Abstract
Background
Thirty-day readmission rates after acute myocardial infarction (AMI) and heart failure are important patient outcome metrics. Early post-discharge physician follow-up has been promoted as a method of reducing 30-day readmission rates. However, the relationships between early post-discharge follow-up and 30-day readmission for AMI and heart failure are inconclusive. We used nationwide population-based data to examine associations between 7-day physician follow-up and 30-day readmission, and further associations of 7-day same physician (during the index hospitalization and at follow-up) and cardiologist follow-up with 30-day readmission for non-ST-segment-elevation myocardial infarction (NSTEMI) or heart failure.
Methods
We analyzed all patients 18 years or older with NSTEMI and heart failure and discharged from hospitals in 2010 in Taiwan through Taiwan’s National Health Insurance Research Database. Cox proportional hazard models with robust sandwich variance estimates and propensity score weighting were performed after adjustment for patient and hospital characteristics to test associations between 7-day physician follow-up and 30-day readmission.
Results
The study population for NSTEMI and heart failure included 5,008 and 13,577 patients, respectively. Early physician follow-up was associated with a lower hazard ratio of readmission compared with no early physician follow-up for patients with NSTEMI (hazard ratio [HR], 0.47; 95% confidence interval [CI], 0.39–0.57), and for patients with heart failure (HR, 0.54; 95% CI, 0.48–0.60). Same physician follow-up was associated with a reduced hazard ratio of readmission compared with different physician follow-up for patients with NSTEMI (HR, 0.56; 95% CI, 0.48–0.65), and for patients with heart failure (HR, 0.69; 95% CI, 0.62–0.76).
Conclusions
For each condition, patients who have an outpatient visit with a physician within 7 days of discharge have a lower risk of 30-day readmission. Moreover, patients who have an outpatient visit with the same physician within 7 days of discharge have a much lower risk of 30-day readmission.
Introduction
Policy makers, clinicians, and payers who seek to improve outcomes in health care are focusing on 30-day readmission rates for patients with acute myocardial infarction and those with heart failure.[1] Early post-discharge physician follow-up has been promoted as a method of reducing readmission rates.[2] However, studies on the relationships between early post-discharge follow-up and patient outcomes for acute myocardial infarction and heart failure are not only rare but also inconclusive. Of only two studies we are aware of on this topic, one showed that discharge from hospitals that have higher early follow-up rates is associated with a reduction in 30-day readmission for heart failure,[3] but another did not establish such relationship for acute myocardial infarction.[4] Moreover, to our knowledge, no study has examined whether early follow-up with the same physician or with a cardiologist is associated with lower 30-day readmission for patients with acute myocardial infarction and those with heart failure.
Early or timely outpatient follow-up with a physician for further assessment or treatment has been hypothesized to have an effect on reduced readmission among discharged patients with heart failure and those with acute myocardial infarction.[3–7] The transition from hospital to home is a period of particularly higher risk. Timely post-discharge follow-up has been suggested as an important component of efforts to optimize transitional care during the high-risk peri-discharge period.[8, 9] With physiological stress and allostatic load derived from hospitalization, the risks in the critical 30-day period after discharge might exist.[10] More importantly, the immediate days that follow discharge are also a vulnerable period owing to the additional therapies or changes in existing medical therapy that may worsen patient outcomes.[3, 11] Seven-day follow-up with the physicians may have the benefit of improving patient outcomes through providing clinical interventions on disease instability (such as diagnostic testing and medication changes),[12] and 7-day follow-up with the same physician (because of physician continuity) or with a specialist (because of physician specialty) may be associated with better outcomes than follow-up with other physicians.[3, 4] However, few studies have examined the relationship between 7-day physician follow-up and patient outcomes.
In Taiwan, the National Health Insurance Administration has been the sole insurer and implemented national health insurance since March 1, 1995. The coverage rate of national health insurance has reached 99.9%, and almost all health care facilities are national health insurance contracted providers. Every enrollee is free to go to any hospital or clinic, and enjoys comprehensive benefits with a low cost-sharing policy (10% coinsurance for inpatient care with a yearly cap of about US$1700, and a US$1.7–12.0 copayment for outpatient visits). The National Health Insurance Administration has reimbursed providers mainly on a fee-for-service basis since the beginning of the national health insurance program. The Hospital Readmissions Reduction Program, which, under the Affordable Care Act, requires the Centers for Medicare & Medicaid Services to reduce payments to hospitals with excessive readmission rates regarding acute myocardial infarction and heart failure,[13] has not yet been introduced in Taiwan. Therefore, Taiwan’s healthcare system provides an excellent opportunity to examine whether early post-discharge follow-up improves patient outcomes for patients with acute myocardial infarction and those with heart failure.
To better understand the relationship between early post-discharge follow-up and patient outcomes, we used nationwide population-based data from Taiwan to examine whether physician follow-up within 7 days of discharge was associated with a reduction in 30-day readmission for patients with acute myocardial infarction and those with heart failure. We also further determined whether early follow-up with the same physician or with a cardiologist was associated with much better patient outcomes.
Methods
Database
In this study, we used the National Health Insurance Research Database, provided by the National Health Insurance Administration and managed by the National Health Research Institutes in Taiwan. The database, which is released annually, consists of the following dimensions: inpatient medical benefit claims, ambulatory care medical benefit claims, pharmaceutical benefit claims, contracted medical care institutions, health professionals in contracted medical care institutions, and beneficiaries. Therefore, the database provides an opportunity to examine the relationship between early post-discharge follow-up and patient outcomes.
Ethical Statement
The protocol for this study was approved by the Institutional Review Board of the National Taiwan University Hospital (protocol # 201601056RINB). The dataset we used in this study was secondary data; all information was de-identified by data owners.
Study Population
This study included all patients aged 18 years and over who were discharged from general acute care hospitals in 2010, with a principal diagnosis of acute myocardial infarction without ST-segment elevation (International Classification of Diseases, 9th revision, clinical modification [ICD-9-CM] code 410.7)[4, 14–16] and heart failure with or without preserved ejection fraction (ICD-9-CM code 428), respectively.[17–20] Only the first admission of patients with multiple hospitalizations was included for the same medical condition.[3, 4] We excluded patients who were admitted with the same medical condition during the past 6 years, died in the hospital, were transferred out, left the hospital against medical advice, or were discharged against medical advice in a terminally critical condition.[4, 21]
Measures of Variables
Early follow-up
Early follow-up was defined as whether discharged patients had an outpatient visit with a physician within 7 days after discharge.[3, 4] The length of seven days was selected to be consistent with current efforts to improve transitional care.[22] Early follow-up with the same physician was measured as whether discharged patients visited the same physician during the hospitalization and during early follow-up.[3] Patients who visit the same physician during the hospitalization and at follow-up are considered to have better continuity of care.[3, 19] Early follow-up with a cardiologist was defined as whether discharged patients visited a cardiologist within 7 days after discharge.[3, 4] To explore whether the combined effect of same physician follow-up and cardiologist follow-up on patient outcomes, the interaction term between same physician follow-up and cardiologist follow-up was also considered.
Patient and hospital characteristics
The covariates included patient and hospital characteristics. The patient covariates included sex, age, comorbid conditions, medical history, in-hospital treatment (percutaneous coronary intervention use, intensive care unit use, administration of surgical operation), length of stay, baseline medications (aspirin, β-blocker, statin, angiotensin-converting enzyme inhibitor/angiotensin receptor blocker), medications within 7 days of discharge, low income, rural residence, number of hospitalizations during the past year, and number of office visits during the past year.[3, 4, 9, 19, 23–26].
The Charlson-Deyo index was used to quantify patient comorbidities.[27] This index is the sum of the weighted scores based on the presence or absence of 17 different medical conditions during the past year and the index hospitalization. A score of 0 means that no comorbid index is present, and higher scores point to a greater burden of comorbidity. In addition, we also measured patients’ medical history specially related to cardiovascular conditions during the past year and the index hospitalization, which included cardiac risk factors (hypertension, diabetes mellitus), prior cardiac conditions (myocardial infarction, heart failure, atrial fibrillation or flutter), and medical comorbidities (peripheral vascular disease, renal disease).[28] The use of the baseline medications was measured according to whether the medications were prescribed during hospital stays and at discharge. Low income was measured as whether the patient was enrolled as a low-income beneficiary. Rural residence was measured whether the patient lived in a rural area based on previous studies using National Health Insurance Research Database.[29–32]
The hospital covariates included hospital volume (low, medium, high), hospital level (academic medical center, regional, district), teaching status (yes/no), and geographic location (Taipei, northern, central, southern, Kao-Ping, eastern). We determined the volume of patients who were treated at hospitals using annual condition-specific volume, and then we divided these “annualized” volumes into tertiles.
Outcome measures
Our primary outcome was 30-day all-cause readmission, which was defined as any re-hospitalization to any acute care hospital within 30 days from index discharge.[3, 4] Hospital readmissions are regarded as potential indicators of poor care or missed opportunities to better coordinate care.[33, 34] Additionally, readmission is expensive to the health care system and commonly represents a preventable adverse event for patients.[24] Secondary outcomes of interest were readmission within 30 days of discharge for cardiovascular cause (primary and secondary ICD-9-CM codes 390–459)[17, 35] and readmission within 30 days of discharge for the same cause as the index hospitalization.
Statistical Analysis
We used Cox proportional hazard models with robust sandwich variance estimates and propensity score weighting, adjusted for all patient and hospital characteristics, to examine the association between 7-day physician follow-up and 30-day readmission for acute myocardial infarction and heart failure.[28, 36] Cox proportional hazard models allows us to take into account the length of survival after discharge to avoid the problem that patients with early visit are the most severe ones and then they were less likely to be re-hospitalized because they die more often. The models focused on time from discharge until the first re-hospitalization date during the 30 days of follow-up. Patients were censored on date of death, or 30 days post-discharge, whichever came first. All analyses were adjusted for clustering at the hospital level with the use of robust sandwich variance estimates. We modeled 30-day readmission as a function of 7-day physician follow-up, sex, age, comorbid conditions, medical history, in-hospital treatment, length of stay, baseline medications, low income, rural residence, number of hospitalizations during the past year, number of office visits during the past year, hospital volume, hospital level, teaching status, and geographic location.
Moreover, we used propensity score analyses to reduce the selection bias and the potential baseline differences between the early follow-up and the no early follow-up groups.[9, 28] Propensity scores were computed by modeling a logistic regression model in which the dependent variable was whether the discharged patient had an outpatient visit with a physician within 7 days after discharge. The independent variables were patient sex, age, comorbid conditions, medical history, in-hospital treatment, length of stay, baseline medications, low income, rural residence, number of hospitalizations during the past year, number of office visits during the past year, hospital volume, hospital level, teaching status, and geographic location. Then, each patient was weighted by the inverse propensity score when performing Cox proportional hazard models with robust sandwich variance estimates to reduce the selection bias.[25, 37–40]
Finally, we further used Cox proportional hazard models with robust sandwich variance estimates, adjusted for all patient (including medications after discharge) and hospital characteristics, to examine the individual and combined associations of early same physician and early cardiologist follow-up with 30-day readmission among the early follow-up group. In sensitivity analyses, we changed the definition of early physician follow-up by allowing early follow-up to occur within 14 days after discharge.[3] Statistical significance was indicated by a 2-tailed value of P<0.05. All analyses were performed with SAS version 9.3 (SAS Institute Inc, Cary, NC).
Results
Baseline Characteristics and Outcomes
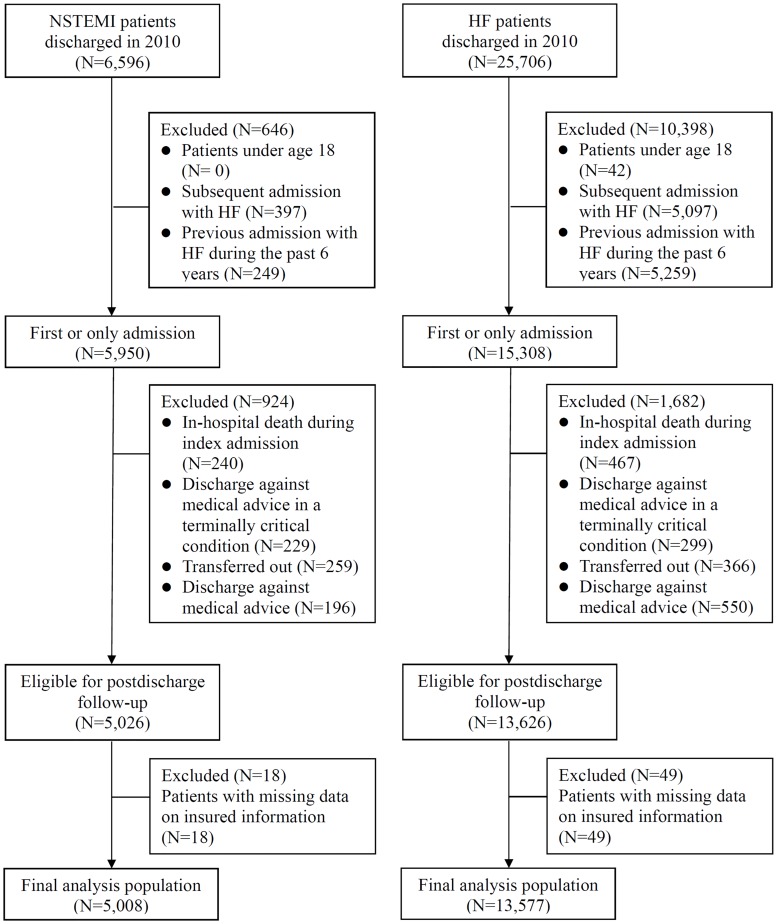
Regarding non-ST-segment-elevation myocardial infarction (NSTEMI), we identified 6596 patients discharged from hospital in 2010. We excluded patients under age 18 (N = 0), and patients who had subsequent admission with NSTEMI (N = 397), or had previous admission with NSTEMI during the past 6 years (N = 249). After exclusions (Fig 1), the final NSTEMI population included 5008 patients. The final population with heart failure consisted of 13577 patients.
Fig 1. Flow diagram of patient selection.
Shown are inclusions and exclusions and the final study cohort. HF indicates heart failure; NSTEMI, non-ST-segment-elevation myocardial infarction.
Table 1 presents these patient characteristics. Among patients with NSTEMI, rates of early follow-up with a physician, with the same physician, and with a cardiologist were 76.7%, 56.1%, and 44.8%, respectively. Among those with heart failure, rates of early follow-up with a physician, with the same physician, and with a cardiologist were 74.9%, 52.9%, and 37.6%, respectively. Thirty-day all-cause readmission rates for patients with NSTEMI and those with heart failure were 19.9% and 23.3%, respectively.
Table 1. Characteristics of the study population.
| NSTEMI | Heart failure | |
|---|---|---|
| N(%) | N(%) | |
| No. of patients | 5008(100.0) | 13577(100.0) |
| Follow-up with a physician | ||
| 7-day | 3841(76.7) | 10164(74.9) |
| 14-day | 4664(93.1) | 12197(89.8) |
| Follow-up with the same physician | ||
| 7-day | 2807(56.1) | 7178(52.9) |
| 14-day | 3614(72.2) | 8996(66.3) |
| Follow-up with a cardiologist | ||
| 7-day | 2242(44.8) | 5103(37.6) |
| 14-day | 2862(57.1) | 6455(47.5) |
| Patient Characteristics | ||
| Male sex | 3367(67.2) | 6824(50.3) |
| Age, y | ||
| 18–49 | 520(10.4) | 1026(7.6) |
| 50–64 | 1456(29.1) | 2345(17.3) |
| 65–79 | 1920(38.3) | 5058(37.3) |
| 80+ | 1112(22.2) | 5148(37.9) |
| Charlson score | ||
| 0–1 | 2181(43.6) | 3838(28.3) |
| 2–3 | 1518(30.3) | 4988(36.7) |
| 4+ | 1309(26.1) | 4751(35.0) |
| Medical history | ||
| Hypertension | 3829(76.5) | 10617(78.2) |
| No | 1179(23.5) | 2960(21.8) |
| Diabetes mellitus | 2439(48.7) | 6194(45.6) |
| No | 2569(51.3) | 7383(54.4) |
| Myocardial infarction | 650(13.0) | 1304(9.6) |
| No | 4358(87.0) | 12273(90.4) |
| Heart Failure | 827(16.5) | 5930(43.7) |
| No | 4181(83.5) | 7647(56.3) |
| Atrial fibrillation or flutter | 511(10.2) | 3889(28.6) |
| No | 4497(89.8) | 9688(71.4) |
| Peripheral vascular disease | 182(3.6) | 564(4.2) |
| No | 4826(96.4) | 13013(95.8) |
| Renal disease | 923(18.4) | 2697(19.9) |
| No | 4085(81.6) | 10880(80.1) |
| In-hospital treatment | ||
| PCI | 2893(57.8) | 458(3.4) |
| Intensive care unit use | 4311(86.1) | 2969(21.9) |
| Surgery use | 471(9.4) | 582(4.3) |
| Length of stay, d | ||
| <5 | 2039(40.7) | 5671(41.8) |
| 6–9 | 1512(30.2) | 4366(32.2) |
| 10+ | 1457(29.1) | 3540(26.1) |
| Baseline medications | ||
| Aspirin | 4710(94.0) | 6573(48.4) |
| β-Blocker | 3183(63.6) | 5268(38.8) |
| Statin | 2961(59.1) | 2283(16.8) |
| ACEI/ARB | 3610(72.1) | 7995(58.9) |
| Medications within 7 days of discharge | ||
| Aspirin | 2590(51.7) | 3571(26.3) |
| β-Blocker | 1832(36.6) | 3233(23.8) |
| Statin | 1670(33.3) | 1292(9.5) |
| ACEI/ARB | 1792(35.8) | 4305(31.7) |
| Medications within 14 days of discharge | ||
| Aspirin | 3425(68.4) | 4637(34.2) |
| β-Blocker | 2450(48.9) | 4380(32.3) |
| Statin | 2272(45.4) | 1752(12.9) |
| ACEI/ARB | 2403(48.0) | 5660(41.7) |
| Low income | 98(2.0) | 305(2.2) |
| Rural residence | 1205(24.1) | 3687(27.2) |
| Number of hospitalizations during the past year | ||
| 0 | 3312(66.1) | 6935(51.1) |
| 1 | 942(18.8) | 3344(24.6) |
| 2+ | 754(15.1) | 3298(24.3) |
| Number of outpatient visits during the past year | ||
| Low | 1696(33.9) | 4610(34.0) |
| Medium | 1648(32.9) | 4447(32.8) |
| High | 1664(33.2) | 4520(33.3) |
| Hospital Characteristics | ||
| Hospital volume | ||
| Low | 1685(33.6) | 4675(34.4) |
| Medium | 1693(33.8) | 4575(33.7) |
| High | 1630(32.5) | 4327(31.9) |
| Hospital level | ||
| Academic medical center | 2797(55.9) | 4571(33.7) |
| Regional | 2077(41.5) | 6984(51.4) |
| District | 134(2.7) | 2022(14.9) |
| Teaching | 4939(98.6) | 12003(88.4) |
| Location | ||
| Taipei | 1743(34.8) | 4608(33.9) |
| Northern | 581(11.6) | 1841(13.6) |
| Central | 799(16.0) | 2534(18.7) |
| Southern | 858(17.1) | 2054(15.1) |
| Kao-Ping | 855(17.1) | 2073(15.3) |
| Eastern | 172(3.4) | 467(3.4) |
| Patient outcomes | ||
| 30-day readmission | ||
| All-cause | 998(19.9) | 3169(23.3) |
| Specific-cause | ||
| Cardiovascular | 935(18.7) | 2842(20.9) |
| Same diagnosis | 182(3.6) | 1983(14.6) |
NSTEMI indicates non-ST-segment-elevation myocardial infarction; and PCI, percutaneous coronary intervention.
Associations of Early Follow-Up with Patient and Hospital Characteristics
Table 2 shows the comparison of the discharges followed by outpatient visits with a physician within 7 days to those without. For NSTEMI, baseline characteristics that differed between the follow-up and the no follow-up groups were medical history (heart failure, atrial fibrillation or flutter),PCI use, length of saty, statin use, number of outpatient visits during the past year, hospital volume, level, and location. For heart failure, baseline characteristics that differed between the follow-up and the no follow-up groups were medical history (hypertension, heart failure), PCI use, length of stay, number of hospitalizations during the past year, number of outpatient visits during the past year, hospital volume, level, teaching status, and location. After propensity score weighting, the two groups for NSTEMI and heart failure were well balanced for the baseline characteristics.
Table 2. Baseline characteristics by early follow-up.
| NSTEMI | Heart failure | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unweighting | Weightinga | Unweighting | Weightinga | |||||||||
| Follow-up | Follow-up | Follow-up | Follow-up | |||||||||
| Yes, % | No, % | P value | Yes, % | No, % | P value | Yes, % | No, % | P value | Yes, % | No, % | P value | |
| Patient Characteristics | ||||||||||||
| Sex | ||||||||||||
| Male | 67.1 | 67.7 | 0.701 | 67.2 | 66.7 | 0.602 | 50.0 | 51.0 | 0.312 | 50.2 | 49.8 | 0.495 |
| Female | 32.9 | 32.3 | 32.9 | 33.3 | 50.0 | 49.0 | 49.8 | 50.2 | ||||
| Age, y | ||||||||||||
| 18–49 | 10.3 | 10.8 | 0.642 | 10.4 | 10.9 | 0.851 | 7.3 | 8.3 | 0.070 | 7.6 | 7.6 | 0.974 |
| 50–64 | 29.2 | 28.7 | 29.1 | 28.4 | 17.2 | 17.6 | 17.2 | 17.0 | ||||
| 65–79 | 38.7 | 37.2 | 38.3 | 38.6 | 37.8 | 35.7 | 37.3 | 37.3 | ||||
| 80+ | 21.9 | 23.3 | 22.2 | 22.2 | 37.8 | 38.4 | 37.9 | 38.1 | ||||
| Charlson score | ||||||||||||
| 0–1 | 43.5 | 43.6 | 0.214 | 43.6 | 43.5 | 0.996 | 28.1 | 28.7 | 0.796 | 28.3 | 28.4 | 0.796 |
| 2–3 | 29.8 | 32.0 | 30.3 | 30.4 | 36.8 | 36.4 | 36.8 | 37.1 | ||||
| 4+ | 26.7 | 24.4 | 26.2 | 26.2 | 35.0 | 34.8 | 35.0 | 34.6 | ||||
| Medical history | ||||||||||||
| Hypertension | ||||||||||||
| Yes | 76.8 | 75.5 | 0.375 | 76.5 | 77.0 | 0.529 | 78.7 | 76.7 | 0.017 | 78.2 | 78.1 | 0.850 |
| No | 23.2 | 24.5 | 23.5 | 23.0 | 21.3 | 23.3 | 21.8 | 21.9 | ||||
| Diabetes mellitus | ||||||||||||
| Yes | 48.6 | 48.9 | 0.860 | 48.7 | 48.7 | 0.980 | 45.8 | 44.9 | 0.360 | 45.6 | 45.4 | 0.781 |
| No | 51.4 | 51.1 | 51.3 | 51.3 | 54.2 | 55.1 | 54.4 | 54.6 | ||||
| Myocardial infarction | ||||||||||||
| Yes | 12.7 | 13.8 | 0.343 | 13.0 | 12.5 | 0.459 | 9.3 | 10.4 | 0.079 | 9.6 | 9.6 | 0.961 |
| No | 87.3 | 86.2 | 87.0 | 87.5 | 90.7 | 89.6 | 90.4 | 90.4 | ||||
| Heart Failure | ||||||||||||
| Yes | 15.6 | 19.5 | 0.002 | 16.5 | 16.4 | 0.917 | 43.0 | 45.6 | 0.009 | 43.7 | 43.5 | 0.828 |
| No | 84.4 | 80.5 | 83.5 | 83.6 | 57.0 | 54.4 | 56.3 | 56.5 | ||||
| Atrial fibrillation or flutter | ||||||||||||
| Yes | 9.7 | 11.9 | 0.028 | 10.2 | 10.0 | 0.788 | 28.8 | 28.1 | 0.415 | 28.7 | 28.9 | 0.642 |
| No | 90.3 | 88.1 | 89.8 | 90.0 | 71.2 | 71.9 | 71.3 | 71.1 | ||||
| Peripheral vascular disease | ||||||||||||
| Yes | 3.7 | 3.5 | 0.801 | 3.6 | 3.7 | 0.865 | 4.1 | 4.2 | 0.749 | 4.2 | 4.1 | 0.835 |
| No | 96.3 | 96.5 | 96.4 | 96.3 | 95.9 | 95.8 | 95.9 | 95.9 | ||||
| Renal disease | ||||||||||||
| Yes | 18.6 | 17.9 | 0.600 | 18.5 | 18.6 | 0.882 | 19.8 | 19.9 | 0.920 | 19.8 | 19.5 | 0.552 |
| No | 81.4 | 82.1 | 81.5 | 81.4 | 80.2 | 80.1 | 80.2 | 80.5 | ||||
| In-hospital treatment | ||||||||||||
| PCI | ||||||||||||
| Yes | 59.1 | 53.3 | <0.001 | 57.7 | 57.4 | 0.748 | 3.7 | 2.3 | <0.001 | 3.4 | 3.3 | 0.583 |
| No | 40.9 | 46.7 | 42.3 | 42.6 | 96.3 | 97.7 | 96.6 | 96.8 | ||||
| Intensive care unit use | ||||||||||||
| Yes | 86.0 | 86.5 | 0.670 | 86.1 | 86.1 | 0.934 | 21.7 | 22.4 | 0.398 | 21.9 | 21.8 | 0.966 |
| No | 14.0 | 13.5 | 13.9 | 13.9 | 78.3 | 77.6 | 78.1 | 78.2 | ||||
| Surgery use | ||||||||||||
| Yes | 9.5 | 9.2 | 0.752 | 9.4 | 10.0 | 0.384 | 4.2 | 4.6 | 0.253 | 4.3 | 4.2 | 0.850 |
| No | 90.5 | 90.8 | 90.6 | 90.0 | 95.8 | 95.4 | 95.7 | 95.8 | ||||
| Length of stay, d | ||||||||||||
| <5 | 41.4 | 38.3 | 0.043 | 40.7 | 40.7 | 0.993 | 42.6 | 39.4 | <0.001 | 41.8 | 41.8 | 0.916 |
| 6–9 | 30.3 | 29.8 | 30.2 | 30.3 | 32.5 | 31.2 | 32.2 | 32.4 | ||||
| 10+ | 28.2 | 31.9 | 29.1 | 29.0 | 24.9 | 29.4 | 26.1 | 25.9 | ||||
| Baseline medications | ||||||||||||
| Aspirin | ||||||||||||
| Yes | 94.4 | 92.9 | 0.055 | 94.1 | 94.2 | 0.773 | 48.5 | 48.1 | 0.683 | 48.4 | 48.3 | 0.832 |
| No | 5.6 | 7.1 | 5.9 | 5.8 | 51.5 | 51.9 | 51.6 | 51.7 | ||||
| β-Blocker | ||||||||||||
| Yes | 63.8 | 62.7 | 0.499 | 63.6 | 64.0 | 0.707 | 38.7 | 39.1 | 0.693 | 38.8 | 38.6 | 0.739 |
| No | 36.2 | 37.3 | 36.4 | 36.0 | 61.3 | 60.9 | 61.2 | 61.4 | ||||
| Statin | ||||||||||||
| Yes | 58.3 | 61.7 | 0.041 | 59.1 | 59.4 | 0.800 | 16.8 | 16.7 | 0.878 | 16.8 | 16.8 | 0.995 |
| No | 41.7 | 38.3 | 40.9 | 40.6 | 83.2 | 83.3 | 83.2 | 83.2 | ||||
| ACEI/ARB | ||||||||||||
| Yes | 71.6 | 73.8 | 0.141 | 72.1 | 71.6 | 0.644 | 58.9 | 58.9 | 0.961 | 58.9 | 58.6 | 0.681 |
| No | 28.4 | 26.2 | 28.0 | 28.4 | 41.1 | 41.1 | 41.1 | 41.4 | ||||
| Low income | ||||||||||||
| Yes | 1.9 | 2.1 | 0.779 | 2.0 | 2.1 | 0.669 | 2.1 | 2.6 | 0.075 | 2.2 | 2.2 | 0.679 |
| No | 98.1 | 97.9 | 98.0 | 97.9 | 97.9 | 97.4 | 97.8 | 97.8 | ||||
| Rural residence | ||||||||||||
| Yes | 24.4 | 23.0 | 0.317 | 24.1 | 23.9 | 0.872 | 27.4 | 26.3 | 0.184 | 27.2 | 27.3 | 0.776 |
| No | 75.6 | 77.0 | 76.0 | 76.1 | 72.6 | 73.7 | 72.8 | 72.7 | ||||
| Number of hospitalizations during the past year | ||||||||||||
| 0 | 66.9 | 63.8 | 0.105 | 66.1 | 65.6 | 0.784 | 52.1 | 48.1 | <0.001 | 51.1 | 51.5 | 0.798 |
| 1 | 18.2 | 20.7 | 18.9 | 19.4 | 24.5 | 25.0 | 24.6 | 24.5 | ||||
| 2+ | 14.9 | 15.5 | 15.1 | 15.0 | 23.4 | 26.9 | 24.3 | 24.0 | ||||
| Number of outpatient visits during the past year | ||||||||||||
| Low | 32.7 | 37.6 | <0.001 | 33.8 | 33.4 | 0.889 | 31.9 | 40.0 | <0.001 | 33.9 | 33.9 | 0.982 |
| Medium | 32.0 | 35.9 | 33.0 | 33.4 | 32.3 | 34.0 | 32.8 | 32.9 | ||||
| High | 35.3 | 26.5 | 33.2 | 33.2 | 35.7 | 26.0 | 33.3 | 33.3 | ||||
| Hospital Characteristics | ||||||||||||
| Hospital volume | ||||||||||||
| Low | 35.3 | 28.2 | <0.001 | 33.7 | 34.4 | 0.783 | 35.5 | 31.4 | <0.001 | 34.4 | 34.3 | 0.819 |
| Medium | 33.9 | 33.5 | 33.8 | 33.6 | 33.9 | 33.2 | 33.7 | 34.1 | ||||
| High | 30.8 | 38.3 | 32.5 | 32.1 | 30.7 | 35.4 | 31.9 | 31.6 | ||||
| Hospital level | ||||||||||||
| Academic medical center | 53.9 | 62.4 | <0.001 | 55.8 | 55.0 | 0.742 | 31.5 | 40.1 | <0.001 | 33.7 | 33.7 | 0.967 |
| Regional | 43.2 | 35.7 | 41.6 | 42.3 | 53.0 | 46.7 | 51.4 | 51.3 | ||||
| District | 2.9 | 1.9 | 2.7 | 2.7 | 15.5 | 13.2 | 14.9 | 15.0 | ||||
| Teaching | ||||||||||||
| Yes | 98.5 | 98.9 | 0.377 | 1.4 | 1.4 | 0.874 | 88.1 | 89.4 | 0.043 | 88.4 | 88.4 | 0.946 |
| No | 1.5 | 1.1 | 98.6 | 98.6 | 11.9 | 10.6 | 11.6 | 11.6 | ||||
| Location | ||||||||||||
| Taipei | 34.0 | 37.4 | <0.001 | 34.7 | 33.8 | 0.934 | 32.9 | 37.0 | <0.001 | 33.9 | 33.9 | 0.997 |
| Northern | 10.9 | 13.9 | 11.6 | 11.6 | 13.7 | 13.0 | 13.5 | 13.4 | ||||
| Central | 15.2 | 18.3 | 16.0 | 16.2 | 18.6 | 18.7 | 18.7 | 18.8 | ||||
| Southern | 18.2 | 13.5 | 17.2 | 17.8 | 16.0 | 12.6 | 15.1 | 15.2 | ||||
| Kao-Ping | 18.4 | 12.9 | 17.1 | 17.3 | 15.2 | 15.6 | 15.3 | 15.3 | ||||
| Eastern | 3.3 | 4.0 | 3.4 | 3.3 | 3.6 | 3.1 | 3.4 | 3.4 | ||||
NSTEMI indicates non-ST-segment-elevation myocardial infarction; and PCI, percutaneous coronary intervention.
aBased on propensity score weighting.
Associations between Early Follow-Up and 30-Day Readmission
Table 3 shows the unadjusted associations of early physician follow-up, and patient and hospital characteristics with 30-day readmission. For each condition, early follow-up with a physician, early follow-up with the same physician, and early follow-up with a cardiologist were associated with reduced 30-day readmission. For two conditions, patient and hospital characteristics associated with 30-day readmission were patient sex, age, comorbid conditions, medical history, in-hospital treatment, length of stay, baseline medications, medications within 7 days of discharge, low income, number of hospitalizations during the past year, number of outpatient visits during the past year, hospital volume, level, and teaching status.
Table 3. 30-day all-cause readmission rates by follow-up and baseline characteristics.
| NSTEMI | Heart failure | |||
|---|---|---|---|---|
| % | P value | % | P value | |
| Early follow-up | ||||
| Yes | 17.4 | <0.001 | 20.7 | <0.001 |
| No | 28.3 | 31.2 | ||
| Early follow-up with the same physician | ||||
| Yes | 14.4 | <0.001 | 18.1 | <0.001 |
| No | 27.0 | 29.2 | ||
| Early follow-up with a cardiologist | ||||
| Yes | 15.3 | <0.001 | 18.1 | <0.001 |
| No | 23.6 | 26.5 | ||
| Patient Characteristics | ||||
| Sex | ||||
| Male | 18.5 | <0.001 | 23.8 | 0.205 |
| Female | 22.9 | 22.9 | ||
| Age (yr) | ||||
| 18–49 | 11.7 | <0.001 | 18.4 | <0.001 |
| 50–64 | 16.9 | 20.0 | ||
| 65–79 | 21.2 | 23.3 | ||
| 80+ | 25.5 | 25.9 | ||
| Charlson score | ||||
| 0–1 | 12.3 | <0.001 | 17.9 | <0.001 |
| 2–3 | 22.0 | 22.0 | ||
| 4+ | 30.2 | 29.1 | ||
| Medical history | ||||
| Hypertension | ||||
| Yes | 21.1 | <0.001 | 23.7 | 0.086 |
| No | 16.0 | 22.2 | ||
| Diabetes mellitus | ||||
| Yes | 24.3 | <0.001 | 24.8 | <0.001 |
| No | 15.8 | 22.1 | ||
| Myocardial infarction | ||||
| Yes | 22.9 | 0.040 | 26.5 | 0.005 |
| No | 19.5 | 23.0 | ||
| Heart Failure | ||||
| Yes | 30.2 | <0.001 | 25.6 | <0.001 |
| No | 17.9 | 21.6 | ||
| Atrial fibrillation or flutter | ||||
| Yes | 24.7 | 0.005 | 22.4 | 0.090 |
| No | 19.4 | 23.7 | ||
| Peripheral vascular disease | ||||
| Yes | 25.3 | 0.066 | 28.9 | 0.001 |
| No | 19.7 | 23.1 | ||
| Renal disease | ||||
| Yes | 30.3 | <0.001 | 28.6 | <0.001 |
| No | 17.6 | 22.0 | ||
| In-hospital treatment | ||||
| PCI | ||||
| Yes | 13.4 | <0.001 | 17.7 | 0.004 |
| No | 28.8 | 23.5 | ||
| Intensive care unit use | ||||
| Yes | 19.9 | 0.751 | 26.3 | <0.001 |
| No | 20.4 | 22.5 | ||
| Surgery use | ||||
| Yes | 27.4 | <0.001 | 26.5 | 0.069 |
| No | 19.2 | 23.2 | ||
| Length of stay (d) | ||||
| <5 | 14.4 | <0.001 | 19.7 | <0.001 |
| 6–9 | 18.8 | 22.7 | ||
| 10+ | 28.9 | 29.9 | ||
| Baseline medications | ||||
| Aspirin | ||||
| Yes | 19.5 | 0.005 | 22.5 | 0.028 |
| No | 26.2 | 24.1 | ||
| β-Blocker | ||||
| Yes | 19.2 | 0.074 | 21.5 | <0.001 |
| No | 21.3 | 24.5 | ||
| Statin | ||||
| Yes | 17.8 | <0.001 | 21.5 | 0.020 |
| No | 23.0 | 23.7 | ||
| ACEI/ARB | ||||
| Yes | 18.9 | 0.003 | 21.8 | <0.001 |
| No | 22.6 | 25.6 | ||
| Medications within 7 days of discharge | ||||
| Aspirin | ||||
| Yes | 14.4 | <0.001 | 19.4 | <0.001 |
| No | 25.8 | 24.8 | ||
| β-Blocker | ||||
| Yes | 15.1 | <0.001 | 18.1 | <0.001 |
| No | 22.7 | 25.0 | ||
| Statin | ||||
| Yes | 13.8 | <0.001 | 17.0 | <0.001 |
| No | 23.0 | 24.0 | ||
| ACEI/ARB | ||||
| Yes | 15.1 | <0.001 | 17.1 | <0.001 |
| No | 22.6 | 26.2 | ||
| Medications within 14 days of discharge | ||||
| Aspirin | ||||
| Yes | 14.6 | <0.001 | 19.3 | <0.001 |
| No | 31.5 | 25.4 | ||
| β-Blocker | ||||
| Yes | 15.3 | <0.001 | 18.1 | <0.001 |
| No | 24.4 | 25.8 | ||
| Statin | ||||
| Yes | 13.8 | <0.001 | 17.6 | <0.001 |
| No | 25.0 | 24.2 | ||
| ACEI/ARB | ||||
| Yes | 14.6 | <0.001 | 17.0 | <0.001 |
| No | 24.9 | 27.8 | ||
| Low income | ||||
| Yes | 32.7 | 0.001 | 27.9 | 0.059 |
| No | 19.7 | 23.2 | ||
| Rural residence | ||||
| Yes | 21.2 | 0.219 | 23.4 | 0.876 |
| No | 19.5 | 23.3 | ||
| Number of hospitalizations during the past year | ||||
| 0 | 15.5 | <0.001 | 18.2 | <0.001 |
| 1 | 26.0 | 23.4 | ||
| 2+ | 32.0 | 34.0 | ||
| Number of outpatient visits during the past year | ||||
| Low | 14.8 | <0.001 | 20.3 | <0.001 |
| Medium | 19.7 | 23.3 | ||
| High | 25.4 | 26.5 | ||
| Hospital Characteristics | ||||
| Hospital volume | ||||
| Low | 21.2 | 0.041 | 25.5 | <0.001 |
| Medium | 20.6 | 23.4 | ||
| High | 17.9 | 21.0 | ||
| Hospital level | ||||
| Academic medical center | 18.0 | <0.001 | 20.0 | <0.001 |
| Regional | 22.0 | 24.3 | ||
| District | 28.4 | 27.6 | ||
| Teaching | ||||
| Yes | 19.7 | 0.001 | 22.9 | <0.001 |
| No | 36.2 | 26.9 | ||
| Location | ||||
| Taipei | 18.1 | 0.127 | 22.1 | 0.134 |
| Northern | 19.1 | 23.1 | ||
| Central | 20.3 | 24.1 | ||
| Southern | 22.1 | 25.1 | ||
| Kao-Ping | 21.1 | 23.7 | ||
| Eastern | 23.3 | 23.6 | ||
NSTEMI indicates non-ST-segment-elevation myocardial infarction; and PCI, percutaneous coronary intervention.
The results of the series of Cox proportional hazard models with robust sandwich variance estimates and propensity score weighting as provided in Table 4 demonstrate the associations between early follow-up and 30-day readmission, after adjustment for patient and hospital characteristics. In model 1, early physician follow-up was associated with a lower hazard ratio of all-cause readmission compared with no early physician follow-up for patients with NSTEMI (hazard ratio [HR], 0.47; 95% confidence interval [CI], 0.39–0.57), and for patients with heart failure (HR, 0.54; 95% CI, 0.48–0.60). Early physician follow-up was also associated with lower 30-day cardiovascular-cause and same-cause readmission.
Table 4. Adjusted relationships between early physician follow-up and 30-day readmission.
| All-cause | Cardiovascular-cause | Same-cause | ||||
|---|---|---|---|---|---|---|
| HR | (95% CI) | HR | (95% CI) | HR | (95% CI) | |
| NSTEMI | ||||||
| Model 1: early physician follow-upa | N = 5008 | |||||
| Yes (ref: No) | 0.47 | (0.39–0.57) | 0.48 | (0.40–0.57) | 0.59 | (0.41–0.86) |
| Model 2: early physician follow-upb | N = 3841 | |||||
| Same physician follow-up (ref: No) | 0.56 | (0.48–0.65) | 0.56 | (0.47–0.66) | 0.62 | (0.38–0.99) |
| Cardiologist follow-up (ref: No) | 0.97 | (0.81–1.16) | 1.03 | (0.86–1.24) | 0.81 | (0.54–1.23) |
| Model 3: 14-Day physician follow-upa | N = 5008 | |||||
| Yes (ref: No) | 0.18 | (0.14–0.24) | 0.20 | (0.15–0.26) | 0.26 | (0.17–0.39) |
| Model 4: 14-Day physician follow-upb | N = 4664 | |||||
| Same physician follow-up (ref: No) | 0.53 | (0.44–0.62) | 0.51 | (0.43–0.61) | 0.59 | (0.39–0.92) |
| Cardiologist follow-up (ref: No) | 0.85 | (0.73–1.00) | 0.89 | (0.76–1.05) | 0.85 | (0.58–1.24) |
| Heart failure | ||||||
| Model 1: early physician follow-upa | N = 13577 | |||||
| Yes (ref: No) | 0.54 | (0.48–0.60) | 0.57 | (0.51–0.64) | 0.59 | (0.52–0.66) |
| Model 2: early physician follow-upb | N = 10164 | |||||
| Same physician follow-up (ref: No) | 0.69 | (0.62–0.76) | 0.69 | (0.62–0.76) | 0.77 | (0.68–0.87) |
| Cardiologist follow-up (ref: No) | 0.94 | (0.85–1.04) | 0.99 | (0.90–1.10) | 1.03 | (0.91–1.17) |
| Model 3: 14-Day physician follow-upa | N = 13577 | |||||
| Yes (ref: No) | 0.28 | (0.25–0.32) | 0.31 | (0.27–0.34) | 0.32 | (0.28–0.36) |
| Model 4: 14-Day physician follow-upb | N = 12197 | |||||
| Same physician follow-up (ref: No) | 0.63 | (0.58–0.68) | 0.64 | (0.59–0.70) | 0.71 | (0.64–0.80) |
| Cardiologist follow-up (ref: No) | 0.94 | (0.86–1.03) | 1.00 | (0.91–1.09) | 1.05 | (0.94–1.18) |
CI indicates confidence interval; HR, hazard ratio; NSTEMI, non-ST-segment-elevation myocardial infarction; and PCI, percutaneous coronary intervention.
aModels included sex, age, comorbid conditions, medical history, in-hospital treatment, length of stay, baseline medications, low income, rural residence, number of hospitalizations during the past year, number of office visits during the past year, hospital volume, level, teaching status, and location, and were weighted by the inverse of a propensity score
bModels included sex, age, comorbid conditions, medical history, in-hospital treatment, length of stay, baseline medications, medications within 7(14) days of discharge, low income, rural residence, number of hospitalizations during the past year, number of office visits during the past year, hospital volume, level, teaching status, and location.
To further determine the individual and combined associations of same physician and cardiologist follow-up with 30-day readmission among patients with early follow-up, we did not find the synergistic associations between the effects of same physician and cardiologist follow-up. Therefore, an interaction term between same physician and cardiologist follow-up was removed in model 2. Same physician follow-up was associated with a lower hazard ratio of all-cause readmission compared with different physician follow-up for patients with NSTEMI (HR, 0.56; 95% CI, 0.48–0.65), and for patients with heart failure (HR, 0.69; 95% CI, 0.62–0.76). Same physician follow-up was also associated with lower 30-day cardiovascular-cause and same-cause readmission. The robustness of our primary results were evaluated by sensitivity analysis. Results were similar when we changed the transitional period from 7 days to 14 days.
Discussion
This study was the first research using nationwide population-based data to examine the association between early physician follow-up and 30-day readmission, and the relative association of early same physician and early cardiologist follow-up with 30-day readmission for NSTEMI and heart failure. For each condition, we found that early physician follow-up was associated with decreased 30-day readmission compared with no early physician follow-up. Moreover, early follow-up with the same physician was associated with lower 30-day readmission compared with early follow-up with a different physician.
In Taiwan, about 75% percent of hospitalized patients with NSTEMI and heart failure had an outpatient visit within 7 days of discharge. Most early follow-up care was handled by the same physician who treated the patient during the index hospitalization, and usually by cardiologists. The rates of early physician, early same physician and early cardiologist follow-up in Taiwan were higher than those in the United States (38.3%, 18.1%, and 7.5%, respectively, for heart failure).[3] These results are because all hospitals in Taiwan are closed systems and are reimbursed for both inpatient and outpatient services on a fee-for-service basis by the National Health Insurance Administration (NHIA). Thus, physicians only employed by hospitals can be allowed to treat inpatients, and hospitals also use variable pay to encourage staff physicians to provide inpatient and outpatient services. Moreover, clinical guidelines recommend early physician follow-up. Therefore, most hospital physicians not only prescribe a week's supply of medicine at discharge, but also schedule a follow-up appointment within 7 days of discharge.
This study had two major findings about the association between early physician follow-up and 30-day readmission for NSTEMI and heart failure. First, we found that early follow-up with any physician was associated with lower 30-day readmission for each condition. This result is consistent with the finding of Hernandez et al.[3] Hernandez et al verified the association between hospital-level early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. However, the aggregate group-level (hospital-level) variable may be tapping into a different construct than its individual-level (patient-level) namesake.[41–43] Thus, the limitations of using an aggregate measure as a proxy for its individual-level namesake relate not only to measurement errors but also to construct validity, that is, whether it is indeed the same construct that is measured by both variables.[41, 43, 44]
It also must be noted that at the patient level, the association between time from hospital discharge to outpatient follow-up with a physician and risk of readmission is confounded by severity of illness. Patients who have more severe acute myocardial infarction or heart failure, or who are medically less stable are not only commonly seen sooner after hospital discharge but also at a greater risk of readmission.[3, 4] Therefore, we used a propensity score approach to correct for the selection bias. The use of a propensity score method can help reduce the selection bias and provide more valid analysis results. This study may support current clinical guidelines advocating for patients with heart failure or NSTEMI who have been discharged from hospital to receive early or timely outpatient follow-up with a physician for further assessment or treatment.[5, 7]
Another notable finding was that early same physician follow-up (physician continuity) was associated with a further reduction in 30-day readmission. This finding is consistent with that of van Walraven et al[23] and of McAlister et al.[19] In Ontario, Canada, Walraven et al found that 30-day follow-up with the same physician, rather than with another physician, was associated with reduced 30-day post-discharge mortality or non-elective readmission for non-elective medical or surgical conditions. In Alberta, Canada, McAlister et al found that 30-day follow-up with a familiar physician was associated with lower 3-month post-discharge mortality or urgent readmission for heart failure compared with no follow-up. Although at discharge disease progression is improved, remission is not achieved. Because of early follow-up with a different physician, if the physician does not know a particular patient’s disease progression, their progression could possibly be interpreted as a deterioration requiring readmission.[23] Moreover, early same physician follow-up is more likely to early determine therapeutic effectiveness and early identify complications of hospital therapies or procedures due to familiarity with the hospital course. Early evaluation and treatment could avoid more serious subsequent problems leading to readmission.
Some limitations existed in this study. First of all, patients were not assigned randomly. This is an observational and retrospective study; therefore, we cannot assign study subjects randomly. The propensity score weighting was adopted for alleviating selection bias.[25, 37–40] Moreover, although, like other studies using administrative databases, no information on disease severity was available for risk adjustment, we adjusted for patient age, comorbid conditions, intensive care unit use, and surgical operation, which are also important for the adjustment of disease complexity.[9, 19, 23–26] However, we cannot completely exclude the possibility of unmeasured confounders such as behavioral risk factors. Differences in outcomes between follow-up and non-follow-up groups may be confounded by unmeasured behavioral risk factors that may influence access to care. Second, this study defined early follow-up as an outpatient visit that occurred within 7 days of discharge. The 7-day window has previously been discussed and was chosen according to historical precedent and clinical plausibility.[3, 4] However, we also did a sensitivity analysis examining the association between 14-day follow-up and 30-day readmission.
Finally, in Taiwan, follow-up with a trained and specialized nurse (care manager) is not common until now. This may be because the service is not reimbursed by the NHIA. Based on two related studies, one study regarding discharged patient with heart failure in Northern California, United States finds that early outpatient follow-up with a physician is associated with a lower chance of 30-day readmission, but telephone follow-up with a trained and specialized nurse or pharmacist is not.[45] Another study regarding ambulatory patients with heart failure in the Apulia Region of Italy finds that the introduction of care managers into the primary health care system has the potential of reducing readmissions because of the strong partnership between the care manager and the patient and the collaboration between the physician and the care manager.[46] Future research needs to examine whether the effect of early follow-up visit with a care manager is the same as that with a physician among discharged patients with heart failure or acute myocardial infarction.
Conclusion
Our national population-based study showed that 7-day physician follow-up was associated with lower 30-day readmission, and physician continuity (7-day same physician follow-up) was associated with much lower 30-day readmission for patients with NSTEMI and those with heart failure. This study may provide evidence in support of guidelines recommending scheduling an early follow-up visit after discharge, and it may provide an evidenced-based approach to improve 30-day readmission following NSTEMI and heart failure.
Acknowledgments
The study was supported by grants from the Ministry of Science and Technology (MOST 103-2410-H-002-209-MY2 and MOST 105-2410-H-002-220-MY2) in Taiwan, and was based in part on data from the National Health Insurance Research Database provided by the National Health Insurance Administration, Ministry of Health and Welfare and managed by National Health Research Institutes. The interpretation and conclusions contained herein do not represent those of National Health Insurance Administration, Ministry of Health and Welfare and National Health Research Institutes.
Data Availability
The dataset used in this study is held by the Taiwan Ministry of Health and Welfare (MOHW). The Ministry of Health and Welfare must approved our application to access this data. Any researcher interested in accessing this dataset can submit an application form to the Ministry of Health and Welfare requesting access. Please contact the staff of MOHW (Email: stcarolwu@mohw.gov.tw) for further assistance. Taiwan Ministry of Health and Welfare Address: No.488, Sec. 6, Zhongxiao E. Rd., Nangang Dist., Taipei City 115, Taiwan (R.O.C.). Phone: +886-2-8590-6848.
Funding Statement
Taiwan Ministry of Science and Technology provides the financial support (MOST 103-2410-H-002-209-MY2 and MOST 105-2410-H-002-220-MY2). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Centers for Medicare and Medicaid Services. Outcome measures 2015 [December 10, 2015]. http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/OutcomeMeasures.html.
- 2.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–28. 10.1056/NEJMsa0803563 [DOI] [PubMed] [Google Scholar]
- 3.Hernandez AF, Greiner MA, Fonarow GC, Hammill BG, Heidenreich PA, Yancy CW, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303(17):1716–22. 10.1001/jama.2010.533 [DOI] [PubMed] [Google Scholar]
- 4.Hess CN, Shah BR, Peng SA, Thomas L, Roe MT, Peterson ED. Association of early physician follow-up and 30-day readmission after non-ST-segment-elevation myocardial infarction among older patients. Circulation. 2013;128(11):1206–13. 10.1161/CIRCULATIONAHA.113.004569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;128(16):e240–e327. 10.1161/CIR.0b013e31829e8776 [DOI] [PubMed] [Google Scholar]
- 6.O’Gara PT, Kushner FG, Ascheim DD, Casey DE, Chung MK, de Lemos JA, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127(4):529–55. 10.1161/CIR.0b013e3182742c84 [DOI] [PubMed] [Google Scholar]
- 7.Amsterdam EA, Wenger NK, Brindis RG, Casey JDE, Ganiats TG, Holmes JDR, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;64(24):e139–e228. 10.1016/j.jacc.2014.09.017 [DOI] [PubMed] [Google Scholar]
- 8.Coleman EA, Williams MV. Executing high-quality care transitions: a call to do it right. J Hosp Med. 2007;2(5):287–90. 10.1002/jhm.276 [DOI] [PubMed] [Google Scholar]
- 9.Field TS, Ogarek J, Garber L, Reed G, Gurwitz JH. Association of early post-discharge follow-up by a primary care physician and 30-day rehospitalization among older adults. J Gen Intern Med. 2015;30(5):565–71. 10.1007/s11606-014-3106-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krumholz HM. Post-hospital syndrome--an acquired, transient condition of generalized risk. N Engl J Med. 2013;368(2):100–2. 10.1056/NEJMp1212324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leendertse AJ, Egberts AC, Stoker LJ, van den Bemt PM, Group HS. Frequency of and risk factors for preventable medication-related hospital admissions in the Netherlands. Arch Intern Med. 2008;168(17):1890–6. 10.1001/archinternmed.2008.3 [DOI] [PubMed] [Google Scholar]
- 12.Ryan J, Kang S, Dolacky S, Ingrassia J, Ganeshan R. Change in readmissions and follow-up visits as part of a heart failure readmission quality improvement initiative. Am J Med. 2013;126(11):989–94 e1. 10.1016/j.amjmed.2013.06.027 [DOI] [PubMed] [Google Scholar]
- 13.Centers for Medicare and Medicaid Services. Readmissions Reduction Program 2012 [August 15, 2014]. http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html.
- 14.Glickman SW, Shofer FS, Wu MC, Scholer MJ, Ndubuizu A, Peterson ED, et al. Development and validation of a prioritization rule for obtaining an immediate 12-lead electrocardiogram in the emergency department to identify ST-elevation myocardial infarction. Am Heart J. 2012;163(3):372–82. Epub 2012/03/20. 10.1016/j.ahj.2011.10.021 [DOI] [PubMed] [Google Scholar]
- 15.Andersson C, Shilane D, Go AS, Chang TI, Kazi D, Solomon MD, et al. beta-blocker therapy and cardiac events among patients with newly diagnosed coronary heart disease. J Am Coll Cardiol. 2014;64(3):247–52. Epub 2014/07/19. 10.1016/j.jacc.2014.04.042 [DOI] [PubMed] [Google Scholar]
- 16.Tung YC, Chang GM, Chien KL, Tu YK. The relationships among physician and hospital volume, processes, and outcomes of care for acute myocardial infarction. Med Care. 2014;52(6):519–27. 10.1097/MLR.0000000000000132 [DOI] [PubMed] [Google Scholar]
- 17.Ezekowitz JA, van Walraven C, McAlister FA, Armstrong PW, Kaul P. Impact of specialist follow-up in outpatients with congestive heart failure. CMAJ. 2005;172(2):189–94. 10.1503/cmaj.1032017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yeung DF, Boom NK, Guo H, Lee DS, Schultz SE, Tu JV. Trends in the incidence and outcomes of heart failure in Ontario, Canada: 1997 to 2007. CMAJ. 2012;184(14):E765–73. 10.1503/cmaj.111958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McAlister FA, Youngson E, Bakal JA, Kaul P, Ezekowitz J, van Walraven C. Impact of physician continuity on death or urgent readmission after discharge among patients with heart failure. CMAJ. 2013;185(14):E681–9. 10.1503/cmaj.130048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chiu HY, Cheng SH, Tung YC. Associations of continuity and level with outcomes and expenses of post-discharge care for patients with heart failure. Taiwan J Public Health. 2016;35(1):66–79. [Google Scholar]
- 21.Krumholz HM, Lin Z, Keenan PS, Chen J, Ross JS, Drye EE, et al. Relationship between hospital readmission and mortality rates for patients hospitalized with acute myocardial infarction, heart failure, or pneumonia. JAMA. 2013;309(6):587–93. 10.1001/jama.2013.333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.American College of Cardiology. Hospital to Home (H2H): American College of Cardiology; 2007 [July 8, 2015]. http://h2hquality.org/.
- 23.van Walraven C, Mamdani M, Fang J, Austin PC. Continuity of care and patient outcomes after hospital discharge. J Gen Intern Med. 2004;19(6):624–31. Epub 2004/06/24. 10.1111/j.1525-1497.2004.30082.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Krumholz HM, Merrill AR, Schone EM, Schreiner GC, Chen J, Bradley EH, et al. Patterns of hospital performance in acute myocardial infarction and heart failure 30-day mortality and readmission. Circ Cardiovasc Qual Outcomes. 2009;2(5):407–13. Epub 2009/12/25. 10.1161/CIRCOUTCOMES.109.883256 [DOI] [PubMed] [Google Scholar]
- 25.Tung YC, Chang GM, Chen YH. Associations of physician volume and weekend admissions with ischemic stroke outcome in Taiwan: a nationwide population-based study. Med Care. 2009;47(9):1018–25. 10.1097/MLR.0b013e3181a81144 [DOI] [PubMed] [Google Scholar]
- 26.Tung YC, Chang GM, Cheng SH. Long-term effect of fee-for-service-based reimbursement cuts on processes and outcomes of care for stroke: interrupted time-series study from Taiwan. Circ Cardiovasc Qual Outcomes. 2015;8(1):30–7. 10.1161/CIRCOUTCOMES.114.001086 [DOI] [PubMed] [Google Scholar]
- 27.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–9. [DOI] [PubMed] [Google Scholar]
- 28.Czarnecki A, Chong A, Lee DS, Schull MJ, Tu JV, Lau C, et al. Association between physician follow-up and outcomes of care after chest pain assessment in high-risk patients. Circulation. 2013;127(13):1386–94. 10.1161/CIRCULATIONAHA.112.000737 [DOI] [PubMed] [Google Scholar]
- 29.Liu CY, Hung YT, Chuang YL, Chen YJ, Weng WS, Liu JS, et al. A stratification study on the urbanization of Taiwan. Journal of Health Management. 2006;4(1):1–22. [Google Scholar]
- 30.Lin YH, Chen YC, Tseng YH, Lin MH, Hwang SJ, Chen TJ, et al. Trend of urban-rural disparities in hospice utilization in Taiwan. PLoS One. 2013;8(4):e62492 Epub 2013/05/10. 10.1371/journal.pone.0062492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chang HY, Bodycombe DP, Huang WF, Weiner JP. Risk-adjusted resource allocation: using Taiwan's National Health Insurance as an example. Asia Pac J Public Health. 2015;27(2):Np958–71. Epub 2013/01/25. 10.1177/1010539512471073 [DOI] [PubMed] [Google Scholar]
- 32.Yu TH, Hou YC, Tung YC, Chung KP. Why do outcomes of CABG care vary between urban and rural areas in Taiwan? A perspective from quality of care. Int J Qual Health Care. 2015;27(5):361–8. Epub 2015/08/05. 10.1093/intqhc/mzv050 [DOI] [PubMed] [Google Scholar]
- 33.Institute of Medicine. Rewarding Provider Performance: Aligning Incentives in Medicare. Washington, DC: National Academies Press; 2007. [Google Scholar]
- 34.Medicare Payment Advisory Commission. Promoting greater efficiency in Medicare, report to the Congress New Jersey (NW): MEDPAC; 2007 [cited 2013 17 July]. http://www.medpac.gov/documents/Jun07_EntireReport.pdf.
- 35.Zhang Y, Kaplan CM, Baik SH, Chang CC, Lave JR. Medication adherence and readmission after myocardial infarction in the Medicare population. Am J Manag Care. 2014;20(11):e498–505. [PMC free article] [PubMed] [Google Scholar]
- 36.Czarnecki A, Wang JT, Tu JV, Lee DS, Schull MJ, Lau C, et al. The role of primary care physician and cardiologist follow-up for low-risk patients with chest pain after emergency department assessment. Am Heart J. 2014;168(3):289–95. 10.1016/j.ahj.2014.05.016 [DOI] [PubMed] [Google Scholar]
- 37.Hirano K, Imbens GW, Ridder G. Efficient estimation of average treatment effects using the estimated propensity score. Econometrica. 2003;71(4):1161–89. [Google Scholar]
- 38.Huang IC, Frangakis C, Dominici F, Diette GB, Wu AW. Application of a propensity score approach for risk adjustment in profiling multiple physician groups on asthma care. Health Serv Res. 2005;40(1):253–78. 10.1111/j.1475-6773.2005.00352.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yang G, Stemkovski S, Saunders WB. A review of propensity score application in healthcare outcome and epidemiology Denver2007 [Feb 18, 2015]. http://www.lexjansen.com/pharmasug/2007/pr/pr02.pdf.
- 40.Chang HY, Zhou M, Tang W, Alexander GC, Singh S. Risk of gastrointestinal bleeding associated with oral anticoagulants: population based retrospective cohort study. Bmj. 2015;350:h1585 10.1136/bmj.h1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schwartz S. The fallacy of the ecological fallacy: the potential misuse of a concept and the consequences. Am J Public Health. 1994;84(5):819–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Susser M. The logic in ecological: I. The logic of analysis. Am J Public Health. 1994;84(5):825–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Diez Roux AV. The study of group-level factors in epidemiology: rethinking variables, study designs, and analytical approaches. Epidemiol Rev. 2004;26(1):104–11. [DOI] [PubMed] [Google Scholar]
- 44.Geronimus AT, Bound J, Neidert LJ. On the validity of using census geocode characteristics to proxy individual socioeconomic characteristics. J Am Stat Assoc. 1996;91(434):529–37. [Google Scholar]
- 45.Lee KK, Yang J, Hernandez AF, Steimle AE, Go AS. Post-discharge follow-up characteristics associated with 30-day readmission after heart failure hospitalization. Med Care. 2016;54(4):365–72. 10.1097/MLR.0000000000000492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ciccone MM, Aquilino A, Cortese F, Scicchitano P, Sassara M, Mola E, et al. Feasibility and effectiveness of a disease and care management model in the primary health care system for patients with heart failure and diabetes (Project Leonardo). Vascular health and risk management. 2010;6:297–305. Epub 2010/05/19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset used in this study is held by the Taiwan Ministry of Health and Welfare (MOHW). The Ministry of Health and Welfare must approved our application to access this data. Any researcher interested in accessing this dataset can submit an application form to the Ministry of Health and Welfare requesting access. Please contact the staff of MOHW (Email: stcarolwu@mohw.gov.tw) for further assistance. Taiwan Ministry of Health and Welfare Address: No.488, Sec. 6, Zhongxiao E. Rd., Nangang Dist., Taipei City 115, Taiwan (R.O.C.). Phone: +886-2-8590-6848.