Abstract
Context:
Specific movement patterns have been identified as possible risk factors for noncontact lower extremity injuries. The Dynamic Integrated Movement Enhancement (DIME) was developed to modify these movement patterns to decrease injury risk.
Objective:
To determine if the DIME is effective for preventing lower extremity injuries in US Military Academy (USMA) cadets.
Design:
Cluster-randomized controlled trial.
Setting:
Cadet Basic Training at USMA.
Patients or Other Participants:
Participants were 1313 cadets (1070 men, 243 women).
Intervention(s):
Participants were cluster randomized to 3 groups. The active warm-up (AWU) group performed standard Army warm-up exercises. The DIME groups were assigned to a DIME cadre-supervised (DCS) group or a DIME expert-supervised (DES) group; the former consisted of cadet supervision and the latter combined cadet and health professional supervision. Groups performed exercises 3 times weekly for 6 weeks.
Main Outcome Measure(s):
Cumulative risk of lower extremity injury was the primary outcome. We gathered data during Cadet Basic Training and for 9 months during the subsequent academic year. Risk ratios and 95% confidence intervals (CIs) were calculated to compare groups.
Results:
No differences were seen between the AWU and the combined DIME (DCS and DES) groups during Cadet Basic Training or the academic year. During the academic year, lower extremity injury risk in the DES group decreased 41% (relative risk [RR] = 0.59; 95% CI = 0.38, 0.93; P = .02) compared with the DCS group; a nonsignificant 25% (RR = 0.75; 95% CI = 0.49, 1.14; P = .18) decrease occurred in the DES group compared with the AWU group. Finally, there was a nonsignificant 27% (RR = 1.27; 95% CI = 0.90, 1.78; P = .17) increase in injury risk during the academic year in the DCS group compared with the AWU group.
Conclusions:
We observed no differences in lower extremity injury risk between the AWU and combined DIME groups. However, the magnitude and direction of the risk ratios in the DES group compared with the AWU group, although not statistically significant, indicate that professional supervision may be a factor in the success of injury-prevention programs.
Key Words: warm-ups, exercises, Dynamic Integrated Movement Enhancement
Key Points
Professional supervision may be a factor in the success of injury-prevention programs.
Cadets who performed the Dynamic Integrated Movement Enhancement program with professional supervision from a certified athletic trainer or physical therapist had a reduction in the risk of acute knee-joint injury compared with cadets who performed the same exercises without professional supervision.
Although exercises led by medically trained personnel may currently be the most effective, programs led by nonmedical personnel will ultimately be required to maximize the benefits of injury-prevention exercises on public health.
More than 800 000 military service members are injured each year, leading to an estimated 25 000 000 days of limited duty annually.1 These injuries range from minor strains and contusions to major ligamentous sprains and bony fractures. Most of these injuries are musculoskeletal in nature and predominantly affect the lower extremity. Although the more severe injuries can lead to a significant loss of training time and long-term sequelae, even mild injuries can result in decreased participation in sport and exercise, which could contribute to a lack of readiness, poorer overall fitness, and obesity.2 At the military academies, cadets sustain injuries that are similar to those of their active-duty counterparts. However, they also have injury risks that are more closely related to those of collegiate athletes as all cadets are required to participate in intercollegiate, club level, or intramural athletics as well as mandatory physical education classes.
Because of the number of potentially negative outcomes associated with training and athletic injuries, effective injury-prevention measures in military and athletic populations are urgently needed.3,4 Within the military, researchers4 have demonstrated a 20% to 30% reduction in injuries when implementing programs that are designed to improve trunk control, agility, and multiaxial movement skills. Among athletes, similar strategies have been used to prevent anterior cruciate ligament (ACL) injury.5–11 Although several groups have demonstrated a decreased risk of injury after an exercise intervention,8,9,12,13 others using very similar programs have not found a decreased risk.14–17 Currently, it is unclear precisely why some programs have successfully mitigated risk whereas others have not, but authors5 of a meta-analysis of injury-prevention program factors noted that the level of supervision was associated with program success. However, no previous researchers have prospectively examined the effect of different levels of injury-prevention–program supervision on injury outcomes.
Another possible reason for the inconsistency of previous injury-prevention efforts is a lack of understanding regarding the modifiable, prospective risk factors for subsequent injury. Previous investigators18 have identified modifiable high-risk movement patterns, such as limited sagittal-plane motion and medial knee displacement, which may contribute to an increased risk of lower extremity injury. The Dynamic Integrated Movement Enhancement (DIME) warm-up was developed to train athletes to avoid these high-risk movement patterns. The DIME consists of 10 exercises that are designed to be performed before engaging in sports or other intense physical training. Although the primary purpose of creating the DIME program was to prevent ACL injuries, previous injury-prevention research suggests that exercise programs that focus on improving movement quality may also decrease the risk for other lower extremity injuries, such as shin splints, patellar tendinopathy, patellofemoral pain, iliotibial band syndrome, and plantar fasciitis due to similar risk factors as for ACL injuries.8,18,19
The objective of our initial study was to determine if implementing the DIME program in a military training environment would reduce the injury risk in this population. Specifically, we examined whether implementing the DIME program during 6 weeks of military training could effectively reduce the overall risk of lower extremity injury in incoming US Military Academy (USMA) cadets during Cadet Basic Training (CBT) and the subsequent academic year. A secondary objective of our study was to determine if the level of supervision was an important factor associated with injury reduction in the DIME group. We also had a specific interest in examining how the DIME program affected the cumulative incidence of acute traumatic knee-joint injuries during the follow-up period. Our hypothesis was that a group of cadets performing the DIME warm-up with supervision from a certified athletic trainer (AT) or physical therapist (PT) would have a reduction in injury risk compared with cadets performing the DIME warm-up without professional supervision from an AT or a PT.
METHODS
Design and Setting
We conducted a cluster-randomized trial during CBT at the US Military Academy to determine if the DIME program was effective in reducing the injury risk in military academy cadets. Each cadet is assigned by the military academy to a company of about 160 cadets. Participants were cluster randomized at the level of their CBT companies into 1 of 2 warm-up groups: (1) 4 companies were assigned to the active warm-up (AWU) group, which served as an active-control condition; (2) the other 4 companies were assigned to the DIME warm-up group. The companies in the DIME group were further randomized as follows: (1) 2 companies were assigned to the DIME cadre-supervised (DCS) group, which performed the DIME warm-up under the supervision of upper-class cadet instructors only and (2) 2 companies were assigned to the DIME expert-supervised (DES) group and performed the DIME warm-up under the direction of the upper-class cadet instructors with the additional supervision of an AT or a PT. Each group performed warm-up exercises 3 times per week for a duration of approximately 10 minutes immediately before physical training as part of the cadet physical fitness program for 6 weeks. The primary outcome of interest was injury risk by intervention group. The study protocol was approved by the institutional review board at our institution before implementation.
Participants
We recruited college freshmen from the incoming class of new cadets at the USMA during the summer of 2010. The 1374 new cadets were given an informed consent briefing. After the briefing, 1313 new cadets (n = 243 women, n = 1070 men; age range = 18–22 years) volunteered to participate in this study. All cadets performed the warm-up program assigned to their military company; however, data were collected and analyzed only for those who provided informed consent.
Intervention
We used a “train the trainer” approach to the DIME program implementation. Several of the authors (D.A.P., S.W.M., L.J.D., S.J.M., A.I.B.) who developed the DIME program trained other members of the study staff, which consisted of ATs and PTs with 1 to 10 years of clinical experience. The study staff then provided standardized training to the faculty in the USMA Department of Physical Education (DPE) regarding the implementation of the DIME program. The study staff supervised and assisted the DPE faculty in training the upper-class cadet instructors (exercise instructors) to implement and deliver the DIME program. All exercise instructors in the DIME groups completed six 30-minute training sessions with the DPE faculty and the study staff to learn, practice, and provide feedback on the proper execution of their group's assigned warm-up exercises. Instructors in the AWU group were also trained in six 30-minute sessions. However, their training was conducted by staff from the USMA DPE without input from the study staff. The training for all groups was standardized; the only difference was the exercises for the programs being implemented. Within each company, the participants (cadets) were divided into groups of approximately 40, which were called platoons. Each platoon was led by a primary exercise instructor who demonstrated exercises while counting repetitions and issuing commands. Additionally, 5 other exercise instructors in each platoon provided feedback and made corrections as the participants performed the warm-up exercises.
The AWU consisted of 10 standard exercises that are commonly used throughout the US Army before unit physical fitness training (Appendix 1).20 The exercises were performed in a group setting using a slow to moderate cadence. The other 2 groups performed the DIME warm-up program before engaging in exercise (Appendix 2). Although both groups performed the DIME warm-up under the direction of the upper-class cadet instructors, for the DES group, a member of the study staff (AT or PT) was assigned to each platoon, was visibly present during all exercise sessions, and provided instant verbal and written feedback to the exercise leaders regarding proper execution of the DIME exercises after each session. Because of academy regulations, study staff were not allowed to directly correct individual new cadets who were performing exercises incorrectly. Instead, the study staff provided instruction and correction to the upper-class cadet exercise leaders and called out verbal cues such as “knees over toes” or “toes straight ahead,” which were clearly audible to all of the new cadets and the upper-class cadre. For the DCS group, exercise instructors were observed for compliance during the implementation and execution of warm-up exercises but did not receive further active instruction or feedback in their execution of the DIME warm-up.
Immediately after the individual group warm-up programs, all groups conducted the same physical training regimen. This regimen consisted of group runs for 2 to 4 mi (3.2 to 6.4 km) at least 2 or 3 times per week. A weekly foot march took place at a distance progressively increasing from 3 to 12 mi (4.8 to 19.3 km) with a rucksack (backpack) weighing 35 lb (15.9 kg). Cadets also performed strength training at least once per week, which consisted primarily of pull-ups, dips, push-ups, and sit-ups. All exercises were performed in a group setting under the direction of the upper-class cadet leadership. The cadets performed this routine throughout their 6 weeks of CBT.
After 3 weeks of training, all of the upper-class instructors for all groups were replaced by a second group of upper-class cadet instructors. This change was done to satisfy USMA summer training requirements for the upper-class cadets. The second group of instructors was trained according to the same standard as the first group with 6 training sessions lasting 30 minutes. When the second group of instructors assumed responsibility for exercise instruction, the exercises in the DIME groups were progressed to a more advanced set. These exercises included a progression from bilateral jumping to unilateral hopping, progression from a forward-plank exercise to a unilateral plank, and from a unilateral balance exercise to a unilateral squat and reach. Although the level of difficulty of the DIME exercises increased, the overall volume of training exercises and the time spent performing warm-up exercises was unchanged. The AWU group performed the same exercises through the duration of CBT.
After the completion of CBT, study personnel did not intervene further during the academic year. Cadets resumed their typical physical activities, including daily intercollegiate, competitive club, or intramural sport participation; physical education classes 2 or 3 days per week; and individual physical fitness programs.
Injury Outcomes
The primary outcome of interest in our study was the cumulative incidence, as measured by the epidemiologic incidence proportion, of musculoskeletal injury to the lower extremities during 3 time frames (CBT, academic year, and CBT and academic year combined).21 Lower extremity musculoskeletal injury was defined as the first musculoskeletal injury to the lower extremity for each participant during the follow-up period that was severe enough to cause him or her to seek treatment from a medical provider. Contusions, lacerations, and skin conditions were not considered lower extremity injuries. In addition to lower extremity injury, we were also interested in the specific risk of acute traumatic knee-joint injury and ACL injury as secondary outcomes of interest. Acute knee-joint injury was defined as any traumatic injury to the ligamentous or meniscal structures of the knee. Participants were dichotomized as being injured or not injured. Multiple injuries to the same participant were not counted. This decision was made because participants who sustained injuries could have subsequent limitations on activities, use crutches for a time, or have a surgical intervention, any of which could confound any attempt to relate future injuries to the previous intervention. Thus, data from participants who were injured during CBT were not analyzed for the academic year period. Injuries occurring from June 30, 2010, until August 15, 2010, were classified as CBT injuries. The second time period that was analyzed was the academic year from August 16, 2010, until May 24, 2011, which corresponded to the duration of the first academic year after CBT for the cadets.
Injury Surveillance
All cadets receive health care through the closed military health care system at the USMA. All injuries to cadets are evaluated through the USMA sports medicine, physical therapy, and orthopedic clinics as described previously.22 The ATs in this study were not involved in diagnosing, treating, or documenting any cadet injuries. The PTs in this study did work in a sick-call clinic where they performed evaluations for cadets with musculoskeletal injuries. The PTs did not ask cadets which group they were assigned to during their evaluations and were blinded to group assignment. The orthopedic surgeons and primary care physicians who evaluated the cadets were also blinded to group assignment.
Injury tracking was performed using the Cadet Illness and Injury Tracking System (CIITS), an injury-surveillance database used at the USMA. Every cadet who is injured to an extent that causes him or her to seek medical care, miss training, or participate in training with imposed limitations due to injury is entered into the CIITS database. Additionally, injury tracking was performed using the Armed Forces Healthcare Longitudinal Technology Application (AHLTA). The AHLTA serves as the Military Health System's electronic medical record. All medical encounters for cadets are recorded in AHLTA with diagnosis information. These databases have been used in previous studies23,24 examining injury incidence in this population. Because all of the participants in this study were new to the military, information about previous injuries was not available in either database. However, all participants were medically screened and deemed healthy according to the medical fitness standards for military service before enrollment in the study. Consequently, all injuries were treated as new injuries for this study.
Data Analysis
Initially, the epidemiologic incidence proportion, along with the 95% confidence interval (CI), was calculated for each intervention group (AWU versus DIME) during each follow-up period of interest (CBT, academic year, CBT and academic year combined). The incidence proportion is a direct measure of the average risk of injury during a specified period of time and represents the cumulative incidence during the follow-up period of interest.21 We calculated the incidence proportion based on the description provided by Knowles et al.21 The first set of analyses examined the association between the intervention group (AWU versus DIME) and the cumulative incidence for the 3 injury outcomes of interest (lower extremity injury, acute traumatic knee-joint injury, and ACL injury). The population at risk for the CBT and the combined CBT and academic year analyses included the entire population at risk at the beginning of the study period; the data for these periods were analyzed in an intention-to-treat fashion. Data for the academic year analysis included only those participants who completed the entire intervention program (AWU and DIME) during CBT in the population at risk; cadets who sustained an injury that prevented them from fully participating in the intervention were excluded. To compare the average risk of injury between groups (eg, AWU versus DIME), we calculated relative risk (RR) ratios and 95% CIs. The association between intervention group and cumulative incidence of injury during the follow-up period was assessed by constructing 2×2 (group-by-injury status) contingency tables and conducting the χ2 or Fisher exact test as appropriate. A second set of analyses assessed whether level of supervision was associated with the cumulative incidence of injury by dividing the DIME group by level of supervision (DCS or DES) and comparing them to each other, as well as to the AWU group. These secondary analyses used techniques similar to those described earlier. The AWU group served as the reference group for all between-groups comparisons, except when the DES group was compared with the DCS group, in which case the DCS group served as the referent category. Statistical analyses were completed using STATA/SE software (version 10.1; StataCorp, College Station, TX).
RESULTS
Lower Extremity Injuries
Of the 1313 participants during CBT, 659 were assigned to the AWU group and 654 were assigned to the DIME group (DCS = 329 and DES = 325; Figure). Of these participants, 196 were injured during CBT. The most common CBT injury was overuse syndrome of the knee (49/196 injuries; 25%). Overall lower extremity injury data for CBT are summarized by type of injury and body part in Table 1. The cumulative incidence of lower extremity injuries during CBT by intervention group is summarized in Table 2. The cumulative incidences of lower extremity injury during CBT between the AWU and both DIME groups combined did not differ (RR = 1.03; 95% CI = 0.79, 1.33; P = .832). Similar results were observed when the cumulative incidence of lower extremity injury during CBT for the AWU group was compared with the DCS (RR = 1.03; 95% CI = 0.75, 1.41; P = .842) and the DES (RR = 1.02; 95% CI = 0.75, 1.41; P = .882) groups separately.
Figure.
CONSORT diagram. Abbreviations: AWU, active warm-up; CBT, cadet basic training; DCS, cadet supervision; DES, combined cadet and health professional supervision; DIME, Dynamic Integrated Movement Enhancement.
Table 1.
Summary of Types of Injuries, No.
| Time Period |
Ankle Sprain |
Knee Sprain |
Foot Overuse |
Ankle Overuse |
Lower Leg Overuse |
Knee Overuse |
Hip Overuse |
Other |
| Cadet Basic Training | 48 | 12 | 15 | 17 | 37 | 49 | 7 | 11 |
| Academic year | 52 | 17 | 7 | 8 | 11 | 18 | 6 | 27 |
| Total | 100 | 29 | 22 | 25 | 48 | 67 | 13 | 38 |
Table 2.
Incident Injuries by Injury Outcome and Group During the Follow-Up Period
| Injury Outcome |
Control Group |
Intervention Group |
||||||||||||||
| Active Warm-Up |
DIME, Cadet Supervised |
DIME, Expert Supervised |
Total DIMEa |
|||||||||||||
| Injured, | At Risk, | IP, | 95% CI | Injured, | At Risk, | IP, | 95% CI | Injured, | At Risk, | IP, | 95% CI | Injured, | At Risk, | IP, | 95% CI | |
| No. |
No. |
% |
No. |
No. |
% |
No. |
No. |
% |
No. |
No. |
% |
|||||
| Lower extremity injury | ||||||||||||||||
| Cadet Basic Training | 97 | 659 | 14.7 | 12.1, 18.1 | 50 | 329 | 15.2 | 11.5, 19.5 | 49 | 325 | 15.1 | 11.4, 19.4 | 99 | 654 | 15.1 | 12.5, 18.1 |
| Academic year | 73 | 562 | 13.0 | 10.3, 16.1 | 46 | 279 | 16.5 | 12.3, 21.4 | 27 | 276 | 9.8 | 6.5, 13.9 | 73 | 555 | 13.2 | 10.5, 16.3 |
| Cadet Basic Training and academic year | 170 | 659 | 25.8 | 22.5, 29.3 | 96 | 329 | 29.2 | 24.3, 34.4 | 76 | 325 | 23.4 | 18.9, 28.4 | 172 | 654 | 26.3 | 23.0, 29.9 |
| Acute knee injuryb | ||||||||||||||||
| Cadet Basic Training | 5 | 659 | 0.8 | 0.2, 1.8 | 6 | 329 | 1.8 | 0.7, 3.9 | 1 | 325 | 0.3 | 0.0, 1.7 | 7 | 654 | 1.1 | 0.4, 2.2 |
| Academic year | 9 | 562 | 1.6 | 0.7, 3.0 | 6 | 279 | 2.2 | 0.8, 4.6 | 2 | 276 | 0.7 | 0.0, 2.6 | 8 | 555 | 1.4 | 0.6, 2.8 |
| Cadet Basic Training and academic year | 14 | 659 | 2.1 | 1.2, 3.5 | 12 | 329 | 3.6 | 1.9, 6.2 | 3 | 325 | 0.9 | 0.2, 2.7 | 15 | 654 | 2.3 | 1.3, 3.8 |
| Anterior cruciate ligament injuryb | ||||||||||||||||
| Cadet Basic Training | 1 | 659 | 0.2 | 0.0, 0.8 | 0 | 329 | 0.0 | NA | 0 | 325 | 0.0 | NA | 0 | 654 | 0.0 | NA |
| Academic year | 4 | 562 | 0.7 | 0.2, 1.8 | 2 | 279 | 0.7 | 0.0, 2.6 | 0 | 276 | 0.0 | NA | 2 | 555 | 0.4 | 0.0, 1.3 |
| Cadet Basic Training and academic year | 5 | 659 | 0.8 | 0.2, 1.8 | 2 | 329 | 0.6 | 0.1, 2.2 | 0 | 325 | 0.0 | NA | 2 | 654 | 0.3 | 0.0, 1.1 |
Abbreviations: CI, confidence interval; DIME, Dynamic Integrated Movement Enhancement; IP, incidence proportion; NA, not applicable.
Combines the cadet-supervised and expert-supervised DIME groups.
Lower bounds of 95% CIs for 0.0% are <0.1%.
Excluding the 196 individuals who were injured during CBT, which prevented them from fully participating in the 3 warm-up programs, left 1117 participants available for analysis during the academic year period. A total of 562 cadets were in the AWU group, 279 were in the DCS group, and 276 were in the DES group. During the academic year, 146 participants experienced a lower extremity injury. The most common academic year injury was an ankle sprain, representing 52 of 146 reported injuries (36%). The cumulative incidence of lower extremity injury by group during the academic year is summarized in Table 2. Similar to the period during CBT, there was no difference in the cumulative incidences of lower extremity injury between the AWU group and both DIME groups combined during the academic year (RR = 1.01; 95% CI = 0.75, 1.37; P = .935). However, the cumulative incidence of lower extremity injury within the DIME group varied significantly by level of supervision. We noted a 41% risk reduction in the DES group compared with the DCS group (RR = 0.59; 95% CI = 0.38, 0.93; P = .02). Although not statistically significant, there was also a 25% risk reduction in the DES group compared with the AWU group (RR = 0.75; 95% CI = 0.49, 1.14; P = .18). Finally, we observed a nonsignificant 27% increase in the risk of injury in the DCS group compared with the AWU group (RR = 1.27; 95% CI = 0.90, 1.78; P = .171).
When we examined the incident injuries from both CBT and the academic year combined, the patterns of incidence estimates by group were similar to those observed during the academic year but to a lesser degree (Table 2). The cumulative incidences between the AWU group and the DIME groups combined did not differ (RR = 1.02; 95% CI = 0.85, 1.22; P = .836). The cumulative incidence in the DES group was 9% lower than the AWU group (RR = 0.91; 95% CI = 0.72, 1.15; P = .411) and 20% lower than the DCS group (RR = 0.80; 95% CI = 0.62, 1.03; P = .092), but these differences were not statistically significant. Finally, the cumulative incidence in the DCS was 13% higher than the AWU group (RR = 1.13; 95% CI = 0.91, 1.40; P = .259), but again the difference was not statistically significant.
Acute Traumatic Knee-Joint Injuries
The pattern for knee injuries by group was similar to that observed for all lower extremity injuries during CBT, the academic year, and both periods combined. A total of 29 acute traumatic knee-joint injuries (7 ACL injuries) were reported during the follow-up period including CBT and the academic year. The incidence proportion of acute traumatic knee-joint injuries by group during the follow-up period is presented in Table 2. Overall, we noted no differences in the cumulative incidence of acute knee-joint injuries when the AWU group was compared with both DIME groups during the entire follow-up period (RR = 1.08; 95% CI = 0.52, 2.22; P = .838). Similar results were observed when the AWU group and DIME groups were compared during CBT and the academic year separately; however, as observed for lower extremity injuries in general, the cumulative incidence of acute knee-joint injury varied by level of supervision within the DIME group. During CBT and the academic year, there was a 75% risk reduction for acute traumatic knee injuries in the DES group compared with the DCS group (RR = 0.24; 95% CI = 0.07, 0.89; P = .020). A nonsignificant 57% risk reduction was evident when we compared the DES group with the AWU group during this same time period (RR = 0.43; 95% CI = 0.13, 1.50; P = .173). Finally, the risk of acute knee-joint injury increased by a nonsignificant 72% in the DCS group compared with the AWU group during CBT and the academic year (RR = 1.72; 95% CI = 0.27, 1.24; P = .159).
The cumulative incidence of ACL injuries by intervention group during the study period is presented in Table 2. No ACL injuries were seen in the DES group during the entire follow-up period. The DCS group experienced 2 ACL injuries during the follow-up period; both occurred during the academic year. The AWU group experienced 5 ACL injuries during the follow-up period; 1 occurred during CBT and the other 4 during the academic year. The risk of ACL injury in the combined DIME group (DCS and DES) was 60% lower compared with the AWU group during the entire follow-up period (RR = 0.40; 95% CI = 0.07, 2.07; P = .260); however, this finding was not statistically significant.
DISCUSSION
We observed no statistically significant differences in injury risk when comparing the combined DIME group (DES and DCS) with the AWU group during any of the follow-up periods (CBT, academic year, or CBT and academic year combined). In further subgroup analyses to examine the association between the cumulative incidence of lower extremity injury and level of supervision in the DIME group, we did note a lower incidence of injury for all injury outcomes in the DES group compared with the other 2 groups; however, only the 41% reduction in the cumulative incidence of lower extremity injury in the DES group compared with the DCS group was statistically significant during the academic year (RR = 0.59; 95% CI = 0.38, 0.93; P = .02). The observed 25% reduction in the cumulative incidence of lower extremity injury in the DES group compared with the AWU group was not statistically significant (RR = 0.75; 95% CI = 0.49, 1.14; P = .18). Furthermore, the width of the CI around the point estimate and the fact that it includes 1 suggest a degree of uncertainty associated with this estimate, which fails to exclude the possibility of increased risk in the DES group. However, the magnitude and direction of the observed point estimate and associated CI in this study favors risk reduction in the DES group and was comparable with the findings of previous authors in similar military populations. In a recent systematic review, Bullock et al4 reported a 20% to 30% injury reduction in military populations using similar programs. Although this result was not statistically significant, if confirmed, it could have clinical importance. Our secondary hypothesis was supported, as the cumulative incidences of lower extremity injury and acute traumatic knee-joint injury during the academic year were lower in participants who performed the DIME program under the supervision of an AT or PT compared with cadets who performed the DIME without professional supervision.
The cumulative incidence of lower extremity injury was nearly identical across all 3 groups during CBT. This may indicate that any movement-pattern correction training likely has a negligible effect on lower extremity injury reduction during the early weeks of implementation. Our finding of no differences among groups during CBT may indicate that an exercise program for reducing injury risk has no immediate effects. This result is consistent with previous research, which suggests that the effects of injury-prevention programs are not observed until later in an athletic season.9,25,26 Therefore, it may be appropriate to begin a program such as the DIME several weeks before a sport season or military basic training. It also seems likely that injuries sustained during CBT are more closely related to a rapid increase in training volume rather than to biomechanical risk factors. If so, this would limit the potential effects of a program such as the DIME over this time period.
We demonstrated no statistically significant difference in injury risk between the DCS group and the AWU group (RR = 1.27; 95% CI = 0.90, 1.78; P = .171), and the width of the CI suggests great uncertainty in this comparison. Although the difference was not significant, the direction and magnitude of the point estimate and CI suggest the possibility of increased risk. Several factors could have contributed to this possible increased risk in the current study. First, although the research staff observed the cadet instructors in the DCS group (just as they did in the DES group) for compliance, they did not provide any further instruction or feedback on program implementation. As a result, participants may have had difficulty learning the DIME exercises and performing them correctly during the 6-week intervention. This may have had a more significant effect when the difficulty of the DIME program was increased at the midpoint of basic training. Progressing this group to more challenging exercises without expert supervision and appropriate feedback might have reinforced faulty movement patterns, which in turn may have contributed to an increased risk of injury. As a result, a combination of lack of professional supervision and increase in injury-prevention–program difficulty in this initial study may have resulted in deleterious effects for those in the DCS group. Furthermore, even though cadet instructors in all 3 programs received similar training (eg, time and number of sessions), many of the instructors in the AWU group had performed these standard military warm-up exercises previously. Thus, they were probably more familiar with the proper execution of these exercises. These factors may explain in part why the observed cumulative injury incidence in the AWU group was lower than that observed in the DCS group.
The importance of professional supervision as it relates to the success of such programs as the DIME is not clearly understood. However, our hypothesis that professional supervision is important to the outcomes of injury-prevention programs was supported, as the DES group had a statistically significant reduction in the risk of lower extremity injury and acute knee-joint injury compared with the DCS group. Although we are the first to directly analyze the different methods of exercise instruction, our findings are consistent with the body of previous research involving injury-prevention programs. The injury-prevention programs that have successfully reduced ACL injury risk have typically been implemented under the supervision of an AT or PT.6,8,9 With the exception of Mandelbaum et al,13 who reported a reduction in ACL injury risk using an exercise program led by coaches, programs led by coaches or other nonmedical personnel have not resulted in an injury reduction.15,16 It is possible that ATs and PTs, being trained to recognize lower extremity impairments and faulty movement patterns, may be better equipped to assess movement patterns and provide the precise corrective feedback required to implement these programs effectively. Although exercises led by medically trained personnel may currently be the most effective, programs led by coaches and other nonmedical personnel will ultimately be required to maximize the effect of injury-prevention exercises on public health. Future studies that prospectively and directly analyze the effect of different models of exercise instruction and supervision are urgently needed.
The mechanism that caused higher levels of supervision to translate into decreased injury risk in this study is not fully understood. Analyzing human movement typically occurs in a one-on-one setting in a clinic or a laboratory, potentially with instrumentation. In this study, only 1 AT or PT was assigned to a group of 35 to 40 cadets. An additional 5 or 6 upper-class cadet instructors were assigned to each platoon of cadets, but this ratio is still insufficient to truly analyze human movement, especially in such a time-constrained environment. We believe the real benefit of professional supervision may have been that the cadre and the participants were aware that they were being scrutinized and attempted to perform the exercises correctly, whereas the DCS group may have just gone through the motions with little concern for proper technique. Furthermore, the ATs and PTs called out oral cues that were clearly audible to the entire group throughout each exercise session. These cues included “knees over toes,” “toes straight forward,” “land softly by bending the ankles, knees, and hips,” and other cues that were used to remind participants to concentrate on good form. In the absence of this oral reinforcement, the participants in the DCS group might have allowed their exercise technique to deteriorate. This possibility underscores the need to train potential leaders of injury-prevention programs in the importance of proper error detection and feedback delivery. A priority for future researchers should be determining the factors that are critical in training coaches and other exercise leaders to effectively implement lower extremity injury-prevention programs.
The magnitude of the differences we observed in injury risk between groups might have been greater if the intervention program had specifically targeted those persons with high-risk biomechanical movement patterns at baseline. All participants randomized to the DIME groups performed the DIME, whether they had faulty movement patterns or not. Because the DIME is a program designed to improve movement, we would anticipate very little effect on the overall injury risk of persons who did not have faulty movement patterns before the intervention. The theory of rapidly screening to identify those with high-risk movement patterns and then focusing appropriate movement retraining exercises on this subpopulation is compelling.27,28 Future investigators should focus on developing more sensitive screening techniques and targeting athletes with faulty movement patterns for intervention.29
The DIME program was initially designed to identify and improve the high-risk biomechanical movement patterns associated with ACL injury. Notable in our study was the reduction in the cumulative incidence of acute traumatic knee-joint injuries in the DES group when injuries from the entire follow-up period (CBT and the academic year combined) were examined. We observed a 75% reduction in risk of acute traumatic knee-joint injury when comparing the DES group with the DCS group (RR = 0.24; 95% CI = 0.07, 0.89; P = .020). When examining the point estimate, we also observed a 57% reduction in the risk of acute traumatic knee-joint injuries comparing the DES group to the AWU group (RR = 0.43; 95% CI = 0.13, 1.50; P = .173); however, this difference was not statistically significant. The CI of this comparison included 1, which leaves the statistical possibility that there was actually an increase in risk in the DES group; however, the width of the CI is due in part to the relatively small number of acute traumatic knee-joint injuries observed across all groups (AWU = 14, DCS = 12, DES = 3) during the follow-up period. The small number of injuries limits our ability to draw statistically meaningful conclusions. When we examined injury data for CBT and the academic year independently, we found similar nonsignificant reductions in acute traumatic knee-joint injuries between the DES group and the AWU group (Table 2). Although the reduction of risk within the DES group compared with the AWU group was not statistically significant and considerable uncertainty remains, the magnitude and direction of the observed difference appear to be clinically important.29 These results should be considered preliminary and interpreted with caution; however, they may be clinically important given the small number of observed knee-joint injuries during the follow-up period and the associated lack of adequate statistical power. Further definitive study is needed to confirm these findings. Because of the severity and potential long-term complications of acute traumatic knee-joint injury, it is important to further investigate this reduction in risk in future studies that are adequately powered for ACL or acute traumatic knee-joint injury as an injury outcome.
As with any study, our study had potential limitations that should be considered. Foremost, the results presented here are from a yearlong investigation to determine if the DIME program could be implemented during military basic training and whether there was any evidence of reduced injury risk in this sample. We enrolled nearly an entire freshman class entering the USMA to participate in this study (1313/1374 = 95.5%), implemented a 6-week intervention, and followed all participants for injury during their first year at the academy. Despite this considerable effort, the study was underpowered for the lower extremity and knee injury outcomes of interest (Table 3). Because we planned to enroll nearly all eligible participants from the entire class, we did not perform an a priori sample-size estimate. Further study comparing the AWU and DES groups with adequate power for these injury outcomes appears to be warranted based on these initial findings. To address this will likely require a longitudinal cohort study over multiple years at a single institution or large multicenter studies. Another potential limitation is that the lower extremity injury outcomes in the current study represent a mix of traumatic and overuse injuries, which occurred in a variety of activities. The broad spectrum of injuries and mechanisms might have diminished our ability to find meaningful results. Another limitation is that we relied on active surveillance information from CIITS and AHLTA to identify incident injuries during the current study. The quality of the administrative data contained in these systems depends on the completeness, validity, consistency, timeliness, and accuracy of the data maintained in these databases. As a result, coding errors associated with incident case diagnoses cannot be ruled out when using large-scale administrative databases for epidemiologic studies. Although we attempted to cross-reference injury data in CIITS and AHLTA to ensure complete injury-data capture during the follow-up period, it is possible that some injuries were missed. In calculating the epidemiologic incidence proportion, we included only the first injury sustained by each person at risk during the follow-up period; as a result, multiple injuries to the same person may have been missed. Because there were no differences in the cumulative incidence of injury between the intervention groups during CBT, we elected to limit our analysis during the academic year to only those who completed the intervention without injury. Although this decision allows us to compare outcomes between those who completed the AWU and DIME programs in each group during the academic year, it might have introduced some bias into this portion of the analysis.
Table 3.
Observed Power and Sample Size Estimates for Comparisons Between the Active Warm-up Group and the Expert-Supervised Dynamic Integrated Movement Enhancement Group During the Academic Year
| Injury Outcome |
Observed Powera |
Sample Size Estimateb |
| Lower extremity injury | 0.223 | 1610 |
| Acute traumatic knee injury | 0.084 | 2420 |
| Anterior cruciate ligament injury | 0.057 | 1388 |
Observed power for the current study.
Sample size estimate per group, based on the incidence proportion data presented in Table 1; assumes a 2-tailed alpha level of .05 and power of .80.
Another potential limitation is that our analysis did not account for the potential correlation that can result from participants being cluster randomized or nested within companies. It is unlikely that this correlation had any notable effect but the small number of clusters or companies studied might have increased the standard errors and widened the CIs around our point estimates. Furthermore, we performed univariate analyses with the incidence proportion as our primary outcome of interest, which did not account for person-time at risk to injury (exposure). We elected not to use incidence rates as our outcome of interest because it was not administratively feasible to document individual person-time at risk in each of the various training events and physical activities that participants were required to complete during the follow-up period. Furthermore, because all participants were cadets at a military academy, nearly all had the same cumulative exposure to training events during the course of CBT and the academic year; however, these exposures occurred at different times throughout the year because of scheduling. As a result, we believe the incidence proportion, which is a recognized measure of disease occurrence in the epidemiologic literature, was the most appropriate outcome for this study. It is possible that other injury outcomes and analytical techniques (eg, Poisson, negative binomial, and Cox proportional hazards regression) could have been used and yielded different results.
CONCLUSIONS
We observed no differences in lower extremity injury risk between the AWU group and the combined DIME (DES and DCS) group. The CIs for all comparisons were fairly wide and many included 1, indicating potential uncertainty in the observed results. This uncertainty underscores the importance of interpreting these results with caution. Although this study was underpowered for the injury outcomes of interest, the magnitude and direction of the risk ratios in the DES group compared with the AWU group appear to be clinically important and indicate that the injury-prevention program, under expert supervision, may be able to reduce injury risk. This is particularly important within the military population, in whom lower extremity musculoskeletal injuries are endemic and costly. Despite the apparent benefit to performing the DIME with expert supervision, our results indicate that the DIME could contribute to increased injury risk if not properly executed. Definitive, adequately powered studies are needed to confirm these initial findings. The significant systematic differences in the incidence of injury between the DES group and the DCS group suggest that level of supervision is an important factor in the successful implementation of lower extremity injury-prevention programs and that inadequate training or supervision may have deleterious effects. A priority for future researchers should be determining the factors that are critical in training coaches and other exercise leaders to effectively implement lower extremity injury-prevention programs.
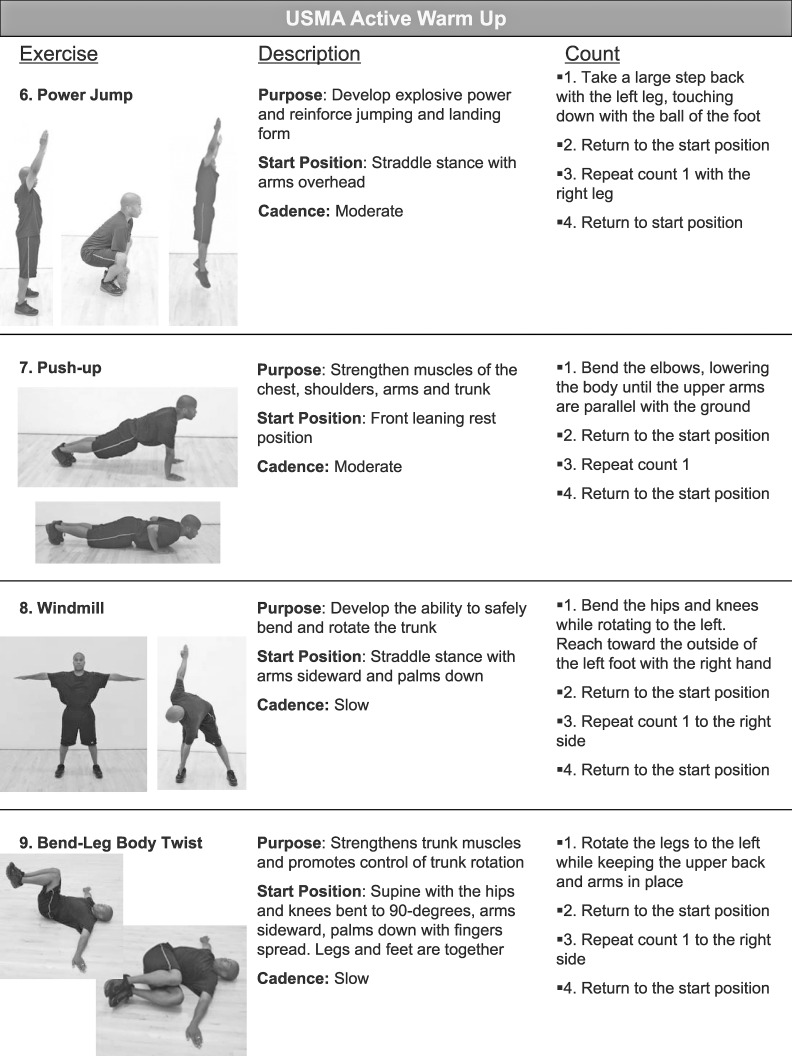
Appendix 1. The Active Warm-Up Program; the 10th Exercise was Jogging in Place, Which was Performed Between Other Exercises Continued on Next Page Appendix 1. Continued From Previous Page
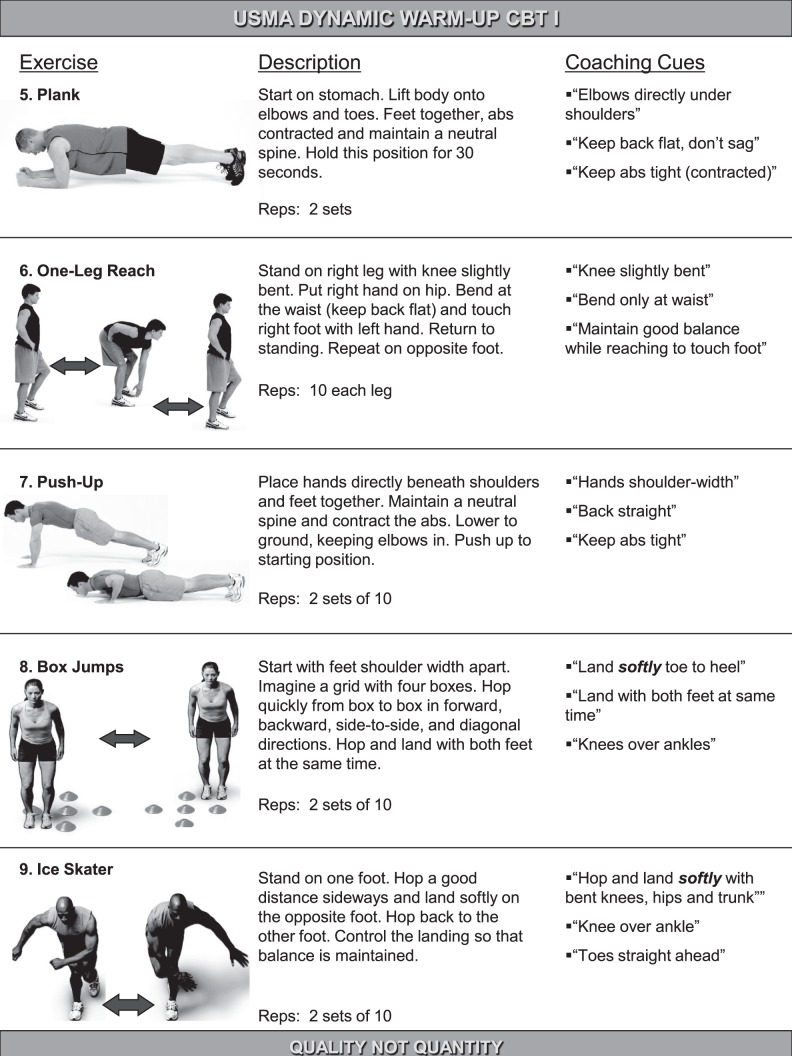
Appendix 2. The Dynamic Integrated Movement Enhancement Warm-Up Program; the 10th Exercise was Jogging in Place, Which was Performed Between Other Exercises Continued on Next Page Appendix 2. Continued From Previous Page
REFERENCES
- 1. Jones BH, Canham-Chervak M, Sleet DA. . An evidence-based public health approach to injury priorities and prevention. Am J Prev Med. 2010; 38 1 suppl: S1– S10. [DOI] [PubMed] [Google Scholar]
- 2. Veigel JD, Pleacher MD. . Injury prevention in youth sports. Curr Sports Med Rep. 2008; 7 6: 348– 352. [DOI] [PubMed] [Google Scholar]
- 3. Finch CF, Ullah S, McIntosh AS. . Combining epidemiology and biomechanics in sports injury prevention research: a new approach for selecting suitable controls. Sports Med. 2011; 41 1: 59– 72. [DOI] [PubMed] [Google Scholar]
- 4. Bullock SH, Jones BH, Gilchrist J, Marshall SW. . Prevention of physical training-related injuries: recommendations for the military and other active populations based on expedited systematic reviews. Am J Prev Med. 2010; 38 suppl 1: S156– S181. [DOI] [PubMed] [Google Scholar]
- 5. Hewett TE, Johnson DL. . ACL prevention programs: fact or fiction? Orthopedics. 2010; 33 1: 36– 39. [DOI] [PubMed] [Google Scholar]
- 6. Myklebust G, Engebretsen L, Braekken IH, Skjolberg A, Olsen OE, Bahr R. . Prevention of anterior cruciate ligament injuries in female team handball players: a prospective intervention study over three seasons. Clin J Sport Med. 2003; 13 2: 71– 78. [DOI] [PubMed] [Google Scholar]
- 7. Kiani A, Hellquist E, Ahlqvist K, Gedeborg R, Michaelsson K, Byberg L. . Prevention of soccer-related knee injuries in teenaged girls. Arch Intern Med. 2009; 170 1: 43– 49. [DOI] [PubMed] [Google Scholar]
- 8. Hewett TE, Lindenfeld TN, Riccobene JV, Noyes FR. . The effect of neuromuscular training on the incidence of knee injury in female athletes; a prospective study. Am J Sports Med. 1999; 27 6: 699– 706. [DOI] [PubMed] [Google Scholar]
- 9. Gilchrist J, Mandelbaum BR, Melancon H, Ryan GW, Silvers HJ, Griffin LY. . A randomized controlled trial to prevent noncontact anterior cruciate ligament injury in female collegiate soccer players. Am J Sports Med. 2008; 36 8: 1476– 1483. [DOI] [PubMed] [Google Scholar]
- 10. Hewett TE, Ford KR, Hoogenboom BJ, Myer GD. . Understanding and preventing ACL injuries: current biomechanical and epidemiologic considerations—update 2010. N Am J Sports Phys Ther. 2010; 5 4: 234– 251. [PMC free article] [PubMed] [Google Scholar]
- 11. Soderman K, Alfredson H, Pietila T, Werner S. . Risk factors for leg injuries in female soccer players: a prospective investigation during one out-door season. Knee Surg Sports Traumatol Arthrosc. 2001; 9 5: 313– 321. [DOI] [PubMed] [Google Scholar]
- 12. Kiani A, Hellquist E, Ahlqvist K, Gedeborg R, Michaelsson K, Byberg L. . Prevention of soccer-related knee injuries in teenaged girls. Arch Intern Med. 2010; 170 1: 43– 49. [DOI] [PubMed] [Google Scholar]
- 13. Mandelbaum BR, Silvers HJ, Watanabe DS, Knarr JF, Thomas SD, Griffin LY. . Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med. 2005; 33 7: 1003– 1010. [DOI] [PubMed] [Google Scholar]
- 14. Heidt RS Jr, Sweeterman LM, Carlonas RL, Traub JA, Tekulve FX. . Avoidance of soccer injuries with preseason conditioning. Am J Sports Med. 2000; 28 5: 659– 662. [DOI] [PubMed] [Google Scholar]
- 15. Pfeiffer RP, Shea KG, Roberts D, Grandstrand S, Bond L. . Lack of effect of a knee ligament injury prevention program on the incidence of non-contact anterior cruciate ligament injury. J Bone Joint Surg Am. 2006; 88 8: 1769– 1774. [DOI] [PubMed] [Google Scholar]
- 16. Steffen K, Myklebust G, Olsen OE, Holme I, Bahr R. . Preventing injuries in female youth football—a cluster-randomized controlled trial. Scand J Med Sci Sports. 2008; 18 5: 605– 614. [DOI] [PubMed] [Google Scholar]
- 17. Engebretsen AH, Myklebust G, Holme I, Engebretsen L, Bahr R. . Prevention of injuries among male soccer players: a prospective, randomized intervention study targeting players with previous injuries or reduced function. Am J Sports Med. 2008; 36 6: 1052– 1060. [DOI] [PubMed] [Google Scholar]
- 18. Boling MC, Padua DA, Marshall SW, Guskiewicz K, Pyne S, Beutler A. . A prospective investigation of biomechanical risk factors for patellofemoral pain syndrome: the Joint Undertaking to Monitor and Prevent ACL Injury (JUMP-ACL) cohort. Am J Sports Med. 2009; 37 11: 2108– 2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Brushoj C, Larsen K, Albrecht-Beste E, Nielsen MB, Loye F, Holmich P. . Prevention of overuse injuries by a concurrent exercise program in subjects exposed to an increase in training load: a randomized controlled trial of 1020 Army recruits. Am J Sports Med. 2008; 36 4: 663– 670. [DOI] [PubMed] [Google Scholar]
- 20. TC 3–22.20: Army Physical Readiness Training. Fort Jackson, SC: Headquarters, Department of the Army; 2010: 432. [Google Scholar]
- 21. Knowles SB, Marshall SW, Guskiewicz KM. . Issues in estimating risks and rates in sports injury research. J Athl Train. 2006; 41 2: 207– 215. [PMC free article] [PubMed] [Google Scholar]
- 22. Mountcastle SB, Posner M, Kragh JF Jr, Taylor DC. . Gender differences in anterior cruciate ligament injury vary with activity: epidemiology of anterior cruciate ligament injuries in a young, athletic population. Am J Sports Med. 2007; 35 10: 1635– 1642. [DOI] [PubMed] [Google Scholar]
- 23. Waterman BR, Belmont PJ Jr, Cameron KL, Deberardino TM, Owens BD. . Epidemiology of ankle sprain at the United States Military Academy. Am J Sports Med. 2010; 38 4: 797– 803. [DOI] [PubMed] [Google Scholar]
- 24. Waterman BR, Belmont PJ Jr, Cameron KL, Svoboda SJ, Alitz CJ, Owens BD. . Risk factors for syndesmotic and medial ankle sprain: role of sex, sport, and level of competition. Am J Sports Med. 2011; 39 5: 992– 998. [DOI] [PubMed] [Google Scholar]
- 25. Hewett TE, Ford KR, Myer GD. . Anterior cruciate ligament injuries in female athletes: part 2, a meta-analysis of neuromuscular interventions aimed at injury prevention. Am J Sports Med. 2006; 34 3: 490– 498. [DOI] [PubMed] [Google Scholar]
- 26. Powers C, Sigward SM, Ota S, Pelley K. . The influence of an ACL injury training program on knee mechanics during a side-step cutting maneuver. J Athl Train. 2004; 39 suppl 2: S27. [Google Scholar]
- 27. Padua DA, Marshall SW, Boling MC, Thigpen CA, Garrett WE Jr, Beutler AI. . The Landing Error Scoring System (LESS) is a valid and reliable clinical assessment tool of jump-landing biomechanics: the JUMP-ACL study. Am J Sports Med. 2009; 37 10: 1996– 2002. [DOI] [PubMed] [Google Scholar]
- 28. Beutler A, de la Motte S, Marshall S, Padua D, Boden B. . Muscle strength and qualitative jump-landing differences in male and female military cadets: the JUMP-ACL Study. J Sports Sci Med. 2009; 8 4: 663– 671. [PMC free article] [PubMed] [Google Scholar]
- 29. Sugimoto D, Myer GD, McKeon JM, Hewett TE. . Evaluation of the effectiveness of neuromuscular training to reduce anterior cruciate ligament injury in female athletes: a critical review of relative risk reduction and numbers-needed-to-treat analyses. Br J Sports Med. 2012; 46 14: 979– 988. [DOI] [PMC free article] [PubMed] [Google Scholar]