Abstract
Psychological interventions have been designed and implemented effectively in a wide range of medical conditions, including Irritable Bowel Syndrome (IBS) and Inflammatory Bowel Diseases (IBD). The psychological treatments for IBS and IBD with the strongest evidence base include: cognitive behavioral therapy, hypnosis, and mindfulness-based therapies. The evidence for each of these therapies is reviewed here for both IBS and IBD. In general, there is a stronger and larger evidence base to support the use of psychological interventions in IBS compared with IBD. This is likely due to the high level of psychiatric comorbidity associated with IBS and the involvement of the stress-response in symptom presentation of IBS. Further research in psychosocial interventions for IBD is necessary. Finally, the importance of conceptualizing both IBS and IBD in a biopsychosocial model is discussed and several resources for accessing Clinical Health Psychology materials and referrals are provided.
INTRODUCTION
Psychological interventions have been designed and implemented effectively in a wide range of medical conditions. The subspecialty area of clinical health psychology aims specifically to identify and target stress-related and psychological factors that may contribute to the impact or expression of medical problems. Over the past several decades, health psychology and gastroenterology have become increasingly aligned, with a large body of research to support the effectiveness of psychological interventions for a range of gastrointestinal (GI) disorders. This review will outline and describe health psychology interventions for two of the most burdensome GI disorders: irritable bowel syndrome (IBS) and inflammatory bowel diseases (IBD).
IBS and IBD are distinct medical conditions that share some similarities in symptoms and illness burden. IBS is a functional disorder characterized by abdominal pain and abnormalities in defecation while IBD represents a range of organic, immune-mediated inflammatory disorders (e.g., Crohn's disease and ulcerative colitis), characterized by abdominal pain, urgent diarrhea, rectal bleeding, weight loss and fatigue. Although the etiologies of these disorders are different, both are associated with high disease burden and low quality of life and psychological interventions can be helpful in both disorders.1, 2 Among patients with IBS, psychological interventions can serve as stand-alone therapies to decrease physical GI symptoms and improve overall functioning. Among patients with IBD, psychological interventions complement and may even optimize existing medical interventions in an effort to improve quality of life, medical adherence, and to help patients cope with the effects of a chronic illness.
The psychological treatments for IBS and IBD with the strongest evidence base include cognitive behavioral therapy, hypnosis, and mindfulness-based therapies. Other treatments that have been tested in IBS and IBD, but have revealed weaker evidence, include psychodynamic and interpersonal therapies. These therapies are discussed in detail below and the literature pertaining to IBS and IBD is reviewed for each. In general, the reader will find that there is a much smaller evidence base for psychological treatments for IBD compared with IBS; psychotherapy for IBD is a much newer area of research. This research gap is largely due to the psychologist being able to clearly demonstrate clinical success, given the functional nature of IBS, the involvement of the stress-response in symptom presentation of IBS, and the very high rate of psychiatric comorbidity with IBS. Nonetheless, there is evidence for the use of certain psychological treatments in IBD and these will be discussed.
It should also be mentioned that there is a high rate of comorbidity between IBS and IBD, with 30–50% of patients diagnosed with IBD also reporting IBS-type symptoms3, 4, 5 (defined as active gastrointestinal symptoms in the setting of endoscopic remission of IBD). With this in mind, psychological treatments that are effective in IBS will likely also be effective in IBD patients who suffer from comorbid IBS, although this has not been adequately studied.
COGNITIVE BEHAVIORAL THERAPY (CBT)
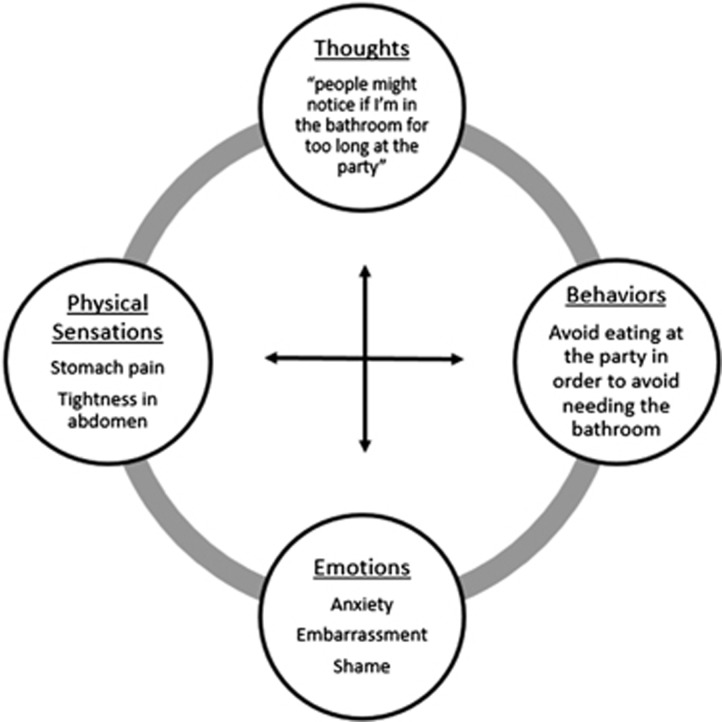
Cognitive behavioral therapy was developed initially as a treatment for depression.6 In the CBT model, the relationship between situations, thoughts, behaviors, physical reactions, and emotions is the primary focus of treatment. Patients build insight into the relationship between each of these factors and learn ways to intervene on their thoughts, their behaviors, and even their physiologic responses to improve mood or emotions (Figure 1). For example, patients may learn to catch and change unhelpful thinking patterns; to engage in relaxation exercises; and to change behaviors (i.e., avoidance and isolation) that may contribute to physical or psychological distress.
Figure 1.
Cognitive behavioral model.
IBS
CBT is the most widely-studied psychotherapy treatment for IBS and there is a strong evidence base to support the use of CBT as a first-line treatment in this patient population. The cognitive behavioral model for treating IBS focuses primarily on the following components: (1) psychoeducation about the stress response and its relationship to GI symptoms; (2) Building insight into cognitive and behavioral responses to IBS symptoms and/or fear of symptoms; and (3) Modifying those responses to decrease distress related to IBS and decrease physical reactivity to stress.7 There is no singular standardized protocol of CBT for IBS, and different research studies have applied this treatment in slightly different ways, typically within 6–12 therapy sessions, although the optimal number of CBT sessions for IBS is not yet known. Research seeking to establish standard ‘dosing' of CBT for IBS has found that 4 therapy sessions delivered over the course of 10 weeks was as effective as 10 sessions over 10 weeks,8 leading to the development of a cost-effective minimal-contact model for CBT,9 which is currently being tested. Although most research has evaluated CBT for IBS using individual, face-to-face treatment, CBT can also be delivered effectively in groups and via telehealth or internet-based protocols.10, 11, 12 However, there is evidence to suggest that a face-to-face format may be preferred by some patients, especially those who are less motivated to make changes or to complete self-monitoring exercises.13
In randomized controlled trials, CBT for IBS has been shown to be effective when compared with control groups14 and to standard medical interventions.15, 16, 17 Recent meta analyses have found that CBT for IBS is highly effective in improving bowel symptoms, quality of life, and psychological distress and that these effects persist beyond the treatment phase and into long-term follow-up.1, 18, 19, 20 Furthermore, a recent study used mediational analysis to identify mechanisms by which CBT affects IBS symptom expression and revealed that CBT has a direct effect on IBS symptoms, independent of its effects on psychological distress.21 Newer forms of CBT are currently being developed to target IBS symptoms and illness-related behaviors directly (e.g., exposure based therapies),22, 23, 24 which may be an appealing option especially for IBS patients without comorbid psychological concerns.
IBD
There is a much smaller body of evidence to evaluate the efficacy of CBT for IBD. In existing studies, proposed cognitive behavioral models for the treatment of IBD focus on coping with illness, adhering to medical recommendations, and addressing any underlying symptoms of anxiety or depression. Just as in CBT for IBS there is no singular CBT protocol for IBD, and different studies have applied the cognitive behavioral model in different ways with this population.
The evidence base for use of CBT with IBD is mixed.25, 26 Unlike in IBS, CBT for IBD has generally not been shown to produce improvements in physical symptoms or overall disease status in adult patients.2 However, CBT for IBD may serve to improve quality of life and coping skills among this patient population.26 Previous studies have shown that individuals who have IBD and a comorbid psychological diagnosis tend to experience increased disease activity and worse complications.27 Thus, most of the available research has suggested that CBT can be effective for individuals with IBD when they also report comorbid psychiatric symptoms or very low quality of life.28 Among adult patients with IBD who do not have comorbid psychiatric symptoms, the data is mixed and is based on a small number of studies.29, 30
Interestingly, CBT for IBD has produced more promising results in adolescents. A 2011 Cochrane review based on 2 adolescent studies31, 32 found that CBT had a small, positive effect for quality of life, coping, depression, and anxiety for adolescents but not adults.33 Since then, a randomized controlled study has revealed that both CBT and supportive therapy can reduce symptoms of depression and improve quality of life in adolescents with IBD and that CBT may be associated with reduced IBD activity.34
For patients who do not exhibit psychiatric symptoms and/or who are not interested in traditional psychotherapy, Behavioral or Self-Management Therapy may be effective, although it requires further study. In Behavioral/Self-Management Therapy, the goal is to target negative health behaviors (e.g., poor medication compliance; dietary non-adherence) to improve overall physical health. This therapy is informed by the CBT model but does not incorporate the cognitive component of traditional CBT, which evaluates negative or distressing thought patterns. The trials that have evaluated Behavioral/Self-Management for IBD have suggested that this may help to improve disease outcomes and quality of life.35, 36
HYPNOTHERAPY
Hypnotherapy has been used in a wide range of medical conditions and has been shown to be effective in reducing or alleviating physical symptoms of cancer,37 arthritis,38 fibromyalgia,39 and chronic pain.40 Gut-directed hypnotherapy is a variation of medical hypnosis that focuses post-hypnotic suggestions on the health of the gastrointestinal tract. This treatment typically involves 7–12 weekly sessions in which patients first learn to achieve and deepen a hypnotic state and are then led through a series of scripted, gut-focused imageries with hypnotic suggestions in each session (Figure 2). Patients practice these exercises at home using audio recordings and are typically asked to track their progress and symptoms using self-monitoring forms.41
Figure 2.
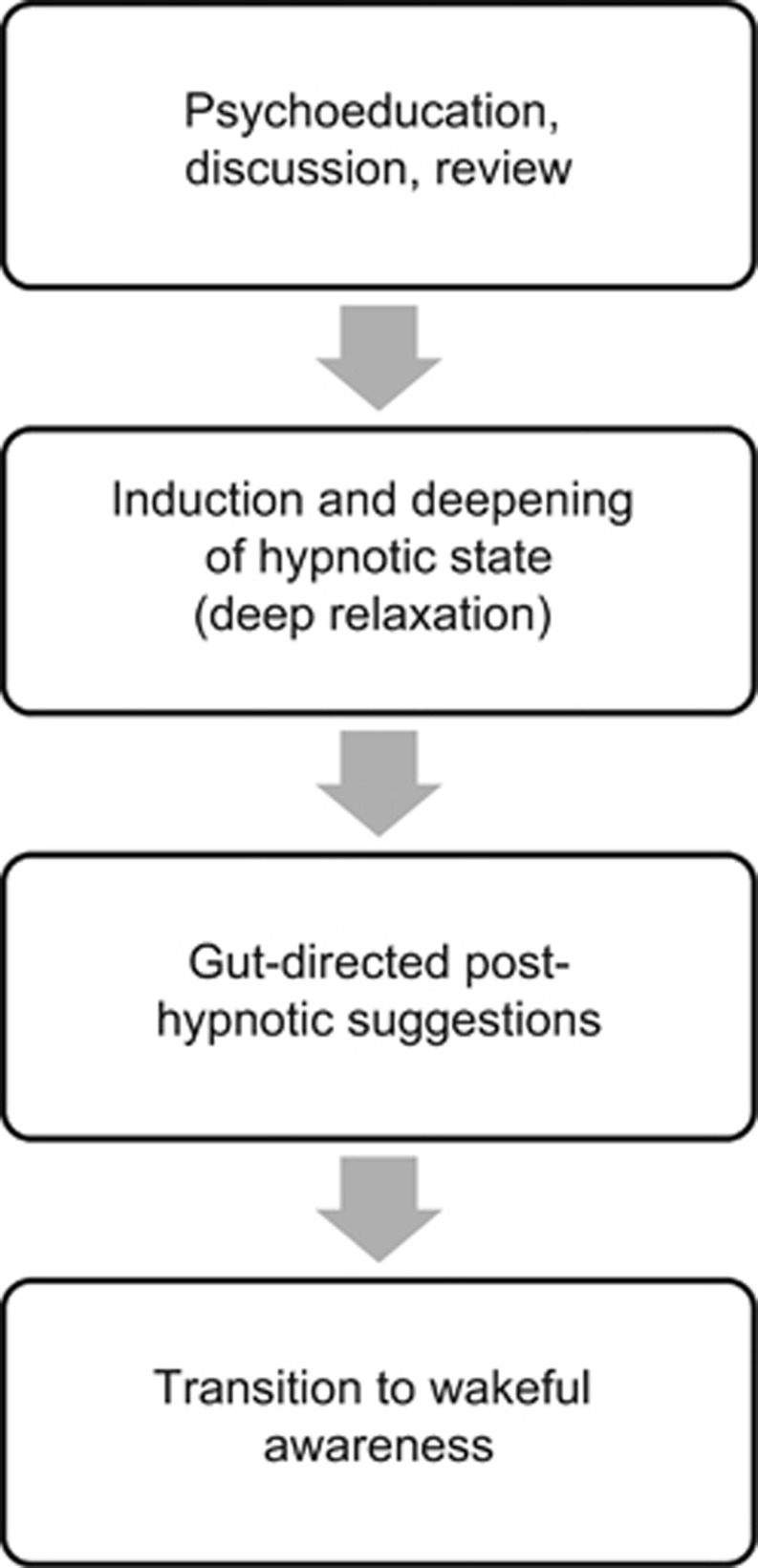
Typical stages of a hypnotherapy session.
IBS
Gut-directed hypnotherapy has been shown to be highly effective in the treatment of IBS, including treatment-refractory IBS.42 There are currently two available standardized hypnotherapy protocols for IBS: the Manchester Approach43 and the North Carolina Protocol.44 Both are scripted, gut-directed hypnotherapy protocols and are meant to be delivered in 7–10 sessions over a 8–12 week period.
The first controlled trial to evaluate hypnotherapy in IBS was published in 1984 and found hypnotherapy to be more effective than control treatment in improving abdominal pain, bloating, bowel dysfunction, and quality of life.45 Since that time, these findings have been replicated and extended by several research groups using both the Manchester Approach and the North Carolina Protocol to demonstrate the efficacy of hypnotherapy in this patient population.46, 47, 48, 49, 50, 51 Hypnotherapy has been shown to have long-term benefits, with 83% of responders in one study maintaining treatment benefits for 1–5 years after the course of treatment.52 It is also at least as effective as dietary treatment (FODMAPS) for IBS51 and has been shown to be a useful addition to standard medical care.53 Similar to the literature evaluating CBT for IBS, the literature evaluating hypnotherapy primarily involves individual, face-to-face treatment. There is some evidence to suggest that group hypnotherapy may be effective in this population of patients,54, 55 although further research in this area is warranted.
The mechanism of action for hypnotherapy in IBS is not fully understood. Hypnotherapy is hypothesized to produce direct effects on gut function,56, 57 visceral sensitivity,58 and psychological factors (e.g., cognitive patterns, anxiety, and depression).59, 60 Furthermore, imaging studies have suggested that hypnotherapy may normalize pain processing in the anterior cingulate cortex, a region of the brain that has been shown to be over-active in some IBS patients.61, 62
IBD
Most of the available literature to support the use of hypnotherapy in IBD involves small samples and case studies. Nonetheless, compelling data have been presented to suggest that hypnotherapy can reduce rectal mucosal inflammatory responses (IL-6, IL-13, TNF-α, substance P, and histamine) in patients with ulcerative colitis after just one session of hypnotherapy.63 In the only randomized controlled study of hypnotherapy in IBD, 54 patients with quiescent ulcerative colitis received 7 sessions of hypnotherapy and demonstrated prolonged clinical remission by ~2.5 months compared with controls.64 Finally, in a study of 15 patients with severe, active IBD who received 12 sessions of gut-directed hypnotherapy followed by 5 years of follow up, 26.6% of patients maintained remission for the entire 5 years and 60% of patients did not require further corticosteroid therapy for entire follow-up period.65 The mechanism of action for hypnotherapy in IBD has not yet been evaluated and future studies should seek to clarify this question.
MINDFULNESS
Mindfulness-based therapy (MBT) is a form of treatment that uses meditation and relaxation to foster awareness and acceptance of the present moment. This kind of therapy requires individuals to practice noticing and observing details about their surroundings without passing judgment or reacting to triggers in the environment. This practice typically takes place through formal exercises with the ultimate goal of learning to engage this non-judgmental and non-reactive mindset in one's day-to-day activities (Table 1). Although there are many variations of MBTs, most are based on Jon Kabat-Zinn's Mindfulness Based Stress Reduction (MBSR) program for coping with chronic illness.66
Table 1. Common mindfulness exercises.
| Exercise | Description |
|---|---|
| Mindful breathing | Purposefully observe breath cycles, noticing and observing the air travel in and out of the body. |
| Mindful eating | Choose a food (e.g. raisin) and practice eating mindfully. Hold the raisin, see, touch, smell, place in mouth, taste, and swallow. Observe this process for 3–5 min. |
| Mindful listening | Close eyes and notice the sounds in the environment |
| Mindful observation | Choose an object and observe it for 2–3 min, noticing the texture, shape, weight, and color etc. |
In IBS and IBD, mindfulness-based exercises are not necessarily specific to GI-illnesses, although they may be practiced in the setting of active GI symptoms and may be modified to focus directly on GI symptoms if indicated. The goal of these exercises is to notice and to accept discomfort (physical and/or mental) without making any judgments or attempts to change the present moment. This skill can be achieved and practiced at first using neutral or day-to-day activities such as breathing or eating. Eventually, this skill may be applied to more salient situations such as active symptom experience in order to promote a calm and non-reactive response to symptoms that may have once caused physical or emotional distress.
IBS
MBTs have been used effectively for a wide range of psychiatric and medical diagnoses,67, 68 including IBS.69, 70 Among patients with IBS, MBT is shown to decrease hypervigilance to visceral sensations, to decrease catastrophization in the setting of active symptoms, and to lead to improvement in overall symptoms and quality of life.71 In, 2011, a randomized control trial demonstrated a 38.2% reduction in IBS symptom severity, along with improvement in quality of life, after having completed 8 weekly training sessions in mindfulness.71 In 2013, another study replicated these findings and demonstrated maintenance of improvements in IBS symptom severity and psychological distress up to 6 months post-treatment.72 However, it should be noted that the participants in these studies were primarily affluent, Caucasian women, and these results may not be generalizable to the larger population of IBS sufferers. Clearly, the evidence base for MBT is much smaller than for CBT or hypnosis and further research is needed. In future research, MBT skills may be incorporated into CBT protocols to produce a hybrid treatment; this treatment blend has been found effective in a preliminary, internet-based treatment trial.73, 74
IBD
Several studies have evaluated the efficacy of mindfulness-based interventions in IBD. These studies have demonstrated effects in patients with both active and inactive disease and have included Ulcerative Colitis and Crohn's Disease. A recent study comparing MBT to waitlist control found that the mindfulness group reported significant improvements in anxiety, quality of life, and depression when compared to the control group.75 This study also found that these effects persisted at 6-month follow-up. Other studies have produced compelling but less clear results. In 2014, a study comparing group MBT to group psychoeducation (time/attention control) did not find any significant differences between groups in terms of disease activity, mindfulness, depression, or anxiety, but did find that the participants who completed MBT reported higher quality of life during their next disease flare.76 Similarly, another study of 55 patients with both IBD and IBS symptoms found that MBT produced higher quality of life scores, although their results were not statistically significant.77
PSYCHODYNAMIC AND INTERPERSONAL THERAPIES
Psychodynamic therapies have not been tested as rigorously as have CBT, hypnosis, and mindfulness in patients with gastrointestinal disorders. This is partly due to the nature of these therapies, which are not manualized and can be difficult to test in a controlled research environment. Of the trials that do exist with GI populations, brief psychodynamic and brief interpersonal therapies have been used (usually lasting 10–12 sessions). These therapies are un-structured and their goal is to build insight into different aspects of one's illness experiences. This is typically achieved through an in-depth discussion of symptoms and interpersonal conflicts. For the purposes of this review, the term “psychodynamic” will be used to refer to both brief interpersonal and brief psychodynamic treatments, which have significant overlap and which are both based in psychodynamic theory.
IBS
There are few available research studies evaluating brief psychodynamic psychotherapy for IBS. The first available study is from 1983 by Svedlund et al.,78 in which 101 patients were randomized to two groups: medical treatment alone (standard care) or medical treatment with 10 weekly sessions of psychodynamic psychotherapy. After 3 months, the patients who received psychotherapy reported more symptom improvement than those who received only medical treatment and these group differences persisted at 1-year follow-up. In the 1990s, Guthrie et al. conducted two studies demonstrating that 12 weeks of psychodynamic therapy was superior to supportive listening, but suggested that this difference might apply only to women.79, 80 More recently, Creed et al. compared psychodynamic therapy to an antidepressant group and a standard care group and found no differences between psychodynamic therapy and antidepressant treatment, although both were superior to standard care.81 Creed's findings also suggested that psychodynamic therapy might be most effective for individuals with trauma histories.82
IBD
Only one study to our knowledge has evaluated psychodynamic treatment for IBD. In 2004, Keller et al. compared 12 weeks of psychodynamic therapy to standard care in a sample of 81 patients with Crohn's Disease.83 No differences were found between psychodynamic therapy and standard care on psychosocial or disease variables, but a tendency towards fewer surgical procedures and fewer relapses in the psychodynamic group was noted.
CONCLUSION
There is strong evidence to support the use of a variety of psychotherapeutic interventions for patients with gastrointestinal illnesses. This paper reviewed three of the most common evidence-based psychological treatments for IBS and IBD (cognitive behavioral therapy; hypnotherapy; and mindfulness-based therapy) and also presented evidence for other psychotherapies that have been tested but have produced weaker results (psychodynamic and interpersonal therapies). There is a large body of literature to support the use of psychological interventions with IBS and a smaller, growing body of literature evaluating these interventions in IBD. This discrepancy is not surprising as IBS is traditionally classified with the functional disorders, which tend to be more psychosocially complex, and IBD is an organic disease with fewer psychiatric and social contributors. Despite this, psychotherapeutic interventions can be useful in both illnesses.
Not only can the interventions reviewed in this paper improve quality of life and mental health among patients with IBS and IBD, these therapies also directly target physiological processes by reducing arousal of the autonomic nervous system, decreasing the stress-response, and even reducing inflammation. This physiologic effect is largely due to the so-called brain-gut axis, which explains in part the common gastrointestinal consequences of stress and anxiety. Although the brain-gut axis is particularly important in the treatment of IBS, it is also relevant among patients with IBD, especially when considering the increased likelihood of an IBD flare in the context of chronic stress.84, 85
In the subspecialty area of clinical health psychology, all physical illness is considered and treated in the framework of the biopsychosocial model in which a patient's symptom presentation and experience is contextualized given his/her unique medical, psychological, and social history. This is especially important when considering functional disorders, like IBS, but is also valuable in the context of chronic relapsing and remitting diseases such as IBD. Furthermore, many patients with IBD present with overlapping functional gastrointestinal symptoms, which may be particularly vulnerable to stress and other psychosocial variables. In IBD patients with comorbid IBS, the psychological approaches mentioned here can be expected to work by reducing or alleviating psychosocial contributors to symptom severity (IBS-focused) while also improving health behaviors such as adherence to dietary and medical recommendations (IBD-focused). For example, if a patient with IBD is in clinical remission based on laboratory tests but is reporting active GI symptoms (e.g., abdominal pain and diarrhea), an evidence-based psychotherapy for IBS might be appropriate. If, on the other hand, a patient is experiencing mild symptoms of active IBD or is reporting distress related specifically to their diagnosis of IBD, an evidence-based psychotherapy for IBD may be indicated. In clinical practice, it is common for these two approaches to be combined to suit the needs of a patient with comorbid IBD and IBS. It should be noted, however, that there are not currently any research studies to evaluate the effects of psychotherapy for IBD with comorbid IBS and future research in this area is necessary.
OUTLOOK
Given the importance of stress and psychosocial variables on the overall functioning of many patients with IBS and IBD, it is clinically valuable to offer all IBS and IBD patients access to multidisciplinary treatment to address disease aspects related to both mind and body. However, this option is not yet available to most gastroenterology patients due largely to the financial barriers of establishing a large multidisciplinary practice as well as to the lack of appropriately trained health psychologists with expertize in psychosocial gastroenterology. When a gastroenterology patient is able to receive multidisciplinary care, it typically takes place through referrals to different, specialized practices and communication between these providers is often poor.
Ideally, a patient would be seen by a multidisciplinary team within the same practice. This would allow providers to collaborate and consult with each other and would provide a richer and more comprehensive treatment plan to each patient. For example, if a gastroenterologist, psychologist, and nutritionist are available to discuss a patient's treatment plan, each of these providers can reinforce and build on the work of the others. The psychologist can help a patient to implement behavioral changes (i.e., dietary and medical adherence) while a nutritionist can remain informed about psychosocial barriers that might impede change or motivation. The gastroenterologist, meanwhile, gains a richer biopsychosocial perspective about a patient that would otherwise be difficult to obtain through regularly scheduled medical follow-ups. Through this collaboration, the patient is more likely to feel nurtured and satisfied with their treatment.
To work towards such a practice as the standard of care, more health psychologists need to be trained in and recruited to work in gastroenterology. Furthermore, the value of multidisciplinary collaboration needs to be demonstrated to medical students and trainees to build the foundation for a medical model in which preventive care and mind-body treatments are regarded as key components in the treatment of functional disorders.
Finally, although we did not cover nursing self-management interventions in this paper, there are several studies supporting their benefit in mild to moderate IBS patients. Having nurses and nurse practitioners develop programs based on the evidence-based, nurse-led IBS self-management protocols developed at University of Washington86, 87, 88 and/or having nurses recommend and support the use of patient self-help books (such as “Master Your IBS: An 8-Week Plan Proven to Control the Symptoms of IBS” 89 or “Controlling IBS the Drug Free Way”90) could bridge existing gaps in psychosocial care for GI disorders.
RESOURCES
Clinical health psychology resources for patients and providers can be found through the following organizations: Society of Behavioral Medicine (www.sbm.org); Association for Behavioral and Cognitive Therapies (http://www.abct.org); International Foundation for Functional Disorders (www.iffgd.org); and “IBShypnosis.com” (http://ibshypnosis.com/). Patient-specific handouts related to functional and motility disorders can be accessed through the University of North Carolina's Functional GI and Motility Disorders website (https://www.med.unc.edu/ibs/patient-education/educational-gi-handouts).
Guarantor of the article: Sarah Ballou, PhD.
Specific author contributions: Drs Sarah Ballou and Laurie Keefer wrote and edited this narrative review.
Financial support: NIDDK Grant/Award Number: T32DK007760-17.
Potential competing interests: None.
References
- Zijdenbos IL, de Wit NJ, van der Heijden GJ et al. Psychological treatments for the management of irritable bowel syndrome. Cochrane Database Syst Rev 2009: (1): CD006442. [DOI] [PubMed]
- von Wietersheim J, Kessler H. Psychotherapy with chronic inflammatory bowel disease patients: a review. Inflamm Bowel Dis 2006; 12: 1175–1184. [DOI] [PubMed] [Google Scholar]
- Keohane J, O'Mahony C, O'Mahony L et al. Irritable bowel syndrome-type symptoms in patients with inflammatory bowel disease: a real association or reflection of occult inflammation? Am J Gastroenterol 2010; 105: 1788, 1789–1794 quiz 1795. [DOI] [PubMed] [Google Scholar]
- Fukuba N, Ishihara S, Tada Y et al. Prevalence of irritable bowel syndrome-like symptoms in ulcerative colitis patients with clinical and endoscopic evidence of remission: prospective multicenter study. Scand J Gastroenterol 2014; 49: 674–680. [DOI] [PubMed] [Google Scholar]
- Jonefjäll B, Strid H, Ohman L et al. Characterization of IBS-like symptoms in patients with ulcerative colitis in clinical remission. Neurogastroenterol Motil 2013; 25: 756–e578. [DOI] [PubMed] [Google Scholar]
- Beck AT. The past and future of cognitive therapy. J Psychother Pract Res 1997; 6: 276–284. [PMC free article] [PubMed] [Google Scholar]
- Hauser G, Pletikosic S, Tkalcic M. Cognitive behavioral approach to understanding irritable bowel syndrome. World J Gastroenterol 2014; 20: 6744–6758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lackner JM, Gudleski GD, Keefer L et al. Rapid response to cognitive behavior therapy predicts treatment outcome in patients with irritable bowel syndrome. Clin Gastroenterol Hepatol 2010; 8: 426–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lackner JM, Keefer L, Jaccard J et al. The Irritable Bowel Syndrome Outcome Study (IBSOS): rationale and design of a randomized, placebo-controlled trial with 12 month follow up of self- versus clinician-administered CBT for moderate to severe irritable bowel syndrome. Contemp Clin Trials 2012; 33: 1293–1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt MG, Moshier S, Milonova M. Brief cognitive-behavioral internet therapy for irritable bowel syndrome. Behav Res Ther 2009; 47: 797–802. [DOI] [PubMed] [Google Scholar]
- Moss-Morris R, McAlpine L, Didsbury LP et al. A randomized controlled trial of a cognitive behavioural therapy-based self-management intervention for irritable bowel syndrome in primary care. Psychol Med 2010; 40: 85–94. [DOI] [PubMed] [Google Scholar]
- van Dulmen AM, Fennis JF, Bleijenberg G. Cognitive-behavioral group therapy for irritable bowel syndrome: effects and long-term follow-up. Psychosom Med 1996; 58: 508–514. [DOI] [PubMed] [Google Scholar]
- Tonkin-Crine S, Bishop FL, Ellis M et al. Exploring patients' views of a cognitive behavioral therapy-based website for the self-management of irritable bowel syndrome symptoms. J Med Internet Res 2013; 15: e190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drossman DA, Toner BB, Whitehead WE et al. Cognitive-behavioral therapy versus education and desipramine versus placebo for moderate to severe functional bowel disorders. Gastroenterology 2003; 125: 19–31. [DOI] [PubMed] [Google Scholar]
- Kennedy T, Jones R, Darnley S et al. Cognitive behaviour therapy in addition to antispasmodic treatment for irritable bowel syndrome in primary care: randomised controlled trial. BMJ 2005; 331: 435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heymann-Mönnikes I, Arnold R, Florin I et al. The combination of medical treatment plus multicomponent behavioral therapy is superior to medical treatment alone in the therapy of irritable bowel syndrome. Am J Gastroenterol 2000; 95: 981–994. [DOI] [PubMed] [Google Scholar]
- Mahvi-Shirazi M, Fathi-Ashtiani A, Rasoolzade-Tabatabaei SK et al. Irritable bowel syndrome treatment: cognitive behavioral therapy versus medical treatment. Arch Med Sci 2012; 8: 123–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L, Xiong L, Zhang S et al. Cognitive-behavioral therapy for irritable bowel syndrome: a meta-analysis. J Psychosom Res 2014; 77: 1–12. [DOI] [PubMed] [Google Scholar]
- Hayee B, Forgacs I. Psychological approach to managing irritable bowel syndrome. BMJ 2007; 334: 1105–1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford AC, Talley NJ, Schoenfeld PS et al. Efficacy of antidepressants and psychological therapies in irritable bowel syndrome: systematic review and meta-analysis. Gut 2009; 58: 367–378. [DOI] [PubMed] [Google Scholar]
- Lackner JM, Jaccard J, Krasner SS et al. How does cognitive behavior therapy for irritable bowel syndrome work? A mediational analysis of a randomized clinical trial. Gastroenterology 2007; 133: 433–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craske MG, Wolitzky-Taylor KB, Labus J et al. A cognitive-behavioral treatment for irritable bowel syndrome using interoceptive exposure to visceral sensations. Behav Res Ther 2011; 49: 413–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boersma K, Ljotsson B, Edebol-Carlman H et al. Exposure-based cognitive behavioral therapy for irritable bowel syndrome. A single-case experimental design across 13 subjects. Cogn Behav Ther 2016; 10: 1–16. [DOI] [PubMed] [Google Scholar]
- Ljótsson B, Andersson E, Lindfors P et al. Prediction of symptomatic improvement after exposure-based treatment for irritable bowel syndrome. BMC Gastroenterol 2013; 13: 160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCombie AM, Mulder RT, Gearry RB. Psychotherapy for inflammatory bowel disease: A review and update. J Crohns Colitis 2013; 7: 935–949. [DOI] [PubMed] [Google Scholar]
- Knowles SR, Monshat K, Castle DJ. The efficacy and methodological challenges of psychotherapy for adults with inflammatory bowel disease: a review. Inflamm Bowel Dis 2013; 19: 2704–2715. [DOI] [PubMed] [Google Scholar]
- Mardini HE, Kip KE, Wilson JW. Crohn's disease: a two-year prospective study of the association between psychological distress and disease activity. Dig Dis Sci 2004; 49: 492–497. [DOI] [PubMed] [Google Scholar]
- Goodhand JR, Wahed M, Rampton DS. Management of stress in inflammatory bowel disease: a therapeutic option? Expert Rev Gastroenterol Hepatol 2009; 3: 661–679. [DOI] [PubMed] [Google Scholar]
- Díaz Sibaja MA, Comeche Moreno MI, Mas Hesse B. Protocolized cognitive-behavioural group therapy for inflammatory bowel disease. Rev Esp Enferm Dig 2007; 99: 593–598. [DOI] [PubMed] [Google Scholar]
- Boye B, Lundin KEA, Jantschek G et al. INSPIRE study: does stress management improve the course of inflammatory bowel disease and disease-specific quality of life in distressed patients with ulcerative colitis or Crohn's disease? A randomized controlled trial. Inflamm Bowel Dis 2011; 17: 1863–1873. [DOI] [PubMed] [Google Scholar]
- Szigethy E, Kenney E, Carpenter J et al. Cognitive-behavioral therapy for adolescents with inflammatory bowel disease and subsyndromal depression. J Am Acad Child Adolesc Psychiatry 2007; 46: 1290–1298. [DOI] [PubMed] [Google Scholar]
- Grootenhuis MA, Maurice-Stam H, Derkx BH et al. Evaluation of a psychoeducational intervention for adolescents with inflammatory bowel disease. Eur J Gastroenterol Hepatol 2009; 21: 340–345. [DOI] [PubMed] [Google Scholar]
- Timmer A, Preiss JC, Motschall E et al. Psychological interventions for treatment of inflammatory bowel disease. Cochrane Database Syst Rev 2011: 2: CD006913. [DOI] [PubMed] [Google Scholar]
- Szigethy E, Bujoreanu SI, Youk AO et al. Randomized efficacy trial of two psychotherapies for depression in youth with inflammatory bowel disease. J Am Acad Child Adolesc Psychiatry 2014; 53: 726–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hommel KA, Herzer M, Ingerski LM et al. Individually tailored treatment of medication nonadherence. J Pediatr Gastroenterol Nutr 2011; 53: 435–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keefer L, Doerfler B, Artz C. Optimizing management of Crohn's disease within a project management framework: results of a pilot study. Inflamm Bowel Dis 2012; 18: 254–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudacek KD. A review of the effects of hypnosis on the immune system in breast cancer patients: a brief communication. Int J Clin Exp Hypn 2007; 55: 411–425. [DOI] [PubMed] [Google Scholar]
- Horton-Hausknecht JR, Mitzdorf U, Melchart D. The effect of hypnosis therapy on the symptoms and disease activity in Rheumatoid Arthritis. Psychol Health 2000; 14: 1089–1104. [DOI] [PubMed] [Google Scholar]
- Bernardy K, Füber N, Klose P et al. Efficacy of hypnosis/guided imagery in fibromyalgia syndrome--a systematic review and meta-analysis of controlled trials. BMC Musculoskelet Disord 2011; 12: 133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen MP. Hypnosis for chronic pain management: a new hope. Pain 2009; 146: 235–237. [DOI] [PubMed] [Google Scholar]
- Whorwell PJ. Review article: the history of hypnotherapy and its role in the irritable bowel syndrome. Aliment Pharmacol Ther 2005; 22: 1061–1067. [DOI] [PubMed] [Google Scholar]
- Gholamrezaei A, Ardestani SK, Emami MH. Where does hypnotherapy stand in the management of irritable bowel syndrome? A systematic review. J Altern Complement Med 2006; 12: 517–527. [DOI] [PubMed] [Google Scholar]
- Gonsalkorale WM. Gut-directed hypnotherapy: the Manchester approach for treatment of irritable bowel syndrome. Int J Clin Exp Hypn 2006; 54: 27–50. [DOI] [PubMed] [Google Scholar]
- Palsson OS. Standardized hypnosis treatment for irritable bowel syndrome: the North Carolina protocol. Int J Clin Exp Hypn 2006; 54: 51–64. [DOI] [PubMed] [Google Scholar]
- Whorwell PJ, Prior A, Faragher EB. Controlled trial of hypnotherapy in the treatment of severe refractory irritable-bowel syndrome. Lancet Lond Engl 1984; 2: 1232–1234. [DOI] [PubMed] [Google Scholar]
- Whorwell PJ, Prior A, Colgan SM. Hypnotherapy in severe irritable bowel syndrome: further experience. Gut 1987; 28: 423–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whorwell PJ. Hypnotherapy: first line treatment for children with irritable bowel syndrome? Arch Dis Child 2013; 98: 243–244. [DOI] [PubMed] [Google Scholar]
- Whorwell PJ. Hypnotherapy for irritable bowel syndrome: the response of colonic and noncolonic symptoms. J Psychosom Res 2008; 64: 621–623. [DOI] [PubMed] [Google Scholar]
- Miller V, Carruthers HR, Morris J et al. Hypnotherapy for irritable bowel syndrome: an audit of one thousand adult patients. Aliment Pharmacol Ther 2015; 41: 844–855. [DOI] [PubMed] [Google Scholar]
- Palsson OS, Turner MJ, Johnson DA et al. Hypnosis treatment for severe irritable bowel syndrome: investigation of mechanism and effects on symptoms. Dig Dis Sci 2002; 47: 2605–2614. [DOI] [PubMed] [Google Scholar]
- Peters SL, Yao CK, Philpott H et al. Randomised clinical trial: the efficacy of gut-directed hypnotherapy is similar to that of the low FODMAP diet for the treatment of irritable bowel syndrome. Aliment Pharmacol Ther 2016; 44: 447–459. [DOI] [PubMed] [Google Scholar]
- Gonsalkorale WM, Miller V, Afzal A et al. Long term benefits of hypnotherapy for irritable bowel syndrome. Gut 2003; 52: 1623–1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahbazi K, Solati K, Hasanpour-Dehkordi A. Comparison of hypnotherapy and standard medical treatment alone on quality of life in patients with irritable bowel syndrome: a randomized control trial. J Clin Diagn Res 2016; 10: OC01–OC04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moser G, Trägner S, Gajowniczek EE et al. Long-term success of GUT-directed group hypnosis for patients with refractory irritable bowel syndrome: a randomized controlled trial. Am J Gastroenterol 2013; 108: 602–609. [DOI] [PubMed] [Google Scholar]
- Gerson CD, Gerson J, Gerson M-J. Group hypnotherapy for irritable bowel syndrome with long-term follow-up. Int J Clin Exp Hypn 2013; 61: 38–54. [DOI] [PubMed] [Google Scholar]
- Chiarioni G, Vantini I, De Iorio F et al. Prokinetic effect of gut-oriented hypnosis on gastric emptying. Aliment Pharmacol Ther 2006; 23: 1241–1249. [DOI] [PubMed] [Google Scholar]
- Whorwell PJ, Houghton LA, Taylor EE et al. Physiological effects of emotion: assessment via hypnosis. Lancet 1992; 340: 69–72. [DOI] [PubMed] [Google Scholar]
- Lea R, Houghton LA, Calvert EL et al. Gut-focused hypnotherapy normalizes disordered rectal sensitivity in patients with irritable bowel syndrome. Aliment Pharmacol Ther 2003; 17: 635–642. [DOI] [PubMed] [Google Scholar]
- Gonsalkorale WM, Toner BB, Whorwell PJ. Cognitive change in patients undergoing hypnotherapy for irritable bowel syndrome. J Psychosom Res 2004; 56: 271–278. [DOI] [PubMed] [Google Scholar]
- Gonsalkorale WM, Houghton LA, Whorwell PJ. Hypnotherapy in irritable bowel syndrome: a large-scale audit of a clinical service with examination of factors influencing responsiveness. Am J Gastroenterol 2002; 97: 954–961. [DOI] [PubMed] [Google Scholar]
- Rainville P, Duncan GH, Price DD et al. Pain affect encoded in human anterior cingulate but not somatosensory cortex. Science 1997; 277: 968–971. [DOI] [PubMed] [Google Scholar]
- Lowén MBO, Mayer EA, Sjöberg M et al. Effect of hypnotherapy and educational intervention on brain response to visceral stimulus in the irritable bowel syndrome. Aliment Pharmacol Ther 2013; 37: 1184–1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mawdsley JE, Jenkins DG, Macey MG et al. The effect of hypnosis on systemic and rectal mucosal measures of inflammation in ulcerative colitis. Am J Gastroenterol 2008; 103: 1460–1469. [DOI] [PubMed] [Google Scholar]
- Keefer L, Taft TH, Kiebles JL et al. Gut-directed hypnotherapy significantly augments clinical remission in quiescent ulcerative colitis. Aliment Pharmacol Ther 2013; 38: 761–771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller V, Whorwell PJ. Treatment of inflammatory bowel disease: a role for hypnotherapy? Int J Clin Exp Hypn 2008; 56: 306–317. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full Catastrophe Living: Using The Wisdom Of Your Body And Mind To Face Stress, Pain, And Illness. Bantam Doubleday Dell Publishing: New York, NY, USA, 1990. [Google Scholar]
- Lakhan SE, Schofield KL. Mindfulness-based therapies in the treatment of somatization disorders: a systematic review and meta-analysis. PLoS One 2013; 8: e71834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiesa A, Serretti A. Mindfulness based cognitive therapy for psychiatric disorders: a systematic review and meta-analysis. Psychiatry Res 2011; 187: 441–453. [DOI] [PubMed] [Google Scholar]
- Gaylord SA, Whitehead WE, Coble RS et al. Mindfulness for irritable bowel syndrome: protocol development for a controlled clinical trial. BMC Complement Altern Med 2009; 9: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Gaylord SA, Palsson O et al. Therapeutic mechanisms of a mindfulness-based treatment for IBS: effects on visceral sensitivity, catastrophizing, and affective processing of pain sensations. J Behav Med 2012; 35: 591–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaylord SA, Palsson OS, Garland EL et al. Mindfulness training reduces the severity of irritable bowel syndrome in women: results of a randomized controlled trial. Am J Gastroenterol 2011; 106: 1678–1688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zernicke KA, Campbell TS, Blustein PK et al. Mindfulness-based stress reduction for the treatment of irritable bowel syndrome symptoms: a randomized wait-list controlled trial. Int J Behav Med 2013; 20: 385–396. [DOI] [PubMed] [Google Scholar]
- Ljótsson B, Falk L, Vesterlund AW et al. Internet-delivered exposure and mindfulness based therapy for irritable bowel syndrome--a randomized controlled trial. Behav Res Ther 2010; 48: 531–539. [DOI] [PubMed] [Google Scholar]
- Ljótsson B, Hedman E, Andersson E et al. Internet-delivered exposure-based treatment vs. stress management for irritable bowel syndrome: a randomized trial. Am J Gastroenterol 2011; 106: 1481–1491. [DOI] [PubMed] [Google Scholar]
- Neilson K, Ftanou M, Monshat K et al. A controlled study of a group mindfulness intervention for individuals living with inflammatory bowel disease. Inflamm Bowel Dis 2016; 22: 694–701. [DOI] [PubMed] [Google Scholar]
- Jedel S, Hoffman A, Merriman P et al. A randomized controlled trial of mindfulness-based stress reduction to prevent flare-up in patients with inactive ulcerative colitis. Digestion 2014; 89: 142–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berrill JW, Sadlier M, Hood K et al. Mindfulness-based therapy for inflammatory bowel disease patients with functional abdominal symptoms or high perceived stress levels. J Crohns Colitis 2014; 8: 945–955. [DOI] [PubMed] [Google Scholar]
- Svedlund J, Sjödin I, Ottosson JO et al. Controlled study of psychotherapy in irritable bowel syndrome. Lancet Lond Engl 1983; 2: 589–592. [DOI] [PubMed] [Google Scholar]
- Guthrie E, Creed F, Dawson D et al. A controlled trial of psychological treatment for the irritable bowel syndrome. Gastroenterology 1991; 100: 450–457. [DOI] [PubMed] [Google Scholar]
- Guthrie E, Creed F, Dawson D et al. A randomised controlled trial of psychotherapy in patients with refractory irritable bowel syndrome. Br J Psychiatry 1993; 163: 315–321. [DOI] [PubMed] [Google Scholar]
- Creed F, Fernandes L, Guthrie E et al. The cost-effectiveness of psychotherapy and paroxetine for severe irritable bowel syndrome. Gastroenterology 2003; 124: 303–317. [DOI] [PubMed] [Google Scholar]
- Creed F, Guthrie E, Ratcliffe J et al. Reported sexual abuse predicts impaired functioning but a good response to psychological treatments in patients with severe irritable bowel syndrome. Psychosom Med 2005; 67: 490–499. [DOI] [PubMed] [Google Scholar]
- Keller W, Pritsch M, Von Wietersheim J et al. Effect of psychotherapy and relaxation on the psychosocial and somatic course of Crohn's disease: main results of the German Prospective Multicenter Psychotherapy Treatment study on Crohn's Disease. J Psychosom Res 2004; 56: 687–696. [DOI] [PubMed] [Google Scholar]
- Mawdsley JE, Rampton DS. Psychological stress in IBD: new insights into pathogenic and therapeutic implications. Gut 2005; 54: 1481–1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollander D. Inflammatory bowel diseases and brain-gut axis. J Physiol Pharmacol 2003; 54 ((Suppl 4)): 183–190. [PubMed] [Google Scholar]
- Heitkemper MM, Jarrett ME, Levy RL et al. Self-management for women with irritable bowel syndrome. Clin Gastroenterol Hepatol 2004; 2: 585–596. [DOI] [PubMed] [Google Scholar]
- Jarrett ME, Cain KC, Burr RL et al. Comprehensive self-management for irritable bowel syndrome: randomized trial of in-person vs. combined in-person and telephone sessions. Am J Gastroenterol 2009; 104: 3004–3014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zia JK, Barney P, Cain KC et al. A comprehensive self-management irritable bowel syndrome program produces sustainable changes in behavior after 1 year. Clin Gastroenterol Hepatol 2016; 14: 212–219-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barney P Master Your IBS: An 8-week Plan To Control The Symptoms Of Irritable Bowel Syndrome. AGA Press: Bethesda, MD, USA, 2010, pp 229..
- Lackner JM Controlling IBS The Drug-free Way: A 10-step Plan For Symptom Relief. Stewart, Tabori & Chang: New York, 2007, p 256.