Abstract
Gastrointestinal disease is a prevalent cause of morbidity and mortality and the use of animal models have been instrumental in studying mechanisms of digestive pathophysiology. As investigators attempt to translate the wealth of basic science information developed from rodent models, large animal models provide a number of translational advantages. The pig, in particular, is arguably one of the most powerful models of human organ systems, including the gastrointestinal tract. The pig has provided important tools and insight into intestinal ischemia/reperfusion injury, intestinal mucosal repair, as well as new insights into esophageal injury and repair. Porcine model development has taken advantage of the size of the animal, allowing increased surgical and endoscopic access. In addition, cellular tools such as the intestinal porcine epithelial cell (IPEC-J2) line and porcine enteroids are providing the methodology to translate basic science findings using in-depth mechanistic analyses. Further opportunities in porcine digestive disease modeling include developing additional transgenic pig strains. Collectively, porcine models hold great promise for the future of clinically relevant digestive disease research.
Keywords: Pig, Ischemia/Reperfusion Injury, Mucosal Repair, Tight Junction
Abbreviations used in this paper: CFTR, cystic fibrosis transmembrane conductance regulator; IPEC-J2, intestinal porcine epithelial cells; NEC, necrotizing enterocolitis
Summary.
Rodent models have been instrumental in furthering our understanding of gastrointestinal pathophysiology. However, there are important limitations to translating findings from rodent models to human digestive disease, and some of these can be overcome by large animal models.
Gastrointestinal diseases account for 10% of annual mortalities in the United States, and approximately 70 million Americans experience gastrointestinal illness each year.1 Because of the limitations of studying human gastrointestinal disease in a clinical environment, the use of animal models to examine the mechanisms of gastrointestinal disease has been of great importance. Rodent models remain the most commonly used animal model for the study of human disease because of their relatively low cost and maintenance requirements, rapid reproduction rates, and availability of research tools such as murine antibodies.2, 3 Transgenic and knockout mice, as well as chemically induced neoplastic and inflammatory disease models in mice, have provided a tremendous amount of information on the underlying mechanisms of clinical diseases.4, 5 However, rodent models frequently fail to fully mimic clinical signs and significant pathologic hallmarks of human diseases.6, 7 Because of this, there has been recent increased interest within the scientific community in developing large animal models that more closely approximate the clinical and pathologic features of human disease.8, 9 Of the large animal species used for translational research, the pig offers a marked advantage because this species has important anatomic and physiological similarities with human beings, particularly in regard to the gastrointestinal tract.10, 11 This review summarizes and evaluates the current uses of large animal models in gastrointestinal research with a particular emphasis on porcine models.
What Is a Large Animal Model and What Are the Advantages?
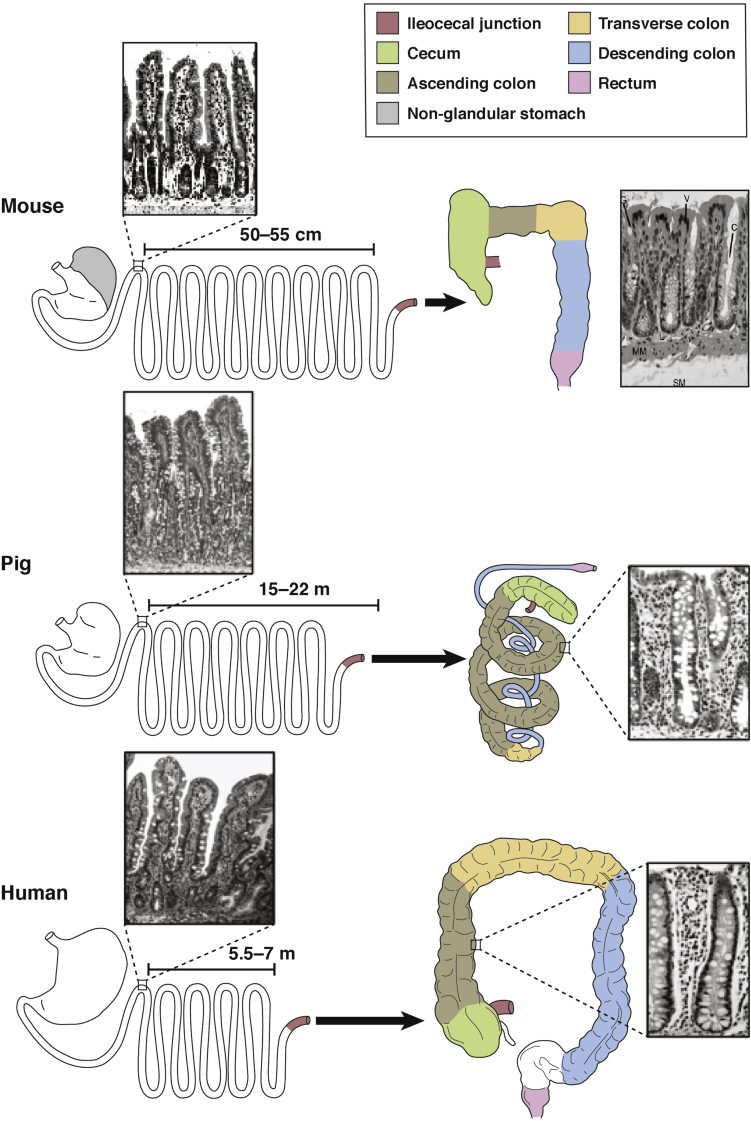
In general, any nonrodent mammalian animal species used for translational research is considered a large animal model. Although rodent models have been invaluable in furthering the mechanistic understanding of human disease, there are circumstances in which choosing a large animal species in place of a rodent model for gastrointestinal work is scientifically justifiable. For instance, when investigating gastric disease, the dog, pig, and monkey all have a glandular-type stomach similar to that of human beings, whereas the murine stomach has both glandular and nonglandular regions and therefore may have differences in gastric pathophysiology (Figure 1).11 Of the large animal species used in translational gastrointestinal research, the dog has been used most extensively because canine gastrointestinal anatomy and physiology are considered to be highly similar to that of human beings, and dogs show spontaneous naturally occurring diseases in common with human beings, particularly neoplasia.12 However, dogs are highly sensitive to some disease models, particularly intestinal ischemia, and experience high rates of mortality.13 In addition, there is growing social aversion to the use of the dog as a laboratory animal.14 Calves have been established as a model for human enteric infectious disease, particularly Salmonellosis. Cattle may become naturally infected with Salmonella enterica serotype typhimurium and they show a disease state very analogous to human salmonellosis. Therefore, the calf commonly is used to study Salmonella species infection and the host–pathogen interaction, translating findings to human disease as well as to veterinary medicine and agriculture.15 This recently was called Dual with Dual Benefit in a Program Announcement from the National Institutes of Health (http://grants.nih.gov/grants/guide/pa-files/PAR-16-366.html). However, the application of ruminant models for the study of other human gastrointestinal biology is limited owing to the fundamental difference in digestive anatomy and physiology. Alternatively, the pig is becoming progressively appreciated as a distinctly advantageous model for human beings in numerous fields of science, and an increasing number of textbooks, articles, and proceedings are being published that outline pig models in biomedical research, including digestive disease research (Table 1).16 The pig has many fundamental anatomic, physiological, genomic, proteomic, immunologic, and nutritional similarities to human beings.12, 16, 17, 18, 19, 20, 21, 22 The pig also shows potential for interspecies transplantation work, as well as the ability to fulfill United States Food and Drug Administration requirements for pharmaceutical testing.23 These features of the pig combined with an increasing availability of biological tools and reagents for use to study porcine tissue make the pig arguably the best model available for translational biomedical research.
Figure 1.
Schematic diagram for comparison of murine, porcine, and human gastrointestinal tract anatomy and histology.
Derived from Nguyen TLA, et al. How informative is the mouse for human gut microbiota research? Disease Models and Mechanisms 2015;8:1–16. http://dx.doi.org/10.1242/dmm.017400. Used under Creative Commons (https://creativecommons.org/licenses/by/4.0/). Modified with permission.
Table 1.
Porcine Digestive Disease Models Available
| Disease or syndrome modeled | References |
|---|---|
| Esophageal metaplasia and neoplasia | 24, 38 |
| Stress-induced intestinal dysfunction | 75, 76, 77, 78, 79, 80, 81 |
| Intestinal ischemia/reperfusion injury and repair | 13, 14, 50, 54, 61, 82, 83, 84, 85, 86, 87 |
| Necrotizing enterocolitis | 40, 41, 88, 89, 90, 91 |
| Short-bowel syndrome | 92, 93 |
| Intestinal transplantation | 67 |
| Colorectal cancer | 94 |
| Cystic fibrosis | 73, 74, 95, 96, 97 |
| Diabetes mellitus | 98, 99 |
Despite the numerous advantages of large animal models, several key limitations have impeded their widespread use in biomedical research in favor of rodent models. The most significant limitation to large animal models is the increased cost of animal maintenance and husbandry. Large animal species require larger, more specialized housing and surgical facilities, with higher expenses related to feed, veterinary care, and surgery costs. In addition, their longer reproductive cycles and growth rates make large animal work slower and more expensive. This has hampered the development of transgenic animals.
Characterization of the Porcine Gastrointestinal Tract
There are many notable similarities between the human and porcine gastrointestinal tracts, which make the porcine model a powerful tool for studying gastrointestinal disease. For example, the esophagus is very similar to that of human beings in that both species have esophageal submucosal glands as do human beings, whereas rodents do not.24 The stomach of the pig is entirely glandular, making it physiologically comparable with that of human beings.11 The structure of the small intestine is comparable in human beings and pigs, and the intestinal length (meters) per bodyweight (kilograms) ratio is approximately 0.1 in both species, compared with approximately 0.16 in mice.10, 25, 26 The epithelial cell population (cell lineages, phenotypes, and expression of distinct protein biomarkers) of the porcine small intestine is similar to that of human beings.27 The villus structure is finger-like in pigs, mice, and human beings, whereas rats have a leaf-like villus structure.28 The subcellular structure of porcine enterocytes within the crypt base have been characterized and found to be similar to the description of these cells in human beings.23, 29 The colon of the pig and human beings both possess sacculations and longitudinal muscular bands (tenia) along their length, which results in similar transit times and thus comparable digestive physiology in the intestine, whereas the colon of the mouse and rat are nonsacculated.30, 31 Pigs and human beings are capable of fermenting digesta within the colon, and have been shown to have similar microbial flora within the small intestine and large intestine.32, 33 Conversely, the microbiota of the mouse and human are significantly divergent, with approximately 85% of mouse gut microbiota being absent from human flora.34 Nonetheless, there are important differences in the pig as compared with human beings, including the absence of an appendix, a much larger and more developed cecum, and the spiral arrangement of the colon in the pig (Figure 1).11, 16
Examples of Large Animal Models in Digestive Disease
Esophageal Disease
The dog and pig have been used extensively to study esophageal disease, with similarities in disease pathophysiology more similar to human beings than that of rodents.35, 36 For instance, in a chronic model of acid reflux disease, the dog develops a phenotype of esophageal adenocarcinoma that is similar to the glandular phenotype seen in human beings as opposed to the mucinous phenotype of mice and rats.37 In pigs, the esophageal and gastroesophageal junctional anatomy and physiology are comparable with that of human beings, both sharing the existence of large, dissectible submucosal glands, making the pig a preferred model for analogous clinical applications.11, 24, 38 In particular, pigs are used commonly to test new surgical and endoscopic techniques in the esophagus. Recently, a pig model of esophageal injury and repair was developed in which endoscopic radiofrequency ablation was used to induce injury, followed by the study of cellular biology of the repair process, including the location and role of proliferative cells.24 This model promises to provide important information on the role of key structures such as esophageal submucosal glands in the repair process.
Necrotizing Enterocolitis
Neonatal mouse models of necrotizing enterocolitis (NEC) have been of limited utility in studies of the disease because of high mortality related to cesarean section rather than to the development of NEC.39 Alternatively, piglets delivered preterm by caesarian section and maintained on a human infant formula diet spontaneously develop NEC within 30 hours of birth in approximately 50% of individuals, providing a powerful tool to investigate the development of this complex multifactorial disease process.40, 41 The piglet is the only animal model described to develop full-scale, clinical NEC in response to the same risk factors correlated to human NEC: prematurity, enteral formula feeding, and unintended bacterial colonization of the intestine.40, 41 The severity of NEC in affected models has made it difficult to use this model repeatedly to produce translational findings, and this work is expensive because of the labor required to maintain NEC model piglets. Nonetheless, the piglet model provides substantial opportunities for further investigation of this devastating disease.
Intestinal Ischemia/Reperfusion Injury
The study of intestinal ischemia/reperfusion injury has been studied in several large animal species. A low-flow ischemic model, as would be seen in hemorrhagic or cardiovascular shock, has been studied extensively and characterized in cats using an adjustable vascular clamp.42, 43 Segmental mesenteric ischemia, as noted in volvulus or trauma, has been induced in the pig, dog, and cat, as well as the horse.44, 45, 46, 47 In each of these models, the choice of animal species has a substantial impact on the pathology and clinical outcome.48 For instance, the porcine small intestinal tract has low levels of the key oxidant-generating enzyme xanthine oxidase, which has been shown to be largely responsible for reperfusion injury in feline and rodent models that have relatively high levels of intestinal xanthine oxidase. Similar to pigs, human beings have low levels of xanthine oxidase, particularly in neonates, as is the case in piglets. This lack of xanthine oxidase has been associated with a minor role of reperfusion injury after segmental ischemia in the pig, and we believe that this is likely the case in the human small intestinal tract.49
Repair and Regeneration of Injured Intestine: Insights From Porcine Studies
One consequence of discovering a minor role of reperfusion injury in porcine small intestinal ischemia was an increased focus on intestinal reparative events.50 Although mucosal epithelial restitution has been studied in an in vitro guinea pig ileum detergent-injury model, many factors have contributed to the feasibility and superiority of the ischemia/reperfusion pig model for the study of the intestinal epithelial barrier.51 In particular, similar intestinal ischemia/reperfusion models in mice result in devitalization of the mucosal tissue in the ex vivo Ussing chamber system, whereas the pig mucosa survives well, allowing intensive study of reparative events.52, 53 The relatively large body size of pigs allows access to long lengths of intestine that can be separated readily into multiple distinct segments for the study of differing periods of ischemia/reperfusion, or the development of more complex models such as Thierry–Vella loops.49 The latter have proved particularly useful for determining the effect of luminal factors on mucosal repair in the conscious animal.54, 55
Early Events in Mucosal Repair
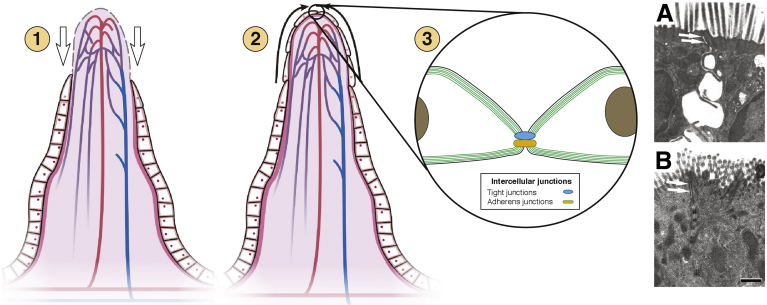
During surgically induced segmental mesenteric ischemia in the small intestine, the epithelium lifts from the basement membrane and sloughs from the villous tips in a time-dependent and highly predictable manner, after which there is a rapid and reproducible early recovery process that occurs before epithelial proliferation: (1) villus contraction, (2) epithelial migration, and (3) tight junction closure (Figure 2).49
Figure 2.
Illustration showing the phases of intestinal epithelial barrier repair. Restoration of barrier function after damage to the epithelium is well characterized to occur in 3 phases. (1) Contraction of villus occurs by smooth muscle fibroblasts in the lamina propria to reduce denuded surface area. (2) Depolarization and migration of wound-associated epithelial cells occurs across the denuded basement membrane to cover the wounded surface. (3) Repolarization and reformation of tight junction structure to seal the paracellular spaces occurs, effectively restoring barrier function. (A) Transmission electron microscopy showing open paracellular space between 2 intestinal epithelial cells with a leaky tight junction (white arrows). (B) TEM showing closed paracellular space and tight junction (white arrows) coinciding with restoration of intestinal barrier function.
Panels A and B were used with permission from Little D, et al. PI3K signaling is required for prostaglandin-induced mucosal recovery in ischemia-injured porcine ileum. Am J Physiol Gastrointest Liver Physiol 2003;284:G46–G56.
Villus contraction
First, individual villi contract, effectively reducing the surface area of denuded basement membrane.56 This process is facilitated by a network of smooth muscle cells and contractile myofibroblasts organized in a 3-dimensional reticular network within the lamina propria.56, 57 Enteric nerves mediate the initial contraction immediately after mucosal injury, whereas the continued contraction is dependent on the production of prostaglandins within the affected tissue.56, 58
Epithelial migration
The second critical step is the depolarization and mobilization of wound-associated epithelial cells that remain in the mucosa after injury, a process termed restitution. This migratory phenotype in the wound-associated epithelial cells begins with a de-differentiation and flattening of the cell (loss of polarity and enterocyte microstructures) and extension of plasma membrane (lamellipodia) in the direction of restitution coinciding with detachment of the trailing edge to facilitate crawling across the denuded basement membrane.51, 59, 60 This process is facilitated by the remodeling of the actin-myosin cytoskeleton to extend and contract the cell plasma membrane; the disassembly, transport, and reassembly of focal adhesion complexes from the trailing edge to the leading edge of the crawling cell; and effective adhesion of transmembrane integrins within these focal adhesions to the extracellular matrix.44
Tight junction restoration
The final and arguably the most critical phase of early barrier repair is resealing of the tight junctions. Once the wound-associated epithelial cells have covered the exposed basement membrane and make cell-to-cell contact over the injured villus tip, tight junctions reassemble at the apical paracellular space and the epithelial barrier is functionally repaired. This process has been studied principally in the porcine ischemia/reperfusion model using ex vivo recovery studies in Ussing chambers, allowing for the measurement of transepithelial electrical resistance and macromolecular fluxes in recovering tissues.61 This work has established a direct correlation between increasing transepithelial electrical resistance, reduction of macromolecular permeability, and recovery of barrier function that is in very large part dependent on the reassembly of tight junctions.62 In other words, although restitution of epithelium is vital for mucosal wound repair, barrier function is not restored until tight junctions are re-assembled. This latter step has been relatively underappreciated in digestive disease research, but emphasized by the pig model as an event that is very likely to be critical to the recovery of barrier function in human beings with a variety of conditions in which the mucosa is injured. As an example of the translational significance of the pig model, tight junction repair has been linked principally to the chloride channel chloride channel 2, and chloride channel 2 agonists presently on the market have been shown to hasten mucosal repair via tight junction modulation in preclinical porcine trials.47
Inflammatory Events
Early reparative events continue unimpeded by inflammation during ex vivo studies in which tissues are not reperfused. However, the role of inflammation in mucosal injury and repair is very important. Other large animal models, particularly studies in the cat, have highlighted the important role of neutrophil-driven reperfusion injury, set off by initial oxidant production by xanthine oxidase.43 As previously mentioned, human and porcine intestine have relatively low expression of xanthine oxidase, with a near-complete absence of reperfusion injury in porcine models of ischemia, hemorrhagic shock, volvulus, and segmental ischemia.49, 63, 64 However, there is an impressive neutrophilic infiltration in postischemic porcine intestine that becomes maximal between 6 and 12 hours in vivo in tissues injured by 2 hours of complete intestinal ischemia. This is essentially the inflammatory phase of wound healing, as would be expected for dermal wounds. Interestingly, although infiltration of neutrophils likely is critical for destroying invading microorganisms, neutrophils damage the recently repaired epithelial barrier as they migrate through the paracellular spaces and physically disrupt tight junctions.63 Porcine studies have shown that blockade of neutrophilic oxidants during the reparative stages of mucosal wound repair can maintain the barrier established by early reparative events.63 Thus, although inflammatory events have been studied extensively in rodent models, the focus on early reperfusion injury in rodent models rather than the role of inflammation during repair, as has been studied to a limited extent in porcine ischemia, has perhaps hampered the translation of anti-inflammatory therapy such as blockade of neutrophil adhesion or function to the level of clinical trials.65 Therefore, the pig may provide findings that can be translated more readily.
Mucosal Proliferative Response
In the subacute period after ischemia/reperfusion, there is an impressive proliferative response from the stem cell niche within the crypts, followed by re-establishment of normal villus structure.49, 66 The latter has been modulated by luminal factors (glutamine and transforming growth factor α) in a Thierry–Vella loop model of porcine ischemic injury.55 In more recent work, the cell lineages that are present along the crypt-villus axis of both pigs and human beings have been shown to have similar morphology and unique biomarkers.27 Importantly, the intestinal crypt base columnar cells of the pig have been characterized morphologically and found to be similar in appearance to human crypt base columnar cells.27 As a model of the stem cell niche, porcine enteroid culture recently was developed, allowing the expansion of epithelial progenitors together with their identification.27 Optimum culture methods to maintain neonatal and adult porcine enteroids for several weeks have been established, and transplantation of intestinal crypts into the omentum of pigs has resulted in the growth of histologically complete intestine including villi, crypts, lamina propria, nerve elements, and muscularis mucosa.27, 67, 68 Methods for cryopreservation and genetic manipulation of porcine enteroids also have been successful, further establishing the porcine enteroid model as a powerful tool for intestinal studies and preclinical assessment.68
Large Animal Cell Culture Models of Intestinal Physiology
To augment the porcine in vivo study of intestinal disease, a novel intestinal epithelial cell line (IPEC-J2) was isolated and cultured from neonatal pig jejunum in 1989 by Helen Berschneider at North Carolina State University that has many unique characteristics. For example, these cells are nontransformed yet have been maintained through 80 to 90 passages. Furthermore, they are derived from the small intestine, unlike frequently used cell lines derived from colonic tissue such as Caco-2, HT-29, and T84 cells, and they consist of a heterogeneous population of cell phenotypes, mimicking the epithelial diversity seen in vivo. IPEC-J2 cells form a fully differentiated columnar epithelial monolayer with an established brush border, tight junction structure, inducible chloride secretion, and a functional barrier as measured by transepithelial electrical resistance and macromolecular fluxes.69, 70 These qualities make this cell line a powerful tool for the study of intestinal biology and disease in the pig that, in turn, means they likely have important translational applications given the similarities between human and porcine intestinal cell populations.27 This cell line has since been used successfully to study key elements of intestinal cell biology, particularly for immunologic and microbiological studies.71 These cells are grown easily on permeable membranes and can be placed in Ussing chambers for advanced barrier physiology studies.69 In addition, the IPEC-J2 line has been transfected successfully by plasmid vector to stably overexpress select targets such as human P-glycoprotein (ABCB1), further supporting this cell line as a powerful tool for the translatable study of small intestinal epithelial biology and disease.72
Future Needs for Large Animal Models and Research Tools
The major limitation of work on large animal models of digestive disease remains the relative lack of genetic models. There are important examples of porcine genetic models of human disease, notably the cystic fibrosis transmembrane conductance regulator (CFTR) knockout pig. Genetically induced cystic fibrosis mouse models do not develop key pathologies in the lung and pancreas seen in human cystic fibrosis, leading Rogers et al73 to produce a CFTR+/- pig to generate a more clinically analogous model of cystic fibrosis to that of human beings. The following generations of CFTR knockout pigs showed cystic fibrosis–like lung disease and severe pancreatic dysfunction within the first few months of life, making this model an important translational model for the study of cystic fibrosis in human beings.74 Although availability of reagents optimized for use in porcine studies lags behind availability for human and murine applications, the market is improving and at the time of this review, a search on the CiteAb database (Bath, United Kingdom) showed in excess of 87,000 antiporcine antibodies cited to perform in biological research applications in pigs. However, additional reagents to identify cellular targets as well as genetic models of disease are needed to further translational work. For example, in the porcine small intestinal stem cell niche, it is not presently possible to identify leucine-rich repeat-containing G-protein–coupled–receptor protein positive crypt-based columnar cells because of a lack of reliable antibodies for this protein marker. In addition, the lack of identifiable Paneth cells in the stem cell niche, based on historically used biomarkers or morphologic features, has presented an interesting dilemma as well as an opportunity to understand the stem cell niche. Specifically, there must be a cell type that supports crypt base columnar cells in the porcine small intestine, as is the case in the colon in pig and human being, where there are no Paneth cells.
Conclusions
Continued work to understand gastrointestinal pathophysiology in the pig using a variety of clinically relevant surgical, interventional, genetic, and cellular models will shed light on the translational significance of recent important basic science findings.
Footnotes
Conflicts of interest The authors disclose no conflicts.
Funding Supported by funding from the National Institutes of Health (DK034987).
References
- 1.Peery A.F., Dellon E.S., Lund J. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology. 2012;143:1179–1187. doi: 10.1053/j.gastro.2012.08.002. e1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Low M.J. Mouse models in gastroenterology research. Gastroenterology. 2012;143:1410–1412. doi: 10.1053/j.gastro.2012.10.011. [DOI] [PubMed] [Google Scholar]
- 3.Chung S.K., Lee A.Y., Chung S.S. Mouse models for human diseases. Hong Kong Med J. 1997;3:201–209. [PubMed] [Google Scholar]
- 4.Wagner S.J., Schmidt A., Effenberger M.J. Semisynthetic diet ameliorates Crohn's disease-like ileitis in TNFDeltaARE/WT mice through antigen-independent mechanisms of gluten. Inflamm Bowel Dis. 2013;19:1285–1294. doi: 10.1097/MIB.0b013e318281f573. [DOI] [PubMed] [Google Scholar]
- 5.Pizarro T.T., Pastorelli L., Bamias G. SAMP1/YitFc mouse strain: a spontaneous model of Crohn's disease-like ileitis. Inflamm Bowel Dis. 2011;17:2566–2584. doi: 10.1002/ibd.21638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boivin G.P., Washington K., Yang K. Pathology of mouse models of intestinal cancer: consensus report and recommendations. Gastroenterology. 2003;124:762–777. doi: 10.1053/gast.2003.50094. [DOI] [PubMed] [Google Scholar]
- 7.Flisikowska T., Merkl C., Landmann M. A porcine model of familial adenomatous polyposis. Gastroenterology. 2012;143:1173–1175. doi: 10.1053/j.gastro.2012.07.110. e1–7. [DOI] [PubMed] [Google Scholar]
- 8.US Department of Health and Human Services. Opportunities and Challenges in Digestive Diseases Research: Recommendations of the National Commission on Digestive Diseases. March 2009; NIH Publication No. 08-6514.
- 9.Cibelli J., Emborg M.E., Prockop D.J. Strategies for improving animal models for regenerative medicine. Cell Stem Cell. 2013;12:271–274. doi: 10.1016/j.stem.2013.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patterson J.K., Lei X.G., Miller D.D. The pig as an experimental model for elucidating the mechanisms governing dietary influence on mineral absorption. Exp Biol Med (Maywood) 2008;233:651–664. doi: 10.3181/0709-MR-262. [DOI] [PubMed] [Google Scholar]
- 11.Kararli T.T. Comparison of the gastrointestinal anatomy, physiology, and biochemistry of humans and commonly used laboratory animals. Biopharm Drug Dispos. 1995;16:351–380. doi: 10.1002/bdd.2510160502. [DOI] [PubMed] [Google Scholar]
- 12.Kirk A.D. Crossing the bridge: large animal models in translational transplantation research. Immunol Rev. 2003;196:176–196. doi: 10.1046/j.1600-065x.2003.00081.x. [DOI] [PubMed] [Google Scholar]
- 13.Block T., Isaksson H.S., Acosta S. Altered mRNA expression due to acute mesenteric ischaemia in a porcine model. Eur J Vasc Endovasc Surg. 2011;41:281–287. doi: 10.1016/j.ejvs.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 14.Yandza T., Tauc M., Saint-Paul M.C. The pig as a preclinical model for intestinal ischemia-reperfusion and transplantation studies. J Surg Res. 2012;178:807–819. doi: 10.1016/j.jss.2012.07.025. [DOI] [PubMed] [Google Scholar]
- 15.Elfenbein J.R., Endicott-Yazdani T., Porwollik S. Novel determinants of intestinal colonization of Salmonella enterica serotype typhimurium identified in bovine enteric infection. Infect Immun. 2013;81:4311–4320. doi: 10.1128/IAI.00874-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Swindle M.M., Makin A., Herron A.J. Swine as models in biomedical research and toxicology testing. Vet Pathol. 2012;49:344–356. doi: 10.1177/0300985811402846. [DOI] [PubMed] [Google Scholar]
- 17.Roura E., Koopmans S.J., Lallès J.P. Critical review evaluating the pig as a model for human nutritional physiology. Nutr Res Rev. 2016;29:60–90. doi: 10.1017/S0954422416000020. [DOI] [PubMed] [Google Scholar]
- 18.Rothkotter H.J., Sowa E., Pabst R. The pig as a model of developmental immunology. Hum Exp Toxicol. 2002;21:533–536. doi: 10.1191/0960327102ht293oa. [DOI] [PubMed] [Google Scholar]
- 19.Bendixen E., Danielsen M., Larsen K. Advances in porcine genomics and proteomics–a toolbox for developing the pig as a model organism for molecular biomedical research. Brief Funct Genomics. 2010;9:208–219. doi: 10.1093/bfgp/elq004. [DOI] [PubMed] [Google Scholar]
- 20.Lunney J.K. Advances in swine biomedical model genomics. Int J Biol Sci. 2007;3:179–184. doi: 10.7150/ijbs.3.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hart E.A., Caccamo M., Harrow J.L. Lessons learned from the initial sequencing of the pig genome: comparative analysis of an 8 Mb region of pig chromosome 17. Genome Biol. 2007;8:R168. doi: 10.1186/gb-2007-8-8-r168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ibrahim Z., Busch J., Awwad M. Selected physiologic compatibilities and incompatibilities between human and porcine organ systems. Xenotransplantation. 2006;13:488–499. doi: 10.1111/j.1399-3089.2006.00346.x. [DOI] [PubMed] [Google Scholar]
- 23.Gonzalez L.M., Moeser A.J., Blikslager A.T. Porcine models of digestive disease: the future of large animal translational research. Transl Res. 2015;166:12–27. doi: 10.1016/j.trsl.2015.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Garman K.S., Orlando R.C., Chen X. Review: experimental models for Barrett's esophagus and esophageal adenocarcinoma. Am J Physiol Gastrointest Liver Physiol. 2012;302:G1231–G1243. doi: 10.1152/ajpgi.00509.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ranjay Chakraborty H.P., Tan C.C., Prunty M. Contribution of body length on axial length during normal eye development in C57BL/6J and 129S1/SvJ wild-type mouse strains. Invest Ophthalmol Vis Sci. 2014;55:3614. [Google Scholar]
- 26.Casteleyn C., Rekecki A., Van der Aa A. Surface area assessment of the murine intestinal tract as a prerequisite for oral dose translation from mouse to man. Lab Anim. 2010;44:176–183. doi: 10.1258/la.2009.009112. [DOI] [PubMed] [Google Scholar]
- 27.Gonzalez L.M., Williamson I., Piedrahita J.A. Cell lineage identification and stem cell culture in a porcine model for the study of intestinal epithelial regeneration. PLoS One. 2013;8:e66465. doi: 10.1371/journal.pone.0066465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen Y.M., Zhang J.S., Duan X.L. Changes of microvascular architecture, ultrastructure and permeability of rat jejunal villi at different ages. World J Gastroenterol. 2003;9:795–799. doi: 10.3748/wjg.v9.i4.795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barker N., van Oudenaarden A., Clevers H. Identifying the stem cell of the intestinal crypt: strategies and pitfalls. Cell Stem Cell. 2012;11:452–460. doi: 10.1016/j.stem.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 30.Graham H., Aman P. The pig as a model in dietary fibre digestion studies. Scand J Gastroenterol Suppl. 1987;129:55–61. doi: 10.3109/00365528709095851. [DOI] [PubMed] [Google Scholar]
- 31.Nguyen T.L.A., Vieira-Silva S., Liston A. How informative is the mouse for human gut microbiota research? Dis Model Mech. 2015;8:1–16. doi: 10.1242/dmm.017400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Miller E.R., Ullrey D.E. The pig as a model for human nutrition. Annu Rev Nutr. 1987;7:361–382. doi: 10.1146/annurev.nu.07.070187.002045. [DOI] [PubMed] [Google Scholar]
- 33.Pang X., Hua X., Yang Q. Inter-species transplantation of gut microbiota from human to pigs. ISME J. 2007;1:156–162. doi: 10.1038/ismej.2007.23. [DOI] [PubMed] [Google Scholar]
- 34.Ley R.E., Backhed F., Turnbaugh P. Obesity alters gut microbial ecology. Proc Natl Acad Sci U S A. 2005;102:11070–11075. doi: 10.1073/pnas.0504978102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abdulnour-Nakhoul S., Nakhoul N.L., Wheeler S.A. Characterization of esophageal submucosal glands in pig tissue and cultures. Dig Dis Sci. 2007;52:3054–3065. doi: 10.1007/s10620-006-9739-3. [DOI] [PubMed] [Google Scholar]
- 36.Long J.D., Orlando R.C. Esophageal submucosal glands: structure and function. Am J Gastroenterol. 1999;94:2818–2824. doi: 10.1111/j.1572-0241.1999.1422_b.x. [DOI] [PubMed] [Google Scholar]
- 37.Kawaura Y., Tatsuzawa Y., Wakabayashi T. Immunohistochemical study of p53, c-erbB-2, and PCNA in Barrett's esophagus with dysplasia and adenocarcinoma arising from experimental acid or alkaline reflux model. J Gastroenterol. 2001;36:595–600. doi: 10.1007/s005350170042. [DOI] [PubMed] [Google Scholar]
- 38.Kapoor H., Lohani K.R., Lee T.H. Animal models of Barrett's esophagus and esophageal adenocarcinoma-past, present, and future. Clin Transl Sci. 2015;8:841–847. doi: 10.1111/cts.12304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tian R., Liu S.X., Williams C. Characterization of a necrotizing enterocolitis model in newborn mice. Int J Clin Exp Med. 2010;3:293–302. [PMC free article] [PubMed] [Google Scholar]
- 40.Azcarate-Peril M.A., Foster D.M., Cadenas M.B. Acute necrotizing enterocolitis of preterm piglets is characterized by dysbiosis of ileal mucosa-associated bacteria. Gut Microbes. 2011;2:234–243. doi: 10.4161/gmic.2.4.16332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sangild P.T., Siggers R.H., Schmidt M. Diet- and colonization-dependent intestinal dysfunction predisposes to necrotizing enterocolitis in preterm pigs. Gastroenterology. 2006;130:1776–1792. doi: 10.1053/j.gastro.2006.02.026. [DOI] [PubMed] [Google Scholar]
- 42.Weixiong H., Aneman A., Nilsson U. Quantification of tissue damage in the feline small intestine during ischaemia-reperfusion: the importance of free radicals. Acta Physiol Scand. 1994;150:241–250. doi: 10.1111/j.1748-1716.1994.tb09683.x. [DOI] [PubMed] [Google Scholar]
- 43.Granger D.N., McCord J.M., Parks D.A. Xanthine oxidase inhibitors attenuate ischemia-induced vascular permeability changes in the cat intestine. Gastroenterology. 1986;90:80–84. doi: 10.1016/0016-5085(86)90078-8. [DOI] [PubMed] [Google Scholar]
- 44.Cook V.L., Jones Shults J., McDowell M. Attenuation of ischaemic injury in the equine jejunum by administration of systemic lidocaine. Equine Vet J. 2008;40:353–357. doi: 10.2746/042516408X293574. [DOI] [PubMed] [Google Scholar]
- 45.Filez L., Stalmans W., Penninckx F. Influences of ischemia and reperfusion on the feline small-intestinal mucosa. J Surg Res. 1990;49:157–163. doi: 10.1016/0022-4804(90)90255-z. [DOI] [PubMed] [Google Scholar]
- 46.Arakawa K., Takeyoshi I., Akao Y. Bradykinin B2 receptor antagonist FR173657 ameliorates small bowel ischemia-reperfusion injury in dogs. Dig Dis Sci. 2005;50:27–36. doi: 10.1007/s10620-005-1273-1. [DOI] [PubMed] [Google Scholar]
- 47.Moeser A.J., Nighot P.K., Engelke K.J. Recovery of mucosal barrier function in ischemic porcine ileum and colon is stimulated by a novel agonist of the ClC-2 chloride channel, lubiprostone. Am J Physiol Gastrointest Liver Physiol. 2007;292:G647–G656. doi: 10.1152/ajpgi.00183.2006. [DOI] [PubMed] [Google Scholar]
- 48.Gonzalez L.M., Moeser A.J., Blikslager A.T. Animal models of ischemia-reperfusion-induced intestinal injury: progress and promise for translational research. Am J Physiol Gastrointest Liver Physiol. 2015;308:G63–G75. doi: 10.1152/ajpgi.00112.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Blikslager A.T., Roberts M.C., Rhoads J.M. Is reperfusion injury an important cause of mucosal damage after porcine intestinal ischemia? Surgery. 1997;121:526–534. doi: 10.1016/s0039-6060(97)90107-0. [DOI] [PubMed] [Google Scholar]
- 50.Blikslager A.T., Moeser A.J., Gookin J.L. Restoration of barrier function in injured intestinal mucosa. Physiol Rev. 2007;87:545–564. doi: 10.1152/physrev.00012.2006. [DOI] [PubMed] [Google Scholar]
- 51.Moore R., Carlson S., Madara J.L. Rapid barrier restitution in an in vitro model of intestinal epithelial injury. Lab Invest. 1989;60:237–244. [PubMed] [Google Scholar]
- 52.Moeser A.J., Nighot P.K., Ryan K.A. Mice lacking the Na+/H+ exchanger 2 have impaired recovery of intestinal barrier function. Am J Physiol Gastrointest Liver Physiol. 2008;295:G791–G797. doi: 10.1152/ajpgi.00538.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nighot P.K., Blikslager A.T. Chloride channel ClC-2 modulates tight junction barrier function via intracellular trafficking of occludin. Am J Physiol Cell Physiol. 2012;302:C178–C187. doi: 10.1152/ajpcell.00072.2011. [DOI] [PubMed] [Google Scholar]
- 54.Blikslager A.T., Rhoads J.M., Bristol D.G. Glutamine and transforming growth factor-alpha stimulate extracellular regulated kinases and enhance recovery of villous surface area in porcine ischemic-injured intestine. Surgery. 1999;125:186–194. [PubMed] [Google Scholar]
- 55.Ahdieh N., Blikslager A.T., Bhat B.G. L-glutamine and transforming growth factor-alpha enhance recovery of monoacylglycerol acyltransferase and diacylglycerol acyltransferase activity in porcine postischemic ileum. Pediatr Res. 1998;43:227–233. doi: 10.1203/00006450-199802000-00012. [DOI] [PubMed] [Google Scholar]
- 56.Moore R., Carlson S., Madara J.L. Villus contraction aids repair of intestinal epithelium after injury. Am J Physiol. 1989;257:G274–G283. doi: 10.1152/ajpgi.1989.257.2.G274. [DOI] [PubMed] [Google Scholar]
- 57.Joyce N.C., Haire M.F., Palade G.E. Morphologic and biochemical evidence for a contractile cell network within the rat intestinal mucosa. Gastroenterology. 1987;92:68–81. doi: 10.1016/0016-5085(87)90841-9. [DOI] [PubMed] [Google Scholar]
- 58.Gookin J.L., Rhoads J.M., Argenzio R.A. Inducible nitric oxide synthase mediates early epithelial repair of porcine ileum. Am J Physiol Gastrointest Liver Physiol. 2002;283:G157–G168. doi: 10.1152/ajpgi.00005.2001. [DOI] [PubMed] [Google Scholar]
- 59.Dignass A., Lynch-Devaney K., Kindon H. Trefoil peptides promote epithelial migration through a transforming growth factor beta-independent pathway. J Clin Invest. 1994;94:376–383. doi: 10.1172/JCI117332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Albers T.M., Lomakina I., Moore R.P. Fate of polarized membrane components and evidence for microvillus disassembly on migrating enterocytes during repair of native intestinal epithelium. Lab Invest. 1995;73:139–148. [PubMed] [Google Scholar]
- 61.Blikslager A.T., Roberts M.C., Argenzio R.A. Prostaglandin-induced recovery of barrier function in porcine ileum is triggered by chloride secretion. Am J Physiol. 1999;276:G28–G36. doi: 10.1152/ajpgi.1999.276.1.G28. [DOI] [PubMed] [Google Scholar]
- 62.Little D., Dean R.A., Young K.M. PI3K signaling is required for prostaglandin-induced mucosal recovery in ischemia-injured porcine ileum. Am J Physiol Gastrointest Liver Physiol. 2003;284:G46–G56. doi: 10.1152/ajpgi.00121.2002. [DOI] [PubMed] [Google Scholar]
- 63.Gayle J., Jones S.L., Argenzio R.A. Neutrophils increase paracellular permeability of restituted ischemic-injured porcine ileum. Surgery. 2002;132:461–470. doi: 10.1067/msy.2002.125320. [DOI] [PubMed] [Google Scholar]
- 64.Kubes P., Hunter J., Granger D.N. Ischemia/reperfusion-induced feline intestinal dysfunction: importance of granulocyte recruitment. Gastroenterology. 1992;103:807–812. doi: 10.1016/0016-5085(92)90010-v. [DOI] [PubMed] [Google Scholar]
- 65.Mallick I.H., Yang W., Winslet M.C. Ischemia-reperfusion injury of the intestine and protective strategies against injury. Dig Dis Sci. 2004;49:1359–1377. doi: 10.1023/b:ddas.0000042232.98927.91. [DOI] [PubMed] [Google Scholar]
- 66.Pucilowska J.B., Williams K.L., Lund P.K. Fibrogenesis. IV. Fibrosis and inflammatory bowel disease: cellular mediators and animal models. Am J Physiol Gastrointest Liver Physiol. 2000;279:G653–G659. doi: 10.1152/ajpgi.2000.279.4.G653. [DOI] [PubMed] [Google Scholar]
- 67.Sala F.G., Kunisaki S.M., Ochoa E.R. Tissue-engineered small intestine and stomach from autologous tissue in a preclinical large animal model. J Surg Res. 2009;156:205–212. doi: 10.1016/j.jss.2009.03.062. [DOI] [PubMed] [Google Scholar]
- 68.Khalil H.A., Lei N.Y., Brinkley G. A novel culture system for adult porcine intestinal crypts. Cell Tissue Res. 2016;365:123–134. doi: 10.1007/s00441-016-2367-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Silke S., Zakrzewski J.F.R., Krug S.M. Improved cell line IPEC-J2, characterized as a model for porcine jejunal epithelium. PLoS One. 2013;8:e79643. doi: 10.1371/journal.pone.0079643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Nossol C., Barta-Boszormenyi A., Kahlert S. Comparing two intestinal porcine epithelial cell lines (IPECs): morphological differentiation, function and metabolism. PLoS One. 2015;10:e0132323. doi: 10.1371/journal.pone.0132323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Brosnahan A.J., Brown D.R. Porcine IPEC-J2 intestinal epithelial cells in microbiological investigations. Vet Microbiol. 2012;156:229–237. doi: 10.1016/j.vetmic.2011.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Saaby L., Helms H.C., Brodin B. IPEC-J2 MDR1, a novel high-resistance cell line with functional expression of human P-glycoprotein (ABCB1) for drug screening studies. Mol Pharm. 2016;13:640–652. doi: 10.1021/acs.molpharmaceut.5b00874. [DOI] [PubMed] [Google Scholar]
- 73.Rogers C.S., Hao Y., Rokhlina T. Production of CFTR-null and CFTR-DeltaF508 heterozygous pigs by adeno-associated virus-mediated gene targeting and somatic cell nuclear transfer. J Clin Invest. 2008;118:1571–1577. doi: 10.1172/JCI34773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Keiser N.W., Engelhardt J.F. New animal models of cystic fibrosis: what are they teaching us? Curr Opin Pulm Med. 2011;17:478–483. doi: 10.1097/MCP.0b013e32834b14c9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Smith F., Clark J.E., Overman B.L. Early weaning stress impairs development of mucosal barrier function in the porcine intestine. Am J Physiol Gastrointest Liver Physiol. 2010;298:G352–G363. doi: 10.1152/ajpgi.00081.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Moeser A.J., Ryan K.A., Nighot P.K. Gastrointestinal dysfunction induced by early weaning is attenuated by delayed weaning and mast cell blockade in pigs. Am J Physiol Gastrointest Liver Physiol. 2007;293:G413–G421. doi: 10.1152/ajpgi.00304.2006. [DOI] [PubMed] [Google Scholar]
- 77.Moeser A.J., Klok C.V., Ryan K.A. Stress signaling pathways activated by weaning mediate intestinal dysfunction in the pig. Am J Physiol Gastrointest Liver Physiol. 2007;292:G173–G181. doi: 10.1152/ajpgi.00197.2006. [DOI] [PubMed] [Google Scholar]
- 78.Overman E.L., Rivier J.E., Moeser A.J. CRF induces intestinal epithelial barrier injury via the release of mast cell proteases and TNF-alpha. PLoS One. 2012;7:e39935. doi: 10.1371/journal.pone.0039935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Schreiber K.L., Brown D.R. Adrenocorticotrophic hormone modulates Escherichia coli O157:H7 adherence to porcine colonic mucosa. Stress. 2005;8:185–190. doi: 10.1080/10253890500188732. [DOI] [PubMed] [Google Scholar]
- 80.Chen C., Lyte M., Stevens M.P. Mucosally-directed adrenergic nerves and sympathomimetic drugs enhance non-intimate adherence of Escherichia coli O157:H7 to porcine cecum and colon. Eur J Pharmacol. 2006;539:116–124. doi: 10.1016/j.ejphar.2006.03.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Schmidt L.D., Xie Y., Lyte M. Autonomic neurotransmitters modulate immunoglobulin A secretion in porcine colonic mucosa. J Neuroimmunol. 2007;185:20–28. doi: 10.1016/j.jneuroim.2006.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Tang Z.H., Qiang J.W., Feng X.Y. Acute mesenteric ischemia induced by ligation of porcine superior mesenteric vein: multidetector CT evaluations. Acad Radiol. 2010;17:1146–1152. doi: 10.1016/j.acra.2010.04.014. [DOI] [PubMed] [Google Scholar]
- 83.Bruhn R.S., Distelmaier M.S., Hellmann-Sokolis M. Early detection of acute mesenteric ischemia using diffusion-weighted 3.0-T magnetic resonance imaging in a porcine model. Invest Radiol. 2013;48:231–237. doi: 10.1097/RLI.0b013e3182809143. [DOI] [PubMed] [Google Scholar]
- 84.Klein H.M., Klosterhalfen B., Kinzel S. CT and MRI of experimentally induced mesenteric ischemia in a porcine model. J Comput Assist Tomogr. 1996;20:254–261. doi: 10.1097/00004728-199603000-00016. [DOI] [PubMed] [Google Scholar]
- 85.Jacobi S.K., Moeser A.J., Corl B.A. Dietary long-chain PUFA enhance acute repair of ischemia-injured intestine of suckling pigs. J Nutr. 2012;142:1266–1271. doi: 10.3945/jn.111.150995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Acosta S., Nilsson T.K., Malina J. L-lactate after embolization of the superior mesenteric artery. J Surg Res. 2007;143:320–328. doi: 10.1016/j.jss.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 87.Gookin J.L., Galanko J.A., Blikslager A.T. PG-mediated closure of paracellular pathway and not restitution is the primary determinant of barrier recovery in acutely injured porcine ileum. Am J Physiol Gastrointest Liver Physiol. 2003;285:G967–G979. doi: 10.1152/ajpgi.00532.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Thymann T., Moller H.K., Stoll B. Carbohydrate maldigestion induces necrotizing enterocolitis in preterm pigs. Am J Physiol Gastrointest Liver Physiol. 2009;297:G1115–G1125. doi: 10.1152/ajpgi.00261.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Van Haver E.R., Sangild P.T., Oste M. Diet-dependent mucosal colonization and interleukin-1beta responses in preterm pigs susceptible to necrotizing enterocolitis. J Pediatr Gastroenterol Nutr. 2009;49:90–98. doi: 10.1097/MPG.0b013e31818de393. [DOI] [PubMed] [Google Scholar]
- 90.Siggers R.H., Siggers J., Boye M. Early administration of probiotics alters bacterial colonization and limits diet-induced gut dysfunction and severity of necrotizing enterocolitis in preterm pigs. J Nutr. 2008;138:1437–1444. doi: 10.1093/jn/138.8.1437. [DOI] [PubMed] [Google Scholar]
- 91.Sangild P.T., Petersen Y.M., Schmidt M. Preterm birth affects the intestinal response to parenteral and enteral nutrition in newborn pigs. J Nutr. 2002;132:3786–3794. doi: 10.1093/jn/132.9.2673. [DOI] [PubMed] [Google Scholar]
- 92.Pereira-Fantini P.M., Thomas S.L., Wilson G. Short- and long-term effects of small bowel resection: a unique histological study in a piglet model of short bowel syndrome. Histochem Cell Biol. 2011;135:195–202. doi: 10.1007/s00418-011-0778-2. [DOI] [PubMed] [Google Scholar]
- 93.Vegge A., Thymann T., Lund P. Glucagon-like peptide-2 induces rapid digestive adaptation following intestinal resection in preterm neonates. Am J Physiol Gastrointest Liver Physiol. 2013;305:G277–G285. doi: 10.1152/ajpgi.00064.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Aigner B., Renner S., Kessler B. Transgenic pigs as models for translational biomedical research. J Mol Med (Berl) 2010;88:653–664. doi: 10.1007/s00109-010-0610-9. [DOI] [PubMed] [Google Scholar]
- 95.Fan N., Lai L. Genetically modified pig models for human diseases. J Genet Genomics. 2013;40:67–73. doi: 10.1016/j.jgg.2012.07.014. [DOI] [PubMed] [Google Scholar]
- 96.Whyte J.J., Prather R.S. Genetic modifications of pigs for medicine and agriculture. Mol Reprod Dev. 2011;78:879–891. doi: 10.1002/mrd.21333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Fisher J.T., Zhang Y., Engelhardt J.F. Comparative biology of cystic fibrosis animal models. Methods Mol Biol. 2011;742:311–334. doi: 10.1007/978-1-61779-120-8_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Grussner R., Nakhleh R., Grussner A. Streptozotocin-induced diabetes mellitus in pigs. Horm Metab Res. 1993;25:199–203. doi: 10.1055/s-2007-1002076. [DOI] [PubMed] [Google Scholar]
- 99.Barb C.R., Cox N.M., Carlton C.A. Growth hormone secretion, serum, and cerebral spinal fluid insulin and insulin-like growth factor-I concentrations in pigs with streptozotocin-induced diabetes mellitus. Proc Soc Exp Biol Med. 1992;201:223–228. doi: 10.3181/00379727-201-43503. [DOI] [PubMed] [Google Scholar]