Abstract
Objective
Mutations of genes encoding the four subunits of succinate dehydrogenase (SDH) have been associated with pheochromocytoma and paraganglioma (PPGLs), gastrointestinal stromal tumors (GISTs) and renal cell carcinomas (RCCs). These tumors have not been characterized in a way that reflects severity of SDH dysfunction. Mass spectrometric analysis now allows measurement of metabolites extracted from formalin fixed paraffin embedded (FFPE) specimens. We assess whether SDH deficiency in various tumor types characterized by loss of SDHB protein expression correlates with SDH dysfunction as assessed by the ratio of succinate:fumarate in FFPE specimens.
Patients and methods
Sections of FFPE tumor specimens from 18 PPGL, 10 GIST and 11 RCC patients with known SDHx mutation status for SDH deficiency were collected for mass spectrometric analysis of succinate and fumarate.
Results
FFPE samples showed higher succinate:fumarate ratios in SDH-deficient PPGLs compared to SDH-sufficient PPGLs. Similarly, a higher succinate:fumarate ratio was able to distinguish SDH-deficient GISTs and RCCs from their SDH-sufficient counterparts with great selectivity. Interestingly, the cut-off value of the succinate:fumarate ratio was two-folds greater in RCCs than GISTs.
Conclusion
Analyzing biochemical imbalances preserved in FFPE specimens with mass spectrometry expands the method and sample type repertoire available for characterisation of multiple neoplasias associated with SDH deficiency.
Keywords: Succinate dehydrogenase deficiency, Mass spectrometry, Pheochromocytoma and paraganglioma, Gastrointestinal stromal tumor, Renal cell carcinoma
1. Introduction
Deregulation of cellular metabolism has been widely recognized as one of the hallmarks of cancer [1]. Accumulation of biomolecules as a result of enzyme impairment has gained interest in the field of cancer biomarker discovery [2]. Mutations in genes encoding subunits of succinate dehydrogenase (SDH) leading to loss or dysfunction of the mitochondrial enzyme involved in both the Krebs cycle and electron transport chain have been associated with multiple neoplasias [3]. These include pheochromocytomas and paragangliomas (PPGLs), gastrointestinal stromal tumors (GISTs) and renal cell carcinomas (RCCs) [4], [5], [6]. Clinical presentations, immunohistochemical (IHC) staining of SDH subunit proteins SDHA/B from resected specimens, and genetic screening of SDHx genes are typically used to characterize these tumors [7], [8]. SDH-deficient tumors, characterized by loss of SDHB IHC, accumulate succinate and secondarily hypoxia inducible factors (HIFs) with downstream consequences referred to as pseudohypoxia [9]. Advances in liquid chromatography tandem mass-spectrometry (LC-MS/MS) allow sensitive measurement of accumulated succinate due to SDH dysfunction [10]. Metabolomic profiling of fresh frozen PPGL tumors suggested a direct link between tumor-associated SDHx mutations and the measurable metabolite imbalance of a high succinate:fumarate ratio [11], [12].
Fresh frozen specimens represent the gold standard sample type for metabolomic analyses, however storage and availability varies greatly across different sites limiting their use [13]. Formalin-fixed paraffin embedded (FFPE) specimens constitute a widely available and accessible archived pathological resource representing a good alternative for fresh-frozen tissue especially in studies involving rare cancers [14]. The use of FFPE tissues in retrospective metabolomic studies has shown potential applicability for LC-MS/MS based profiling of sarcomas and thyroid cancer tissue [15], [16], [17]. This led us to question whether FFPE specimens from SDH-deficient tumors could be used for metabolomic profiling.
The aim of this study was to assess whether elevated succinate:fumarate ratios, as assessed by LC-MS/MS from FFPE samples, are a consistent biochemical signature in SDH-deficient GISTs and RCCs in the same manner as previously observed in PPGLs.
2. Material and methods
2.1. FFPE specimens
FFPE specimens from 18 cases of PPGLs encompassing 9 pheochromocytoma and 9 paraganglioma patients, 10 cases of GISTs and 11 cases of RCCs were obtained from surgical resection of primary tumors. The use of specimens in this study was approved by Northern Sydney Local Health District Human Research Ethics Committee (LNR 1312-417M). The presence of neoplastic tissue in the sections were confirmed by an experienced surgical pathologist (AJG) in all samples and all samples were confirmed to have a neoplastic cellularity of > 60%. SDH-deficiency was defined by the standard IHC approach requiring loss of SDHB protein expression in neoplastic cells, with preserved expression in non-neoplastic cells which act as an internal positive control [18], whereas SDH-sufficient specimens were defined by positive granular cytoplasmic SDHB staining. SDHx mutation status was confirmed in SDH-deficient specimens from PPGL group with 2 SDHA, 5 SDHB, 2 SDHD germline mutations and RCC group with 2 SDHB, 1 SDHD germline mutations. In GIST group, SDHA mutation was confirmed in 2 of 5 SDH-deficient tumors (Supplementary Table 1). However, based on previous reports, approximately half of SDH-deficient GISTs have no underlying SDHx mutation [6], [18], [19]. The first section cut from each FFPE specimen block was discarded to minimize contamination due to prolonged environmental exposure. Two 50 μm sections were then cut from each block and pooled into a 1.5 mL microfuge tube [12].
2.2. Sample preparation
Succinate and fumarate certified reference materials were purchased from Sigma-Aldrich (Australia) for the creation of calibration curves. 13C4 succinate was also purchased from Sigma-Aldrich and 13C4 fumarate was purchased from Cambridge Isotope Laboratories (USA) for use as internal standards. 1 mL of extraction solution (20% LC/MS grade H2O, 80% LC/MS grade methanol containing 0.1 μg/mL 13C4 fumarate and 0.5 μg/mL 13C4 succinate) was added to each microfuge tube containing FFPE sections. After a brief vortex, mixtures were incubated for 45 min at 70 °C followed by 5 min on ice. Metabolites were extracted from melted paraffin by collecting and combining supernatants from two consecutive centrifugations at 14,000 × g for 10 min at 4 °C. Samples were dried by evaporating methanol for 2 h using a Speedvac and then stored at − 80 °C until further use [12].
2.3. LC-MS/MS analysis
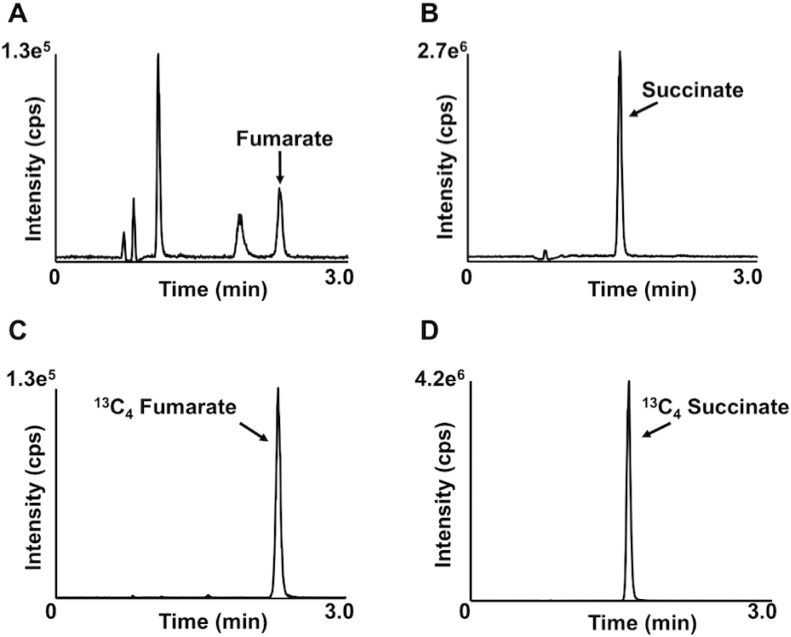
Analysis of extracts was performed on a Prominence high performance liquid chromatography system (Shimadzu, Australia) coupled to an API QTRAP 5500 mass spectrometer (SCIEX, Australia) operated in negative electrospray ionisation. Separation of target analytes from isobaric interferences was achieved using an Ascentis Express 100 × 3.0 mm 2.7 μm RP Amide (Sigma Aldrich, Australia) analytical column held at 40 °C and isocratic elution using aqueous 0.4% formic acid with a flow rate of 0.5 mL/min. Succinate eluted at 1.57 min and fumarate eluted at 2.29 min with chromatographic resolution between interferences and a total run time of 3 min (Fig. 1).
Fig. 1.
Multiple reaction monitoring chromatograms from an extracted FFPE sample for (A) fumarate (B) succinate (C) 13C4 fumarate and (D) 13C4 succinate.
Initially 1 μL of extracted samples were injected onto the system with a linear calibration range of 22.5–90,000 ng/mL for succinate and 9–450 ng/mL for fumarate. Extracts that demonstrated fumarate levels between the lower two calibrators (0.9 and 9 ng/mL) were reinjected, along with calibrators, with a 10 μL injection for quantitation to 0.9 ng/mL. At the end of every batch the column was cleaned with acetonitrile at 0.8 mL/min for 10 min to remove any strongly retaining compounds. Analytes were detected by monitoring multiple reaction monitoring m/z transitions of 116.9 > 73.1 and 116.9 > 99.1 as quantifier and qualifier transitions, respectively, for succinate, 121.0 > 76.1 for the 13C4 succinate internal standard, 114.9 > 71.0 for fumarate and 119 > 74 for the 13C4 fumarate internal standard. Unlike previous reports we were unable to find a suitable qualifier transition for fumarate.
2.4. Statistical analysis
Statistical analyses of LC-MS/MS results were performed using Prism 6.0 f. Unpaired two-tailed t-tests were used to determine the differences in succinate:fumarate ratio between SDH-deficient and SDH-sufficient tumor groups. Results were considered significant if p < 0.05. The optimal cut-off value for discriminating SDH-deficient tumors using the succinate:fumarate ratio was determined by generating a receiver-operating characteristic (ROC) curve. Values are represented as mean ± SEM unless otherwise stated.
3. Results
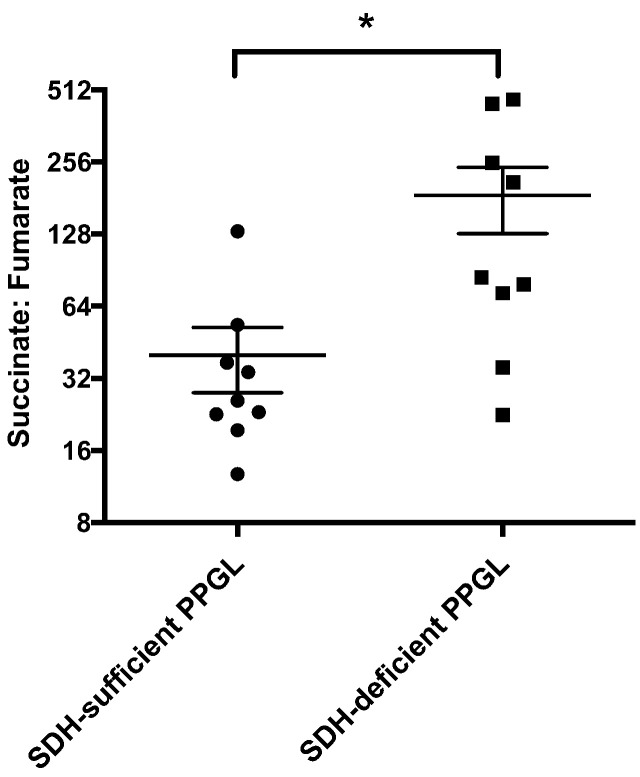
3.1. SDH-deficient vs SDH-sufficient PPGLs
Analysis of metabolites extracted from FFPE PPGL specimens showed a significantly higher succinate:fumarate ratio in SDH-deficient PPGL tumors (185.75 ± 57.24, n = 9) when compared to SDH-sufficient PPGL tumors (40.02 ± 12.11, n = 9) (p < 0.05) (Fig. 2). Although statistical analysis of these two groups showed a significantly different metabolite imbalance, a cut-off ratio of succinate:fumarate (63.12) generated by ROC curve (Supplementary Fig. 1) could not clearly separate these tumor types; 1 false positive and 2 false negatives (Supplementary Table 2). Interestingly among SDH-sufficient samples, those with highest succinate:fumarate ratios were from specimens with germline VHL mutations. The succinate:fumarate ratio was not able to distinguish VHL mutated PPGLs from SDH-deficient PPGLs (Supplementary Fig. 2).
Fig. 2.
Scatter plot comparing succinate:fumarate ratio between SDH-sufficient (n = 9) and SDH-deficient PPGLs (n = 9), error bars representing SEM from mean (*p < 0.05).
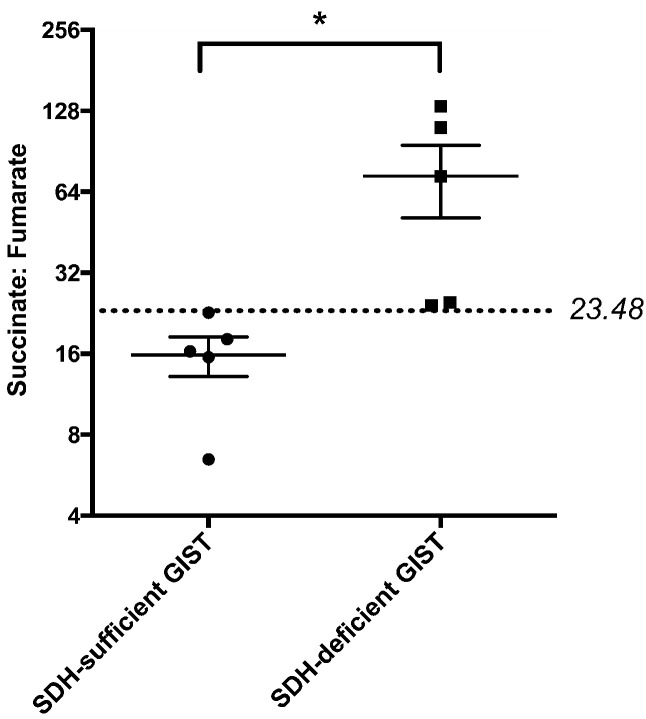
3.2. SDH-deficient vs SDH-sufficient GISTs
The succinate:fumarate ratio in five SDH-deficient GISTs (73.25 ± 22.06) was shown to be significantly higher than five SDH-sufficient GISTs (representing patients with KIT or PDGRA gene mutations; 15.84 ± 2.65) (p < 0.05) (Fig. 3). Using logistic regression, an area under the ROC curve of 1.00 was calculated and a cut-off succinate:fumarate ratio of 23.48 was determined that distinguished SDH-deficient and SDH-sufficient GISTs (Supplementary Fig. 3).
Fig. 3.
Scatter plot comparing succinate:fumarate ratio between SDH-sufficient (n = 5) and SDH-deficient GISTs (n = 5), error bars representing SEM from mean (*p < 0.05). ROC curve analysis was used to determine cut-off value of 23.48 marked as a dashed line.
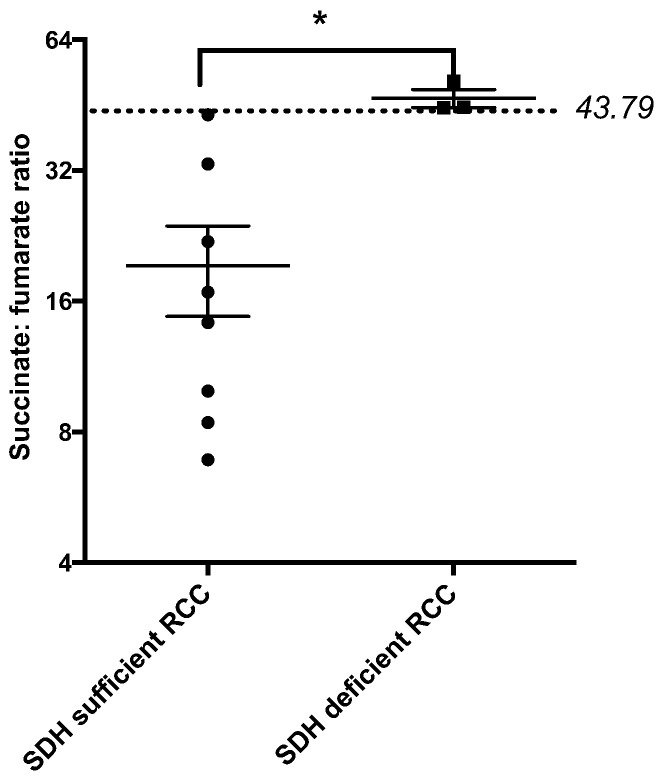
3.3. SDH-deficient vs SDH-sufficient RCCs
The mean succinate:fumarate ratio in three SDH-deficient RCCs (46.9 ± 2.234) was significantly higher than eight SDH-sufficient RCCs (19.30 ± 4.53) (p < 0.05) (Fig. 4). With an area under the ROC curve of 1.00, a succinate:fumarate ratio of 43.79 was calculated as the cut-off value that distinguished SDH-deficient RCCs from SDH-sufficient RCCs (Supplementary Fig. 4).
Fig. 4.
Scatter plot comparing succinate:fumarate ratio between SDH-sufficient (n = 8) and SDH-deficient RCCs (n = 3), error bars representing SEM from mean (*p < 0.05). ROC curve analysis was used to determine cut-off value of 43.79 marked as a dashed line.
4. Discussion
Expression of functional SDH in the mitochondria is essential for cellular respiration and energy production [20], [21]. “Pseudohypoxia”, in which HIF is stabilized despite normoxic conditions as a consequence of succinate-mediated prolyl hydroxylase domain (PHD) inhibition, has been associated with SDH-deficient neoplasias such as PPGLs, GISTs and RCCs [22], [23]. Analyzing the substrate-to-product ratio provides direct assessment of enzymatic function and this has been implemented in the discovery of accumulated metabolites associated with cancer, now labelled as ‘onco-metabolites’ [2]. High succinate measurement relative to fumarate in the tumors represents a direct link to functional aspects associated with SDH-deficiency. In this study we have shown for the first time that an elevated succinate:fumarate ratio is a consistent biomolecular phenotype of SDH-deficient tumors that include GISTs and RCCs as well as PPGLs. We confirmed a previous report that measurement of these metabolites is possible from FFPE specimens [12]. Of note, one of our SDH-deficient specimens had been stored for 25 years in archive.
Our study is the first to report significantly higher succinate:fumarate ratios in SDH-deficient GISTs and RCCs compared to corresponding SDH-sufficient GISTs and RCCs. Clear separation of GIST and RCC tumor groups with 100% specificity suggests potential diagnostic application of LC/MS-MS based profiling of metabolites extracted from FFPE specimens as previously observed for PPGLs. Interestingly, our cut-off succinate:fumarate ratio determined by ROC curve analysis was almost two-fold higher for discriminating SDH-deficient RCCs compared to SDH-deficient GISTs. This suggests the extent of biochemical imbalance caused by SDH-deficiency is likely to be tissue-specific.
We have confirmed the earlier finding by Richter et al. [12] that VHL-mutated PPGLs have higher succinate:fumarate ratios within the SDH-sufficient group (Supplementary Fig. 2), suggesting that VHL-deficiency causes functional SDH-deficiency. PPGL tumor specimens with VHL gene mutations have been associated with variably impaired SDHB protein expression [24], and although the mechanism for this is unknown several hypotheses have been advanced including pseudohypoxic expression of miR-210 that in turns downregulates SDHD expression [25].
Just as higher succinate levels were detected in nuclear magnetic resonance (NMR) spectroscopy of SDHx tumors in vivo [26], [27], direct measurement of succinate and fumarate by LC-MS/MS based analysis appears therefore to be a powerful technique to interrogate SDH function ex vivo. These methods now allow quantitative analysis of SDH dysfunction in a manner that complements qualitative assessment of SDHB protein expression by IHC. Elevated succinate:fumarate appears to have at least three potential causes: (a) inactivation by germline mutation in SDHx gene (together with somatic loss of the other allele) herein shown to be true for SDHx-mutated RCCs as well for PPGLs; (b) hypermethylation of the SDHC promoter, as first described in Carney triad [28] and more recently in PPGL by Richter et al. [29], and which is possibly also the mechanism for SDH-deficiency in at least some of our GIST samples; and (c) by germline VHL mutation which is associated with variably impaired SDH function.
Our data also sound a note of caution in that a very few SDHx-mutated PPGLs were associated with normal succinate:fumarate values (i.e. ‘false negatives’, Supplementary Table 2). The SDHx-mutated PPGL with the lowest succinate:fumarate (i.e. indistinguishable from SDH-sufficient samples) contained SDHB mutation c.380T > G, p.Ile127Ser. This was particularly interesting to us, since we have recently described a method for measuring mutant SDH function in vitro, and this same mutation was found to have minimal impact on enzymatic function [30]. It is intriguing therefore to speculate that SDH-deficient PPGLs with normal succinate:fumarate ratios are associated with mutations that do not primarily alter SDH activity and may otherwise cause tumor development through alternative mechanisms (e.g. via electron transport abnormalities).
A limitation of this study was the heterogeneous nature and variable tumor content in sections of our samples. Although all of our samples were reviewed by a pathologist to confirm the presence of neoplastic tissue in relatively high cellularity (> 60% neoplastic in all cases), we did not specifically micro-dissect the sections, and we acknowledge that there may have been dilution of the metabolite signal by normal cells in the surrounding tissue. However, despite this limitation, a significant difference in the succinate:fumarate ratio between the SDH-sufficient and -deficient group was still observed in most of the samples and tumors with similar morphologies and growth patterns could be expected to demonstrate similar neoplastic cellularities. That is, SDH-deficient GISTs would have similar neoplastic cellularity to other GISTs, and SDH-deficient PPGLs could be expected to have similar neoplastic cellularity to other PPGLs and so on.
5. Conclusion
We have demonstrated that SDH-deficient PPGLs, GISTs and RCCs retain a significantly higher succinate:fumarate ratio compared to SDH-sufficient counterparts, and can be readily assayed from archived samples. Our study highlights the importance of metabolomic analysis to directly measure SDH dysfunction that is associated with multiple types of neoplasias.
The following are the supplementary data related to this article.
FFPE specimens from 18 cases of PPGLs, 10 cases of GISTs and 11 cases of RCCs with known mutation status.
PPGL FFPE specimens with false-negatives and false-positive succinate:fumarate ratios.
ROC curve for discriminating SDH-deficient PPGLs from SDH-sufficient PPGLs according to succinate:fumarate ratio. Arrow marks cut-off (highest sensitivity and specificity) value. Area under the curve was equal to 0.80.
Scatter plot comparing succinate:fumarate ratio between SDH-sufficient PPGLs with VHL mutation (n = 3) and SDH-deficient PPGLs (n = 9), error bars representing SEM from mean (p > 0.05).
ROC curve for discriminating SDH-deficient GISTs from SDH-sufficient GISTs according to succinate:fumarate ratio. Arrow marks cut-off (highest sensitivity and specificity) value. Area under the curve was equal to 1.0.
ROC curve for discriminating SDH-deficient RCCs from SDH-sufficient RCCs according to succinate:fumarate ratio. Arrow marks cut-off (highest sensitivity and specificity) value. Area under the curve was equal to 1.0.
Disclosure statement
The authors have nothing to disclose.
Acknowledgments
This work was supported by the Hillcrest Foundation (Perpetual Trustees) to DB, and by NHMRC project grant 1108032 to RCB, TD, DB and AG.
Footnotes
This work was supported by the Hillcrest Foundation (Perpetual Trustees) (IPAP201600914) and by NHMRC project grant 1108032.
References
- 1.Hanahan D., Weinberg R.A. Hallmarks of cancer: the next generation. Cell. Mar 4 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 2.Yang M., Soga T., Pollard P.J. Oncometabolites: linking altered metabolism with cancer. J. Clin. Invest. Sep 2013;123:3652–3658. doi: 10.1172/JCI67228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gottlieb E., Tomlinson I.P. Mitochondrial tumour suppressors: a genetic and biochemical update. Nat. Rev. Cancer. 2005;5:857–866. doi: 10.1038/nrc1737. [DOI] [PubMed] [Google Scholar]
- 4.Bardella C., Pollard P.J., Tomlinson I. SDH mutations in cancer. Biochim. Biophys. Acta. Nov 2011;1807:1432–1443. doi: 10.1016/j.bbabio.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 5.Gill A.J., Hes O., Papathomas T., Sedivcova M., Tan P.H., Agaimy A. Succinate dehydrogenase (SDH)-deficient renal carcinoma: a morphologically distinct entity: a clinicopathologic series of 36 tumors from 27 patients. Am. J. Surg. Pathol. Dec 2014;38:1588–1602. doi: 10.1097/PAS.0000000000000292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dwight T., Benn D.E., Clarkson A., Vilain R., Lipton L., Robinson B.G. Loss of SDHA expression identifies SDHA mutations in succinate dehydrogenase-deficient gastrointestinal stromal tumors. Am. J. Surg. Pathol. Feb 2013;37:226–233. doi: 10.1097/PAS.0b013e3182671155. [DOI] [PubMed] [Google Scholar]
- 7.Lenders J.W., Duh Q.-Y., Eisenhofer G., Gimenez-Roqueplo A.-P., Grebe S.K., Murad M.H. Pheochromocytoma and paraganglioma: an endocrine society clinical practice guideline. The Journal of Clinical Endocrinology & Metabolism. 2014;99:1915–1942. doi: 10.1210/jc.2014-1498. [DOI] [PubMed] [Google Scholar]
- 8.Evenepoel L., Papathomas T.G., Krol N., Korpershoek E., de Krijger R.R., Persu A. Toward an improved definition of the genetic and tumor spectrum associated with SDH germ-line mutations. Genetics in Medicine. 2014 doi: 10.1038/gim.2014.162. [DOI] [PubMed] [Google Scholar]
- 9.Denko N.C. Hypoxia, HIF1 and glucose metabolism in the solid tumour. Nat. Rev. Cancer. 2008;8:705–713. doi: 10.1038/nrc2468. [DOI] [PubMed] [Google Scholar]
- 10.Lendvai N., Pawlosky R., Bullova P., Eisenhofer G., Patocs A., Veech R.L. Succinate-to-fumarate ratio as a new metabolic marker to detect the presence of SDHB/D-related paraganglioma: initial experimental and ex vivo findings. Endocrinology. Jan 2014;155:27–32. doi: 10.1210/en.2013-1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Imperiale A., Moussallieh F.-M., Sebag F., Brunaud L., Barlier A., Elbayed K. A new specific succinate-glutamate metabolomic hallmark in SDHx-related paragangliomas. PLoS One. 2013;8:e80539. doi: 10.1371/journal.pone.0080539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Richter S., Peitzsch M., Rapizzi E., Lenders J.W., Qin N., de Cubas A.A. Krebs cycle metabolite profiling for identification and stratification of pheochromocytomas/paragangliomas due to succinate dehydrogenase deficiency. The Journal of Clinical Endocrinology & Metabolism. 2014;99:3903–3911. doi: 10.1210/jc.2014-2151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Crockett D.K., Lin Z., Vaughn C.P., Lim M.S., Elenitoba-Johnson K.S. Identification of proteins from formalin-fixed paraffin-embedded cells by LC-MS/MS. Lab. Investig. 2005;85:1405–1415. doi: 10.1038/labinvest.3700343. [DOI] [PubMed] [Google Scholar]
- 14.Huang S.K., Darfler M.M., Nicholl M.B., You J., Bemis K.G., Tegeler T.J. LC/MS-based quantitative proteomic analysis of paraffin-embedded archival melanomas reveals potential proteomic biomarkers associated with metastasis. PLoS One. 2009;4:e4430. doi: 10.1371/journal.pone.0004430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kelly A.D., Breitkopf S.B., Yuan M., Goldsmith J., Spentzos D., Asara J.M. Metabolomic profiling from formalin-fixed, paraffin-embedded tumor tissue using targeted LC/MS/MS: application in sarcoma. PLoS One. 2011;6:e25357. doi: 10.1371/journal.pone.0025357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wojakowska A., Chekan M., Marczak L., Polanski K., Lange D., Pietrowska M. Detection of metabolites discriminating subtypes of thyroid cancer: molecular profiling of FFPE samples using the GC/MS approach. Mol. Cell. Endocrinol. Sep 28 2015 doi: 10.1016/j.mce.2015.09.021. [DOI] [PubMed] [Google Scholar]
- 17.Wojakowska A., Marczak L., Jelonek K., Polanski K., Widlak P., Pietrowska M. An Optimized Method of Metabolite Extraction from Formalin-Fixed Paraffin-Embedded Tissue for GC/MS Analysis. PLoS One. 2015;10:e0136902. doi: 10.1371/journal.pone.0136902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gill A.J. Succinate dehydrogenase (SDH) and mitochondrial driven neoplasia. Pathology-Journal of the RCPA. 2012;44:285–292. doi: 10.1097/PAT.0b013e3283539932. [DOI] [PubMed] [Google Scholar]
- 19.Miettinen M., Lasota J. Succinate dehydrogenase deficient gastrointestinal stromal tumors (GISTs) — a review. Int. J. Biochem. Cell Biol. Aug 2014;53:514–519. doi: 10.1016/j.biocel.2014.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rustin P. Mitochondria, from cell death to proliferation. Nat. Genet. 2002;30:352–353. doi: 10.1038/ng0402-352. [DOI] [PubMed] [Google Scholar]
- 21.Rustin P., Munnich A., Rotig A. Succinate dehydrogenase and human diseases: new insights into a well-known enzyme. Eur. J. Hum. Genet. 2002;10 doi: 10.1038/sj.ejhg.5200793. [DOI] [PubMed] [Google Scholar]
- 22.Wallace D.C. Mitochondria and cancer. Nat. Rev. Cancer. 2012;12:685–698. doi: 10.1038/nrc3365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vicha A., Taieb D., Pacak K. Current views on cell metabolism in SDHx-related pheochromocytoma and paraganglioma. Endocrine-Related Cancer. 2014;21:R261–R277. doi: 10.1530/ERC-13-0398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gill A.J., Benn D.E., Chou A., Clarkson A., Muljono A., Meyer-Rochow G.Y. Immunohistochemistry for SDHB triages genetic testing of SDHB, SDHC, and SDHD in paraganglioma-pheochromocytoma syndromes. Hum. Pathol. 2010;41:805–814. doi: 10.1016/j.humpath.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 25.Tsang V.H., Dwight T., Benn D.E., Meyer-Rochow G.Y., Gill A.J., Sywak M. Overexpression of miR-210 is associated with SDH-related pheochromocytomas, paragangliomas, and gastrointestinal stromal tumours. Endocr Relat Cancer. Jun 2014;21:415–426. doi: 10.1530/ERC-13-0519. [DOI] [PubMed] [Google Scholar]
- 26.Lussey-Lepoutre C., Hollinshead K.E., Ludwig C., Menara M., Morin A., Castro-Vega L.-J. Loss of succinate dehydrogenase activity results in dependency on pyruvate carboxylation for cellular anabolism. Nat. Commun. 2015;6 doi: 10.1038/ncomms9784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Varoquaux A., le Fur Y., Imperiale A., Reyre A., Montava M., Fakhry N. Magnetic resonance spectroscopy of paragangliomas: new insights into in vivo metabolomics. Endocrine-Related Cancer. 2015;22:M1–M8. doi: 10.1530/ERC-15-0246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Killian J.K., Miettinen M., Walker R.L., Wang Y., Zhu Y.J., Waterfall J.J. Recurrent epimutation of SDHC in gastrointestinal stromal tumors. Sci. Transl. Med. 2014;6:268ra177. doi: 10.1126/scitranslmed.3009961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.S. Richter, B. Klink, B. Nacke, A.A. de Cubas, A. Mangelis, E. Rapizzi et al., "Epigenetic mutation of the succinate dehydrogenase C promoter in a patient with two paragangliomas," The Journal of Clinical Endocrinology & Metabolism, pp. jc. 2015-3856, 2015. [DOI] [PubMed]
- 30.Kim E., Rath E., Tsang V., Duff A., Robinson B., Church W. Structural and functional consequences of succinate dehydrogenase subunit B mutations. Endocrine-Related Cancer. 2015;22:387–397. doi: 10.1530/ERC-15-0099. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
FFPE specimens from 18 cases of PPGLs, 10 cases of GISTs and 11 cases of RCCs with known mutation status.
PPGL FFPE specimens with false-negatives and false-positive succinate:fumarate ratios.
ROC curve for discriminating SDH-deficient PPGLs from SDH-sufficient PPGLs according to succinate:fumarate ratio. Arrow marks cut-off (highest sensitivity and specificity) value. Area under the curve was equal to 0.80.
Scatter plot comparing succinate:fumarate ratio between SDH-sufficient PPGLs with VHL mutation (n = 3) and SDH-deficient PPGLs (n = 9), error bars representing SEM from mean (p > 0.05).
ROC curve for discriminating SDH-deficient GISTs from SDH-sufficient GISTs according to succinate:fumarate ratio. Arrow marks cut-off (highest sensitivity and specificity) value. Area under the curve was equal to 1.0.
ROC curve for discriminating SDH-deficient RCCs from SDH-sufficient RCCs according to succinate:fumarate ratio. Arrow marks cut-off (highest sensitivity and specificity) value. Area under the curve was equal to 1.0.