Abstract
The molecular mechanisms used by the gonococcus to initiate infection exhibit gender specificity. The clinical presentations of disease are also strikingly different upon comparison of gonococcal urethritis to gonococcal cervicitis. An intimate association occurs between the gonococcus and the urethral epithelium and is mediated by the asialoglycoprotein receptor. Gonococcal interaction with the urethral epithelia cell triggers cytokine release, which promotes neutrophil influx and an inflammatory response. Similarly, gonococcal infection of the upper female genital tract also results in inflammation. Gonococci invade the nonciliated epithelia, and the ciliated cells are subjected to the cytotoxic effects of tumor necrosis factor alpha induced by gonococcal peptidoglycan and lipooligosaccharide. In contrast, gonococcal infection of the lower female genital tract is typically asymptomatic. This is in part the result of the ability of the gonococcus to subvert the alternative pathway of complement present in the lower female genital tract. Gonococcal engagement of complement receptor 3 on the cervical epithelia results in membrane ruffling and does not promote inflammation. A model of gonococcal pathogenesis is presented in the context of the male and female human urogenital tracts.
INTRODUCTION
Neisseria gonorrhoeae, the gonococcus, is a gram-negative diplococcus which causes the sexually transmitted disease gonorrhea. Reference to the contagious nature of gonococcal infection dates back to biblical times (Lev. 15:1-15:19), making gonorrhea one of the oldest recorded human diseases. Today, gonococcal infection remains a major global health problem, as more than sixty million cases are reported annually worldwide (78). The highest incidence of disease and disease sequelae occurs in less well developed countries; however, greater than 300,000 cases are reported to the Centers for Disease Control and Prevention in the United States each year (41). Teenagers and young adults are at high risk for infection, which is unsettling in view of the increased risk associated with gonorrhea for infection with human immunodeficiency virus (HIV) type 1 (264). The gonococcus-induced increase in the local expression of viral RNA, in conjunction with the acute inflammatory response generated with gonococcal disease and the subsequent loss of mucosal integrity, is associated with the increased susceptibility to HIV type 1 (42). In addition, susceptibility to chronic complications associated with N. gonorrhoeae disease is a specific problem in women because of the asymptomatic nature commonly associated with gonococcal cervicitis and the subsequent spread to the upper genital tract (26, 58, 59, 134, 229). Ascending gonococcal infection occurs in up to 45% of infected women (26, 109, 134, 229) and can result in pelvic inflammatory disease (PID), which can cause permanent fallopian tube scarring and blockage, with subsequent infertility and ectopic pregnancies. One in 10 women suffers from PID (8), of which N. gonorrhoeae is the etiological agent in 40% of all reported cases (241).
N. gonorrhoeae is an exclusive human pathogen that primarily infects the urogenital epithelia. Although the urethra and the uterine cervix serve as the initial sites for gonococcal infection in men and women, respectively, infections of the conjunctiva, pharynx, and rectal mucosa are also reported. N. gonorrhoeae infection of these distinctly different epithelial cell surfaces leads to a spectrum of clinical manifestations of disease (reviewed in references 58, 109, and 229). Disseminated disease, although uncommon, can cause arthritis-dermatitis syndrome, endocarditis, and/or meningitis. Studies reveal that the gonococcus can enter human cells (257), but only recently has it been shown that the organism is intracellular during human infection (5). A repertoire of virulence factors have been identified and allow this bacterium to successfully adapt to variable microenvironments within its sole human host. This human adaptability and the repeated phase and antigenic change displayed by the gonococcus have hampered vaccine development. Many of the major virulence factors undergo phase and/or antigenic variation (227), including the pilus (56, 73), opacity-associated (Opa) outer membrane proteins (139, 229), and lipooligosaccharide (LOS) (32, 53, 211, 270). Porin expression is stable for any given strain of N. gonorrhoeae, and the porin is present as either a PI.A or a PI.B isotype. Porin is highly immunogenic (104, 226). However, porin is intimately associated with reduction-modifiable protein (Rmp or P.III) (21, 25, 27, 152, 180) and with LOS (107) in the outer gonococcal membrane. Blocking antibodies to Rmp (68, 121, 151, 203, 204, 205) and to LOS (68) impair an efficacious immune response developed against porin. Therefore, a functional immune response may be only minimally stimulated by gonococcal infection or by vaccination (105, 245).
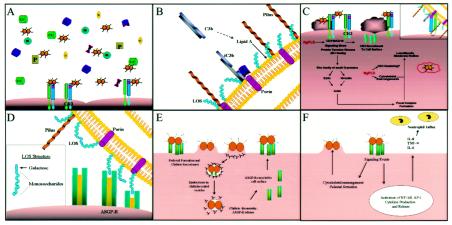
This paper is not a global review of neisserial pathogenesis but rather attempts to incorporate into a working model recent advances made in understanding the molecular factors involved in gonococcal infection and in disease progression and transmission. It is hoped that assembling such a model in the context of the human male and female (uro)genital tracts (Fig. 1) will complement our understanding of gonococcal pathogenesis at the level of human disease. The reader is directed to the writings of several researchers who have eloquently reviewed specific factors currently thought to contribute to neisserial pathogenesis (55, 102, 163, 192).
FIG. 1.
(A to C) Working model of gonococcal pathogenesis within the lower female genital tract. Alternative pathway complement components are produced and released by the cervical epithelia (A). Upon N. gonorrhoeae infection, complement is activated. Gonococcal pilus binds to the I-domain of CR3 allowing the bacterium to overcome the electrostatic repulsion between its own cell surface and that of the host cell. This places the gonococcus within proximity to the cervical cell surface where complement components would be sufficient to allow deposition upon the bacterial cell surface (B). C3b forms a covalent association with the lipid A core of gonococcal LOS and is rapidly inactivated to iC3b. The affinity of gonococcal porin for factor H may augment iC3b formation. The proximity of porin to LOS in the outer membrane may spatially favor the intimate association between iC3b and porin with the CR3 I-domain (C [inset]). Engagement of CR3 triggers a complex signal transduction cascade mediated by the Src-family tyrosine kinases and Rho GTPases (C). These processes result in vinculin- and ezrin-enriched focal complex formation and membrane ruffling, i.e., trigger mechanism of invasion. Secreted NgPLD modulates cervical cell signal transduction by playing a role in CR3 recruitment to the cervical cell surface and by modulating cytoskeletal reorganization. Additionally this protein augments intracellular survival of gonococci after their internalization within macropinosomes. Sialylated gonococci are eventually released from the cervical cell, where they are free to invade more of the cervical epithelia or where they become primed for transmission to the male urethra upon sialic acid removal by sialidases present within the female genital tract. (D) Invasion of the male urethral epithelium is mediated by an interaction between the terminal galactose moiety of LOS and the ASGP-R. (E) An intimate association occurs between the gonococcus and the urethral cell membrane, i.e., the zippering mechanism of invasion. Clathrin is recruited to the site of ASGP-R, and gonococcus-ASGP-R complexes are internalized in clathrin-coated pits in an actin-dependent process. Within the endosome a drop in pH is proposed to release the ASGP-R from the gonococcus surface, and clathrin molecules are lost. ASGP-R is recruited to the urethral cell surface, where it is available to serve as a receptor for more gonococci. (F) Engagement of the ASGP-R triggers cellular responses resulting in membrane pedestal formation beneath receptor-gonococcus complexes and activation of transcription factors required for the production of the inflammatory cytokines IL-6, IL-8, and TNF-α. Neutrophil influx accompanies cytokine release. Sialylated gonococci are eventually released from the urethral epithelium, where they can then be transmitted to a female partner. However, sialic acid on the gonococcus surface does not influence the ability of these organisms to associate with the uterine cervix.
GONORRHEA: A HISTORICAL PERSPECTIVE
Reference to N. gonorrhoeae infection can be found in biblical text within the Book of Leviticus (229) and in ancient Chinese writings (95), making gonorrhea one of the oldest diseases known to humans. Hippocrates referred to acute gonorrhea as “strangury” obtained from the “pleasures of Venus” in the fourth and fifth centuries b.c. (229). It was not until A.D. 130 that Galen, who mistakenly confused the purulent discharge associated with gonococcal urethritis with semen, introduced the term gonorrhea, i. e., “flow of seed” (95, 229). The most notable account of N. gonorrhoeae infection is found in the personal diary of James Boswell, the famous biographer of Samuel Johnson. Within these pages, Boswell described more than 19 separate infections with the gonococcus, the consequences of which ultimately led to his death (182). Boswell also described what might possibly be the consequence of asymptomatic infection in women, in that his wife, who reportedly never exhibited symptoms of gonococcal infection, lost four of her nine pregnancies (182). Neisser described the causative agent of gonorrhea, N. gonorrhoeae, in 1879; however, it was not until 1882 that Leistikow and Löffler finally cultivated the gonococcus (95, 229).
The advent of sulfonamide (in 1936) and penicillin (in 1943) antibiotic therapy for the treatment of N. gonorrhoeae infection led to a rapid decrease in gonorrhea prevalence (95, 109, 229). In the early 1960s this trend reversed with the onset of oral contraceptive methods, and N. gonorrhoeae infections reached a peak incidence of over one million reported cases in 1978 in the United States (95, 134). In the late 1980s, with the onset of the HIV epidemic and a coincident widespread use of barrier contraceptives, the incidence of gonococcal infection again declined (134). A recent increase in all sexually transmitted diseases is currently observed globally, as is the emergence of antibiotic resistance among organisms causing these diseases (19, 25, 112, 248). Today the incidence of gonorrhea in the United States is greater than five times that observed in Europe, although comparable high-risk groups exist in both regions (248). Additionally, the gonorrhea incidence in Australia is currently the highest that it has been in 20 years (25).
Close sexual contact with an infected individual serves as the primary mode of N. gonorrhoeae transmission; however, pregnant women with gonococcal disease can transmit this bacterium to their children during delivery. The gonococcus is transmitted more efficiently from an infected man to a woman (50 to 73% probability, independent of number of exposures) (26, 95, 141) than from an infected woman to a man (20 to 35% probability with one exposure) (30, 95, 109). The efficiency with which the gonococcus is transmitted to a woman is thought to correlate with the extended length of time that target membranes are in contact with this pathogen after sexual exposure, because of the anatomical differences in the genitalia of males and females (26, 109). Successful colonization by the gonococcus results in a broad spectrum of clinical manifestations of disease that are, in part, determined by the particular strain that initiates the diseased state and the anatomical site of infection.
MODELS USED TO STUDY GONOCOCCAL PATHOGENESIS
Despite the historic prevalence of N. gonorrhoeae within the human population and the considerable severity and frequency with which adverse complications accompany disease (most notably in women), it has only been in recent years that we have begun to understand gonococcal pathogenesis as it occurs within its sole human host. Discernment of gonococcal pathogenesis is hindered by the lack of an animal model that closely mimics human disease and that can be efficiently used to study the pathology of N. gonorrhoeae infection. Although several animal models have been described (for reviews, see references 10 and 11), no animal model exists that mirrors the full spectrum of disease caused by the gonococcus at any given site within the human body. Consequently, researchers have relied on the use of human volunteers, tissue and organ cultures, and immortalized or malignant tissue culture cell lines to study gonococcal pathogenesis (26, 35, 119, 154, 228, 233, 258). Logic would dictate that the propensity of gonococci to undergo both phase and antigenic variation, in a seemingly random process, would be subject to variable selective environmental pressures dependent upon a chosen model system. Therefore, in selecting a model system by which to study gonococcal pathogenesis, it is paramount to consider the specific question under study.
The human male experimental challenge model (48) and the development of a primary human male urethral epithelial cell culture system (97) have greatly enhanced our knowledge of the specific factors involved in early events permitting N. gonorrhoeae colonization of the urethral epithelium. These models do not evaluate cellular and molecular events occurring with sustained infection. Additionally, clinical observations and data obtained from in vitro infection studies suggest that conclusions drawn from the study of these male infection models cannot be extrapolated to pertain to infection in women. The severity of adverse complications associated with N. gonorrhoeae infection in women ethically limits human studies to male volunteers. Microscopic analyses of clinical biopsies (64, 67, 69, 120) and of male urethral exudates (5) have provided some insight into successful gonococcal infection as it occurs in vivo, but these analyses are also not without caveats in that they are subject to personal observation and interpretation. Additionally, observations made cannot be correlated to pertain to any given time point postinfection.
Primary cell and organ culture systems have also been developed to examine the gonococcal interaction within the lower and upper female genital tracts; however, these systems are site specific, and, consequently, a global analysis of the female genital tract is not possible. The female genital tract is composed of a heterogeneous mixture of epithelia, forming a complex microenvironment which is not easily replicated in vitro and which is subject to change concurrent with a woman's menses cycle. Thus, it is possible that data obtained from primary cell and organ culture might provide only a small hint of gonococcal pathogenesis as it occurs in vivo at any site within the female genital tract. The development of a female mouse model of genital tract infection has served and will continue to serve as a valuable tool by which to study gonococcal pathogenesis in an immunologically defined environment (116, 132, 243). However, it is currently not clear whether data obtained from the mouse model of female genital tract infection is reflective of infection as it occurs within the human female genital tract, because mice fail to express several human-specific receptors (e.g., CR3, CD46, and CEACAM) that are believed to play critical roles in potentiating gonococcal disease. Additionally, high levels of estrogen are required to establish infection in mice (116, 243), and the contribution of increased estrogen to the data obtained is not known (15).
Researchers routinely rely on the use of immortal and malignant cell lines to study molecular factors involved in gonococcal pathogenesis. These systems are advantageous in that they are readily available, easy to maintain, and amenable to manipulation. Cell lines are often altered in their protein and receptor expression patterns because of their immortal nature and continued laboratory maintenance (54, 60, 76, 111, 127, 135, 137, 140, 144, 145, 165, 166, 188, 215, 219, 220, 222, 223, 224, 237, 255). Additionally, altered protein expression can result in additive or synergistic alternative functional responses within these immortal cells compared to their respective parental tissues. It is also noteworthy that some cell lines commonly used to study gonococcal pathogenesis are of ambiguous or irrelevant (with respect to natural infection) origin. It is therefore difficult to extrapolate data obtained from the use of immortal cell lines to gonococcal infection at any specific site within the sole human host, and caution must be exercised when drawing conclusions from these studies because immortal cell lines may not be truly representative of the epithelia encountered by the gonococcus in vivo. However, the use of immortal cells has greatly contributed to our knowledge of both the human and the gonococcal constituents that might play a role in potentiating disease in vivo. Gonococcal outer membrane constituents that are predominately thought to play a role in epithelial cell colonization and invasion include pili, Opa, porin, and LOS.
OUTER MEMBRANE CONSTITUENTS ASSOCIATED WITH GONOCOCCAL VIRULENCE
Several groups have demonstrated that pili play a critical role in forming an initial attachment with host cells (28, 29, 48, 155, 128, 238). Through their ability to exhibit twitching motility, pili may also provide one mechanism by which nonmotile gonococci are able to colonize and to ascend mucosal surfaces (106, 256). The complement regulatory protein, CD46 (or membrane cofactor receptor), is a human-specific, transmembrane protein that is expressed by all nucleated cells. In some cells, CD46 has been demonstrated to serve as a receptor for gonococcal pilus (124, 126). In ME-180 cervical carcinoma cells, the association of pili with CD46 results in a rapid cytoplasmic calcium flux derived from intracellular calcium stores (125). In a separate study using the A431 epidermoid carcinoma cell line, a pilus-induced calcium flux resulted in the exocytosis of host cell lysosomal contents, with some lysosome-associated membrane protein 1 (Lamp1) redistribution to the plasma membrane (12, 13). Pilus engagement has also been demonstrated to play a role in host cell cytoskeletal rearrangements (90, 161, 162). Collectively, these data suggest that pili modulate host cell signaling mechanisms to aid gonococcal epithelial invasion.
Opa proteins are thought to contribute to the cellular trophisms exhibited by gonococci and are divided into two classes based on their ability to differentially recognize host cell surface molecules. These classes are represented by Opa50, i.e., Opa proteins that recognize host cell heparin sulfate proteoglycans (HSPG), and Opa52, i.e., Opa proteins that recognize members of the carcinoembryonic antigen-related family of cell adhesion molecules (CEACAM or CD66) (40). Vitronectin (61, 62, 81) and fibronectin (250) function as required bridging molecules between the gonococcus and its target HSPG receptor(s). Association with an integrin coreceptor (αvβ3 or αvβ5 for vitronectin-mediated adherence or αvβ1 for fibronectin-mediated adherence) triggers a signaling cascade within the target cell that is dependent upon the activation of protein kinase C (55).
In Chang conjunctiva epithelial cells, a direct Opa50-HSPG interaction has been demonstrated (84). This interaction is thought to trigger a signal transduction cascade resulting in phosphatidylcholine-dependent phospholipase C-mediated generation of diacylglycerol (84). Generation of diacylglycerol in turn activates acidic spingomyelinase and results in ceramide production from spingomyelin (84). These processes are speculated to modulate the cytoskeletal rearrangements required for endocytosis of the cell-associated gonococcus (84, 85).
CEACAMs exist as variable isoforms that are differentially expressed by a variety of different cell types. Two isoforms, CEACAM1 (or CD66a) and CEACAM5 (or CD66e), are found on some epithelial cells. Although Opa proteins have been demonstrated to colocalize with CEACAM in tissue culture cell lines (45, 86, 252, 253), CEACAM expression is altered in immortal cells (108, 110, 133, 138, 179, 181, 213), and therefore an Opa-CEACAM interaction at the level of the mucosal epithelia may or may not actually occur in vivo. However, Virji et al. have suggested that more than 95% of Opa-expressing N. gonorrhoeae clinical isolates are able to bind CEACAM1, suggesting that an Opa-CEACAM association can occur in vivo (253). Opa-CEACAM interactions have also been demonstrated on professional phagocytic cells (1, 44, 87, 252). CEACAM engagement on professional phagocytic cells results in the activation of the host cell Src tyrosine kinases, Hck and Fgr (221), which is then followed by Rac activation (103). Rac activation, in turn, triggers cytoskeletal rearrangement and internalization of the gonococcus (103).
Opa proteins were originally identified by their ability to confer opacity and color changes to colonies of N. gonorrhoeae grown on translucent agar when they are viewed under diffused light with a stereomicroscope (113, 239). Subsequent studies revealed that opacity is the result of Opa-LOS interactions that occur between adjacent bacteria (22, 24, 189, 251). Therefore, the interaction of Opa with a target host cell may be modulated by specific LOS moieties expressed by a gonococcus. In contrast to the lipopolysaccharide (LPS) that is prevalent among gram-negative bacteria, the pathogenic neisseriae possess within their outer membranes LOS molecules, which lack the repeating O-antigen sugar that comprises the polysaccharide side chain of LPS (reviewed in references 79, 147, 190, and 251). The oligosaccharide substitutions of LOS exhibit both inter- and intrastrain variability (7, 57, 91). Interconversion of LOS oligosaccharides occurs spontaneously and is dependent upon the presence or absence of available substrates for and enzymes involved in LOS biosynthesis (32, 53, 130, 211, 270). The spontaneous conversion of oligosaccharide determinants can change the manner in which the gonococcus associates with host tissues and, hence, can potentially alter the course of gonococcal disease. LOS oligosaccharide side chains terminate in epitopes that mimic sugar moieties of mammalian glycosphingolipids (100, 146, 147, 148, 269, 251). This form of molecular mimicry not only provides the bacterium with a method of immune avoidance but also allows the bacterium to use host-derived molecules that normally associate with the mimicked structure.
Some LOS structures can serve as acceptor molecules for sialic acid deposition. LOS sialylation is mediated by gonococcus-encoded sialyltransferase (147, 150) that is present in the gonococcal outer membrane (218). The gonococcus lacks the ability to synthesize CMP-N-acetylneuraminic acid and must parasitize this substrate from its human host (6, 74, 185, 225). The presence of sialic acid on gonococcal LOS confers unstable resistance to the bactericidal action of normal human serum, i.e., serum resistance (178, 184, 185, 186, 225); however, it also impairs Opa-mediated entry into some cell lines (249). This has led to the suggestion that LOS antigenic phase variation may allow the gonococcus to fluctuate between invasive and serum-resistant phenotypes and thus promote bacterial survival in vivo (249). This idea is supported by the work of Shafer and colleagues, who have recently provided evidence that phase variation, resulting in elongated LOS structures, also increases the serum sensitivity of gonococci bearing these structures (216). Additionally, although it has not been examined for the gonococcus, recent studies performed with Neisseria meningitidis have demonstrated that the oligosaccharide determinant of LOS may also influence the defensin-enhanced mucosal adherence observed with these bacteria (83).
Porin, the water-filled channel through which small molecules traverse the gonococcal outer membrane, is thought to play multiple roles in potentiating disease caused by N. gonorrhoeae. Porin molecules trigger variable functional responses within host cells depending upon the particular porin and the host cell type under study. A unique feature ascribed to gonococcal porin is its ability to translocate into eukaryotic cell membranes (23, 24, 143, 259), where it forms a voltage-gated channel that is modulated by host cell ATP and GTP (206). Porin translocation is thought to require the intimate juxtaposition of the gonococcus with its target cell membrane; consequently, translocation occurs at discrete sites on the host cell surface (24, 206, 259). It has also been demonstrated that N. gonorrhoeae infection of HeLa carcinoma cells results in selective porin transport to the mitochondria (175). Within the HeLa cell mitochondrial membrane, porin initiates apoptosis by inducing a calcium influx and, consequently, calpain and caspase activity within these cells (176). Recent data suggest that the ability of porin to induce apoptosis in epithelial cells may play a role in the cytotoxicity observed in fallopian tube organ culture (FTOC) and in the shedding of epithelial cells (56) which occurs in vivo during mucosal infection. In contrast to the porin-induced apoptosis observed in HeLa cells, gonococcal infection of primary human male urethral epithelial cells results in antiapoptotic events (18). Antiapoptotic events were not observed in parallel studies using Chang epithelial cells (18). A central role for porin in inhibiting apoptosis in primary male urethral epithelial cells has recently been demonstrated (17). It is hypothesized that the enhanced survival of the urethral epithelial cell may allow the bacterium to proliferate within an intracellular, protective environment and, consequently, promote gonococcal colonization (18). In Chang cells, porin mediates Opa-HSPG- and Opa-independent invasion that occurs in the absence of phosphate. Furthermore, while porin appears to inhibit polymorphonuclear leukocyte (PMN) actin polymerization in response to chemoattractants (20), Wen et al. have demonstrated that porin acts as an actin-nucleating protein in epithelial cells (261). In this respect porin may facilitate the cytoskeletal rearrangements required for actin-mediated entry of the gonococcus into its target host cell. Porin treatment of PMNs also inhibits phagosome maturation (56, 173), and it down regulates immunologically important, opsonin-dependent cell surface receptors, e.g., immunoglobulin G, Fcγ receptors II and III, complement receptor 1, and complement receptor 3 (CR3) (20). Phagocytosis of gonococci is not impaired by porin treatment of PMNs (142).
THE GONOCOCCUS AND OXIDATIVE VERSUS NONOXIDATIVE KILLING RESPONSES
PMN activation results in an oxidative burst within these cells (reviewed in references 94 and 164), which is dependent upon NADPH oxidase assembly at the phagosome membrane and on the reduction of molecular oxygen to superoxide anion (O2−). O2− is converted to hydrogen peroxide (H2O2), which serves as the substrate for a more sustained PMN oxidative response and which includes myeloperoxidase (MPO)-dependent generation of hypohalous acids, potent cytotoxic oxidants, including hypochlorous acid (HOCl). It is generally thought that HOCl and other reactive oxidants associated with MPO activity serve as the primary antimicrobial agents of the bacterial phagolysosome. The ability of porin to modify cellular responses generated with PMN engagement and activation, therefore, has significant consequences to disease progression.
Gonococcal porin increases formyl-methionine-leucine-phenylalanine-mediated hydrogen peroxide production in PMNs upon engagement with opsonized bacteria (20, 92). Similarly, an approximate 6.9-fold increase in lucigenin-enhanced chemiluminescence and a 3.8-fold increase in luminol-enhanced chemiluminescence, which are indicative of NADPH oxidase- and MPO-associated responses, respectively, are observed for porin treated, formyl-methionine-leucine-phenylalanine-stimulated PMNs (142). However, in the presence of viable gonococci or cytochalasin B, which prevents phagolysosome formation, the porin-induced MPO-associated response is significantly decreased (142). This suggests that porin may play a role in preventing the release of reactive oxygen species from PMNs to the extracellular milieu (142), which was observed by Naids and Rest (177) and which is consistent with the degranulation inhibition attributed to the action of porin (21, 93, 142).
Gonococci possess multiple gene products that aid in their survival under conditions of oxidative stress, and it is generally believed that production of O2− and H2O2 is largely ineffective in eradicating infecting gonococci (2, 9, 75, 200, 202, 214, 246, 272). In vitro studies and the culturing of isolated patient exudates, indicating that at least some gonococci associated with PMNs survive, support this idea (38, 39, 202, 217). Similarly, the demonstration that porin can modify MPO-associated oxidative responses (20, 142, 177) suggests that oxygen-independent antimicrobial defenses may play a critical role in controlling gonococcal disease. This is not surprising given that the primary niche for gonococci is the mucosal epithelia of a human host and that antimicrobial peptides are produced locally by the mucosa epithelia, where they serve as a primary defense mechanism guarding against infectious agents (14, 71, 77, 262). It is known that PMN granule extracts (37, 199) and PMNs isolated from patients with chronic granulomatous disease (200), and therefore lack a functional NADPH oxidase, efficiently kill gonococci. These data further support a role for nonoxidative killing in antigonococcal defenses. One hallmark of symptomatic gonococcal disease is the presence of large numbers of PMNs at the site of infection, indicating that at some sites and under some circumstances gonococci may reside in a hypoxic environment. Gonococci have been demonstrated to survive the cytotoxic activity of both anaerobically and aerobically cultured PMNs, but individual gonococci differ in their ability to survive oxidative or nonoxidative killing mechanisms depending upon the conditions under which they were cultured (2, 7, 38, 199, 202, 217). In vivo, both oxidative and nonoxidative mechanisms probably play a role in gonococcus eradication, and the efficacy of either type of defense system may be dependent upon the sight of infection, the phenotypic characteristics of the infecting organism, and the individual mounting the response.
EMBRYOLOGICAL ORIGINS OF THE MALE AND FEMALE GENITAL EPITHELIA
In terms of evolutionary development, the female urogenital systems of apes and humans undergo further differentiation than their male counterparts (129). (See references 129, 207, and 169 for reviews of the embryological origins of the male and female genital tracts.) In humans, the nephrogenic mesoderm differentiates to form the mesonephros and the metanephros; the metanephros gives rise to the renal glomerulus, while the mesonephros regresses. Remnants of the mesonephric tubules exist in males as the vas deferens and in females as blind tubules in the ovarian dorsal mesentery. A complete division of the cloaca gives rise to the rectum and a urogenital sinus in both the male and the female. The caudal-most portion of the urogenital sinus becomes the membranous and penile portions of the urethra in the male and a portion of the vestibule in the female. In males the Muellerian ducts regress, and the urogenital sinus receives the mesonephric ducts, after which the rectum elongates and differentiation occurs. In females, the Muellerian, or paramesonephric, ducts differentiate to form that portion of the genital tract ranging from the fallopian tubes to the cephalic vagina. An additional partitioning event of the urogenital sinus occurs to form the terminal vagina, the rectum, and the urethra. The different embryological origins of the male and female (uro)genital tracts have endowed these epithelial surfaces with different cell surface molecules capable of serving as receptors and coreceptors for invasive microorganisms, including the gonococcus. As we shall see, it is not surprising that N. gonorrhoeae has evolved variable pathogenic mechanisms to ensure its survival in the distinctly different microenvironments found within the male and female (uro)genital tracts.
GONOCOCCAL INFECTION OF THE MALE URETHRA
N. gonorrhoeae infection of men most commonly occurs as an acute urethritis, which develops from the concomitant inflammatory response directed at infecting gonococci (197). However, a small percentage of men will develop asymptomatic gonococcal urethritis (95, 109, 229). One hallmark of symptomatic gonococcal disease in men is the presence of a purulent discharge, which is associated with PMN influx and shedding of urethral epithelial cells. Human volunteer studies indicate that there is an incubation period from the time of infection to the onset of clinical symptoms of disease (209). During this time gonococci are quiescent and cannot be cultured from the urethra for up to 40 h after the initiation of infection, after which a purulent exudative process begins. These data suggest that gonococci enter a protective environment early in disease where they survive and replicate. We would propose that, in men, the urethral epithelial cell is this sanctuary. In vitro infection assays and microscopic analyses of patient exudates indicate that gonococci are released from epithelial cells and that infected epithelial cells are subsequently shed from the mucosal surface to the urethral lumen. Experimental infection of men also demonstrates that the chemokine interleukin-8 (IL-8) and the cytokines IL-6 and tumor necrosis factor alpha (TNF-α) are prevalent within the urethral lumen with progressive gonococcal disease (197). Recent evidence reveals that LOS elicits TNF-α, IL-1β, IL-6, and IL-8 secretion from primary urethral epithelial cells (99). Release of cytokines and chemokines from the urethral epithelium may, therefore, potentially initiate the inflammatory response associated with gonococcal urethritis by triggering PMN influx (Fig. 1). PMN influx in conjunction with cytokine release from the urethral epithelium subsequently might potentiate the clinical symptoms associated with disease. Unless it is intercepted by effective antimicrobial therapy, this process is cyclic during the course of infection, with extension into the upper male genital tract. The human acquired immune response is ineffective in slowing disease progression or preventing reinfection. This is exemplified in the diaries of Boswell, which attest to his numerous separate instances of gonococcal infection, which persisted for months without therapy (182).
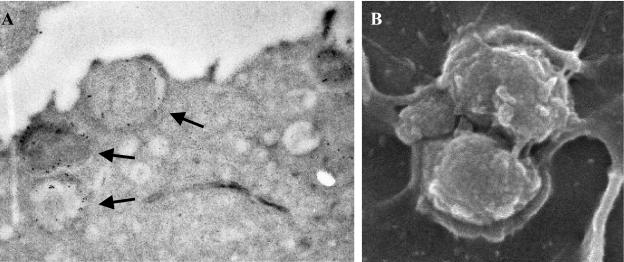
Microscopic examination of urethral exudates from men documented to have culture-proven gonorrhea indicates that gonococci are found within PMNs and urethral epithelial cells (Fig. 2). The interaction of gonococci with PMNs is dependent upon the presence of Opa, but it does not require pili (200, 217). Experimental infection of men with Opa− gonococci results in a shift to an Opa+ phenotype (209). An Opa+ phenotype is also prevalent in clinical isolates obtained from men with naturally acquired gonococcal infection (172). Primary male urethral epithelial cells do not express CEACAM (our unpublished data), and experimental challenge of men with an N. gonorrhoeae strain FA1090ΔOpa mutant results in an infection indistinguishable from that observed with the wild-type parental strain (N. Fulcher, M. Binnicker, M. A. Apicella, and J. G. Cannon, unpublished data). This suggests that the role of Opa proteins in promoting gonococcal urethritis in men resides in their ability to facilitate a gonococcus-PMN interaction. A single, primary receptor that uniquely modulates the interaction of the gonococcus with PMNs has not been identified; however, this association occurs independently of CR3 (70). Fcγ, CEACAM, HSPG, and integrin receptors present on the PMN cell surface may potentially all play a role in gonococcal adherence and/or internalization. It is also possible that one particular receptor mediates the PMN-gonococcus association under one set of environmental conditions (e.g., within the urethral lumen), whereas another receptor may mediate this association within a different microenvironment (e.g., within circulation).
FIG. 2.
Interaction of the gonococcus with male urethral epithelia. (A) Transmission electron micrograph of a urethral epithelial cell within a urethral exudate obtained from a male with naturally acquired gonococcal urethritis. Gonococci are indicated by arrows. (B) Scanning electron micrograph of primary male urethral epithelial cells after a 2-h infection. Notice the intimate association that occurs between the gonococcal and the host cell membranes in both panels. Magnifications, ×23,000 (A) and×40,000 (B).
CEACAMs can serve as coreceptors for other cell surface receptors (e.g., integrins) present on professional phagocytic cells. Engagement of CEACAM sends a priming signal within PMNs that activates adhesion receptors without triggering a respiratory burst or the release of inflammatory mediators (236). Therefore, an Opa-CEACAM interaction could potentially enhance gonococcal survival within these cells. Opa proteins also promote intracellular survival by sequestering pyruvate kinase as a means to acquire pyruvate (263), which is required for gonococcal viability. A role for Opa proteins in promoting gonococcal survival is supported by the work of Jerse, who demonstrated that the intravaginal inoculation of female mice with gonococci of an Opa− phenotype results in their conversion to an Opa+ phenotype (116). CEACAMs are human-specific molecules and as such are not expressed by mice. This perhaps indicates that the observed selection for gonococci of an Opa+ phenotype occurs independently of their ability to bind CEACAMs but rather might reside in their ability to sequester pyruvate. Schmitter et al. recently presented evidence suggesting that an Opa-CEACAM interaction may actually deter gonococcal colonization by stimulating bactericidal events within granulocytes upon CEACAM3 (CD66d) engagement (208). It is currently not know if this interaction with CEACAM3 is mediated by a particular subset of those Opa proteins demonstrated to bind CEACAM receptors (45) or if all CEACAM-binding Opa proteins are equally efficient in their ability to serve as ligands for CEACAM3 and to trigger oxidative responses by granulocytes.
Studies performed by using the human challenge model of gonococcal disease have demonstrated that the ability of gonococci to acquire iron (e.g., in the form of lactoferrin or transferrin) from its sole human host is required for successful colonization of, at least, the male urethra (3, 50). The initial site of gonococcal colonization in men is the urethral epithelial cell (Fig. 1). Disease is thought to occur as a sequential process in which an initial interaction between the gonococcal pilus and the urethral epithelium occurs. Although CD46 has been shown to bind gonococcal pilus (126), more recent data indicate that the presence of CD46 in several cell lines is inversely related to the association of gonococci with these same cells (244). The receptor for gonococcal pilus has not been examined by using primary urethral epithelial cells, nor has a pilus-CD46 interaction been shown in male exudates; consequently, it is not clear whether CD46 serves as the pilus receptor within the male urethra. Pilus expression, however, is required for successful infection of the urethral epithelium.
Analysis of primary male urethral epithelial cells demonstrates that the observed intimate association between the urethral epithelium and the gonococcus (Fig. 2) is probably achieved through the interaction of the asialoglycoprotein receptor (ASGP-R) and gonococcal LOS (96), a major constituent of the gonococcus cell membrane. In primary cell culture, engagement of the ASGP-R by the gonococcus results in pedestal formation beneath the bacterium (97). Pedestal formation beneath the bacterium is also observed with microscopic analysis of exudates collected from men with naturally acquired gonococcal urethritis (5, 97). Evidence suggests that endocytosis ensues primarily because of actin-dependent (80) and clathrin-dependent (97) processes. Endocytosis mediated by the ASGP-R results in endosomal fusion and acidification, which results in clathrin coat disassembly and uncoupling of the ASGP-R-ligand complex (235, 260). It is not known whether similar events occur with gonococcal internalization within urethral epithelial cells. Following gonococcal internalization, it is suggested that ASGP-R is recycled to the urethral cell surface, where it is available to bind more gonococci (96). Small proportions of infecting gonococci are also observed to enter primary urethral epithelial cells by a macropinocytic mechanism, although membrane ruffling is not observed (271). The intracellular fate of the gonococcus within the urethral epithelium is currently unclear.
Adherence of the gonococcus to the ASGP-R is dependent upon the presence of a terminal lacto-N-neotetraose (LNnT) moiety on LOS (96). This moiety mimics human paragloboside and provides one means by which the gonococcus escapes immune recognition. Additionally, the LNnT epitope can serve as a sialic acid acceptor. The importance of the LNnT moiety to gonococcal pathogenesis in men can be inferred from human experimental infection studies and from clinical data obtained from men with naturally acquired gonorrhea, which demonstrate that LNnT is selected for in vivo (33, 118, 210). One study demonstrates that gonococci bearing the LNnT moiety on their LOS exhibit enhanced infectivity in humans (210). It is thought that serum resistance conferred by LOS sialylation allows a greater proportion of gonococci to survive the harsh microenvironment of the urethral lumen during disease (184, 185, 225). Consequently, a lower infectious dose is required to establish disease because a greater proportion of the infection inoculum survive and proliferate.
Sialylation of gonococci occurs within the male urogenital tract (6, 149, 210). Sialylation of the LNnT epitope, in vitro, impairs the ability of gonococci to invade primary urethral epithelial cells (96) and epithelial cell lines (249, 251) and to be phagocytosed by neutrophils (131, 201). These data are supported by one study in which, in vivo, sialylation of gonococci also impaired the ability of these organisms to cause disease in human volunteers (212). Gonococcal infectivity is restored with sialic acid removal by neuraminidase or, presumably, by the replication of gonococci within the lumen of the urethra in the absence of host-derived CMP-N-acetylneuraminic acid. Neuraminidase (158, 232) and the ASGP-R (98) are present on human sperm. Neuraminidase is also present on the surface of professional phagocytic cells (51), which are, generally, abundant in the urethral lumen under conditions favoring progressive gonococcal disease. Sialylated gonococci in proximity to any of these cells might then be expected to become desialylated through exogenous neuraminidase activity. It can be speculated that subsequent gonococcal adherence to the ASGP-R on sperm (98) would then, in turn, facilitate disease transmission.
INFECTION OF THE LOWER FEMALE GENITAL TRACT
The majority of gonococci transmitted from men to their partners have sialylated LOS. However, the presence or the absence of sialic acid on LOS does not influence the interaction of the gonococcus with primary cervical epithelial cells (63). It is interesting to speculate that within the lower female genital tract sialylated gonococci may become modified to enhance disease transmission to men. That is, neuraminidases produced by the vaginal microflora can potentially remove sialic acid from sialylated gonococci. Cervical epithelia also produce neuraminidase; however, the specificity of this enzyme to cleave endogenous or exogenous substrates exhibits cyclic variability (187). The level of sialic acid found within the microenvironment of the cervix also exhibits cyclic variation (187).
In contrast to the inflammatory response generated predominately with gonococcal infection of the male urethra, 50 to 80% of women with lower genital tract N. gonorrhoeae infection are asymptomatic (58, 59, 109, 229), and 70 to 90% of women with disseminated infection lack signs of genital tract involvement (58, 95, 109). Analysis of cervical secretions obtained from normal (i.e., uninfected) women and from women infected with the gonococcus also reveal that an antibody response is not generated with uncomplicated infection (105). These clinical findings are consistent with the ability of the gonococcus to evade and subvert host immune function. Further support for this idea is found in the work of Hedges et al., who found that women with gonococcal cervicitis did not exhibit elevated local levels of IL-1, IL-6, and IL-8 (105). We have obtained similar results with multiplex reverse transcription-PCR analysis of RNA collected from infected and uninfected primary cervical cells and with enzyme-linked immunosorbent assay analysis of supernatants collected from primary human ecto- and endocervical infection studies performed with N. gonorrhoeae (our unpublished data). In contrast, Fichorova et al. have reported increased IL-1, IL-6, and IL-8 expression in similar studies performed with immortalized vaginal and cervical epithelia (72), which we have demonstrated to have lost CR3 expression (64). The release of inflammatory cytokines by the cervical epithelium in response to N. gonorrhoeae infection therefore remains under question.
Within the lower female genital tract, the cervical epithelia provide a source of alternative pathway complement activity, albeit at a level comparable to only approximately 10% of that observed for human serum (191, 247). Within minutes of infection of primary cervical epithelial cells, complement protein C3b is deposited on the lipid A portion of gonococcal LOS (63) and is rapidly inactivated to iC3b (64) (Fig. 1). These data are supported by the predominance of iC3b (in comparison to C3b) on the surface of clinically isolated gonococci (114, 157, 254). The affinity of complement factor H (fH) for sialylated LOS (196) and for porin of a PI.A isotype (195) may augment C3b inactivation. However, in primary cervical cell culture, C3b inactivation occurs in a kinetically similar manner on gonococci of either a PI.A or a PI.B isotype and on sialylated gonococci or on gonococci that are not sialylated (65). fH activity is increased with decreasing polysaccharide chain length (136). Thus, C3b inactivation could be augmented by the presence of an LOS within the gonococcal outer membrane, as opposed to the LPS prevalent among gram-negative bacteria. The resemblance of gonococcal LOS to human paraglobosides and glycosphingolipids, some of which serve as precursors for cervical mucus synthesis and which, consequently, may not be recognized as a complement-activating surface within the microenvironment of the cervix (146, 147, 148, 170), may also augment C3b inactivation. In addition to the factor I (fI) cofactor activity of fH, CD46 can function as a cofactor for fI. However, infection studies performed with primary cervical epithelial cell cultures suggest that CD46 is not required for C3b inactivation on gonococci at the level of the uterine cervix (65).
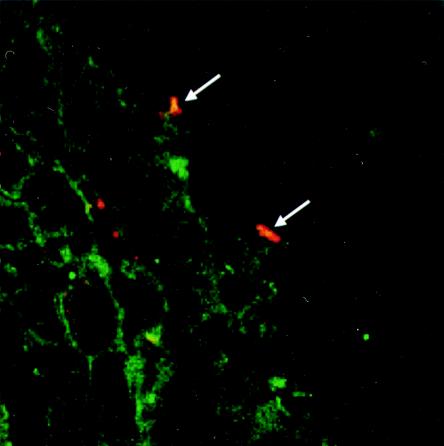
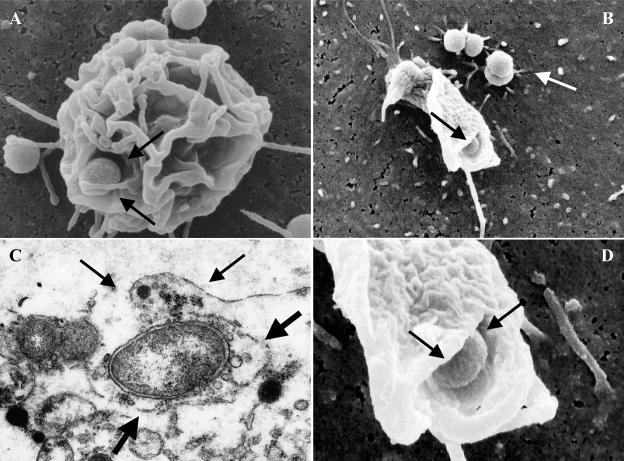
Analysis of clinical biopsies obtained from women with culture-documented gonococcal cervicitis and infection studies performed with primary human cervical epithelial cells indicate that CR3 serves as the primary receptor for N. gonorrhoeae adherence to and invasion of the ectocervix and endocervix (Fig. 1 and 3) (64). Binding of gonococcal pilus to the I domain of CR3 (65) probably allows the gonococcus to overcome the electrostatic repulsion between its own cell surface and that of the cervical cell and may juxtapose the gonococcus at the cervical cell surface, where complement concentrations would be expected to allow efficient opsonization for the subsequent intimate adherence of iC3b and gonococcal porin to the I-domain. Binding of the gonococcus to CR3 requires the cooperative action of iC3b bound to the gonococcal surface in conjunction with gonococcal porin and pilus (65). Opa proteins do not appear to be required for adherence to or invasion of primary cervical epithelial cells (65, 240). Engagement of CR3 on primary cervical epithelial cells results in vinculin- and ezrin-enriched focal complex formation before membrane ruffle formation (67). A signal transduction cascade that is dependent upon the activation of wortmannin-sensitive kinases (i.e., phosphatidylinositol 3-kinase or mitogen-activated protein kinases) (67) and Rho GTPases (64) initiates ruffling (Fig. 4). Gonococci are then internalized within macropinosomes (67).
FIG. 3.
Gonococci colocalize with CR3 in vivo. Clinical biopsies were obtained from women with culture-documented gonococcal cervicitis and immunoprocessed for confocal microscopy. CR3 present on the cervical cell surface is visible as green fluorescence, and gonococci are visible as red fluorescence. Colocalization of the gonococcus with CR3 occurs as yellow fluorescence because of the combined signal of the two fluorophores. Areas of colocalization are indicated by arrows. Magnification, ×40.
FIG. 4.
Scanning and transmission electron microscopy demonstrates that membrane ruffling occurs upon gonococcal cervical infection in vitro and in vivo. Membrane ruffling is observed after a 90-min infection of primary endocervical cells (A) and after a 2-h infection of primary ectocervical cells (B and D). A large membrane protrusion (small arrows) surrounds a gonococcus in a clinical biopsy obtained from a woman with culture-documented gonococcal cervicitis and is indicative of membrane ruffling (C). Additionally, this bacterium is found residing within a large spacious structure (large arrows), which is also suggestive of membrane ruffling (C). Panel D shows a high magnification of the gonococcus wrapped in the membrane ruffle shown in panel B. Gonococci are indicated by arrows in panels A, B, and D. Magnifications, ×11,000 (A), ×13,000 (B), ×40,000 (C), and ×45,000 (D).
Upon infection of primary cervical epithelial cells, gonococci release a phospholipase D homolog that gains access to the cervical intracellular environment nonspecifically through macropinocytosis of gonococci (66). Gonococcal phospholipase D (NgPLD) appears to promote infection of primary cervical epithelial cells in several ways. Recent data indicate that this secreted gonococcal protein augments signaling events that trigger CR3 mobilization to the surface of primary cervical cells (66). This would ensure gonococcal receptor availability and, consequently, efficient targeting to and association with the cervical cell surface. NgPLD also modulates cervical cell signal transduction events leading to membrane ruffling. Mutant gonococci that lack functional NgPLD activity do not elicit membrane ruffling, and they are impaired in their ability to associate with and to invade primary human cervical cells (66). The specific mechanism(s) (e.g., alternate trafficking and/or inactivation of reactive oxygen species or other antimicrobial agents) by which NgPLD confers protection to the gonococcus within the intracellular cervical microenvironment remains to be determined.
As with invasion of male urethral epithelial cells, the intracellular fate of gonococci within the cervical epithelium is unclear. Ligand binding to the I-domain of CR3 does not invoke a proinflammatory response in professional phagocytic cells (16, 36, 174, 265, 266, 267, 268). Consequently, although this is speculative, the ability of gonococci to subvert cervical cell signal transduction cascades and the complement system in such a manner to allow a cooperative mechanism of CR3-mediated adherence to and invasion of the cervical epithelium may also enhance its survival within the lower female genital tract. Gonococcal invasion in the absence of a respiratory burst would be expected to increase the number of gonococci that survive intracellularly, while inactivation of the complement system would enhance gonococcal survival extracellularly. Consequently, subversion of host cell signal transduction and the complement system by the gonococcus within the lower female genital tract may potentially allow this bacterium to attain a carrier-like state. Ascending infection of the uterus and fallopian tubes may occur as a consequence of hormonal changes that alter the mucosal epithelia, molecules available for gonococcal use, and/or virulence factors expressed by the gonococcus (for a review, see reference 26). In this regard, it of interest that menses is associated with an increased risk to women for PID and for disseminated infection (242). C3 production by the cervical epithelium exhibits cyclic variability, and the highest levels of C3 are detected during menses (101, 183). Additionally, a correlation can be made between the presence or the absence of Opa and the site of gonococcal isolation (i.e., infection). Transparent, or Opa−, gonococci are predominate within the fallopian tubes and in the cervix at the time of menses (172). Conversely, Opa+ gonococci are found predominately within the male urethra and within the cervix at the time of ovulation (172). The ability of gonococci to use heme, hemoglobin, and haptoglobin-hemoglobin is also postulated to be responsible for the increased risk observed for women to develop PID and disseminated disease during menses (31, 241). Analyses of gonococci clinically isolated from women support this idea in that there may be a correlation between the expression of the hemoglobin receptor by gonococci and the onset of the menses cycle (4). Similar results are obtained in the female mouse model of genital tract infection in that the presence of hemoglobin selects for gonococci expressing the hemoglobin receptor (117).
INFECTION OF THE UPPER FEMALE GENITAL TRACT
Approximately 45%percent of women with gonococcal cervicitis will develop an ascending infection (26, 134), the prerequisite to PID. Ascent to the upper female genital tract might be facilitated through the ability of gonococci to exhibit twitching motility, in conjunction with hormonal changes which influence the expression of complement and molecules serving as gonococcal receptors within the female genital tract. Microscopic analysis of tissue biopsies indicates that the expression of CR3 progressively decreases in an ascending manner from the ectocervix to the fallopian tubes (64). Conversely, expression of the lutropin receptor (LHr) increases in an ascending manner from the endometrium to the fallopian tubes, and expression is up regulated at the time of menses (26, 101, 198). It is speculated that the LHr serves as a receptor for gonococcal invasion of endometrial and fallopian tube epithelia (43, 82, 230). The interaction of the gonococcus with the LHr increases the invasive character of the gonococcus for Hec1B adenocarcinoma endometrial cells and, therefore, is said to occur in a contact-inducible manner (43, 82, 230). Human chorionic gonadotropin (hCG), a natural ligand for LHr, can competitively inhibit the association of gonococci with FTOC and Hec1B cells, presumably by interfering with an LHr-gonococcus interaction (82, 230). These data suggest that gonococci possess a surface molecule that mimics hCG. Recently, Spence et al. reported that this hCG-like molecule is the ribosomal protein L12 (231). The LHr is also present on the human uterus, placenta, decidua, and fetal membranes (198). Although this is speculative, a gonococcus-LHr interaction occurring on decidua and placental membranes could potentially result in severe complications of disease and may, in part, contribute to the increased risk of spontaneous abortion associated with N. gonorrhoeae infection.
Gonococcal adherence to fallopian tube epithelia occurs selectively on nonciliated cells (82, 154, 156); however, it is the ciliated cells of the fallopian tube epithelia that are subsequently shed (234). If left untreated, complete loss of ciliary action can occur. Cytotoxicity of ciliated cells is attributed to gonococcal peptidoglycan (160) and LOS (49, 88, 89, 159) either directly or indirectly through the induction of increased local production of the inflammatory cytokine TNF-α (153). It is presumed that the loss of the ciliated cells within the fallopian tube provides the gonococcus access to subepithelial tissues. Access to subepithelial tissue is also speculated to be obtained with invasion of nonciliated cells, after which gonococci are transcytosed to the basal lateral surface of these cells and released (156). In Hec1B cells, the gonococcal protein L12 mediates transcytosis to the basal lateral surface (231); however, this has yet to be demonstrated in FTOC. Sialylation of intracellular gonococci (before their exocytosis) might potentially prime these organisms for disseminated infection by the increased serum resistance observed with sialylation. It is also postulated that while gonococci appear to initiate upper genital tract infections, gonococcal colonization is short-lived with increasing anoxic environmental conditions associated with inflammation and the introduction of secondary, invasive, microorganisms (47, 52, 167, 168). It is additionally suggested that with extended infections, gonococci may actually reside within the uterine cul-de-sac of the peritoneal cavity (47, 168).
COMPLEMENT-GONOCOCCUS INTERACTION WITHIN HUMAN SERUM
Within normal human serum, the interaction of the gonococcus with complement is governed by factors that are distinctly different from those observed at the level of the cervical epithelium; most notable is the presence of classical pathway (CP) complement components. Several studies have indicated that the CP serves as the primary mechanism of complement-mediated killing of gonococci. The ability of gonococci of a particular isotype to inactivate the CP, therefore, confers a considerable survival advantage to these bacteria and increases their ability to cause disease.
Disseminated gonococcal infection is associated predominately with gonococci that express PI.A (34, 171). Porin molecules of the PI.A, but not the PI.B, isotype bind fH at a site distinct from that observed for sialylated LOS (195). Binding of fH favors alternative pathway complement inactivation and increases the serum resistance observed for PI.A-expressing gonococci. Within the CP, C4-binding protein (C4bp) functions in a manner analogous to that of fH by serving as a cofactor for fI-mediated inactivation of C4b. Another mechanism gonococci have adapted to increase their survival within human serum is the ability of gonococci of a PI.B isotype to bind C4bp (194). Binding of C4bp is specific for gonococci that are not sialylated. Deposition of C4b occurs on the phosphoethanolamine substitution of LOS (193). Porin is intimately associated with LOS within the outer membrane of gonococci. Consequently, the juxtaposition of porin with LOS may facilitate CP inactivation by mediating the interaction of either fH or C4bp with C4b.
Crucial to the bactericidal action of the complement system is the assembly of a functional membrane attack complex (MAC). Studies performed by Joiner and coworkers demonstrate that the serum resistance or sensitivity exhibited by a gonococcus is correlated with how MAC assembly occurs on the bacterium's surface, which they also show to occur in an aberrant manner on the surface of serum-resistant gonococci (122, 123). The need for MAC involvement in controlling neisserial disease is further evidenced by the increased risk for neisserial infections associated with complement deficiencies (58). Individuals deficient in terminal (i.e., MAC) complement proteins C5, C6, C7, C8, and/or C9 commonly exhibit recurrent, often systemic, neisserial infections, indicating the importance of MAC in controlling neisserial colonization and dissemination. In addition to the ability of sialylated LOS to bind fH to mediate increased serum resistance, the presence of sialic acid on LOS decreases C9 deposition upon the gonococcal surface (115). Consequently, a functional MAC is not formed and gonococcus lysis cannot occur. Opa may also play a role in inhibiting MAC assembly on the surface of gonococci. Increased serum resistance is observed among gonococci in the presence of heparin, which binds to Opa (46). Although the mechanism by which serum resistance is conferred has not been elucidated, one possibility is that the binding of heparin to Opa augments the inhibitory effect of vitronectin on MAC assembly.
CONCLUSIONS
The gonococcus is exquisitely adapted to survival within its sole human host. It is uniquely capable of sensing and adapting to a particular host microenvironment. This is evident from the different mechanisms used by this bacterium to invade mucosal surfaces and to survive in the presence of human serum. Based on the contributions of many researchers, we have proposed the following model of gonococcal disease, in which immediately following infection of the male urethra, gonococci cannot be cultured as the result of residence within the male urethral epithelial cell. Colonization of the male urethral epithelium is dependent upon the presence of transferrin or lactoferrin. The interaction of gonococcal LOS with the ASGP-R present on the urethral epithelial cell mediates invasion and results in cytokine production. Cytokine release contributes to the (usually) symptomatic nature of gonococcal disease in men and is accompanied by a large influx of PMNs, which in turn contribute to the observed cytokine release and inflammation. The interaction of gonococci with PMNs is mediated by the interaction of two broad families of proteins, Opa gonococcal proteins and CEACAM host cell proteins. The specific interactions occurring between these two families of proteins may dictate specific host cellular responses and the survival or death of phagocytosed gonococci. The PMN response to gonococci is further modulated by gonococcal porin, which inhibits PMN degranulation and the production and release of toxic oxidants from the host cell to the extracellular milieu. In this respect, porin may promote gonococcus survival, but gonococci possess multiple gene products that promote survival from varied host defense mechanisms. In vitro studies and the ability to cultivate gonococci from patient exudates indicate that at least some gonococci survive the cytotoxic action of PMNs. Gonococci are sialylated upon their LOS molecules while in residence within the PMN and must become desialylated before they are able to invade the urethral epithelial cell. Sialidases are present on human sperm, PMNs, and macrophages, and consequently, they could potentially desialylate proximal gonococci and thus contribute to disease progression. Transmission of gonococci to a sexual partner is aided, in part, by the ability of gonococci to bind to human sperm. Within the lower female genital tract the presence or absence of sialic acid on the gonococcal surface does not appear to influence colonization, although sialidases present within the lower female gental tract may prime the gonococcus for transmission to the male urethra. The interaction of gonococci with the uterine cervix is mediated by the cooperative actions of host and gonococcal constituents. Gonococcal pilus binds to CR3 present on the ectocervix and endocervix, positioning the bacterium at the cervical cell surface where complement is produced and activated. Activation of the alternative complement pathway results in C3b deposition upon gonococci. C3b is inactivated to form iC3b; these processes are probably mediated by the affinity of porin for factor H of the alternative pathway and the proximity of porin to LOS in the gonococcal outer membrane. iC3b and porin form a tight association with CR3 on the cervical cell surface by binding to the I-domain of this receptor. Engagement of CR3 triggers gonococcal internalization within macropinosomes. Secreted gonococcal proteins, which ensure CR3 recruitment to the cervical cell surface, mediate these processes. Ascension to the upper female genital tract is mediated by both host and gonococcal factors that are subject to cyclic environmental changes occurring within the female genital tract. The LHr present on the endometrial and fallopian tube epithelia mediates the interaction of gonococci with the upper female genital tract. The ribosomal protein L12 serves as the gonococcal ligand mediating LHr adherence. The association of the gonococcus with fallopian tube epithelia is limited to the nonciliated cells; however, ciliated cells are lost because of the toxicity associated with LOS and peptidoglycan release. Cytotoxicity is further mediated by a local increase in TNF-α. Nonciliated cells are invaded by the gonococcus, and gonococci are transcytosed to the basal lateral surface where they are released and gain access to the subepithelial tissues. Access to subepithelial spaces provides a gateway by which disseminated gonococcal infection can occur. Within the bloodstream, the interaction of the gonococcus with the complement system becomes critical for bacterial eradication and is thought to be dependent upon classical pathway activity and the presence of efficacious antibody. However, gonococci have adapted multiple mechanisms by which they are able to evade the lytic action of the complement system, including C4b inactivation and the formation of a nonfunctional MAC on their cell surface.
The gonococcus is unique in that it appears to possess a seemingly endless repertoire of pathogenic mechanisms by which it efficiently colonizes discrete microenvironments found within its sole human host. This review has attempted to incorporate some of our current knowledge into a working model of how disease and disease transmission might occur in vivo, and in doing so we have attempted to highlight the differences in gonococcal pathogenesis observed between infection in males and infection in females. Whereas an intimate association occurs between the gonococcus and the male urethral epithelium, i.e., a zipper mechanism of invasion, the association of gonococci with epithelia of the lower female genital tract occurs as a trigger mechanism of invasion, with gonococci residing in spacious macropinosomes. Infection of the male urethra and infection of the upper female genital tract are usually associated with an inflammatory response. In contrast, a significant proportion of women with lower genital tract infections exhibit asymptomatic or subclinical disease. The intracellular fate of the gonococcus within any given cell type is currently unclear. It will therefore be of interest to determine whether the signal transduction cascades triggered with host cell engagement and the intracellular fate of this bacterium are as varied as are the portals of entry that it uses to become intracellular. Future studies will undoubtedly further our understanding of this unique human pathogen and the mechanisms it uses to exploit its human host. In view of the increasing prevalence of antibiotic-resistant strains of gonococci, it is hoped that these studies will lead to the development of new effective therapeutic agents for the treatment and prevention of gonorrhea. In light of our current knowledge, it is doubtful that a single agent or vaccine candidate will prove efficacious in all disease settings; however, with continued study it may be possible to develop strategies that would confer protection to a particular subgroup of individuals or prevent colonization of a discrete microenvironment within a human host.
Acknowledgments
We thankfully acknowledge B. Evans, D. Orr, and D. Fortenberry for providing us with the clinical cervical biopsies and P. Rice for male urethral exudates. We are grateful to the Departments of Urology and Obstetrics and Gynecology at the University of Iowa for allowing us to obtain urethral and cervical tissues used to seed the primary cell cultures used in these studies. We also express our gratitude to M. Ketterer, H. Harvey, and J. Shao for their assistance in compiling the manuscript.
The work described in this paper was supported by NIAID grants AI45728 and AI43924.
REFERENCES
- 1.Aderem, A. A., S. D. Wright, S. C. Silverstein, and Z. A. Cohn. 1985. Ligated complement receptors do not activate the arachidonic acid cascade in resident macrophages. J. Exp. Med. 161:617-622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alcorn, T. M., H. Y. Zheng, M. R. Gunther, D. J. Hassett, and M. S. Cohen. 1994. Variation in hydrogen peroxide sensitivity between different strains of Neisseria gonorrhoeae is dependent on factors in addition to catalase activity. Infect. Immun. 62:2138-2140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anderson, J. E., M. M. Hobbs, G. D. Biswas, and P. F. Sparling. 2003. Opposing selective forces for expression of the gonococcal lactoferrin receptor. Mol. Microbiol. 48:1325-1337. [DOI] [PubMed] [Google Scholar]
- 4.Anderson, J. E., P. A. Leone, W. C. Miller, C. Chen, M. M. Hobbs, and P. F. Sparling. 2001. Selection for expression of the gonococcal hemoglobin receptor during menses. J. Infect. Dis. 184:1621-1623. [DOI] [PubMed] [Google Scholar]
- 5.Apicella, M. A., M. Ketterer, F. K. Lee, D. Zhou, P. A. Rice, and M. S. Blake. 1996. The pathogenesis of gonococcal urethritis in men: confocal and immunoelectron microscopic analysis of urethral exudates from men infected with Neisseria gonorrhoeae. J. Infect. Dis. 173:636-646. [DOI] [PubMed] [Google Scholar]
- 6.Apicella, M. A., R. E. Mandrell, M. Shero, M. E. Wilson, J. M. Griffiss, G. F. Brooks, C. Lammel, J. F. Breen, and P. A. Rice. 1990. Modification by sialic acid of Neisseria gonorrhoeae lipooligosaccharide epitope expression in human urethral exudates: an immunoelectron microscopic analysis. J. Infect. Dis. 162:506-512. [DOI] [PubMed] [Google Scholar]
- 7.Apicella, M. A., M. Shero, G. A. Jarvis, J. M. Griffiss, R. E. Mandrell, and H. Schneider. 1987. Phenotypic variation in epitope expression of the Neisseria gonorrhoeae lipooligosaccharide. Infect. Immun. 55:1755-1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aral, S. O., W. D. Mosher, and W. Cates. 1991. Self-reported pelvic inflammatory disease in the United States. JAMA 266:2570-2573. [PubMed] [Google Scholar]
- 9.Archibald, F. S., and M.-N. Duong. 1986. Superoxide dismutase and oxygen toxicity defenses in the genus Neisseria. Infect. Immun. 51:631-641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arko, R. J. 1972. Neisseria gonorrhoeae: experimental infection of laboratory animals. Science 177:200-201. [DOI] [PubMed] [Google Scholar]
- 11.Arko, R. J. 1989. Animal models for pathogenic Neisseria species. Clin. Microbiol. Rev. 2:S56-S59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ayala, B. P., L. Lin, S. Hopper, M. Fukuda, and M. So. 1998. Infection of epithelial cells by pathogenic neisseriae reduces the levels of multiple lysosomal constituents. Infect. Immun. 66:5001-5007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ayala, B. P., B. Vasquez, S. Clary, J. A. Tainer, K. Rodland, and M. So. 2001. The pilus-induced Ca2+ flux triggers lysosome exocytosis and increases the amount of Lamp1 accessible to Neisseria IgA1 protease. Cell. Microbiol. 3:265-275. [DOI] [PubMed] [Google Scholar]
- 14.Bals, R. 2000. Epithelial antimicrobial peptides in host defense against infection. Respir. Res. 1:141-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beagley, K. W., and C. M. Gockel. 2003. Regulation of innate and adaptive immunity by the female sex hormones oestradiol and progesterone. FEMS Immunol. Med. Microbiol. 38:13-22. [DOI] [PubMed] [Google Scholar]
- 16.Berton, G., C. Laudanna, C. Sorio, and F. Rossi. 1992. Generation of signals activating neutrophil functions by leukocyte integrins: LFA-1 and gp150/95, but not CR3, are able to stimulate the respiratory burst of human neutrophils. J. Cell Biol. 116:1007-1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Binnicker, M. J., R. D. Williams, and M. A. Apicella. Infect. Immun., in press. [DOI] [PMC free article] [PubMed]
- 18.Binnicker, M. J., R. D. Williams, and M. A. Apicella. 2003. Infection of human urethral epithelium with Neisseria gonorrhoeae elicits an upregulation of host anti-apoptotic factors and protects cells from staurosporine-induced apoptosis. Cell. Microbiol. 5:549-560. [DOI] [PubMed] [Google Scholar]
- 19.Birley, H., B. I. Duerden, and C. A. Hart. 2002. Sexually transmitted diseases: microbiology and management. J. Med. Microbiol. 51:793-807. [DOI] [PubMed] [Google Scholar]
- 20.Bjerknes, R., H.-K. Guttormsen, C. O. Solberg, and L. M. Wetzler. 1995. Neisserial porins inhibit human neutrophil actin polymerization, degranulation, opsonin receptor expression, and phagocytosis but prime the neutrophils to increase their oxidative burst. Infect. Immun. 63:160-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Blake, M. S. 1985. Implications of the active role of gonococcal porins in disease, p. 251-258 In G. K. Schoolnik (ed.), The pathogenic neisseriae: proceedings of the Fourth International Symposium. American Society for Microbiology, Washington D.C.
- 22.Blake, M. S., C. M. Blake, M. A. Apicella, and R. E. Mandrell. 1995. Gonococcal opacity: lectin-like interactions between Opa proteins and lipooligosaccharide. Infect. Immun. 63:1434-1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Blake, M. S., and E. C. Gotschlich. 1981. Purification and partial characterization of the major outer membrane protein of Neisseria gonorrhoeae. Infect. Immun. 36:277-303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blake, M. S., and E. C. Gotschlich. 1987. Functional and immunological properties pathogenic Neisseria surface proteins, p. 377-400. In M. Inouye (ed.), Bacterial outer membranes as model systems. John Wiley and Sons, New York, N.Y.
- 25.Blake, M. S., L. M. Wetzler, E. C. Gotschlich, and P. A. Rice. 1989. Protein III: structure, function, and genetics. Clin. Microbiol. Rev. 2:S60-S63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bolan, G., A. A. Ehrhardt, and J. N. Wasserheit. 1999. Gender perspectives and STDs, p. 117-127. In K. K.Holmes, P.-A. Mardh, P. F. Sparling, S. M. Lemon, W. E. Stamm, P. Piot, and J. N. Wasserheit (ed.), Sexually transmitted diseases, 3rd ed. McGraw-Hill, New York, N.Y.
- 27.Bowden, F. J., S. N. Tabrizi, S. M. Garland, and C. K. Fairley. 2002. Sexually transmitted infections: new diagnostic approaches and treatments. Med. J. Aust. 176:551-557. [DOI] [PubMed] [Google Scholar]
- 28.Brodeur, B. R., W. M. Johnson, K. G. Johnson, and B. B. Diena. 1977. In vitro interaction of Neisseria gonorrhoeae type 1 and type 4 with tissue culture cells. Infect Immun. 15:560-567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brooks, G. F. 1985. Structures and characteristics of the gonococcal cell envelope, p. 9-12. In G. F. Brooks and E. A. Donegan (ed.), Gonococcal infection. Butler and Tanner, Ltd., London, United Kingdom.
- 30.Brooks, G. F. 1985. Pathogenesis and immunology of gonococcal infection, p. 51-82. In G. F. Brooks and E. A. Donegan (ed.), Gonococcal infection. Butler and Tanner, Ltd., London, United Kingdom.
- 31.Brooks, G. F. 1985. Disseminated gonococcal infection, p. 121-131. In G. F. Brooks and E. A. Donegan (ed.), Gonococcal infection. Butler and Tanner, Ltd., London, United Kingdom.
- 32.Burch, C. L., R. J. Danaher, and D. C. Stein. 1997. Antigenic variation in Neisseria gonorrhoeae: production of multiple lipooligosaccharides. J. Bacteriol. 179:982-986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Campagnari, A. A., S. M. Spinola, A. J. Lesse, Y. A. Kwaik, R. E. Mandrell, and M. A. Apicella. 1990. Lipooligosaccharide epitopes shared among gram-negative non-enteric mucosal pathogens. Microb. Pathog. 8:353-362. [DOI] [PubMed] [Google Scholar]
- 34.Cannon, J. G., T. M. Buchanan, and P. F. Sparling. 1983. Confirmation of association of protein I serotype of Neisseria gonorrhoeae with ability to cause disseminated infection. Infect. Immun. 40:816-819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Carney, Jr., F. E., and D. Taylor-Robinson. 1973. Growth and effect of Neisseria gonorrhoeae in organ cultures. Br. J. Vener. Dis. 49:435-440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Caron, E., and A. Hall. 1998. Identification of two distinct mechanisms of phagocytosis controlled by different Rho GTPases. Science 282:1717-1720. [DOI] [PubMed] [Google Scholar]
- 37.Casey, S. G., W. M. Shafer, and J. K. Spitznagel. 1985. Anaerobiosis increases resistance of Neisseria gonorrhoeae to O2-independent antimicrobial proteins from human polymorphonuclear granulocytes. Infect. Immun. 47:401-407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Casey, S. G., W. M. Shafer, and J. K. Spitznagel. 1986. Neisseria gonorrhoeae survive intraleukocytic oxygen-independent antimicrobial capacities of anaerobic and aerobic granulocytes in the presence of pyocin lethal for extracellular gonococci. Infect. Immun. 52:384-389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Casey, S. G., D. R. Veale, and H. Smith. 1979. Demonstration of intracellular growth of gonococci in human phagocytes using spectinomycin to kill extracellular organisms. J. Gen. Microbiol. 113:395-398. [DOI] [PubMed] [Google Scholar]
- 40.CEA/PSG Workshop Group. 1999. Nomenclature announcement: redefined nomenclature for members of the carcinoembryonic antigen family. Exp. Cell Res. 252:243-249. [DOI] [PubMed] [Google Scholar]
- 41.Centers for Disease Control and Prevention. 2001. Summary of notifiable diseases—United States, 2001. Morb. Mortal. Wkly. Rep. 50:1-108. [PubMed] [Google Scholar]
- 42.Chen, A., I. C. Boulton, J. Pongoski, A. Cochrane, and S. D. Gray-Owen. 2003. Induction of HIV-1 long terminal repeat-mediated transcription by Neisseria gonorrhoeae. AIDS 17:625-628. [DOI] [PubMed] [Google Scholar]
- 43.Chen, J. C.-R., P. Bavoil, and V. L. Clark. 1991. Enhancement of the invasive ability of Neisseria gonorrhoeae by contact with HecIB, an adenocarcinoma endometrial cell line. Mol. Microbiol. 5:1531-1538. [DOI] [PubMed] [Google Scholar]
- 44.Chen, T., and E. C. Gotschlich. 1996. CGM1a antigen of neutrophils, a receptor of gonococcal opacity proteins. Proc. Natl. Acad. Sci. USA 93:14851-14856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chen, T., F. Grunert, A. Medina-Marino, and E. C. Gotschlich. 1997. Several carcinoembryonic antigens (CD66) serve as receptors for gonococcal opacity proteins. J. Exp. Med. 185:1557-1564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chen, T. C., J. Swanson, J. Wilson, and R. J. Belland. 1995. Heparin protects Opa+ Neisseria gonorrhoeae from the bactericidal action of normal human serum. Infect. Immun. 63:1790-1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chow, A. W., K. L. Malkasian, J. R. Marshall, and L. B. Guze. 1975. The bacteriology of pelvic inflammatory disease. Am. J. Obstet. Gynecol. 122:876-879. [DOI] [PubMed] [Google Scholar]
- 48.Cohen, M. S., J. G. Cannon, A. E. Jerse, L. M. Charniga, S. F. Isbey, and L. G. Whicker. 1994. Human experimentation with Neisseria gonorrhoeae: rationale, methods, and implications for the biology of infection and vaccine development. J. Infect. Dis. 169:532-537. [DOI] [PubMed] [Google Scholar]
- 49.Cooper, M. D., P. A. McGraw, and M. A. Melly. 1986. Localization of gonococcal lipopolysaccharide and its relationship to toxic damage in human fallopian tube mucosa. Infect. Immun. 51:425-430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cornelissen, C. N., M. Kelley, M. M. Hobbs, J. E. Anderson, J. G. Cannon, M. S. Cohen, and P. F. Sparling. 1998. The transferrin receptor expressed by gonococcal strain FA1090 is required for experimental infection of human male volunteers. Mol. Microbiol. 27:611-616. [DOI] [PubMed] [Google Scholar]
- 51.Cross, A. S., and D. G. Wright. 1991. Mobilization of sialidase from intracellular stores to the surface of human neutrophils and its role in stimulated adhesion responses to these cells. J. Clin. Investig. 88:2067-2076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cunningham, F. G., J. C. Hauth, L. C. Gilstrap, W. N. P. Herbert, and S. S. Kappus. 1978. The bacterial pathogenesis of acute pelvic inflammatory disease. Obstet. Gynecol. 52:161-164. [PubMed] [Google Scholar]
- 53.Danaher, R. J., J. C. Levin, D. Arking, C. L. Burch, R. Sandlin, and D. C. Stein. 1995. Genetic basis of Neisseria gonorrhoeae lipooligosaccharide antigenic variation. J. Bacteriol. 177:7275-7279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Darmon, M., C. Delescluse, A. Semat, B. Bernard, J. Bailly, and M. Prunieras. 1984. A keratin of fetal skin is reexpressed in human keratinocytes transformed by SV40 virus or treated with the tumor promoter TPA. Exp. Cell Res. 154:315-319. [DOI] [PubMed] [Google Scholar]
- 55.Dehio, M., O. G., Gomez-Duaret, C. Dehio, and T. F. Meyer. 1998. Vitronectin-dependent invasion of epithelial cells by Neisseria gonorrhoeae involves αv integrin receptors. FEBS Lett. 424:84-88. [DOI] [PubMed] [Google Scholar]
- 56.Dehio, C., S. D. Gray-Owen, and T. F. Meyer. 2000. Host cell invasion by pathogenic neisseriae, p 61-96. In T. A. Oelschlaeger and J. Hacker (ed.), Subcellular biochemistry, vol. 33. Bacterial invasion into eukaryotic cells. Plenum Publishers, New York, N.Y. [DOI] [PubMed]
- 57.Demarco de Hormaeche, R., H. Jessop, and K. Senior. 1988. Gonococcal variants selected by growth in vivo or in vitro have antigenically different LPS. Microb. Pathog. 4:289-297. [DOI] [PubMed] [Google Scholar]
- 58.Densen, P. 1989. Interaction of complement with Neisseria meningitidis and Neisseria gonorrhoeae. Clin. Microbiol. Rev. 2:S11-S17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Densen, P., L. A. MacKeen, and R. A. Clark. 1982. Dissemination of gonococcal infection is associated with delayed stimulation of complement-dependent neutrophil chemotaxis in vitro. Infect. Immun. 38:563-572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.DiPaolo, J. A., N. C. Popescu, L. Alvarez, and C. D. Woodworth. 1993. Cellular and molecular alterations in human epithelial cells transformed by recombinant human papillomavirus DNA. Crit. Rev. Oncogen. 4:337-360. [PubMed] [Google Scholar]
- 61.Duensing, T. D., and J. P. M. van Putten. 1997. Vitronectin binds to the gonococcal adhesin OpaA through a glycoaminoglycan molecular bridge. Biochem. J. 334:133-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Duensing, T. D., and J. P. M. van Putten. 1997. Vitronectin mediates internalization of Neisseria gonorrhoeae by Chinese hamster ovary cells. Infect. Immun. 65:964-970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Edwards, J. L., and M. A. Apicella. 2002. The role of lipooligosaccharide in Neisseria gonorrhoeae pathogenesis of cervical epithelia: lipid A serves as a C3 acceptor molecule. Cell. Microbiol. 4:585-598. [DOI] [PubMed] [Google Scholar]
- 64.Edwards, J. L., E. J. Brown, K. A. Ault, and M. A. Apicella. 2001. The role of complement receptor 3 (CR3) in Neisseria gonorrhoeae infection of human cervical epithelia. Cell. Microbiol. 3:611-622. [DOI] [PubMed] [Google Scholar]
- 65.Edwards, J. L., E. J. Brown, S. Uk-Nham, J. G. Cannon, M. S. Blake, and M. A. Apicella. 2002. A co-operative interaction between Neisseria gonorrhoeae and complement receptor 3 mediates infection of primary cervical epithelial cells. Cell. Microbiol. 4:571-584. [DOI] [PubMed] [Google Scholar]
- 66.Edwards, J. L., D. D. Entz, and M. A. Apicella. 2003. Gonococcal phospholipase D modulates the expression and function of complement receptor 3 in primary cervical epithelial cells. Infect. Immun. 71:6381-6391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Edwards, J. L., J. Q. Shao, K. A. Ault, and M. A. Apicella. 2000. Neisseria gonorrhoeae elicits membrane ruffling and cytoskeletal rearrangements upon infection of primary human endocervical and ectocervical cells. Infect. Immun. 68:5354-5363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Elkins, C., N. H. Carbonetti, V. A. Varela, D. Stirewait, D. G. Klapper, and P. F. Sparling. 1992. Antibodies to N-terminal peptides of gonococcal porin are bactericidal when gonococcal lipopolysaccharide is not sialylated. Mol. Microbiol. 6:2617-2630. [DOI] [PubMed] [Google Scholar]
- 69.Evans, B. A. 1977. Ultrastructure study of cervical gonorrhea. J. Infect. Dis. 136:248-255. [DOI] [PubMed] [Google Scholar]
- 70.Farrell, C. F., and R. F. Rest. 1990. Up-regulation of human neutrophil receptors for Neisseria gonorrhoeae expressing PII outer membrane proteins. Infect Immun. 58:2777-2784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Fellermann, K., and E. F. Stange. 2001. Defensins—innate immunity at the epithelial frontier. Eur. J. Gastroenterol. Hepatol. 13:771-776. [DOI] [PubMed] [Google Scholar]
- 72.Fichorova, R. N., P. J. Desai, F. C. Gibson III, and C. A. Genco. 2001. Distinct proinflammatory host responses to Neisseria gonorrhoeae infection in immortalized human cervical and vaginal epithelial cells. Infect Immun. 69:5840-5848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Forest, K. T., and J. A. Tainer. 1997. Type-4 pilus-structure: outside to inside and top to bottom. Gene 192:165-169. [DOI] [PubMed] [Google Scholar]
- 74.Frangipane, J. V., and R. F. Rest. 1993. Anaerobic growth and cytidine 5′-monophospho-N-acetylneuraminic acid act synergistically to induce high-level serum resistance in Neisseria gonorrhoeae. Infect. Immun. 61:1657-1666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Fu, K.-S., D. J. Hassett, and M. S. Cohen. 1989. Oxidant stress in Neisseria gonorrhoeae: adaptation and effects on l-(+)-lactate dehydrogenase activity. Infect. Immun. 57:2173-2178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gadzar, A. F., V. Kurvari, A. Virmani, L. Gollahon, M. Sakaguchi, M. Westerfield, D. Kodagoda, V. Stasny, H. T. Cunningham, I. I. Wistuba, G. Tomlinson, V. Tonk, R. Ashfaq, A. M. Leitch, J. D. Minna, and J. W. Shay. 1998. Characterization of paired tumor and non-tumor cell lines established from patients with breast cancer. Int. J. Cancer 78:766-774. [DOI] [PubMed] [Google Scholar]
- 77.Ganz, T. 2003. Defensins: antimicrobial peptides of innate immunity. Nat. Rev. Immunol. 3:710-720. [DOI] [PubMed] [Google Scholar]
- 78.Gerbase, A. C., J. T. Rowley, and T. E. Mertens. 1998. Global epidemiology of sexually transmitted diseases. Lancet 351(Suppl. 3):2-4. [DOI] [PubMed] [Google Scholar]
- 79.Giardina, P. C., M. A. Apicella, B. Gibson, and A. Preston. 1999. Antigenic mimicry in Neisseria species, p. 55-65. In H. Brade, S. M. Opal, S. N. Vogel, and D. C. Morrison (ed.). Endotoxin in health and disease. Marcel Dekker, Inc., New York, N.Y.
- 80.Giardina, P. C., R. Williams, D. Lubaroff, and M. A. Apicella. 1998. Neisseria gonorrhoeae induces focal polymerization of actin in primary human urethral epithelium. Infect. Immun. 66:3416-3419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gómez-Duarte, O. G., M. Dehio, C. A. Guzmán, G. S. Chatwal, C. Dehio, and T. F. Meyer. 1997. Binding of vitronectin to Opa-expressing Neisseria gonorrhoeae mediates invasion of HeLa cells. Infect. Immun. 65:3857-3866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gorby, G. L., C. M. Clemens, L. R. Barley, and Z. A. McGee. 1991. Effect of human chorionic gonadotropin (hCG) on Neisseria gonorrhoeae invasion of and IgA secretion by human fallopian tube mucosa. Microb. Pathog. 10:373-384. [DOI] [PubMed] [Google Scholar]
- 83.Gorter, A. D., J. Oostrik, P. van der Lay, P. S. Hiemstra, J. Dankert, and L. van Alphen. 2003. Involvement of lipooligosaccharides of Haemophilus influenzae and Neisseria meningitidis in defensin-enhanced bacterial adherence to epithelial cells. Microb. Pathog. 34:121-130. [DOI] [PubMed] [Google Scholar]
- 84.Grassmé, H., E. Gulbins, B. Brenner, K. Ferlinz, K. Sandhoff, K. Harzer, F. Lang, and T. F. Meyer. 1997. Acidic sphingomyelinase mediates entry of Neisseria gonorrhoeae into nonphagocytic cells. Cell 91:605-615. [DOI] [PubMed] [Google Scholar]
- 85.Grassmé, H. U. C., R. M. Ireland, and J. P. M. van Putten. 1996. Gonococcal opacity protein promotes bacterial entry-associated rearrangements of the epithelial cell actin cytoskeleton. Infect. Immun. 64:1621-1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Gray-Owen, S. D., D. R. Lorenzen, A. Haude, T. F. Meyer, and C. Dehio. 1997. Differential Opa specificities for CD66 receptors influence tissue interactions and cellular response to Neisseria gonorrhoeae. Mol. Microbiol. 26:971-980. [DOI] [PubMed] [Google Scholar]
- 87.Gray-Owen, S. D., C. Dehio, A. Haude, F. Grunert, and T. F. Meyer. 1997. CD66 carcinoembryonic antigens mediate interactions between Opa-expressing Neisseria gonorrhoeae and human polymorphonuclear phagocytes. EMBO J. 16:3435-3445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Gregg, C. R., A. P. Johnson, D. Taylor-Robinson, M. A. Melly, and Z. A. McGee. 1981. Host species-specific damage to oviduct mucosa by Neisseria gonorrhoeae lipopolysaccharide. Infect. Immun. 34:1056-1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Gregg, C. R., M. A. Melly, and Z. A. McGee. 1980. Gonococcal lipopolysaccharide: a toxin for human fallopian tube mucosa. Am. J. Obstet. Gynecol. 138:981-984. [DOI] [PubMed] [Google Scholar]
- 90.Griffiss, J. M., C. J. Lammel, J. Wang, N. P. Dekker, and G. F. Brooks. 1999. Neisseria gonorrhoeae coordinately uses pili and Opa to activate HEC-1-B cell microvilli, which causes engulfment of the gonococci. Infect. Immun. 67:3469-3480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Griffiss, J. M., J. P. O'Brien, R. Yamasaki, G. D. Williams, P. A. Rice, and H. Schneider. 1987. Physical heterogeneity of neisserial lipooligosaccharides reflects oligosaccharides that differ in apparent molecular weight, chemical composition, and antigenic expression. Infect. Immun. 55:1792-1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Haines, K. A., J. Reibman, X. Tang, M. S. Blake, and G. Weissmann. 1991. Effects of protein I of Neisseria gonorrhoeae on neutrophil activation: generation of diacylglycerol from phosphatidylcholine via a specific phospholipase C is associated with exocytosis. J. Cell Biol. 114:433-442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Haines, K. A., L. Yeh, M. S. Blake, P. Cristello, H. Korchak, and G. Weissmann. 1988. Protein I, a translocatable ion channel from Neisseria gonorrhoeae, selectively inhibits exocytosis from human neutrophils without inhibiting O2− generation. J. Biol. Chem. 263:945-951. [PubMed] [Google Scholar]
- 94.Hampton, M. B., A. J. Kettle, and C. C. Winterbourn. 1998. Inside the neutrophil phagosome: oxidants, myeloperoxidase, and bacterial killing. Blood 92:3007-3017. [PubMed] [Google Scholar]
- 95.Handsfield, H. H. 1990. Neisseria gonorrhoeae, p. 1613-1631. In G. L. Mandell, R. G. Douglas, Jr., and J. E. Bennett (ed.), Principles and practice of infectious disease 3rd ed., Churchill Livingstone, New York, N.Y.
- 96.Harvey, H. A., M. P. Jennings, C. A. Campbell, R. Williams, and M. A. Apicella. 2001. Receptor-mediated endocytosis of Neisseria gonorrhoeae into primary human urethral epithelial cells: the role of the asialoglycoprotein receptor. Mol. Microbiol. 42:659-672. [DOI] [PubMed] [Google Scholar]
- 97.Harvey, H. A., M. R. Ketterer, A. Preston, D. Lubaroff, R. Williams, and M. A. Apicella. 1997. Ultrastructure analysis of primary human urethral epithelial cell cultures infected with Neisseria gonorrhoeae. Infect. Immun. 65:2420-2427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Harvey, H. A., N. Porat, C. A. Campbell, M. P. Jennings, B. W. Gibson, N. J. Phillips, M. A. Apicella, and M. S. Blake. 2000. Gonococcal lipooligosaccharide is a ligand for the asialoglycoprotein receptor on human sperm. Mol. Microbiol. 36:1059-1070. [DOI] [PubMed] [Google Scholar]
- 99.Harvey, H. A., D. M. B. Post, and M. A. Apicella. 2002. Immortalization of human urethral epithelial cells: a model for the study of the pathogenesis of and the inflammatory cytokine response to Neisseria gonorrhoeae infection. Infect. Immun. 70:5808-5815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Harvey, H. A., W. E. Swords, and M. A. Apicella. 2001. The mimicry of human glycolipids and glycosphingolipids in the lipooligosaccharides of pathogenic Neisseria and Haemophilus. J. Autoimmun. 16:257-262. [DOI] [PubMed] [Google Scholar]
- 101.Hasty, L. A., J. D. Lambris, B. A. Lessey, K. Pruksananoda, and C. R. Lyttle. 1994. Hormonal regulation of the complement components and receptors throughout the menstrual cycle. Am. J. Obstet. Gynecol. 170:168-175. [DOI] [PubMed] [Google Scholar]
- 102.Hauck, C. R., and T. F. Meyer. 2003. ‘Small’ talk: Opa proteins as mediators of Neisseria-host-cell communication. Curr. Opin. Microbiol. 6:43-49. [DOI] [PubMed] [Google Scholar]
- 103.Hauck, C. R., T. F. Meyer, F. Lang, and E. Gulbins. 1998. CD66-mediated phagocytosis of Opa52 Neisseria gonorrhoeae requires a Src-like tyrosine kinase- and Rac1-dependent signaling pathway. EMBO J. 17:443-454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Heckels, J. E., M. Virji, K. Zak, and J. N. Fletcher. 1987. Immunobiology of gonococcal outer membrane protein I. Antonie Leeuwenhoek 53:461-464. [DOI] [PubMed] [Google Scholar]
- 105.Hedges, S. R., M. S. Mayo, L. Kallman, J. Mestecky, E. W. Hook III, and M. W. Russell. 1999. Limited local and systemic antibody responses to Neisseria gonorrhoeae during uncomplicated genital infections. Infect. Immun. 67:3937-3946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Henrichsen, J. 1983. Twitching motility. Annu. Rev. Microbiol. 37:81-93. [DOI] [PubMed] [Google Scholar]
- 107.Hitchcock, P. J. 1984. Analysis of gonococcal lipopolysaccharide in whole-cell lysates by sodium dodecyl sulfate-polyacrylamide gel electrophoresis: stable association of lipopolysaccharide with the major outer membrane protein (protein I) of Neisseria gonorrhoeae. Infect. Immun. 46:202-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Hixson, D. C., K. D. McEntire, and B. Obrink. 1985. Alterations in the expression of a hepatocyte cell adhesion molecule by transplantable rat hepatocellular carcinomas. Cancer Res. 45:3742-3749. [PubMed] [Google Scholar]
- 109.Hook, E. W., III, and H. H. Handsfield. 1999. Gonococcal infections in the adult, p. 451-466. In K. K. Holmes, P.-A. Mårdh, P. F. Sparling, S. M. Lemon, W. E. Stamm, P. Piot, and J. N. Wasserheit (ed.), Sexually transmitted diseases, 3rd ed. McGraw-Hill, New York, N.Y.
- 110.Hsieh, J.-T., W. Luo, W. Song, Y. Wang, D. I. Kleinerman, D. T. Van, and S. H. Lin. 1995. Tumor suppressive role of an androgen-regulated epithelial cell adhesion molecule (C-CAM) in prostate carcinoma cell revealed by sense and anti-sense approaches. Cancer Res. 55:190-197. [PubMed] [Google Scholar]
- 111.Iglesias, M., G. D. Plowman, and C. D. Woodworth. 1995. Interleukin-6 and interleukin-6 soluble receptor regulate proliferation of normal, human papillomavirus-immortalized, and carcinoma-derived cervical cells in vitro. Am. J. Pathol. 146:944-952. [PMC free article] [PubMed] [Google Scholar]
- 112.Ison, C. A., A. Dillon, Jr., and J. W. Tapsall. 1998. The epidemiology of global antibiotic resistance among Neisseria gonorrhoeae and Haemophilus ducreyi. Lancet 351(Suppl. III):8-11. [DOI] [PubMed] [Google Scholar]
- 113.James, J. F., and J. Swanson. 1978. Studies on gonococcal infection. XIII. Occurrence of color/opacity colonial variants in clinical cultures. Infect. Immun. 19:332-340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Jarvis, G. A. 1994. Analysis of C3 deposition and degradation on Neisseria meningitidis and Neisseria gonorrhoeae. Infect. Immun. 62:1755-1760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Jarvis, G. A. 1995. Recognition and control of neisserial infection by antibody and complement. Trends Microbiol. 3:198-201. [DOI] [PubMed] [Google Scholar]
- 116.Jerse, A. E. 1999. Experimental gonococcal genital tract infection and opacity protein expression in estradiol-treated mice. Infect. Immun. 67:5699-5708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Jerse, A. E., E. T. Crow, A. N. Bordner, I. Rahman, C. N. Cornelissen, T. R. Moench, and K. Mehrazar. 2002. Growth of Neisseria gonorrhoeae in the female mouse genital tract does not require the gonococcal transferrin or hemoglobin receptors and may be enhanced by commensal lactobacilli. Infect. Immun. 70:2549-2558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.John, C. M., H. Schneider, and J. M. Griffiss. 1999. Neisseria gonorrhoeae that infect men have lipooligosaccharides with terminal N-acetyllactosamine repeats. J. Biol. Chem. 274:1017-1025. [DOI] [PubMed] [Google Scholar]
- 119.Johnson, A. P., J. B. Clark, M. F. Osborn, and D. Taylor-Robinson. 1980. A comparison of the association of Neisseria gonorrhoeae with human and guinea-pig genital mucosa maintained in organ culture. Br. J. Exp. Pathol. 61:521-527. [PMC free article] [PubMed] [Google Scholar]
- 120.Johnson, A. P., D. Taylor-Robinson, and Z. A. McGee. 1977. Species specificity of attachment and damage to oviduct mucosa by Neisseria gonorrhoeae. Infect. Immun. 18:833-839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Joiner, K. A., R. Scales, K. A. Warren, M. M. Frank, and P. A. Rice. 1985. Mechanism of action of blocking immunoglobulin G for Neisseria gonorrhoeae. J. Clin. Investig. 76:1765-1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Joiner, K. A., K. A. Warren, E. J. Brown, J. Swanson, and M. M. Frank. 1983. Studies on the mechanism of bacterial resistance to complement-mediated killing. IV. C5b-9 forms high molecular weight complexes with bacterial outer membrane constituents on serum-resistant but not on serum-sensitive Neisseria gonorrhoeae. J. Immunol. 131:1443-1451. [PubMed] [Google Scholar]
- 123.Joiner, K. A., K. A. Warren, C. Hammer, and M. M. Frank. 1985. Bactericidal but not nonbactericidal C5b-9 is associated with distinctive outer membrane proteins in Neisseria gonorrhoeae. J. Immunol. 134:1920-1925. [PubMed] [Google Scholar]
- 124.Källström, H., D. Blackmer Gill, B. Albiger, M. K. Liszewski, J. P. Atkinson, and A.-B. Jonsson. 2001. Attachment of Neisseria gonorrhoeae to the cellular pilus receptor CD46: identification of domains important for bacterial adherence. Cell. Microbiol. 3:133-143. [DOI] [PubMed] [Google Scholar]
- 125.Källström, H., Md.S. Islam, P.-O. Berggren, and A.-B. Jonsson. 1998. Cell signaling by the type IV pili of pathogenic Neisseria. J. Biol. Chem. 273:21777-21782. [DOI] [PubMed] [Google Scholar]
- 126.Källström, H., M. K. Liszewski, J. P. Atkinson, and A.-B. Jonsson. 1997. Membrane cofactor protein (MCP or CD46) is a cellular pilus receptor for pathogenic Neisseria. Mol. Microbiol. 25:639-647. [DOI] [PubMed] [Google Scholar]
- 127.Kaur, P., and J. K. McDougall. 1988. Characterization of primary human keratinocytes transformed by human papillomavirus type 18. J. Virol. 62:1917-1924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Kellogg, D. S., Jr., I. R. Cohen, L. C. Norins, A. L. Schroeter, and G. Reising. 1968. Neisseria gonorrhoeae. II. Colonial variation and pathogenicity during 35 months in vitro. J. Bacteriol. 96:596-605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Kent, G. C. 1992. The urogenital system, p. 494-542. In R. J. Callanan, R. Lauck, G. M. Morris, D. L. Walls, and L. Fett (ed.), Comparative anatomy of the vertebrates, 7th ed. Mosby-Yearbook, Inc., St. Louis, Mo.
- 130.Kerwood, D. E., H. Schneider, and R. Yamasaki. 1992. Structural analysis of lipooligosaccharide produced by Neisseria gonorrhoeae, strain MS11mk (variant A): a precursor for a gonococcal lipooligosaccharide associated with virulence. Biochemistry 31:12760-12768. [DOI] [PubMed] [Google Scholar]
- 131.Kim, J. J., D. Zhou, R. E. Mandrell, and J. M. Griffiss. 1992. Effect of exogenous sialylation of the lipooligosaccharide of Neisseria gonorrhoeae on opsonophagocytosis. Infect. Immun. 60:4439-4442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Kita, E., H. Matsuura, and S. Kashiba. 1981. A mouse model for the study of gonococcal genital infection. J. Infect. Dis. 143:67-70. [DOI] [PubMed] [Google Scholar]
- 133.Kleinerman, D. I., P. Troncoso, S. H. Lin, L. L. Pisters, E. R. Sherwood, T. Brooks, A. C. von Eschenbach, and J. T. Hsieh. 1995. Consistent expression of an epithelial cell adhesion molecule (C-CAM) during human prostate development and loss of expression in prostate cancer: implication as a tumor suppressor. Cancer Res. 55:1215-1220. [PubMed] [Google Scholar]
- 134.Knapp, J. S., and R. J. Rice. 1995. Neisseria and Branhamella, p. 324-340. In P. R. Murray, E. J. Baron, M. A. Pfaller, F. C. Tenover, and R. H. Yolken (ed.), Manual of clinical microbiology, 6th ed. ASM Press, Washington, D.C.
- 135.Kondo, T., K. Mihara, Y. Inoue, and M. Namba. 1996. Two-dimensional electrophoretic studies on down-regulated intracellular transferrin in human fibroblasts immortalized by treatment with either 4-nitroquinoline 1-oxide or 60Co gamma rays. Electrophoresis 17:1638-1642. [DOI] [PubMed] [Google Scholar]
- 136.Kraus, D., M. E. Medof, and C. Mold. 1998. Complementary recognition of alternative pathway activators by decay-accelerating factor and factor H. Infect. Immun. 66:399-405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Krepler, R., H. Denk, U. Artlieb, and R. Moll. 1982. Immunocytochemistry of intermediate filament proteins present in pleomorphic adenomas of the human parotid gland: characterization of different cell types in the same tumor. Differentiation 21:191-199. [DOI] [PubMed] [Google Scholar]
- 138.Kunath, T., C. Ordoñez-Garcia, C. Turbide, and N. Beauchemin. 1997. Inhibition of colonic tumor cell growth by biliary glycoprotein. Oncogene 11:2375-2382. [PubMed] [Google Scholar]
- 139.Lemon, S. M., and P. F. Sparling. 1999. Pathogenesis of sexually transmitted viral and bacterial infections. p. 433-449. In K. K. Holmes, P.-A. Mardh, P. F. Sparling, S. M. Lemon, W. E. Stamm, P. Piot, and J. N. Wasserheit (ed.), Sexually transmitted diseases, 3rd ed. McGraw-Hill, New York, N.Y.
- 140.Lin, J., Z. M. Lei, S. Lojun, C. V. Rao, P. G. Satyaswaroop, and T. G. Day. 1994. Increased expression of luteinizing hormone/human chorionic gonadotropin receptor gene in human endometrial carcinomas. J. Clin. Endocrinol. Metab. 79:1483-1491. [DOI] [PubMed] [Google Scholar]
- 141.Lin, J.-S. L., S. P. Donegan, T. C. Heeren, M. Greenberg, E. F. Flaherty, R. Haivanis, X.-H. Su, D. Dean, W. J. Newhall, J. S. Knapp, S. K. Sarafian, R. J. Rice, S. A. Morse, and P. A. Rice. 1994. Transmission of Chlamydia trachomatis and Neisseria gonorrhoeae among men with urethritis and their female sex partners. J. Infect. Dis. 178:1707-1712. [DOI] [PubMed] [Google Scholar]
- 142.Lorenzen, D. R., D. Gunther, J. Pandit, T. Rudel, E. Brandt, and T. F. Meyer. 2000. Neisseria gonorrhoeae porin modifies the oxidative burst of human professional phagocytes. Infect. Immun. 68:6215-6222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Lynch, E. C., M. S. Blake, E. C. Gotschlich, and A. Mauro. 1984. Studies on porins: spontaneously transferred from whole cells and from proteins of Neisseria gonorrhoeae and Neisseria meningitidis. Biophys. J. 45:104-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Maitra, A., I. I. Wistuba, A. K. Virmani, M. Sakaguchi, I. Park, A. Stucky, S. Milchgrub, D. Gibbons, J. D. Minna, and A. F. Gazdar. 1999. Enrichment of epithelial cells for molecular studies. Nat. Med. 5:459-463. [DOI] [PubMed] [Google Scholar]
- 145.Maitra, A., I. I. Wistuba, D. Gibbons, A. F. Gazdar, and J. Albores-Saavedra. 1999. Allelic losses at chromosome 3p are seen in human papilloma virus 16 associated transitional cell carcinoma of the cervix. Gynecol. Oncol. 74:361-368. [DOI] [PubMed] [Google Scholar]
- 146.Mandrell, R. E. 1992. Further antigenic similarities of Neisseria gonorrhoeae lipooligosaccharides and human glycosphingolipids. Infect. Immun. 60:3017-3020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Mandrell, R. E., and M. A. Apicella. 1993. Lipo-oligosaccharides (LOS) of mucosal pathogens: molecular mimicry and host-modification of LOS. Immunobiology 187:382-402. [DOI] [PubMed] [Google Scholar]
- 148.Mandrell, R. E., J. M. Griffiss, and B. A. Machers. 1988. Lipooligosaccharides (LOS) of Neisseria gonorrhoeae and Neisseria meningitidis have components that are immunochemically similar to precursors of human blood group antigens. J. Exp. Med. 168:107-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Mandrell, R. E., A. J. Lesse, J. V. Sugai, J. M. Griffiss, J. A. Cole, N. J. Parsons, H. Smith, S. A. Morse, and M. A. Apicella. 1990. In vitro and in vivo modification of Neisseria gonorrhoeae lipopolysaccharide epitope structure by sialylation. J. Exp. Med. 171:1649-1664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Mandrell, R. E., H. Smith, G. A. Jarvis, J. M. Griffiss, and J. A. Cole. 1993. Detection and some properties of the sialyltransferase implicated in the sialylation of lipopolysaccharide of Neisseria gonorrhoeae. Microb. Pathog. 14:307-313. [DOI] [PubMed] [Google Scholar]
- 151.McCutchan, J. A., D. Katzenstein, D. Norquist, G. Chikami, A. Wunderlich, and A. I. Braude. 1978. Role of blocking antibody in disseminated gonococcal infection. J. Immunol. 121:1884-1888. [PubMed] [Google Scholar]
- 152.McDade, Jr., R. L., and K. H. Johnson. 1980. Characterization of serologically dominant outer membrane proteins of Neisseria gonorrhoeae. J. Bacteriol. 141:1183-1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.McGee, Z. A., C. M. Clemens, R. L. Jensen, J. J. Klein, L. R. Barley, and G. L. Gorby. 1992. Local induction of tumor necrosis factor as a molecular mechanism of mucosal damage by gonococci. Microb. Pathog. 12:333-341. [DOI] [PubMed] [Google Scholar]
- 154.McGee, Z. A., A. P. Johnson, and D. Taylor-Robinson. 1976. Human fallopian tubes in organ culture: preparation, maintenance, and quantitation of damage by pathogenic microorganisms. Infect Immun. 13:608-618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.McGee, Z. A., A. P. Johnson, and D. Taylor-Robinson. 1981. Pathogenic mechanisms of Neisseria gonorrhoeae: observations on damage to human fallopian tubes in organ culture by gonococci of colony type 1 or type 4. J. Infect. Dis. 143:413-422. [DOI] [PubMed] [Google Scholar]
- 156.McGee, Z. A., D. S. Stephens, L. H. Hoffman, W. F. Schlech III, and R. G. Horn. 1983. Mechanisms of mucosal invasion by pathogenic Neisseria. Rev. Infect. Dis. 5:S708-S714. [DOI] [PubMed] [Google Scholar]
- 157.McQuillen, D. P., S. Gulati, S. Ram, A. K. Turner, D. B. Jani, T. C. Heeren, and P. A. Rice. 1999. Complement processing and immunoglobulin binding to Neisseria gonorrhoeae determined in vitro simulates in vivo effects. J. Infect. Dis. 179:124-135. [DOI] [PubMed] [Google Scholar]
- 158.McRorie, R. A., and W. L. Williams. 1974. Biochemistry of mammalian fertilization. Annu. Rev. Biochem. 43:777-803. [DOI] [PubMed] [Google Scholar]
- 159.Melly, M. A., C. R. Gregg, and Z. A. McGee. 1981. Studies of toxicity of Neisseria gonorrhoeae for human fallopian tube mucosa. J. Infect. Dis. 143:423-431. [DOI] [PubMed] [Google Scholar]
- 160.Melly, M. A., Z. A. McGee, and R. S. Rosenthal. 1984. Ability of monomeric peptidoglycan fragments from Neisseria gonorrhoeae to damage human fallopian-tube mucosa. J. Infect. Dis. 149:378-386. [DOI] [PubMed] [Google Scholar]
- 161.Merz, A. J., C. A. Enns, and M. So. 1999. Type IV pili of pathogenic Neisseriae elicit cortical plaque formation in epithelial cells. Mol. Microbiol. 32:1316-1332. [DOI] [PubMed] [Google Scholar]
- 162.Merz, A. J., and M. So. 1997. Attachment of piliated, Opa− and Opc− gonococci and meningococci to epithelial cells elicits cortical actin rearrangements and clustering of tyrosine-phosphorylated proteins. Infect. Immun. 65:4341-4349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Merz, A. J., and M. So. 2000. Interactions of pathogenic Neisseriae with epithelial cell membranes. Annu. Rev. Cell Dev. Biol. 16:423-457. [DOI] [PubMed] [Google Scholar]
- 164.Miller, R. A. And B. E. Britigan. 1997. Role of oxidants in microbial pathophysiology. Clin. Microbiol. Rev. 10:1-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Moll, R., W. W. Franke, D. L. Schiller, B. Geiger, and R. Krepler. 1982. The catalog of human cytokeratins: patterns of expression in normal epithelia, tumors and cultured cells. Cell 31:11-24. [DOI] [PubMed] [Google Scholar]
- 166.Moll, R., D. B. von Bassewitz, U. Schulz, and W. W. Franke. 1982. An unusual type of cytokeratin filament in cells of a human cloacogenic carcinoma derived from the anorectal transition zone. Differentiation 22:25-40. [DOI] [PubMed] [Google Scholar]
- 167.Monif, G. R. G. 1980. Significance of polymicrobial bacterial superinfection in the therapy of gonococcal endometritis-salpingitis-peritonitis. Obstet. Gynecol. 55:154S-161S. [DOI] [PubMed] [Google Scholar]
- 168.Monif, G. R. G., S. L. Welkos, H. Baer, and R. J. Thompson. 1976. Cul-de-sac isolates from patients with endometritis-salpingitis-peritonitis and gonococcal endocervicitis. Am. J. Obstet. Gynecol. 126:158-161. [DOI] [PubMed] [Google Scholar]
- 169.Moore, K. L., and T. V. N. Persaud. 1998. The developing human: clinically oriented embryology, 5th ed., p. 265-303. W. B. Saunders, Philadelphia, Pa.
- 170.Moran, A. P., M. M. Prendergast, and B. J. Appelmelk. 1996. Molecular mimicry of host structures by bacterial lipopolysaccharides and its contribution to disease. FEMS Immunol. Med. Microbiol. 16:105-115. [DOI] [PubMed] [Google Scholar]
- 171.Morello, J. A., and M. Bohnhoff. 1989. Serovars and serum resistance of Neisseria gonorrhoeae from disseminated and uncomplicated infections. J. Infect. Dis. 160:1012-1017. [DOI] [PubMed] [Google Scholar]
- 172.Morse, S. A., and G. F. Brooks. 1985. Neisseria gonorrhoeae taxonomy, colony phenotypes and disease, p. 3-8. In G. F. Brooks and E. A. Donegan (ed.), Gonococcal infection. Butler and Tanner, Ltd., London, United Kingdom.
- 173.Mosleh, I. M., L. A. Huber, P. Steinlein, C. Pasquali, D. Günther, and T. F. Meyer. 1998. Neisseria gonorrhoeae porin modulates phagosome maturation. J. Biol. Chem. 273:35332-35338. [DOI] [PubMed] [Google Scholar]
- 174.Mosser, D. M., and P. J. Edelson. 1987. The third component of complement (C3) is responsible for the intracellular survival of Leishmania major. Nature 327:329-331. [DOI] [PubMed] [Google Scholar]
- 175.Muller, A., D. Gunther, V. Brinkmann, R. Hurwitz, T. F. Meyer, and T. Rudel. 2000. Targeting of the pro-apoptotic VDAC-like porin (PorB) of Neisseria gonorrhoeae to mitochondria of infected cells. EMBO J. 19:5332-5343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Muller, A., D. Gunther, F. Dux, M. Naumann, T. F. Meyer, and T. Rudel. 1999. Neisserial porin (PorB) causes rapid calcium influx in target cells and induces apoptosis by the activation of cysteine proteases. EMBO J. 18:339-352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Naids, F. L., and R. F. Rest. 1991. Stimulation of human neutrophil oxidative metabolism by nonopsonized Neisseria gonorrhoeae. Infect. Immun. 59:4383-4390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Nairn, C. A., J. A. Cole, P. V. Patel, N. J. Parsons, J. E. Fox, and H. Smith. 1988. Cytidine 5′-monophospho-N-acetylneuraminic acid or a related compound is the low Mr factor from human red blood cells which induces gonococcal resistance to killing by human serum. J. Gen. Microbiol. 134:3295-3306. [DOI] [PubMed] [Google Scholar]
- 179.Neumaier, M., S. Paululat, A. Chan, P. Matthaes, and C. Wagener. 1993. Biliary glycoprotein, a potential human cell adhesion molecule, is down-regulated in colorectal carcinomas. Proc. Natl. Acad. Sci. USA 90:10744-10748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Newhall, W. J., W. D. Sawyer, and R. A. Hank. 1980. Cross-linking analysis of the outer membrane proteins of Neisseria gonorrhoeae. Infect. Immun. 28:785-791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Nollau, P., H. Scheller, M. Kona-Horstmann, S. Rhode, F. Hagenmuller, C. Wagener, and M. Neurmaier. 1997. Expression of CD66a (human C-CAM) and other members of the carcinoembryonic antigen gene family of adhesion molecules in human colorectal adenomas. Cancer Res. 57:2354-2357. [PubMed] [Google Scholar]
- 182.Ober, W. B. 1970. Boswell's clap. JAMA 212:91-95. [PubMed] [Google Scholar]
- 183.Oglesby, T. J. 1998. The complement system in reproduction, p. 355-373. In J. E. Volanakis and M. M. Frank (ed.), The human complement system in health and disease. Marcel Dekker, Inc., New York, N.Y.
- 184.Parsons, N. J., A. Curry, A. J. Fox, D. M. Jones, J. A. Cole, and H. Smith. 1992. The serum resistance of gonococci in the majority of urethral exudates is due to sialylated lipopolysaccharide seen as a surface coat. FEMS Microbiol. Lett. 69:295-299. [DOI] [PubMed] [Google Scholar]
- 185.Parsons, N. J., P. V. Patel, E. L. Tan, J. R. C. Andrade, C. A. Nairn, M. Goldner, J. A. Cole, and H. Smith. 1988. Cytidine 5′-monophospho-N-acetyl neuraminic acid and a low molecular weight factor from human blood cells induce lipopolysaccharide alteration in gonococci when conferring resistance to killing by human serum. Microb. Pathog. 5:303-309. [DOI] [PubMed] [Google Scholar]
- 186.Patel, P. V., P. M. Martin, E. L. Tan, C. A. Nairn, N. J. Parsons, M. Goldner, and H. Smith. 1988. Protein changes associated with induced resistance of Neisseria gonorrhoeae to killing by human serum are relatively minor. J. Gen. Microbiol. 134:499-507. [DOI] [PubMed] [Google Scholar]
- 187.Paulesu, L., and G. P. Pessina. 1982. Cyclic changes of sialidase in human cervical mucus. Int. J. Biochem. 14:561-563. [DOI] [PubMed] [Google Scholar]
- 188.Pellegrino, M. B., B. B. Asch, J. L. Connolly, and H. L. Asch. 1988. Differential expression of keratins 13 and 16 in normal epithelium, benign lesions, and ductal carcinomas of the human breast determined by the monoclonal antibody Ks8.12. Cancer Res. 48:5831-5836. [PubMed] [Google Scholar]
- 189.Porat, N., M. A. Apicella, and M. S. Blake. 1995. A lipooligosaccharide-binding site on HepG2 cells similar to the gonococcal opacity-associated surface protein Opa. Infect. Immun. 63:2164-2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Preston, A., R. E. Mandrell, B. W. Gibson, and M. A. Apicella. 1996. The lipooligosaccharides of pathogenic gram-negative bacteria. Crit. Rev. Microbiol. 22:139-180. [DOI] [PubMed] [Google Scholar]
- 191.Price, R. J., and B. Boettcher. 1979. The presence of complement in human cervical mucus and its possible relevance to infertility in women with complement-dependent sperm-immobilizing antibodies. Fertil. Steril. 32:61-66. [DOI] [PubMed] [Google Scholar]
- 192.Pujol, C., E. Eugene, P. Morand, and X. Nassif. 2000. Do pathogenic Neisseriae need several ways to modify the host cell cytoskeleton? Microbes Infect. 2:821-827. [DOI] [PubMed] [Google Scholar]
- 193.Ram, S., A. D. Cox, J. C. Wright, U. Vogel, S. Getzlaff, R. Boden, J. Li, J. S. Plested, S. Meri, S. Gulati, D. C. Stein, J. C. Richards, E. R. Moxon, and P. A. Rice. 2003. Neisserial lipooligosaccharide is a target for complement component C4b: inner core phosphoethanolamine residues define C4b linkage specificity. J. Biol. Chem. 278:50853-50862. [DOI] [PubMed] [Google Scholar]
- 194.Ram, S., M. Cullinane, A. M. Blom, S. Gulati, D. P. McQuillen, R. Boden, B. G. Monks, C. O'Connell, C. Elkins, M. K. Pangburn, B. Dahlbäck, and P. A. Rice. 2001. C4bp binding to porin mediates stable serum resistance of Neisseria gonorrhoeae. Int. Immunopharmacol. 1:423-432. [DOI] [PubMed] [Google Scholar]
- 195.Ram, S., D. P. McQuillen, S. Gulati, C. Elkins, M. K. Pangburn, and P. A. Rice. 1998. Binding of complement factor H to loop 5 of porin protein 1A: a molecular mechanism of serum resistance of nonsialylated Neisseria gonorrhoeae. J. Exp. Med. 188:671-680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Ram, S., A. K. Sharma, S. D. Simpson, S. Gulati, D. P. McQuillen, M. K. Pangburn, and P. A. Rice. 1998. A novel sialic acid binding site on factor H mediates serum resistance of sialylated Neisseria gonorrhoeae. J. Exp. Med. 187:743-752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Ramsey, K. H., H. Schneider, A. S. Cross, J. W. Boslego, D. L. Hoover, T. L. Staley R. A. Kuschner, and C. D. Deal. 1995. Inflammatory cytokines produced in response to experimental human gonorrhea. J. Infect. Dis. 172:186-191. [DOI] [PubMed] [Google Scholar]
- 198.Reshef, E., Z. M. Lei, Ch. V. Rao, D. D. Pridham, N. Chegini, and J. L. Luborsky. 1990. The presence of gonadotropin receptors in nonpregnant human uterus, human placenta, fetal membranes, and decidua. J. Clin. Endocrinol. Metab. 70:421-430. [DOI] [PubMed] [Google Scholar]
- 199.Rest, R. F. 1979. Killing of Neisseria gonorrhoeae by human polymorphonuclear neutrophil granule extracts. Infect. Immun. 25:574-579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Rest, R. F., S. H. Fischer, Z. Z. Ingham, and J. F. Jones. 1982. Interactions of Neisseria gonorrhoeae with human neutrophils: effects of serum and gonococcal opacity on phagocyte killing and chemiluminescence. Infect. Immun. 36:737-744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Rest, R. F., and J. V. Frangipane. 1992. Growth of Neisseria gonorrhoeae in CMP-N-acetylneuraminic acid inhibits nonopsonic (opacity-associated outer membrane protein-mediated) interactions with human neutrophils. Infect. Immun. 60:989-997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Rest, R. F., J. Liu, R. Talukdar, J. V. Frangipane, and D. Simon. 1994. Interaction of pathogenic Neisseria with host defenses. What happens in vivo? Ann. N. Y. Acad. Sci. 730:182-196. [DOI] [PubMed] [Google Scholar]
- 203.Rice, P. A. 1989. Molecular basis for serum resistance in Neisseria gonorrhoeae. Clin. Microbiol. Rev. 2:S112-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Rice, P. A., and D. L. Kasper. 1982. Characterization of serum resistance of Neisseria gonorrhoeae that disseminate. J. Clin. Investig. 70:157-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Rice, P. A., H. E. Vayo, M. R. Tam, and M. S. Blake. 1986. Immunoglobulin G antibodies directed against protein III block killing of serum-resistant Neisseria gonorrhoeae by immune sera. J. Exp. Med. 164:1735-1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Rudel, T., H.-J. Boxberger, and T. F. Meyer. 1996. Modulation of Neisseria porin (PorB) by cytosolic ATP/GTP of target cells: parallels between pathogen accommodation and mitochondrial endosymbiosis. Cell 85:391-402. [DOI] [PubMed] [Google Scholar]
- 207.Sadler, T. W. 2000. Urogenital system, p. 272-311. In P. Coryell, C. Taylor, and B. Cady (ed.), Langman's medical embryology, 8th ed. Lippincott, Williams, and Wilkins, Baltimore, Md.
- 208.Schmitter, T., F. Agerer, L. Peterson, P. Munzner, and C. R. Hauck. 2004. Granulocyte CEACAM3 is a phagocytic receptor of the innate immune system that mediates recognition and elimination of human-specific pathogens. J. Exp. Med. 199:35-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Schneider, H., A. S. Cross, R. A. Kuschner, D. N. Taylor, J. C. Sandoff, J. W. Boslego, and C. D. Deal. 1995. Experimental human gonococcal urethritis: 250 Neisseria gonorrhoeae MS11mkC are infective. J. Infect. Dis. 172:180-185. [DOI] [PubMed] [Google Scholar]
- 210.Schneider, H., J. M. Griffiss, J. W. Boslego, P. J. Hitchcock, K. M. Zahos, and M. A. Apicella. 1991. Expression of paragloboside-like lipooligosaccharides may be a necessary component of gonococcal pathogenesis in men. J. Exp. Med. 174:1601-1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Schneider, H., C. A. Hammack, M. A. Apicella, and J. M. Griffiss. 1988. Instability of expression of lipooligosaccharides and their epitopes in Neisseria gonorrhoeae. Infect. Immun. 56:942-946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Schneider, H., K. A. Schmidt, D. R. Skillman, L. Van De Verg, R. L. Warren, H. J. Wylie, J. C. Sadoff, C. D. Deal, and A. S. Cross. 1996. Sialylation lessens the infectivity of Neisseria gonorrhoeae MS11mkC. J. Infect. Dis. 173:1422-1427. [DOI] [PubMed] [Google Scholar]
- 213.Screaton, R. A., L. Z. Penn, and C. P. Stanners. 1997. Carcinoembryonic antigen, a human tumor marker, cooperates with Myc and Bcl-2 in cellular transformation. J. Cell Biol. 137:939-952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Seib, K. L., M. P. Jennings, and A. G. McEwan. 2003. A Sco homologue plays a role in defense against oxidative stress in pathogenic Neisseria. FEBS Lett. 546:411-415. [DOI] [PubMed] [Google Scholar]
- 215.Seya, T., T. Hara, M. Matsumoto, and H. Akedo. 1990. Quantitative analysis of membrane cofactor protein (MCP) of complement. High expression of MCP on human leukemia cell lines, which is down-regulated during cell differentiation. J. Immunol. 145:238-245. [PubMed] [Google Scholar]
- 216.Shafer, W. M., A. Datta, V. S. Kolli, M. M. Rahman, J. T. Balthazar, L. E. Martin, W. L. Veal, D. S. Stephens, and R. Carlson. 2002. Phase variable changes in genes lgtA and lgtC within the lgtABCDE operon of Neisseria gonorrhoeae can modulate gonococcal susceptibility to normal human serum. J. Endotoxin. Res. 8:47-58. [PubMed] [Google Scholar]
- 217.Shafer, W. M. And R. F. Rest. 1989. Interactions of gonococci with phagocytic cells. Annu. Rev. Microbiol. 43:121-145. [DOI] [PubMed] [Google Scholar]
- 218.Shell, D. M., L. Chiles, R. C. Judd, S. Seal, and R. F. Rest. 2002. The Neisseria lipooligosaccharide-specific alpha-2,3-sialyltransferase is a surface-exposed outer membrane protein. Infect. Immun. 70:3744-3751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Shivapurkar, N., S. Sood, I. I. Wistuba, A. K., Virmani, A. Maitra, S. Milchgrub, J. D. Minna, and A. F. Gazdar. 1999. Multiple regions of chromosome 4 demonstrating allelic losses in breast carcinomas. Cancer Res. 59:3576-3580. [PubMed] [Google Scholar]
- 220.Sizemore, N., and E. A. Rorke. 1993. Human papillomavirus 16 immortalization of normal ectocervical epithelial cells alters retinoic acid regulation of cell growth and epidermal growth factor receptor expression. Cancer Res. 53:4511-4517. [PubMed] [Google Scholar]
- 221.Skubitz, K. M., K. D. Campbell, K. Ahmed, and A. P. N. Skubitz. 1995. CD66 family members are associated with tyrosine activity in human neutrophils. J. Immunol. 155:5382-5390. [PubMed] [Google Scholar]
- 222.Smedts, F., F. Ramaekers, H. Robben, M. Pruszczynski, G. van Muijen, B. Lane, I. Leigh, and P. Vooijs. 1990. Changing patterns of keratin expression during progression of cervical intraepithelial neoplasia. Am. J. Pathol. 136:657-668. [PMC free article] [PubMed] [Google Scholar]
- 223.Smedts, F., F. Ramaekers, S. Troyanovsky, M. Pruszczynski, M. Link, B. Lane, I. Leigh, C. Schijf, and P. Vooijs. 1992. Keratin expression in cervical cancer. Am. J. Pathol. 141:497-511. [PMC free article] [PubMed] [Google Scholar]
- 224.Smedts, F., F. Ramaekers, and P. Vooijs. 1993. The dynamics of keratin expression in malignant transformation of cervical epithelium: a review. Obstet. Gynecol. 82:465. [PubMed] [Google Scholar]
- 225.Smith, H., N. J. Parsons, and J. A. Cole. 1995. Sialylation of neisserial lipopolysaccharides: a major influence on pathogenicity. Microb. Pathog. 19:365-377. [DOI] [PubMed] [Google Scholar]
- 226.Snapper, C. M., F. R. Rosas, M. R. Kehry, J. J. Mond, and L. M. Wetzler. 1997. Neisserial porins may provide critical second signals to polysaccharide-activated murine B cells for induction of immunoglobulin secretion. Infect. Immun. 65:3202-3208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Snyder, L. A., S. A. Butcher, and N. J. Saunders. 2001. Comparative whole-genome analyses reveal over 100 putative phase-variable genes in the pathogenic Neisseria spp. Microbiology 147:2321-2332. [DOI] [PubMed] [Google Scholar]
- 228.Sowter, C., and Z. A. McGee. 1976. Evaluation of a new technique for the demonstration of gonococci and other micro-organisms in host cells. J. Clin. Pathol. 29:433-437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Sparling, P. F. 1999. Biology of Neisseria gonorrhoeae, p. 433-449. In K. K. Holmes, P.-A. Mardh, P. F. Sparling, S. M. Lemon, W. E. Stamm, P. Piot, and J. N. Wasserheit (ed.), Sexually transmitted diseases, 3rd ed. McGraw-Hill, New York, N.Y.
- 230.Spence, J. M., J. C.-R. Chen, and V. L. Clark. 1997. A proposed role for the lutropin receptor in contact-inducible gonococcal invasion of Hec1B cells. Infect. Immun. 65:3736-3742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Spence, J. M., R. E. Tyler, R. A. Domaoal, and V. L. Clark. 2002. L12 enhances gonococcal transcytosis of polarized Hec1B cells via the lutropin receptor. Microb. Pathog. 32:117-125. [DOI] [PubMed] [Google Scholar]
- 232.Srivastava, P. N., L. J. Zaneveld, and W. L. Williams. 1970. Mammalian sperm acrosomal neuraminidases. Biochem. Biophys. Res. Commun. 39:575-582. [DOI] [PubMed] [Google Scholar]
- 233.Stephens, D. S. 1989. Gonococcal and meningococcal pathogenesis as defined by human cell, cell culture, and organ culture assays. Clin. Microbiol. Rev. 2:S104-S111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Stephens, D. S., Z. A. McGee, and M. D. Cooper. 1987. Cytopathic effects of pathogenic Neisseria. Studies using human fallopian tube organ cultures and nasopharyngeal organ cultures. Antonie Leeuwenhoek. 53:575-584. [DOI] [PubMed] [Google Scholar]
- 235.Stockert, R. J. 1995. The asialoglycoprotein receptor: relationships between structure, function, and expression. Physiol. Rev. 75:591-609. [DOI] [PubMed] [Google Scholar]
- 236.Stocks, S. C., M. A. Kerr, C. Haslett, and I. Dransfield. 1995. CD66-dependent neutrophil activation: a possible mechanism for vascular selectin-mediated regulation of neutrophil adhesion. J. Leukoc. Biol. 58:40-48. [DOI] [PubMed] [Google Scholar]
- 237.Sun, Q., K. Tsutsumi, M. Yokoyama, M. M. Pater, and A. Pater. 1993. In vivo cytokeratin-expression pattern of stratified squamous epithelium from human papillomavirus-type-16-immortalized ectocervical and foreskin keratinocytes. Int. J. Cancer 54:656-662. [DOI] [PubMed] [Google Scholar]
- 238.Swanson, J. 1973. Studies on gonococcus infection. IV. Pili: their role in attachment of gonococci to tissue culture cells. J. Exp. Med. 137:571-589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Swanson, J. 1978. Studies on gonococcus infection XIV. Cell wall protein differences among color/opacity colony variants of Neisseria gonorrhoeae. Infect. Immun. 21:292-302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Swanson, K. V., G. A. Jarvis, G. F. Brooks, B. J. Barham, M. D. Cooper, and J. M. Griffiss. 2001. CEACAM is not necessary for Neisseria gonorrhoeae to adhere to and invade female genital epithelial cells. Cell. Microbiol. 3:681-691. [DOI] [PubMed] [Google Scholar]
- 241.Sweet, R. L., M. Blankfort-Doyle, M. O. Robbie, and J. Schacter. 1986. The occurrence of chlamydial and gonococcal salpingitis during the menstrual cycle. JAMA 255:2062-2064. [PubMed] [Google Scholar]
- 242.Tauber, P. F., W. Wettich, M. Nohlen, and L. J. Zaneveld. 1985. Diffusible proteins of the mucosa of the human cervix, uterus, and fallopian tubes: distribution and variations during the menstrual cycle. Am. J. Obstet. Gynecol. 151:1115-1125. [DOI] [PubMed] [Google Scholar]
- 243.Taylor-Robinson, D., P. M. Furr, and C. M. Hetherington. 1990. Neisseria gonorrhoeae colonizes the genital tract of oestradiol-treated germ-free female mice. Microb. Pathog. 9:369-373. [DOI] [PubMed] [Google Scholar]
- 244.Tobiason, D. M., and H. S. Seifert. 2001. Inverse relationship between pilus-mediated gonococcal adherence and surface expression of the pilus receptor, CD46. Microbiology 147:2333-2340. [DOI] [PubMed] [Google Scholar]
- 245.Tramont, E. C. 1989. Gonococcal vaccines. Clin. Microbiol. Rev. 2:S74-S77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Tseng, H. J., Y. Srikhanta, A. G. McEwan, and M. P. Jennings. 2001. Accumulation of manganese in Neisseria gonorrhoeae correlates with resistance to oxidative killing by superoxide anion and is independent of superoxide dismutase activity. Mol. Microbiol. 40:1175-1186. [DOI] [PubMed] [Google Scholar]
- 247.Vanderpuye, O. A., C. A. Labarrere, and J. A. McIntyre. 1992. The complement system in reproduction. Fertil. Immunol. 27:145-155. [DOI] [PubMed] [Google Scholar]
- 248.van Duynhoven, Y. T. H. P. 1999. The epidemiology of Neisseria gonorrhoeae in Europe. Microbes Infect. 1:455-464. [DOI] [PubMed] [Google Scholar]
- 249.van Putten, J. P. 1993. Phase variation of lipopolysaccharide directs interconversion of invasive and immuno-resistant phenotypes of Neisseria gonorrhoeae. EMBO J. 12:4043-4051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.van Putten, J. P. M., T. D. Duensing, and R. L. Cole. 1998. Entry of Opa+ gonococci into Hep-2 cells requires concerted action of glycosaminoglycans, fibronectin and integrin receptors. Mol. Microbiol. 29:369-379. [DOI] [PubMed] [Google Scholar]
- 251.van Putten, J. P. M., and B. D. Robertson. 1995. Molecular mechanisms and implications for infection of lipopolysaccharide variation in Neisseria. Mol. Microbiol. 16:847-853. [DOI] [PubMed] [Google Scholar]
- 252.Virji, M., K. Makepeace, D. J. Ferguson, and S. M. Watt. 1996. Carcinoembryonic antigens (CD66) on epithelial cells and neutrophils are receptors for Opa proteins of pathogenic Neisseriae. Mol. Microbiol. 22:941-950. [DOI] [PubMed] [Google Scholar]
- 253.Virji, M., S. M. Watt, S. Barker, K. Makepeace, and R. Doyonnas. 1996. The N-domain of the human CD66a adhesion molecule is a target for Opa proteins of Neisseria meningitidis and Neisseria gonorrhoeae. Mol. Microbiol. 22:929-939. [DOI] [PubMed] [Google Scholar]
- 254.Vogel, U., and M. Frosch. 1999. Mechanisms of neisserial serum resistance. Mol. Microbiol. 32:1133-1139. [DOI] [PubMed] [Google Scholar]
- 255.von Bassewitz, D. B., A. Roessner, and E. Grundmann. 1982. Intermediate-sized filaments in cells of normal human colon mucosa, adenomas and carcinomas. Pathol. Res. Pract. 175:238-255. [DOI] [PubMed] [Google Scholar]
- 256.Wall, D., and D. Kaiser. 1999. Type IV pili and cell motility. Mol. Microbiol. 32:1-10. [DOI] [PubMed] [Google Scholar]
- 257.Ward, M. E., J. N. Robertson, P. M. Englefield, and P. J. Watt. 1975. Gonococcal infection: invasion of the mucosal surfaces of the genital tract, p. 188-199. In D. Schlessinger (ed.), Microbiology. American Society for Microbiology, Washington, D.C.
- 258.Ward, M. E., P. J. Watt, and J. N. Robertson. 1974. The human fallopian tube: a laboratory model for gonococcal infection. J. Infect. Dis. 129:650-659. [DOI] [PubMed] [Google Scholar]
- 259.Weel, J. F. L., and J. P. M. van Putten. 1991. Fate of the major outer membrane protein P.IA in early and late events of gonococcal infection of epithelial cells. Res. Microbiol. 142:985-993. [DOI] [PubMed] [Google Scholar]
- 260.Weigel, P. H., and J. A. Oka. 1998. The dual coated pit pathway hypothesis: vertebrate cells have both ancient and modern coated pit pathways for receptor mediated endocytosis. Biochem. Biophys. Res. Commun. 246:563-569. [DOI] [PubMed] [Google Scholar]
- 261.Wen, K.-K., P. C. Giardina, M. S. Blake, J. L. Edwards, M. A. Apicella, and P. A. Rubenstein. 2000. Interaction of the gonococcal porin P.IB with G- and F-actin. Biochemistry 39:8638-8647. [DOI] [PubMed] [Google Scholar]
- 262.Wiesenfeld, H. C., R. P. Heine, M. A. Krohn, S. L. Hillier, A. A. Amortegui, M. Nicolazzo, and R. L. Sweet. 2002. Association between elevated neutrophil defensin levels and endometritis. J. Infect. Dis. 186:792-797. [DOI] [PubMed] [Google Scholar]
- 263.Williams, J. M., G.-C. Chen, L. Zhu, and R. F. Rest. 1998. Using the yeast two-hybrid system to identify human epithelial cell proteins that bind gonococcal Opa proteins: intracellular gonococci bind pyruvate kinase via their Opa proteins and require host pyruvate for growth. Mol. Microbiol. 27:171-186. [DOI] [PubMed] [Google Scholar]
- 264.Workowski, K. A., and W. C. Levine. 2002. Sexually transmitted diseases treatment guidelines—2002. Morb. Mortal. Wkly. Rep. 51(RR06):1-80. [Google Scholar]
- 265.Wright, S. D., P. E. Rao, W. C. van Voorhis, L. S. Craigmyle, K. Iida, M. A. Talle, E. F. Westberg, G. Goldstein, and S. C. Silverstein. 1983. Identification of the C3bi receptor of human monocytes and macrophages by using monoclonal antibodies. Proc. Natl. Acad. Sci. USA 80:5699-5703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Wright, S. D., and S. C. Silverstein. 1983. Receptors for C3b and C3bi promote phagocytosis but not the release of toxic oxygen from human phagocytes. J. Exp. Med. 158:2016-2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Würzner, R. 1999. Evasion of pathogens by avoiding recognition or eradication by complement, in part via molecular mimicry. Mol. Immunol. 36:249-260. [DOI] [PubMed] [Google Scholar]
- 268.Yamamoto, K., and R. B. Johnston. 1984. Dissociation of phagocytosis from stimulation of the oxidative metabolic burst in macrophages. J. Exp. Med. 159:405-416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Yamasaki, R., H. Koshino, S. Kurono, Y. Nishinaka, D. P. McQuillen, A. Kume, S. Gulati, and P. A. Rice. 1999. Structural and immunochemical characterization of a Neisseria gonorrhoeae epitope defined by a monoclonal antibody 2C7; the antibody recognizes a conserved epitope on specific lipo-oligosaccharides in spite of the presence of human carbohydrate epitopes. J. Biol. Chem. 274:36550-36558. [DOI] [PubMed] [Google Scholar]
- 270.Yang, Q. L., and E. C. Gotschlich. 1996. Variation of gonococcal lipooligosaccharide structure is due to alterations in poly-G tracts in lgt genes encoding glycosyl transferases. J. Exp. Med. 183:323-327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Zenni, M. K., P. C. Giardina, H. A. Harvey, J. Shao, M. R. Ketterer, D. M. Lubaroff, R. D. Williams, and M. A. Apicella. 2000. Macropinocytosis as a mechanism of entry into primary human urethral epithelial cells by Neisseria gonorrhoeae. Infect. Immun. 68:1696-1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Zheng, H. Y., D. J. Hassett, K. Bean, and M. S. Cohen. 1992. Regulation of catalase in Neisseria gonorrhoeae. Effects of oxidant stress and exposure to human neutrophils. J. Clin. Investig. 90:1000-1006. [DOI] [PMC free article] [PubMed] [Google Scholar]