Abstract
The serodiagnostic efficiencies of five different approaches to detecting antibodies (immunoglobulins G, A, and M) developed in clinically proven infections with Francisella tularensis have been assessed. Fifty serum samples from patients suffering from tularemia during an outbreak in Sweden were compared with samples from 50 healthy blood donors (controls) by using an enzyme-linked immunosorbent assay (ELISA), microagglutination (MA), Western blotting (WB), an indirect immunofluorescence assay (IIFA), and flow cytometry (FC). ELISA, WB, and FC were based on the use of preparations of lipopolysaccharides (LPS) of the live vaccine strain of Francisella tularensis subsp. holarctica (ATCC 29684) as a capture antigen. Whole methanol-fixed bacteria were used for IIFA and MA. Optimized protocols yielded a diagnostic sensitivity and specificity of 100% for WB, MA, and FC, 98% for ELISA, and 93% for IIFA. A total of 6,632 serum samples from individuals between the ages of 18 and 79 years, representatively recruited from all regions of Germany, were screened to estimate and confirm the positive predictive value (PVpos) of the ELISA. Serum samples from 15 (0.226%) individuals tested positive for F. tularensis-specific antibodies by ELISA and confirmatory WB. The resulting prevalence-dependent PVpos of 10.2% and specificity of 98.1% were consistent with our findings for tularemia patients and controls. We conclude that the combined usage of a screening ELISA and a confirmatory WB based on LPS as a common antigen, as well as the MA, is a suitable serodiagnostic tool, while the quality of the IIFA is hampered by subjective variations of the results. FC is a promising new approach that might be improved further in terms of multiplex analyses or high-throughput applications.
Tularemia is a zoonotic disease caused by the highly infective, virulent, nonsporulating gram-negative coccobacillus Francisella tularensis. It is found throughout most of the northern hemisphere in a wide range of animal reservoir hosts including mammals, birds, and insects and can persist for a long time in contaminated environmental sources such as water and mud. It is not known to be transmitted from one person to another. Epidemics can often be traced to concurrent epizootics involving rodents and other small mammals (for a detailed review, see reference 15). Furthermore, in the past, tularemia was one of the most common laboratory-acquired diseases (10).
There are several tularemia syndromes in humans, most of them depending on the portal of infection. The clinical appearance ranges from skin lesions to multiorgan involvement. The severity, furthermore, varies with the dose inoculated and the virulence of the bacterium, which is related to the biotype. Francisella tularensis biovar holarctica (type B), which is spread over the whole northern hemisphere, is less virulent than Francisella tularensis biovar tularensis (type A), which exists mainly in North America and is associated with severe and often fatal tularemia if left untreated.
The usual incubation period is 3 to 5 days, although it can be as long as 21 days. In most cases, antibodies appear 6 to 10 days after the onset of symptoms, i.e., usually about 2 weeks after infection, reach their peaks at 4 to 7 weeks, and, despite decreasing in level, are still present 0.5 to 25 years later, probably even longer (16, 28). Even though early identification of the pathogen is important, neither isolation by cultivation, immunologic detection of antigens, nor molecular approaches are always successful or suitable (22, 25, 29, 35). Considering the facultatively intracellular localization of the pathogen, cell-mediated immunity is likely to be the best correlate for assessing exposure or immunity to F. tularensis (26). A tularin skin test is very helpful in this regard and is still used in some parts of Eastern Europe (12) but is not licensed in most other countries. Thus, clinical investigations and epidemiological studies on humans and animals or confirmation of immunoreactivity after vaccination depends on the availability of reliable, convenient, and affordable assays to detect and monitor the appearance of specific antibodies. During the immune response, epitopes of Francisella lipopolysaccharides (LPS) are the main target for the development of species-specific antibodies (1, 32). These antibodies, however, confer virtually no or low protection on mice against challenges with virulent type A strains of the pathogen (13). Several other antigens have been used to confirm seroconversion after exposure to F. tularensis (7). Preparations of outer membrane antigens can be applied to several methodological platforms such as enzyme-linked immunosorbent assays (ELISA), microagglutination, and Western blotting (5, 6, 8). Assays based on LPS as a capture antigen, with different approaches to purification and detection, have been described previously (11, 20, 21, 37). These preparations have yielded high specificity for Francisella type A and B strains, the assays are easy to carry out, and antigens were stable over a long period (22).
In this study, we compared different preparations and platforms routinely used for the detection of F. tularensis-specific antibodies. The efficiencies of the different tests were assessed, and the plausibility of our findings was confirmed in a large-scale field investigation. Additionally, we set up a new approach toward further antigen purification and detection of specific antibodies, employing flow cytometry, a rapid detection technique which is increasingly used in clinical laboratories (36).
MATERIALS AND METHODS
Bacteria and LPS preparation.
The live vaccine strain (LVS) of F. tularensis biovar holarctica (ATCC 29648) was grown over 2 days on heart-cysteine-blood agar and harvested into sterile distilled water, and bacterial concentrations were adjusted photometrically at 560 nm. Therefore, the LPS concentration is given as “bacterial equivalents. ” For the ELISA, the bacteria were adjusted to an optical density at 560 nm (OD560) of 1.0, which corresponded to 109 bacteria/ml. A 1/100 dilution (107 bacterial equivalents/ml) of this preparation was determined in titration experiments to be the optimal concentration for coating the microtiter plates.
To extract and solubilize the LPS from bacteria, a Chlamydia specimen extraction buffer (Abbott, Wiesbaden, Germany) was added to a final dilution of 1/2 and incubated for 30 min at 60°C. It was not expected that a highly purified LPS preparation would be obtained by this procedure. However, in another set of experiments, we purified the LPS to a high degree by phenol-water extraction and compared the purified LPS with the standard product. We did not find an improvement in specificity due to the use of the highly purified product compared with the LPS preparation described here. It was therefore concluded that the purification described here is sufficient.
To further purify the LPS, the antigen was filtered and treated with 3.3 mg of proteinase K (Boehringer, Mannheim, Germany)/ml for 2 h at 60°C in order to digest residues of proteins. The enzyme was heat inactivated for 25 min. LPS was finally purified by overnight dialysis (Slide-A-Lyzer 3.5 K; Pierce, Rockford, Ill.) in phosphate-buffered saline (PBS, pH 7.2) and stored at −20°C until use. For Western blotting, the whole bacterial lysate was used without the preparation of LPS in order to detect additional protein bands which could be cross-reactive with other bacteria. The bacterial suspension was therefore adjusted to an OD560 of 2.5.
Sera.
Positive-control sera from tularemia patients with confirmed seroconversion were kindly provided by A. Sjostedt, Umea, Sweden (35). Anonymous negative-control sera collected from healthy blood donors were obtained from the Bavarian Red Cross. Fifty positive and 50 negative samples were selected randomly for comparative analysis. All the serum samples used were retained by the contributors and rendered anonymous. The usage of such serum samples is in accordance with German laws.
Pooled sera from individuals who had recovered from confirmed tularemia were used as positive quality control samples. Pooled negative-control sera were obtained from individuals with no history of tularemia. All the sera were stored as aliquots at −25°C until use.
Sera for epidemiological investigations were kindly provided by the Robert Koch Institute. These samples were collected on behalf of the Federal Ministry of Health in the context of a study to assess the health status of the population in unified Germany (3). A total of 7,200 randomized individuals aged 18 to 79 years participated in the survey. Serum samples from 6,617 individuals were assayed for the presence of F. tularensis-specific antibodies.
ELISA.
The LPS solution was diluted 1/100 in carbonate-bicarbonate buffer (pH 9.0). Ninety-six-well microtiter plates (Polysorb; NUNC, Wiesbaden, Germany) were coated with 50 μl of antigen for 1 h at 37°C. The wells were washed with PBS-Tween (0.05%; pH 7.2) and blocked with 75 μl of 10% goat serum in PBS-Tween. After another washing step, 50 μl of patient serum samples, as well as positive and negative controls, diluted 1/500 in 10% goat serum, was added and incubated for 1 h at 4°C. After the plates had been washed four times, 50 μl (each) of horseradish peroxidase (Sigma, Taufkirchen, Germany)-conjugated goat anti-human immunoglobulin G (IgG), IgM, and IgA (Gibco, Eggenstein, Germany), diluted 1/2,000 in 10% goat serum, was added and incubated for 1 h at 37°C. Goat anti-human immunoglobulins were found not to be reactive with Francisella antigen. After six rinses with PBS-Tween, a substrate reaction was started with 50 μl of 66% tetramethylbenzidine (TMB; Seramun, Dolgenbroth, Germany) and stopped after 10 min with 50 μl of 2.5 N sulfuric acid. OD405 values were determined by using an Asys Hitech microplate reader.
Western blotting.
The LVS suspension was inactivated with 1% formalin overnight and adjusted to an OD560 of 2.5. Subsequently, 150 μl was treated with 50 μl of NuPAGE sample buffer (Invitrogen, Karlsruhe, Germany) and 10 μl of mercaptoethanol for 10 min at 70°C. After 15 min of boiling, the suspension was centrifuged for 20 min at 7,000 × g, and the soluble fraction was subjected to polyacrylamide gel electrophoresis (PAGE) at 130 V on a 4 to 12% NuPAGE gel (Invitrogen) for 1.5 h.
The gel was soaked for 10 min in transfer buffer (Novex, Frankfurt, Germany), and the bacterial antigens were transferred to a nitrocellulose membrane (Millipore, Billerica, Mass.) at 30 V for 1 h. The remaining binding sites on the membrane were blocked with 4% skim milk in Tris-buffered saline (pH 8.1) overnight at 4°C. The cut membrane strips were incubated with sera diluted 1/500 in 10% goat serum in PBS at room temperature for 2 h. For evaluation purposes, sera were diluted up to 1/2,000. After three rinses with washing buffer (Y.P. kit; Microgene, Munich, Germany), the strips were incubated with a polyvalent goat anti-human IgA-IgM-IgG horseradish peroxidase conjugate (Sigma) at room temperature for 1 h. Following another three rinses, the membrane strips were developed with precipitating TMB (Seramun). Sera were considered positive when they showed the typical LPS banding pattern at a dilution of 1/2,000.
Microagglutination.
Colonies of F. tularensis LVS were harvested into 0.9% NaCl from plates after cultivation for 2 days. After inactivation by 1% paraformaldehyde overnight, bacteria were washed twice and adjusted to an OD560 of 2.5 in PBS with 0.05% thiomersal and 0.1% crystal violet. This suspension of stained bacteria was used as an antigen. Serial dilutions of the sera up to 1/256 in PBS were applied. Fifty microliters of antigen suspensions was mixed with 50 μl of diluted sera by using 96-well round-bottom microtiter plates (NUNC), and the mixture was incubated overnight at room temperature. Wells were subsequently examined visually for a typically blue color indicating agglutination.
Flow cytometry.
The IgG1 monoclonal antibody (MAb) 11/1/6 was produced by myeloma cells fused with mouse (BALB/c) spleen cells after immunization with F. tularensis ATCC 6223 as previously described (21). No cross-reactivity with a wide range of gram-negative bacteria was observed (22).
The assay is based on the coupling of MAb 11/1/6, specific for F. tularensis LPS, on magnetic M-450 goat anti-mouse-DynaBeads (Dynal, Hamburg, Germany) and the subsequent preincubation with F. tularensis LPS. The bead-antibody-LPS complex was incubated with sera. F. tularensis LPS-specific antibodies were detected by fluorescein isothiocyanate (FITC)-labeled goat anti-human IgG, IgA, and IgM antibodies (Sigma).
The incubation time, dilution of sera, antibodies, and antigen were pretested in order to optimize assay settings. In the final protocol, 5 μl of beads (absolute number, 3 × 105) was intensively washed and resuspended in 1 ml of fluorescence-activated cell sorter (FACS) buffer containing PBS (pH 7.2; Sigma-Aldrich, Taufkirchen, Germany), 2% fetal calf serum (Gibco), and 0.02% sodium azide (Merck, Darmstadt, Germany).
Single washing steps were usually performed. If intensive washing was required, the procedure was repeated three times. Beads were incubated with 40 μg of MAb 11/1/6/ml at room temperature for 30 min. F. tularensis LPS was 1/2 diluted and incubated at room temperature for 30 min with the beads. Loaded beads were then transferred to FACS tubes and incubated with the sera at a final dilution of 1/25 for 30 min. Polyvalent FITC-labeled anti-human immunoglobulin was diluted 1/100, and 200 μl was added to each tube. After incubation for 30 min at room temperature, samples were resuspended in 500 μl of FACS buffer and subjected to flow cytometry by using an EPICS XL (Beckman Coulter, Krefeld, Germany). Between incubation steps, beads were washed by magnetic separation using the MCP-1 magnetic particle collector (Dynal).
Indirect immunofluorescence assay (IIFA).
Suspensions of the LVS (OD560, 1.0) were diluted 1/20, and 20 μl was placed on immunofluorescence slides (BioMerieux, Marcy l'Etoile, France). Slides were dried overnight and fixed with methanol. Serial dilutions of 20 μl of sera were added and incubated at 37°C for 1 h. FITC-labeled polyvalent anti-human immunoglobulin antibodies (DAKO, Hamburg, Germany) were diluted 1/100 in PBS containing 0.05% Evans blue. The secondary antibodies used were found not to be reactive with Francisella antigen. After a wash with PBS, slides were covered with 20 μl of the secondary antibody-dye mixture, incubated at 37°C for 30 min, and washed with PBS. Slides were subsequently covered with fluorescent mounting medium (DAKO) The fluorescence intensity was judged microscopically by the brightness, which corresponded to a semiquantitative scale from negative to quadruple-cross positive. Antibody titers were defined as the highest serum dilution that showed a specific fluorescence corresponding to double-cross positive (if not otherwise indicated). Lower brightness led to a relatively high subjective variation of the results when investigators were blinded.
Statistics.
The diagnostic performance of a test was assessed by receiver operating characteristic (ROC) analysis including ROC curves, a complete sensitivity-specificity report, and disease prevalence-dependent predictive values (39). A sample size of 50 patients and 50 controls was used, according to the method of Metz (30), in order to draw meaningful conclusions from ROC experiments.
Linear regression and correlation analyses were performed in order to assess the relationship and association between two variables. MedCalc, version 7.2.0.2, was used for all statistical analysis purposes.
RESULTS AND DISCUSSION
Setup and comparison of serodiagnostic approaches.
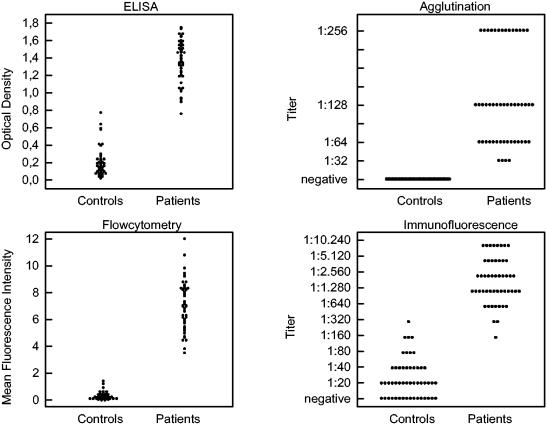
In the present study, five different methods of detecting Francisella-specific antibodies were evaluated. F. tularensis LPS is one of the major targets for antibodies (1, 32). While whole bacterial suspensions are needed for immunofluorescence tests and microagglutination, lysed bacteria were used for Western blotting. Further purification of LPS by elimination of contaminating proteins was necessary for ELISA and flow cytometry in order to reduce nonspecific binding of serum antibodies in presumptively nonexposed subjects. The diagnostic performance of these assays was evaluated by using random samples from 50 patients who had suffered from clinically proven tularemia and 50 healthy blood donors (controls). The distributions of antibody levels obtained by the different diagnostic approaches are depicted in Fig. 1. Calculations of sensitivity, specificity, and the underlying cutoff levels are given in Table 1 and are discussed below. A comparison of ELISA ODs at a serum dilution of 1/500 with end point titers of microagglutination and IIFA, respectively, showed no significant correlation (data not shown). It is most likely that the optical densities of positive and negative sera in ELISA were not measured in the linear range of the standard curve, so no conclusions can be drawn as to the end point titers. In contrast, mean fluorescence intensities obtained by flow cytometry from patients' sera correlated significantly with the ODs of the ELISA (see below).
FIG. 1.
Distribution of F. tularensis LPS-specific immunoglobulin levels. Levels in sera of patients (n = 50) and healthy controls (n = 50) were determined by the methods given above the plots. Sera for ELISA were diluted 1/640.
TABLE 1.
Cutoff values, diagnostic sensitivity, and specificity of four approaches for the detection of tularemia-specific antibodiesa
| Method | Unit | At 100% sensitivity
|
At 100% specificity
|
||
|---|---|---|---|---|---|
| Cutoff | Specificity (%) (95% CI) | Cutoff | Sensitivity (%) (95% CI) | ||
| ELISA | Optical density | >0.648 | 98.0 (89.3-99.7) | >0.780 | 98.0 (89.3-99.7) |
| Flow cytometry | Mean fluorescence intensity | >1.59 | 100.0 (92.8-100) | >1.59 | 100.0 (92.8-100) |
| Indirect immunofluorescence assay | Intensity, titer | >1/80 | 92.0 (80.7-97.7) | >1/320 | 94.0 (83.4-98.7) |
| Microagglutination | Agglutination, titer | >1/16 | 100 (92.8-100) | >1/16 | 100.0 (92.8-100) |
| Western blotting | Visible LPS pattern, titer | 1/2,000 | 100 (92.8-100) | 1/2,000 | 100.0 (92.8-100) |
Fifty serum samples from clinically proven tularemia patients and 50 from healthy controls were analyzed for F. tularensis LPS-specific immunoglobulin. Methods were evaluated by ROC analysis. 95% CI, 95% confidence intervals.
Western blotting.
As shown in Table 1, Western blot analysis clearly distinguished between patients and controls. Dilution of sera down to 1/2,000 did not affect the appearance of the typical LPS banding pattern but eliminated nonspecific bands seen in some of the control sera. Cross-reactivity has been assumed for proteins homologous to the highly conserved chaperone proteins DnaK, GroEL, and GroES of Escherichia coli (17). Enzymatic digestion of the LPS extract decreased the amount of contaminating proteins. However, some heat shock proteins may have been resistant to proteinase K, since the respective bands remained visible in the Western blot after digestion.
IIFA.
Elevated optical densities in the screening ELISA and a high background immunofluorescence of negative controls might result from antibodies against those heat shock proteins. By IIFA, there was a clear overlap between patients and controls (Table 1). Decision criteria were defined as the highest titer of serum dilution that still allows the clear detection of fluorescence. Lower fluorescence intensities led to a higher subjective variation in determining the end point titers of sera.
Microagglutination.
Microagglutination resulted in 100% sensitivity and specificity. No agglutination was visible in any of the control sera at dilutions below 1/16, while in 92% (n = 46) of the patients' sera, titers reached 1/64 or higher (Fig. 1). Since the sera from all patients were collected more than 7 days after clinical manifestation of the infection, our results were in line with those of a former study that reported 24, 50, and 100% sensitivity of microagglutination 4, 5, and 7 days after clinical manifestation, respectively (33). These observations confirmed that microagglutination is a useful tool for the early and specific serodiagnosis of tularemia. However, cross-reactions with different species of Brucella, Yersinia enterocolitica, and Proteus must be considered and ruled out in the case of positive test results (2, 27).
Flow cytometry.
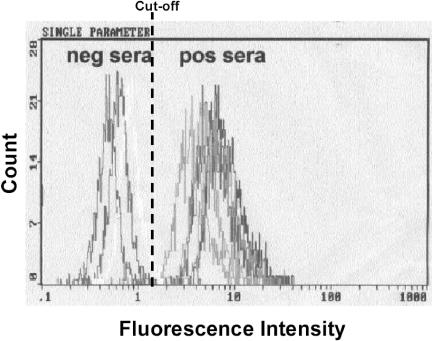
The panel of routinely used methods was extended by an innovative approach that combines flow cytometry and immunomagnetic separation. Recently, flow cytometry has been reported to be a new platform for serological investigations of plague (36). We therefore set up a procedure to couple F. tularensis LPS on goat anti-mouse paramagnetic beads (GAM-Dynabeads; Dynal, Hamburg, Germany) and used MAb 11/1/6, specific for LPS of all F. tularensis subspecies but not for Francisella novicida (22), as a linker. The coupling of beads, MAb 11/1/6, and LPS formed stable complexes. The stability of the coated beads was tested by comparing freshly prepared beads with those coated at the beginning of the test period (7 days) and stored at 4°C. Measuring positive- and negative-control samples revealed no significant differences in mean fluorescence intensity between fresh and stored beads (data not shown). We did not test stability over a longer period, even though we assume that stability might last even longer. Since the usage of precoated beads saved about 2 h of assay time, beads were prepared on Monday and used over the week. As shown in the overlay graph (Fig. 2), the optimized assay settings allowed a sufficient distinction to be revealed between the fluorescence intensities of patients and controls. The lower background of controls in flow cytometry than in ELISA might be caused by the additional purification of the LPS antigen due to the binding and washing of antibody-bead complexes. Systematic analysis of patient and control sera revealed a complete distinction between the two groups (Fig. 1).
FIG. 2.
Determination of F. tularensis antibodies by flow cytometry. Representative histograms of green fluorescence intensities of five serum samples from tularemia patients and two from healthy controls are shown.
ELISA.
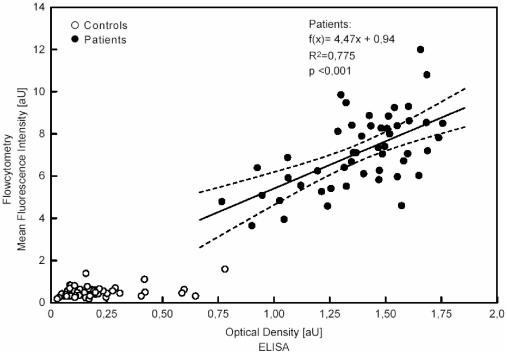
Enzyme-linked immunosorbent assays are among the methods of choice for large-scale investigations in the context of outbreak scenarios or epidemiological surveillance studies (4, 6, 28). LPS preparations immobilized on Polysorb microtiter plates were identical to those used for flow cytometry. Nevertheless, flow cytometry was obviously superior to ELISA in terms of test efficiency. The scatter graph in Fig. 3 indicates that ELISA results for patient samples correlated significantly with mean fluorescence intensities obtained by flow cytometry. In contrast, ELISA results for the control sera spread over a wide range and did not correlate with the outcomes of corresponding measurements by flow cytometry. Dilution of sera down to 1/640 reduced the nonspecific background observed in control sera and increased the test efficiency of ELISA as assessed by ROC analysis. However, further dilution again led to an increased overlap of titers between patients and controls due to the decreased sensitivity of the assay (data not shown). A certain number of negative sera showed a relatively high background; however, these sera were probably overrepresented in this random sample. In larger studies (see “Seroepidemiology” below), the proportion of false-negative sera was much lower, even when a lower cutoff level was used.
FIG. 3.
Comparison of ELISA and flow cytometry methods. A scatter plot of mean fluorescence intensities obtained by flow cytometry and optical densities obtained by ELISA is shown. Linear regression analysis assessing the association of test results obtained for patients' sera (n = 50) by flow cytometry with those obtained by ELISA is indicated. Dashed lines, 95% confidence intervals of the regression function. Sera for ELISA were diluted 1/640.
Sensitivity and specificity assessed for optimized ELISA settings reached 98% and thus did not differ significantly from those reported from a former study that evaluated an ELISA with 57 tularemia cases (4). That assay was based on an outer membrane preparation that included several immunologic reactive antigens and reached a sensitivity of 93% for the simultaneous detection of IgG, IgA, and IgM and 97.5% for the separate analysis of immunoglobulin isotypes. Furthermore, Bevanger et al. described a competitive ELISA using a purified 43-kDa outer membrane protein that was tested with 23 tularemia patients (7). The sensitivity and specificity reported were 95.7 and 96%, respectively, after a serum dilution of 1/64.
Seroepidemiology.
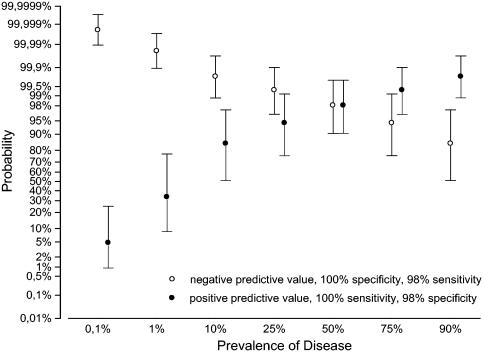
Assuming that the optimized LPS-based ELISA has a specificity of 98%, the pretest probability of the disease was calculated for a hypothetical range of disease prevalence. The prevalence-dependent positive predictive values of ELISA results are shown in Fig. 4.
FIG. 4.
Tularemia prevalence-dependent predictive values of ELISA. Positive (filled circles) and negative (open circles) predictive values of ELISA for a hypothetical range of disease prevalence were calculated based on the results given in Table 1. Ninety-five percent confidence intervals are indicated.
Especially in a setting with a low serological prevalence of tularemia, such as seroepidemiological investigations conducted to estimate the risk of exposure or to survey for subclinical courses of tularemia, 95% false-positive results by ELISA will appear, assuming there is a seroprevalence of 1:1,000.
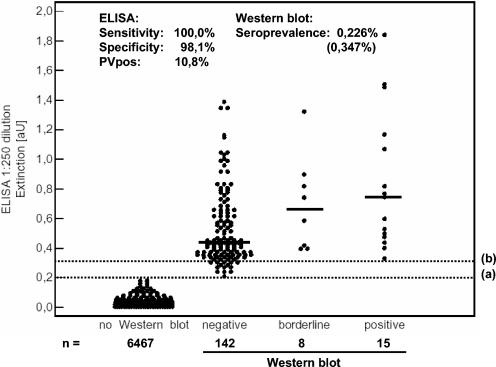
In order to confirm our results, we tested 6,632 sera that were randomly collected in the context of a health survey initiated by the German health authorities (3). The cross-sectional sample was representative of the German population in the years 1997 to 1998. A cutoff level of 0.200 for performing confirmatory Western blotting was derived from measurement of the negative-control sera on 200 distinct microtiter plates and calculation of 3 times the standard deviation. We found 165 sera above the cutoff level. In contrast to the distribution of our initial ELISA results, shown in Fig. 1, the percentage of serologically negative individuals with high background levels was significantly lower. We therefore concluded that such sera were accidentally overrepresented in our initial sampling. Fifteen positive sera were confirmed by Western blotting (Fig. 5). Another eight sera had slightly elevated values but exhibited only a weak or incomplete LPS banding pattern. Since all sera confirmed as positive (Fig. 5, line b) were clearly separated from the cutoff value (Fig. 5, line a), we assumed 100% sensitivity of our approach. The calculated specificity of 98.1% resulted in a positive predictive value of 10.8% for the ELISA and matched our initial findings obtained by using tularemia patients as positive controls and healthy individuals as negative controls (Fig. 4). As a consequence, a seroprevalence of 226 per 100,000 was calculated and therefore has to be assumed for the German population. None of the positive sera exhibited elevated IgM levels. In a comparable approach, 4,825 healthy people from Castilla y Leon, Spain, were examined for the presence of antibodies against F. tularensis by microagglutination (24). The observed prevalence of 0.19% was consistent with our results. Also, we found no obvious preference for gender, age, or geographical distribution. Both the findings in Spain and our present observations seem to conflict with the low incidence of suspected tularemia cases. Direct or indirect laboratory evidence for acute tularemia is a certifiable state according to the regulations in German law on protection against infectious diseases. Nevertheless, only 0 to 5 sporadic cases per year have been reported over the last four decades (our own meta-analysis of German data provided by German health authorities). Extrapolation of our data would result in a considerably higher annual F. tularensis infection rate in Germany than that which is currently assumed.
FIG. 5.
Survey of serum anti-F. tularensis antibody levels in Germany (n = 6,632). The distribution of ELISA results stratified by a cutoff level of 0.200 (line a) and results of confirmatory Western blotting are shown. Line b indicates the threshold value of confirmed positive samples. For calculation of specificity, sera with values between lines a and b (n = 18) were considered true negatives by ELISA, since all of them were negative by Western blotting. All serum samples were diluted 1/250. The cutoff was determined by 200 independent measurements of the negative-control serum and calculation of the range of values equal to 3 times the standard deviation. For a better overview, results for only 1/50 of the serum samples without subsequent Western blotting, randomly selected, are given.
Several approaches have been adopted to assess the prevalence of ticks and animals infected with F. tularensis (9, 23, 38), and a serosurvey of landscapers in an area of tularemia endemicity has been conducted (18). According to the reports of these studies, some of which have been located in Europe, tularemia might make a significant contribution to tick-borne zoonoses in Germany, and the risk of exposure to carcasses or excrement of small mammals that carry the pathogen might be underestimated. Tick-borne tularemia appears to be a mild illness, characterized by fever and cervical or occipital lymphadenopathy (34). Persons at particular risk include hunters, as recently reported from Austria (14). Five out of 149 (3%) hunters examined exhibited antibodies against F. tularensis, without severe clinical symptoms. Besides tularemia, these individuals were also disproportionately seropositive for a wide variety of other zoonotic pathogens. Yet only sparse efforts have been made in Germany to conduct systematic surveillance of natural foci of tularemia, such as hares (19), in order to forecast the enzootic situation and to take preventive measures. In addition, there is a need for increased awareness of the clinical entities that arise from such a zoonosis. Improved recognition of clinical syndromes, combined with laboratory investigations, will lead to higher diagnostic accuracy. Our study highlighted the availability of a variety of reliable laboratory means to ensure the diagnostic quality needed in this context.
Concluding remarks.
Among the assays evaluated, the combined usage of ELISA and confirmatory Western blotting seems to be the most suitable approach for serodiagnosis of tularemia. Microagglutination has advantages in terms of costs and the equipment needed and is therefore preferable in laboratories without sophisticated equipment or during field investigations (31). However, cross-reactions with Brucella, Y. enterocolitica, and Proteus spp. have to be considered. Even though the preparation of the antigen for the indirect immunofluorescence assay is most convenient and implementation of the assay is simple, its employment is hampered by the lack of test efficiency. However, an experienced investigator can compensate for this disadvantage. Flow cytometry has been tested for the first time as a new platform for serodiagnosis of tularemia. Our initial findings suggest that in terms of test efficiency, it is superior to ELISA and comparable to Western blotting and microagglutination. The lack of commercial availability of diagnostics and the cost-intensive, highly sophisticated technical equipment required may hamper its usage in routine diagnostic work. However, the use of array-based applications might allow the development of high-throughput or multiplex analyses on this platform in the future.
Acknowledgments
We thank Mandy Macholeth, Ulli Hohenester, and Frank Feist for excellent technical assistance.
REFERENCES
- 1.Aronova, N. V., and N. V. Pavlovich. 2001. Comparative analysis of the immune response of a rabbit to antigens to live and killed Francisella species bacteria. Mol. Gen. Mikrobiol. Virusol. 2001:26-30. (In Russian.) [PubMed] [Google Scholar]
- 2.Behan, K. A., and G. C. Klein. 1982. Reduction of Brucella species and Francisella tularensis cross-reacting agglutinins by dithiothreitol. J. Clin. Microbiol. 16:756-757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bellach, B. M., H. Knopf, and W. Thefeld. 1998. The German Health Survey, 1997/98. Gesundheitswesen 60(Suppl. 2):S59-S68. (In German.) [PubMed] [Google Scholar]
- 4.Berdal, B. P., R. Mehl, H. Haaheim, M. Loksa, R. Grunow, J. Burans, C. Morgan, and H. Meyer. 2000. Field detection of Francisella tularensis. Scand. J. Infect. Dis. 32:287-291. [DOI] [PubMed] [Google Scholar]
- 5.Bevanger, L., J. A. Maeland, and A. I. Kvan. 1994. Comparative analysis of antibodies to Francisella tularensis antigens during the acute phase of tularemia and eight years later. Clin. Diagn. Lab. Immunol. 1:238-240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bevanger, L., J. A. Maeland, and A. I. Naess. 1988. Agglutinins and antibodies to Francisella tularensis outer membrane antigens in the early diagnosis of disease during an outbreak of tularemia. J. Clin. Microbiol. 26:433-437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bevanger, L., J. A. Maeland, and A. I. Naess. 1989. Competitive enzyme immunoassay for antibodies to a 43,000-molecular-weight Francisella tularensis outer membrane protein for the diagnosis of tularemia. J. Clin. Microbiol. 27:922-926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bhatti, A. R., J. P. Wong, and D. E. Woods. 1993. Production and partial characterization of hybridoma clones secreting monoclonal antibodies against Francisella tularensis. Hybridoma 12:197-202. [DOI] [PubMed] [Google Scholar]
- 9.Billings, A. N., J. A. Rawlings, and D. H. Walker. 1998. Tick-borne diseases in Texas: a 10-year retrospective examination of cases. Tex. Med. 94:66-76. [PubMed] [Google Scholar]
- 10.Burke, D. S. 1977. Immunization against tularemia: analysis of the effectiveness of live Francisella tularensis vaccine in prevention of laboratory-acquired tularemia. J. Infect. Dis. 135:55-60. [DOI] [PubMed] [Google Scholar]
- 11.Carlsson, H. E., A. A. Lindberg, G. Lindberg, B. Hederstedt, K. A. Karlsson, and B. O. Agell. 1979. Enzyme-linked immunosorbent assay for immunological diagnosis of human tularemia. J. Clin. Microbiol. 10:615-621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cerny, Z. 1991. Group immunity against tularemia in employees of the Zelenina Processing Plant in Brno. Cesk. Epidemiol. Mikrobiol. Imunol. 40:193-203. (In Czech.) [PubMed] [Google Scholar]
- 13.Conlan, J. W., H. Shen, A. Webb, and M. B. Perry. 2002. Mice vaccinated with the O-antigen of Francisella tularensis LVS lipopolysaccharide conjugated to bovine serum albumin develop varying degrees of protective immunity against systemic or aerosol challenge with virulent type A and type B strains of the pathogen. Vaccine 20:3465-3471. [DOI] [PubMed] [Google Scholar]
- 14.Deutz, A., K. Fuchs, W. Schuller, N. Nowotny, H. Auer, H. Aspock, D. Stunzner, U. Kerbl, C. Klement, and J. Kofer. 2003. Seroepidemiological studies of zoonotic infections in hunters in southeastern Austria—prevalences, risk factors, and preventive methods. Berl. Munch. Tierarztl. Wochenschr. 116:306-311. (In German.) [PubMed] [Google Scholar]
- 15.Ellis, J., P. C. Oyston, M. Green, and R. W. Titball. 2002. Tularemia. Clin. Microbiol. Rev. 15:631-646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ericsson, M., G. Sandstrom, A. Sjostedt, and A. Tarnvik. 1994. Persistence of cell-mediated immunity and decline of humoral immunity to the intracellular bacterium Francisella tularensis 25 years after natural infection. J. Infect. Dis. 170:110-114. [DOI] [PubMed] [Google Scholar]
- 17.Ericsson, M., A. Tarnvik, K. Kuoppa, G. Sandstrom, and A. Sjostedt. 1994. Increased synthesis of DnaK, GroEL, and GroES homologs by Francisella tularensis LVS in response to heat and hydrogen peroxide. Infect. Immun. 62:178-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Feldman, K. A., D. Stiles-Enos, K. Julian, B. T. Matyas, S. R. Telford III, M. C. Chu, L. R. Petersen, and E. B. Hayes. 2003. Tularemia on Martha's Vineyard: seroprevalence and occupational risk. Emerg. Infect. Dis. 9:350-354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Frolich, K., J. Wisser, H. Schmuser, U. Fehlberg, H. Neubauer, R. Grunow, K. Nikolaou, J. Priemer, S. Thiede, W. J. Streich, and S. Speck. 2003. Epizootiologic and ecologic investigations of European brown hares (Lepus europaeus) in selected populations from Schleswig-Holstein, Germany. J. Wildl. Dis. 39:751-761. [DOI] [PubMed] [Google Scholar]
- 20.Fulop, M. J., T. Webber, R. J. Manchee, and D. C. Kelly. 1991. Production and characterization of monoclonal antibodies directed against the lipopolysaccharide of Francisella tularensis. J. Clin. Microbiol. 29:1407-1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Greiser-Wilke, I., C. Soine, and V. Moennig. 1989. Monoclonal antibodies reacting specifically with Francisella sp. Zentbl. Veterinarmed. B 36:593-600. [DOI] [PubMed] [Google Scholar]
- 22.Grunow, R., W. Splettstoesser, S. McDonald, C. Otterbein, T. O'Brien, C. Morgan, J. Aldrich, E. Hofer, E. J. Finke, and H. Meyer. 2000. Detection of Francisella tularensis in biological specimens using a capture enzyme-linked immunosorbent assay, an immunochromatographic handheld assay, and a PCR. Clin. Diagn. Lab. Immunol. 7:86-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gurycova, D., V. Vyrostekova, G. Khanakah, E. Kocianova, and G. Stanek. 2001. Importance of surveillance of tularemia natural foci in the known endemic area of Central Europe, 1991-1997. Wien. Klin. Wochenschr. 113:433-438. [PubMed] [Google Scholar]
- 24.Gutierrez, M. P., M. A. Bratos, J. I. Garrote, A. Duenas, A. Almaraz, R. Alamo, M. H. Rodriguez, M. J. Rodriguez Recio, M. F. Munoz, A. Orduna, and A. Rodriguez-Torres. 2003. Serologic evidence of human infection by Francisella tularensis in the population of Castilla y Leon (Spain) prior to 1997. FEMS Immunol. Med. Microbiol. 35:165-169. [DOI] [PubMed] [Google Scholar]
- 25.Junhui, Z., Y. Ruifu, L. Jianchun, Z. Songle, C. Meiling, C. Fengxiang, and C. Hong. 1996. Detection of Francisella tularensis by the polymerase chain reaction. J. Med. Microbiol. 45:477-482. [DOI] [PubMed] [Google Scholar]
- 26.Kamennova, L. S., V. I. Pokrovskaia, V. P. Vasil'eva, L. I. Petrova, and V. B. Liubomudrov. 1983. Comparative study of the basic immunological reactions for assessing tularemia immunity in inoculated persons or those who have had the disease. Zh. Mikrobiol. Epidemiol. Immunobiol. 11:92-95. (In Russian.) [PubMed] [Google Scholar]
- 27.Koskela, P., and E. Herva. 1982. Immunity against Francisella tularensis in northern Finland. Scand. J. Infect. Dis. 14:195-199. [DOI] [PubMed] [Google Scholar]
- 28.Koskela, P., and A. Salminen. 1985. Humoral immunity against Francisella tularensis after natural infection. J. Clin. Microbiol. 22:973-979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Long, G. W., J. J. Oprandy, R. B. Narayanan, A. H. Fortier, K. R. Porter, and C. A. Nacy. 1993. Detection of Francisella tularensis in blood by polymerase chain reaction. J. Clin. Microbiol. 31:152-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Metz, C. E. 1978. Basic principles of ROC analysis. Semin. Nuclear Med. 8:283-298. [DOI] [PubMed] [Google Scholar]
- 31.Reintjes, R., I. Dedushaj, A. Gjini, T. R. Jorgensen, B. Cotter, A. Lieftucht, F. D'Ancona, D. T. Dennis, M. A. Kosoy, G. Mulliqi-Osmani, R. Grunow, A. Kalaveshi, L. Gashi, and I. Humolli. 2002. Tularemia outbreak investigation in Kosovo: case control and environmental studies. Emerg. Infect. Dis. 8:69-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sandstrom, G., A. Sjostedt, T. Johansson, K. Kuoppa, and J. C. Williams. 1992. Immunogenicity and toxicity of lipopolysaccharide from Francisella tularensis LVS. FEMS Microbiol. Immunol. 5:201-210. [DOI] [PubMed] [Google Scholar]
- 33.Sato, T., H. Fujita, Y. Ohara, and M. Homma. 1990. Microagglutination test for early and specific serodiagnosis of tularemia. J. Clin. Microbiol. 28:2372-2374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schmid, G. P., A. N. Kornblatt, C. A. Connors, C. Patton, J. Carney, J. Hobbs, and A. F. Kaufmann. 1983. Clinically mild tularemia associated with tick-borne Francisella tularensis. J. Infect. Dis. 148:63-67. [DOI] [PubMed] [Google Scholar]
- 35.Sjostedt, A., U. Eriksson, L. Berglund, and A. Tarnvik. 1997. Detection of Francisella tularensis in ulcers of patients with tularemia by PCR. J. Clin. Microbiol. 35:1045-1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Splettstoesser, W. D., R. Grunow, L. Rahalison, T. J. Brooks, S. Chanteau, and H. Neubauer. 2003. Serodiagnosis of human plague by a combination of immunomagnetic separation and flow cytometry. Cytometry 53A:88-96. [DOI] [PubMed] [Google Scholar]
- 37.Viljanen, M. K., T. Nurmi, and A. Salminen. 1983. Enzyme-linked immunosorbent assay (ELISA) with bacterial sonicate antigen for IgM, IgA, and IgG antibodies to Francisella tularensis: comparison with bacterial agglutination test and ELISA with lipopolysaccharide antigen. J. Infect. Dis. 148:715-720. [DOI] [PubMed] [Google Scholar]
- 38.Vyrostekova, V., G. Khanakah, E. Kocianova, D. Gurycova, and G. Stanek. 2002. Prevalence of coinfection with Francisella tularensis in reservoir animals of Borrelia burgdorferi sensu lato. Wien. Klin. Wochenschr. 114:482-488. [PubMed] [Google Scholar]
- 39.Zweig, M., and G. Campbell. 1993. Receiver operating characteristic (ROC) plots: a fundamental evaluation tool in clinical medicine. Clin. Chem. 39:561-577. [PubMed] [Google Scholar]