Supplemental Digital Content is available in the text.
Key Words: patient safety, medical errors, hospital quality, hospital performance, administrative hospital data
Abstract
Background:
There is little satisfactory evidence on the harm of safety incidents to patients, in terms of lost potential health and life-years.
Objective:
To estimate the healthy life-years (HLYs) lost due to 6 incidents in English hospitals between the years 2005/2006 and 2009/2010, to compare burden across incidents, and estimate excess bed-days.
Research Design:
The study used cross-sectional analysis of the medical records of all inpatients treated in 273 English hospitals. Patients with 6 types of preventable incidents were identified. Total attributable loss of HLYs was estimated through propensity score matching by considering the hypothetical remaining length and quality of life had the incident not occurred.
Results:
The 6 incidents resulted in an annual loss of 68 HLYs and 934 excess bed-days per 100,000 population. Preventable pressure ulcers caused the loss of 26 HLYs and 555 excess bed-days annually. Deaths in low-mortality procedures resulted in 25 lost life-years and 42 bed-days. Deep-vein thrombosis/pulmonary embolisms cost 12 HLYs, and 240 bed-days. Postoperative sepsis, hip fractures, and central-line infections cost <6 HLYs and 100 bed-days each.
Discussion:
The burden caused by the 6 incidents is roughly comparable with the UK burden of Multiple Sclerosis (80 DALYs per 100,000), HIV/AIDS and Tuberculosis (63 DALYs), and Cervical Cancer (58 DALYs). There were marked differences in the harm caused by the incidents, despite the public attention all of them receive. Decision makers can use the results to prioritize resources into further research and effective interventions.
Patient safety incidents cause significant harm to patients, and their treatment leads to excess costs for health care providers. Most countries spend significant resources on the prevention of safety incidents.1–5 However, hospitals have limited budgets, and many competing demands for improvement initiatives. It is therefore important to understand the harm and costs associated with patient safety incidents to provide guidance on where to prioritize preventive efforts. Incidents may increase hospital expenditure, in the form of longer lengths of stay and additional treatment. From its own narrow perspective, a hospital should clearly implement any preventive intervention that reduces its net treatment costs, by averting incidents. However, even costly prevention may be worthwhile implementing if the associated gains to patient health are sufficient.6 The health gains are the harm caused by safety incidents that can be averted by the preventive measure.
Harm of incidents has been estimated by a number of studies,3,7–15 but usually simply as the number of deaths attributable to the incidents, calculated from incidence and excess mortality risk. Attributable deaths are misleading estimates of health loss because they do not consider how long and in what health a patient would have lived if care had been optimal.16,17 In reaction to the seminal Institute of Medicine18 report, McDonald et al17 stated early on that “Unlike most people who step into motor vehicles, most patients admitted to hospitals have high disease burdens and high death risks even before they enter the hospital.” Previous attempts to adjust for baseline health status mostly relied on retrospective record reviews,19 but they were limited in scope and could not predict future health and life-years. Some studies estimated the loss to patients based on compensatory damages paid,20–22 but their value is affected by other factors apart from the adverse health impacts, most notably forfeited earnings.
The loss of health depends on baseline health of patients at the time of the incident, and on future health had these incidents not occurred. Fewer healthy years are lost to incidents that predominantly affect older and sicker patient groups, compared with incidents that affect generally younger and healthier patients. The objective of this study was to compare the loss of health caused by 6 commonly studied safety incidents. We used econometric methods to estimate the healthy life-years (HLYs) lost due to deaths attributable to the incidents. We further estimated excess bed-days as a proxy for additional treatment costs.
METHODS
Study Sample
The Hospital Episode Statistics for the financial years 2005/2006–2009/2010 were used for analysis. This is an administrative database containing medical records with detailed clinical data for all hospitalized patients in 273 English public hospitals.23 We identified cases from up to 5.9 million inpatients at risk annually. There are considerable variations in the number of patients considered at risk across incidents and years (see “control patients” Table SDC4, Supplemental Digital Content 1, http://links.lww.com/MLR/B270). Data on staffing levels, bed numbers, teaching status, and bed occupancy were obtained from the Web site of the Health & Social Care Information Centre maintained by the UK Department of Health.24 We identified 6 types of patient safety indicators via software modules developed by the Agency for Healthcare Research and Quality (AHRQ) that identify specific combinations of diagnoses and procedure codes in medical records25 (see section 1 Supplementary Data: The Patient Safety Indicators in the SDC, Supplemental Digital Content 1, http://links.lww.com/MLR/B270). The 6 indicators were chosen because of the attention they receive by the public, policy makers, and academics, and because translations of the AHRQ algorithms into the English coding system had previously been developed.13 Incidents were identified from all patients in whom the event is considered preventable according to AHRQ criteria. Incidence rates per 1000 hospitalizations in our data are comparable with similar results for the AHRQ indicators from previous studies on general hospitalizations of all ages from the United Kingdom,11,13 the United States,4,7,10,26 and OECD countries.3 Estimates range from <1 case per 1000 patients at risk for comparably rare events such as central-line infections, postoperative hip fractures, and deaths in low-mortality Healthcare Resource Groups (HRGs) to 14 cases for preventable pressure ulcers (Table SDC1, Supplemental Digital Content 1, http://links.lww.com/MLR/B270 and SDC2, Supplemental Digital Content 1, http://links.lww.com/MLR/B270 for incidence in an average English hospital). Average patient characteristics vary quite markedly across incidents, in particular age (Tables SDC3a–f, Supplemental Digital Content 1, http://links.lww.com/MLR/B270), underlining the importance of adjusting for hypothetical future health and life expectancy in patients who die.
Statistical Analysis
We first calculated attributable deaths as the products of excess mortality and incidence, as previous studies have done. However, we then went further to estimate HLYs lost to these incidents, thus more truly demonstrating their impact on the patients and families concerned. To calculate the loss of HLYs by incident and year, we estimated hypothetical healthy life expectancy (HLE) of all patients with incidents from quality-of-life reductions due to preexisting comorbidities unrelated to the safety incident, and life expectancy estimates.27 HLE is a combined estimate of the health and the length of life the patient would have had if the incident had not occurred. Life-years lived in less than perfect health were adjusted—or “devalued”—according to the extent of unrelated conditions suffered by the patients affected. Remaining HLE was calculated as the sum of the quality-adjusted life-years. To determine by how much hypothetical life-years needed to be devalued, we used estimates of the quality-of-life reductions associated with 141 common chronic conditions for the population in the United Kingdom28 (see Tables SDC7, Supplemental Digital Content 1, http://links.lww.com/MLR/B270 and SDC8, Supplemental Digital Content 1, http://links.lww.com/MLR/B270). Some patients may have died from causes unrelated to the safety incident. We therefore adjusted calculation of lost HLYs by estimates of the average excess mortality associated with the incidents, to calculate excess mortality by comparing incident patients and a group of matched control patients without incidents. We further used this control group for estimating the hypothetical HLEs, to assure that they were unaffected by the adverse health consequences of the incidents. The control patients were matched to patients with incidents using propensity score matching, and they were therefore observationally near identical—except that they did not suffer an incident. Patients were matched on age, sex, the weighted Charlson comorbidity index, index of multiple social deprivation of patients’ residence, number of diagnoses, and several characteristics of the treating hospital (teaching status, medical and nursing staffing, number of beds, and bed occupancy). Matching successfully eliminated bias in the covariates between incident and control patients to acceptable levels according to standard tests (see Tables SDC3a–f, Supplemental Digital Content 1, http://links.lww.com/MLR/B270) and overlay plots (see Figs. SDC1a–f, Supplemental Digital Content 1, http://links.lww.com/MLR/B270). Our estimates of HLE for patients with incidents were substantially smaller than ordinary life expectancy, except for very old patients (Fig. 1). This demonstrates that loss of health would be overestimated if unadjusted for existing comorbidities and age. Excess bed-days were estimated as the average difference in length of stay of incident and matched control patients (see section 2 Supplementary Methods in the SDC, Supplemental Digital Content 1, http://links.lww.com/MLR/B270 for a detailed explanation of the methods).
FIGURE 1.
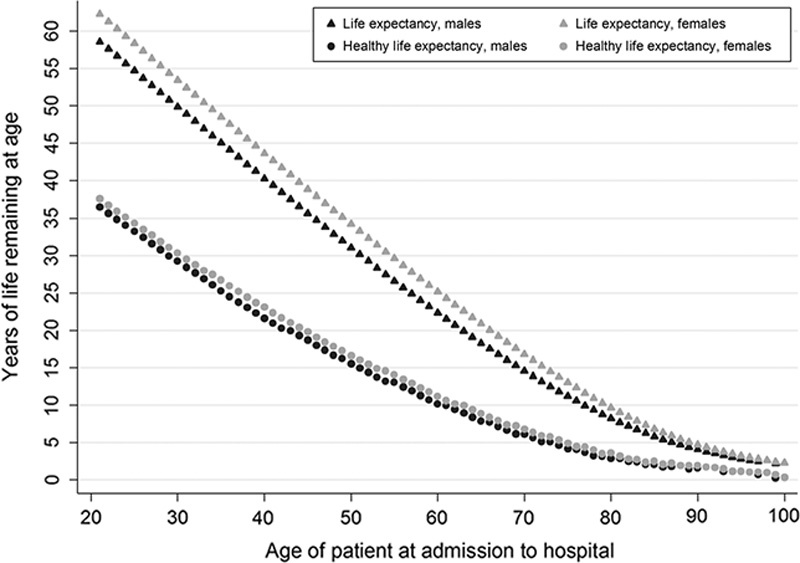
Life expectancy and healthy life expectancy, control patients for pressure ulcers. This figure shows expected remaining life expectancy and healthy life expectancy for males and females. Healthy life expectancy is adjusted for observed comorbidities that were associated with significant reductions in quality of life in matched control patients, and were estimated as part of this study. The values in this figure are for pressure ulcers control patients, and averaged across all English hospitals and the years 2005/2006–2009/2010. Values for other incidents are very similar (see Table SDC9, Supplemental Digital Content 1, http://links.lww.com/MLR/B270). For example, a male of age 50 years in the general population has a remaining life expectancy of around 34 years, and a (population level) healthy life expectancy of 24 years. However, an average 50-year-old male admitted to a hospital in England is in less good health, and has a remaining healthy life expectancy of only around 16 years on average because of comorbidities that are expected to result in reduced quality-of-life over the remaining life-years. If a 50-year-old male hospital patient would contract a pressure ulcer in hospital and die from it, a calculation of lost life-years that did not adjust for quality-of-life would overestimate lost healthy life-years by 18 years.
RESULTS
A total of 68 HLYs and 934 bed-days were lost to the 6 preventable patient safety incidents per 100,000 population annually, averaged over 5 years (Table SDC12, Supplemental Digital Content 1, http://links.lww.com/MLR/B270). The typical English hospital lost approximately 165 HLYs and 2024 bed-days in capacity in total (Figs. 2, 3, and Tables SDC10, Supplemental Digital Content 1, http://links.lww.com/MLR/B270 and SDC11, Supplemental Digital Content 1, http://links.lww.com/MLR/B270). Assuming 1 HLY is valued at about £12,900,29 the total loss of health due to 6 preventable safety incidents amounted to about £2.1 million in a typical English hospital annually (£877,000 or $1.3 million per 100,000 population). There is considerable uncertainty around both estimates. If an inpatient day in hospital costs £273,30 annual excess bed-days amounted to about £553,000 (£255,000 or $390,000 per 100,000). Average excess mortality risks and bed-days per incident are shown in Table 1.
FIGURE 2.
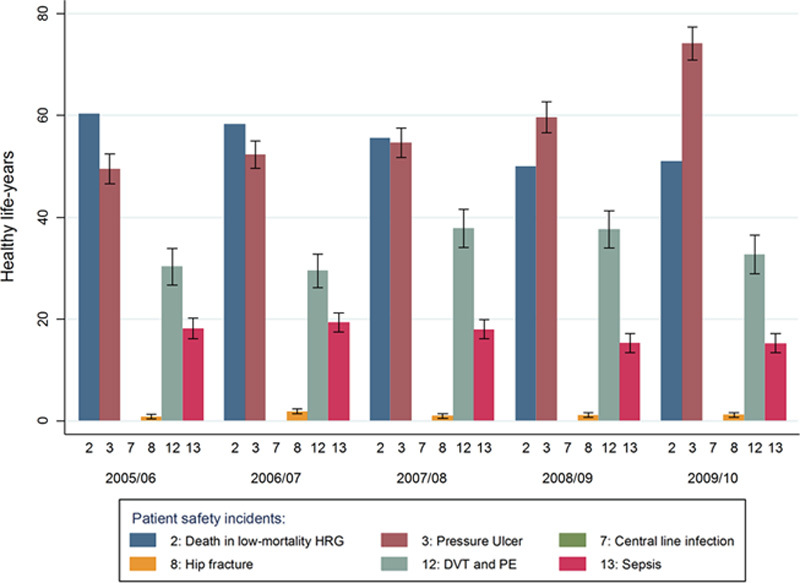
Healthy life-years lost due to 6 preventable patient safety incidents, annual totals for an average English hospital. Estimates of annual total healthy life-years lost to incidents for all hospitalized inpatients (≥1 night) at risk in an English hospital with the average number of incidents per year. 95% confidence intervals are indicated by the black bars. The estimate for deaths in low-mortality HRGs is deterministic by definition. The loss is zero for central line infections because mortality risk of patients with incidents was not statistically significantly different from mortality risk of matched control patients without incidents. DVT indicates deep-vein thrombosis; HRG, Healthcare Resource Groups; PE, pulmonary embolism.
FIGURE 3.
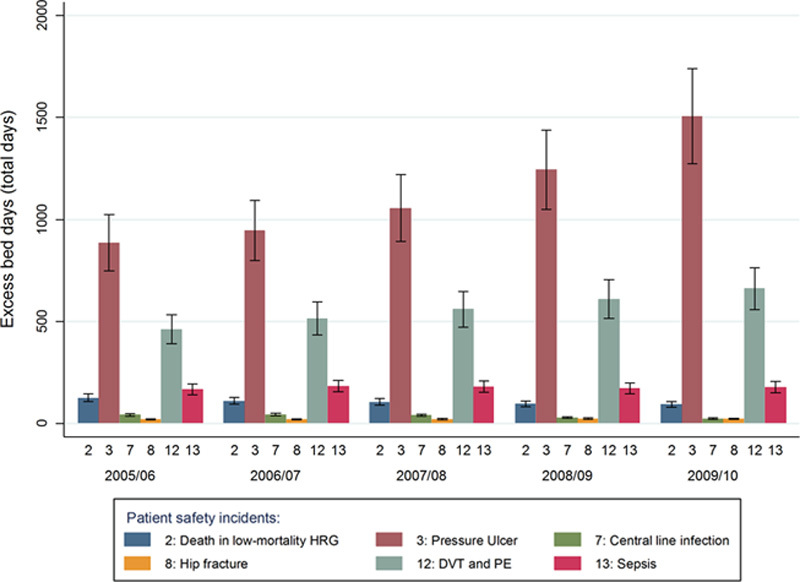
Excess bed-days due to 6 preventable patient safety incidents, annual totals for an average English hospital. Estimates of annual excess bed-days due to incidents for all hospitalized inpatients at risk in an average English hospital. DVT indicates deep-vein thrombosis; PE, pulmonary embolism.
TABLE 1.
Excess Mortality Risk and Average Bed-Days, Averages 2005/2006–2009/2010
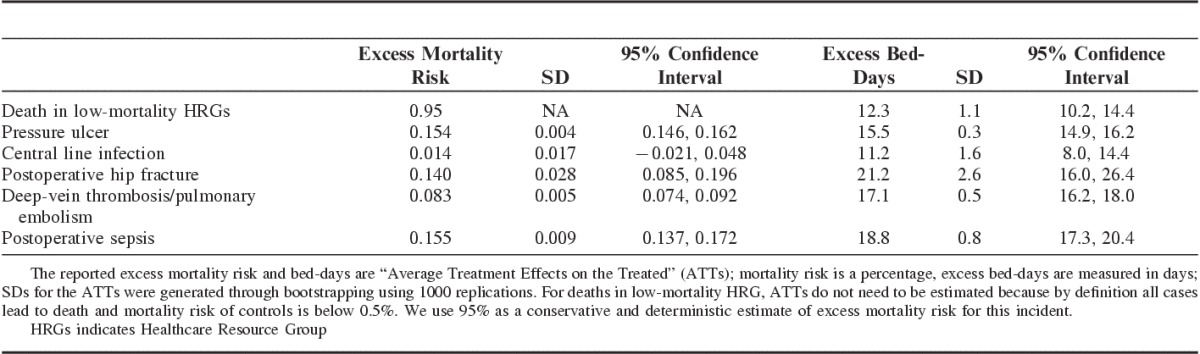
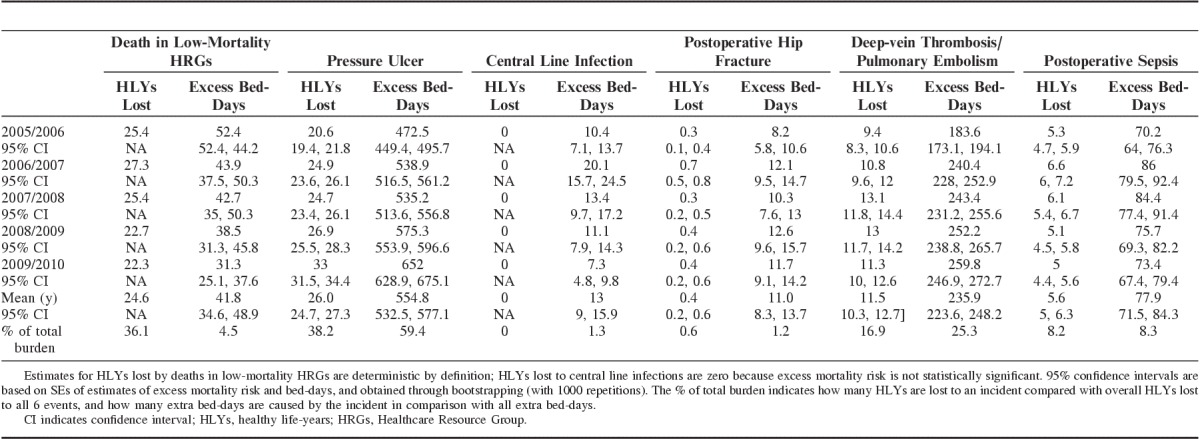
The greatest loss in health and excess bed-days was caused by preventable pressure ulcers at 26 lost HLYs and 555 days per 100,000 on average annually (Table 2). The high burden attributable to preventable ulcers in comparison with other incidents is confirmed by previous US studies based on legal claims data that found compensatory damages paid for this incident highest among all under investigation.20,21 Deaths in low-mortality HRGs were the close second-highest cause of lost health and excess bed-days among the 6 incidents at 25 HLYs and 42 days. Although incidence was low, excess mortality was high at 95% because all cases by definition lead to death and loss of remaining life-years in relatively healthy patients. Previous studies have found inconsistencies with this general incident category, therefore our results should be subjected to further research.31 DVT/PE caused comparably few lost HLYs at 12, but a considerable number of excess bed-days at 236, second only to ulcers. Preventable DVT/PE had low incidence and a comparably small excess mortality risk of 8%, compared with all cases of DVT/PE in hospitals, a result confirmed by other studies.32 Postoperative sepsis caused only 6 lost HLYs and 78 bed-days. In the United States, the costs of sepsis have been estimated at $400 billion annually, which seems high in comparison.33 Our results for the small health losses at <1 HLY due to postoperative hip fractures and central-line infections may be surprising, considering the attention that these 2 incidents receive. The results are explained by low incidence. Also, there was no increased mortality risk for central-line infections, a result found before.34 Although excess average length of stay for hip fractures was highest among all incidents at 22 days, total excess bed-days were just 11 per 100,000, because incidence was low at 300 cases annually.
TABLE 2.
Loss of Healthy Life-Years and Excess Bed-Days Due to 6 Patient Safety Incidents, Annual Estimates Per 100,000 Population, All English Hospitals
Our study has limitations. First, weaknesses in the coding and completeness of administrative hospital data are well-known and understood.35 Although the AHRQ algorithms are considered the most sophisticated routines for identifying safety incidents in administrative data, the ICD-10 system was not specifically designed to identify medical injuries, resulting in potential errors.36 AHRQ indicator rates may represent a lower limit of incidents currently recorded in administrative databases; the true rates could be substantially higher.37 Further, we do not consider the impact of incidents on long-term health. Propensity score method can only adjust for observable confounders, and unobservable sources of patient complexity may have resulted in overestimates of the outcomes attributable to incidents.
CONCLUSIONS
There are now a variety of effective patient safety programs,38 but no easy way of deciding which should have priority in an overarching patient safety strategy. Decision makers can use our research to prioritize among the 6 incidents, and allocate resources into further research and implementation of actual interventions according to the overall burden that is caused by each class of incident. Our results suggest placing high attention on the prevention of pressure ulcers. If burden to patients is main concern, then equal attention should be given to preventing deaths in low-mortality HRGs. This is not straightforward because these deaths may have varied causes related to general hospital performance. If financial burden to hospitals is a concern, then interventions to prevent and treat DVT/PE should receive high priority for policy action. Our results suggest that preventable postoperative sepsis, hip fractures, and central-line infections cause comparably small burden, which of course may reflect the considerable efforts that have already been invested in their prevention.
To place our findings in context, the burden caused by the 6 safety incidents is roughly comparable with the UK burden of Multiple Sclerosis (80 DALYs per 100,000), HIV/AIDS and Tuberculosis (63 DALYs), Cervical Cancer (58 DALYs), or Interpersonal Violence (57 DALYs).39 Our estimate is higher than the Global Burden-of-Disease estimate of Disability-adjusted Life-years lost to “Adverse effects of medical treatment” for the United Kingdom in 2010 of 44.39 However, these estimates were based on a different methodology, focused on a different set of incidents, and covered a larger population. The question which incidents should receive priority attention requires in addition information on the efficacy and costs of alternative interventions. Our findings can be used in cost-effectiveness studies to place a monetary value on the economic benefits of interventions that prevent incidents and mitigate their negative effects. Studies evaluating patient safety interventions can, when indicator data are available, use our methodology to assess the impact and cost-effectiveness of interventions. It can also be applied to the evaluation of other safety incidents. This will enable us to build a much more accurate picture of the overall burden of unsafe care and the potential clinical and economic benefits of improvements in hospital quality. Ultimately, we hope that our research will help reduce the regrettable and preventable loss of HLYs in hospitals.
Supplementary Material
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website, www.lww-medicalcare.com.
ACKNOWLEDGMENT
The authors thank the Health and Information Centre of the Department of Health England for provision of the data. The authors also thank participants of the meetings of the American Society of Health Economists, Los Angeles, July 2014, and the UK Health Economics Study Group, Lancaster, June 2015, for their comments on earlier versions of this paper.
Footnotes
Supported by The Health Foundation, the Centre for Patient Safety and Service Quality (National Institute for Health Research), and the National Institute for Health Research Health Protection Research Unit (NIHR HPRU) in Modelling Methodology at Imperial College London in partnership with Public Health England (PHE).
The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR, the Department of Health, or Public Health England.
The authors declare no conflict of interest.
REFERENCES
- 1.Landrigan CP, Parry GJ, Bones CB, et al. Temporal trends in rates of patient harm resulting from medical care. New England Journal of Medicine. 2010;363:2124–2134. [DOI] [PubMed] [Google Scholar]
- 2.Downey JR, Hernandez-Boussard T, Banka G, et al. Is patient safety improving? National trends in patient safety indicators: 1998–2007. Health Services Research. 2012;47:414–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Drosler SE, Klazinga NS, Romano PS, et al. Application of patient safety indicators internationally: a pilot study among seven countries. Int J Qual Health Care. 2009;21:272–278. [DOI] [PubMed] [Google Scholar]
- 4.Agency for Healthcare Research and Quality. AHRQ Quality Indicators: Patient Safety Indicator v4.5 Benchmark Data Tables. Prepared by Battelle for the Agency for Healthcare Research and Quality. Rockville, MD: US Department of Health and Human Services; 2013. [Google Scholar]
- 5.Wang Y, Eldridge N, Metersky ML, et al. National trends in patient safety for four common conditions, 2005–2011. New England Journal of Medicine. 2014;370:341–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Graves N, Halton K, Lairson D. Economics and preventing hospital-acquired infection: broadening the perspective. Infection Control and Hospital Epidemiology. 2007;28:178–184. [DOI] [PubMed] [Google Scholar]
- 7.Zhan C, Miller MR. Excess length of stay, charges, and mortality attributable to medical injuries during hospitalization. Journal of the American Medical Association. 2003;290:1868–1874. [DOI] [PubMed] [Google Scholar]
- 8.Zhan C, Friedman B, Mosso A, et al. Medicare payment for selected adverse events: building the business case for investing in patient safety. Health Affairs. 2006;25:1386–1393. [DOI] [PubMed] [Google Scholar]
- 9.Meurer LN, Yang H, Guse CE, et al. Excess mortality caused by medical injury. The Annals of Family Medicine. 2006;4:410–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rivard PE, Luther SL, Christiansen CL, et al. Using patient safety indicators to estimate the impact of potential adverse events on outcomes. Medical Care Research and Review. 2008;65:67–87. [DOI] [PubMed] [Google Scholar]
- 11.Raleigh VS, Cooper J, Bremner SA, et al. Patient safety indicators for England from hospital administrative data: case-control analysis and comparison with US data. BMJ. 2008;337:a1702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Encinosa WE, Hellinger FJ. The impact of medical errors on ninety-day costs and outcomes: an examination of surgical patients. Health Services Research. 2008;43:2067–2085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bottle A, Aylin P. Application of AHRQ patient safety indicators to English hospital data. Quality and Safety in Health Care. 2009;18:303–308. [DOI] [PubMed] [Google Scholar]
- 14.Trentino KM, Swain SG, Burrows SA, et al. Measuring the incidence of hospital-acquired complications and their effect on length of stay using CHADx. Med J Aust. 2013;199:543–547. [DOI] [PubMed] [Google Scholar]
- 15.Hauck K, Zhao X. How dangerous is a day in hospital?: a model of adverse events and length of stay for medical inpatients. Medical Care. 2011;49:1068–1075. [DOI] [PubMed] [Google Scholar]
- 16.Hayward RA, Hofer TP. Estimating hospital deaths due to medical errors: preventability is in the eye of the reviewer. JAMA. 2001;286:415–420. [DOI] [PubMed] [Google Scholar]
- 17.McDonald CJ, Weiner M, Hui SL. Deaths due to medical errors are exaggerated in institute of medicine report. JAMA. 2000;284:93–95. [DOI] [PubMed] [Google Scholar]
- 18.Kohn LT, Corrigan J, Donaldson MS, eds; Committee on Quality of Health Care in America, Institute of Medicine To Err is Human: Building a Safer Health System. Washington, D.C.: National Academies Press; 2000. [PubMed] [Google Scholar]
- 19.de Vries EN, Ramrattan MA, Smorenburg SM, et al. The incidence and nature of in-hospital adverse events: a systematic review. Quality and Safety in Health Care. 2008;17:216–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shreve J, Van Den Bos J, Gray T, et al. The Economic Measurement of Medical Errors. Milliman. Sponsored by Society of Actuaries' Health Section. Schaumburg, Illinois; 2010. [Google Scholar]
- 21.Van Den Bos J, Rustagi K, Gray T, et al. The $17.1 billion problem: the annual cost of measurable medical errors. Health Affairs. 2011;30:596–603. [DOI] [PubMed] [Google Scholar]
- 22.David G, Gunnarsson CL, Waters HC, et al. Economic measurement of medical errors using a hospital claims database. Value in Health. 2013;16:305–310. [DOI] [PubMed] [Google Scholar]
- 23.Health & Social Care Information Centre. HSCIC. Hospital episode statistics. Hospital Episode Statistics. London, UK: Health & Social Care Information Centre; 2013. Available at: http://digital.nhs.uk/hes. Accessed August 30, 2016. [Google Scholar]
- 24.Health & Social Care Information Centre. Statistical publications catalogue. 2015. Available at: http://digital.nhs.uk/searchcatalogue Accessed February 2, 2016.
- 25.Agency for Healthcare Research and Quality. Patient safety indicators. 2015. Available at: http://www.qualityindicators.ahrq.gov. Accessed February 2, 2016. [DOI] [PubMed]
- 26.Carey K, Stefos T. Measuring the cost of hospital adverse patient safety events. Health Economics. 2011;20:1417–1430. [DOI] [PubMed] [Google Scholar]
- 27.Office for National Statistics. National Life Tables, England, 2011-2013 [database online]. Office for National Statistics, 2014. Updated 25 September 2014. Available at: http://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/lifeexpectancies/bulletins/nationallifetablesunitedkingdom/2014-09-25. Accessed May 13, 2015.
- 28.Sullivan PW, Slejko JF, Sculpher MJ, et al. Catalogue of EQ-5D scores for the United Kingdom. Medical Decision Making. 2011;31:800–804. [DOI] [PubMed] [Google Scholar]
- 29.Claxton K, Martin S, Soares M, et al. Methods for the estimation of the National Institute for Health and Care Excellence cost-effectiveness threshold. Health Technol Assess. 2015;19:1-503, v-vi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Monitor. Reference costs 2012-13. In: Department of Health, ed. London: The Stationary Office; 2013. Available at: http://www.gov.uk/government/uploads/system/uploads/attachment_data/file/261154/nhs_reference_costs_2012-13_acc.pdf. Accessed August 30, 2016.
- 31.Mihrshahi S, Brand C, Ibrahim JE, et al. Validity of the indicator ‘death in low-mortality diagnosis-related groups’ for measuring patient safety and healthcare quality in hospitals. Internal Medicine Journal. 2010;40:250–257. [DOI] [PubMed] [Google Scholar]
- 32.National Institute for Health and Clinical Excellence. Venous thromboembolic diseases: the management of venous thromboembolic diseases and the role of thrombophilia testing. Costing report. In: National Institute for Health and Clinical Excellence, ed. Manchester; 2012.
- 33.Agency for Healthcare Research and Quality. Postoperative sepsis rate—technical specifications. Patient Safety Indicators 13 (PSI 13), AHRQ Quality Indicators, Version 4.5a, July 2014, Provider-level Indicator. Rockville, MD: US Department of Health and Human Services; 2014. [Google Scholar]
- 34.O’Grady NP, Alexander M, Burns LA, et al. Guidelines for the prevention of intravascular catheter-related infections. Clinical infectious diseases. 2011;52:e162–e193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wardle G, Wodchis WP, Laporte A, et al. The sensitivity of adverse event cost estimates to diagnostic coding error. Health Services Research. 2012;47:984–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tsang C, Palmer W, Bottle A, et al. A review of patient safety measures based on routinely collected hospital data. American Journal of Medical Quality. 2012;27:154–169. [DOI] [PubMed] [Google Scholar]
- 37.Zhan C, Miller MR. Administrative data based patient safety research: a critical review. Quality and Safety in Health Care. 2003;12:ii58–ii63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shekelle PG, Pronovost PJ, Wachter RM, et al. Advancing the science of patient safety. Annals of Internal Medicine. 2011;154:693–696. [DOI] [PubMed] [Google Scholar]
- 39.Murray CJ, Richards MA, Newton JN, et al. UK health performance: findings of the Global Burden of Disease Study 2010. The Lancet. 2013;381:997–1020. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website, www.lww-medicalcare.com.


