Abstract
Obesity and obesity-related diseases are important public health challenges. In this study, we aimed to provide updated trends in the prevalence of these conditions. We conducted two independent cross-sectional surveys of the general population aged 20–75 years in 2007 and 2013 in Jilin, China. A total of 3636 (1719 males) and 1359 (602 males) participants were enrolled in the 2007 and 2013 surveys, respectively. Obesity-related diseases were defined as type 2 diabetes, hypertension, dyslipidemia and non-alcoholic fatty liver disease (NAFLD). The age-standardized prevalence of obesity, overweight, diabetes, pre-diabetes, dyslipidemia and NAFLD increased from 2007 to 2013 from 15.82% to 19.41%, 35.85% to 41.80%, 6.37% to 9.23%, 16.77% to 23.49%., 53.46% to 65.50%, and 23.48% to 44.31% in males, respectively, and from 13.18% to 18.77%, 31.11% to 37.54%, 4.41% to 8.48%, 8.10% to 16.49%, 41.96% to 54.70%, and 17.56% to 43.06% in females, respectively. However, the prevalence of hypertension remained stable (males: 38.10% vs. 38.63% and females: 33.04% vs. 33.01% in 2007 and 2013, respectively). The prevalence of obesity and obesity-related diseases, except for hypertension, increased significantly in the general population in Northeastern China. More targeted measures should be implemented to address the serious challenges presented by these diseases.
Obesity is a significant global health challenge, and its increasing prevalence has been considered a global pandemic, affecting countries worldwide including China1,2. The global prevalence of obesity in 2030 has been projected to be 1.12 billion3. Furthermore, obesity and overweight were estimated to have caused 3.4 million deaths in 20104. Obesity is associated with a number of health issues, ranging from specific diseases such as type 2 diabetes, dyslipidemia, hypertension and non-alcoholic fatty liver disease (NAFLD) to reduced quality of life, psychosocial disturbances, decreased life expectancy, and increased economic burden5. The morbidity and mortality of obesity-related diseases can be reduced by maintaining strict control of obesity, and this approach should therefore be emphasized.
China is a large developing country, and the rapid economy development has led to changes in lifestyle, such as in dietary habits and physical activity; for example, meat consumption has increased drastically, vegetable and fruit intake has decreased slightly, and levels of physical activity have also been reduced6. Many studies have evaluated the prevalence of obesity and obesity-related diseases in China2,7,8,9,10,11,12, but data on the recent prevalence trends of these diseases in China are rare13,14,15,16,17,18,19. Jilin Province which located in northeast China has a population of approximately 27 million20. In 2007, we conducted a study to screen for the prevalence of obesity and obesity-related diseases (diabetes, hypertension, dyslipidemia and NAFLD) in Dehui City, which is representative of Jilin Province. Six years later, the prevalence of these diseases was reassessed. Our study aimed to assess the changes in the prevalence of obesity, diabetes, hypertension, dyslipidemia and NAFLD in China from 2007 to 2013 and provides evidence for health care providers to effectively address the challenges presented by obesity and obesity-related diseases.
Results
Characteristics of Chinese adults in Dehui aged 20–75 years in the 2007 and 2013 surveys
As shown in Table 1, a total of 3636 (1719 male) and 1359 subjects (602 male) completed the surveys in 2007 and 2013, respectively. All participants were of Han origin. The mean age of the participants was 45 years (36, 55) in 2007 and significantly increased to 52 years (44, 60) in 2013, whereas the sex composition did not differ. The proportion of residents engaged in agricultural work markedly decreased in 2013 compared with 2007. BMI, WC, SBP, DBP, and TC, TG, fasting blood glucose (FBG), alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels were much higher in 2013 survey than in the 2007 survey (P < 0.05). However, LDL-C and HDL-C were significantly lower in 2013.
Table 1. General characteristics of the study population in 2007 and 2013.
| 2007(n = 3636) | 2013(n = 1359) | P value | |
|---|---|---|---|
| Sex (male) | 1719(47.3%) | 602(44.3%) | 0.064 |
| Age | 45(36,55) | 52(44,60) | <0.01* |
| BMI | 23.89(21.48,26.45) | 24.46(22.05,27.07) | <0.01* |
| WC | 81(74,89) | 83.5(77,91) | <0.01* |
| SBP | 125(115,140) | 130(118,146) | <0.01* |
| DBP | 80(75,90) | 82(78,90) | 0.037* |
| TC | 4.28(3.71,4.92) | 5.00(4.00,5.00) | <0.01* |
| LDL-C | 3.00(2.60,3.40) | 2.65(2.12,3.18) | <0.01* |
| TG | 1.22(0.83,1.90) | 1.60(1.12,2.32) | <0.01* |
| HDL-C | 1.3(1.2,1.6) | 1.2(1.0,1.5) | <0.01* |
| FBG | 4.86(4.48,5.33) | 5.20(4.80,5.70) | <0.01* |
| ALT | 18.0(13.5,26.9) | 20.0(14.0,27.0) | 0.022* |
| AST | 21.3(17.6,26.0) | 24.0(21.0,29.0) | <0.01* |
| Occupation (farmer) | 1785(49.1%) | 605(44.5%) | <0.01* |
Result are expressed as the median (25th quartile, 75th quartile) or frequency (percentage).
BMI, body mass index; WC, waist circumference; SBP, systolic blood pressure; DBP, diastolic blood pressure; TC, total cholesterol; LDL-C, low-density lipoprotein cholesterol; TG, triglycerides; HDL-C, high-density lipoprotein cholesterol; FBG, fasting blood glucose; ALT, alanine aminotransferase; AST, aspartate aminotransferase.
*Indicates statistical significance.
In view of different prevalence between female and male, we divided subjects by gender in the following analyses. Age, BMI, SBP, TC, LDL-C, TG, HDL-C, FBG and AST in 2007 and 2013 maintained significant differences in both genders. Women had significantly higher WC and ALT levels in 2013 (P < 0.01); however, the difference in men was not significant. DBP in both genders did not significantly change between the two surveys (Table 2).
Table 2. General characteristics of the study population by gender in 2007 and 2013.
| Male | Female | |||||
|---|---|---|---|---|---|---|
| 2007(n = 1719) | 2013(n = 602) | P value | 2007(n = 1917) | 2013(n = 757) | P value | |
| Age | 45(36,55) | 53(45,61) | <0.01* | 46(37,55) | 51(44,60) | <0.01* |
| BMI | 24.17(21.73,26.71) | 24.95(22.53,27.32) | <0.01* | 23.59(21.53,26.22) | 24.18(21.85,26.83) | <0.01* |
| WC | 84(77,92) | 85(78.4.92.2) | 0.055 | 79(73,87) | 82(76.5,89) | <0.01* |
| SBP | 130(120,140) | 130(120,144) | <0.01* | 125(110,140) | 130(116,148) | <0.01* |
| DBP | 85(80,90) | 85(80,90) | 0.091 | 80(70,90) | 80(74,90) | 0.105 |
| TC | 4.36(3.78,4.97) | 5.00(4.00,5.00) | <0.01* | 4.22(3.64,4.86) | 5.00(4.00,5.00) | <0.01* |
| LDL-C | 3.00(2.60,3.14) | 2.60(2.12,3.16) | <0.01* | 2.97(2.50,3.40) | 2.70(2.13,3.21) | <0.01* |
| HDL-C | 1.3(1.1,1.5) | 1.2(1.0,1.5) | <0.01* | 1.4(1.2,1.6) | 1.3(1.1,1.5) | <0.01* |
| TG | 1.29(0.85,2.05) | 1.57(1.06,2.39) | <0.01* | 1.19(0.81,1.74) | 1.63(1.16,2.25) | <0.01* |
| FBG | 5.01(4.57,5.55) | 5.30(4.90,5.80) | <0.01* | 4.74(4.39,5.15) | 5.10(4.80,5.60) | <0.01* |
| ALT | 22.5(16.0,32.9) | 22.0(17.0,30,0) | 0.439 | 16.0(11.5,22.5) | 18.0(13.0,24.0) | <0.01* |
| AST | 23.2(18.8,28.2) | 26.0(22.0,32.0) | <0.01* | 20.1(16.9,23.8) | 23.0(20.0,27.0) | <0.01* |
BMI, body mass index; WC, waist circumference; SBP, systolic blood pressure; DBP, diastolic blood pressure; TC, total cholesterol; LDL-C, low-density lipoprotein cholesterol; TG, triglycerides; HDL-C, high-density lipoprotein cholesterol; FBG, fasting blood glucose; ALT, alanine aminotransferase; AST, aspartate aminotransferase.
*Indicates statistical significance.
Prevalence of obesity and obesity-related diseases
Table 3 shows the crude and age-standardized prevalence rates of obesity and obesity-related diseases among males and females in the two surveys. Compared with 2007, the age-standardized prevalences of obesity, overweight, diabetes, pre-diabetes, dyslipidemia and NAFLD increased by 3.59%, 5.95%, 2.86%, 6.72%, 12.04% and 20.83% in males respectively and 5.59%, 6.43%, 4.07%, 8.39%, 12.74% and 25.50% in females respectively in 2013. On the other hand, the prevalence of hypertension did not change significantly for either gender. Males had a higher prevalence of obesity and obesity-related diseases (hypertension, diabetes, pre-diabetes, obesity, overweight, dyslipidemia and NAFLD) than females in both 2007 and 2013.
Table 3. Comparisons of the prevalence of obesity, overweight, and obesity-related diseases between 2007 and 2013.
| Male | P value | Female | P value | P+ value | P++ value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2007(n = 1719) | 2013(n = 602) | 2007(n = 1917) | 2013(n = 757) | |||||||||
| Crude | ASR | Crude | ASR | Crude | ASR | Crude | ASR | |||||
| Obesity | 15.60% | 15.82% | 17.77% | 19.41% | <0.01* | 13.46% | 13.18% | 16.25% | 18.77% | <0.01* | <0.01* | <0.05* |
| Overweight | 36.60% | 35.85% | 41.69% | 41.80% | <0.01* | 32.39% | 31.11% | 36.20% | 37.54% | <0.01* | <0.01* | <0.01* |
| Diabetes | 6.98% | 6.37% | 11.79% | 9.23% | <0.01* | 5.16% | 4.41% | 8.59% | 8.48% | <0.01* | <0.01* | <0.01* |
| Pre-diabetes | 16.46% | 16.77% | 24.58% | 23.49% | <0.01* | 8.29% | 8.10% | 17.31% | 16.49% | <0.01* | <0.01* | <0.01* |
| Hypertension | 40.49% | 38.10% | 45.02% | 38.63% | >0.05 | 35.89% | 33.04% | 41.22% | 33.01% | >0.05 | <0.01* | <0.01* |
| Dyslipidemia | 54.40% | 53.46% | 64.80% | 65.50% | <0.01* | 45.30% | 41.96% | 60.60% | 54.70% | <0.01* | <0.01* | <0.01* |
| NAFLD | 23.79% | 23.48% | 40.53% | 44.31% | <0.01* | 18.83% | 17.56% | 47.42% | 43.06% | <0.01* | <0.01* | <0.01* |
ASR, age-standardized incidence rate (using the standard Chinese population in 2010); NAFLD, non-alcoholic fatty liver diseases.
P value, 2007 vs. 2013; p + value, males vs. females in 2007; p + + value, males vs. females in 2013.
*Indicates statistical significance.
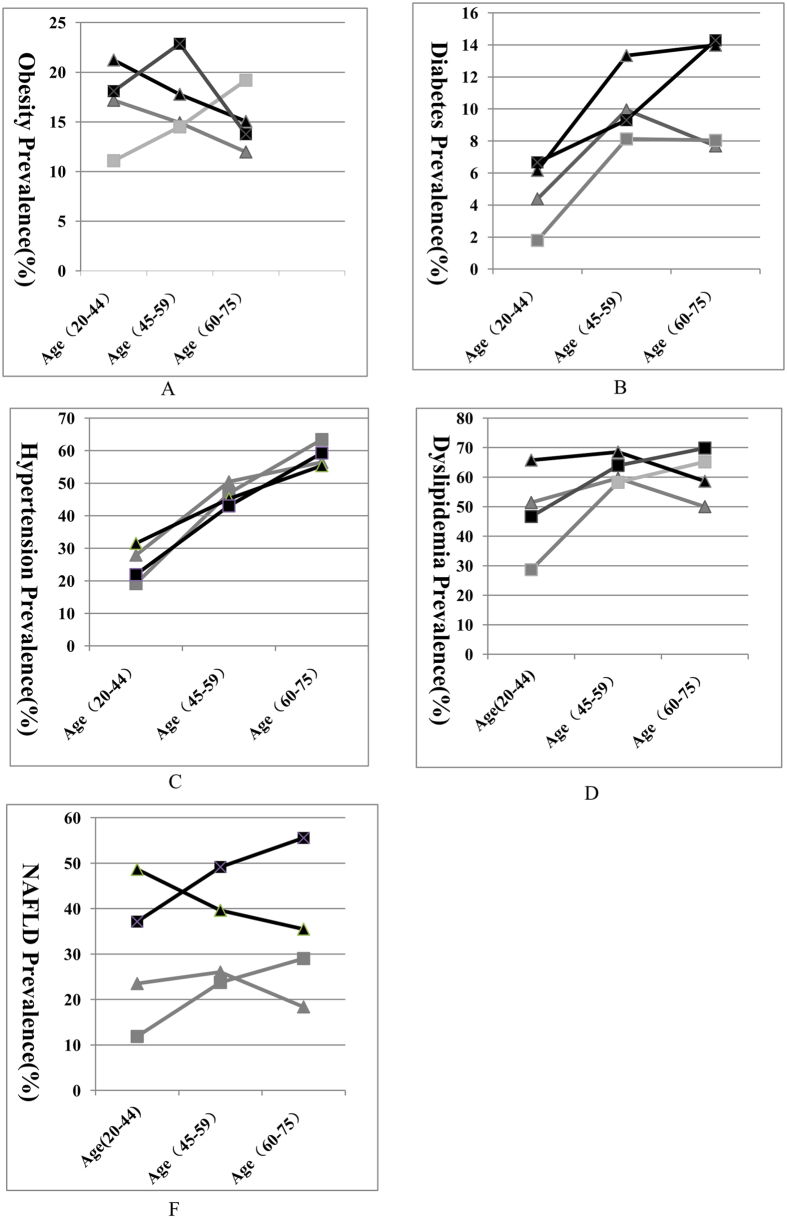
The prevalences of obesity and obesity-related diseases stratified by the three age groups according to the above criteria for age-standardization21 are shown in Fig. 1. Obesity (Fig. 1A): In males, the prevalence of obesity decreased with age in the two surveys. In females, the prevalence of obesity increased with age in 2007, but in 2013, the highest prevalence was in the age range of 45–59 years, not 60–75 years. Diabetes (Fig. 1B): In 2007, the highest prevalence of diabetes occurred in the 45- to 59-year-old age group in both genders. However, in 2013, the prevalence showed increasing trends with age in both males and females. Hypertension (Fig. 1C): The overall prevalence increased with age in males and females in the two surveys. Dyslipidemia (Fig. 1D): In the two surveys, the highest prevalence among males was in those aged 45–59 years, and the lowest was in males 60–75 years; however, the prevalence increased with age in females. NAFLD (Fig. 1E): In females, the prevalence of NAFLD increased with age in both surveys, whereas middle-aged males tended to have more NAFLD.
Figure 1. The prevalence of obesity and obesity-related diseases in different age groups.
NAFLD, non-alcoholic fatty liver diseases; (A) Obesity prevalence; (B) Diabetes prevalence; (C) Hypertension prevalence; (D) Dyslipidemia prevalence; (E) NAFLD prevalence. The black line means 2013 years; the grey line means 2007 years; The triangle blot means males while the square blot means females.
The prevalence of dyslipidemia components is shown in Table 4. The age-standardized prevalence of high TG and low HDL-C levels increased significantly, but the prevalence of high LDL-C decreased significantly in both genders in 2013 compared with 2007. The prevalence of high TC decreased by 1.14% in men but increased by 4.07% in women from the 2007 to the 2013 survey.
Table 4. The frequency of abnormal components in subjects with dyslipidemia between 2007 and 2013.
| Male | Female | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2007 | 2013 | 2007 | 2013 | |||||||
| Crude | ASR | Crude | ASR | P value | Crude | ASR | Crude | ASR | P value | |
| TC | 17.80% | 17.12% | 18.94% | 15.98% | <0.01* | 16.74% | 14.84% | 23.38% | 18.91% | <0.01* |
| TG | 33.86% | 33.49% | 44.35% | 43.49% | <0.01* | 26.66% | 24.73% | 47.29% | 41.77% | <0.01* |
| LDL-C | 28.50% | 26.76% | 18.11% | 15.47% | <0.01* | 27.49% | 24.57% | 20.21% | 16.48% | <0.01* |
| HDL-C | 15.30% | 15.58% | 32.72% | 34.96% | <0.01* | 7.62% | 7.71% | 22.32% | 22.96% | <0.01* |
TC, total cholesterol; LDL-C, low-density lipoprotein cholesterol; TG, triglycerides; HDL-C, high-density lipoprotein cholesterol; ASR, age-standardized incidence rate (using the standard Chinese population in 2010).
*Indicates statistical significance.
Discussion
Two independent cross-sectional surveys were conducted with participants aged 20–75 years in the same district (Dehui, Jilin, China) and with the same methods in both 2007 and 2013. In this study, the changes in obesity and obesity-related diseases prevalence in Dehui were explored. The age-standardized prevalence of obesity, overweight, diabetes, pre-diabetes, dyslipidemia and NAFLD increased significantly in both males and females from 2007 to 2013, whereas the age-standardized prevalence of hypertension did not significantly change.
Globally, the prevalence of obesity increased 1.9-fold (6.4% in 1980 vs. 12% in 2008)22 from 1980 to 2013, and the prevalence of overweight and obesity combined rose 47.1% among adults during the same period1. The trends in the prevalence of obesity and overweight in our study were consistent with those identified in previous studies. Obesity has a complex etiology, resulting from the combined effects of genetic, environmental, and lifestyle factors and the interactions between them23. Although genetic background is crucial to explaining individuals’ susceptibility to most chronic diseases, changes in lifestyle, including rapid urbanization, increased consumption of high energy density foods, and parallel decreases in physical activity, are considered the most likely factors contributing to this increase23,24,25. Under these circumstances, individuals develop high rates of obesity and obesity-related diseases such as type 2 diabetes, dyslipidemia and NAFLD1,23,26,27,28.
The prevalence of type 2 diabetes mellitus was estimated to be 21.5% in the 2002 World Health Organization (WHO) STEPwise approach to Surveillance (STEPS) survey; however, the corresponding prevalence in the 2013 STEPS survey was reported to be 45.8%29. The prevalence of diabetes in the US population increased from 5.5% to 9.3% from 1988–1994 to 1999–201030. In Shanghai, China, the overall prevalence of diabetes increased from 27.93% to 34.78% between 2002 and 2012 in subjects with known risk factors for diabetes, such as a family history of diabetes, overweight or obesity, previously identified impaired fasting glucose or impaired glucose tolerance, history of gestational diabetes, polycystic ovary syndrome, hypertension, and dyslipidemia31. The global age-standardized diabetes prevalence increased from 4.3% in 1980 to 9.0% in 2014 in men and from 5.0% to 7.9% in women32. Although the contribution of each factor to the increased diabetes incidence cannot be discerned, the increase in diabetes overlaps with the increase in obesity in other studies29,33,34. Therefore, it is not surprising that the prevalence of diabetes and pre-diabetes increased over the 6-year period in our study.
In real-life settings, the management of dyslipidemia remains far from optimal, both in primary and secondary prevention35. Data from a Beijing adult population showed that the prevalence of dyslipidemia was 30.3% in 2007 and 35.4% in 200836,37. In our study, the prevalence of dyslipidemia also showed an increasing trend. However, data based on a Lithuanian middle-aged population showed a declining prevalence of dyslipidemia from 1985–201338. Obesity is an independent risk factor of dyslipidemia, and the prevalence of dyslipidemia increases with BMI39,40. In our study, the rising trend in dyslipidemia was mainly attributable to the increased prevalence of high TG and low HDL-C levels, but not to high LDL-C. The prevalence of high LDL-C in this study decreased significantly in both men and women, and a similar result was also reported in a previous study, which showed a significant 5.7% decrease in LDL-C levels in adults aged 35–65 years from 1996 to 200741. The variation in LDL-C levels may be explained by subjects’ use of lipid-lowering drugs41.
In this study, we observed a significant increase in the prevalence of NAFLD in both genders. The global prevalence of NAFLD is reported to be 25.24%, with the highest prevalence occurring in the Middle East and South America and the lowest in Africa42. NAFLD is strongly associated with obesity, in particular with visceral fat and insulin resistance, and with the increasing prevalence of obesity43. In addition, regarding clinical characteristics, NAFLD patients tend to be obese and to have insulin resistance and/or type 2 diabetes, hypertriglyceridemia, and hypertension44,45,46. NAFLD is increasingly recognized as a hepatic component of metabolic syndrome47. As the global epidemic of obesity fuels the metabolic conditions necessary for NAFLD, the clinical and economic burden of NAFLD are expected to become substantial. Our results are thus consistent with the increasing trends observed elsewhere.
In our study, the age-standardized prevalence of hypertension remained relatively stable from 2007 to 2013 in both genders (males: 38.10% vs. 38.63%; females: 33.04% vs. 33.01%, respectively), and this stability was consistent with a study in Turkey and another study in Italy48,49. The prevalence of hypertension did not show increasing trends as observed in all other diseases. The reason for this finding may be associated with a decrease in salt consumption. The Nutrition and Chronic Diseases in Chinese Residents study (2015) showed that the average daily salt consumption was 10.5 grams in 2012, indicating a decrease of 1.5 grams from the consumption in 20026. However, some previous Chinese studies showed increasing trends of hypertension prevalence13,50. Data from the 24 geographically defined populations in the WHO Multinational MONItoring of trends and determinants in CArdiovascular disease (MONICA) Project showed that the age-adjusted prevalence of hypertension decreased in most and increased in only a few populations51.
The prevalence of hypertension increased with age in males and females in the two surveys. As age increases, a range of physiological changes occur, such as increased arterial stiffness, decreased renal salt excretion, declined renal function, and changes in the automatic nervous response to pharmacotherapy, which is used to manage hypertension52. However, the prevalence of the other diseases did not show the expected increasing trends with age.
Our results showed that men tended to have more obesity and obesity-related diseases than women in 2007 and 2013. The gender differences in these prevalences could be partially explained by men’s increased exposure to drinking and smoking.
This study is the first to assess the trends in the prevalence of obesity and obesity-related diseases using two cross-sectional health surveys in northeastern China with adjustments to minimize the differences in sample selection, measurements and case definitions.
It is important to acknowledge several limitations of our results. First, because of the nature of cross-sectional studies, causal relations could not be directly established. Second, we did not collect detailed information on diet, and we were thus unable to detect relationships between diet and the prevalence of the related diseases. Third, we measured FBG and blood pressure at a single visit, which might have led to an over- or underestimation of the true conditions. Finally, other confounders, such as different nationalities, socioeconomic status, residential density, noise pollution, drug use, diet, and physical activity, may also have influenced the results.
In conclusion, the results of these two cross-sectional surveys demonstrate a high prevalence of obesity and obesity-related diseases in the general population in northeastern China. Moreover, the prevalence of obesity, overweight, diabetes, pre-diabetes, dyslipidemia and NAFLD increased significantly from 2007 to 2013 in both men and women, whereas the prevalence of hypertension remained stable. Obesity and obesity-related diseases are the main risk factors of cardiometabolic diseases and pose a serious threat to the health of the general population1,32,46,53. More than 80% of the global diabetes and cardiovascular disease burden is expected to occur in low- and middle-income countries such as China and India by 202554. Thus, urgent action, optimal treatment approaches and appropriate public health strategies are needed to prevent and manage these diseases, with the ultimate goal of lowering the incidence of cardiometabolic disease.
Materials and Methods
Study population
Two independent population-based cross-sectional studies of obesity and obesity-related diseases were conducted in Dehui City in Jilin, China, one in 2007 and one in 2013. Dehui is located 81 km from Changchun, which is the largest city in the area. Most inhabitants in Dehui earn in the average income range. The fifth National Population Census of China (2000) showed that the population composition, namely the sex and age distribution, of Dehui inhabitants was similar to those of Jilin in general; furthermore, the Dehui City Comprehensive Development Index (which considers regional, economic, cultural and other factors) represents the average of Jilin Province. Therefore, Dehui City was selected to represent other areas in the province. The designs of both cross-sectional studies were similar. Survey participants were selected using a stratified, multistage cluster probability sampling method. The questionnaire-based study was supervised and assisted by the National Bureau of Statistics of China. The study was approved by the Ethics Committee of the First Hospital of Jilin University, and all subjects participating in the study provided their written informed consent. All methods were carried out in accordance with the approved guidelines. A total of 3,636 and 1359 subjects aged 20–75 years were enrolled in the 2007 and 2013 cross-sectional studies, respectively.
Data collection
All selected participants completed a standardized medical history and lifestyle questionnaire and underwent a comprehensive health examination according to routine procedures. A trained interviewer conducted face-to-face interviews with all participants and provided assistance to participants who had difficulty completing the questionnaire.
The participants fasted overnight (between 12 and 14 h) prior to receiving a comprehensive medical examination that included waist circumference (WC), standing height, weight and blood pressure (BP) measurements; a liver ultrasound; fasting blood samples to assess biochemical variables including liver enzymes, lipids, glucose and other routine blood measurements; and hepatitis B surface antigen (HBsAg) and anti-hepatitis C virus (anti-HCV) tests. Body weight and height were measured with the participants barefoot and in light clothing. Body mass index (BMI) was calculated as body weight divided by standing height squared. WC was measured on the horizontal plane between the inferior costal margin and the iliac crest on the mid-axillary line. Resting blood pressure was measured twice at 2-min intervals using a standard mercury sphygmomanometer after a 10-minute rest. Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were defined as the average of the two readings. If the two measurements differed by over 10 mmHg, blood pressure was measured a third time, and the average of the three measurements was used as the final measurement. Abdominal ultrasonography (US) was performed by trained experienced radiologists to detect the presence of fatty infiltration in the liver, and the same equipment was used across studies (180 ultrasound machine with a 3.5 MHZ probe (GE Health care, Wilmington, MA, USA)) to minimize procedure-related variability55. Blood samples were centrifuged at the examination location, and the sera were stored at −20 °C until being tested at the First Hospital of Jilin University.
Disease definition
In this study, diabetes was defined as a fasting plasma glucose (FPG) level ≥ 7.0 mmol/L, a previous diagnosis by a physician, or the use of insulin or oral hypoglycemic agents. Pre-diabetes was defined as 5.6 mmol/L ≤FPG < 7.0 mmol/L56.
Hypertension was defined as an average SBP ≥ 140 mmHg, an average DBP ≥ 90 mmHg, previously diagnosed disease, and/or the use of antihypertensive medication, regardless of BP readings57.
According to the Chinese Working Group on obesity, BMI < 18.5 kg/m2 was considered underweight, 18.5 kg/m2 ≤ BMI < 24 kg/m2 was considered normal, 24 kg/m2 ≤ BMI < 28 kg/m2 was defined as overweight, and BMI ≥ 28 kg/m2 was considered obese58.
According to the criteria of the “Chinese Guidelines on the Prevention and Treatment of Dyslipidemia in Adults”, hyperlipidemia was defined by a physician’s diagnosis and/or abnormal blood lipids (total cholesterol (TC) ≥ 5.18 mmol/L, triglycerides (TG) ≥ 1.7 mmol/L, high-density lipoprotein cholesterol (HDL-C) < 1.04 mmol/L or low-density lipoprotein cholesterol (LDL-C) ≥ 3.37 mmol/L)59.
Individuals with the following criteria were defined as having NAFLD: 1) a mean ethanol intake <140 g/week for men and <70 g/week for women in the past month, 2) a negative HBsAg and anti-HCV result, 3) fatty liver based on US, and 4) no other liver disease60.
Statistical analysis
All analyses were stratified by sex. The Kolmogorov–Smirnov test was applied to continuous variables to test for normality. Non-normal data were presented as the median and quartiles, and Mann-Whitney U test was used to assess the differences between the two groups. Categorical variables were expressed as frequencies (percentage) calculated with Pearson’s Chi-square test. The prevalence of obesity and obesity-related diseases was standardized by age (ASR) using direct standardization based on the population composition of the Sixth National Population Census of China (2010). For standardization, we divided the participants into three age ranges (20–44 years; 45–59 years; and 60–75 years); these age groups were in accordance with the criteria of the WHO in 2012, except for a minor change, in which subjects 75 years old were included in the third range21. We compared the ASRs between 2007 and 2013 with the following formula:  (SEASR, standardization standard error). Data were analyzed using SPSS software version 20.0 (SPSS Inc., Chicago, IL, USA) with a significance level of P < 0.05 for all analyses.
(SEASR, standardization standard error). Data were analyzed using SPSS software version 20.0 (SPSS Inc., Chicago, IL, USA) with a significance level of P < 0.05 for all analyses.
Additional Information
How to cite this article: Wu, J. et al. Six-year changes in the prevalence of obesity and obesity-related diseases in Northeastern China from 2007 to 2013. Sci. Rep. 7, 41518; doi: 10.1038/srep41518 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Material
Acknowledgments
This study was made possible in part by the statistical support provided by the Health Department in Jilin Province, China. We would also like to thank the nursing staff at the First Hospital of Jilin University for enabling this study by contributing their professional skills. This study was supported by the National Science and Technology Major Project (2014ZX10002002), the National Basic Research Program of China (973 Program) (2015CB554304), and the National Natural Science Foundation of China (grants 81373057, 81301472, 81270484, and 81301415).
Footnotes
The authors declare no competing financial interests.
Author Contributions Conceived and designed the experiment: N.J. and H.S.; Collected the data: H.X., W.C., S.J., W.J., X.H. and Y.Y.; Analyzed the data: W.J. and X.H.; Wrote the paper: W.J.; All authors reviewed the manuscript.
References
- Ng M. et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 384, 766–781 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi X. D. et al. Prevalence of obesity and associated risk factors in northeastern China. Diabet. Res. Clin. Pract. 91, 389–394 (2011). [DOI] [PubMed] [Google Scholar]
- Kelly T., Yang W., Chen C. S., Reynolds K. & He J. Global burden of obesity in 2005 and projections to 2030. Int. J. Obes. (Lond.). 32, 1431–1437 (2008). [DOI] [PubMed] [Google Scholar]
- Lim S. S. et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 380, 2224–2260 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon J. B. The effect of obesity on health outcomes. Mol. Cell. Endocrinol. 316, 104–108 (2010). [DOI] [PubMed] [Google Scholar]
- National Health and Family Planning Commission. Nutrition and chronic diseases in chinese residents (People’s Health Publishing House, 2015). [Google Scholar]
- Qin Y. et al. Prevalence, awareness, treatment and control of diabetes mellitus-a population based study in Shanghai, China. Int. J. Environ. Res. Public Health. 13, (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang F. et al. Prevalence, awareness, treatment and control of diabetes mellitus in rural China: results from Shandong Province. Diabet. Med. 33, 454–458 (2016). [DOI] [PubMed] [Google Scholar]
- Zhang P. et al. Prevalence of central obesity among adults with normal BMI and its association with metabolic diseases in northeast China. PLoS One. 11, e0160402 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu M. et al. Awareness, treatment and control of type 2 diabetes among Chinese elderly and its changing trend for past decade. BMC Public Health. 16, 278 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X. et al. Prevalence, awareness, treatment, control of type 2 diabetes mellitus and risk factors in Chinese rural population: the RuralDiab study. Sci. Rep. 6, 31426 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen X., Vaidya A., Wu S. & Gao X. The diabetes epidemic in China: an integrated review of national surveys. Endocr. Pract. 22, 1119–1129 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu L. et al. Trends in prevalence, awareness, treatment and control of hypertension during 2001–2010 in an urban elderly population of China. PLoS One. 10, e0132814 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z. et al. Trends in prevalence, awareness, treatment and control of hypertension in the middle-aged population of China, 1992–1998. Hypertens. Res. 27, 703–709 (2004). [DOI] [PubMed] [Google Scholar]
- Zhao Y. et al. Trends in hypertension prevalence, awareness, treatment, and control rates in Shandong Province of China. J. Clin. Hypertens. (Greenwich). 14, 637–643 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu B., Xu Z., Xu X., Cai Q. & Xu Y. Prevalence, awareness, treatment, and control of hypertension among residents in Guangdong Province, China, 2004 to 2007. Circ. Cardiovasc. Qual. Outcomes. 6, 217–222 (2013). [DOI] [PubMed] [Google Scholar]
- Hou X. et al. Ten-year changes in the prevalence of overweight, obesity and central obesity among the Chinese adults in urban Shanghai, 1998–2007 - comparison of two cross-sectional surveys. BMC Public Health. 13, 1064 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li M. Z. et al. Trends in prevalence, awareness, treatment, and control of diabetes mellitus in mainland china from 1979 to 2012. Int. J. Endocrinol. 2013, 753150 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin C. C. et al. Time trend analysis of the prevalence and incidence of diagnosed type 2 diabetes among adults in Taiwan from 2000 to 2007: a population-based study. BMC Public Health. 13, 318 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C. et al. Awareness, treatment, control of diabetes mellitus and the risk factors: survey results from northeast China. PLoS One. 9, e103594 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Letter from the editor: World Health Day 2012 focuses on ageing and health. East Mediterr. Health J. 18, 303 (2012). [PubMed] [Google Scholar]
- Stevens G. A. et al. National, regional, and global trends in adult overweight and obesity prevalences. Popul. Health Metr. 10, 22 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uauy R., Albala C. & Kain J. Obesity trends in Latin America: transiting from under- to overweight. J. Nutr. 131, 893S–899S (2001). [DOI] [PubMed] [Google Scholar]
- Astrup A. & Brand-Miller J. Diet composition and obesity. Lancet. 379, 1100; author reply 1100–1101 (2012). [DOI] [PubMed] [Google Scholar]
- Church T. S. et al. Trends over 5 decades in U.S. occupation-related physical activity and their associations with obesity. PLoS One. 6, e19657 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atiase Y. et al. A comparison of indices of glucose metabolism in five black populations: data from modeling the epidemiologic transition study (METS). BMC Public Health. 15, 895 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez-Velazquez J. A. et al. The prevalence of nonalcoholic fatty liver disease in the Americas. Ann. Hepatol. 13, 166–178 (2014). [PubMed] [Google Scholar]
- Luo J. Y. et al. Prevalence, awareness, treatment and control of dyslipidemia among adults in northwestern China: the cardiovascular risk survey. Lipids Health Dis. 13, 4 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin S. et al. Trends in diabetes and obesity in Samoa over 35 years, 1978–2013. Diabet. Med. 10.1111/dme.13197 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selvin E., Parrinello C. M., Sacks D. B. & Coresh J. Trends in prevalence and control of diabetes in the United States, 1988–1994 and 1999–2010. Ann. Intern. Med. 160, 517–525 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C. et al. Prevalence of type 2 diabetes among high-risk adults in Shanghai from 2002 to 2012. PLoS One. 9, e102926 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Risk N. C. D. Factor Collaboration. Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 387, 1513–1530 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin S. et al. Diabetes and obesity trends in Fiji over 30 years. J. Diabet. 8, 533–543 (2016). [DOI] [PubMed] [Google Scholar]
- Lin S. et al. Diabetes and obesity trends in Tonga over 40 years. Asia-Pac. J. Public Health. 28, 475–485 (2016). [DOI] [PubMed] [Google Scholar]
- Antiochos P., Marques-Vidal P., Waeber G. & Vollenweider P. Five year trends in dyslipidaemia prevalence and management in Switzerland: the CoLaus study. Nutr. Metab. Cardiovasc. Dis. 25, 1007–1015 (2015). [DOI] [PubMed] [Google Scholar]
- Cai L., Zhang L., Liu A., Li S. & Wang P. Prevalence, awareness, treatment, and control of dyslipidemia among adults in Beijing, China. J. Atheroscler. Thromb. 19, 159–168 (2012). [DOI] [PubMed] [Google Scholar]
- Zhang L., Qin L. Q., Liu A. P. & Wang P. Y. Prevalence of risk factors for cardiovascular disease and their associations with diet and physical activity in suburban Beijing, China. J. Epidemiol. 20, 237–243 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamosiunas A. et al. Trends in major risk factors and mortality from main non-communicable diseases in Lithuania, 1985–2013. BMC Public Health. 16, 717 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alkerwi A., Pagny S., Lair M. L., Delagardelle C. & Beissel J. Level of unawareness and management of diabetes, hypertension, and dyslipidemia among adults in Luxembourg: findings from ORISCAV-LUX study. PLoS One. 8, e57920 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bays H. E., Chapman R. H. & Grandy S. & Shield Investigators’ Group. The relationship of body mass index to diabetes mellitus, hypertension and dyslipidaemia: comparison of data from two national surveys. Int. J. Clin. Pract. 61, 737–747 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrieres J. et al. Trends in plasma lipids, lipoproteins and dyslipidaemias in French adults, 1996–2007. Arch. Cardiovasc. Dis. 102, 293–301 (2009). [DOI] [PubMed] [Google Scholar]
- Younossi Z. M. et al. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 64, 73–84 (2016). [DOI] [PubMed] [Google Scholar]
- Kelly A. S. et al. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation. 128, 1689–1712 (2013). [DOI] [PubMed] [Google Scholar]
- Vernon G., Baranova A. & Younossi Z. M. Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment. Pharmacol. Ther. 34, 274–285 (2011). [DOI] [PubMed] [Google Scholar]
- Li Z. et al. Prevalence of nonalcoholic fatty liver disease in mainland of China: a meta-analysis of published studies. J. Gastroenterol. Hepatol. 29, 42–51 (2014). [DOI] [PubMed] [Google Scholar]
- Speliotes E. K. et al. Fatty liver is associated with dyslipidemia and dysglycemia independent of visceral fat: the Framingham Heart Study. Hepatology. 51, 1979–1987 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chalasani N. et al. The diagnosis and management of non-alcoholic fatty liver disease: practice Guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Hepatology. 55, 2005–2023 (2012). [DOI] [PubMed] [Google Scholar]
- Sengul S. et al. Changes in hypertension prevalence, awareness, treatment, and control rates in Turkey from 2003 to 2012. J. Hypertens. 34, 1208–1217 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tocci G. et al. Trends in prevalence, awareness, treatment, and control of blood pressure recorded from 2004 to 2014 during World Hypertension Day in Italy. J. Clin. Hypertens. (Greenwich). 18, 551–556 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J. et al. Trends of hypertension prevalence, awareness, treatment and control in rural areas of northern China during 1991–2011. J. Hum. Hypertens. 28, 25–31 (2014). [DOI] [PubMed] [Google Scholar]
- Antikainen R. L. et al. Trends in the prevalence, awareness, treatment and control of hypertension: the WHO MONICA Project. Eur. J. Cardiovasc. Prev. Rehabil. 13, 13–29 (2006). [DOI] [PubMed] [Google Scholar]
- Pont L. & Alhawassi T. Challenges in the management of hypertension in older populations. Adv. Exp. Med. Biol. 10.1007/5584_2016_149 (2016). [DOI] [PubMed] [Google Scholar]
- Oguoma V. M., Nwose E. U. & Richards R. S. Prevalence of cardio-metabolic syndrome in Nigeria: a systematic review. Public Health. 129, 413–423 (2015). [DOI] [PubMed] [Google Scholar]
- Mohan I. et al. Disparities in prevalence of cardiometablic risk factors in rural, urban-poor, and urban-middle class women in India. PLoS One. 11, e0149437 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanyal A. J. & American Gastroenterological Association. AGA technical review on nonalcoholic fatty liver disease. Gastroenterology. 123, 1705–1725 (2002). [DOI] [PubMed] [Google Scholar]
- American Diabetes Association. Standards of medical care in diabetes–2011. Diabet. Care. 34 Suppl 1, S11–61 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chobanian A. V. et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 42, 1206–1252 (2003). [DOI] [PubMed] [Google Scholar]
- Zhou B. F. & Cooperative Meta-Analysis Group of the Working Group on Obesity in China. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults–study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed. Environ. Sci. 15, 83–96 (2002). [PubMed] [Google Scholar]
- Joint Committee for Developing Chinese guidelines on Prevention Treatment of Dyslipidemia in Adults. [Chinese guidelines on prevention and treatment of dyslipidemia in adults]. Zhonghua Xin Xue Guan Bing Za Zhi. 35, 390–419 (2007). [PubMed] [Google Scholar]
- Wang J. et al. ZJU index: a novel model for predicting nonalcoholic fatty liver disease in a Chinese population. Sci. Rep. 5, 16494 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.