Supplemental Digital Content is available in the text
Keywords: age–period–cohort model, gastric cancer, incidence, mortality rate, population-based cancer registry
Abstract
Gastric cancer (GC) is the second leading cause of cancer death in China. It is well known that Cixian in Hebei Province is one of the highest risk areas of GC in China and worldwide. This study aims to accurate assessment of GC burden and trend in high-risk area (Hebei Province) from 1973 to 2013. The authors analyzed GC data from 21 population-based cancer registries which represented 15.25% of the entire population of Hebei Province. The collected data were stratified by 5-year age groups, gender, and area. Mortality of GC was extracted from national death surveys from 1973 to 1975, 1990 to 1992, 2004 to 2005, and 2011 to 2013. Trend analysis (1988–2013) in a high-risk area (Cixian) used the Joinpoint Model. The age–period–cohort model was used to estimate the effects of age, period, and birth cohort in GC incidence in Cixian from 1988 to 2013. The crude incidence of GC in 2011 to 2013 was 40.37/100,000 (57.53/100,000 in males and 22.55/100,000 in females). The corresponding age-standardized rate by world age-standard population was 32.18/100,000 (48.87/100,000 in males and 17.53/100,000 in females), which was 2.66-fold (2.81-fold in male and 2.34-fold in female) higher than that in the world (12.1/100,000, 17.4/100,000 in males and 7.5/100,000 in females). Males in rural areas had the highest incidence, with an age-standardized rate of 70.51/100,000. Gastric cardia cancer was primary anatomical subsite which accounting for 59.59% in GC, followed by gastric corpus (13.92%), gastric antrum (11.43%), gastric fundus (4.99%), and overlapping lesion of gastric (4.17%). The age-standardized rate of mortality from GC displayed a significant downward trend (P = 0.019) in Hebei Province from the 1990s (31.44/100,000) to the 2010s (24.63/100,000). In Cixian, the incidence of GC rose from 1988 (38.25/100,000) to 2009 (65.11/100,000). Cixian, where population-based screening of upper gastrointestinal cancer was performed, experienced the increasing rate of GC from 2000 (37.59/100,000) to 2009 (65.11/100,000) and then had a sharp decrease from 2009 to 2013 (55.30/100,000), with annual percentage change of −6.69%. Gastric cardia cancer had an increasing trend from 1988 (6.88/100,000) to 2013 (26.56/100,000). Both age and birth cohort effects played important roles in these changes. In conclusion, males in rural areas had the highest risk of GC. GC mortality rate decreased from the 1990s in Hebei Province. Endoscopic screening project for GC is an effective method of controlling the disease.
1. Introduction
According to Globocan 2012, gastric cancer (GC) was the fifth most common cancer worldwide and was also the third leading cause of death across all types of cancer in the world. Its incidence and mortality rate represented approximately 6.8% and 8.8% among all malignancies, respectively.[1] Although incidence and mortality of GC have been substantially falling in some regions, 5-year survival rate of GC is still less than 25%.[2–5] GC represents a tremendous burden in developing country, including China.
The incidence and mortality rate of GC distinctly varies in different geographical areas. More than 70% of cases happened in developing countries, and approximately 50% of total cases occurred in China. Moreover, the distribution of GC in China presents significant regional disparity. Hebei Province is located in North China along the Taihang Mountain chain, with a relatively developing economy. It was recognized as high-risk area of GC in 1970s. In 2015, it had 21 population-based cancer registries that covered 11,185,626 households (approximately 15.25% of the total population in Hebei Province). In addition, Hebei Province participated in 3 national death surveys which were conducted during the periods of 1973 to 1975,[6] 1990 to 1992,[7,8] and 2004 to 2005.[9] Cixian, one of counties in Hebei Province, showed a 2.4-fold higher mortality rate than the national level.[10] The high risk of GC in this region aroused the interest of researchers, a series of investigations regarding potential risk factors and etiological prevention methods were conducted. In addition, the cancer registry was established in 1974.
The study provides an updated outline of GC burden and subcategory of GC in Hebei Province for the first time. We also analyzed mortality data from 1970s to 2013 to explore the underlying causes of the observed changes. It also presents the epidemiological character of GC in Cixian. Monitoring and studying the incidence as well as mortality provides important information, which enables effective assessment and generates strategy of potential GC prevention and control based on the different distribution patterns. It may guide for research directions for GC prevention and treatment and may act as a sentinel for other areas of China.
2. Materials and methods
2.1. Data source
The Hebei Provincial Cancer Registry in China was established in 2009, and it is responsible for cancer data collection, evaluation, and publication. To date, it has 21 local population-based registries that include 16 counties (Cixian, Shexian, Qianxi, Wu’an, Zanhuang, Fengning, Xingtai, Xinji, Zhangbei, Haixing, Yanshan, Xuanhua, Anguo, Neiqiu, Renxian, and Shenze) and 5 cities (Baoding city, Qinhuangdao city, Cangzhou city, Shijiazhuang city, and Chengde city). The reported cases were from multiple sources, including local hospitals, community health centers, as well as the Urban Resident Basic Medical Insurance Program and the New Rural Cooperative Medical Scheme. All the data on cancer in Hebei Province were obtained from the Hebei Cancer Registry database, and we also extracted incidence and mortality data on GC from 1988 to 2013 in Cixian. According to the International Classification of Diseases for Oncology, third edition, GC, which is C16.0 to C16.9, was the focus of the analysis. The anatomical subsite was assigned by the World Health Organization (WHO) classification: gastric cardia, gastric fundus, gastric corpus, gastric antrum, gastric pylorus, gastric lesser curvature, gastric greater curvature, overlapping lesion of gastric, and unspecified (Supplementary figure 1). Our study did not use personal information from cancer registry data. Institutional review board approval and informed consent were not applicable for this study.
2.2. National retrospective survey of mortality
In the mid-1970s, a nationwide retrospective survey on the causes of mortality was conducted in 29 provinces, including all 153 cities and counties covering 47.725 million people in Hebei Province.[6] The registry provided a profile of cancer mortality in Hebei Province.
The second national retrospective sampling survey on cancer mortality was held from 1990 to 1992. This survey used a stratified sampling method and covered approximately 10% of the population in China.[7,8] A total of 21 cities and counties covering 6.375 million people from Hebei Province were enrolled as sampling areas.
The third national retrospective stratified sampling survey on all causes of death, performed from 2004 to 2005, was conducted in 31 provinces/municipalities/autonomous regions and included Hebei Province. A total of 18 cities and counties were selected as sampling areas covering 13.79 million people with 20.15% of total population of Hebei Province.[9]
2.3. Quality control
The inclusion criteria for data were based on the Guidelines of Chinese Cancer Registration[11] and the International Agency for Research on Cancer (IARC)/International Association of Cancer Registries.[12] We assessed the data quality using MS-Excel (Excel, Microsoft Corp.; Redmond, WA), SAS (version 9.2, SAS Institute Inc.; Cary, NC), and IARC Tools (IARC; Lyon, France). The analyzed data are required to meet the basic inclusion criteria, which are the percentage of morphological verification higher than 66%, the percentage of cancer cases identified with death certification only less than 15%, and the mortality-to-incidence ratio between 0.6 and 0.8.
2.4. Statistical analysis
All data analyses were performed with SPSS (version 20, Inc; Chicago, IL), SAS, and Ms-Excel. The world age-standardized rate (ASRW) and Chinese age-standardized rate (ASRC) were calculated by Segi population and the Chinese population in 2000. The cumulative rate (Cum) (aged 0–74 years) is the risk of developing or dying from cancer before the age of 75 years. Long-term trends of GC in Cixian were analyzed using Joinpoint regression software (version 4.0.4, US National Cancer Institute; Bethesda, MD). The slope of the regression equation can estimate annual percentage change (APC). We also used the age–period–cohort model to estimate the effect of age, period, and birth cohort of GC in Cixian from 1988 to 2013. We extracted 13 5-year age groups from 25 to 29 to 85+ years and 5 periods ranging from 1988 to 1992 to 2008 to 2013, producing birth cohorts from 1903 to 1907 to 1983 to 1988. The 3 components (cohort, period, and age) in the age–period–cohort model are linearly dependent. Therefore, we adopted the common method of an additional arbitrary reference constraint for the period effect.[13–15] In addition, the over 85-year age group, the periods of 2003 to 2007 and 2008 to 2013, and the birth cohort of 1908 to 1912 were chosen as reference groups.
3. Results
3.1. Gastric cancer incidence rate in 2011 to 2013
During the period of 2011 to 2013, the cancer registries covered 15.25% of the residents in Hebei Province (including 20,745,718 person-year populations). In addition, there were 8375 new GC diagnosis cases (6081 in males and 2294 in females) in cancer registry areas that accounted for 16.97% of all types of cancer. The crude rate across all areas was 40.37 per 100,000. The ASRW was 32.18/100,000, and the ASRC was 32.44/100,000. The Cum for 0- to 74-year-old patients was 4.09% (Table 1). Almost 80% of new cases (6716 cases) were in rural cancer registries. The incidence was 3.09-fold higher in rural areas (57.07/100,000) than in urban areas (18.48/100,000). The male rate in rural areas (81.68/100,000) was the highest. It showed that GC was more prevalent in males than in females after 40-year-old age groups, no matter in rural or in urban. The incidence reached a peak at 75-year-old age group in males in rural areas and others who reached the highest rate was in the over 85-year-old age group (Fig. 1).
Table 1.
Gastric cancer incidence in Hebei Province, 2011 to 2013.
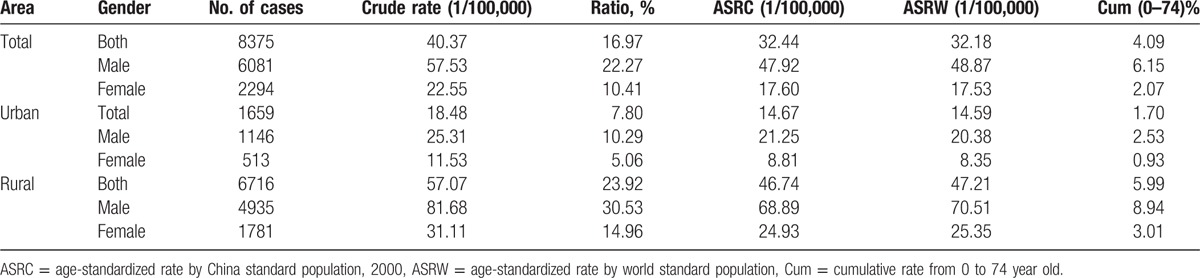
Figure 1.
Age-specific incidence rate of gastric cancer in 2011 to 2013.
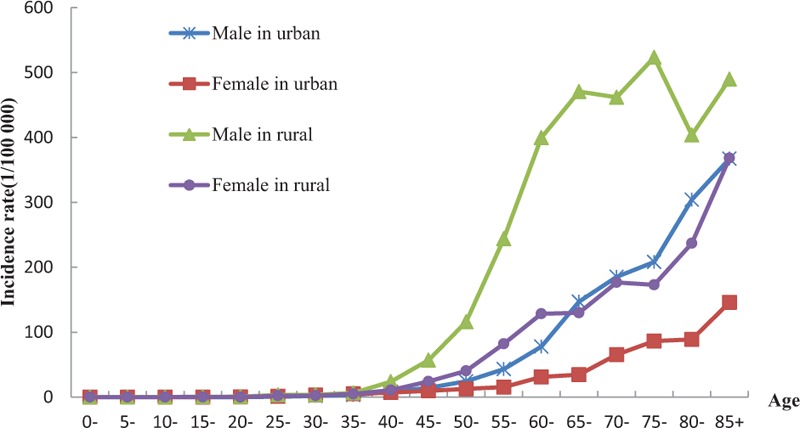
3.2. Anatomical subsite-specific distribution of gastric cancer
There were a total of 5108 (60.99%) cases diagnosed with anatomical subsite of GC in 2011 to 2013. For all groups, gastric cardia cancer occupied the highest proportion of GC. It accounted for 59.59% of all cases, followed by gastric corpus (13.92%), gastric antrum (11.43%), gastric fundus (4.99%), and overlapping lesion of gastric (4.17%). The proportion of gastric cardia cancer in male (61.72%) was much higher than that of the female (53.57%). On the other side, the proportion of gastric corpus and gastric antrum in male were much lower than that in female. In urban areas, gastric antrum cancer was the second most common subsite of GC. While gastric corpus cancer ranked second in all subsite of gastric in rural areas. In the age group of below 45 years, gastric corpus cancer and gastric antrum cancer ranked as the second and the third, respectively. Distribution of GC in other age groups was similar with the total trend (Table 2, Supplement figure 1).
Table 2.
Subsite-specific distribution of gastric cancer in 2011 to 2013.
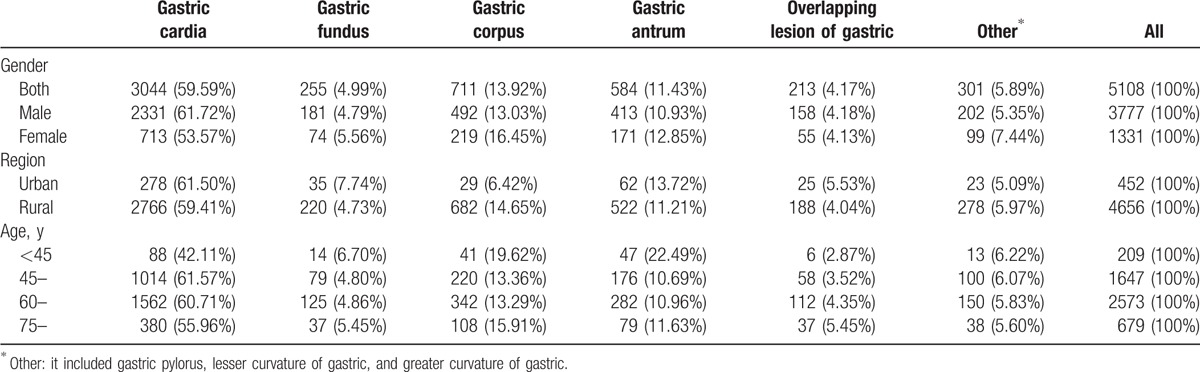
3.3. The mortality trend of GC
In 2011 to 2013, the ASRW mortality rate of male (35.20/100,000) was 2.35-fold higher than that in female (14.99/100,000). The median age of death (interquartile range [QR]) in female (70 [18]) was more than that in male (68 [16]). Though an increased crude mortality rate for GC was observed from 1973 to 1975 (19.67/100,000) and 2011 to 2013 (29.66/100,000), the ASRW mortality rate and the GC proportion of all kinds of cancer in 2011 to 2013 were significantly decreasing from 1990s (P = 0.019). The ASRW mortality decreased 21.66% from 1990 to 1992 (31.44/100,000) to 2011 to 2013 (24.63/100,000). The rate was basically flat in the 1970s. The proportion of GC in all kinds of cancer dropped 20.88% from 1990 to 1992 (24.33%) to 2011 to 2013 (19.25%). Meanwhile, the median age of death (QR) was increasing from 65 (14) to 68 (17) years during the same period. For males and females, the trend for ASRW was similar to the overall trend (Table 3, Fig. 2A and B).
Table 3.
The mortality of gastric cancer in Hebei Province from 1970s to 2013.
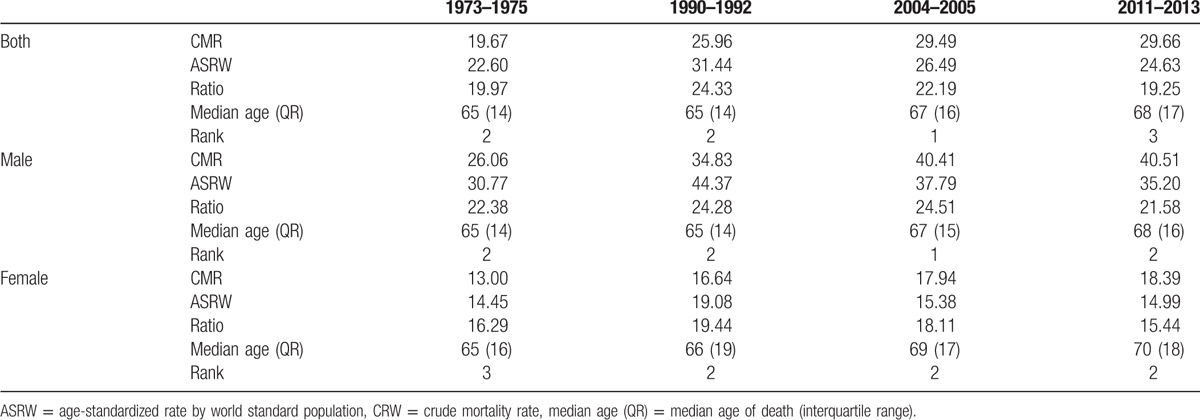
Figure 2.
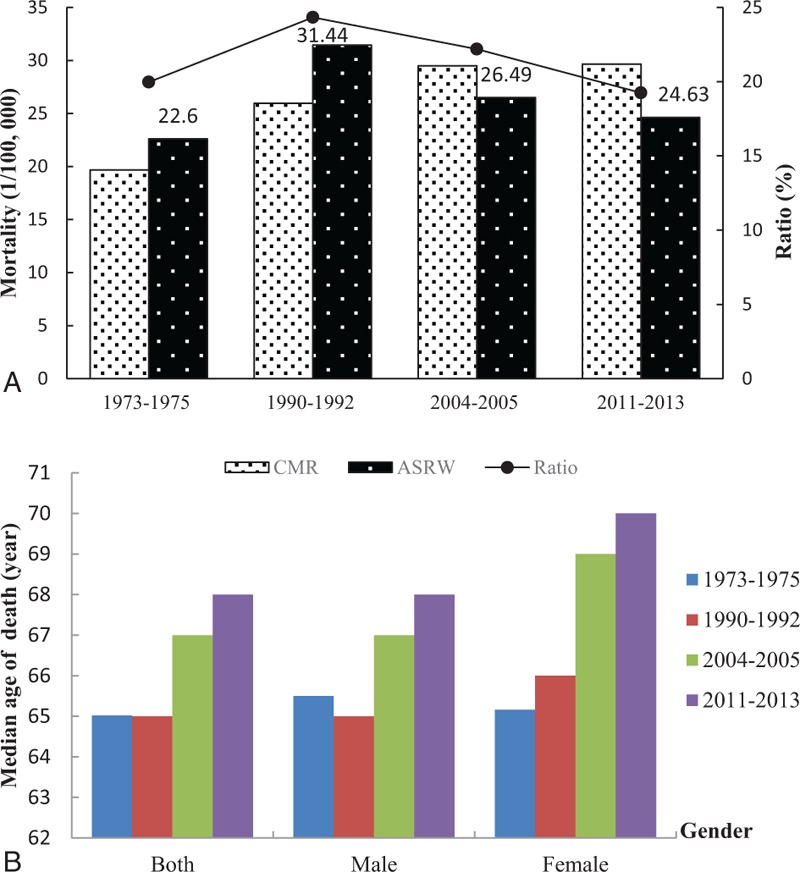
Described mortality trend of gastric cancer from 1970s to 2010s. (A) Mortality rate and ratio of GC. (B) Median age of death because of gastric cancer. ASRW = age-standardized rate by world standard population, CMR = crude mortality rate.
3.4. Trend of GC incidence in Cixian which was a high-risk area
3.4.1. Annual percentage change in rate
According to the results of the Joinpoint model, the APCs in adjusted incidence rate of GC in Cixian were 1.71% and −6.69% in 1988 to 2009 and 2009 to 2013, respectively. For both sexes, males and females, the incidence rate in Cixian decreased in 2009. Significant increasing trend was observed for gastric cardia cancer from 1970s (P < 0.05). In contrast, noncardia GC was decreasing in 1988 to 2001 with the APCs of −5.25%, while it kept stable from 2001 to 2013 (APC = 0.29%) (Fig. 3).
Figure 3.
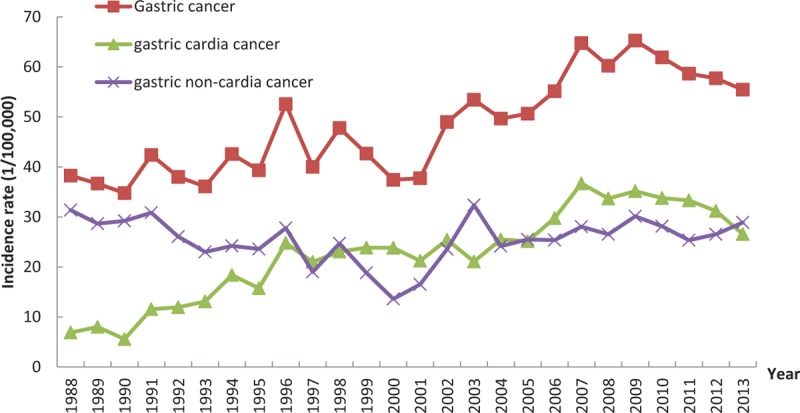
Age-specific incidence rate of gastric cancer, cardia cancer, and noncardia cancer in Cixian from 1988 to 2013. Gastric cancer: the annual percentage change (APC) was 1.71% in 1988 to 2009 (P < 0.05); gastric cardia cancer: APC was 16.76% in 1988 to 1996 and 2.74% in 1996 to 2013 (P < 0.05).
3.4.2. Age, period, and cohort effects in Cixian
In general, the trend of GC's incidence rate was decreased by the year of birth. The incidence rate was increased after decreasing, and then decreased again above 55-year age group, whereas it remained steady at age 25 to 54 years (Table 4, Fig. 4).
Table 4.
Incidence of gastric cancer in Cixian (1988–2013), by period.
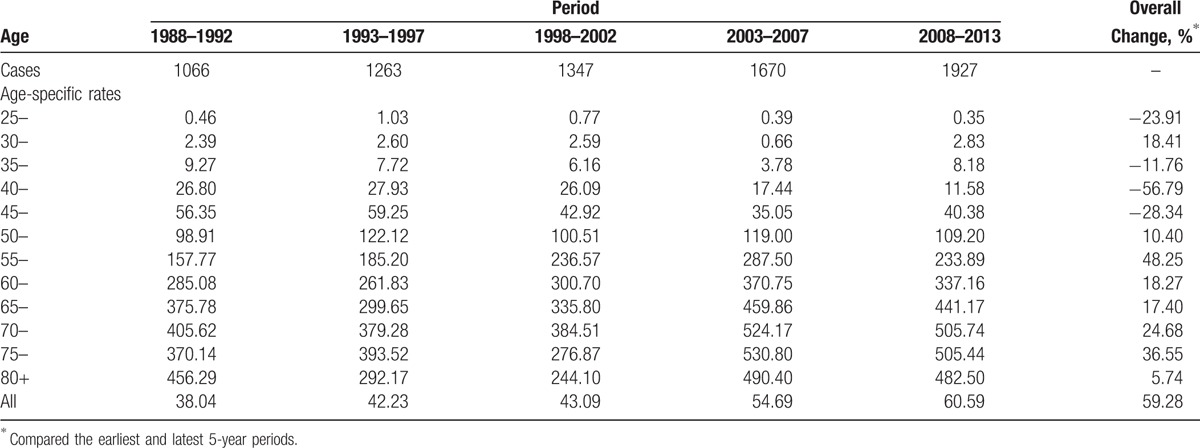
Figure 4.
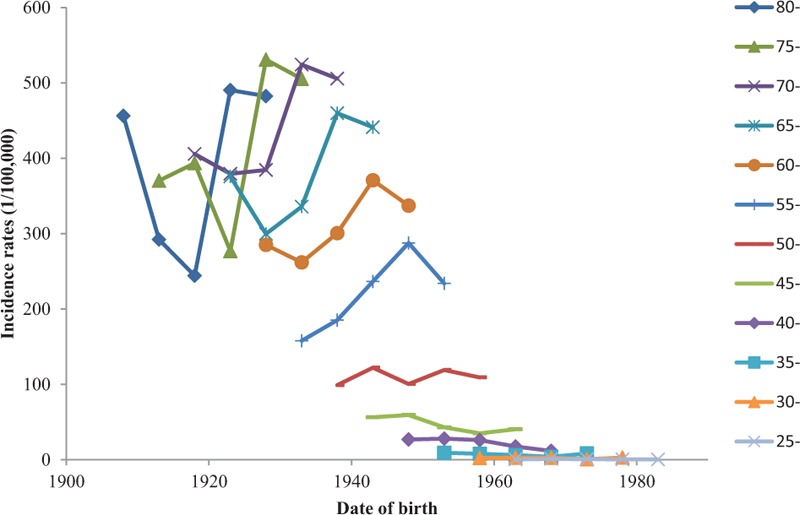
Age-specific gastric cancer in Cixian, by birth cohort.
Age, period, and cohort effects contributed to the observed changes in GC incidence. A model including 3 components fit best, as indicated by having the lowest Akaike Information Criterion Values (512.47).
Incidence increased with age and decreased with cohort. The figure regarding age effects showed an increase in incidence in those aged 25 to 69 years and indicated that the 70 to 74 years had the highest relative risk (RR = 1.45) compared with the reference group (85+-year-old age group). The birth cohort effect indicated a consistent decline in incidence in all cohorts for those who were born in the early 1900s, with the exception of those born in 1918 to 1923, 1938 to 1945, and 1970 to 1978. The highest RR was 1.15 in the 1903 to 1907 birth cohort compared with the reference birth cohort in 1908 to 1912. The RR of period effects in 1988 to 1997 was lower than that of the reference groups. We found that in 1994 to 1999, the rates of GC in 80- and over 85-year-old group were very low. The corresponding birth cohort was approximately in 1915. In addition, in the 1913 cohort, the RR was relatively lower (Fig. 5).
Figure 5.
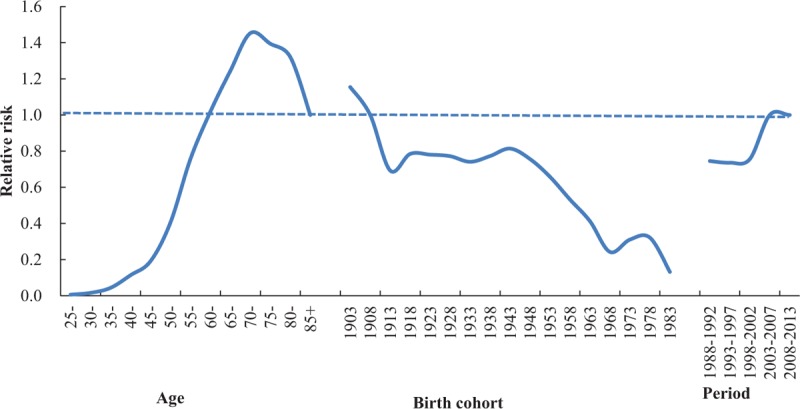
The estimation of age, period, and birth cohort effects of gastric cancer incidence in Cixian, 1988 to 2013.
4. Discussion
In this study, we provide the GC burden, anatomical subsite of GC in Hebei Province and trends of GC incidence rate in Cixian which was a high-risk area for GC during the years of 1988 to 2013. In addition, our study is also the first in-depth analysis of burden and trend in GC in Hebei Province. We found that males in rural areas were the predominant population of developing GC. In addition, gastric cardia was the primary anatomical subsite of GC, followed by gastric corpus, gastric antrum, gastric fundus, and overlapping lesion of gastric. The age-standardized mortality rate and the ratio of GC in all kinds of cancer had a downward trend from 1990s. GC incidence rate Cixian was observed as an increasing trend from 1988 to 2009 and then had a decreasing trend from 2009.
The crude incidence of GC was 40.37/100,000 in Hebei Province in 2011 to 2013, which was approximately 1.3 times higher than the overall Chinese incidence (31.28/100,000).[11,16] After adjusting for Segi population, the adjusted incidence was 32.18/100,000, which was 2.66-fold higher than the worldwide rate (12.1/100.000).[1] In Hebei Province, newly diagnosed GC cases occupied 16.97% of all types of new cancer, while the ratio was only 6.8% in the world. For both sexes, males and females, the incidence in urban area (14.59/100,000, 20.38/100,000, and 8.35/100,000, respectively) were consistent with those worldwide level (12.1/100,000, 17.4/100,000, and 7.5/100,000). However, in rural areas, the ASRW incidence rate (47.21/100,000) was 3.90-fold higher than the worldwide GC incidence (12.1/100,000). The ASRW incidence rates of males (70.51/100,000) and females (25.35/100,000) in rural areas were 4.05- and 3.38-fold higher than those worldwide (17.4/100,000 in males and 7.5/100,000 in females), respectively. Its incidence ranked the second, and mortality ranked the third among all types of cancer. The adjusted mortality rate in Hebei Province (24.63/100,000) also presented 1.62- and 2.77-fold higher than that in China (15.16/100,000) and world (8.9/100,000). The ASRW mortality rate in male (35.20/100,000) and female (14.99/100,000) was 2.75 and 2.63 times the world's level (12.8/100,000 in males and 5.7/100,000 in females). The proportion of GC in all cancer cases was 19.25%, while in the world it was only 8.8%. According to the data analysis, we found that GC was a major disease burden in Hebei Province. Males in rural areas of Hebei Province were high-risk population and accounted for 58.93% of all new GC cases. GC remains a tremendous health problem and cause of mortality in Hebei Province. Males in rural areas hold a large proportion of GC incidence and mortality.
The pathogenesis of gastric carcinoma is not fully understood. Economic, environmental, and genetic risk factors may be responsible for the high incidence and mortality rates of the disease.[17–20] First of all, low socioeconomic conditions may increase the incidence and mortality rates of GC.[21] Low socioeconomic status has been closely associated with limited education, poor living conditions, and limited medical care.[22–24] Based on the 2012 worldwide data, nearly 57% of new GC cases and 65% of cancer deaths occurred in less-developed regions.[1] For Hebei Province, there was an approximately 80.19% increase in newly diagnosed cases in rural areas from 2011 to 2013. The per capita annual net incomes of rural and urban households were approximately ¥6539 and ¥17,278 in the 2010s in Hebei Province.[25] Second, behavioral risk factors could increase the chance of developing gastric carcinoma, such as tobacco smoking exposure, high intake of salty and smoked foods, and low consumption of vegetables and fruit. The IARC indicates that there is a causal association between smoking and GC.[26] A meta-analysis of cohort studies indicated that male smokers may increase their risk of developing GC by 60% (RR = 1.6).[27] In China, the smoking rate was 52.9% for males, and the second-hand smoking rate was approximately 72.4%, which was significantly higher than that worldwide.[28] In Hebei Province, the cigarette smoking rate of both sexes was 26.08%, and it was 48.09% for males.[29] In addition, the popularity of eating salty and smoked foods contributed to a high risk of GC in Hebei Province in rural areas. The World Cancer Research Fund/American institute for Cancer Research has concluded that “salt, and also salt-preserved food, are probably causes of GC.”[30] The meta-analysis also showed that consumption of highly salty foods may increase the risk of GC by 22%.[31] Due to low economic conditions, pickles with starchy grains were the main food in rural areas. Fresh vegetable consumption in rural areas was lower than that in urban areas. The third reason for the high GC rate was the high rate of Helicobacter pylori infection. The WHO had classified H. pylori as a class I carcinogen in 1994,[32] and this has been reinforced more recently by the IARC.[33] The research reported that nearly 74.7% of all the noncardia GCs being related to this infection.[34] Over the last 2 decades, researchers had indicated that H. pylori may be an incontrovertible cause of noncardiac GC, with an RR of approximately 6 (RR ≈ 6.0).[35,36] The study demonstrated that there were significant differences between urban and rural areas in Hebei Province and that the incidence of H. pylori infection increased from the plains to the mountains.[37] The last reason for increased GC involved geographical factors. Some high-risk areas of GC in China are located along the Taihang Mountain chain, such as Cixian and Shexian in Hebei Province. The research showed that the levels of nitrate, nitrite, nitrogen, and ammonia in drinking water in high-risk areas, which were 7 times higher than in low-risk regions, exceeded the national standards for drinking water.[38] The IARC has demonstrated that nitrate and nitrite could lead to GC. Other risk factors, including genetic variation, family history, and life habits, may also play an important role in GC.[2] These factors may be associated with the high incidence and mortality rate of GC in rural areas in Hebei Province.
According to data analysis, we found that mortality rate of GC in Hebei Province decreased from 1970s to 2010s, which consisted with the trend observed in most parts of the world.[39,40] In Hebei Province, data from cancer registry indicated that mortality rate in 2011 to 2013 had decreased by 0.04%, 21.66%, and 13.25% compared with the 3 National Causes of Death Sampling Survey (1973–1975, 1990–1992, and 2004–2005), respectively. In the period from the 1970s to the 1990s, the mortality rate increased sharply. Then, mortality rate was decreasing from 1990s. However, the overall mortality rate showed a downward trend in the period between 1990s and 2010s. In those periods, increased life expectancy and improvements in the diagnosis of cancer may also contribute to the high mortality rates in recent years in the aging population. A total of 80+-year-old age group incidence was 1.44-fold higher in 2010s than in 1970s, with rates of 270.75 and 188.05 per 100,000, respectively. In particular, in males, the mortality rate rose more quickly than in females on aging. The ratio of GC in all causes of cancer dropped steadily from 24.33% to 19.25 %during from 1990–1992 to 2011–2013.
From 1990s to now, we had enhanced primary and secondary prevention of GC to project the burden of this health issue. Because of nonclinical symptoms in the early stages of disease, many patients are treated for GC in the advanced stages. Primary prevention, such as smoking cession, reducing salty food intake, and improving health habits, may be useful for reducing the incidence and mortality rate of GC in high-risk areas. In addition, the socioeconomic conditions and healthy living behaviors had improved. The most important measure is endoscopic examination screening in population who have a family history of GC or aged 45 years and older.[41] Cixian and Shexian have been chosen as demonstration bases of endoscopic examination screening for upper gastrointestinal cancer including GC. More efforts have been put into screening and early detection to identify precancerous lesions of GC. Since 2000, a national screening program using endoscopy with mucosal iodine staining and index biopsy combined with pathological examination for confirming and staging the disease had become available at 17 areas in Hebei Province, including Cixian and Shexian.[28] Checkout of cancer rate was about 2%, and the early detection rate could reach 80%. It is one of the possibilities of the decreasing trend.
Cixian was chosen as a point of endoscopic screening of upper gastrointestinal cancer in 2000. It performed the first round of population-based screening from 2000 to 2009. Using endoscopic technology as an early detection and treatment method, the number of cancer cases increased in 2000 to 2009, and the incidence rate increased over the next 10 years from 2000. During the process of screening, the project covered 10,914 people. High-risk population was found and treated. In addition, we followed high-risk population by doctors every year. In 2009, the incidence reached a peak with 65.11/100,000. Endoscopy with mucosal iodine staining was a sensitive technique for identifying clinically relevant upper gastrointestinal cancer. Sensitivity and specificity of endoscopy examinations were about 80% and 93.4%, respectively.[42] For identifying early GC, the specificity is dramatically increased with the aid of biopsy and histologic diagnosis. The 5-year survival rate of early GC could reach 90%. In this program, the residents were educated about healthy behaviors and improving their awareness, which reduced the incidence of GC. Through 10-year efforts, the incidence rate of GC in Cixian experienced a sharp decrease from 2009 to 2013. The program shows that endoscopy with mucosal iodine staining and index biopsy combined with pathological examination is necessary for rural areas.
Our study has described the incidence, mortality, and temporal trends of GC in Hebei Province, which is a high-risk area for GC in China. Gastric cardiac was the primary anatomic subsite in GC. Males in rural areas were the predominant population developing GC. The condition was strongly associated with geographical factors, life habits, and genetic variation. Our study also had some limitations. The survey could not cover the total population of Hebei Province. In addition, we do not have long-term incidence data on GC in Hebei Province. We own only Cixian county data from 1988 to 2013. According to the data analyzed herein, we should focus on primary and secondary prevention in rural areas.
Supplementary Material
Acknowledgments
We gratefully thank the cooperation partner of all population-based cancer registries in Hebei Province for providing cancer data, sorting, and verifying cancer data. The authors assume full responsibility for the analyses and interpretations of the data.
Footnotes
Abbreviations: APC = annual percentage change, ASRC = age-standardized rate by the Chinese population in 2000, ASRW = age-standardized rate by world Segi population, Cum = cumulative rate, GC = gastric cancer, IARC/IACR = International Agency for Research on Cancer/International Association of Cancer Registries, QR = interquartile range.
Funding/support: The study was supported by grants from the National Natural Scientific Foundation of China (81272682).
The authors have no conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 2010;127:2893–917. [DOI] [PubMed] [Google Scholar]
- [2].Pasechnikov V, Chukov SJ, Fedorov E, et al. Gastric cancer: prevention, screening and early diagnosis. World J Gastroenterol 2014;20:13842–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Parkin DM. Global cancer statistics in the year 2000. Lancet Oncol 2001;2:533–43. [DOI] [PubMed] [Google Scholar]
- [4].Zeng H, Zheng R, Guo Y, et al. Cancer survival in China, 2003–2005: a population-based study. Int J Cancer 2015;136:1921–30. [DOI] [PubMed] [Google Scholar]
- [5].Lin YS, Ueda J, Kikuchi S, et al. Comparative epidemiology of gastric cancer between Japan and China. World J Gastroenterol 2011;17:4421–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Cancer Prevention and Control, Ministry of Health, P.R. China Malignant Tumor Mortality Survey Report. 1st ed.1980;Beijing:People's Medical Publishing House, 53–70. [Google Scholar]
- [7].Cancer Prevention and Control, Ministry of Health, P.R. China Survey of Cancer Mortality in China 1990–1992. 1st ed.1993;Beijing:People's Health Publishing House, 165–192. [Google Scholar]
- [8].Zhang GS, He YT, Hou J. The geographical distribution of cancer death in Hebei Province 1990–1992. Chin Cancer 1998;7:5–21. [Google Scholar]
- [9].Cancer Prevention and Control, Ministry of Health, P.R. China Malignant Tumor Mortality Survey Report (2004–2005). 1st ed.2007;Beijing:People's Medical Publishing House, 256–291. [Google Scholar]
- [10].Chen WQ, Zhang SW, Chen ZF. An epidemiologic trend analysis on cardiac cancer in high incidence areas of esophageal cancer and gastric cancer in China. Chin Cancer 2008;17:668–70. [Google Scholar]
- [11].National Cancer Center, Ministry of Health, P.R. China Chinese Cancer Registry Annual Report 2012. 1st ed.2012;Beijing:People's Medical Publishing House, 16–17. [Google Scholar]
- [12].Ferlay JBC, Whelan S, Parkin DM. Check and conversion programs for cancer registries (IARC/IACR Tools for Cancer Registries). IARC Technical Report No. 42. Lyon, France:IARC Press; 2005. [Google Scholar]
- [13].Jeon SY, Reither EN, Masters RK. A population-based analysis of increasing rates of suicide mortality in Japan and South Korea, 1985–2010. BMC Public Health 2016;16:356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Gangnon RE, Sprague BL, Stout NK, et al. The contribution of mammography screening to breast cancer incidence trends in the United States: an updated age–period–cohort model. Cancer Epidemiol Biomarkers Prev 2015;24:905–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Ryan-Ibarra S, Milet M, Lutzker L, et al. Age, period, and cohort effects in adult lifetime asthma prevalence in California: an application of hierarchical age–period–cohort analysis. Ann Epidemiol 2016;26:87–92. [DOI] [PubMed] [Google Scholar]
- [16].Chen WQ, Zheng RS, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin 2016;66:115–32. [DOI] [PubMed] [Google Scholar]
- [17].Kato M, Asaka M. Recent knowledge of the relationship between Helicobacter pylori and gastric cancer and recent progress of gastroendoscopic diagnosis and treatment for gastric cancer. Jpn J Clin Oncol 2010;40:828–37. [DOI] [PubMed] [Google Scholar]
- [18].Yaghoobi M, Bijarchi R, Narod SA. Family history and the risk of gastric cancer. Br J Cancer 2010;102:237–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Kobayashi M, Tsubono Y, Sasazuki S, et al. Vegetables, fruit and risk of gastric cancer in Japan: a 10-year follow-up of the JPHC Study Cohort I. Int J Cancer 2002;102:39–44. [DOI] [PubMed] [Google Scholar]
- [20].Shin CM, Kim N, Lee HS, et al. Intrafamilial aggregation of gastric cancer: a comprehensive approach including environmental factors, Helicobacter pylori virulence, and genetic susceptibility. Eur J Gastroenterol Hepatol 2011;23:411–7. [DOI] [PubMed] [Google Scholar]
- [21].Tabuchi T, Ito Y, Ioka A, et al. Tobacco smoking and the risk of subsequent primary cancer among cancer survivors: a retrospective cohort study. Ann Oncol 2013;24:2699–3270. [DOI] [PubMed] [Google Scholar]
- [22].Rahman R, Asombang AW, Ibdah JA. Characteristics of gastric cancer in Asia. World J Gastroenterol 2014;20:4483–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Mendoza D, Herrera P, Gilman RH, et al. Variation in the prevalence of gastric cancer in Perú. Int J Cancer 2008;123:414–20. [DOI] [PubMed] [Google Scholar]
- [24].Hu QD, Zhang Q, Chen W, et al. Human development index is associated with mortality-to-incidence ratios of gastrointestinal cancers. World J Gastroenterol 2013;19:5261–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Statistics Hebei Province. Available from: http://www.hetj.gov.cn/hetj/tjsj/. Accessed December 3, 2014. [Google Scholar]
- [26].IARC Working Group on the Evaluation of Carcinogenic Risks to Humans IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Ingested nitrate and nitrite, and cyanobacterial peptide toxins. IARC Monogr Eval Carcinog Risks Hum 2010;94:v–ii. 1–412. [PMC free article] [PubMed] [Google Scholar]
- [27].Ladeiras-Lopes R, Pereira AK, Nogueira A, et al. Smoking and gastric cancer: systematic review and meta-analysis of cohort studies. Cancer Causes Control 2008;19:689–701. [DOI] [PubMed] [Google Scholar]
- [28].National Health and Family Planning Commission of the PRC. 2015 report on Chinese nutrition and chronic disease. NHFPC Beijing, 2015. [Google Scholar]
- [29].Lu A, Wang X, Gao G. Comparative study on cigarette smoking between urban and rural residents in Hebei Province. Chin J Public Health 2005;21:908–9. [Google Scholar]
- [30].Wiseman M. The second World Cancer Research Fund/American Institute for Cancer Research expert report. Food, nutrition, physical activity, and the prevention of cancer: a global perspective. Proc Nutr Soc 2008;67:253–6. [DOI] [PubMed] [Google Scholar]
- [31].Ge S, Feng X, Shen L, et al. Association between habitual dietary salt intake and risk of gastric cancer: a systematic review of observational studies. Gastroenterol Res Pract 2012;2012:808120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].IARC Working Group on the Evaluation of Carcinogenic Risks to Humans Schistosomes, liver flukes and Helicobacter pylori. IARC Monogr Eval Carcinog Risks Hum 1996;61:1–241. [PMC free article] [PubMed] [Google Scholar]
- [33].IARC Working Group on the Evaluation of Carcinogenic Risks to Humans Diesel and gasoline engine exhausts and some nitroarens. IARC Monogr Eval Carcinog Risks Hum 2014;105:9–699. [PMC free article] [PubMed] [Google Scholar]
- [34].Martel C, Ferlay J, Franceschi S, et al. Global burden of cancers attributable to infections in 2008: a review and synthetic analysis. Lancet Oncol 2012;13:607–15. [DOI] [PubMed] [Google Scholar]
- [35].Helicobacter and Cancer Collaborative Group Gastric cancer and Helicobacter pylori: a combined analysis of 12 case control studies nested within prospective cohorts. Gut 2001;49:347–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Kamangar F, Sheikhattari P, Mohebtash M. Helicobacter pylori and its effects on human health and disease. Arch Iran Med 2011;14:192–9. [PubMed] [Google Scholar]
- [37].Wen D, Zhang N, Shan B, et al. Helicobacter pylori infection may be implicated in the topography and geographic variation of upper gastrointestinal cancers in the Taihang Mountain high-risk region in northern China. Helicobacter 2010;15:416–21. [DOI] [PubMed] [Google Scholar]
- [38].Liang SY, Cao Y. Research of the “three nitrogen” content in drinking water in rural of high incidence of esophageal, Cixian. Chin J Cancer Prev Treat 2012;19:649–51. [Google Scholar]
- [39].Bosetti C, Bertuccio P, Malvezzi M, et al. Cancer mortality in Europe, 2005–2009, and an overview of trends since 1980. Ann Oncol 2013;24:2657–71. [DOI] [PubMed] [Google Scholar]
- [40].Kamangar F, Dores GM, Anderson WF. Patterns of cancer incidence, mortality, and prevalence across five continents: defining priorities to reduce cancer disparities in different geographic regions of the world. J Clin Oncol 2006;24:2137–50. [DOI] [PubMed] [Google Scholar]
- [41].Zhou M, Wang H, Zhu J, et al. Cause-specific mortality for 240 causes in China during 1990–2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet 2016;387:251–72. [DOI] [PubMed] [Google Scholar]
- [42].Zheng X, Mao X, Xu K, et al. Massive endoscopic screening for esophageal and gastric cancers in a high-risk area of China. PLoS One 2015;10:e0145097. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


