Abstract
Background and objectives
Diet soda consumption is common in the United States and is associated with impaired glucose metabolism, diabetes, and metabolic syndrome.
Design, setting, participants, & measurements
We prospectively analyzed diet soda consumption, assessed by food frequency questionnaire at baseline (1987–1989) and a follow-up examination (1993–1995), and incident ESRD through December 31, 2012 in the Atherosclerosis Risk in Communities study (n=15,368).
Results
Baseline mean age of participants was 54 years, 55% were female, and 27% were black. The majority of participants (43.5%) consumed <1 glass/wk of diet soda; 17.8% consumed 1–4 glasses/wk; 25.3% consumed 5–7 glasses/wk; and 13.5% consumed >7 glasses/wk. Over a median follow-up of 23 years, 357 incident ESRD cases were observed. Relative to <1 glass/wk of diet soda, consuming 1–4 glasses/wk, 5–7 glasses/wk, and >7 glasses/wk, respectively, was associated with 1.08-times (95% confidence interval [95% CI], 0.75 to 1.55), 1.33-times (95% CI, 1.01 to 1.75), and 1.83-times (95% CI, 1.01 to 2.52) higher risk of ESRD after adjusting for age, sex, race-center, education level, smoking status, physical activity, total caloric intake, eGFR, body mass index category, diabetes, systolic BP, and serum uric acid (P value for trend <0.001). Results were similar after additional adjustment for dietary acid load, diet quality, dietary sodium, dietary fructose, sugar-sweetened beverages, and dietary phosphorus. Risk estimates were similar by body mass index category (P value for interaction = 0.82), but the association between diet soda and ESRD was only significant for those who were overweight or obese at baseline. Sugar-sweetened beverage consumption was not significantly associated with ESRD in the fully adjusted model.
Conclusions
Diet soda consumption was associated with higher ESRD risk in this general population sample. Further research is necessary to validate these findings in other study populations and to examine potential mechanisms through which diet soda could impact kidney disease.
Keywords: atherosclerosis; beverages; blood pressure; body mass index; diabetes, mellitus; diet; energy intake; female; follow-up studies; fructose; glomerular filtration rate; glucose; kidney failure, chronic; metabolic syndrome X; motor activity; obesity; overweight; phosphorus, dietary; smoking; sodium, dietary; surveys and questionnaires; sweetening agents; United States; uric acid
Introduction
Soft drinks are a major source of calories (5% of total caloric intake) and the primary source of added sugar (33% of total added sugar intake) in the United States diet (1). These types of beverages are associated with weight gain, type 2 diabetes mellitus, and cardiovascular disease (2–4). Therefore, the 2015 Dietary Guidelines for Americans and the American Heart Association recommend limiting dietary intake of added sugars, in part, by avoiding soft drinks and other sugar-sweetened beverages (5,6). Numerous policy initiatives have been implemented (e.g., taxing the purchase of soda) to reduce sugar-sweetened beverage consumption at the population-level and to fund health promotion programs (7,8).
As a result of the widespread public awareness of the sugar content, caloric burden, and adverse health consequences of regular soda, diet soda has become an increasingly common substitute in the United States (8,9). Consumption of diet beverages is higher in North America than any other region in the world (8). Recent studies have shown that diet soda and artificial sweeteners contained in diet soda may adversely affect glucose levels, and may increase the risk of developing metabolic syndrome and diabetes, in part, through impairment of glucose and increase in waist circumference (10–12). With respect to kidney disease, the results of the few existing studies on diet soda have been inconsistent and the overall evidence base is inconclusive (13–16).
The objective of this study was to investigate the relationship between diet soda with the development of incident ESRD in a general population sample and to assess the independence of this association from established ESRD risk factors and dietary factors related to diet soda.
Materials and Methods
Study Design
The Atherosclerosis Risk in Communities (ARIC) study is a prospective cohort of 15,792 middle-aged (45–64 years), predominantly black and white men and women from four United States communities: Forsyth County, North Carolina; Jackson, Mississippi; suburbs of Minneapolis, Minnesota; and Washington County, Maryland (17). Participants enrolled in 1987–1989 (baseline, visit 1) and follow-up visits occurred in 1990–1992 (visit 2), 1993–1995 (visit 3), and 1996–1998 (visit 4), with the most recent visit in 2011–2013 (visit 5). The protocol was approved by the Institutional Review Board. Procedures were followed in accordance with the Declaration of Helsinki.
Study Population
After excluding participants with missing diet data (≥10 food items not reported) or implausible total caloric intake (women: <500 or >3500 kcal; men: <700 or >4500 kcal) (n=364); those who were neither black nor white (n=47); and those with baseline eGFR<45 ml/min per 1.73 m2 (n=13), the analytic sample size was 15,368.
Assessment of Diet Soda Intake
Usual dietary intake was assessed by a semiquantitative, 66-item food frequency questionnaire (FFQ) administered by trained interviewers at baseline (1987–1989, visit 1) and a follow-up visit (1993–1995, visit 3) (18). Participants reported how often they consumed food items on average over the past year. Visual aids (glasses, measuring cups) were used to illustrate portion sizes in order to improve accuracy. The reliability of this FFQ was previously demonstrated in a random subset of 419 ARIC study participants who repeated the FFQ at a follow-up visit (visit 2) (19). The cumulative average diet, incorporating data from both assessments of dietary intake (baseline and visit 3), was used to depict beverage intake (20).
Diet soda was described on the FFQ as one 8-ounce glass of low-calorie soft drinks such as Diet Coke, Diet Pepsi, or Diet 7-Up. To provide a more complete assessment of beverage intake, we also assessed sugar-sweetened beverage consumption, which consisted of regular soft drinks (Coke, Pepsi, 7-Up, or ginger ale) as well as fruit-flavored punch or noncarbonated beverages (lemonade, Kool-Aid, or Hawaiian Punch). Consumption frequency was categorized as <1 glass/wk, 1–4 glasses/wk, 5–7 glasses/wk, and >7 glasses/wk.
Ascertainment of Incident ESRD
Incident ESRD was defined as the initiation of RRT (transplant, dialysis) between baseline (1987–1989) and December 31, 2012 as identified by linkage with the US Renal Data System (USRDS) registry. Study participants were censored at the date of death or the end of the observation period for this study (December 31, 2012). In a validation study of this definition of ESRD compared with physician-determined treated kidney failure on the basis of medical chart review in the ARIC study, sensitivity was 95% and specificity was 100% (21).
As a secondary outcome, incident CKD was defined as meeting one of the following criteria: (1) eGFR<60 ml/min per 1.73 m2 at any follow-up visit accompanied by ≥25% eGFR decline, (2) CKD-related hospitalization using International Classification of Diseases-9/10 codes, (3) CKD-related death using International Classification of Diseases-9/10 codes, or (4) USRDS-identified ESRD (22).
Measurement of Covariates
Demographic characteristics (age, sex, race), socioeconomic status (education), health behaviors (smoking, physical activity), and health history (disease diagnosis, medication use) were captured using a structured questionnaire administered by trained interviewers at baseline. A modified Baecke questionnaire was used to create an index of leisure-time sports and exercise, incorporating frequency, duration, and intensity of each type of activity on average over the preceding year (23).
We quantified diet quality with the Alternative Healthy Eating Index 2010, which we modified to exclude alcohol given its missingness (45%) (24). Higher scores represent higher diet quality. Dietary intake of protein, phosphorus, potassium, magnesium, calcium, sodium, and fructose was calculated by combining frequency of consumption, portion size, and nutritional content of each food item on the FFQ. Dietary acid load was estimated with the Remer and Manz equation for potential renal acid load: 0.49 × protein + 0.037 × phosphorus − 0.021 × potassium − 0.026 × magnesium − 0.013 × calcium (25–28).
Weight and height were measured while participants wore light clothing and no shoes, and body mass index (BMI) was categorized as normal (<25 kg/m2), overweight (25 to <30 kg/m2), or obese (≥30 kg/m2). After resting for at least 5 minutes, three measurements of BP were taken using a random-zero sphygmomanometer by a certified technician and the average of the second and third readings was used. Hypertension was defined as systolic BP ≥140 mmHg, diastolic BP ≥90 mmHg, or current use of antihypertensive medication in the preceding 2 weeks. Serum glucose was quantified by the modified hexokinase/glucose-6-phosphate dehydrogenase method. Diabetes was defined as fasting blood glucose ≥126 mg/dl, nonfasting blood glucose ≥200 mg/dl, self-report of diagnosed diabetes, or current use of diabetes medication in the preceding 2 weeks. Serum creatinine was measured by the modified kinetic Jaffe method and standardized to the National Institute of Standards and Technology standard (29). eGFR was estimated using the 2009 CKD Epidemiology Collaboration equation on the basis of creatinine (30). Serum uric acid was measured using the uricase method (31).
Statistical Analyses
Baseline characteristics were examined according to categories of diet soda consumption using descriptive statistics, and differences were tested using a nonparametric test for trend across ordered groups (32).
We used Cox proportional hazards regression to calculate hazard ratios (HR) and 95% confidence intervals (95% CI) for the association between diet soda consumption and incident ESRD risk, incorporating time until ESRD. We conducted a test of linear trend using the median value of diet soda consumption within each category in the regression models. In addition to categorical analysis, diet soda intake was modeled continuously and effect estimates were expressed per one additional glass consumed. We conducted stratified analyses and tested for interaction by sex, race, diabetes status, and BMI category.
Five successive regression models were constructed. Model 1 included demographic characteristics (age, sex, race-center), education level as a proxy for socioeconomic status, health behaviors (smoking status, physical activity), total caloric intake as the standard method for energy adjustment, and baseline eGFR modeled as two linear spline terms with one knot at 90 ml/min per 1.73 m2 considering the nonlinear relationship between eGFR and kidney disease risk and the relatively high level of kidney function in this general population sample (20,33). The race-center interaction term was used given the nonuniform distribution of racial groups across study sites. Model 2 additionally adjusted for comorbidities (BMI category, diabetes, systolic BP, serum uric acid). Models 3a–c investigated the independence of the association between diet soda consumption and ESRD after accounting for dietary factors related to diet soda. To avoid collinearity between multiple dietary factors, they were added to the regression model separately. Model 3a adjusted for dietary acid load in addition to Model 2 covariates. Model 3b adjusted for diet quality (modified Alternative Healthy Eating Index 2010), dietary intake of sodium, dietary intake of fructose, and frequency of sugar-sweetened beverage consumption in addition to Model 2 covariates. Model 3c adjusted for dietary intake of phosphorus and the Model 2 covariates. Analyses were performed using Stata statistical software version 14.1 (StataCorp LP, College Station, TX).
Results
In the overall study population, baseline mean age was 54 years, 55% were female, 27% were black, 12% had diabetes, 35% had hypertension, and baseline mean eGFR was 102.5 ml/min per 1.73 m2. The majority of participants (43.5%) consumed <1 glass/wk of diet soda, 17.8% consumed 1–4 glasses/wk, 25.3% consumed 5–7 glasses/wk, and 13.5% consumed >7 glasses/wk (Table 1). Those who consumed the highest amount of diet soda (>7 glasses/wk) were more likely to be female, white, and obese, and to have diabetes. Higher frequency of diet soda consumption was associated with lower intake of sugar-sweetened beverages and higher dietary intake of phosphorus and dietary acid load (P<0.001).
Table 1.
Baseline characteristics according to categories of diet soda consumption
| Characteristics | Categories of Diet Soda Consumption, glasses/wk | P Value for Trend | |||
|---|---|---|---|---|---|
| <1 | 1–4 | 5–7 | >7 | ||
| (n=6678; 43.5%) | (n=2728; 17.8%) | (n=3885; 25.3%) | (n=2077; 13.5%) | ||
| Age, yr | 54.4 (5.8) | 54.8 (5.6) | 54.0 (5.7) | 52.9 (5.6) | <0.001 |
| Female, % (n) | 52.2 (3486) | 55.5 (1515) | 58.4 (2268) | 58.3 (1210) | <0.001 |
| Black, % (n) | 34.6 (2311) | 21.6 (588) | 23.7 (921) | 14.1 (292) | <0.001 |
| High school education, % (n) | 72.2 (4810) | 81.3 (2215) | 78.3 (3040) | 79.6 (1651) | <0.001 |
| Current smoker, % (n) | 33.3 (2222) | 19.0 (517) | 19.4 (754) | 24.5 (508) | <0.001 |
| Physical activity index | 2.37 (0.78) | 2.49 (0.80) | 2.49 (0.81) | 2.43 (0.79) | 0.001 |
| Fasting glucose, mg/dl | 102.8 (26.7) | 104.9 (29.4) | 111.1 (42.6) | 114.3 (42.0) | <0.001 |
| Diabetes, % (n) | 7.7 (505) | 8.9 (242) | 16.1 (621) | 20.8 (430) | <0.001 |
| SBP, mmHg | 122.0 (19.6) | 120.5 (17.6) | 121.2 (18.8) | 119.9 (17.7) | <0.001 |
| Hypertension, % (n) | 34.8 (2315) | 33.4 (905) | 36.6 (1,414) | 34.6 (717) | 0.65 |
| BMI, kg/m2 | 26.8 (5.2) | 27.5 (5.0) | 28.4 (5.4) | 29.4 (5.7) | <0.001 |
| BMI category | |||||
| Normal (<25 kg/m2), % (n) | 40.0 (2655) | 34.1 (931) | 27.1 (1051) | 21.2 (440) | <0.001 |
| Overweight (25 to <30 kg/m2), % (n) | 38.1 (2543) | 40.4 (1101) | 40.7 (1581) | 40.1 (832) | |
| Obese (≥30 kg/m2), % (n) | 22.1 (1477) | 25.5 (696) | 32.2 (1249) | 38.6 (801) | |
| eGFR, ml/min per 1.73 m2 | 103.2 (16.1) | 101.6 (14.1) | 102.1 (15.7) | 102.4 (15.0) | 0.21 |
| Dietary acid load, mEq/d | 3.7 (12.6) | 3.2 (11.5) | 5.0 (12.1) | 8.1 (13.6) | <0.001 |
| Diet quality score | 42.4 (9.7) | 45.4 (9.2) | 45.6 (9.1) | 44.6 (9.2) | <0.001 |
| SSB, glasses/wk | 5.3 (6.9) | 3.0 (4.2) | 2.5 (4.0) | 2.9 (5.6) | <0.001 |
| Dietary phosphorus, mg/d | 1021 (392) | 1070 (372) | 1088 (370) | 1214 (407) | <0.001 |
| Total caloric intake, kcal | 1645 (572) | 1584 (525) | 1565 (521) | 1680 (566) | 0.02 |
Data are displayed as mean (SD) for continuous variables or indicated as % (n) for categorical variables. SBP, systolic BP; BMI, body mass index; mEq, milliequivalents; SSB, sugar-sweetened beverage.
Over a median follow-up of 23 years, there were 357 incident ESRD cases. Relative to <1 glass/wk of diet soda, consuming 1–4 glasses/wk, 5–7 glasses/wk, and >7 glasses/wk, respectively, was associated with 1.08-times (95% CI, 0.75 to 1.55), 1.33-times (95% CI, 1.01 to 1.75), and 1.83-times (95% CI, 1.01 to 2.52) higher risk of ESRD after adjusting for age, sex, race-center, education level, smoking status, physical activity, total caloric intake, eGFR, BMI category, diabetes, systolic BP, and serum uric acid (Model 2, P value for trend <0.001; Table 2). In the continuous analysis, for each additional glass of diet soda consumed per day, there was a 29% higher risk of ESRD (Model 2, HR, 1.29; 95% CI, 1.16 to 1.43; P<0.001). In both categorical and continuous analyses, effect estimates were similar after additional adjustment for dietary acid load (Model 3a), after accounting for diet quality, dietary sodium, dietary fructose, and sugar-sweetened beverage consumption (Model 3b), and after adjusting for dietary intake of phosphorus (Model 3c). Results were similar, although attenuated, for the association between diet soda consumption and the secondary outcome of incident CKD (Supplemental Table 1).
Table 2.
Risk (95% CI) of incident ESRD by frequency of diet soda consumption
| Variables | Categories of Diet Soda Consumption, glasses/wk | P Value for Trend | Continuous Diet Soda Consumption | ||||
|---|---|---|---|---|---|---|---|
| <1 (n=6678) | 1–4 (n=2728) | 5–7 (n=3885) | >7 (n=2077) | HR (95% CI) | P value | ||
| ESRD, n (%) | 125 (1.9) | 42 (1.5) | 116 (3.0) | 73 (3.5) | <0.001 | – | – |
| Model 1 | 1 (Ref) | 1.32 (0.91 to 1.89) | 2.21 (1.69 to 2.88) | 3.27 (2.40 to 4.45) | <0.001 | 1.53 (1.40 to 1.67) | <0.001 |
| Model 2 | 1 (Ref) | 1.08 (0.75 to 1.55) | 1.33 (1.01 to 1.75) | 1.83 (1.01 to 2.52) | <0.001 | 1.29 (1.16 to 1.43) | <0.001 |
| Model 3a | 1 (Ref) | 1.08 (0.75 to 1.55) | 1.33 (1.01 to 1.75) | 1.83 (1.33 to 2.53) | <0.001 | 1.29 (1.17 to 1.43) | <0.001 |
| Model 3b | 1 (Ref) | 1.03 (0.71 to 1.48) | 1.22 (0.92 to 1.62) | 1.71 (1.23 to 2.38) | 0.001 | 1.27 (1.14 to 1.41) | <0.001 |
| Model 3c | 1 (Ref) | 1.03 (0.71 to 1.48) | 1.24 (0.94 to 1.64) | 1.64 (1.18 to 2.28) | 0.002 | 1.25 (1.12 to 1.39) | <0.001 |
Model 1: Adjusted for age, sex, race-center, education level, smoking status, physical activity, total caloric intake, baseline eGFR (linear spline terms with one knot at 90 ml/min per 1.73 m2). Model 2: Model 1 + body mass index category, diabetes, systolic BP, serum uric acid. Model 3a: Model 2 + dietary acid load. Model 3b: Model 2 + diet quality (modified Alternative Healthy Eating Index 2010), dietary sodium, dietary fructose, frequency of consumption of sugar-sweetened beverages. Model 3c: Model 2 + dietary phosphorus. 95% CI, 95% confidence interval; HR, hazard ratio; –, not applicable.
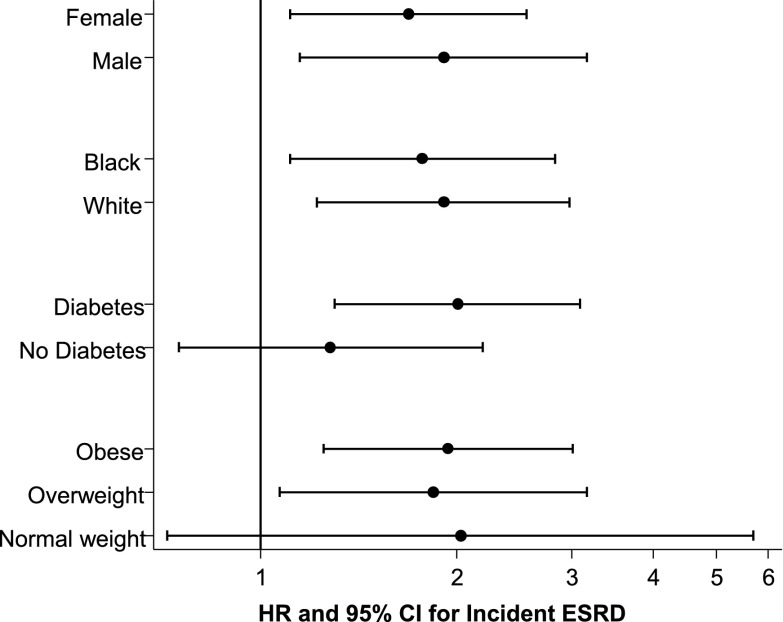
ESRD risk for the highest versus lowest categories of diet soda consumption were similar by sex (P value for interaction = 0.59) and racial group (P value for interaction = 0.41; Figure 1). Associations were slightly stronger among those with diabetes and not significant among those without diabetes, but there was no statistical evidence of interaction (P value for interaction = 0.34). Although risk estimates were similar by BMI category (P value for interaction = 0.82), the association between diet soda and ESRD was only significant for those who were overweight or obese at baseline.
Figure 1.
Risk of incident ESRD for highest versus lowest consumption frequency category for diet soda in subgroups of the study population. Adjusted for age, sex, race-center, education level, smoking status, physical activity, total caloric intake, baseline eGFR (linear spline terms with one knot at 90 ml/min per 1.73 m2), body mass index category, diabetes, systolic BP, and serum uric acid. 95% CI, 95% confidence interval; HR, hazard ratio.
In the minimally adjusted model (Model 1), the highest (>7 glasses/wk) versus lowest (<1 glass/wk) consumption category for sugar-sweetened beverages appeared to be associated with lower risk of incident ESRD (Table 3). This association was no longer statistically significant in nearly all subsequent models with further adjustment.
Table 3.
Risk (95% CI) of incident ESRD by frequency of sugar-sweetened beverage consumption
| Variables | Categories of SSB Consumption, glasses/wk | P value for trend | Continuous SSB Consumption | ||||
|---|---|---|---|---|---|---|---|
| <1 (n=5204) | 1–4 (n=3766) | 5–7 (n=3870) | >7 (n=2525) | HR (95% CI) | P value | ||
| ESRD, n (%) | 117 (2.3) | 92 (2.4) | 101 (2.6) | 46 (1.8) | 0.23 | – | – |
| Model 1 | 1 (Ref) | 0.90 (0.68 to 1.19) | 0.58 (0.43 to 0.78) | 0.32 (0.21 to 0.47) | <0.001 | 0.63 (0.52 to 0.77) | <0.001 |
| Model 2 | 1 (Ref) | 1.30 (0.88 to 1.92) | 1.12 (0.74 to 1.71) | 0.68 (0.40 to 1.16) | 0.05 | 0.86 (0.68 to 1.08) | 0.20 |
| Model 3a | 1 (Ref) | 1.30 (0.88 to 1.92) | 1.12 (0.74 to 1.70) | 0.68 (0.40 to 1.16) | 0.05 | 0.86 (0.68 to 1.08) | 0.20 |
| Model 3b | 1 (Ref) | 1.35 (0.91 to 2.01) | 1.09 (0.69 to 1.71) | 0.52 (0.27 to 1.00) | 0.01 | 0.73 (0.53 to 0.99) | 0.05 |
| Model 3c | 1 (Ref) | 1.32 (0.89 to 1.96) | 1.16 (0.76 to 1.79) | 0.73 (0.41 to 1.32) | 0.11 | 0.90 (0.69 to 1.16) | 0.42 |
Model 1: Adjusted for age, sex, race-center, education level, smoking status, physical activity, total caloric intake, baseline eGFR (linear spline terms with one knot at 90 ml/min per 1.73 m2). Model 2: Model 1 + body mass index category, diabetes, systolic BP, serum uric acid. Model 3a: Model 2 + dietary acid load. Model 3b: Model 2 + diet quality (modified Alternative Healthy Eating Index 2010), dietary sodium, dietary fructose, frequency of consumption of diet soda. Model 3c: Model 2 + dietary phosphorus. 95% CI, 95% confidence interval; SBB, sugar-sweetened beverage; HR, hazard ratio; –, not applicable.
Discussion
In this diverse, community-based population of 15,368 black and white men and women, higher consumption of diet soda was associated with a graded risk of developing ESRD over a median follow-up of 23 years. This dose-response relationship was independent of several known ESRD risk factors and other dietary factors related to diet soda, and results were consistent in population subgroups.
To the best of our knowledge, this study is the first to report an association between diet soda and incident ESRD. There is a paucity of literature on diet soda and other artificially-sweetened beverages, and only a few studies have related this beverage type to kidney outcomes. In a subset of 3318 participants in the Nurses’ Health Study, a study population which is predominantly white and exclusively female, consuming ≥2 artificially-sweetened beverages per day relative to <1 per month was associated with a 2-fold higher risk of ≥30% eGFR decline after adjusting for age, caloric intake, hypertension, BMI, diabetes, cigarette smoking, physical activity, and cardiovascular disease (odds ratio, 2.02; 95% CI, 1.36 to 3.01) (14). These investigators found a similar association with rapid eGFR decline defined as ≥3 ml/min per 1.73 m2 per year (odds ratio, 2.20; 95% CI, 1.36 to 3.55). A case-control study was conducted in 1980–1983 with 465 CKD patients from four North Carolina hospitals and 467 community-dwelling controls with frequency matching on age, sex, race, and proximity to a study hospital (15). After restricting the analysis to self-respondents only (214 cases and 422 controls), drinking ≥2 artificially-sweetened sodas/d relative to never or <1 drink/wk was significantly associated with CKD after adjusting for matching factors, BMI, income, education, analgesic use, and diabetes (odds ratio, 4.21; 95% CI, 1.21 to 14.61). In a cross-sectional analysis of 9358 participants in the 1999–2004 National Health and Nutrition Examination Survey (NHANES), diet soda consumption was not associated with albuminuria after adjusting for sugar-sweetened soda consumption, age, race-ethnicity, gender, and poverty status (odds ratio, 0.94; 95% CI, 0.64 to 1.39) (16). Inconsistency in the literature may be due to differences in study design, outcome definition, exposure classification, and covariates. Replicating these findings will be essential to establishing more definitive knowledge about the kidney health implications of artificially-sweetened beverage intake.
There are several potential mechanisms through which diet soda could cause renal damage. Sodas (both diet and regular) contain phosphorus as an additive for color and flavor (34). Dietary phosphorus may affect serum levels of phosphorus and fibroblast growth factor-23 (35,36). In a separate analysis of the ARIC study, the highest versus lowest quintile of fibroblast growth factor-23 was associated with a 2-fold higher risk of incident ESRD (37). Driven by its phosphorus content, diet soda could increase dietary acid load and thereby increase kidney disease risk (27,28). In another ARIC study analysis, the highest versus lowest quartile of dietary acid load was associated with 1.13-times higher risk of developing CKD (26). Alternatively, high consumption of diet soda could be perceived as a proxy for poor diet quality, considering that diet soda is often consumed as a substitute for sugar-sweetened beverages in an attempt to reduce caloric intake and body weight. Poor diet quality has been assessed by various indices and shown to increase the risk of albuminuria and kidney function decline (38). However, we evaluated these dietary factors in multivariable regression models and found that the association between diet soda and ESRD was independent of diet quality, dietary acid load, and dietary intake of phosphorus.
Diet soda consumption could also plausibly affect kidney disease risk by modifying glucose metabolism. In the ARIC study, higher consumption of diet soda was associated with incident metabolic syndrome, which, in part, is defined by hyperglycemia and treatment for diabetes (11). In the Multi-Ethnic Study of Atherosclerosis, higher diet soda consumption was associated with incident diabetes, incident metabolic syndrome, and individual components of metabolic syndrome (waist circumference and glucose) (12). Others have shown that artificial sweeteners are associated with glucose intolerance through alterations in intestinal bacteria (10). Alterations in the gut microbiome are associated with inflammation and several chronic conditions including obesity, cardiovascular disease, and CKD (39,40). It should also be noted that the findings for beverage consumption (diet soda and sugar-sweetened beverages) from epidemiologic studies versus clinical trials are sometimes inconsistent (41). Taken together, these findings suggest that high consumption of diet soda could induce metabolic changes, development of metabolic disorders and diabetes, and thereby increase the risk of kidney disease. In this study, there was no statistical evidence of interaction by diabetes status and associations persisted after adjusting for diabetes status.
There are strengths and limitations of our study to acknowledge. The main study limitation is that the dietary data were self-reported and, as such, could be affected by measurement error. Further, although the FFQ can be used to rank individuals according to frequency of consumption of food items (e.g., diet soda), it is not the ideal instrument for quantifying absolute amounts of micronutrients (e.g., dietary intake of phosphorus). Those individuals with diagnosed disease, including diabetes, may have modified their diet for disease management. Specifically, the study participants who were classified as high consumers of diet soda in our study could have substituted this beverage after receiving counseling to reduce their dietary intake of sugar-sweetened beverages for the purpose of weight loss or glycemic control (42). Therefore, dietary intake assessed at visits 1 and 3 may not represent the relevant exposure period for individuals with comorbidities – diabetes and obesity in particular. Another limitation is the lack of measurement of albuminuria. As a result, we were unable to adjust for this covariate and we were unable to incorporate albuminuria into our outcome definition. However, diet soda consumption was not associated with albuminuria in NHANES; thus, albuminuria is not likely to confound the observed association (16). The regression models that include potential mediating factors (models 2–3c) remove some of the true association between diet soda consumption and ESRD risk; thus, these hazard ratios may be under-estimated. The association between diet soda and earlier stages of kidney disease was weaker than that for more advanced kidney disease. Residual confounding due to unmeasured or imprecisely measured confounders could, in part, explain the observed association. The primary study strengths mainly relate to the study design. Given the large sample size (n=15,368) and long-term follow-up (median=23 years) in the ARIC study, we were able to ascertain a sufficient number of cases of the clinically-relevant and validated outcome of ESRD (n=357) (21). The ARIC study population is more diverse than prior studies on this topic and is representative of middle-aged black and white men and women from several United States communities.
In conclusion, there was a dose-response relationship between diet soda consumption and ESRD risk. Given the high prevalence of diet soda consumption in the United States, this finding could have a significant public health effect. Further research is needed to validate these findings in other study populations as well as to examine mechanisms through which diet soda could affect kidney disease risk.
Disclosures
None.
Supplementary Material
Acknowledgments
The authors thank the staff and participants of the Atherosclerosis Risk in Communities (ARIC) study for their important contributions. The ARIC study is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute contracts (HHSN268201100005C, HHSN268201100006C, HHSN268201100007C, HHSN268201100008C, HHSN268201100009C, HHSN268201100010C, HHSN268201100011C, and HHSN268201100012C).
C.M.R. is supported by grant K01 DK107782, M.E.G. is supported by grant K08 DK092287, and D.C.C. is supported by grant K23 DK097184, all from the National Institute of Diabetes and Digestive and Kidney Diseases.
Parts of this study were presented in abstract form at the American Heart Association Epidemiology and Prevention/Lifestyle and Cardiometabolic Health Scientific Sessions held March 1–4, 2016 in Phoenix, Arizona.
Some of the data reported here have been supplied by the US Renal Data System. The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as official policy or interpretation of the United States government.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.03390316/-/DCSupplemental.
References
- 1.Huth PJ, Fulgoni VL, Keast DR, Park K, Auestad N: Major food sources of calories, added sugars, and saturated fat and their contribution to essential nutrient intakes in the U.S. diet: data from the National Health and Nutrition Examination Survey (2003-2006). Nutr J 12: 116, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vartanian LR, Schwartz MB, Brownell KD: Effects of soft drink consumption on nutrition and health: a systematic review and meta-analysis. Am J Public Health 97: 667–675, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schulze MB, Manson JE, Ludwig DS, Colditz GA, Stampfer MJ, Willett WC, Hu FB: Sugar-sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle-aged women. JAMA 292: 927–934, 2004 [DOI] [PubMed] [Google Scholar]
- 4.Malik VS, Popkin BM, Bray GA, Després JP, Hu FB: Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation 121: 1356–1364, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.US Department of Agriculture and US Department of Health and Human Services : Dietary Guidelines for Americans, 2015-2020, Washington, DC, U.S. Government Printing Office, 2015 [Google Scholar]
- 6.Johnson RK, Appel LJ, Brands M, Howard BV, Lefevre M, Lustig RH, Sacks F, Steffen LM, Wylie-Rosett J; American Heart Association Nutrition Committee of the Council on Nutrition, Physical Activity, and Metabolism and the Council on Epidemiology and Prevention : Dietary sugars intake and cardiovascular health: a scientific statement from the American Heart Association. Circulation 120: 1011–1020, 2009 [DOI] [PubMed] [Google Scholar]
- 7.Jacobson MF, Brownell KD: Small taxes on soft drinks and snack foods to promote health. Am J Public Health 90: 854–857, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Popkin BM, Hawkes C: Sweetening of the global diet, particularly beverages: patterns, trends, and policy responses. Lancet Diabetes Endocrinol 4: 174–186, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Singh GM: Sugar sweetened beverages are associated with greater incidence of diabetes but there is a paucity of evidence on healthfulness of artificially-sweetened beverages and fruit juices. Evid Based Med 21: 35, 2016 [DOI] [PubMed] [Google Scholar]
- 10.Suez J, Korem T, Zeevi D, Zilberman-Schapira G, Thaiss CA, Maza O, Israeli D, Zmora N, Gilad S, Weinberger A, Kuperman Y, Harmelin A, Kolodkin-Gal I, Shapiro H, Halpern Z, Segal E, Elinav E: Artificial sweeteners induce glucose intolerance by altering the gut microbiota. Nature 514: 181–186, 2014 [DOI] [PubMed] [Google Scholar]
- 11.Lutsey PL, Steffen LM, Stevens J: Dietary intake and the development of the metabolic syndrome: the Atherosclerosis Risk in Communities study. Circulation 117: 754–761, 2008 [DOI] [PubMed] [Google Scholar]
- 12.Nettleton JA, Lutsey PL, Wang Y, Lima JA, Michos ED, Jacobs DR Jr : Diet soda intake and risk of incident metabolic syndrome and type 2 diabetes in the Multi-Ethnic Study of Atherosclerosis (MESA). Diabetes Care 32: 688–694, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Karalius VP, Shoham DA: Dietary sugar and artificial sweetener intake and chronic kidney disease: a review. Adv Chronic Kidney Dis 20: 157–164, 2013 [DOI] [PubMed] [Google Scholar]
- 14.Lin J, Curhan GC: Associations of sugar and artificially sweetened soda with albuminuria and kidney function decline in women. Clin J Am Soc Nephrol 6: 160–166, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Saldana TM, Basso O, Darden R, Sandler DP: Carbonated beverages and chronic kidney disease. Epidemiology 18: 501–506, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shoham DA, Durazo-Arvizu R, Kramer H, Luke A, Vupputuri S, Kshirsagar A, Cooper RS: Sugary soda consumption and albuminuria: results from the National Health and Nutrition Examination Survey, 1999-2004. PLoS One 3: e3431, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.The ARIC Investigators : The Atherosclerosis Risk in Communities (ARIC) study: design and objectives. The ARIC investigators. Am J Epidemiol 129: 687–702, 1989 [PubMed] [Google Scholar]
- 18.Shimakawa T, Sorlie P, Carpenter MA, Dennis B, Tell GS, Watson R, Williams OD; ARIC Study Investigators : Dietary intake patterns and sociodemographic factors in the atherosclerosis risk in communities study. Prev Med 23: 769–780, 1994 [DOI] [PubMed] [Google Scholar]
- 19.Stevens J, Metcalf PA, Dennis BH, Tell GS, Shimakawa T, Folsom AR: Reliability of a food frequency questionnaire by ethnicity, gender, age and education. Nutr Res 16: 735–745, 1996 [Google Scholar]
- 20.Hu FB, Stampfer MJ, Rimm E, Ascherio A, Rosner BA, Spiegelman D, Willett WC: Dietary fat and coronary heart disease: A comparison of approaches for adjusting for total energy intake and modeling repeated dietary measurements. Am J Epidemiol 149: 531–540, 1999 [DOI] [PubMed] [Google Scholar]
- 21.Rebholz CM, Coresh J, Ballew SH, McMahon B, Whelton SP, Selvin E, Grams ME: Kidney Failure and ESRD in the Atherosclerosis Risk in Communities (ARIC) study: Comparing Ascertainment of Treated and Untreated Kidney Failure in a Cohort study. Am J Kidney Dis 66: 231–239, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grams ME, Rebholz CM, McMahon B, Whelton S, Ballew SH, Selvin E, Wruck L, Coresh J: Identification of incident CKD stage 3 in research studies. Am J Kidney Dis 64: 214–221, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Baecke JA, Burema J, Frijters JE: A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr 36: 936–942, 1982 [DOI] [PubMed] [Google Scholar]
- 24.Chiuve SE, Fung TT, Rimm EB, Hu FB, McCullough ML, Wang M, Stampfer MJ, Willett WC: Alternative dietary indices both strongly predict risk of chronic disease. J Nutr 142: 1009–1018, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Remer T, Manz F: Potential renal acid load of foods and its influence on urine pH. J Am Diet Assoc 95: 791–797, 1995 [DOI] [PubMed] [Google Scholar]
- 26.Rebholz CM, Coresh J, Grams ME, Steffen LM, Anderson CA, Appel LJ, Crews DC: Dietary acid load and incident chronic kidney disease: Results from the ARIC study. Am J Nephrol 42: 427–435, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Banerjee T, Crews DC, Wesson DE, Tilea A, Saran R, Rios Burrows N, Williams DE, Powe NR; Centers for Disease Control and Prevention Chronic Kidney Disease Surveillance Team : Dietary acid load and chronic kidney disease among adults in the United States. BMC Nephrol 15: 137, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Banerjee T, Crews DC, Wesson DE, Tilea AM, Saran R, Ríos-Burrows N, Williams DE, Powe NR; Centers for Disease Control and Prevention Chronic Kidney Disease Surveillance Team : High dietary acid load predicts ESRD among adults with CKD. J Am Soc Nephrol 26: 1693–1700, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lustgarten JA, Wenk RE: Simple, rapid, kinetic method for serum creatinine measurement. Clin Chem 18: 1419–1422, 1972 [PubMed] [Google Scholar]
- 30.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd , Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J; CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) : A new equation to estimate glomerular filtration rate. Ann Intern Med 150: 604–612, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Iribarren C, Folsom AR, Eckfeldt JH, McGovern PG, Nieto FJ: Correlates of uric acid and its association with asymptomatic carotid atherosclerosis: the ARIC study. Atherosclerosis Risk in Communities. Ann Epidemiol 6: 331–340, 1996 [DOI] [PubMed] [Google Scholar]
- 32.Cuzick J: A Wilcoxon-type test for trend. Stat Med 4: 87–90, 1985 [DOI] [PubMed] [Google Scholar]
- 33.Willett WC, Howe GR, Kushi LH: Adjustment for total energy intake in epidemiologic studies. Am J Clin Nutr 65: 1220S–1228S; discussion 1229S–1231S, 1997 [DOI] [PubMed]
- 34.Moser M, White K, Henry B, Oh S, Miller ER, Anderson CA, Benjamin J, Charleston J, Appel LJ, Chang AR: Phosphorus content of popular beverages. Am J Kidney Dis 65: 969–971, 2015 [DOI] [PubMed] [Google Scholar]
- 35.Scialla JJ, Wolf M: Roles of phosphate and fibroblast growth factor 23 in cardiovascular disease. Nat Rev Nephrol 10: 268–278, 2014 [DOI] [PubMed] [Google Scholar]
- 36.Ix JH, Anderson CA, Smits G, Persky MS, Block GA: Effect of dietary phosphate intake on the circadian rhythm of serum phosphate concentrations in chronic kidney disease: a crossover study. Am J Clin Nutr 100: 1392–1397, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rebholz CM, Grams ME, Coresh J, Selvin E, Inker LA, Levey AS, Kimmel PL, Vasan RS, Eckfeldt JH, Feldman HI, Hsu CY, Lutsey PL; Chronic Kidney Disease Biomarkers Consortium : Serum fibroblast growth factor-23 is associated with incident kidney disease. J Am Soc Nephrol 26: 192–200, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lin J, Fung TT, Hu FB, Curhan GC: Association of dietary patterns with albuminuria and kidney function decline in older white women: a subgroup analysis from the Nurses’ Health study. Am J Kidney Dis 57: 245–254, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wong JM: Gut microbiota and cardiometabolic outcomes: influence of dietary patterns and their associated components. Am J Clin Nutr 100[Suppl 1]: 369S–377S, 2014 [DOI] [PubMed] [Google Scholar]
- 40.Sabatino A, Regolisti G, Brusasco I, Cabassi A, Morabito S, Fiaccadori E: Alterations of intestinal barrier and microbiota in chronic kidney disease. Nephrol Dial Transplant 30: 924–933, 2015 [DOI] [PubMed] [Google Scholar]
- 41.Bellisle F, Drewnowski A: Intense sweeteners, energy intake and the control of body weight. Eur J Clin Nutr 61: 691–700, 2007 [DOI] [PubMed] [Google Scholar]
- 42.Mullie P, Aerenhouts D, Clarys P: Demographic, socioeconomic and nutritional determinants of daily versus non-daily sugar-sweetened and artificially sweetened beverage consumption. Eur J Clin Nutr 66: 150–155, 2012 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.