Abstract
Objective:
To investigate whether the progressive recuperation of consciousness was associated with the reconsolidation of sleep and wake states in hospitalized patients with acute traumatic brain injury (TBI).
Methods:
This study comprised 30 hospitalized patients (age 29.1 ± 13.5 years) in the acute phase of moderate or severe TBI. Testing started 21.0 ± 13.7 days postinjury. Consciousness level and cognitive functioning were assessed daily with the Rancho Los Amigos scale of cognitive functioning (RLA). Sleep and wake cycle characteristics were estimated with continuous wrist actigraphy. Mixed model analyses were performed on 233 days with the RLA (fixed effect) and sleep-wake variables (random effects). Linear contrast analyses were performed in order to verify if consolidation of the sleep and wake states improved linearly with increasing RLA score.
Results:
Associations were found between scores on the consciousness/cognitive functioning scale and measures of sleep-wake cycle consolidation (p < 0.001), nighttime sleep duration (p = 0.018), and nighttime fragmentation index (p < 0.001). These associations showed strong linear relationships (p < 0.01 for all), revealing that consciousness and cognition improved in parallel with sleep-wake quality. Consolidated 24-hour sleep-wake cycle occurred when patients were able to give context-appropriate, goal-directed responses.
Conclusions:
Our results showed that when the brain has not sufficiently recovered a certain level of consciousness, it is also unable to generate a 24-hour sleep-wake cycle and consolidated nighttime sleep. This study contributes to elucidating the pathophysiology of severe sleep-wake cycle alterations in the acute phase of moderate to severe TBI.
Nonsedated patients in the acute stage of a moderate to severe traumatic brain injury (TBI) have serious alterations of their sleep-wake cycle,1,2 characterized by short sleep and wake bouts, a few minutes in length, dispersed over 24 hours.1 Pain, medication, and the hospital environment are possible causes of these sleep-wake disturbances.3 However, recent experimental models of TBI have shown that the injured brain itself has a direct effect on the sleep-wake cycle by increasing fragmentation of sleep and wake periods.4–6
In patients with acute TBI, the reconsolidation of the 24-hour sleep-wake cycle predicts emergence from posttraumatic amnesia at hospital discharge1 as well as cognitive impairment in rehabilitation settings.7,8 Studies on chronic disorders of consciousness also suggest that the circadian variation of the sleep-wake cycle reemerges with improving consciousness.9 Overall, these observations point to an intrinsic association between recovery of the sleep-wake cycle, consciousness, and cognition following a brain injury. However, we have yet to characterize how the sleep-wake cycle recovers on a day-to-day basis in relation to improving consciousness and higher cognitive functions in acute TBI.
The objective of this study was to verify whether an association exists between the evolution of the sleep-wake cycle and the recovery of consciousness and cognition in acute moderate to severe TBI. A second objective was to determine which improved first, or whether they evolved synchronously. We predicted that the consolidation of sleep-wake states would increase synchronously with improving consciousness and cognition, because they depend on overall brain integrity.
METHODS
Patients.
We recruited patients from Hôpital du Sacré-Coeur de Montréal, a level 1 trauma center affiliated with the Université de Montréal, between January 2010 and May 2015. We defined TBI as an alteration in brain function or other evidence of brain pathology caused by an external force,10 and assessed TBI severity upon emergency room admission, prior to intubation, using the Glasgow Coma Scale (GCS).11 We included patients if they were hospitalized in the intensive care unit (ICU) for their TBI. In order to characterize our study sample, we documented the following for all patients: mechanism of injury, GCS score at emergency room admission, ICU and hospital lengths of stay, number of days with elevated intracranial pressure (>20 mm Hg), Marshall and Rotterdam scores,12,13 which are qualitative CT classification systems, Disability Rating Scale score within 72 hours of hospital discharge,14 and patient orientation at hospital discharge. We obtained written informed consent for study participation from patients' families and the hospital ethical standards committee on human experimentation approved the study. We excluded patients if they were younger than 16 or older than 65 years; were quadriplegic; had a history of substance abuse, psychiatric, or neurologic disorders; had a diagnosed sleep disorder prior to injury; had any damage to the eyes or the optic nerve (modifying light perception); or had a history of prior TBI or concussion.
Experimental design.
During the ICU and post-ICU hospital stay, patients wore an activity monitor to assess their sleep-wake patterns continuously for several days, during which a daily assessment of consciousness and cognition was also carried out.
Assessment of consciousness and cognitive level.
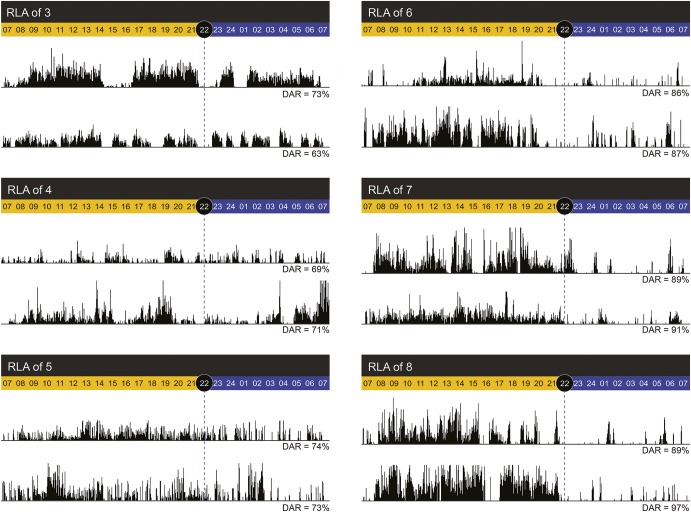
We used the Rancho Los Amigos scale of cognitive functioning (RLA),15 a comprehensive behavioral rating scale developed specifically to monitor the stages of recovery in the adult TBI population,16 which can be easily administered at bedside. The RLA evaluates key features of consciousness and cognitive functioning, such as level of awareness of the environment, response to stimuli, ability to follow command, confusion, attention, and the appropriateness of verbalization and motor actions. The RLA scale consists of 8 hierarchical levels, with level 1 representing no response and level 8 representing purposeful and appropriate cognitive function (table 1). Duration of RLA assessment ranges from 5 to 40 minutes and is carried out when patients are fully awake and all aspects of the scale are assessable. Trained occupational therapists with experience with the acute TBI population assessed the RLA scale daily on weekdays.
Table 1.
Rancho Los Amigos scale of cognitive functioning (RLA), including the number of days and patients representing each RLA score
Sleep-wake assessments.
Patients wore a wrist actigraph (Actiwatch-L or Actiwatch-Spectrum; Philips Healthcare, Andover, MA) on a nonparalyzed arm starting in the ICU and continuing throughout hospitalization in regular wards. As described in a previous study,1 actigraphy recording began when continuous sedation and analgesia had ceased for at least 24 hours, and once patients reached a RLA score ≥3, indicative of a more apparent physical reactivity to internal and external stimuli. With its low invasiveness, actigraphy enables the long-term measurement of the rest-activity cycle, and is recognized as a proxy measure of the sleep-wake cycle.17
We measured activity counts per 1-minute epoch and derived 3 variables from actigraphic recordings to estimate sleep-wake quality:
Daytime activity ratio (DAR).
We estimated consolidation of the 24-hour sleep-wake cycle with the DAR.1 The DAR represents the percentage of total 24-hour activity occurring in the daytime ([daytime activity/24-hour activity] × 100). A high DAR reflects a more consolidated sleep-wake cycle, with a high concentration of activity (wake) during the day (7:00–21:59 hours) and rest (sleep) during the night (22:00–6:59 hours). A DAR ≥80% represents a consolidated 24-hour sleep-wake cycle.1
Nighttime sleep duration.
Given that sleep diaries could not be used, we defined nighttime as the period when light and noise were minimized in the hospital, which was from 22:00 to 06:59 hours. We estimated sleep duration based on periods of inactivity, using the designated actigraphy software (Actiware 5.0) with a medium wake threshold (40 activity counts per minute). The total of 1-minute epochs scored as sleep between 22:00 and 06:59 hours defined nighttime sleep duration.
Nighttime fragmentation index.
The dedicated software also computes a nighttime fragmentation index, which is an index of restlessness that reflects the frequency of changes between mobility and immobility, and is correlated to the arousal index, as measured by polysomnography.18,19 This fragmentation index corresponds to the summed percentage of mobile bouts and immobile bouts of 1 minute for the given interval, divided by the total number of immobile bouts of >1 minute ([% mobile bouts of 1 minute + % immobile bouts of 1 minute]/no. immobile bouts >1 minute). A mobile bout is a 1-minute epoch with ≥4 activity counts.
Statistical analyses.
In order to assess the relationship between consciousness/cognition and consolidation of sleep and wake states on a day-to-day basis, we integrated the RLA score into linear mixed model analyses with DAR, nighttime sleep duration, and fragmentation index, using alternatively autoregressive (AR1) and compound symmetry (CS) covariance structures. The CS structure assumes that variance and covariance of observations of a single patient are homogenous, while the AR1 structure posits that covariance between observations on the same patient comes from the exponential decrease in covariance between observations as they get farther apart in time.20 We entered the RLA as the fixed effect and the DAR, nighttime sleep duration, and fragmentation index as random effects (each in a separate analysis).
In order to verify if consolidation of the sleep and wake states improve linearly with increasing RLA score, we performed linear contrast analyses within the mixed model analyses for the 3 variables (DAR, nighttime sleep duration, fragmentation index).
Finally, we performed cross-correlation analyses, which enable the identification of the best-fit lag, in order to determine whether sleep parameters or consciousness and cognitive recovery improved first, or whether they evolved synchronously. We averaged the RLA score and actigraphy variables per day over 10 days, and performed cross-correlation analyses between RLA score and each actigraphy variable separately, with a maximum lag of 3 days (30%), to minimize bias.21
We set statistical significance at p < 0.01 and report only results from the best fitting mixed model, based on the smallest Akaike information criterion.
Control for potentially confounding variables.
To ensure that our 4 variables of interest (i.e., RLA, DAR, nighttime sleep duration, and nighttime fragmentation index) were not indirect measures of time since ICU discharge, and were not influenced by the cumulative dose of sedatives and analgesics received in the ICU, we submitted these variables to Pearson correlations. We found no association (r < 0.45, NS for all). RLA and our 3 sleep-wake variables were therefore not indirect measures of the passage of time and the natural improvement of patients' overall condition, nor were they influenced by the quantity of sedatives and analgesics received during the patients' ICU stay.
To ensure that reactivity to internal/external stimuli (RLA score) was not simply an indirect measure of daytime sleep duration, we evaluated the association between RLA and duration of daytime sleep using a Pearson correlation and found no association (r = 0.06, p = 0.35).
Finally, we verified if time of morning increase in lighting (≥10 lux) measured through the Actiwatch differed according to RLA score, and no association was found (r = 0.105, p = 0.122).
RESULTS
Patient characteristics.
We recruited the 30 consecutive patients who fitted our inclusion criteria, were hospitalized sufficiently long to participate in the study, and provided consent for participation. Patients were 29.1 ± 13.5 years old (range 17–58 years; 22 men) and the average GCS score at admission was 7.7 ± 3.6 (range 3–14). Two patients had a GCS score of 14 and 1 had a GCS of 13 at admission, but received a diagnosis of moderate or severe TBI by the neurosurgeon given that they had decompressive craniectomy. Mechanisms of injury were motor vehicle accident (n = 20), fall (n = 7), recreational/sports injury (n = 2), and blow to the head (n = 1). Patients had an average ICU stay of 22.9 ± 14.2 days and a hospital length of stay of 44.6 ± 21.2 days. Fifteen patients (50%) had elevated intracranial pressure during their ICU stay of an average duration of 10.4 ± 4.6 days. Twenty-eight (93.3%) patients had evidence of traumatic injuries on their initial brain CT scans, and average Marshall and Rotterdam scores were 2.9 ± 1.4 (range 1–5) and 3.3 ± 1.3 (range 2–6), respectively. Average score on the Disability Rating Scale was 10.2 ± 4.4 prior to hospital discharge, corresponding to moderate to severe deficits. Overall, 23 patients (76.7%) were transferred to an inpatient rehabilitation center.
Association between level of consciousness/cognition and sleep-wake patterns.
Patients wore the actigraph for 11.3 ± 4.1 days, starting 21.0 ± 13.7 days postinjury (in the ICU for 60% of the patients). Overall, there were 233 days of both actigraphy recording and RLA assessment.
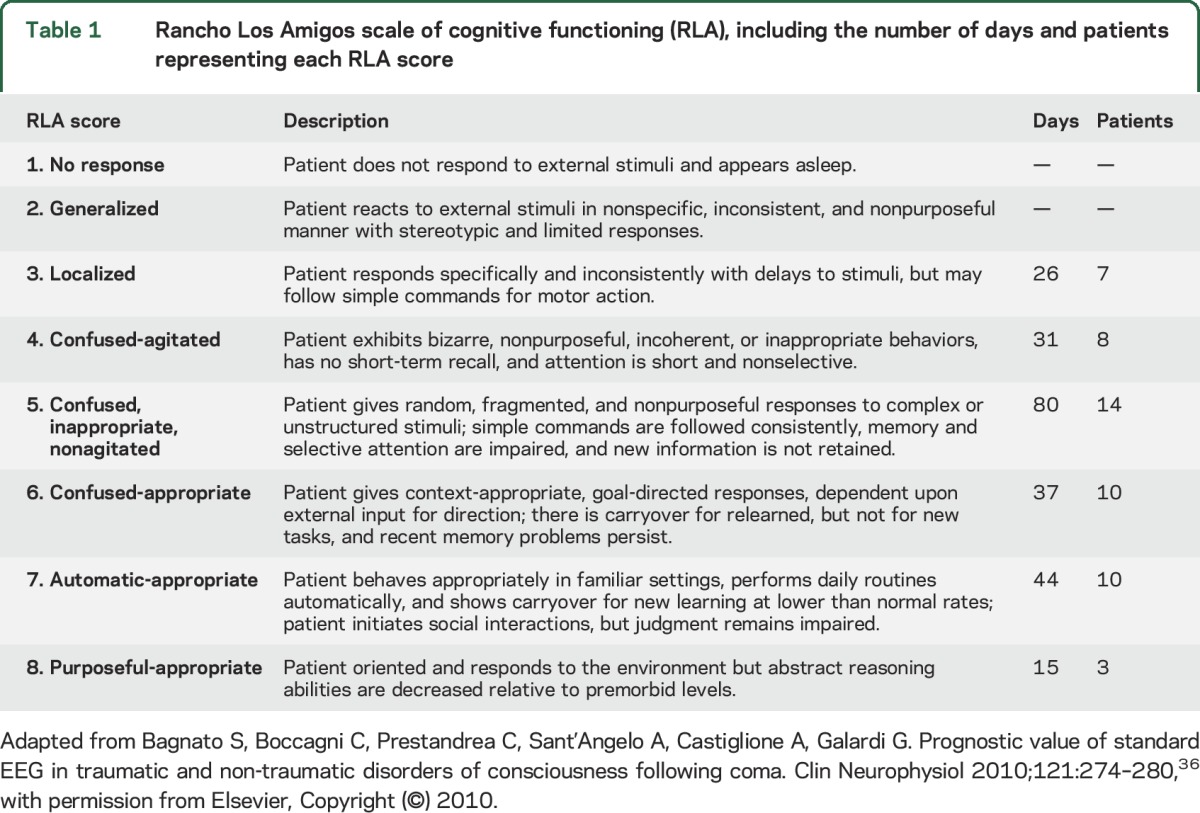
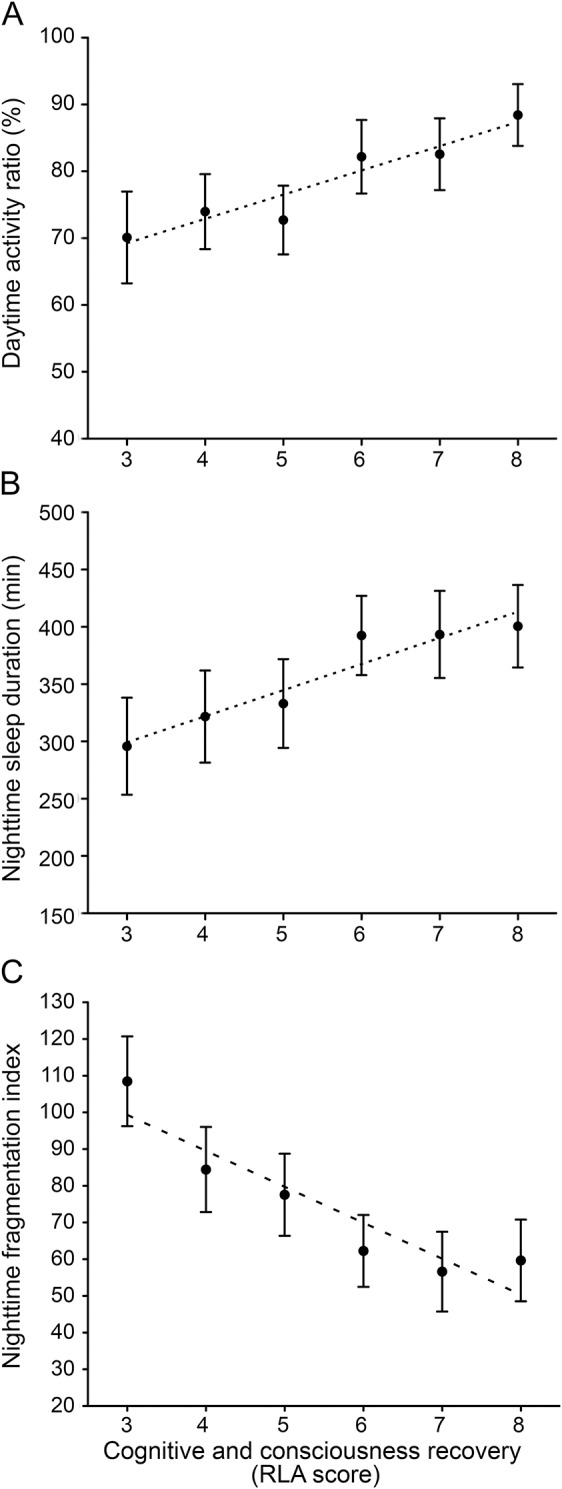
Daytime activity ratio.
We observed a strong association between RLA and DAR (table 2). Our results showed that an increase in RLA score was associated with a linear improvement in the consolidation of the 24-hour sleep-wake cycle, as measured by the DAR (figure 1A). When we used a DAR criterion of ≥80% to determine the occurrence of a consolidated sleep-wake cycle,1 we observed that patients attained a consolidated 24-hour sleep-wake cycle when they evolved from an RLA score of 5 (confused, nonpurposeful response, but able to answer simple commands) to 6 (goal-directed behavior). Figure 2 shows examples of actigraphic findings in relation to RLA scores.
Table 2.
Association between sleep-wake patterns and level of consciousness/cognition
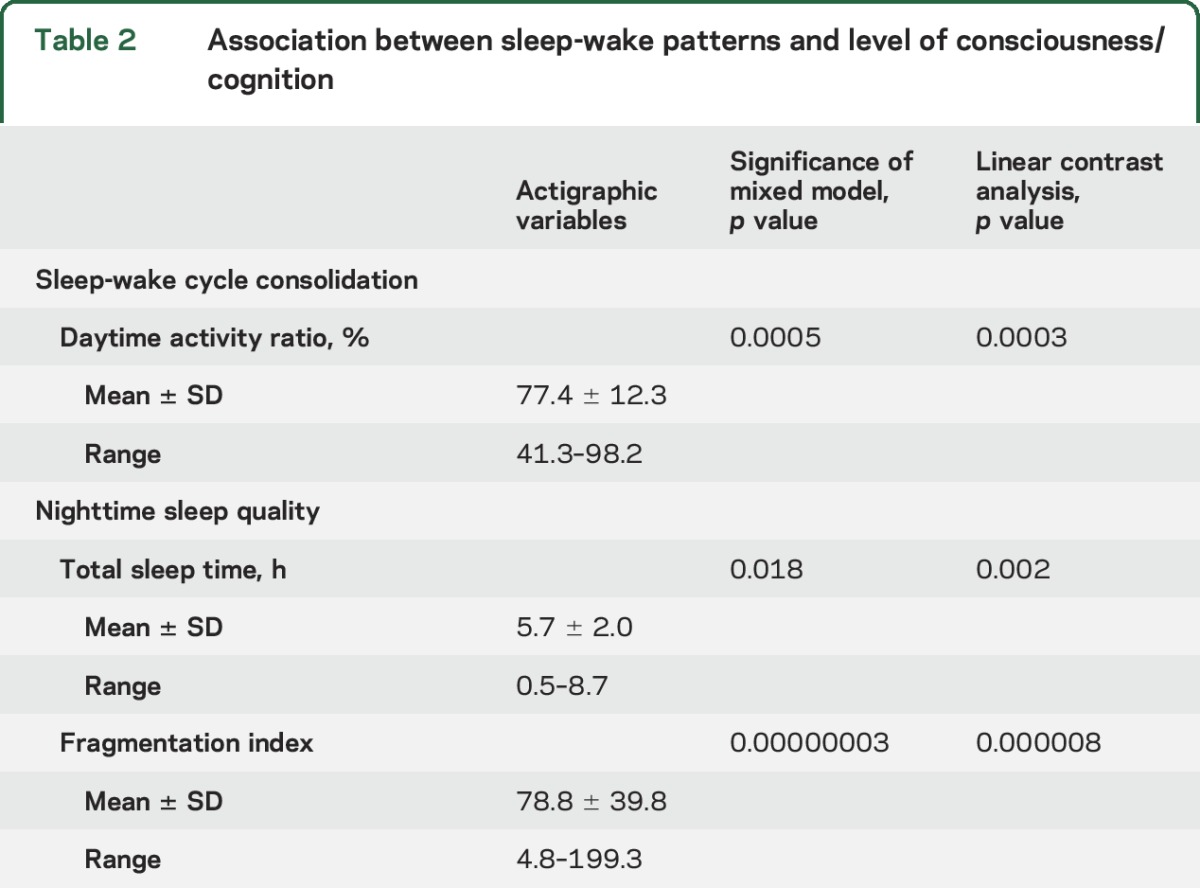
Figure 1. Association between cognitive and consciousness recovery and the sleep-wake cycle.
(A) Parallel evolution of the Rancho Los Amigos scale of cognitive functioning (RLA) score and daytime activity ratio in the 30 patients assessed over 233 days. Black dots indicate the mean daytime activity ratio per score on the RLA scale, generated within the mixed model equation, and black bars represent SEM. The linear contrast analysis was statistically significant (p < 0.001). (B) Parallel evolution of the RLA score and nighttime sleep duration. Black dots indicate the mean nighttime sleep duration (minutes) per score on the RLA scale, generated within the mixed model equation, and black bars represent SEM. The linear contrast analysis was statistically significant (p = 0.002). (C) Parallel evolution of RLA score and nighttime fragmentation index. Black dots indicate the mean nighttime fragmentation index per score on the RLA scale, generated within the mixed model equation, and black bars represent SEM. The linear contrast analysis was statistically significant (p < 0.001).
Figure 2. Examples of actigraphic findings in relation to Rancho Los Amigos scale of cognitive functioning (RLA) scores.
Examples of typical actigraphic findings for RLA ranging from 3 to 5 (left panel), and RLA ranging from 6 to 8 (right panel). Total activity counts for each minute of recording are illustrated by vertical dark lines, on a scale of 0 to 1,000 activity counts. Daytime hours (07:00–22:00 hours) are shown in yellow and nighttime hours (22:00–07:00 hours) in blue. Daily daytime activity ratios (DAR) are indicated at the bottom of each actogram.
Nighttime sleep duration.
We observed a moderate association between RLA score and nighttime sleep duration (trend for significance when the Bonferroni correction was applied), and an increase in RLA score was associated with a linear improvement in nighttime sleep duration (table 2 and figure 1B).
Nighttime fragmentation index.
We also found a strong association between RLA score and fragmentation index, such that an increase in RLA score was associated with a linear decrease in nighttime fragmentation index (table 2 and figure 1C).
Cross-correlations revealed that the best-fit lag between RLA and DAR was 0 (R2 = 0.816, p < 0.001), suggesting that improvements in DAR were simultaneous to that of RLA scores. Cross-correlations with nighttime sleep duration and nighttime fragmentation index were not significant, although a trend for a correlation at lag 0 was observed between RLA and fragmentation index (r = −0.60, p = 0.069).
DISCUSSION
In this study of 30 hospitalized patients in the acute phase of moderate and severe TBI, we demonstrate that the recovery of consciousness and higher cognitive functions occurs in parallel with improvements in consolidation of the sleep-wake cycle, as measured with actigraphy. Increasing consciousness and cognitive functioning was also tightly timed with the increase in the estimated nighttime sleep duration and the decrease in the estimated nighttime fragmentation index. This study establishes a clear link between acute sleep-wake disturbances and recovery of brain functions after TBI. No previous study investigated this temporal association in acute TBI following emergence from coma. Some research groups showed that the presence of sleep elements measured by EEG (i.e., sleep spindles, K-complexes, and REM sleep) are associated with level of consciousness, cognition or prognosis in posttraumatic coma, in the subacute phase of brain injuries, and in chronic disorders of consciousness.22–24 Other studies focused on the presence or absence of a 24-hour sleep-wake cycle in chronic disorders of consciousness. For example, a study25 compared the strength of the circadian rest-activity cycle of patients in chronic unresponsive wake syndrome (RLA score ∼2) to that of patients in chronic minimally conscious states (MCS; RLA score ∼3–5), using 4-day actigraphy, and showed a more robust circadian rhythm of rest-activity in patients in MCS. Our study shows that this parallel improvement continues with further improvement of the cognitive state, and demonstrates the linearity of the relationship. Our results also suggest that in acute TBI, consolidation of a circadian sleep-wake cycle attains an acceptable level (DAR ≥80%) only when patients emerge from MCS, marked by the capacity for functional communication or functional use of objects (RLA score ≥6).26 Prior to this stage of consciousness recovery, sleep and wake states are present, but are fragmented and dispersed throughout the day and night rather than consolidated in a circadian rhythm. Although we cannot confirm the causal relationship between the injured brain and sleep-wake patterns, our results suggest that when the brain has not sufficiently recovered a level of consciousness to sustain both arousal and awareness of one's surroundings, it is also unable to generate consolidated sleep and wake.
Though the linearity of the relationship between RLA and the actigraphy variables is strong, the 3 sleep-wake variables seem to plateau at RLA scores of 6, 7, and 8. This plateauing may reflect the optimal level of consolidation of the sleep-wake cycle and nocturnal sleep quality that patients can reach in this context, given the limitations of the hospital environment, nursing interventions, and residual pain. Future studies should aim to assess what constitutes normal sleep parameters among critically ill patients in the ICU and regular wards without brain injury, to better situate the sleep of TBI patients.
Given that in healthy individuals, sleep restriction negatively affects cognition, particularly memory formation,27 the inability to consolidate sleep and wake may hinder the recovery of consciousness and cognitive function after TBI. Impaired sleep is hypothesized to impede memory by preventing synaptic homeostasis.28 Without sleep, the brain is less able to encode and consolidate new information in memory. Synaptic plasticity and hippocampal neurogenesis, 2 crucial processes for recovery following TBI, are also highly sleep-dependent.29 In this context, poor sleep consolidation may impede cognitive recovery after a brain injury. However, in the present study, cross-correlation analyses suggest a synchronous recovery of sleep quality, cognition, and consciousness, rather than a causal relationship. This suggests that in the context of acute TBI, it is most likely overall neuronal recovery that drives the progressive return of consciousness, cognition, and sleep.
Strengths and limitations.
Actigraphy is a measure of physical motion and therefore indirectly measures sleep and wake through assessment of the rest-activity cycle. Actigraphy is closely correlated to polysomnography in healthy individuals and is well-validated for the estimation of sleep parameters across age groups.17 Moreover, one research team recently showed that actigraphy correlated with polysomnography-measured total sleep time and sleep efficiency among severe TBI inpatients in a rehabilitation setting.30 Still, results of the present study reflect an indirect measure of sleep and wake, though actigraphy remains the best-suited method for the long-term assessment of sleep-wake cycles within this clinical population.
Results from cross-correlations are sometimes criticized because they tend to overestimate the strength of time-lagged relationships, mainly because of data autocorrelations and intramultiplicity.21 However, given the strength of the cross-correlation analysis between RLA and DAR (r = 0.816) and a moderate autocorrelation (0.5) in our data, we estimate our type I error rate bias to be under 0.10,21 which is negligible. Moreover, given the high variability of RLA scores and actigraphy data on each day of actigraphy recording, averaging our RLA and actigraphy data per day most likely weakened interday differences. Such pooling of data to create averages per day, as required to perform cross-correlation analyses, reduces variability and the number of data points, and may thus explain why no cross-correlation was significant with nighttime sleep duration and fragmentation index (trend for significance only).
Clinical implications.
This study showed that the consolidation of sleep and wake states goes hand in hand with the recovery of consciousness and cognition in acute TBI, though the directionality (or bidirectionality) of this relationship remains unknown. Insight into the association between neuronal recovery and the sleep-wake cycle could help shed light on the pathophysiology of post-TBI sleep-wake disturbances, which frequently persist up to several years postinjury.31–35 This association also suggests that assessment of the sleep-wake cycle in acute TBI may be a useful tool for monitoring patient evolution and recovery. Moreover, the possibility of a positive feedback action of improved consolidation of sleep and wake states on consciousness and cognitive recovery may be worthy of further investigation. The role of hospital lighting and noise could be interesting to assess in future studies in order to better appraise their implications in sleep-wake disturbances. However, given that patients in the present study were hospitalized in the same environment but had different sleep-wake cycle consolidation and quality depending on their level of consciousness, this may suggest that environmental factors only partly account for the sleep-wake disturbances observed in hospitalized TBI patients. Results from the present study could have implications for the development of interventions targeting sleep-wake cycles and aimed at optimizing functional recovery in both acute and chronic disorders of consciousness.
Supplementary Material
ACKNOWLEDGMENT
The authors thank Elyse Laflamme and Jeanne Woo, occupational therapists at Hôpital du Sacré-Coeur de Montréal, for providing the RLA evaluations and scores of the patients included in this study; Dr. Harrison Westwick for scoring CT scans according to Marshall and Rotterdam criteria; the patients and their families for their collaboration; as well as the nursing staff of the Intensive Care Unit and Neurological Ward for their help in monitoring patients during actigraphy recordings.
GLOSSARY
- AR1
autoregressive
- CS
compound symmetry
- DAR
daytime activity ratio
- GCS
Glasgow Coma Scale
- ICU
intensive care unit
- MCS
minimally conscious state
- RLA
Rancho Los Amigos scale of cognitive functioning
- TBI
traumatic brain injury
Footnotes
Editorial, page 226
AUTHOR CONTRIBUTIONS
Catherine Duclos: acquisition of data, analysis and interpretation of data, drafting and critically revising the manuscript. Marie Dumont: conception and design of the study, analysis and interpretation of data, drafting and revising the manuscript. Caroline Arbour: analysis and interpretation of data, drafting and revising the manuscript. Jean Paquet: analysis and interpretation of data, drafting and revising the manuscript. Hélène Blais: conception and design of the study, acquisition of data, analysis and interpretation of data, drafting and revising the manuscript. David K. Menon: conception and design of the study, interpretation of data, drafting and revising the manuscript. Louis De Beaumont: interpretation of data, drafting and revising the manuscript. Francis Bernard: conception and design of the study, interpretation of data, drafting and revising the manuscript. Nadia Gosselin: led conception and design of the study, analysis and interpretation of data, drafting and revising the manuscript.
STUDY FUNDING
This study was supported by the Canadian Institutes of Health Research (grant no. 115172) and by the Fonds pour la Recherche du Québec–Santé (grant no. 24742).
DISCLOSURE
C. Duclos received studentship funding from the Université of Montréal. M. Dumont, C. Arbour, J. Paquet, H. Blais, D. Menon, L. De Beaumont, F. Bernard, and N. Gosselin report no disclosures relevant to the manuscript. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Duclos C, Dumont M, Blais H, et al. Rest-activity cycle disturbances in the acute phase of moderate to severe traumatic brain injury. Neurorehabil Neural Repair 2013;28:472–482. [DOI] [PubMed] [Google Scholar]
- 2.Chiu HY, Chen PY, Chen NH, Chuang LP, Tsai PS. Trajectories of sleep changes during the acute phase of traumatic brain injury: a 7-day actigraphy study. J Formos Med Assoc 2013;112:545–553. [DOI] [PubMed] [Google Scholar]
- 3.Gabor JY, Cooper AB, Crombach SA, et al. Contribution of the intensive care unit environment to sleep disruption in mechanically ventilated patients and healthy subjects. Am J Respir Crit Care Med 2003;167:708–715. [DOI] [PubMed] [Google Scholar]
- 4.Olson E, Badder C, Sullivan S, Smith C, Propert KJ, Margulies SS. Alterations in daytime and nighttime activity in piglets after focal and diffuse brain injury. J Neurotrauma 2015;33:734–740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sabir M, Gaudreault PO, Freyburger M, et al. Impact of traumatic brain injury on sleep structure, electrocorticographic activity and transcriptome in mice. Brain Behav Immun 2015;47:118–130. [DOI] [PubMed] [Google Scholar]
- 6.Skopin MD, Kabadi SV, Viechweg SS, Mong JA, Faden AI. Chronic decrease in wakefulness and disruption of sleep-wake behavior after experimental traumatic brain injury. J Neurotrauma 2015;32:289–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Makley MJ, Johnson-Greene L, Tarwater PM, et al. Return of memory and sleep efficiency following moderate to severe closed head injury. Neurorehabil Neural Repair 2009;23:320–326. [DOI] [PubMed] [Google Scholar]
- 8.Holcomb EM, Towns S, Kamper JE, et al. The relationship between sleep-wake cycle disturbance and trajectory of cognitive recovery during acute traumatic brain injury. J Head Trauma Rehabil 2016;31:108–116. [DOI] [PubMed] [Google Scholar]
- 9.Blume C, Del Giudice R, Wislowska M, Lechinger J, Schabus M. Across the consciousness continuum: from unresponsive wakefulness to sleep. Front Hum Neurosci 2015;9:105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Menon DK, Schwab K, Wright DW, Maas AI. Position statement: definition of traumatic brain injury. Arch Phys Med Rehabil 2010;91:1637–1640. [DOI] [PubMed] [Google Scholar]
- 11.Teasdale G, Jennett B. Assessment of coma and impaired consciousness: a practical scale. Lancet 1974;2:81–84. [DOI] [PubMed] [Google Scholar]
- 12.Marshall LF, Marshall SB, Klauber MR, et al. The diagnosis of head injury requires a classification based on computed axial tomography. J Neurotrauma 1992;9(suppl 1):S287–S292. [PubMed] [Google Scholar]
- 13.Maas AI, Hukkelhoven CW, Marshall LF, Steyerberg EW. Prediction of outcome in traumatic brain injury with computed tomographic characteristics: a comparison between the computed tomographic classification and combinations of computed tomographic predictors. Neurosurgery 2005;57:1173–1182. [DOI] [PubMed] [Google Scholar]
- 14.Rappaport M, Hall KM, Hopkins K, Belleza T, Cope DN. Disability rating scale for severe head trauma: coma to community. Arch Phys Med Rehabil 1982;63:118–123. [PubMed] [Google Scholar]
- 15.Hagen C, Malkmus D, Durham P. Rancho Los Amigos Levels of Cognitive Functioning Scale. Downey, CA: Professional Staff Association of Rancho Los Amigos National Rehabilitation Center; 1972. [Google Scholar]
- 16.Dowling GA. Levels of cognitive functioning: evaluation of interrater reliability. J Neurosurg Nurs 1985;17:129–134. [DOI] [PubMed] [Google Scholar]
- 17.Martin JL, Hakim AD. Wrist actigraphy. Chest 2011;139:1514–1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Han HJ. Comparison of results with actigraphy and polysomnography in two sleep disorders: obstructive sleep apnea syndrome and primary insomnia. J Korean Neurol Assoc 2003;21:156–162. [Google Scholar]
- 19.Wang D, Wong KK, Dungan GC II, Buchanan PR, Yee BJ, Grunstein RR. The validity of wrist actimetry assessment of sleep with and without sleep apnea. J Clin Sleep Med 2008;4:450–455. [PMC free article] [PubMed] [Google Scholar]
- 20.Littell RC, Pendergast J, Natarajan R. Modelling covariance structure in the analysis of repeated measures data. Stat Med 2000;19:1793–1819. [DOI] [PubMed] [Google Scholar]
- 21.Olden DJ, Neff DB. Cross-correlation bias in lag analysis of aquatic time series. Mar Biol 2001;138:1063–1070. [Google Scholar]
- 22.Bergamasco B, Bergamini L, Doriguzzi T, Fabiani D. EEG sleep patterns as a prognostic criterion in post-traumatic coma. Electroencephalogr Clin Neurophysiol 1968;24:374–377. [DOI] [PubMed] [Google Scholar]
- 23.de Biase S, Gigli GL, Lorenzut S, et al. The importance of polysomnography in the evaluation of prolonged disorders of consciousness: sleep recordings more adequately correlate than stimulus-related evoked potentials with patients' clinical status. Sleep Med 2014;15:393–400. [DOI] [PubMed] [Google Scholar]
- 24.Ron S, Algom D, Hary D, Cohen M. Time-related changes in the distribution of sleep stages in brain injured patients. Electroencephalogr Clin Neurophysiol 1980;48:432–441. [DOI] [PubMed] [Google Scholar]
- 25.Cruse D, Thibaut A, Demertzi A, et al. Actigraphy assessments of circadian sleep-wake cycles in the vegetative and minimally conscious states. BMC Med 2013;11:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Giacino JT, Ashwal S, Childs N, et al. The minimally conscious state: definition and diagnostic criteria. Neurology 2002;58:349–353. [DOI] [PubMed] [Google Scholar]
- 27.Walker MP, Stickgold R. Sleep, memory, and plasticity. Annu Rev Psychol 2006;57:139–166. [DOI] [PubMed] [Google Scholar]
- 28.Tononi G, Cirelli C. Sleep and the price of plasticity: from synaptic and cellular homeostasis to memory consolidation and integration. Neuron 2014;81:12–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kreutzmann JC, Havekes R, Abel T, Meerlo P. Sleep deprivation and hippocampal vulnerability: changes in neuronal plasticity, neurogenesis and cognitive function. Neuroscience 2015;309:173–190. [DOI] [PubMed] [Google Scholar]
- 30.Kamper JE, Garofano J, Schwartz DJ, et al. Concordance of actigraphy with polysomnography in traumatic brain injury neurorehabilitation admissions. J Head Trauma Rehabil 2016;31:117–125. [DOI] [PubMed] [Google Scholar]
- 31.Baumann CR, Werth E, Stocker R, Ludwig S, Bassetti CL. Sleep-wake disturbances 6 months after traumatic brain injury: a prospective study. Brain 2007;130:1873–1883. [DOI] [PubMed] [Google Scholar]
- 32.Sommerauer M, Valko PO, Werth E, Baumann CR. Excessive sleep need following traumatic brain injury: a case-control study of 36 patients. J Sleep Res 2013;22:634–639. [DOI] [PubMed] [Google Scholar]
- 33.Imbach LL, Valko PO, Li T, et al. Increased sleep need and daytime sleepiness 6 months after traumatic brain injury: a prospective controlled clinical trial. Brain 2015;138:726–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Duclos C, Dumont M, Wiseman-Hakes C, et al. Sleep and wake disturbances following traumatic brain injury. Pathol Biol 2014;62:252–261. [DOI] [PubMed] [Google Scholar]
- 35.Ouellet MC, Beaulieu-Bonneau S, Morin CM. Sleep-wake disturbances after traumatic brain injury. Lancet Neurol 2015;14:746–757. [DOI] [PubMed] [Google Scholar]
- 36.Bagnato S, Boccagni C, Prestandrea C, Sant'Angelo A, Castiglione A, Galardi G. Prognostic value of standard EEG in traumatic and non-traumatic disorders of consciousness following coma. Clin Neurophysiol 2010;121:274–280. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.