and randomized, double-blinded, placebo-controlled, crossover study. J Agric Food Chem. 2008;56: 8326–8333. 10.1021/jf8016157 [DOI] [PubMed] [Google Scholar]
- 71.Cardona F, Andrés-Lacueva C, Tulipani S, Tinahones FJ, Queipo-Ortuño MI. Benefits of polyphenols on gut microbiota and implications in human health. J Nutr Biochem. 2013;24: 1415–1422. 10.1016/j.jnutbio.2013.05.001 [DOI] [PubMed] [Google Scholar]
- 72.Scholz S, Williamson G. Interactions affecting the bioavailability of dietary polyphenols in vivo. Int J Vitam Nutr Res. 2007;77: 224–235. 10.1024/0300-9831.77.3.224 [DOI] [PubMed] [Google Scholar]
- 73.Manach C, Scalbert A, Morand C, Remesy C, Jimenez L. Polyphenols: food sources and bioavailability. Am J Clin Nutr. 2004;79: 727–747. [DOI] [PubMed] [Google Scholar]
- 74.D’Archivio M, Filesi C, Di Benedetto R, Gargiulo R, Giovannini C, Masella R. Polyphenols, dietary sources and bioavailability. Ann 1st Super Sanita. 2007;43: 348–361. [PubMed] [Google Scholar]
- 75.Jacobs DM, Gaudier E, van Duynhoven J, Vaughan EE. Non-digestible food ingredients, colonic microbiota and the impact on gut health and immunity: a role for metabolomics. Curr Drug Metab. 2009;10: 41–54. [DOI] [PubMed] [Google Scholar]
- 76.Kroon PA, Clifford NM, Crozier A, Day AJ, Donovan JL, Manach C, et al. How should we assess the effects of exposure to dietary polyphenols in vitro? Am J Clin Nutr. 2004;80: 15–21. [DOI] [PubMed] [Google Scholar]
- 77.Manach C, Donovan JL. Pharmacokinetics and metabolism of dietary flavonoids in humans. Free Radic Res. 2004;38: 771–785. [DOI] [PubMed] [Google Scholar]
- 78.Manach C, Williamson G, Morand C, Scalbert A, Rémésy C. Bioavailability and bioefficacy of polyphenols in humans. I. Review of 97 bioavailability studies. Am J Clin Nutr. 2005;81: 230S–242S. [DOI] [PubMed] [Google Scholar]
- 79.Clifford MN, van der Hooft JJ, Crozier A. Human studies on the absorption, distribution, metabolism, and excretion of tea polyphenols. Am J Clin Nutr. 2013;98: 1619S–1630S. 10.3945/ajcn.113.058958 [DOI] [PubMed] [Google Scholar]
- 80.Serrano J, Puupponen-Pimiä R, Dauer A, Aura AM, Saura-Calixto F. Tannins: current knowledge of food sources, intake, bioavailability and biological effects. Mol Nutr Food Res. 2009;53: S310–S329. 10.1002/mnfr.200900039 [DOI] [PubMed] [Google Scholar]
- 81.Appeldoorn MM, Vincken JP, Aura AM, Hollman PC, Gruppen H. Procyanidin dimers are metabolized by human microbiota with 2-(3,4-dihydroxyphenyl) acetic acid and 5-(3,4-dihydroxyphenyl)-gamma-valerolactone as the major metabolites. J Agric Food Chem. 2009;57: 1084–1092. 10.1021/jf803059z [DOI] [PubMed] [Google Scholar]
- 82.Urpi-Sarda M, Garrido I, Monagas M, Góméz-Cordoves C, Medina-Remon A, Andres-Lacueva C, et al. Profile of plasma and urine metabolites after the intake of almond [Prunus dulcis (Mill.) D.A. Webb] polyphenols in humans. J Agric Food Chem. 2009;57: 10134–10142. 10.1021/jf901450z [DOI] [PubMed] [Google Scholar]
- 83.Stoupi S, Williamson G, Drynan JW, Barron D, Clifford MN. A comparison of the in vitro biotransformation of (−)-epicatechin and procyanidin B2 by human faecal microbiota. Mol Nutr Food Res. 2010;54: 747–759. 10.1002/mnfr.200900123 [DOI] [PubMed] [Google Scholar]
- 84.Déprez S, Brezillon C, Rabot S, Philippe C, Mila I, Lapierre C, et al. Polymeric proanthocyanidins are catabolized by human colonic microflora into low molecular-weight phenolic acids. J Nutr. 2000;130: 2733–2738. [DOI] [PubMed] [Google Scholar]
- 85.Mulholland PJ, Ferry DR, Anderson D, Hussain SA, Young AM, Cook JE, et al. Pre-clinical and clinical study of QC12, a water-soluble, pro-drug of quercetin. Ann Oncol. 2001;12: 245–248. [DOI] [PubMed] [Google Scholar]
- 86.Lin S, Yang B, Chen F, Jiang G, Li Q, Duan X, et al. Enhanced DPPH radical scavenging activity and DNA protection effect of litchi pericarp extract by Aspergillus awamori bioconversion. Chem Cent J. 2012;6: 108 10.1186/1752-153X-6-108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lee HS, Kim MR, Park Y, Park HJ, Chang UJ, Kim SY, et al. Fermenting red ginseng enhances its safety and efficacy as a novel skin care anti-aging ingredient: In vitro and animal study. J Med Food. 2012;15: 1015–1023. 10.1089/jmf.2012.2187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ryu JS, Lee HJ, Bae SH, Kim SY, Park Y, Suh HJ, et al. The bioavailability of red ginseng extract fermented by Phellinus linteus. J Ginseng Res. 2013;37: 108–116. 10.5142/jgr.2013.37.108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Georgetti SR, Casagrande R, Vicentini FT, Baracat MM, Verri WA, Fonseca MJ. Protective effect of fermented soybean dried extracts against TPA-induced oxidative stress in hairless mice skin. Biomed Res Int. 2013;2013: 340626 10.1155/2013/340626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Krumholz LR, Bryant MP. Characterization of the pyrogallol-phloroglucinol isomerase of Eubacterium oxidoreducens. J Bacteriol. 1988;170: 2472–2479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Islam KB, Fukiya S, Hagio M, Fujii N, Ishizuka S, Ooka T, et al. Bile acid is a host factor that regulates the composition of the cecal microbiota in rats. Gastroenterology. 2011;141: 1773–1781. 10.1053/j.gastro.2011.07.046 [DOI] [PubMed] [Google Scholar]
- 92.Hara Y. Influence of tea catechins on the digestive tract. J Cell Biochem Suppl. 1997;27: 52–58. [PubMed] [Google Scholar]
- 93.Lee HC, Jenner AM, Low CS, Lee YK. Effect of tea phenolics and their aromatic fecal bacterial metabolites on intestinal microbiota. Res Microbiol. 2006;157: 876–884. 10.1016/j.resmic.2006.07.004 [DOI] [PubMed] [Google Scholar]
- 94.Peppercon MA, Goldman P. Caffeic acid and metabolism by gnotobiotic rats and their intestinal bacteria. Proc Natl Acad Sci U S A. 1972;69: 1413–1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Tamura A, Fukushima M, Shimada K, Han KH, Sekikawa M, Watanabe S, et al. Cholesterol metabolism in rat is affected by protocatechuic acid. J Nutr Sci Vitaminol. 2004;50: 13–18. [PubMed] [Google Scholar]
- 96.Bhat CS, Ramasarma T. Effect of phenyl and phenolic acids on mevalonate-5-phosphate kinase and mevalonate-5-pyrophosphate decarboxylase of the rat brain. J Neurochem. 1979;32: 1531–1537. [DOI] [PubMed] [Google Scholar]
- 97.Lee JS, Choi MS, Jeon SM, Jeong TS, Park YB, Lee MK, et al. Lipid-lowering and antioxidative activities of 3,4-di(OH)-cinnamate and 3,4-di(OH)-hydrocinnamate in cholesterol-fed rats. Clin Chim Acta. 2001;314: 221–229. [DOI] [PubMed] [Google Scholar]
- 98.Cai EP, Lin JK. Epigallocatechin gallate (EGCG) and rutin suppress the glucotoxicity through activating IRS2 and AMPK signaling in rat pancreatic beta cells. J Agric Food Chem. 2009;57: 9817–9827. 10.1021/jf902618v [DOI] [PubMed] [Google Scholar]
- 99.Fu Z, Zhang W, Zhen W, Lum H, Nadler J, Bassaganya-Riera J, et al. Genistein induces pancreatic beta-cell proliferation through activation of multiple signaling pathways and prevents insulin deficient diabetes in mice. Endocrinology. 2010;151: 3026–3037. 10.1210/en.2009-1294 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.