Key Points
The immune response comprises not only pro-inflammatory and anti-inflammatory pathways but also pro-resolution mechanisms that serve to balance the need of the host to target microbial pathogens while preventing excess inflammation and bystander tissue damage.
Specialized pro-resolving mediators (SPMs) are enzymatically derived from essential fatty acids to serve as a novel class of immunoresolvents that limit acute responses and orchestrate the clearance of tissue pathogens, dying cells and debris from the battlefield of infectious inflammation.
SPMs are composed of lipoxins, E-series and D-series resolvins, protectins and maresins. Individual members of the SPM family serve as agonists at cognate receptors to induce cell-type specific responses.
Important regulatory roles for SPMs have been uncovered in host responses to several microorganisms, including bacterial, viral, fungal and parasitic pathogens.
SPMs also promote the resolution of non-infectious inflammation and tissue injury. Defects in host SPM pathways contribute to the development of chronic inflammatory diseases.
With the capacity to enhance host defence and modulate inflammation, SPMs represent a promising translational approach to enlist host resolution programmes for the treatment of infection and excess inflammation.
Supplementary information
The online version of this article (doi:10.1038/nri.2015.4) contains supplementary material, which is available to authorized users.
Subject terms: Inflammation, Infectious diseases, Mucosal immunology, Respiratory tract diseases
Here, the authors detail our current understanding of specialized pro-resolving mediators (SPMs), a family of endogenous mediators that have important roles in promoting the resolution of inflammation. With a focus on the lungs, they discuss the contribution of SPMs to infectious and chronic inflammatory diseases and their emerging therapeutic potential.
Supplementary information
The online version of this article (doi:10.1038/nri.2015.4) contains supplementary material, which is available to authorized users.
Abstract
Specialized pro-resolving mediators (SPMs) are enzymatically derived from essential fatty acids and have important roles in orchestrating the resolution of tissue inflammation — that is, catabasis. Host responses to tissue infection elicit acute inflammation in an attempt to control invading pathogens. SPMs are lipid mediators that are part of a larger family of pro-resolving molecules, which includes proteins and gases, that together restrain inflammation and resolve the infection. These immunoresolvents are distinct from immunosuppressive molecules as they not only dampen inflammation but also promote host defence. Here, we focus primarily on SPMs and their roles in lung infection and inflammation to illustrate the potent actions these mediators play in restoring tissue homeostasis after an infection.
Supplementary information
The online version of this article (doi:10.1038/nri.2015.4) contains supplementary material, which is available to authorized users.
Main
Acute inflammation is a vital response to infection that is initiated within seconds of pathogen detection1. Granulocytes are rapidly recruited to sites of infection2, where they become activated and augment the resident capacity of infected tissue to kill and ultimately clear the pathogen3. These early events in the host response to infection are essential for survival and are coordinated by several families of pro-inflammatory mediators, including lipid mediators (such as prostaglandins and leukotrienes), cytokines and chemokines. These pro-inflammatory mediators have overlapping and distinct functions and ultimately induce an increase in vascular permeability and orchestrate leukocyte recruitment. This leads to the cardinal signs of tissue inflammation — namely calor, rubor, tumor, dolor and potentially functio laesa (Fig. 1).
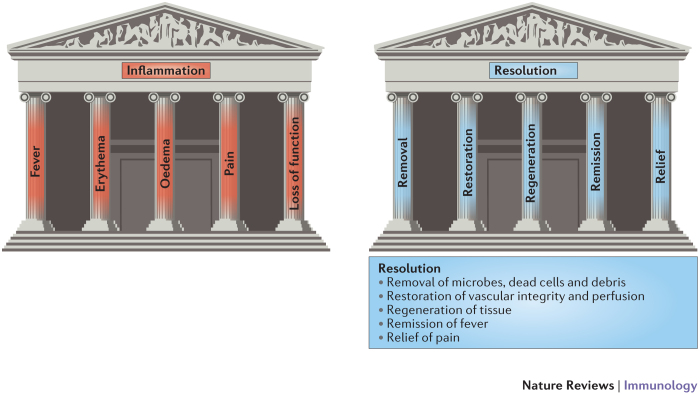
Figure 1. Cardinal signs of inflammation and its resolution.
Tissue- and organism-level responses to inflammation have been well recognized for centuries and can be summarized as the 'five pillars of inflammation'; namely, calor (fever), rubor (redness), tumor (swelling and oedema), dolor (pain) and functio laesa (loss of function). With the recognition that the resolution of inflammation is an active process, recent research has identified molecular and cellular processes that promote catabasis. These can be summarized as the 'five pillars of resolution'; that is, removal of microorganisms, dead cells and debris, restoration of vascular integrity and perfusion, tissue regeneration, remission of fever and relief from inflammatory pain.
Recently, a new array of molecules that function in the resolution of inflammation were elucidated and named specialized pro-resolving mediators (SPMs)4,5. Many of these SPMs are produced during the acute inflammatory response6, and their structure, biosynthesis and organic synthesis have been recently reviewed (see Ref. 5). Typically, acute inflammatory responses to pathogens are self-limiting, and there is a growing appreciation that SPMs have pivotal anti-inflammatory and anti-infective roles in tissue catabasis4. For effective resolution of inflammation to occur in tissues, cessation of granulocyte recruitment is required in conjunction with the recruitment and differentiation of macrophages, which help clear inflammatory cells and tissue debris to restore tissue homeostasis7. Granulocytes in the tissue undergo apoptosis during the resolution of inflammation to prevent bystander tissue injury occurring from the release of potentially toxic cellular contents8. Removal of apoptotic neutrophils prompts a switch from a pro- to an anti-inflammatory macrophage phenotype, which is a prerequisite for macrophage efferocytosis and egress via the lymphatic vessels9. Efferocytosis also leads to further production of additional SPMs that signal for restoration of vascular integrity, regeneration and/or repair of injured tissues, remission of fever by inhibition of pro-inflammatory lipid mediators and cytokines, and relief of inflammatory pain10. Together, the SPMs and these cellular events in resolution can be summarized as the newly recognized five cardinal signs of resolution (Fig. 1).
In this Review, we address the functions of SPMs in infectious immunity and chronic inflammatory diseases, with a focus on how SPMs affect lung physiology and pathology in these diseases. Recent discoveries11,12,13,14,15 regarding anti-inflammatory, anti-infective and pro-resolving roles for SPMs point to their potential translational applications in harnessing endogenous resolution responses for novel host-directed therapeutic strategies in sterile and infectious inflammation. Additional roles in these homeostatic processes for non-lipid mediators of resolution will not be covered in detail here but have been recently reviewed (see Refs 16,17,18). Cellular and molecular mechanisms for catabasis have now been determined in multiple organ systems and diseases. Here, we will primarily focus on lung infection and inflammation. The resolution responses that occur in non-pulmonary sites of infection and inflammation have recently been reviewed (see Refs 7,19,20,21). Finally, we consider how new therapeutic strategies that incorporate immunoresolvents may have the potential to synergize with antibiotics and to mitigate the growing problem of antibiotic resistance.
SPM production
In response to pathogen invasion or tissue injury, polyunsaturated fatty acids are released locally from membrane phospholipids or delivered to sites of inflammation by tissue oedema for subsequent conversion to specialized mediators by cells in the exudates22. Within minutes, the generation of eicosanoids (that is, prostaglandins and cysteinyl leukotrienes) from arachidonic acid (C20:4n-6) metabolism helps to direct peripheral blood neutrophils to infected sites. Prostaglandin E2 (PGE2) and PGI2 regulate blood flow, whereas leukotriene C4 (LTC4) and LTD4 regulate vascular permeability1,23. Furthermore, neutrophils transmigrate towards chemotactic gradients of LTB4 (Ref. 24). With selected cytokines, chemokines and complement components (namely C5a and C3b), these eicosanoids induce neutrophil entry into the tissue to engulf and kill invading pathogens3,25. Early in the acute inflammatory response, the origins are laid for biosynthesis of resolution-phase mediators through lipid mediator class-switching, in which arachidonic acid metabolism switches from the production of leukotrienes to the production of lipoxins — the lead family of pro-resolving mediators26. Disruption of lipoxin formation or lipoxin receptor availability delays the resolution response27,28,29,30.
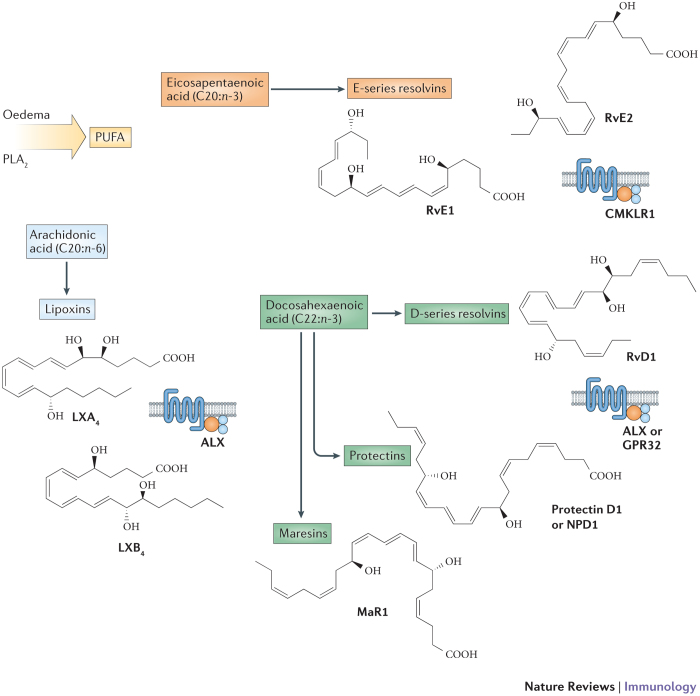
As a class, the SPMs are enzymatically derived from essential fatty acids, including arachidonic acid, eicosapentaenoic acid (EPA; C20:5n-3) and docosahexaenoic acid (DHA; C22:6n-3) in a lipoxygenase (LOX)-dependent manner (Fig. 2). SPMs are stereoselective, and complete stereochemical assignment for the majority of the SPMs has been established (reviewed in Ref. 31). Lipoxins are formed by transcellular biosynthesis via multiple distinct pathways. One pathway involves leukocyte-derived 5-LOX and platelet-derived 12-LOX in the vasculature32. A second pathway involves the conversion of arachidonic acid by epithelial cell-, eosinophil- or monocyte-derived 15-LOX and leukocyte-derived 5-LOX33,34. Although aspirin inhibits prostaglandin production, aspirin-mediated acetylation of cyclooxygenase 2 (COX2; also known as PTGS2) leads to the conversion of arachidonic acid to 15(R)-hydroxyeicosatetraenoic acid (15(R)-HETE), which can serve as a substrate for 5-LOX-mediated conversion to 15-epi-lipoxins (also known as aspirin-triggered (AT) lipoxins)35. Of note, in the absence of aspirin, 15(R)-HETE can also be produced by cytochrome P450 enzymes to act as a substrate for 15-epi-lipoxin transcellular biosynthesis36,37.
Figure 2. Polyunsaturated fatty acids are substrates for specialized pro-resolving mediators.
Stereoselective mediators that enhance host defence, resolve tissue inflammation and stimulate tissue regeneration have been described4. These specialized pro-resolving mediators (SPMs) are produced in a spatio-temporally regulated manner from essential polyunsaturated fatty acids (PUFAs) that are either released enzymatically by phospholipase A2 (PLA2) from cell membranes for secondary conversion by biosynthetic enzymes or delivered with oedema fluid from plasma to exudates. The principal SPM families are lipoxins from arachidonic acid (C20:4n-6; in light blue), as well as the E-series resolvins from eicosapentaenoic acid (C20:5n-3; in pink) and D-series resolvins, protectins and maresins from docosahexaenoic acid (C22:6n-3; in green). The SPM precursors eicosapentaenoic acid and docosahexaenoic acid are essential omega-3 PUFAs. Representative members of these families, their structures and receptors are shown here. CMKLR1, chemokine-like receptor 1; GPR32, probable G protein-coupled receptor 32; LX, lipoxin; MaR1, maresin 1; NPD1, neuroprotectin D1; RvD1, resolvin D1; RvE, resolvin E.
In addition to lipoxins, resolving exudates also contain pro-resolving mediators derived from omega-3 fatty acids. These include resolvins, protectins and maresins (reviewed in Ref. 38) (Fig. 2). E-series and D-series resolvins are enzymatically derived from EPA and DHA, respectively. Similarly to 15-epi-lipoxins, resolvins are generated through interactions between aspirin-acetylated COX2 and LOX activities39. For example, in the vasculature, resolvin E1 (RvE1) transcellular synthesis in the presence of aspirin is notable for transformation of EPA to 18(R)-hydroxyEPA (18(R)-HEPE) by aspirin-acetylated COX2 in endothelial cells and 18(R)-HEPE conversion to RvE1 by leukocyte 5-LOX40,41. There are two major series of resolvins that are derived from DHA, namely D-series resolvins (RvD1–RvD6) and their positional AT isomers (AT-RvD1–RvD6)42. The D-series resolvins are enzymatically generated by 15-LOX-mediated conversion of DHA to 17(S)-hydroperoxyDHA (17(S)-HpDHA) and subsequent transformation by 5-LOX. For the AT-resolvins, DHA is initially converted by aspirin-acetylated COX2 to 17(R)-HpDHA that can also serve as a substrate for 5-LOX-mediated transformation to epimeric resolvins. Additional families of pro-resolution mediators derived from DHA have also been identified in resolving inflammatory exudates that display protective bioactivities, namely protectins and maresins43,44. At sites of inflammation, 15-LOX-derived 17(S)-HpDHA can be converted to protectin D1 (Ref. 45), and 12-LOX-derived 14(S)-HpDHA can be converted to maresin 1 (MaR1) (for a detailed review, see Ref. 31). The respiratory tract mucosa in health is enriched with DHA46, and both 17(S)-hydroxy-DHA and protectin D1 are generated in human airways47.
These SPMs exert their bioactions as molecular signals via agonist properties at cognate receptors (Fig. 2). The lipoxin A4 (LXA4) receptor ALX (also known as FPR2) is a G protein-coupled receptor that binds LXA4 and 15-epi-LXA4 with high affinity. High-affinity receptors have also been identified for RvE1 (namely, chemokine-like receptor 1 (CMKLR1; also known as CHEMR23))41, for RvD1 (namely, the probable G protein-coupled receptor GPR32) and for RvD2 (namely, the N-arachidonyl glycine receptor GPR18)48,49. Of interest, RvD1 can also activate ALX with high affinity and is equipotent to LXA4 in binding and activating this receptor49. In addition to RvD1, AT-RvD1 and RvD3 bind to GPR32 with high affinity49,50,51. These SPMs display potent receptor-mediated cell-specific actions (Table 1). Pharmacological structure activity relationships support receptor-dependent signalling mechanisms for the remaining SPMs; however, the molecular identity of their cognate receptors is still to be determined.
Table 1. SPMs display cell-type specific actions.
| Mediator | Target cell | Action(s) | Refs |
|---|---|---|---|
| Lipoxin A4 | Neutrophil | Inhibits chemotaxis, trans-endothelial and trans-epithelial migration | 140,141 |
| Inhibits neutrophil–epithelial cell interactions | 75,77,140 | ||
| Inhibits superoxide anion generation and degranulation | 142,144 | ||
| Monocyte | Stimulates chemotaxis and adhesion | 145 | |
| Inhibits peroxynitrite generation | 146 | ||
| Reduces IL-8 release by cells from individuals with asthma | 147 | ||
| Macrophage | Increases engulfment of apoptotic neutrophils | 62 | |
| Eosinophil | Inhibits migration and chemotaxis | 148 | |
| Inhibits generation of eotaxin and IL-5 | 112 | ||
| NK cell | Inhibits NK cell cytotoxicity | 149 | |
| Increases granulocyte apoptosis | 67 | ||
| ILC2 | Inhibits IL-13 release | 67 | |
| Dendritic cell | Inhibits IL-12 production | 110 | |
| Epithelial cell | Increases proliferation after acid injury, blocks IL-6 and IL-8 release | 77 | |
| Endothelial cell | Stimulates PKC-dependent prostacyclin formation | 150 | |
| Blocks the generation of reactive oxygen species | 151 | ||
| Inhibits VEGF-induced endothelial-cell migration | 152 | ||
| Fibroblast | Inhibits IL-1β-induced IL-6, IL-8 and MMP3 production | 153 | |
| Inhibits CTGF-induced proliferation | 154 | ||
| Smooth muscle | Inhibits LTC4-initiated migration | 155 | |
| Resolvin E1 | Neutrophil | Inhibits trans-epithelial and trans-endothelial migration | 156 |
| Inhibits superoxide generation | 87 | ||
| Macrophage | Stimulates non-phlogistic phagocytosis of apoptotic neutrophils | 30 | |
| Dendritic cell | Inhibits IL-12 production | 157 | |
| Inhibits migration | 41 | ||
| NK cell | Expresses CMKLR1 receptors | 67 | |
| Resolvin E3 | Neutrophil | Inhibits infiltration | 158 |
| Resolvin D1 | Neutrophil | Inhibits transmigration | 159 |
| Macrophage | Inhibits LPS-induced TNF release | 160 | |
| Increases phagocytosis of allergen and apoptotic cells | 9,63 | ||
| Protectin D1 | Neutrophil | Inhibits TNF and IFNγ release | 161 |
| Inhibits PMN transmigration | 11 | ||
| Upregulates CCR5 expression | 72 | ||
| Macrophage | Stimulates non-phlogistic phagocytosis of apoptotic PMNs | 30 | |
| Maresin 1 | ILC2 | Inhibits IL-13 production and stimulates amphiregulin production | 70 |
| Regulatory T cell | Induces regulatory T cell formation and stimulates amphiregulin production | 70 | |
| Bronchial epithelial cell | Inhibits organic dust-induced cytokine production | 162 |
CCR5, CC-chemokine receptor 5; CMKLR1, chemokine-like receptor 1; CTGF, connective tissue growth factor; IFNγ, interferon-γ; IL, interleukin; ILC2, group 2 innate lymphoid cell; LPS, lipopolysaccharide; LTC4, leukotriene C4; MMP3, matrix metalloproteinase 3; NK, natural killer; PKC, protein kinase C; PMN, polymorphonuclear leukocyte; SPM, specialized pro-resolving mediator; TNF, tumour necrosis factor; VEGF, vascular endothelial growth factor.
As is the case with lipoxins, defects in these SPM pathways can undermine resolution and contribute to chronic inflammation27,30,52,53,54,55. Failure of the resolution response may occur as a result of defects in receptor expression, enzyme synthesis, intracellular signalling or nutritional deficiencies in essential polyunsaturated fatty acids. Functional roles bring these structurally distinct families of lipoxins, resolvins, protectins and maresins together as SPMs — a genus of endogenous molecules that pharmacologically act as immunoresolvents4.
Pro-resolving mediators are active in the picogram to nanogram dose range, whereby they are able to control inflammation, limit tissue damage, shorten resolution intervals, promote healing and alleviate pain in experimental models of inflammation and resolution. These fatty acid-derived mediators are part of a larger resolution programme that includes annexin A1 protein16, several cytokines (for example, transforming growth factor-β (TGFβ) and interleukin-10 (IL-10))11, microRNAs51 and carbon monoxide56. Inhibitors of cyclin-dependent kinases can also pharmacologically promote resolution57.
Cellular targets of SPMs
Counter-regulation of the acute inflammatory response evolved to neutralize and eliminate pathogens and enable repair of inflamed or injured tissues. The main cellular events of resolution are the cessation of neutrophil influx and activation, in conjunction with macrophage recruitment, efferocytosis and phagocytosis of microorganisms and debris6,58. As a class of mediators, SPMs are partly defined by their overlapping function to limit neutrophil tissue accumulation, counter-regulate pro-inflammatory cytokines and encourage macrophage phagocytosis (Fig. 3). During efferocytosis, phagocytes generate SPMs that serve as autacoids to inhibit neutrophil activation, increase apoptotic cell expression of CC-chemokine receptor 5 (CCR5) for chemokine clearance and promote bacterial killing and efferocytosis by macrophages (Table 1). In addition to phagocytes, lymphoid cells have vital roles in host defence, express SPM receptors and can serve as cellular effectors for SPMs. In this section, we highlight selected cell types with important functions in resolution and host defence that respond to SPMs.
Figure 3. Cellular mechanisms for SPMs in lung anti-inflammation and pro-resolution.
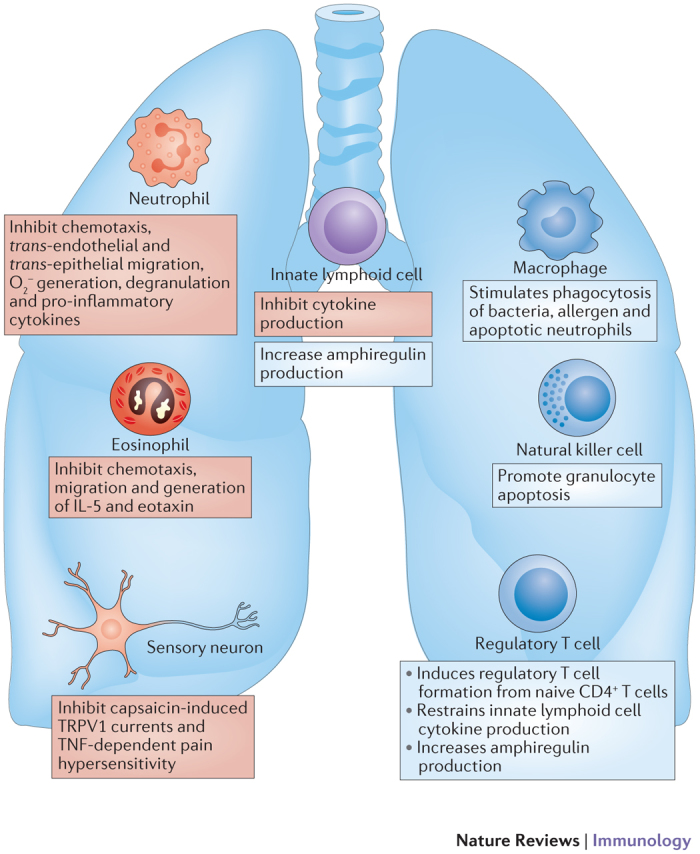
During a self-limited inflammatory response, resolution of inflammation is an active process governed by specialized pro-resolving mediators (SPMs) that transmit both anti-inflammatory (red) and pro-resolving (blue) actions to leukocytes and tissue-resident cells. This class of endogenous immunoresolvents induces an anti-inflammatory response by inhibiting granulocyte migration and activation, disrupting sensory neuron activation and dampening cytokine production by a variety of structural cells, including epithelial cells, endothelial cells and fibroblasts. SPMs have a multipronged action to regulate sentinel innate lymphoid cells to decrease cytokine and increase amphiregulin production. These mediators also promote resolution by inducing regulatory T cells to control innate lymphoid cells, stimulating natural killer cells to trigger granulocyte apoptosis and engaging macrophages in a non-phlogistic manner to engulf bacteria and noxious stimuli, and clear apoptotic cells by efferocytosis. IL-5, interleukin-5; O2−, superoxide; TNF, tumour necrosis factor; TRPV1, transient receptor potential cation channel subfamily V member 1.
Neutrophils. For tissue resolution of inflammation, it is essential to prevent further neutrophil entry, inhibit tissue neutrophil activation and promote the clearance of apoptotic neutrophils. All of these cellular actions are mediated by SPMs. Of particular note, SPMs initiate leukocyte shape changes that limit neutrophil migration in vitro22, diapedesis in vivo and reduce tissue inflammation and damage29,47,59,60,61. For neutrophils, SPMs have potent anti-inflammatory actions, including decreased cell activation, adhesion and reactive oxygen species generation and increased microbial clearance (reviewed in Ref. 4).
Macrophages. Both tissue-resident and recruited inflammatory macrophages serve pivotal roles in responses to infection and inflammation. SPMs augment macrophage functions to clear microorganisms, tissue debris and apoptotic cells (reviewed in Ref. 6). In contrast to neutrophils, SPMs lead to macrophage shape changes that prepare the cells for phagocytosis of microorganisms, apoptotic cells and debris9,12,62,63. Key macrophage actions for SPMs include increased phagocytosis and IL-10 production and decreased pro-inflammatory cytokine production9,64,65.
Natural killer cells. Natural killer (NK) cells can help promote the resolution of an inflammatory response by inducing neutrophil66 and eosinophil apoptosis67, which is a non-inflammatory mechanism for cell removal from tissues and has a crucial role in successful resolution of the inflammatory response8. Apoptotic granulocytes can subsequently be removed by tissue macrophage efferocytosis before tissues are exposed to their potentially toxic contents. By accelerating granulocyte apoptosis, NK cells can limit pathogen-mediated inflammatory responses. NK cells express ALX67, and LXA4 increases NK cell-mediated apoptosis of eosinophils and neutrophils67. NK cells also express CMKLR1, which is the receptor for RvE1 (Ref. 67), and NK cell depletion markedly impairs the protective actions of RvE1 in vivo68.
Innate lymphoid cells. Group 2 innate lymphoid cells (ILC2s) are members of the family of innate-like leukocytes. ILC2s do not express T cell or B cell antigen receptors, or markers of other leukocyte lineages, but they serve important roles for host defence against helminth infections69. In response to epithelial-derived cytokines, such as IL-25, IL-33, thymic stromal lymphopoietin and mast cell-derived prostanoids (that is, PGD2), ILC2s generate type 2 cytokines — IL-5 and IL-13 — in an antigen-independent manner67. Similarly to NK cells, ILC2s express receptors for pro-resolving mediators, including LXA4 and RvE1 (Ref. 67). LXA4 and MaR1 can potently inhibit ILC2 release of pro-inflammatory cytokines67,70. MaR1 also promotes amphiregulin release by ILC2s70, a protective response for restoring lung mucosal homeostasis after influenza infection71.
Lymphocytes. Adaptive immune cells also have important roles in the active resolution of inflammation. CCR5 expression on apoptotic, activated T cells acts to sequester pro-inflammatory cytokines and terminate inflammation; a mechanism that is augmented by SPMs72. RvE1 decreases the production of pro-inflammatory cytokines, such as IL-23 and IL-17, to dampen the adaptive immune response, particularly T helper 17 (TH17) cell responses73. Regulatory T cells are pivotal to controlling effector T cell proliferation and activation. Of note, MaR1 was recently identified as a potent inducer for the formation of regulatory T cells in vivo and in vitro in combination with TGFβ70. Only limited information is available on SPM actions on B cells, but RvD1 was recently shown to augment B cell antibody production and increase the number of antibody-producing B cells in a mouse influenza vaccination model74. These emerging data on the regulation of adaptive immunity by SPMs extend their range of actions and suggest a pivotal role for these imunoresolvents in the transition from innate to adaptive inflammation.
Mucosal epithelial cells. In mucosal host defence, transmigrating neutrophils initiate a respiratory burst and degranulation response to invading pathogens; however, excessive neutrophil activation can cause 'bystander' tissue damage and contribute to pathobiology of mucosal inflammatory disease75. During resolution, the activated neutrophils are cleared apically from the intestinal lumin by decay accelerating factor (also known as CD55), which is an anti-adhesive molecule76. SPMs potently inhibit neutrophil trans-epithelial migration and the production of pro-inflammatory cytokines by epithelial cells77. In addition, SPMs promote decay accelerating factor expression in mucosal epithelia as well as expression of the anti-infective peptide bactericidal permeability-increasing protein and the lipopolysaccharide (LPS) detoxification enzyme alkaline phosphatase78,79.
SPMs in infection
Although the role of SPMs has only recently been uncovered in tissue homeostasis, there is already a push to understand the functions of SPMs in infections. Studies on the role of SPMs in the modulation of host responses to various infectious diseases have highlighted a new therapeutic opportunity for targeting the host in infectious inflammation to complement antibiotic therapy. Some recent examples are provided in Table 2 and the following sections, in which we consider the roles of SPMs in bacterial, viral and fungal diseases.
Table 2. SPMs influence host defence and infectious inflammation.
| Infection or infective agent | Mediator | Role | Refs |
|---|---|---|---|
| Virus | |||
| Influenza A | Lipoxins | H5N1, a more virulent strain, is associated with a decrease in lipoxin signalling leading to increased leukocyte recruitment and extrapulmonary dissemination of the virus | 98 |
| Protectins | Protectin D1 is suppressed in virulent H5N1; treatment with protectin D1 improves survival | 102 | |
| RSV | Lipoxins | Lipoxins are required to elicit alternatively activated macrophages, leading to resolution of lung pathology | 106 |
| HIV | Lipoxins | Lipoxins are produced in HIV infection, but their function is uncertain | 163 |
| HSV | Resolvins | Reduce neutrophil and CD4+ T cell recruitment (TH1 cells and TH17 cells), increase IL-10 and decrease pro-inflammatory cytokines and stromal keratitis lesions | 107 |
| Protectins | Reduce neutrophil and CD4+ T cell recruitment (TH1 cells and TH17 cells), increase IL-10 and decrease pro-inflammatory cytokines and stromal keratitis lesions | 108 | |
| Bacterial infection | |||
| Mycobacterium tuberculosis | Lipoxins | 5-lipoxygenase deficient mice have lower circulating levels of LXA4, increased TH1-type inflammation and lower rates of resistance | 92 |
| LXA4 associates with plasma membrane repair and necrosis of infected macrophages | 164,165 | ||
| Mycobacterial susceptibility is linked to LTA4 hydrolase activity that controls LTB4 production directly and LXA4 production indirectly | 15 | ||
| Variations in the ALOX5 gene (which encodes 5-lipoxygenase) are associated with variation in tuberculosis susceptibility | 93 | ||
| Periodontitis | Lipoxins | In rabbits, overexpression of lipoxin or treatment with a lipoxin analogue decreases bone loss and tissue inflammation | 85 |
| Decrease PMN infiltration to sites of Porphyromonas gingivalis infection | 84 | ||
| LXA4 analogue promotes regeneration of hard and soft tissue loss in pig models of periodontitis | 166 | ||
| Resolvins | Resolve local inflammation and promote tissue regeneration after infection-mediated destruction | 61 | |
| Decrease inflammation and protect against bone loss | 87 | ||
| Decrease neutrophil infiltration and pro-inflammatory cytokine levels | 88 | ||
| Restore impaired phagocyte activity of macrophages | 90 | ||
| RvE1 is bone-protective in murine models, mediating preservation and accelerating regeneration | 167 | ||
| Salmonella spp. | Lipoxins | Increase BPI and enhanced bacterial killing | 79 |
| Gram-negative bacteria-associated sepsis | Lipoxins | Decrease pro-inflammatory mediators via NF-κB mediated mechanism, decrease bacterial load and increase peritoneal macrophages and survival | 96 |
| Decrease PMN recruitment, attenuate inflammation and, in combination with antibiotics, improve survival | 95 | ||
| Resolvins | Decrease bacterial burden, limit cytokine production, increase macrophage phagocytosis and improve survival | 14 | |
| Decrease antibiotic requirements, enhance actions of ciprofloxacin and accelerate resolution | 12 | ||
| Burn-associated sepsis | Resolvins | Enhance and/or restore neutrophil recruitment and improve overall survival | 168 |
| Escherichia coli (pneumonia and ARDS) | Lipoxins | Promote apoptosis of neutrophils | 80 |
| Resolvins | Decrease neutrophil recruitment, enhance bacterial clearance, decrease IL-1 and IL6, and improve survival | 13 | |
| Enhance neutrophil apoptosis and improve survival | 81 | ||
| Staphylococcus aureus | Resolvins | Enhance vancomycin-mediated clearance of bacteria | 12 |
| Borrelia burgdorferi | Lipoxins | In the absence of 5-lipoxygenase, mice develop persistent arthritis | 91 |
| Parasites | |||
| Toxoplasma gondii | Lipoxins | Infected mice have high serum levels of lipoxins | 115 |
| 5-lipoxygenase deficient animals have higher levels of IL-12 and IFNγ with improved parasite control but have higher mortality from excess inflammation | 111 | ||
| LXA4 suppressed IL-12 production in dendritic cells | 110 | ||
| Trypanosoma cruzi | Lipoxins | Aspirin-triggered lipoxins are elevated, and increased 15-epi-LXA4 levels improve parasite load, cardiac inflammation and mortality | 114 |
| Plasmodium spp. (malaria parasite) | Lipoxins | 5-lipoxygenase deficient mice have higher levels of IL-12 and IFNγ and increased mortality. Treatment with lipoxins decreases brain inflammation and improves survival | 113 |
| Angiostrongylus costaricensis | Lipoxins | Treatment of infected rats with an LXA4 analogue shortens the duration of the allergic response to the parasitic infection | 112 |
| Yeast | |||
| Candida albicans | Resolvins | Reduces neutrophil chemotaxis, enhances phagocytosis and promotes clearance | 117 |
ARDS, acute respiratory distress syndrome; BPI, bactericidal permeability-increasing protein; HSV, herpes simplex virus; IFNγ, interferon-γ; IL, interleukin; LT, leukotriene; LXA4, lipoxin A4; NF-κB, nuclear factor-κB; PMN, polymorphonuclear leukocyte; RSV, respiratory syncytial virus; RvE1, resolvin E1; SPM, specialized pro-resolving mediator; TH, T helper.
SPMs in bacterial infection
Pneumonia. Although pneumonia typically initiates a self-limiting acute inflammatory response, in some individuals the inflammation is so severe that it leads to life-threatening hypoxaemia and respiratory failure — namely, the acute respiratory distress syndrome (ARDS) — which is discussed in greater detail in the next section. In Escherichia coli-induced pneumonia, the SPM LXA4 promotes neutrophil apoptosis by inducing the phosphorylation of BCL-2-associated death promoter (BAD) and reducing the expression of the anti-apoptotic protein myeloid cell leukaemia sequence 1 (MCL1)80, whereas RvE1 promotes neutrophil apoptosis through activation of caspases81. In both cases, promotion of neutrophil death leads to a reduction in the severity of acute lung inflammation81,82. These findings highlight a direct interaction between the SPMs and apoptotic pathways in immune cells. In addition, RvE1 enhances bacterial clearance and reduces local production of pro-inflammatory cytokines in E. coli aspiration pneumonia, which results in enhanced survival of mice13.
Periodontitis. Bacterial periodontitis is a well-established experimental model that has been used to elucidate the role of SPMs in controlling localized bacterial infection, its associated tissue damage and systemic effects. Periodontitis is generally caused by a polymicrobial insult, resulting in the generation of biofilms, overgrowth of resident Gram-negative bacteria in the oral cavity and mucosal inflammation. The disease process is thought to be mediated by an overly robust immune response to the bacteria, including to Porphyromonas gingivalis in chronic infection and Actinobacillus spp. in the localized aggressive form of the disease. Periodontitis also carries a more generalized implication to human health, as localized periodontitis elicits a systemic response, increasing systemic inflammation and risk for accelerated atherosclerosis82,83.
In localized P. gingivalis infection models, introduction of stable analogues of lipoxins and AT-lipoxins results in a reduction of neutrophil recruitment to the site of infection84. In a rabbit model of the same infection, rabbits that either transgenically overexpress 15-LOX, the enzyme responsible for production of lipoxins and protectins, or are treated with a topical formulation of LXA4 had a reduction in leukocyte infiltration in inflammation at the site of injury and a reduction in bone loss85, highlighting a suppressive role for the lipoxins in the control of localized inflammation in this chronic infection. Furthermore, the systemic response to infection is attenuated, resulting in a decrease in neutrophil–platelet interactions86 and limiting generalized systemic inflammation, as indicated by a reduction in biomarkers such as C-reactive protein61.
Resolvins also have a role in promoting protection against bacterial periodontitis. In localized aggressive periodontitis (LAP), RvE1 suppresses neutrophil superoxide generation87, neutrophil infiltration88 and the production of pro-inflammatory cytokines88, and enhances macrophage activity89. At least some of its actions are mediated through its interaction with CMKLR1, which is highly expressed on macrophages and dendritic cells (DCs)41. In models of LAP, treatment of animals with topical RvE1 results in a decrease in localized and systemic inflammation and allows the host to regenerate lost tissue and bone mass61. The ability of RvE1 to re-establish homeostasis at the local tissue level proceeds in part through its ability to restore phagocyte activity of macrophages, which is impaired in LAP90. Lipoxin analogues or AT-lipoxins have no significant effect on neutrophil activity in LAP, which is in contrast to chronic periodontitis, in which LXA4 has a regulatory role, highlighting a context-specific mechanism for the pro-resolving mediators.
Lyme disease. In a similar manner to periodontitis, a pattern of localized and systemic control of inflammation is seen in mouse models of Lyme disease. In 5-LOX-deficient mice, which have a defect in SPM production, the development of arthritis in animals infected with Borrelia burgdorferi is similar to that in wild-type animals; however, the absence of lipoxins and resolvins impairs the host ability to resolve arthritis, resulting in chronic disease91 and a lack of control of the chronic systemic inflammatory response long after the triggering infectious agent has been cleared.
Tuberculosis. The protective roles for SPMs in acute infections, such as pneumonia, are also integral to the host immune response to Mycobacterium tuberculosis. In this host response, there is a delicate balance between pro-inflammatory mediators, such as PGE2 and LTB4, and pro-resolving mediators, such as LXA4, that can dictate the intensity of the pathogen-mediated inflammation as well as microbial clearance. In a mouse model of M. tuberculosis infection, there is a rise in the levels of both the pro-inflammatory LTB4 and the pro-resolving LXA4 after infection, with LXA4 high levels persisting throughout the chronic infection92. In animals deficient in 5-LOX (a deficiency that leads to defective leukotriene and lipoxin production), M. tuberculosis infection is associated with enhanced survival92. Host lipoxin generation is related to M. tuberculosis strain virulence, suggesting a vital role for SPMs in modulating the host inflammatory responses to M. tuberculosis. Excessive production of either LTB4 or LXA4 can result in aberrant host responses to M. tuberculosis infection that, intriguingly, converge on dysregulated expression of TNF15. This accentuates the importance of both pro-inflammatory and pro-resolving responses for host defence and regulation of pathogen-mediated inflammation. Crucial roles for arachidonic acid metabolism in immune responses may be linked to the different infectious rates observed with human variants in the ALOX5 (encoding 5-LOX) locus93 and the LTA4H (which encodes LTA4 hydrolase, an enzyme involved in the final step of LTB4 production) locus94, which both appear to disrupt LTB4 and LXA4 production as well as altering protection against naturally occurring M. tuberculosis infection. Together, these findings suggest that a combinatorial approach to tuberculosis therapy would be most effective, including antibiotics to help endogenous mechanisms kill the microorganism and SPMs to control the host immune response.
Sepsis. Sepsis is the most serious complication of acute bacterial infection. The host response in sepsis leads to diffuse systemic immune dysregulation that progresses rapidly, frequently resulting in shock. In Gram-negative bacteria-initiated sepsis, there appears to be a protective and potentially therapeutic role for lipid mediators. In mice with sepsis after caecal ligation and puncture, treatment with LXA4 reduced the production of pro-inflammatory cytokines, while simultaneously promoting a reduction in Gram-negative bacteria loads that improved survival95,96. Resolvins also have an important protective role in sepsis models. RvD2 serves as a potent regulator of the systemic inflammatory response in sepsis14. This reduction in pro-inflammatory signals is a consequence, in part, of reduction in nuclear factor-κB (NF-κB) activity13,60,96. Treatment of septic mice with RvD2 leads to a profound reduction in the production of cytokines, including IL-6, IL-10 and interferon-α (IFNα), and leukocyte infiltration to the site of infection is reduced. Of interest, control of the inflammatory response leads to an overall reduction in bacterial loads, both at the local site of insult and systemically within the blood, and an improvement in overall animal survival14. Sepsis is a disease of overwhelming infectious insult, compounded by an overly robust inflammatory response, whereby treatment with anti-inflammatory therapies potentially subjects the host to further harm. Modulation of pro-resolution responses appears to promote dampening of the inflammatory response while still allowing for adequate, and possibly improved, clearance of the bacterial infection. The ability to clear the source of infection while still limiting the immune response provides an attractive therapeutic paradigm for this disease of substantial health-care burden.
The biological demand for an initial robust response against a bacterial insult is juxtaposed against the need to control prolonged and overly exuberant inflammatory responses that are potentially harmful, raising potential challenges for the therapeutic use of pro-resolving mediators. For example, in a pneumosepsis model, early treatment with LXA4 appears to limit the immune response by decreasing leukocyte infiltration, reducing bacterial clearance and worsening the survival rate97. By contrast, in the same model, later treatment with LXA4 had positive effects, allowing for adequate clearance of infection but dampening the protracted and pathological immune response, therefore enhancing survival97. In the future, timing and dosing considerations and concomitant antibiotic use will be important for developing SPM therapeutic strategies in sepsis.
Overall, in bacterial infection, SPMs have significant therapeutic potential with ongoing research focused on their anti-infective mechanisms and optimal dose and timing strategies to harness their beneficial actions. In animal models, the augmentation of resolution also appears to reduce the needed dosage for antibiotics in the clearance of bacterial infections12,95. Given the worldwide crisis of emerging antibiotic resistance, therapies that could reduce antibiotic usage provide an attractive alternative in the quest to develop new and enhanced antimicrobial therapeutic approaches.
SPMs in viral infections
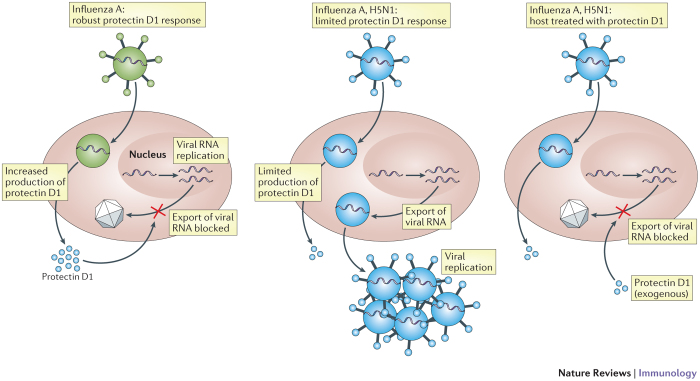
Influenza. Viral pathogens also appear to interact with the host in a way that is modifiable by pro-resolving factors. Influenza viruses are a well-suited model to understand the role of resolution mediators and the mechanisms in viral infections, as different strains of the virus elicit varied host immune responses and outcomes. In studies that compare more virulent strains of the influenza virus to less virulent strains, pro-resolving mediators inversely correlated with biological activity of the virus. More virulent strains of influenza led to suppression of lipoxins98, which is associated with enhanced viral dissemination. Protectin D1 has pivotal and multiple roles in regulating viral pathogenicity. More virulent influenza strains, such as H5N1, downregulate protectin D1 levels, and the pathogenicity of various isolates correlates inversely with levels of protectins99. In addition to host inflammatory responses, protectin D1 has direct antiviral actions on influenza; both protectin D1 and its isomer protectin DX (which is formed by LOX-mediated double oxygenation) interfere with viral RNA nuclear export machinery, thereby limiting viral replication100,101,102. Treatment of infected mice with protectin D1 improves survival (Fig. 4) even when administered as late as 48 hours after infection102, at a time when current antiviral therapies are no longer significantly effective103.
Figure 4. Selected SPMs increase antiviral host defence.
In hosts infected with influenza viruses, endogenous protectin D1 production is increased. Protectin D1 limits influenza pathogenicity by directly interacting with the RNA replication machinery to inhibit viral RNA nuclear export. In particularly virulent strains of influenza, such as the H5N1 avian (A) strain, protectin D1 formation is not sufficiently upregulated, leading to more efficient viral replication and host demise. Treatment of the host with exogenous protectin D1 can restore inhibition of viral RNA export, thereby limiting viral replication and improving host survival.
Respiratory syncytial virus. Respiratory syncytial virus (RSV) infection results in a bronchiolitis that is driven by classically activated macrophages and eventually resolved by alternatively activated macrophages104. Promotion of these two alternative macrophage fates appears related to RSV-induced COX2 (Ref. 105) and LXA4- and RvE1-mediated protective actions106. Host responses to RSV again highlight roles for SPMs and lipid mediator class-switching in the initial control and eventual clearance of infection.
Herpes simplex virus. Herpes simplex virus (HSV) ocular infection represents another example in which local control of the virus results from a robust inflammatory response, with long-term consequences of chronic inflammation that persists after clearance of the virus, including the potential for eventual blindness from stromal keratitis. In animals with HSV, topical administration of RvE1 results in decreased influx of effector CD4+ T cells (both TH1 cells and TH17 cells) and neutrophils, reduced production of pro-inflammatory cytokines, including IFNγ and IL-6, increased levels of the anti-inflammatory cytokine IL-10 and decreased pro-angiogenic factors107. Overall, RvE1 significantly decreased stromal keratitis. Similar results have been demonstrated for protectin D1 (Ref. 108), further illustrating the potential therapeutic benefits of SPM control of pathogen-mediated inflammation to lessen injury to bystander tissues.
The interaction of the host immune system with infectious insults from viruses represents a novel opportunity for exploitation of SPMs. Finding the delicate balance between the need for a sufficient immune response to clear infection and rapid dampening of that response to prevent host damage is a well-suited target for SPMs, and further research is needed to identify opportunities for optimizing this balance in human viral infectious disease.
SPMs in parasitic infections
Responses to parasitic infections also appear to engage SPMs in host defence. With Toxoplasma gondii, there is a robust DC response with production of IL-12 (Ref. 109). Lipoxins are generated in vivo during toxoplasmosis and act in an autacoid mechanism on DCs via ALX leading to reduction of CCR5 expression and diminished IL-12 production110. In animal models, 5-LOX deficiency results in the production of significantly more IL-2 and IFNγ compared with wild-type animals, as well as severe encephalitis and increased mortality, all of which can be reversed by administration of LXA4 analogues111. Similar protective roles for lipoxins have been suggested for other intracellular and extracellular parasites, including Angiostrongylus costaricensi s112, Plasmodium spp.113 and Trypanosoma cruz i114.
Pathogen–host interactions for SPM biosynthesis
The generation of SPMs may not always be beneficial to the host. As discussed previously in M. tuberculosis infections, experimental models that strongly favour the generation of lipoxins over leukotrienes can have detrimental effects on pathogen clearance. If given early in pharmacologically large amounts, SPM regulation of the pathogen-mediated immune response may impair microbial clearance. In addition, there are now examples identified of select pathogens using local SPM production as an immune evasion and survival strategy. T. gondii is able to generate components of SPM biosynthetic pathways, resulting in local collaboration with host cells to increase lipoxin production with the consequence of a dampened immune response to T. gondi i115. Recruitment of neutrophils, lymphocytes and eosinophils to the site of infection are all decreased by this mechanism115. In addition to T. gondii, the opportunistic bacteria Pseudomonas aeruginosa can express a secreted LOX that can augment SPM production in the local milieu to modulate host defence116. Similarly, Candida albicans can biosynthesize RvE1 that limits IL-8-mediated neutrophil infiltration in the host, enabling colonization117. These examples further illustrate the delicate balance between the pathogen and the host in SPM production and control of host immune responses.
SPMs in chronic inflammatory diseases
Non-infectious inflammation is a common and often devastating cause of human disease. Most current therapies rely on blunting the inappropriate immune response through the use of anti-inflammatory medications, all of which have significant undesirable side effects, including increasing the host susceptibility to infection. Although the roles of SPMs have been investigated in many inflammatory diseases (Table 3), below we focus on the role of SPMs in inflammation of the lung by highlighting data from preclinical animal models.
Table 3. Roles for SPMs in non-pulmonary settings.
| Disease or procedure | Mediator | Role | Refs |
|---|---|---|---|
| Murine models of organ transplantation | Lipoxins | Lipoxin analogue and increased LXA4 receptor expression prolong orthotopic heart transplant survival | 169 |
| Lipoxin prevents acute rejection after liver transplantation | 170 | ||
| Resolvins | RvE1 prolongs survival of vascularized renal transplant | 169 | |
| RvD1 analogue prolongs corneal transplant survival | 171 | ||
| Graft versus host disease | Lipoxins | LXA4 and 15-epi-LXA4 administration improves clinical symptoms | 172 |
| Alzheimer disease | Lipoxins | LXA4 decreases NF-κB expression and recruits microglia, promoting clearance of amyloid-β deposits and improving cognition in mouse models | 173 |
| Protectins | NPD1 promotes brain cell survival and an anti-apoptotic gene expression programme in human tissue | 174 | |
| Resolvins | RvD1 stimulates macrophage phagocytosis of amyloid-β in vitro in PBMCs from patients with Alzheimer disease | 175 | |
| Amyotrophic lateral sclerosis | Resolvins | RvD1 inhibits IL-6 and TNF production in macrophages derived from post mortem samples | 176 |
| Murine models of inflammatory bowel disease or colitis | Lipoxins | 15-epi-LXA4 enhances phagocytic clearance of bacteria and limits the inflammatory cytokine milieu | 177 |
| LXA4, through NF-κB, downregulates pro-inflammatory cytokines and improves mortality | 178 | ||
| Resolvins | RvE1 suppresses pro-inflammatory response of macrophages | 179 | |
| RvE1 blocks leukocyte inflammation and protects against colitis | 157 | ||
| RvD2 and AT-RvD1 decrease neutrophil infiltration and cytokine response, and improves clinical metrics | 180 | ||
| Diabetes | Resolvins | RvD1 improves glucose tolerance and insulin sensitivity associated with obesity-induced diabetes in mice | 181 |
| The RvD1 precursor 17-HDHA reduces adipose tissue inflammation and improves glucose tolerance in mouse models | 182 | ||
| Chronic pancreatitis | Resolvins | RvD1 limits inflammation in the dorsal horn, limiting allodynia in rat models | 183 |
| Murine models of corneal healing | Lipoxins | LXA4 and protectin D1 improve corneal healing and limit tissue injury | 184 |
| Resolvins | RvE1 limits goblet cell loss in chronic dry eye | 185 | |
| RvE1 improves goblet cell function and tear formation and limits inflammation | 186,187,188 | ||
| Retinopathy | Resolvin and protectins | RvD1, RvE1 and protectin D1 all protect against revascularization in mouse models | 189 |
| Glomerulonephritis | Lipoxins | Lipoxin upregulation promotes preservation of function in experimental glomerulonephritis | 190 |
| Renal fibrosis | Lipoxins | LXA4 limits collagen deposition and promotes IL-10 while inhibiting pro-inflammatory cytokines in rat models | 191 |
| Resolvins | In mouse models of ischaemia–reperfusion injury, RvD1 restores function, reduces infiltration of leukocytes and blocks macrophage activation | 160 | |
| RvE1 inhibits fibroblast proliferation in mouse post-obstruction injury models | 192 | ||
| Protectins | In ischaemia–reperfusion injury, protectin D1 restores function, reduces infiltration of leukocytes and blocks macrophage activation | 160 | |
| Arthritis | Lipoxins | LXA4 resolves inflammation mediated by PGE2 in mouse models of autoimmune arthritis | 52 |
| LXA4 receptor agonist decreases histological joint destruction and decreases clinical severity in murine collagen-induced arthritis | 193 | ||
| Resolvins | RvD1 and AT-RvD1 improves hyperalgesia through modulation of NF-κB and COX2 in dorsal root ganglia in rat models of arthritis | 194 | |
| Cardiac reperfusion injury | Resolvins | RvE1 is cardioprotective and limits infarct size in rat cardiac ischaemia models | 195 |
| Atherosclerosis | Lipoxins | Overexpression of 15-lipoxygenase protects against lipid deposition and limits plaque development in rabbit transgenic models | 196 |
| Ischaemic stroke | Resolvins | AT-Resolvins are neuroprotective and limit leukocyte infiltration in mouse stroke models | 197 |
| Atopic dermatitis | Resolvins | RvE1 improves skin lesions through reduction of IL-4, IFNγ and eosinophill infiltration in murine models | 198 |
| Fibromyalgia | Resolvins | RvD2 and AT-RvD1 inhibit allodynia and limit depressive symptoms in a mouse disease model | 199 |
| Inflammatory pain in murine models | Resolvins | RvD1 limits pain and reverse thermal and mechanical injury in inflamed tissue | 200 |
| RvE1 limits inflammation, as well as heat and mechanical pain | 128 | ||
| Protectins | Protectin D1 inhibits capsaicin-induced TRPV1 currents and TNF-dependent pain hypersensitivity | 125 | |
| Maresins | MaR1 inhibits capsaicin-induced TPRV currents and reduces inflammation and chemotherapy-induced pain | 127 |
17-HDHA, 17-hydroxy docosahexaenoic acid; AT, aspirin-triggered; COX2, cyclooxygenase 2; IFNγ, interferon-γ; IL-4, interleukin-4; LXA4, lipoxin A4; MaR1, maresin 1; NF-κB, nuclear factor-κB; NPD1, neuroprotectin D1; PBMC, peripheral blood mononuclear cell; PGE2, prostaglandin E2; RvD, resolvin D; RvE1, resolvin E1; SPM, specialized pro-resolving mediator; TNF, tumour necrosis factor; TRPV, transient receptor potential cation channel subfamily V.
Asthma and allergic inflammation. Asthma is a disease of excessive airway inflammation and hyperresponsiveness induced by irritant triggers and subsequently driven by a multitude of factors, including the trafficking of neutrophils, eosinophils and the generation of type 2 inflammatory responses in many cases. Severe asthma is poorly responsive to existing therapies, and it is characterized by increased oxidative stress and decreased lipoxin production in the airways55,118,119. Recently, the increased oxidative stress in uncontrolled asthma was linked to decreased lipoxin levels through a compensatory increase in soluble epoxide hydrolase activity118. As a consequence of the soluble epoxide hydrolase activity, levels of 14,15-epoxyeicosatrienoic acid levels were decreased, which adversely impacted lipoxin production118, providing a biochemical mechanism for oxidative insults to disrupt lung resolution programmes. Low SPM levels in severe asthma are likely to have the functional consequence of chronic inflammation and airway hyperreactivity because airway LXA4 blunts leukotriene-mediated bronchoprovocation in humans120, and in mice stable analogues of LXA4 block airway hyperresponsiveness, mucus metaplasia and type 2 lung inflammation121,122, and accelerate resolution of the inflammatory response73.
RvE1 has protective effects in preclinical models of allergic lung inflammation; it decreases eosinophil recruitment, type 2 cytokine production and airway hyperresponsiveness73,123. RvE1 targets NK cells in mouse models of asthma through the RvE1 receptor CMKLR1, promoting NK cell migration and cytotoxicity. With NK cell depletion, the pro-resolving function of RvE1 is partially impaired68. In allergic inflammation, RvE1 increases lipoxin formation, suggesting the possibility of redundant pathway effects to limit chronic inflammation. RvE1 inhibits IL-6, IL-23 and IL-17 release, thereby dampening the development and activation of TH17 cells. Similarly to RvE1, lipoxins can inhibit IL-17 production but do not inhibit IL-23, which is indicative of convergent but not overlapping signalling pathways. Of note, as mentioned above, RvE1 and LXA4 also engage distinct receptors, namely CMKLR1 and ALX, respectively73. RvD1 acts in a complementary manner, similarly promoting the resolution of eosinophil tissue accumulation and pro-inflammatory responses with a macrophage directed action to enhance allergen phagocytosis and clearance63. Similarly, protectin D1 has been shown to promote resolution of the lung inflammatory response and block airway hyperresponsiveness47. Of interest, protectin D1 regulates IL-5 and IL-13 but not IL-4 levels, suggesting that ILC2s rather than TH2 cells are likely to be a principal cellular target for protectin D1. It is notable that protectin D1 levels are decreased in exhaled breath condensates during asthma exacerbations47.
Recently, lung sensory neurons were identified as early inducers of ILC2 activation in type 2 lung inflammation124. These activated neurons express transient receptor potential (TRP) channels, which can serve as SPM targets. Of note, mouse models have suggested a role for RvD1, RvE1, neuroprotectin D1 (NPD1) and MaR1 in attenuating pain by inhibition of TRP channels125,126,127,128. Because SPMs act at these pain receptors in the nervous system and on inflammatory pathways, these findings suggest that regulation of sensory neuron activation could be a crucial mechanism for SPM inhibition of both pain and lung inflammation. Together, these findings highlight an integrated network of pro-resolving mediators in asthma and allergic inflammation and suggest several potential therapeutic targets.
Chronic obstructive pulmonary disease. Chronic obstructive pulmonary disease (COPD) is a pulmonary inflammatory disease most often triggered by cigarette smoke and propagated through maladaptive and prolonged pro-inflammatory responses, predisposing the host to recurrent infections. Pro-inflammatory lipid mediators, including leukotrienes, have been observed at elevated levels in patients with COPD119. Roles for SPMs remain to be determined in these individuals. In addition to LXA4, the acute phase reactant serum amyloid A (SAA) can also interact with ALX, and it is increased in COPD exacerbations27, which are largely caused by viral and bacterial respiratory tract infections. In acute exacerbations of COPD, levels of SAA are more than 2 log orders higher than LXA4 (Ref. 27). In sharp contrast to LXA4, when SAA engages ALX, it triggers a pro-inflammatory, neutrophil driven response. Although SAA-mediated inflammation is glucocorticoid-resistant, it can be regulated by pharmacological dosing of lipoxins27, suggesting a new therapeutic approach for steroid-resistant lung inflammation.
The role of resolvins in COPD is a subject of active investigation. Cigarette smoke exposure results in the development of classically activated macrophages, which produce a pro-inflammatory response. Alternatively activated, or M2, macrophages also play a part in the clearance of inhaled particles and quelling of the initial response to the cigarette smoke. RvD1 polarizes cigarette smoke-exposed macrophages towards the M2 pathway, resulting in enhanced phagocytosis as well as upregulated production of IL-10 (Ref. 64). RvE1 also acts on cigarette smoke-activated macrophages, reducing superoxide production and limiting inflammation129. The ability of resolvins to polarize the macrophage population towards the M2 phenotype suggests a novel mechanism for SPM control in this chronic inflammatory disorder.
Cystic fibrosis. Cystic fibrosis is a genetic disorder with multi-organ defects caused by a single mutation. Patients with cystic fibrosis have viscous respiratory tract secretions, recurrent airway infections and an over-exuberant immune response, eventually resulting in the deterioration of lung function. Genetic modifier analysis suggests that patients with cystic fibrosis who carry a polymorphism in PTGS2 (encoding COX2) that leads to reduced production of pro-inflammatory mediators have improved clinical status130. Profiling of lipid mediators in the airways of patients with cystic fibrosis showed that lipoxin levels may be lower in these patients compared with healthy control subjects54. Moreover, patients with cystic fibrosis who had detectable levels of RvE1 in the airways showed improved lung function compared with patients without any detectable RvE1 (Ref. 131). Furthermore, in animal models of cystic fibrosis, lipoxin administration suppresses neutrophil infiltration and reduces bacterial burden, resulting in an overall reduction in disease severity54.
Fibrotic lung disease. Multiple pulmonary injurious exposures have a unifying endpoint in the development of extensive tissue scarring, resulting in poor gas exchange, air movement and demise of the host. These fibrotic lung diseases can be mediated by a poorly controlled inflammatory response that triggers a fibrotic response in a maladaptive attempt to heal the damaged lung parenchyma. These diseases represent a devastating human burden, as very few treatments exist to slow or reverse this fibrotic process. Pro-resolving mediators could represent a novel strategy in a sparse arsenal. Bleomycin is an important chemotherapeutic agent but carries a known risk of pulmonary fibrosis. Treatment with LXA4 or 15-epi-LXA4 results in an attenuation of pulmonary fibrosis in animals exposed to bleomycin through reduction of the pro-fibrotic cytokine TGFβ132, as well as an increase in the prevalence of M2 macrophages133, both resulting in decrease fibrotic matrix and improved pulmonary function. In humans, scleroderma lung disease is characterized by idiopathic progressive lung inflammation and fibrosis and, of interest, patients with scleroderma lung disease underproduce pro-resolving mediators, in comparison to their pro-inflammatory counterparts134.
Acute respiratory distress syndrome. ARDS is a prevalent condition with high rates of morbidity and mortality. It is characterized by an overly robust inflammatory response to infection (for example, pneumonia and sepsis) or injury that fills the alveoli with oedema and pus, resulting in life-threatening respiratory failure. Many unsuccessful attempts have been made to therapeutically target an inflammatory pathway to limit this over-exuberant host response. In contrast to these anti-inflammatory strategies, a pro-resolving therapeutic strategy directed at harnessing host pro-resolving mechanisms is showing promise in preclinical model systems. Using a sterile model of ARDS from gastric acid aspiration, an important clinical risk factor for ARDS, several SPMs, including LXA4, 15-epi-LXA4, RvE1, RvD1 and MaR1, have proven effective as pharmacological agents in limiting acute lung inflammation and injury, and accelerating lung tissue catabasis13,29,59,60,135. Because SPMs engage endogenous resolution pathways, these mediators have the potential to both decrease pathogen-mediated inflammation and enhance host defence, which distinguishes SPMs from immunosuppressive agents. Early inflammation in ARDS is mediated by platelet–neutrophil interactions59,136, and this interaction can lead to transcellular production of lipoxins or of the most recently discovered member of the SPM family, MaR1 (Ref. 59). Treatment with MaR1 is organ protective and limits the extent of lung inflammation. Furthermore, the timing of MaR1 production appears specific and regulated, as does the production of RvD1 (Ref. 137). Together, these findings highlight the potential roles SPMs could have in decreasing the severity and duration of ARDS and, more generally, the data support a targeted pro-resolving approach as a new therapeutic strategy for this devastating condition that is currently without available medical treatment.
Human translation
As momentum grows to leverage these natural resolution pathways for rational new therapeutic strategies for diseases of acute and chronic inflammation, it is essential to clarify the roles of SPMs in human host defence and in the regulation of pathogen-mediated inflammation. As discussed above, preclinical data for bacterial infection points to important and pivotal roles for lipid mediators, in particular SPMs, in the regulation of host responses to infection12,13 with the potential for host SPM-directed interventions to decrease antibiotic requirements12,95. In addition, for viral host responses, SPMs lessened the severity of influenza and HSV infections102,107,108. Several lines of evidence have suggested dysregulation of SPM pathways in several human diseases27,47,55.
Clinical trials with SPM analogues that resist metabolic inactivation are still in early phases. A recent study of children with infantile eczema compared a topical stable LXA4 analogue (15-(R/S)-methyl-LXA4) to the current clinical approach of topical corticosteroids (specifically, mometasone). 15-(R/S)-methyl-LXA4 was well tolerated and controlled clinical symptoms and disease as effectively as topical steroids138. This trial is the first to report successful treatment with an SPM in humans. Moreover, for allergic diseases, inhaled LXA4 decreases LTC4-initiated bronchoprovocation in patients with asthma120. Several clinical trials using a topical formulation of an RvE1 analogue for ocular conditions are also underway (NCT01639846, NCT01675570, NCT00799552 and NCT02329743).
Conclusion
Host responses to infection naturally trigger both an acute inflammatory response and its resolution. Counter-regulation of pathogen-mediated inflammation is an active process with specific cellular and biochemical events that are tightly regulated in health. With the identification of several families of endogenous pro-resolving mediators, their potent anti-inflammatory properties are now being determined. Distinct from immunosuppressive agents, these endogenous pro-resolving mediators generally display protective actions in host defence, including direct antimicrobial actions. There is still much to be done to more fully understand the intersection of these novel endogenous pathways in control of pathogen-mediated inflammation and the diversity of their mechanisms in microbial pathogenesis. The abundant presence of SPMs in human healthy breast milk139 suggests important protective actions for these mediators. Clinically, acute infections are principally treated with antibiotics with current approaches devoid of host-directed therapy. In light of the current serious threat of emerging pathogens, in particular those that display antibiotic resistance, the development of therapies to augment host anti-infective mechanisms are needed. Members of the growing new genus of SPMs or their bioactive stable analogues represent potential candidates to harness endogenous anti-inflammatory resolution mechanisms to limit overly exuberant pathogen-mediated inflammation in future therapeutic strategies.
Acknowledgements
he authors wish to acknowledge C. N. Serhan for his helpful advice in the preparation of this manuscript. This work was funded in part by US National Institutes of Health grants HL122531, U10HL109172, U01HL108712 and P01GM095467.
Glossary
- Catabasis
An active process at the cellular and tissue level governed by specific mediators that promote a return to tissue homeostasis.
- Efferocytosis
The cellular process by which phagocytes engulf dying and dead cells (for example, apoptotic or necrotic) for removal from tissues. It is part of the resolution programme to restore tissue homeostasis.
Biographies
Maria C. Basil completed her M.D. and Ph.D. at the Perelman School of Medicine at the University of Pennsylvania, USA, where she worked on the mechanisms of asymmetric cell division in T cell immune responses. She is now a resident at Brigham and Women's Hospital, Boston, Massachusetts, USA, in the Department of Medicine.
Bruce D. Levy is the Parker B. Francis Professor of Medicine at Harvard Medical School and Chief of Pulmonary and Critical Care Medicine at Brigham and Women's Hospital, Boston, Massachusetts, USA. The research in his laboratory is focused on endogenous mediators and mechanisms for the resolution of lung inflammation, infection and injury. Bruce D. Levy's hopmepage
Related links
DATABASES
PowerPoint slides
Competing interests
B.D.L. is a co-inventor on patents assigned to Brigham and Women's Hospital; some of these patents (those pertaining to resolvins) are licensed to Resolvyx Pharmaceuticals. The interests of B.D.L. were reviewed and are managed by the Brigham and Women's Hospital and Partners HealthCare in accordance with their conflict-of-interest policies.
References
- 1.Nathan C. Points of control in inflammation. Nature. 2002;420:846–852. doi: 10.1038/nature01320. [DOI] [PubMed] [Google Scholar]
- 2.Vaporciyan AA, et al. Involvement of platelet-endothelial cell adhesion molecule-1 in neutrophil recruitment in vivo. Science. 1993;262:1580–1582. doi: 10.1126/science.8248808. [DOI] [PubMed] [Google Scholar]
- 3.Mizgerd JP. Acute lower respiratory tract infection. New Engl. J. Med. 2008;358:716–727. doi: 10.1056/NEJMra074111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Serhan CN. Pro-resolving lipid mediators are leads for resolution physiology. Nature. 2014;510:92–101. doi: 10.1038/nature13479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Serhan CN, Dalli J, Colas RA, Winkler JW, Chiang N. Protectins and maresins: new pro-resolving families of mediators in acute inflammation and resolution bioactive metabolome. Biochim. Biophys. Acta. 2015;1851:397–413. doi: 10.1016/j.bbalip.2014.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Serhan CN, Savill J. Resolution of inflammation: the beginning programs the end. Nat. Immunol. 2005;6:1191–1197. doi: 10.1038/ni1276. [DOI] [PubMed] [Google Scholar]
- 7.Buckley CD, Gilroy DW, Serhan CN. Proresolving lipid mediators and mechanisms in the resolution of acute inflammation. Immunity. 2014;40:315–327. doi: 10.1016/j.immuni.2014.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Savill J. Apoptosis. Phagocytic docking without shocking. Nature. 1998;392:442–443. doi: 10.1038/33025. [DOI] [PubMed] [Google Scholar]
- 9.Dalli J, Serhan CN. Specific lipid mediator signatures of human phagocytes: microparticles stimulate macrophage efferocytosis and pro-resolving mediators. Blood. 2012;120:e60–e72. doi: 10.1182/blood-2012-04-423525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Freire-de-Lima CG, et al. Apoptotic cells, through transforming growth factor-β, coordinately induce anti-inflammatory and suppress pro-inflammatory eicosanoid and NO synthesis in murine macrophages. J. Biol. Chem. 2006;281:38376–38384. doi: 10.1074/jbc.M605146200. [DOI] [PubMed] [Google Scholar]
- 11.Bannenberg GL, et al. Molecular circuits of resolution: formation and actions of resolvins and protectins. J. Immunol. 2005;174:4345–4355. doi: 10.4049/jimmunol.174.7.4345. [DOI] [PubMed] [Google Scholar]
- 12.Chiang N, et al. Infection regulates pro-resolving mediators that lower antibiotic requirements. Nature. 2012;484:524–528. doi: 10.1038/nature11042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seki H, et al. The anti-inflammatory and proresolving mediator resolvin E1 protects mice from bacterial pneumonia and acute lung injury. J. Immunol. 2010;184:836–843. doi: 10.4049/jimmunol.0901809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Spite M, et al. Resolvin D2 is a potent regulator of leukocytes and controls microbial sepsis. Nature. 2009;461:1287–1291. doi: 10.1038/nature08541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tobin DM, et al. Host genotype-specific therapies can optimize the inflammatory response to mycobacterial infections. Cell. 2012;148:434–446. doi: 10.1016/j.cell.2011.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Perretti M, D'Acquisto F. Annexin A1 and glucocorticoids as effectors of the resolution of inflammation. Nat. Rev. Immunol. 2009;9:62–70. doi: 10.1038/nri2470. [DOI] [PubMed] [Google Scholar]
- 17.Savill J, Dransfield I, Gregory C, Haslett C. A blast from the past: clearance of apoptotic cells regulates immune responses. Nat. Rev. Immunol. 2002;2:965–975. doi: 10.1038/nri957. [DOI] [PubMed] [Google Scholar]
- 18.Wallace JL, Ianaro A, Flannigan KL, Cirino G. Gaseous mediators in resolution of inflammation. Semin. Immunol. 2015;3:227–233. doi: 10.1016/j.smim.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 19.Gilroy DW, De Maeyer R. New insights into the resolution of inflammation. Semin. Immunol. 2015;3:161–168. doi: 10.1016/j.smim.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 20.Romano M, Cianci E, Simiele F, Recchiuti A. Lipoxins and aspirin-triggered lipoxins in resolution of inflammation. Eur. J. Pharmacol. 2015;760:49–63. doi: 10.1016/j.ejphar.2015.03.083. [DOI] [PubMed] [Google Scholar]
- 21.Viola J, Soehnlein O. Atherosclerosis – a matter of unresolved inflammation. Semin. Immunol. 2015;3:184–193. doi: 10.1016/j.smim.2015.03.013. [DOI] [PubMed] [Google Scholar]
- 22.Kasuga K, et al. Rapid appearance of resolvin precursors in inflammatory exudates: novel mechanisms in resolution. J. Immunol. 2008;181:8677–8687. doi: 10.4049/jimmunol.181.12.8677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Badr KF, DeBoer DK, Schwartzberg M, Serhan CN. Lipoxin A4 antagonizes cellular and in vivo actions of leukotriene D4 in rat glomerular mesangial cells: evidence for competition at a common receptor. Proc. Natl Acad. Sci. USA. 1989;86:3438–3442. doi: 10.1073/pnas.86.9.3438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Malawista SE, de Boisfleury Chevance A, van Damme J, Serhan CN. Tonic inhibition of chemotaxis in human plasma. Proc. Natl Acad. Sci. USA. 2008;105:17949–17954. doi: 10.1073/pnas.0802572105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dinarello CA, Simon A, van der Meer JW. Treating inflammation by blocking interleukin-1 in a broad spectrum of diseases. Nat. Rev. Drug Discov. 2012;11:633–652. doi: 10.1038/nrd3800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Levy BD, Clish CB, Schmidt B, Gronert K, Serhan CN. Lipid mediator class switching during acute inflammation: signals in resolution. Nat. Immunol. 2001;2:612–619. doi: 10.1038/89759. [DOI] [PubMed] [Google Scholar]
- 27.Bozinovski S, et al. Serum amyloid A opposes lipoxin A4 to mediate glucocorticoid refractory lung inflammation in chronic obstructive pulmonary disease. Proc. Natl Acad. Sci. USA. 2012;109:935–940. doi: 10.1073/pnas.1109382109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dufton N, et al. Anti-inflammatory role of the murine formyl-peptide receptor 2: ligand-specific effects on leukocyte responses and experimental inflammation. J. Immunol. 2010;184:2611–2619. doi: 10.4049/jimmunol.0903526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fukunaga K, Kohli P, Bonnans C, Fredenburgh LE, Levy BD. Cyclooxygenase 2 plays a pivotal role in the resolution of acute lung injury. J. Immunol. 2005;174:5033–5039. doi: 10.4049/jimmunol.174.8.5033. [DOI] [PubMed] [Google Scholar]
- 30.Schwab JM, Chiang N, Arita M, Serhan CN. Resolvin E1 and protectin D1 activate inflammation-resolution programmes. Nature. 2007;447:869–874. doi: 10.1038/nature05877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Serhan CN, Petasis NA. Resolvins and protectins in inflammation resolution. Chem. Rev. 2011;111:5922–5943. doi: 10.1021/cr100396c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Serhan CN, Sheppard KA. Lipoxin formation during human neutrophil-platelet interactions. Evidence for the transformation of leukotriene A4 by platelet 12-lipoxygenase in vitro. J. Clin. Invest. 1990;85:772–780. doi: 10.1172/JCI114503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Levy BD, et al. Human alveolar macrophages have 15-lipoxygenase and generate 15(S)-hydroxy-5,8,11-cis-13-trans-eicosatetraenoic acid and lipoxins. J. Clin. Invest. 1993;92:1572–1579. doi: 10.1172/JCI116738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Serhan CN, Hamberg M, Samuelsson B. Lipoxins: novel series of biologically active compounds formed from arachidonic acid in human leukocytes. Proc. Natl Acad. Sci. USA. 1984;81:5335–5339. doi: 10.1073/pnas.81.17.5335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Claria J, Serhan CN. Aspirin triggers previously undescribed bioactive eicosanoids by human endothelial cell-leukocyte interactions. Proc. Natl Acad. Sci. USA. 1995;92:9475–9479. doi: 10.1073/pnas.92.21.9475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Claria J, Lee MH, Serhan CN. Aspirin-triggered lipoxins (15-epi-LX) are generated by the human lung adenocarcinoma cell line (A549)-neutrophil interactions and are potent inhibitors of cell proliferation. Mol. Med. 1996;2:583–596. [PMC free article] [PubMed] [Google Scholar]
- 37.Chiang N, et al. Aspirin-triggered 15-epi-lipoxin A4 (ATL) generation by human leukocytes and murine peritonitis exudates: development of a specific 15-epi-LXA4 ELISA. J. Pharmacol. Exp. Ther. 1998;287:779–790. [PubMed] [Google Scholar]
- 38.Serhan CN. The resolution of inflammation: the devil in the flask and in the details. FASEB J. 2011;25:1441–1448. doi: 10.1096/fj.11-0502ufm. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Serhan CN, et al. Resolvins: a family of bioactive products of omega-3 fatty acid transformation circuits initiated by aspirin treatment that counter proinflammation signals. J. Exp. Med. 2002;196:1025–1037. doi: 10.1084/jem.20020760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Serhan CN, et al. Novel functional sets of lipid-derived mediators with antiinflammatory actions generated from omega-3 fatty acids via cyclooxygenase 2-nonsteroidal anti-inflammatory drugs and transcellular processing. J. Exp. Med. 2000;192:1197–1204. doi: 10.1084/jem.192.8.1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Arita M, et al. Stereochemical assignment, antiinflammatory properties, and receptor for the omega-3 lipid mediator resolvin E1. J. Exp. Med. 2005;201:713–722. doi: 10.1084/jem.20042031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Serhan CN, Arita M, Hong S, Gotlinger K. Resolvins, docosatrienes, and neuroprotectins, novel omega-3-derived mediators, and their endogenous aspirin-triggered epimers. Lipids. 2004;39:1125–1132. doi: 10.1007/s11745-004-1339-7. [DOI] [PubMed] [Google Scholar]
- 43.Hong S, Gronert K, Devchand PR, Moussignac RL, Serhan CN. Novel docosatrienes and 17S-resolvins generated from docosahexaenoic acid in murine brain, human blood, and glial cells. Autacoids in anti-inflammation. J. Biol. Chem. 2003;278:14677–14687. doi: 10.1074/jbc.M300218200. [DOI] [PubMed] [Google Scholar]
- 44.Serhan CN, et al. Maresins: novel macrophage mediators with potent antiinflammatory and proresolving actions. J. Exp. Med. 2009;206:15–23. doi: 10.1084/jem.20081880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Serhan CN, et al. Anti-inflammatory actions of neuroprotectin D1/protectin D1 and its natural stereoisomers: assignments of dihydroxy-containing docosatrienes. J. Immunol. 2006;176:1848–1859. doi: 10.4049/jimmunol.176.3.1848. [DOI] [PubMed] [Google Scholar]
- 46.Freedman SD, et al. Association of cystic fibrosis with abnormalities in fatty acid metabolism. N. Engl. J. Med. 2004;350:560–569. doi: 10.1056/NEJMoa021218. [DOI] [PubMed] [Google Scholar]
- 47.Levy BD, et al. Protectin D1 is generated in asthma and dampens airway inflammation and hyperresponsiveness. J. Immunol. 2007;178:496–502. doi: 10.4049/jimmunol.178.1.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chiang N, Dalli J, Colas RA, Serhan CN. Identification of resolvin D2 receptor mediating resolution of infections and organ protection. J. Exp. Med. 2015;212:1203–1217. doi: 10.1084/jem.20150225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Krishnamoorthy S, et al. Resolvin D1 binds human phagocytes with evidence for proresolving receptors. Proc. Natl Acad. Sci. USA. 2010;107:1660–1665. doi: 10.1073/pnas.0907342107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Krishnamoorthy S, Recchiuti A, Chiang N, Fredman G, Serhan CN. Resolvin D1 receptor stereoselectivity and regulation of inflammation and proresolving microRNAs. Am. J. Pathol. 2012;180:2018–2027. doi: 10.1016/j.ajpath.2012.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Recchiuti A, Krishnamoorthy S, Fredman G, Chiang N, Serhan CN. MicroRNAs in resolution of acute inflammation: identification of novel resolvin D1-miRNA circuits. FASEB J. 2011;25:544–560. doi: 10.1096/fj.10-169599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chan MM, Moore AR. Resolution of inflammation in murine autoimmune arthritis is disrupted by cyclooxygenase-2 inhibition and restored by prostaglandin E2-mediated lipoxin A4 production. J. Immunol. 2010;184:6418–6426. doi: 10.4049/jimmunol.0903816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gilroy DW, et al. Inducible cyclooxygenase may have anti-inflammatory properties. Nat. Med. 1999;5:698–701. doi: 10.1038/9550. [DOI] [PubMed] [Google Scholar]
- 54.Karp CL, et al. Defective lipoxin-mediated anti-inflammatory activity in the cystic fibrosis airway. Nat. Immunol. 2004;5:388–392. doi: 10.1038/ni1056. [DOI] [PubMed] [Google Scholar]
- 55.Levy BD, et al. Diminished lipoxin biosynthesis in severe asthma. Am. J. Respir. Crit. Care Med. 2005;172:824–830. doi: 10.1164/rccm.200410-1413OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shinohara M, et al. Cell-cell interactions and bronchoconstrictor eicosanoid reduction with inhaled carbon monoxide and resolvin D1. Am. J. Physiol. Lung Cell. Mol. Physiol. 2014;307:L746–L757. doi: 10.1152/ajplung.00166.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Leitch AE, et al. Cyclin-dependent kinases 7 and 9 specifically regulate neutrophil transcription and their inhibition drives apoptosis to promote resolution of inflammation. Cell Death Differ. 2012;19:1950–1961. doi: 10.1038/cdd.2012.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Maderna P, Godson C. Lipoxins: resolutionary road. Br. J. Pharmacol. 2009;158:947–959. doi: 10.1111/j.1476-5381.2009.00386.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Abdulnour RE, et al. Maresin 1 biosynthesis during platelet-neutrophil interactions is organ-protective. Proc. Natl Acad. Sci. USA. 2014;111:16526–16531. doi: 10.1073/pnas.1407123111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Eickmeier O, et al. Aspirin-triggered resolvin D1 reduces mucosal inflammation and promotes resolution in a murine model of acute lung injury. Mucosal Immunol. 2013;6:256–266. doi: 10.1038/mi.2012.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hasturk H, et al. Resolvin E1 regulates inflammation at the cellular and tissue level and restores tissue homeostasis in vivo. J. Immunol. 2007;179:7021–7029. doi: 10.4049/jimmunol.179.10.7021. [DOI] [PubMed] [Google Scholar]
- 62.Godson C, et al. Cutting edge: lipoxins rapidly stimulate nonphlogistic phagocytosis of apoptotic neutrophils by monocyte-derived macrophages. J. Immunol. 2000;164:1663–1667. doi: 10.4049/jimmunol.164.4.1663. [DOI] [PubMed] [Google Scholar]
- 63.Rogerio AP, et al. Resolvin D1 and aspirin-triggered resolvin D1 promote resolution of allergic airways responses. J. Immunol. 2012;189:1983–1991. doi: 10.4049/jimmunol.1101665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hsiao HM, et al. A novel anti-inflammatory and pro-resolving role for resolvin D1 in acute cigarette smoke-induced lung inflammation. PLoS ONE. 2013;8:e58258. doi: 10.1371/journal.pone.0058258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Palmer CD, et al. 17(R)-Resolvin D1 differentially regulates TLR4-mediated responses of primary human macrophages to purified LPS and live E. coli. J. Leukocyte Biol. 2011;90:459–470. doi: 10.1189/jlb.0311145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Thoren FB, et al. Human NK Cells induce neutrophil apoptosis via an NKp46- and Fas-dependent mechanism. J. Immunol. 2012;188:1668–1674. doi: 10.4049/jimmunol.1102002. [DOI] [PubMed] [Google Scholar]
- 67.Barnig C, et al. Lipoxin A4 regulates natural killer cell and type 2 innate lymphoid cell activation in asthma. Sci. Transl Med. 2013;5:174ra26. doi: 10.1126/scitranslmed.3004812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Haworth O, Cernadas M, Levy BD. NK cells are effectors for resolvin E1 in the timely resolution of allergic airway inflammation. J. Immunol. 2011;186:6129–6135. doi: 10.4049/jimmunol.1004007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Molofsky AB, et al. Innate lymphoid type 2 cells sustain visceral adipose tissue eosinophils and alternatively activated macrophages. J. Exp. Med. 2013;210:535–549. doi: 10.1084/jem.20121964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Krishnamoorthy N, et al. Cutting edge: maresin-1 engages regulatory T cells to limit type 2 innate lymphoid cell activation and promote resolution of lung inflammation. J. Immunol. 2015;194:863–867. doi: 10.4049/jimmunol.1402534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Monticelli LA, et al. Innate lymphoid cells promote lung-tissue homeostasis after infection with influenza virus. Nat. Immunol. 2011;12:1045–1054. doi: 10.1031/ni.2131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ariel A, et al. Apoptotic neutrophils and T cells sequester chemokines during immune response resolution through modulation of CCR5 expression. Nat. Immunol. 2006;7:1209–1216. doi: 10.1038/ni1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Haworth O, Cernadas M, Yang R, Serhan CN, Levy BD. Resolvin E1 regulates interleukin 23, interferon-γ and lipoxin A4 to promote the resolution of allergic airway inflammation. Nat. Immunol. 2008;9:873–879. doi: 10.1038/ni.1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ramon S, et al. The specialized proresolving mediator 17-HDHA enhances the antibody-mediated immune response against influenza virus: a new class of adjuvant? J. Immunol. 2014;193:6031–6040. doi: 10.4049/jimmunol.1302795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Colgan SP, Serhan CN, Parkos CA, Delp-Archer C, Madara JL. Lipoxin A4 modulates transmigration of human neutrophils across intestinal epithelial monolayers. J. Clin. Invest. 1993;92:75–82. doi: 10.1172/JCI116601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lawrence DW, et al. Antiadhesive role of apical decay-accelerating factor (CD55) in human neutrophil transmigration across mucosal epithelia. J. Exp. Med. 2003;198:999–1010. doi: 10.1084/jem.20030380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bonnans C, Fukunaga K, Levy MA, Levy BD. Lipoxin A4 regulates bronchial epithelial cell responses to acid injury. Am. J. Pathol. 2006;168:1064–1072. doi: 10.2353/ajpath.2006.051056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Campbell EL, et al. Resolvin E1-induced intestinal alkaline phosphatase promotes resolution of inflammation through LPS detoxification. Proc. Natl Acad. Sci. USA. 2010;107:14298–14303. doi: 10.1073/pnas.0914730107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Canny G, et al. Lipid mediator-induced expression of bactericidal permeability-increasing protein (BPI) in human mucosal epithelia. Proc. Natl Acad. Sci. USA. 2002;99:3902–3907. doi: 10.1073/pnas.052533799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.El Kebir D, et al. 15-epi-lipoxin A4 inhibits myeloperoxidase signaling and enhances resolution of acute lung injury. Am. J. Respir. Crit. Care Med. 2009;180:311–319. doi: 10.1164/rccm.200810-1601OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.El Kebir D, Gjorstrup P, Filep JG. Resolvin E1 promotes phagocytosis-induced neutrophil apoptosis and accelerates resolution of pulmonary inflammation. Proc. Natl Acad. Sci. USA. 2012;109:14983–14988. doi: 10.1073/pnas.1206641109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Amar S, et al. Periodontal disease is associated with brachial artery endothelial dysfunction and systemic inflammation. Arterioscler. Thromb. Vasc. Biol. 2003;23:1245–1249. doi: 10.1161/01.ATV.0000078603.90302.4A. [DOI] [PubMed] [Google Scholar]
- 83.Jain A, et al. Role for periodontitis in the progression of lipid deposition in an animal model. Infect. Immun. 2003;71:6012–6018. doi: 10.1128/IAI.71.10.6012-6018.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Pouliot M, Clish CB, Petasis NA, Van Dyke TE, Serhan CN. Lipoxin A4 analogues inhibit leukocyte recruitment to Porphyromonas gingivalis: a role for cyclooxygenase-2 and lipoxins in periodontal disease. Biochemistry. 2000;39:4761–4768. doi: 10.1021/bi992551b. [DOI] [PubMed] [Google Scholar]
- 85.Serhan CN, et al. Reduced inflammation and tissue damage in transgenic rabbits overexpressing 15-lipoxygenase and endogenous anti-inflammatory lipid mediators. J. Immunol. 2003;171:6856–6865. doi: 10.4049/jimmunol.171.12.6856. [DOI] [PubMed] [Google Scholar]
- 86.Borgeson E, et al. Lipoxin A4 inhibits Porphyromonas gingivalis-induced aggregation and reactive oxygen species production by modulating neutrophil-platelet interaction and CD11b expression. Infect. Immun. 2011;79:1489–1497. doi: 10.1128/IAI.00777-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hasturk H, et al. RvE1 protects from local inflammation and osteoclast- mediated bone destruction in periodontitis. FASEB J. 2006;20:401–403. doi: 10.1096/fj.05-4724fje. [DOI] [PubMed] [Google Scholar]
- 88.Oh SF, Pillai PS, Recchiuti A, Yang R, Serhan CN. Pro-resolving actions and stereoselective biosynthesis of 18S E-series resolvins in human leukocytes and murine inflammation. J. Clin. Invest. 2011;121:569–581. doi: 10.1172/JCI42545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hong S, et al. Resolvin E1 metabolome in local inactivation during inflammation-resolution. J. Immunol. 2008;180:3512–3519. doi: 10.4049/jimmunol.180.5.3512. [DOI] [PubMed] [Google Scholar]
- 90.Fredman G, et al. Impaired phagocytosis in localized aggressive periodontitis: rescue by Resolvin E1. PLoS ONE. 2011;6:e24422. doi: 10.1371/journal.pone.0024422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Blaho VA, Zhang Y, Hughes-Hanks JM, Brown CR. 5-Lipoxygenase-deficient mice infected with Borrelia burgdorferi develop persistent arthritis. J. Immunol. 2011;186:3076–3084. doi: 10.4049/jimmunol.1003473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bafica A, et al. Host control of Mycobacterium tuberculosis is regulated by 5-lipoxygenase-dependent lipoxin production. J. Clin. Invest. 2005;115:1601–1606. doi: 10.1172/JCI23949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Herb F, et al. ALOX5 variants associated with susceptibility to human pulmonary tuberculosis. Hum. Mol. Genet. 2008;17:1052–1060. doi: 10.1093/hmg/ddm378. [DOI] [PubMed] [Google Scholar]
- 94.Tobin DM, et al. The lta4h locus modulates susceptibility to mycobacterial infection in zebrafish and humans. Cell. 2010;140:717–730. doi: 10.1016/j.cell.2010.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ueda T, et al. Combination therapy of 15-epi-lipoxin A4 with antibiotics protects mice from Escherichia coli-induced sepsis*. Crit. Care Med. 2014;42:e288–e295. doi: 10.1097/CCM.0000000000000162. [DOI] [PubMed] [Google Scholar]
- 96.Walker J, et al. Lipoxin a4 increases survival by decreasing systemic inflammation and bacterial load in sepsis. Shock. 2011;36:410–416. doi: 10.1097/SHK.0b013e31822798c1. [DOI] [PubMed] [Google Scholar]
- 97.Sordi R, et al. Dual role of lipoxin A4 in pneumosepsis pathogenesis. Int. Immunopharmacol. 2013;17:283–292. doi: 10.1016/j.intimp.2013.06.010. [DOI] [PubMed] [Google Scholar]
- 98.Cilloniz C, et al. Lethal dissemination of H5N1 influenza virus is associated with dysregulation of inflammation and lipoxin signaling in a mouse model of infection. J. Virol. 2010;84:7613–7624. doi: 10.1128/JVI.00553-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Tam VC, et al. Lipidomic profiling of influenza infection identifies mediators that induce and resolve inflammation. Cell. 2013;154:213–227. doi: 10.1016/j.cell.2013.05.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Baillie JK, Digard P. Influenza—time to target the host? New Engl. J. Med. 2013;369:191–193. doi: 10.1056/NEJMcibr1304414. [DOI] [PubMed] [Google Scholar]
- 101.Imai Y. Role of omega-3 PUFA-derived mediators, the protectins, in influenza virus infection. Biochim. Biophys. Acta. 2015;1851:496–502. doi: 10.1016/j.bbalip.2015.01.006. [DOI] [PubMed] [Google Scholar]
- 102.Morita M, et al. The lipid mediator protectin D1 inhibits influenza virus replication and improves severe influenza. Cell. 2013;153:112–125. doi: 10.1016/j.cell.2013.02.027. [DOI] [PubMed] [Google Scholar]
- 103.Ng S, et al. Effects of oseltamivir treatment on duration of clinical illness and viral shedding and household transmission of influenza virus. Clin. Infect. Dis. 2010;50:707–714. doi: 10.1086/650458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Shirey KA, et al. Control of RSV-induced lung injury by alternatively activated macrophages is IL-4Rα-, TLR4-, and IFN-β-dependent. Mucosal Immunol. 2010;3:291–300. doi: 10.1038/mi.2010.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Richardson JY, et al. Respiratory syncytial virus (RSV) infection induces cyclooxygenase 2: a potential target for RSV therapy. J. Immunol. 2005;174:4356–4364. doi: 10.4049/jimmunol.174.7.4356. [DOI] [PubMed] [Google Scholar]
- 106.Shirey KA, et al. Role of the lipoxygenase pathway in RSV-induced alternatively activated macrophages leading to resolution of lung pathology. Mucosal Immunol. 2014;7:549–557. doi: 10.1038/mi.2013.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Rajasagi NK, et al. Controlling herpes simplex virus-induced ocular inflammatory lesions with the lipid-derived mediator resolvin E1. J. Immunol. 2011;186:1735–1746. doi: 10.4049/jimmunol.1003456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Rajasagi NK, Reddy PB, Mulik S, Gjorstrup P, Rouse BT. Neuroprotectin D1 reduces the severity of herpes simplex virus-induced corneal immunopathology. Invest. Ophthalmol. Visual Sci. 2013;54:6269–6279. doi: 10.1167/iovs.13-12152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Reis e Sousa C, et al. In vivo microbial stimulation induces rapid CD40 ligand-independent production of interleukin 12 by dendritic cells and their redistribution to T cell areas. J. Exp. Med. 1997;186:1819–1829. doi: 10.1084/jem.186.11.1819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Aliberti J, Hieny S, Reis e Sousa C, Serhan CN, Sher A. Lipoxin-mediated inhibition of IL-12 production by DCs: a mechanism for regulation of microbial immunity. Nat. Immunol. 2002;3:76–82. doi: 10.1038/ni745. [DOI] [PubMed] [Google Scholar]
- 111.Aliberti J, Serhan C, Sher A. Parasite-induced lipoxin A4 is an endogenous regulator of IL-12 production and immunopathology in Toxoplasma gondii infection. J. Exp. Med. 2002;196:1253–1262. doi: 10.1084/jem.20021183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Bandeira-Melo C, et al. Cyclooxygenase-2-derived prostaglandin E2 and lipoxin A4 accelerate resolution of allergic edema in Angiostrongylus costaricensis-infected rats: relationship with concurrent eosinophilia. J. Immunol. 2000;164:1029–1036. doi: 10.4049/jimmunol.164.2.1029. [DOI] [PubMed] [Google Scholar]
- 113.Shryock N, et al. Lipoxin A4 and 15-epi-lipoxin A4 protect against experimental cerebral malaria by inhibiting IL-12/IFN-γ in the brain. PLoS ONE. 2013;8:e61882. doi: 10.1371/journal.pone.0061882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Molina-Berrios A, et al. Protective role of acetylsalicylic acid in experimental Trypanosoma cruzi infection: evidence of a 15-epi-lipoxin A4-mediated effect. PLoS Negl Trop. Dis. 2013;7:e2173. doi: 10.1371/journal.pntd.0002173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Bannenberg GL, Aliberti J, Hong S, Sher A, Serhan C. Exogenous pathogen and plant 15-lipoxygenase initiate endogenous lipoxin A4 biosynthesis. J. Exp. Med. 2004;199:515–523. doi: 10.1084/jem.20031325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Vance RE, Hong S, Gronert K, Serhan CN, Mekalanos JJ. The opportunistic pathogen Pseudomonas aeruginosa carries a secretable arachidonate 15-lipoxygenase. Proc. Natl Acad. Sci. USA. 2004;101:2135–2139. doi: 10.1073/pnas.0307308101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Haas-Stapleton EJ, et al. Candida albicans modulates host defense by biosynthesizing the pro-resolving mediator resolvin E1. PLoS ONE. 2007;2:e1316. doi: 10.1371/journal.pone.0001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ono E, et al. Lipoxin generation is related to soluble epoxide hydrolase activity in severe asthma. Am. J. Respir. Crit. Care Med. 2014;190:886–897. doi: 10.1164/rccm.201403-0544OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Vachier I, et al. Severe asthma is associated with a loss of LX4, an endogenous anti-inflammatory compound. J. Allergy Clin. Immunol. 2005;115:55–60. doi: 10.1016/j.jaci.2004.09.038. [DOI] [PubMed] [Google Scholar]
- 120.Christie PE, Spur BW, Lee TH. The effects of lipoxin A4 on airway responses in asthmatic subjects. Am. Rev. Respir. Dis. 1992;145:1281–1284. doi: 10.1164/ajrccm/145.6.1281. [DOI] [PubMed] [Google Scholar]
- 121.Levy BD, et al. Multi-pronged inhibition of airway hyper-responsiveness and inflammation by lipoxin A4. Nat. Med. 2002;8:1018–1023. doi: 10.1038/nm748. [DOI] [PubMed] [Google Scholar]
- 122.Levy BD, et al. Lipoxin A4 stable analogs reduce allergic airway responses via mechanisms distinct from CysLT1 receptor antagonism. FASEB J. 2007;21:3877–3884. doi: 10.1096/fj.07-8653com. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Aoki H, et al. Resolvin E1 dampens airway inflammation and hyperresponsiveness in a murine model of asthma. Biochem. Biophys. Res. Commun. 2008;367:509–515. doi: 10.1016/j.bbrc.2008.01.012. [DOI] [PubMed] [Google Scholar]
- 124.Talbot S, et al. silencing nociceptor neurons reduces allergic airway inflammation. Neuron. 2015;87:341–354. doi: 10.1016/j.neuron.2015.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Park CK, et al. Resolving TRPV1- and TNF-α-mediated spinal cord synaptic plasticity and inflammatory pain with neuroprotectin D1. J. Neurosci. 2011;31:15072–15085. doi: 10.1523/JNEUROSCI.2443-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Park CK, et al. Resolvin D2 is a potent endogenous inhibitor for transient receptor potential subtype V1/A1, inflammatory pain, and spinal cord synaptic plasticity in mice: distinct roles of resolvin D1, D2, and E1. J. Neurosci. 2011;31:18433–18438. doi: 10.1523/JNEUROSCI.4192-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Serhan CN, et al. Macrophage proresolving mediator maresin 1 stimulates tissue regeneration and controls pain. FASEB J. 2012;26:1755–1765. doi: 10.1096/fj.11-201442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Xu ZZ, et al. Resolvins RvE1 and RvD1 attenuate inflammatory pain via central and peripheral actions. Nat. Med. 2010;16:592–597. doi: 10.1038/nm.2123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Takamiya R, et al. Resolvin E1 maintains macrophage function under cigarette smoke-induced oxidative stress. FEBS Open Bio. 2012;2:328–333. doi: 10.1016/j.fob.2012.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Czerska K, et al. Prostaglandin-endoperoxide synthase genes COX1 and COX2 - novel modifiers of disease severity in cystic fibrosis patients. J. Appl. Genet. 2010;51:323–330. doi: 10.1007/BF03208862. [DOI] [PubMed] [Google Scholar]
- 131.Yang J, Eiserich JP, Cross CE, Morrissey BM, Hammock BD. Metabolomic profiling of regulatory lipid mediators in sputum from adult cystic fibrosis patients. Free Radic. Biol. Med. 2012;53:160–171. doi: 10.1016/j.freeradbiomed.2012.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Martins V, et al. ATLa, an aspirin-triggered lipoxin A4 synthetic analog, prevents the inflammatory and fibrotic effects of bleomycin-induced pulmonary fibrosis. J. Immunol. 2009;182:5374–5381. doi: 10.4049/jimmunol.0802259. [DOI] [PubMed] [Google Scholar]
- 133.Guilherme RF, et al. Pulmonary antifibrotic mechanisms aspirin-triggered lipoxin A4 synthetic analog. Am. J. Respir. Cell Mol. Biol. 2013;49:1029–1037. doi: 10.1165/rcmb.2012-0462OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Kowal-Bielecka O, et al. Cyclooxygenase- and lipoxygenase-derived eicosanoids in bronchoalveolar lavage fluid from patients with scleroderma lung disease: an imbalance between proinflammatory and anti-inflammatory lipid mediators. Arthritis Rheum. 2005;52:3783–3791. doi: 10.1002/art.21432. [DOI] [PubMed] [Google Scholar]
- 135.Planaguma A, et al. Lovastatin decreases acute mucosal inflammation via 15-epi-lipoxin A4. Mucosal Immunol. 2010;3:270–279. doi: 10.1038/mi.2009.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Zarbock A, Singbartl K, Ley K. Complete reversal of acid-induced acute lung injury by blocking of platelet-neutrophil aggregation. J. Clin. Invest. 2006;116:3211–3219. doi: 10.1172/JCI29499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Sun W, et al. Endogenous expression pattern of resolvin D1 in a rat model of self-resolution of lipopolysaccharide-induced acute respiratory distress syndrome and inflammation. Int. Immunopharmacol. 2014;23:247–253. doi: 10.1016/j.intimp.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 138.Wu SH, Chen XQ, Liu B, Wu HJ, Dong L. Efficacy and safety of 15(R/S)-methyl-lipoxin A4 in topical treatment of infantile eczema. Br. J. Dermatol. 2013;168:172–178. doi: 10.1111/j.1365-2133.2012.11177.x. [DOI] [PubMed] [Google Scholar]
- 139.Weiss GA, et al. High levels of anti-inflammatory and pro-resolving lipid mediators lipoxins and resolvins and declining docosahexaenoic acid levels in human milk during the first month of lactation. Lipids Health Dis. 2013;12:89. doi: 10.1186/1476-511X-12-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Serhan CN, et al. Design of lipoxin A4 stable analogs that block transmigration and adhesion of human neutrophils. Biochemistry. 1995;34:14609–14615. doi: 10.1021/bi00044a041. [DOI] [PubMed] [Google Scholar]
- 141.Papayianni A, Serhan CN, Brady HR. Lipoxin A4 and B4 inhibit leukotriene-stimulated interactions of human neutrophils and endothelial cells. J. Immunol. 1996;156:2264–2272. [PubMed] [Google Scholar]
- 142.Levy BD, et al. Polyisoprenyl phosphate (PIPP) signaling regulates phospholipase D activity: a 'stop' signaling switch for aspirin-triggered lipoxin A4. FASEB J. 1999;13:903–911. doi: 10.1096/fasebj.13.8.903. [DOI] [PubMed] [Google Scholar]
- 143.Lee TH, et al. Lipoxin A4 and lipoxin B4 inhibit chemotactic responses of human neutrophils stimulated by leukotriene B4 and N-formyl-L-methionyl-L-leucyl-L-phenylalanine. Clin. Sci. 1989;77:195–203. doi: 10.1042/cs0770195. [DOI] [PubMed] [Google Scholar]
- 144.Gewirtz AT, Fokin VV, Petasis NA, Serhan CN, Madara JL. LXA4, aspirin-triggered 15-epi-LXA4, and their analogs selectively downregulate PMN azurophilic degranulation. Am. J. Physiol. 1999;276:C988–C994. doi: 10.1152/ajpcell.1999.276.4.C988. [DOI] [PubMed] [Google Scholar]
- 145.Maddox JF, Serhan CN. Lipoxin A4 and B4 are potent stimuli for human monocyte migration and adhesion: selective inactivation by dehydrogenation and reduction. J. Exp. Med. 1996;183:137–146. doi: 10.1084/jem.183.1.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Jozsef L, Zouki C, Petasis NA, Serhan CN, Filep JG. Lipoxin A4 and aspirin-triggered 15-epi-lipoxin A4 inhibit peroxynitrite formation, NF-κB and AP-1 activation, and IL-8 gene expression in human leukocytes. Proc. Natl Acad. Sci. USA. 2002;99:13266–13271. doi: 10.1073/pnas.202296999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Bonnans C, et al. Lipoxins are potential endogenous anti-inflammatory mediators in asthma. Am. J. Respir. Crit. Care Med. 2002;165:1531–1535. doi: 10.1164/rccm.200201-053OC. [DOI] [PubMed] [Google Scholar]
- 148.Soyombo O, Spur BW, Lee TH. Effects of lipoxin A4 on chemotaxis and degranulation of human eosinophils stimulated by platelet-activating factor and N-formyl-L-methionyl-L-leucyl-L-phenylalanine. Allergy. 1994;49:230–234. doi: 10.1111/j.1398-9995.1994.tb02654.x. [DOI] [PubMed] [Google Scholar]
- 149.Ramstedt U, et al. Lipoxin A-induced inhibition of human natural killer cell cytotoxicity: studies on stereospecificity of inhibition and mode of action. J. Immunol. 1987;138:266–270. [PubMed] [Google Scholar]
- 150.Brezinski ME, Gimbrone MA, Jr, Nicolaou KC, Serhan CN. Lipoxins stimulate prostacyclin generation by human endothelial cells. FEBS Lett. 1989;245:167–172. doi: 10.1016/0014-5793(89)80214-5. [DOI] [PubMed] [Google Scholar]
- 151.Nascimento-Silva V, Arruda MA, Barja-Fidalgo C, Fierro IM. Aspirin-triggered lipoxin A4 blocks reactive oxygen species generation in endothelial cells: a novel antioxidative mechanism. Thromb. Haemostasis. 2007;97:88–98. [PubMed] [Google Scholar]
- 152.de-Mello PF, Nascimento-Silva V, Villela CG, Fierro IM. Aspirin-triggered Lipoxin A4 inhibition of VEGF-induced endothelial cell migration involves actin polymerization and focal adhesion assembly. Oncogene. 2006;25:122–129. doi: 10.1038/sj.onc.1209002. [DOI] [PubMed] [Google Scholar]
- 153.Sodin-Semrl S, Taddeo B, Tseng D, Varga J, Fiore S. Lipoxin A4 inhibits IL-1β-induced IL-6, IL-8, and matrix metalloproteinase-3 production in human synovial fibroblasts and enhances synthesis of tissue inhibitors of metalloproteinases. J. Immunol. 2000;164:2660–2666. doi: 10.4049/jimmunol.164.5.2660. [DOI] [PubMed] [Google Scholar]
- 154.Wu SH, Wu XH, Lu C, Dong L, Chen ZQ. Lipoxin A4 inhibits proliferation of human lung fibroblasts induced by connective tissue growth factor. Am. J. Respir. Cell Mol. Biol. 2006;34:65–72. doi: 10.1165/rcmb.2005-0184OC. [DOI] [PubMed] [Google Scholar]
- 155.Parameswaran K, et al. Modulation of human airway smooth muscle migration by lipid mediators and Th-2 cytokines. Am. J. Respir. Cell Mol. Biol. 2007;37:240–247. doi: 10.1165/rcmb.2006-0172OC. [DOI] [PubMed] [Google Scholar]
- 156.Campbell EL, et al. Resolvin E1 promotes mucosal surface clearance of neutrophils: a new paradigm for inflammatory resolution. FASEB J. 2007;21:3162–3170. doi: 10.1096/fj.07-8473com. [DOI] [PubMed] [Google Scholar]
- 157.Arita M, et al. Resolvin E1, an endogenous lipid mediator derived from omega-3 eicosapentaenoic acid, protects against 2,4,6-trinitrobenzene sulfonic acid-induced colitis. Proc. Natl Acad. Sci. USA. 2005;102:7671–7676. doi: 10.1073/pnas.0409271102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Isobe Y, et al. Identification and structure determination of novel anti-inflammatory mediator resolvin E3, 17,18-dihydroxyeicosapentaenoic acid. J. Biol. Chem. 2012;287:10525–10534. doi: 10.1074/jbc.M112.340612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Sun YP, et al. Resolvin D1 and its aspirin-triggered 17R epimer. Stereochemical assignments, anti-inflammatory properties, and enzymatic inactivation. J. Biol. Chem. 2007;282:9323–9334. doi: 10.1074/jbc.M609212200. [DOI] [PubMed] [Google Scholar]
- 160.Duffield JS, et al. Resolvin D series and protectin D1 mitigate acute kidney injury. J. Immunol. 2006;177:5902–5911. doi: 10.4049/jimmunol.177.9.5902. [DOI] [PubMed] [Google Scholar]
- 161.Ariel A, et al. The docosatriene protectin D1 is produced by TH2 skewing and promotes human T cell apoptosis via lipid raft clustering. J. Biol. Chem. 2005;280:43079–43086. doi: 10.1074/jbc.M509796200. [DOI] [PubMed] [Google Scholar]
- 162.Nordgren TM, et al. Maresin-1 reduces the pro-inflammatory response of bronchial epithelial cells to organic dust. Respir. Res. 2013;14:51. doi: 10.1186/1465-9921-14-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Genis P, et al. Cytokines and arachidonic metabolites produced during human immunodeficiency virus (HIV)-infected macrophage-astroglia interactions: implications for the neuropathogenesis of HIV disease. J. Exp. Med. 1992;176:1703–1718. doi: 10.1084/jem.176.6.1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Chen M, et al. Lipid mediators in innate immunity against tuberculosis: opposing roles of PGE2 and LXA4 in the induction of macrophage death. J. Exp. Med. 2008;205:2791–2801. doi: 10.1084/jem.20080767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Divangahi M, et al. Mycobacterium tuberculosis evades macrophage defenses by inhibiting plasma membrane repair. Nat. Immunol. 2009;10:899–906. doi: 10.1038/ni.1758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Van Dyke TE, et al. Proresolving nanomedicines activate bone regeneration in periodontitis. J. Dent. Res. 2015;94:148–156. doi: 10.1177/0022034514557331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Gao L, et al. Resolvin E1 and chemokine-like receptor 1 mediate bone preservation. J. Immunol. 2013;190:689–694. doi: 10.4049/jimmunol.1103688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Kurihara T, et al. Resolvin D2 restores neutrophil directionality and improves survival after burns. FASEB J. 2013;27:2270–2281. doi: 10.1096/fj.12-219519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Levy BD, et al. The endogenous pro-resolving mediators lipoxin A4 and resolvin E1 preserve organ function in allograft rejection. Prostaglandins Leukot. Essent. Fatty Acids. 2011;84:43–50. doi: 10.1016/j.plefa.2010.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Liao W, et al. Lipoxin A4 attenuates acute rejection via shifting TH1/TH2 cytokine balance in rat liver transplantation. Transplant. Proc. 2013;45:2451–2454. doi: 10.1016/j.transproceed.2013.01.069. [DOI] [PubMed] [Google Scholar]
- 171.Hua J, et al. The resolvin D1 analogue controls maturation of dendritic cells and suppresses alloimmunity in corneal transplantation. Invest. Ophthalmol. Vis. Sci. 2014;55:5944–5951. doi: 10.1167/iovs.14-14356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Devchand PR, et al. A synthetic eicosanoid LX-mimetic unravels host-donor interactions in allogeneic BMT-induced GvHD to reveal an early protective role for host neutrophils. FASEB J. 2005;19:203–210. doi: 10.1096/fj.04-2565com. [DOI] [PubMed] [Google Scholar]
- 173.Medeiros R, et al. Aspirin-triggered lipoxin A4 stimulates alternative activation of microglia and reduces Alzheimer disease-like pathology in mice. Am. J. Pathol. 2013;182:1780–1789. doi: 10.1016/j.ajpath.2013.01.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Lukiw WJ, et al. A role for docosahexaenoic acid-derived neuroprotectin D1 in neural cell survival and Alzheimer disease. J. Clin. Invest. 2005;115:2774–2783. doi: 10.1172/JCI25420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Mizwicki MT, et al. 1α, 25-dihydroxyvitamin D3 and resolvin D1 retune the balance between amyloid- β phagocytosis and inflammation in Alzheimer's disease patients. J. Alzheimer's Dis. 2013;34:155–170. doi: 10.3233/JAD-121735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Liu G, et al. Neuronal phagocytosis by inflammatory macrophages in ALS spinal cord: inhibition of inflammation by resolvin D1. Am. J. Neurodegener. Dis. 2012;1:60–74. [PMC free article] [PubMed] [Google Scholar]
- 177.Prescott D, McKay DM. Aspirin-triggered lipoxin enhances macrophage phagocytosis of bacteria while inhibiting inflammatory cytokine production. Am. J. Physiol. Gastrointestinal Liver Physiol. 2011;301:G487–G497. doi: 10.1152/ajpgi.00042.2011. [DOI] [PubMed] [Google Scholar]
- 178.Gewirtz AT, et al. Lipoxin a4 analogs attenuate induction of intestinal epithelial proinflammatory gene expression and reduce the severity of dextran sodium sulfate-induced colitis. J. Immunol. 2002;168:5260–5267. doi: 10.4049/jimmunol.168.10.5260. [DOI] [PubMed] [Google Scholar]
- 179.Ishida T, et al. Resolvin E1, an endogenous lipid mediator derived from eicosapentaenoic acid, prevents dextran sulfate sodium-induced colitis. Inflamm. Bowel Dis. 2010;16:87–95. doi: 10.1002/ibd.21029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Bento AF, Claudino RF, Dutra RC, Marcon R, Calixto JB. Omega-3 fatty acid-derived mediators 17(R)-hydroxy docosahexaenoic acid, aspirin-triggered resolvin D1 and resolvin D2 prevent experimental colitis in mice. J. Immunol. 2011;187:1957–1969. doi: 10.4049/jimmunol.1101305. [DOI] [PubMed] [Google Scholar]
- 181.Hellmann J, Tang Y, Kosuri M, Bhatnagar A, Spite M. Resolvin D1 decreases adipose tissue macrophage accumulation and improves insulin sensitivity in obese-diabetic mice. FASEB J. 2011;25:2399–2407. doi: 10.1096/fj.10-178657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Neuhofer A, et al. Impaired local production of proresolving lipid mediators in obesity and 17-HDHA as a potential treatment for obesity-associated inflammation. Diabetes. 2013;62:1945–1956. doi: 10.2337/db12-0828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Quan-Xin F, et al. Resolvin D1 reverses chronic pancreatitis-induced mechanical allodynia, phosphorylation of NMDA receptors, and cytokines expression in the thoracic spinal dorsal horn. BMC Gastroenterol. 2012;12:148. doi: 10.1186/1471-230X-12-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Gronert K, et al. A role for the mouse 12/15-lipoxygenase pathway in promoting epithelial wound healing and host defense. J. Biol. Chem. 2005;280:15267–15278. doi: 10.1074/jbc.M410638200. [DOI] [PubMed] [Google Scholar]
- 185.de Paiva CS, Schwartz CE, Gjorstrup P, Pflugfelder SC. Resolvin E1 (RX-10001) reduces corneal epithelial barrier disruption and protects against goblet cell loss in a murine model of dry eye. Cornea. 2012;31:1299–1303. doi: 10.1097/ICO.0b013e31823f789e. [DOI] [PubMed] [Google Scholar]
- 186.Dartt DA, et al. Conjunctival goblet cell secretion stimulated by leukotrienes is reduced by resolvins D1 and E1 to promote resolution of inflammation. J. Immunol. 2011;186:4455–4466. doi: 10.4049/jimmunol.1000833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Li D, et al. Resolvin D1 and aspirin-triggered resolvin D1 regulate histamine-stimulated conjunctival goblet cell secretion. Mucosal Immunol. 2013;6:1119–1130. doi: 10.1038/mi.2013.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Li N, He J, Schwartz CE, Gjorstrup P, Bazan HE. Resolvin E1 improves tear production and decreases inflammation in a dry eye mouse model. J. Ocular Pharmacol. Ther. 2010;26:431–439. doi: 10.1089/jop.2010.0019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Connor KM, et al. Increased dietary intake of omega-3-polyunsaturated fatty acids reduces pathological retinal angiogenesis. Nat. Med. 2007;13:868–873. doi: 10.1038/nm1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Munger KA, et al. Transfection of rat kidney with human 15-lipoxygenase suppresses inflammation and preserves function in experimental glomerulonephritis. Proc. Natl Acad. Sci. USA. 1999;96:13375–13380. doi: 10.1073/pnas.96.23.13375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Borgeson E, et al. Lipoxin A4 and benzo-lipoxin A4 attenuate experimental renal fibrosis. FASEB J. 2011;25:2967–2979. doi: 10.1096/fj.11-185017. [DOI] [PubMed] [Google Scholar]
- 192.Qu X, et al. Resolvins E1 and D1 inhibit interstitial fibrosis in the obstructed kidney via inhibition of local fibroblast proliferation. J. Pathol. 2012;228:506–519. doi: 10.1002/path.4050. [DOI] [PubMed] [Google Scholar]
- 193.Zhang L, et al. BML-111, a lipoxin receptor agonist, modulates the immune response and reduces the severity of collagen-induced arthritis. Inflamm. Res. 2008;57:157–162. doi: 10.1007/s00011-007-7141-z. [DOI] [PubMed] [Google Scholar]
- 194.Lima-Garcia JF, et al. The precursor of resolvin D series and aspirin-triggered resolvin D1 display anti-hyperalgesic properties in adjuvant-induced arthritis in rats. Br. J. Pharmacol. 2011;164:278–293. doi: 10.1111/j.1476-5381.2011.01345.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Keyes KT, et al. Resolvin E1 protects the rat heart against reperfusion injury. Am. J. Physiol. Heart Circ. Physiol. 2010;299:H153–H164. doi: 10.1152/ajpheart.01057.2009. [DOI] [PubMed] [Google Scholar]
- 196.Shen J, et al. Macrophage-mediated 15-lipoxygenase expression protects against atherosclerosis development. J. Clin. Invest. 1996;98:2201–2208. doi: 10.1172/JCI119029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Marcheselli VL, et al. Novel docosanoids inhibit brain ischemia-reperfusion-mediated leukocyte infiltration and pro-inflammatory gene expression. J. Biol. Chem. 2003;278:43807–43817. doi: 10.1074/jbc.M305841200. [DOI] [PubMed] [Google Scholar]
- 198.Kim TH, Kim GD, Jin YH, Park YS, Park CS. Omega-3 fatty acid-derived mediator, Resolvin E1, ameliorates 2,4-dinitrofluorobenzene-induced atopic dermatitis in NC/Nga mice. Int. Immunopharmacol. 2012;14:384–391. doi: 10.1016/j.intimp.2012.08.005. [DOI] [PubMed] [Google Scholar]
- 199.Klein CP, et al. Effects of D-series resolvins on behavioral and neurochemical changes in a fibromyalgia-like model in mice. Neuropharmacology. 2014;86:57–66. doi: 10.1016/j.neuropharm.2014.05.043. [DOI] [PubMed] [Google Scholar]
- 200.Bang S, et al. Resolvin D1 attenuates activation of sensory transient receptor potential channels leading to multiple anti-nociception. Br. J. Pharmacol. 2010;161:707–720. doi: 10.1111/j.1476-5381.2010.00909.x. [DOI] [PMC free article] [PubMed] [Google Scholar]