Abstract
Falling significantly affects quality of life, morbidity, and mortality among older adults. We sought to evaluate the prospective association between sedentary time, physical activity, and falling among post-menopausal women aged 50–79 y recruited to the Women's Health Initiative Observational Study between 1993 and 1998 from 40 clinical centers across the United States. Baseline (B) and change in each of the following were evaluated at year 3 (Y3) and year 6 (Y6; baseline n=93,676; Y3 n=76,598; Y6 n=75,428): recreational physical activity (MET-h/wk), sitting, sleeping (min/d), and lean body mass by dual energy X-ray absorptiometry (subset N=6,475). Falls per year (0, 1, 2, ≥3) were assessed annually by self-report questionnaire and then dichotomized as ≤1 and ≥2 falls/year. Logistic regression models were adjusted for demographics, body mass index, fall history, tobacco and alcohol use, medical conditions, and medications. Higher baseline activity was associated with greater risk of falling at Y6 (18%; p for trend <0.0001). Increasing sedentary time minimally decreased falling (1% Y3; 2% Y6; p<0.05). Increasing activity up to ≥ 9 MET-h/wk (OR: 1.12, 95%CI: 1.03-1.22) or maintaining ≥ 9 MET-h/wk (OR: 1.20, 95% CI: 1.13-1.29) increased falling at Y3 and Y6 (p for trend <0.001). Adding lean body mass to the models attenuated these relationships. Physically active lifestyles increased falling among post-menopausal women. Additional fall prevention strategies, such as balance and resistance training, should be evaluated to assist post-menopausal women in reaching or maintaining levels of aerobic activity known to prevent and manage several chronic diseases.
Keywords: accidental falls, falls, exercise, menopause, sedentary lifestyle
Introduction
The propensity to fall increases with aging, often due to other age related issues, such as impaired vision, balance, and mental acuity (Rubenstein, 2006). Although many falls result in minor injuries, approximately 10% will result in fractures which are associated with significant morbidity and mortality in the aged (Gillespie et al., 2012). Reductions in falls among community dwelling older adults engaging exercise interventions offers hope (Gillespie et al., 2012), as does the protection against fracture with higher baseline physical activity demonstrated in the Women's Health Initiative (WHI) (Robbins et al., 2007), but overall, the association between physical activity and falls in the literature has been inconsistent (Clarke et al., 2015). Physical activity patterns over time may prove to be more predictive of falls than exercise interventions or assessment of physical activity at a single time point. Longitudinal changes in physical activity and body composition, which may mediate the falls benefit of physical activity through preservation of muscle mass (LaStayo et al., 2003), are needed to better understand their independent and joint roles in falls risk. However, because prospective studies on older adults typically do not have repeated prospective measures on these factors, they have yet to be fully explored with respect to incidence of falling.
In the United States, physical activity decreases dramatically in adulthood, stabilizing at relatively low levels in middle aged women (Caspersen et al., 2000). Low levels of physical activity have been associated with decreased muscle mass (Morley et al., 2001). Meanwhile, sedentary time, distinctly different than insufficient moderate to vigorous physical activity (Owen et al., 2010), increases with aging (Clark et al., 2010). High sedentary time may also aid in skeletal muscle decline and has been shown to be a risk factor for falling in studies with 1-2 years follow-up (Thibaud et al., 2012).
We sought to determine whether prospectively assessed physical activity patterns, including sedentary time, are associated with the risk of falling over several years and whether risk of falling is mediated by body composition. We hypothesized that decreasing physical activity over time would be associated with increased risk of falling among postmenopausal women (Figure 1). High sedentary time was also hypothesized to increase risk of falling.
Figure 1.
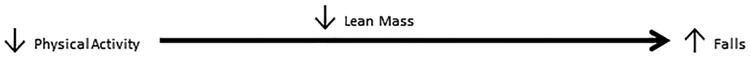
Hypothesized mediation model among participants in the Women's Health Initiative Observational Study recruited between 1993 and 1998 from 40 clinical centers across the United States (n=93,676)
Methods
Study Population
The WHI Study recruited postmenopausal women aged 50-79 y at 40 WHI clinical centers across the United States between 1993 and 1998 to four clinical trials and an observational study (1998; Hays et al., 2003). Only women enrolled in the observational study were included in this analysis (N=93,676); body composition was measured in those enrolled at the Pittsburgh, PA; Birmingham, AL; and Tucson-Phoenix, AZ sites (N=6,475) (Chen et al., 2008). The protocol and consent forms were approved by each institutional review board at each site and all participants provided written informed consent. For the present study, measurements taken at baseline, year 3 and year 6 of follow-up were used. The average follow-up time for incident falls in this study was 54 months.
Physical Activity Assessment
The frequency, intensity, and duration of walking, as well as moderate and vigorous recreational physical activity, were assessed using a reliable and valid questionnaire. Test-retest reliability was 0.67 - 0.71 (weighted κ coefficient) for individual physical activity variables on the WHI questionnaire and the questionnaire assessed activity levels correlated well with accelerometry (r=0.73) in a subset of the WHI. (Eaglehouse et al., 2016; Johnson-Kozlow et al., 2007; Langer et al., 2003; Manson et al., 2002; Meyer et al., 2009; Nguyen et al., 2013). Energy expenditure (MET-h/wk) was computed, as previously published (Ainsworth et al., 2000; Sims et al., 2012).
Based on the continuous physical activity data, 4 categories of baseline physical activity were created: no physical activity (0 MET-h/wk), ≤ 3 MET-h/wk, 3.1 to 8.9 MET-h/wk, and ≥ 9 MET-h/wk. Participants were classified as physically inactive (0 MET-h/wk), insufficiently active (>0 to < 9 MET-h/wk), and active (≥ 9 MET-h/wk of moderate-vigorous intensity physical activity) in approximate alignment with recommended physical activity levels (2008). Change in physical activity from baseline to year 3 and year 6 was categorized as follows.
change/inactive: remaining in the inactive or insufficiently active category at baseline and follow-up
increased activity: inactive or insufficiently active at baseline, but increased to ≥ 9 MET-h/wk at follow-up
active maintainer: maintained ≥ 9 MET-h/wk at baseline and follow-up
decreased/inactive: decreased physical activity categories from sufficiently active to insufficiently active or inactive, or decreased from insufficiently active to inactive category
Sedentary time was quantified separately by two questions in the questionnaire that asked how much time was spent sitting per day and lying down per day (hrs/d). Sedentary time is not equivalent to the inactive or insufficiently active terms above.
Anthropometry and Body Composition Assessment
Height and weight were measured without shoes on a wall-mounted stadiometer to the nearest 0.1 cm and balance-beam scale to the nearest 0.1 kg, respectively. BMI was calculated as weight (kg)/height (m)2. Body composition was determined by performing dual energy X-ray absorptiometry scans (DXA; QDR2000, 2000+, or 4500W; Hologic Inc, Bedford, MA) at 3 WHI clinical centers (Pittsburgh, PA; Birmingham, AL; and Tucson-Phoenix, AZ), each using the rigorous WHI quality assurance program (Chen et al., 2005). Measurements included both whole body and regional bone mineral density, lean body mass, and fat mass. Calibration equations were developed when an older DXA machine was replaced with a newer model (QDR2000 to QDR4500W) (Chen et al., 2005). Participants who completed the baseline and at least year 3 or year 6 follow-up visits were included in this analysis.
Assessment of Falls
A self-report medical history questionnaire that included the following question was collected at baseline and by mail annually: “During the past 12months, how many times did you fall and land on the floor or ground: none, 1 time, 2 times, 3 or more times?” Participants were asked not to include falls due to sports activities such as snow- or water-skiing or horseback riding.(Anderson et al., 2003)
Assessment of Covariates
Years since menopause were determined by last reported menstrual bleeding, time of bilateral oophorectomy, or initiation of menopausal hormone therapy. Self-report questionnaires were used to obtain information on demographics, medical history, medications, smoking and alcohol use, and prior hormone therapy use at baseline. Diet and physical function were assessed by a validated food frequency questionnaire (Block et al., 1990) and the Medical Outcomes Study Scale (Ware and Sherbourne, 1992), respectively.
Statistical Analysis
Descriptive statistics were computed and tests for significant differences were performed using analysis of variance (ANOVA) for continuous variables and Chi Squared tests for categorical variables. Logistic regression models were developed to determine the odds of falling based on baseline physical activity category and sedentary time, as well as change in physical activity (categories and continuous) over three and six years. In alignment with a prior WHI publications, (Bea et al., 2011; Cauley et al., 2007; Chen et al., 2004) a binary variable of ≥2 falls per year was used for risk of falling in all models. A history of ≥2 falls per year is a significant predictor of a recurrent faller (Stalenhoef et al., 2002) and higher fall rates are associated with frailty related fractures (Schwartz et al., 2005). Factors that have been associated with falling and body composition in the literature were selected a priori as covariates, including age, BMI, ethnicity, education, years since menopause, tobacco and alcohol use, number of falls at baseline, diabetes, hypertension, fainting, general health, physical function, and medication use including hormone therapy, beta blocker, antianxiety agent, hypnotic, narcotic, and sedative use. Geographic region, by latitude of the responsible clinical center at the time of enrollment, waist circumference, and total body fat did not significantly affect the models, so were not included. Exclusions included those with prior stroke, peripheral artery disease, multiple sclerosis, and Parkinson's Disease, or missing covariates. Change in activity models were stratified by body mass index (BMI ≥ 30kg/m2) due to previous associations with falls (Beck et al., 2009).
Results
Overall, the mean physical activity level for the cohort was 13.7 (±14.4) MET-h/wk at baseline, 13.6 (±14.6) MET-h/wk at year 3, and 13.1 (±14.2) MET-h/wk at year 6. The change in physical activity across the cohort was -0.4 (±12.4) MET-h/wk from baseline to year 3 and -0.9 (±13.5) MET-h/wk from baseline to year 6. Total sedentary time (hrs/d spent sitting or sleeping) was 15.0 (±4.2) hrs/d at baseline, 14.7 (±3.7) hrs/d at year 3 and 14.7(±3.8) hrs/d at year 6. Inactive time was reduced by -0.38 (±3.9) from baseline to year 3 and remained stable at year 6.
Baseline activity levels varied by race/ethnicity, highest level of education, years postmenopausal, and baseline fall history. There were more obese individuals in the inactive group. The less-active and non-active groups were more likely to report medical conditions, medication use, smoking, and lower alcohol consumption compared to others. Women in the highest category of physical activity had the highest lean mass at baseline (Table 1) and follow-up, however, they decreased physical activity and lost greater absolute appendicular lean mass over time compared to others (Table 2).
Table 1.
Baseline demographic and medical history characteristics by physical activity group among participants in the Women's Health Initiative Observational Study recruited between 1993 and 1998 from 40 clinical centers across the United States (n=93,676)
| 0METs (N=12,636) | >0-3METs (N=9,954) | 3.1-8.9METs (N=21,192) | ≥9METs (N=48,843) | p-value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | |||
| Age group at screening | 50-59 | 4215 | 33.36 | 3142 | 31.57 | 6610 | 31.19 | 15411 | 31.55 | <0.001 |
| 60-69 | 5341 | 42.27 | 4323 | 43.43 | 9147 | 43.16 | 21925 | 44.89 | . | |
| 70-79 | 3080 | 24.37 | 2489 | 25.01 | 5435 | 25.65 | 11507 | 23.56 | . | |
| Race/ ethnicity | White | 9707 | 76.82 | 7823 | 78.59 | 17456 | 82.37 | 42223 | 86.45 | <0.001 |
| Black | 1612 | 12.76 | 1132 | 11.37 | 1874 | 8.84 | 2943 | 6.03 | . | |
| Hispanic | 692 | 5.48 | 492 | 4.94 | 868 | 4.10 | 1423 | 2.91 | . | |
| American Indian | 80 | 0.63 | 63 | 0.63 | 94 | 0.44 | 179 | 0.37 | . | |
| Asian/Pacific Islander | 351 | 2.78 | 300 | 3.01 | 580 | 2.74 | 1422 | 2.91 | . | |
| Unknown | 194 | 1.54 | 144 | 1.45 | 320 | 1.51 | 653 | 1.34 | . | |
| Education | 0-8 years | 386 | 3.08 | 234 | 2.37 | 380 | 1.81 | 476 | 0.98 | <0.001 |
| Some high school | 766 | 6.11 | 519 | 5.26 | 836 | 3.98 | 1116 | 2.30 | . | |
| High school diploma/GED | 2841 | 22.67 | 1993 | 20.18 | 3745 | 17.82 | 6370 | 13.15 | . | |
| School after high school | 4817 | 38.44 | 3875 | 39.24 | 7875 | 37.46 | 16999 | 35.09 | . | |
| College degree or higher | 3722 | 29.70 | 3255 | 32.96 | 8184 | 38.93 | 23484 | 48.48 | . | |
| Years | < 10 yrs | 3539 | 29.46 | 2712 | 28.72 | 6086 | 29.90 | 14849 | 31.39 | <0.001 |
| menopausal | >=10 yrs | 8472 | 70.54 | 6730 | 71.28 | 14266 | 70.10 | 32453 | 68.61 | . |
| Smoking status | Never | 6332 | 50.68 | 5198 | 52.96 | 11077 | 52.84 | 24026 | 49.76 | <0.001 |
| Past | 4878 | 39.04 | 3769 | 38.40 | 8422 | 40.17 | 22134 | 45.84 | . | |
| Current | 1284 | 10.28 | 848 | 8.64 | 1466 | 6.99 | 2128 | 4.41 | . | |
| Alcohol intake | Non Drinker | 7028 | 55.71 | 5111 | 51.42 | 9327 | 44.06 | 17292 | 35.45 | <0.001 |
| <= 1 drink/day | 4437 | 35.17 | 3913 | 39.37 | 9522 | 44.98 | 24292 | 49.80 | . | |
| > 1 drink/day | 1150 | 9.12 | 915 | 9.21 | 2319 | 10.96 | 7200 | 14.76 | . | |
| Treated diabetes (pills or shots) | No | 11797 | 93.50 | 9285 | 93.43 | 20191 | 95.40 | 47383 | 97.12 | <0.001 |
| Yes | 820 | 6.50 | 653 | 6.57 | 973 | 4.60 | 1403 | 2.88 | . | |
| History of hypertension | Never hypertensive | 7454 | 59.71 | 5937 | 60.31 | 13410 | 63.95 | 34250 | 70.68 | <0.001 |
| Untreated hypertensive | 1123 | 9.00 | 826 | 8.39 | 1742 | 8.31 | 3613 | 7.46 | . | |
| Treated hypertensive | 3906 | 31.29 | 3081 | 31.30 | 5816 | 27.74 | 10595 | 21.86 | . | |
| Hormone Therapy use | Never used | 5635 | 44.63 | 4502 | 45.26 | 8875 | 41.91 | 18527 | 37.97 | <0.001 |
| Past user | 1924 | 15.24 | 1497 | 15.05 | 3190 | 15.06 | 7147 | 14.65 | . | |
| Current user | 5067 | 40.13 | 3948 | 39.69 | 9110 | 43.02 | 23122 | 47.39 | . | |
| Beta blockers use | No | 11399 | 90.21 | 9025 | 90.67 | 19174 | 90.48 | 45422 | 93.00 | <0.001 |
| Yes | 1237 | 9.79 | 929 | 9.33 | 2017 | 9.52 | 3421 | 7.00 | . | |
| Antianxiety agents use | No | 12035 | 95.24 | 9531 | 95.75 | 20387 | 96.21 | 47423 | 97.09 | <0.001 |
| Yes | 601 | 4.76 | 423 | 4.25 | 804 | 3.79 | 1420 | 2.91 | . | |
| Hypnotics use | No | 12197 | 96.53 | 9652 | 96.97 | 20578 | 97.11 | 47612 | 97.48 | <0.001 |
| Yes | 439 | 3.47 | 302 | 3.03 | 613 | 2.89 | 1231 | 2.52 | . | |
| Narcotics use | No | 12167 | 96.29 | 9651 | 96.96 | 20732 | 97.83 | 48115 | 98.51 | <0.001 |
| Yes | 469 | 3.71 | 303 | 3.04 | 459 | 2.17 | 728 | 1.49 | . | |
| Sedative use | No | 12501 | 98.93 | 9854 | 99.00 | 21015 | 99.17 | 48458 | 99.21 | 0.007 |
| Yes | 135 | 1.07 | 100 | 1.00 | 176 | 0.83 | 385 | 0.79 | . | |
| Fainted, last 12 months | No | 12157 | 97.05 | 9599 | 97.28 | 20507 | 97.44 | 47406 | 97.64 | 0.001 |
| Yes | 369 | 2.95 | 268 | 2.72 | 539 | 2.56 | 1144 | 2.36 | . | |
| Prior falls, last 12 months | None | 8390 | 66.87 | 6585 | 66.50 | 14184 | 67.35 | 33297 | 68.51 | <0.001 |
| 1 time | 2498 | 19.91 | 1988 | 20.08 | 4253 | 20.19 | 9524 | 19.60 | . | |
| 2 times | 1023 | 8.15 | 858 | 8.66 | 1787 | 8.48 | 3851 | 7.92 | . | |
| 3 or more times | 635 | 5.06 | 471 | 4.76 | 837 | 3.97 | 1930 | 3.97 | . | |
| Physical function > 90 | No | 9585 | 77.64 | 7463 | 76.60 | 14252 | 68.40 | 25128 | 52.28 | <0.001 |
| Yes | 2760 | 22.36 | 2280 | 23.40 | 6584 | 31.60 | 22935 | 47.72 | . | |
| Body Mass Index (kg/m2), baseline | <25 | 3376 | 27.12 | 2881 | 29.24 | 7744 | 36.95 | 23408 | 48.48 | <0.001 |
| 25 - <30 | 3988 | 32.03 | 3268 | 33.17 | 7461 | 35.60 | 16408 | 33.99 | . | |
| >=30 | 5085 | 40.85 | 3704 | 37.59 | 5755 | 27.46 | 8464 | 17.53 | . | |
| Body composition | Mean | SD | Mean | SD | Mean | SD | Mean | SD | p-value | |
| Whole body lean mass (%) | 54.60 | 7.42 | 54.06 | 6.88 | 56.25 | 7.29 | 58.70 | 7.34 | <0.001 | |
| Appendicular lean mass (kg) | 15.05 | 2.98 | 14.83 | 3.12 | 14.47 | 2.85 | 14.26 | 2.46 | <0.001 | |
| Activity | ||||||||||
| Total Physical activity, (MET-hrs/wk) | 0.00 | 0.00 | 1.62 | 0.69 | 5.72 | 1.74 | 23.15 | 13.94 | <0.001 | |
| Time spent sitting (hrs/d) | 7.94 | 3.72 | 7.57 | 3.43 | 7.40 | 3.36 | 6.87 | 3.19 | <0.001 | |
| Time spent sleeping (hrs/d) | 7.76 | 2.60 | 7.79 | 2.47 | 7.83 | 2.33 | 7.92 | 2.18 | <0.001 | |
Table 2.
Change in lean body mass, energy expenditure and physical activity from baseline to years three and six of follow-up by physical activity group among participants in the Women's Health Initiative Observational Study recruited between 1993 and 1998 from 40 clinical centers across the United States (n=93,676)
| Inactive 0 METs | (>0-3) METs | (3.1- 8.9) METs | >= 9 METS | p-value | |||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||
| Change from Baseline to Year 3 | |||||||||
| Whole body lean mass (%) | -0.46 | 3.19 | -0.37 | 3.31 | -0.60 | 3.18 | -0.87 | 3.17 | <0.001 |
| Appendicular lean mass (kg) | -0.60 | 3.19 | -0.41 | 3.21 | -0.74 | 3.26 | -1.17 | 3.47 | <0.001 |
| Physical activity, (MET-hrs/wk) | 3.54 | 7.13 | 3.56 | 7.51 | 2.56 | 8.61 | -3.29 | 14.58 | <0.001 |
| Time spent sitting (hrs/d) | -0.49 | 3.41 | -0.48 | 3.25 | -0.45 | 3.17 | -0.37 | 3.01 | <0.001 |
| Time spent sleeping (hrs/d) | 0.19 | 2.62 | 0.13 | 2.56 | 0.05 | 2.39 | -0.04 | 2.23 | <0.001 |
| Change from Baseline to Year 6 | |||||||||
| Whole body lean mass (%) | -0.23 | 4.43 | -0.06 | 3.89 | -0.55 | 3.87 | -1.02 | 3.85 | <0.001 |
| Appendicular lean mass (kg) | -1.13 | 4.16 | -1.02 | 3.31 | -1.27 | 3.67 | -2.23 | 3.78 | <0.001 |
| Physical activity, (MET-hrs/wk) | 4.27 | 7.84 | 4.25 | 8.49 | 2.84 | 9.62 | -4.71 | 15.32 | <0.001 |
| Time spent sitting (hrs/d) | -0.53 | 3.68 | -0.57 | 3.46 | -0.53 | 3.35 | -0.42 | 3.20 | <0.001 |
| Time spent sleeping (hrs/d) | 0.25 | 2.69 | 0.22 | 2.54 | 0.13 | 2.45 | 0.03 | 2.27 | <0.001 |
Overall, the risk of falling was significantly increased (18%) over six, but not three years of follow up among those with ≥9MET-h/wk of physical activity at baseline compared to being inactive at baseline (p for trend < 0.001; Table 3). However, when stratified on BMI, the non-obese women were at 12% greater risk of falling over three years if they were active as compared to their inactive counterparts (p for trend = 0.04).
Table 3.
Baseline physical activity and falling at years three and six among participants in the Women's Health Initiative Observational Study recruited between 1993 and 1998 from 40 clinical centers across the United States (n=93,676)
| Non-Fallers | Fallers* | Odds Ratio | 95% CI | p value | ||
|---|---|---|---|---|---|---|
| Three Years Follow-up | ||||||
| All | 0METs | 8871 | 1034 | . | . . | . |
| >0-3METs | 7041 | 860 | 0.95 | (0.86, 1.05) | 0.02 | |
| 3.1- 8.9METs | 15689 | 1757 | 0.95 | (0.87, 1.03) | . | |
| ≥9METS | 37886 | 3460 | 1.04 | (0.96, 1.12) | . | |
| BMI≥30 | 0METs | 3482 | 458 | . | . . | . |
| >0-3METs | 2510 | 383 | 0.85 | (0.73, 0.99) | 0.10 | |
| 3.1- 8.9METs | 4048 | 568 | 0.86 | (0.75, 0.99) | . | |
| ≥9METS | 6143 | 751 | 0.93 | (0.81, 1.06) | . | |
| BMI<30 | 0METs | 5389 | 576 | . | . . | . |
| >0-3METs | 4531 | 477 | 1.04 | (0.91, 1.18) | 0.04 | |
| 3.1- 8.9METs | 11641 | 1189 | 1.02 | (0.91, 1.14) | . | |
| ≥9METS | 31743 | 2709 | 1.12 | (1.01, 1.24) | . | |
| Six Years Follow-up | ||||||
| All | 0METs | 8556 | 1085 | . | . . | . |
| >0-3METs | 6843 | 859 | 1.01 | (0.92, 1.12) | <0.001 | |
| 3.1- 8.9METs | 15389 | 1735 | 1.04 | (0.95, 1.13) | . | |
| ≥9METS | 37579 | 3382 | 1.18 | (1.09, 1.27) | . | |
| BMI≥30 | 0METs | 3332 | 510 | . | . . | . |
| >0-3METs | 2470 | 347 | 1.11 | (0.95, 1.29) | 0.12 | |
| 3.1- 8.9METs | 3995 | 523 | 1.10 | (0.96, 1.26) | . | |
| ≥9METS | 6126 | 712 | 1.17 | (1.03, 1.34) | . | |
| BMI<30 | 0METs | 5224 | 575 | . | . . | . |
| >0-3METs | 4373 | 512 | 0.95 | (0.84, 1.09) | <0.001 | |
| 3.1- 8.9METs | 11394 | 1212 | 1.00 | (0.90, 1.12) | . | |
| ≥9METS | 31453 | 2670 | 1.16 | (1.05, 1.28) | . | |
Faller≥2falls per year. All models were adjusted for age, BMI (Body Mass Index), ethnicity, education, years since menopause, smoking, alcohol, number of falls at baseline, diabetes, hypertension, fainted, general health, hormone status, Beta blocker, Antianxiety agents, Hypnotics, narcotics, sedatives, physical function >= 90.
The odds of falling increased by 1% with increased walking at both three and six years (p=0.02) and increased vigorous activity at three, but not at six years, when evaluating change in activity as a continuous variable. Increased sitting slightly decreased falls over 6 years (OR: 0.98, 95%CI: 0.98-0.99, p<0.001), while time spent lying down decreased odds of falling by 2% and 3% at three and six years, respectively (p<0.001). Stratification by obesity did not significantly affect these results (data not shown).
In categorical analyses, increased or maintained adequate physical activity (≥9MET-h/wk) significantly increased odds of falling, by 12% and 20%, respectively, compared to those that remained inactive between baseline and year three (Table 4; p for trend <0.001). Models stratified by obesity were consistent with results from the entire cohort. After 6 years, the odds of falling increased to 30% for those that maintained a physically active lifestyle overall (p for trend <0.001), but 36% among the non-obese (p for trend <0.001).
Table 4.
Odds falling based on change in physical activity (METs/wk) categories among participants in the Women's Health Initiative Observational Study recruited between 1993 and 1998 from 40 clinical centers across the United States (n=93,676)
| Base Model | Change in % Lean Body Mass Adjusted | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Non-Fallers | Fallers* | OR 95% CI | p value | Non-Fallers | Fallers* | OR 95% CI | p value | ||
| Baseline to Year 3 | |||||||||
| All | No change/ Inactive | 22466 | 2721 | . . . | . | 1528 | 185 | . . . | . |
| Increase | 7711 | 774 | 1.12 (1.02, 1.22) | <0.001 | 481 | 41 | 1.35 (0.93, 1.97) | 0.010 | |
| Active maintainer | 28003 | 2281 | 1.21 (1.13, 1.29) | . | 1362 | 120 | 1.16 (0.88, 1.52) | . | |
| Decrease | 8929 | 1066 | 0.95 (0.88, 1.03) | . | 538 | 82 | 0.73 (0.54, 0.98) | . | |
| BMI≥30 | No change/ Inactive | 7560 | 1100 | . . . | . | 500 | 78 | . . . | . |
| Increase | 1878 | 237 | 1.13 (0.96, 1.32) | 0.03 | 126 | 13 | 1.44 (0.74, 2.81) | 0.60 | |
| Active maintainer | 3777 | 415 | 1.15 (1.01, 1.30) | . | 192 | 28 | 0.93 (0.56, 1.54) | . | |
| Decrease | 2126 | 313 | 0.92 (0.80, 1.07) | . | 126 | 19 | 0.84 (0.47, 1.52) | . | |
| BMI<30 | No change/ Inactive | 14906 | 1621 | . . . | . | 1020 | 106 | . . . | . |
| Increase | 5833 | 537 | 1.12 (1.00, 1.24) | <0.001 | 351 | 28 | 1.33 (0.83, 2.12) | 0.006 | |
| Active maintainer | 24226 | 1866 | 1.23 (1.14, 1.33) | . | 1160 | 90 | 1.23 (0.88, 1.71) | . | |
| Decrease | 6803 | 753 | 0.96 (0.87, 1.06) | . | 408 | 62 | 0.66 (0.46, 0.95) | . | |
| Baseline to Year 6 | |||||||||
| All | No change/Inactive | 20943 | 2588 | . . . | . | 1312 | 157 | . . . | . |
| Increase | 8278 | 841 | 1.11 (1.02, 1.21) | <0.001 | 434 | 44 | 1.04 (0.72, 1.51) | 0.72 | |
| Active maintainer | 25906 | 2007 | 1.30 (1.22, 1.39) | . | 1136 | 92 | 1.19 (0.88, 1.60) | . | |
| Decrease | 10543 | 1218 | 1.03 (0.95, 1.11) | . | 567 | 68 | 1.03 (0.74, 1.42) | . | |
| BMI≥30 | No change/Inactive | 6979 | 1006 | . . . | . | 424 | 62 | . . . | . |
| Increase | 2127 | 273 | 1.04 (0.90, 1.21) | 0.30 | 125 | 11 | 1.51 (0.74, 3.08) | 0.65 | |
| Active maintainer | 3361 | 369 | 1.12 (0.98, 1.28) | . | 146 | 16 | 1.18 (0.63, 2.22) | . | |
| Decrease | 2472 | 309 | 1.11 (0.96, 1.28) | . | 148 | 22 | 0.94 (0.53, 1.67) | . | |
| BMI<30 | No change/ Inactive | 13964 | 1582 | . . . | . | 876 | 94 | . . . | . |
| Increase | 6151 | 568 | 1.15 (1.03, 1.27) | <0.001 | 308 | 33 | 0.91 (0.58, 1.41) | 0.72 | |
| Active maintainer | 22545 | 1638 | 1.36 (1.26, 1.47) | . | 980 | 75 | 1.16 (0.82, 1.66) | . | |
| Decrease | 8071 | 909 | 1.01 (0.92, 1.11) | . | 414 | 46 | 1.05 (0.70, 1.57) | . | |
Faller≥2falls per year. All models were adjusted for age, BMI (Body Mass Index), ethnicity, education, years since menopause, smoking, alcohol, number of falls at baseline, diabetes, hypertension, fainted, general health, hormone status, Beta blocker, Antianxiety agents, Hypnotics, narcotics, sedatives, physical function ≥90.
When adjusted for change in lean mass, the pattern of increased odds of falling with increasing physical activity was similar to that of the entire cohort for the first three years (p for trend = 0.01), while decreased physical activity appeared to have a protective effect against falling when adjusting for changes in lean mass. Those with a BMI < 30kg/m2 drove the relationship between decreases in physical activity and falling over 3 years. This relationship did not persist over six years.
Discussion
Contrary to our hypothesis, we found that active lifestyles and increases in physical activity over time were associated with increased fall risks among postmenopausal women aged 50-79 at baseline. Although reduction in falls has been supported by several exercise interventions (Gillespie et al., 2012), the positive studies tended to include multifactorial interventions (i.e. combination of physical activity, balance training, home hazards assessment, medication assessment, technical aids, etc.) and were typically limited to adults older than those in the WHI and those at high risk of falling. Community dwelling adults often do not employ multifactorial activity programs or activities designed to improve physical function (Lewis et al., 2015). Large longitudinal studies examining physical activity associations with falls in community dwelling older adults have suggested that physical activity may increase fall risk, although the risk is likely modified by type of activity and level of physical function or mobility (Jefferis et al., 2015; Lewis et al., 2015; Mertz et al., 2010; Peeters et al., 2010). Walking, in particular, the physical activity often selected by older women (Booth et al., 1997; Garcia et al., 2015; Sorkin et al., 2015), has been problematic for older adults in other studies (Mertz et al., 2010; Nikander et al., 2011 [Feb 15 2011 Epub ahead of print]). Postmenopausal women who spent greater time walking (>3hrs/wk) in a large, five-year study (N=2780) experienced more fractures, which authors suggest may be attributable to increased falls (Nikander et al., 2011 [Feb 15 2011 Epub ahead of print]).
In spite of these results, the benefits of physical activity for prevention and management of most of the prevalent chronic diseases in the United States, including osteoporosis, diabetes, cardiovascular disease, and some cancers (2008), likely outweigh the risks of falling. Further, exercise has been shown to reduce the risk of injury given a fall (Uusi-Rasi et al., 2015) and those who are more mobile prior to injury tend to have better outcomes (Thorngren et al., 2005). The minimal protection against falls due to greater sedentary time herein should be interpreted with caution, as well, as cardiovascular and other health benefits would be sacrificed with reduced activity. The distribution of medical conditions, medications, and falls across physical activity categories at baseline imply that the women self-limited physical activity if balance impairing medications, chronic conditions, or prior falls were present, as noted by others (2011; Bruce et al., 2002).
The results support the notion that aerobic activity alone among older adults is not enough to prevent falling in older populations (Clarke et al., 2015; Voukelatos et al., 2015). The increased opportunities for interaction with environmental hazards, and therefore greater opportunities for falling (Feldman and Chaudhury, 2008), need to be counterbalanced by the ability to adapt to these challenges. We would suggest that the complimentary strength and balance activities recommended by both the Physical Activity Guidelines for Americans (2008) and the Clinical Practice Guideline for Prevention of Falls in Older Persons (2011) be further publicized and evaluated. The adoption rate and efficacy of these multifactorial recommendations longitudinally (Clarke et al., 2015), along with suggested environmental strategies in older adults (Feldman and Chaudhury, 2008) requires further exploration, though early pilot work suggests an effective multifactorial fall prevention strategy can be habituated (Fleig et al., 2016).
The similarity in results with and without lean mass adjustment aligns with the lack of association between change in lean mass and physical activity demonstrated in the WHI previously (Sims et al., 2013) and further supports the need for activities beyond aerobic training to enhance physical function and potentially muscle quality, rather than lean mass per se. In support of this assertion, the Hispanic Established Population for the Epidemiologic Study of the Elderly (H-EPESE; N=1011 aged ≥75yrs) recently demonstrated that participants with high physical activity and low physical function had a greater fall risk than those with high physical activity and high physical function (Lewis et al., 2015). However, in The British Regional Heart Study (N=3137) those with initial low mobility participating benefited from increasing activity, while those without mobility limitations did not (Jefferis et al., 2015), suggesting the need to better understand the utility of initial mobility screening and activity planning in older adults.
Limitations
Statistical adjustment for potential confounding factors, may not fully account for differences between activity groups. Additionally, self-report physical activity measures, although validated herein and practical in large cohorts, have limitations. We could not separate falls occurring during activity from other falls which might be differentially related with physical activity and sedentary time. Objective measures of physical function were not available across this subset of WHI and fall data collection did not fully conform to Prevention of Falls Network Europe recommendations due to study completion prior to the consensus statement (Lamb et al., 2005). The study is not generalizable to younger women or men.
Conclusion
Physically active lifestyles increased falling among post-menopausal women. Additional fall prevention strategies, such as balance and resistance training, should be evaluated to assist post-menopausal women in reaching or maintaining the level of aerobic activity known to prevent and manage several chronic diseases.
Highlights.
Among postmenopausal women:
Increasing physical activity (PA) may be associated with a greater risk of falling.
Increasing sedentary time may slightly decrease risk of falling.
Falls risk must be weighed against PA benefits for prevention of chronic diseases.
Further research is needed to improve safety and support continued PA with aging.
Acknowledgments
We are thankful for the contribution of the WHI Investigators and staff at the clinical centers, clinical coordinating center, and project office.
Funding: This work was supported by National Cancer Institute (CA023074); and the WHI program which is funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services (HHSN268201100046C, HHSN268201100001C, HHSN268201100002C, HHSN268201100003C, HHSN268201100004C, and HHSN271201100004C).
Abbreviations
- ANOVA
analysis of variance
- BMI
body mass index
- DXA
dual energy X-ray absorptiometry
- MET
metabolic equivalent of task
- H-EPESE
Hispanic Established Population for the Epidemiologic Study of the Elderly
- SD
standard deviation
- WHI
Women's Health Initiative
Footnotes
Disclosure Statement: The authors have declared no conflicts of interest.
Short List of WHI Investigators: Program Office: (National Heart, Lung, and Blood Institute, Bethesda, Maryland) Jacques Rossouw, Shari Ludlam, Dale Burwen, Joan McGowan, Leslie Ford, and Nancy Geller
Clinical Coordinating Center: (Fred Hutchinson Cancer Research Center, Seattle, WA) Garnet Anderson, Ross Prentice, Andrea LaCroix, and Charles Kooperberg
Investigators and Academic Centers: (Brigham and Women's Hospital, Harvard Medical School, Boston, MA) JoAnn E. Manson; (MedStar Health Research Institute/Howard University, Washington, DC) Barbara V. Howard; (Stanford Prevention Research Center, Stanford, CA) Marcia L. Stefanick; (The Ohio State University, Columbus, OH) Rebecca Jackson; (University of Arizona, Tucson/Phoenix, AZ) Cynthia A. Thomson; (University at Buffalo, Buffalo, NY) Jean Wactawski-Wende; (University of Florida, Gainesville/Jacksonville, FL) Marian Limacher; (University of Iowa, Iowa City/Davenport, IA) Robert Wallace; (University of Pittsburgh, Pittsburgh, PA) Lewis Kuller; (Wake Forest University School of Medicine, Winston-Salem, NC) Sally Shumaker
Women's Health Initiative Memory Study: (Wake Forest University School of Medicine, Winston-Salem, NC) Sally Shumaker
For a list of all the investigators who have contributed to WHI science, please visit: https://www.whi.org/researchers/Documents%20%20Write%20a%20Paper/WHI%20Investigator%20Long%20List.pdf
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Design of the Women's Health Initiative clinical trial and observational study. The Women's Health Initiative Study Group. Controlled clinical trials. 1998;19:61–109. doi: 10.1016/s0197-2456(97)00078-0. [DOI] [PubMed] [Google Scholar]
- 2.U.S.D.o.H.a.H, editor. Services. Physical Activities Guidelines Advisory Committee; Washington (DC): 2008. Physical Activity Guidelines Advisory Committee Report. [Google Scholar]
- 3.Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59:148–57. doi: 10.1111/j.1532-5415.2010.03234.x. [DOI] [PubMed] [Google Scholar]
- 4.Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, O'Brien WL, Bassett DR, Jr, Schmitz KH, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32:S498–504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 5.Anderson GL, Manson J, Wallace R, Lund B, Hall D, Davis S, Shumaker S, Wang CY, Stein E, et al. Implementation of the Women's Health Initiative study design. Ann Epidemiol. 2003;13:S5–17. doi: 10.1016/s1047-2797(03)00043-7. [DOI] [PubMed] [Google Scholar]
- 6.Bea JW, Zhao Q, Cauley JA, LaCroix AZ, Bassford T, Lewis CE, Jackson RD, Tylavsky FA, Chen Z. Effect of hormone therapy on lean body mass, falls, and fractures: 6-year results from the Women's Health Initiative hormone trials. Menopause. 2011;18:44–52. doi: 10.1097/gme.0b013e3181e3aab1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beck TJ, Petit MA, Wu G, Leboff MS, Cauley JA, Chen Z. Does Obesity Really Make the Femur Stronger? Bone Mineral Density, Geometry and Fracture Incidence in the Women's Health Initiative-Observational Study. J Bone Miner Res. 2009 doi: 10.1359/JBMR.090307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Block G, Woods M, Potosky A, Clifford C. Validation of a self-administered diet history questionnaire using multiple diet records. J Clin Epidemiol. 1990;43:1327–35. doi: 10.1016/0895-4356(90)90099-b. [DOI] [PubMed] [Google Scholar]
- 9.Booth ML, Bauman A, Owen N, Gore CJ. Physical activity preferences, preferred sources of assistance, and perceived barriers to increased activity among physically inactive Australians. Prev Med. 1997;26:131–7. doi: 10.1006/pmed.1996.9982. [DOI] [PubMed] [Google Scholar]
- 10.Bruce DG, Devine A, Prince RL. Recreational physical activity levels in healthy older women: the importance of fear of falling. J Am Geriatr Soc. 2002;50:84–9. doi: 10.1046/j.1532-5415.2002.50012.x. [DOI] [PubMed] [Google Scholar]
- 11.Caspersen CJ, Pereira MA, Curran KM. Changes in physical activity patterns in the United States, by sex and cross-sectional age. Med Sci Sports Exerc. 2000;32:1601–9. doi: 10.1097/00005768-200009000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Cauley JA, Wu L, Wampler NS, Barnhart JM, Allison M, Chen Z, Jackson R, Robbins J. Clinical risk factors for fractures in multi-ethnic women: the Women's Health Initiative. J Bone Miner Res. 2007;22:1816–26. doi: 10.1359/jbmr.070713. [DOI] [PubMed] [Google Scholar]
- 13.Chen Z, Bassford T, Green SB, Cauley JA, Jackson RD, LaCroix AZ, Leboff M, Stefanick ML, Margolis KL. Postmenopausal hormone therapy and body composition--a substudy of the estrogen plus progestin trial of the Women's Health Initiative. Am J Clin Nutr. 2005;82:651–6. doi: 10.1093/ajcn.82.3.651. [DOI] [PubMed] [Google Scholar]
- 14.Chen Z, Beck TJ, Cauley JA, Lewis CE, LaCroix A, Bassford T, Wu G, Sherrill D, Going S. Hormone therapy improves femur geometry among ethnically diverse postmenopausal participants in the Women's Health Initiative hormone intervention trials. J Bone Miner Res. 2008;23:1935–45. doi: 10.1359/JBMR.080707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen Z, Kooperberg C, Pettinger MB, Bassford T, Cauley JA, LaCroix AZ, Lewis CE, Kipersztok S, Borne C, et al. Validity of self-report for fractures among a multiethnic cohort of postmenopausal women: results from the Women's Health Initiative observational study and clinical trials. Menopause. 2004;11:264–74. doi: 10.1097/01.gme.0000094210.15096.fd. [DOI] [PubMed] [Google Scholar]
- 16.Clark BK, Sugiyama T, Healy GN, Salmon J, Dunstan DW, Shaw JE, Zimmet PZ, Owen N. Socio-demographic correlates of prolonged television viewing time in Australian men and women: the AusDiab study. J Phys Act Health. 2010;7:595–601. doi: 10.1123/jpah.7.5.595. [DOI] [PubMed] [Google Scholar]
- 17.Clarke CL, McMurdo ME, Witham MD. Falls research: stumbling or striding? Age Ageing. 2015;44:350–2. doi: 10.1093/ageing/afv047. [DOI] [PubMed] [Google Scholar]
- 18.Eaglehouse YL, Talbott EO, Chang Y, Kuller LH. Participation in Physical Activity and Risk for Amyotrophic Lateral Sclerosis Mortality Among Postmenopausal Women. JAMA Neurol. 2016;73:329–36. doi: 10.1001/jamaneurol.2015.4487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Feldman F, Chaudhury H. Falls and the physical environment: a review and a new multifactorial falls-risk conceptual framework. Can J Occup Ther. 2008;75:82–95. doi: 10.1177/000841740807500204. [DOI] [PubMed] [Google Scholar]
- 20.Fleig L, McAllister MM, Chen P, Iverson J, Milne K, McKay HA, Clemson L, Ashe MC. Health behaviour change theory meets falls prevention: Feasibility of a habit-based balance and strength exercise intervention for older adults. Psychol Sport Exerc Volume. 2016;22:114–22. [Google Scholar]
- 21.Garcia DO, Wertheim BC, Manson JE, Chlebowski RT, Volpe SL, Howard BV, Stefanick ML, Thomson CA. Relationships between dog ownership and physical activity in postmenopausal women. Prev Med. 2015;70:33–8. doi: 10.1016/j.ypmed.2014.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, Lamb SE. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;9:CD007146. doi: 10.1002/14651858.CD007146.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hays J, Hunt JR, Hubbell FA, Anderson GL, Limacher M, Allen C, Rossouw JE. The Women's Health Initiative recruitment methods and results. Ann Epidemiol. 2003;13:S18–77. doi: 10.1016/s1047-2797(03)00042-5. [DOI] [PubMed] [Google Scholar]
- 24.Jefferis BJ, Merom D, Sartini C, Wannamethee SG, Ash S, Lennon LT, Iliffe S, Kendrick D, Whincup PH. Physical Activity and Falls in Older Men: The Critical Role of Mobility Limitations. Med Sci Sports Exerc. 2015;47:2119–28. doi: 10.1249/MSS.0000000000000635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johnson-Kozlow M, Rock CL, Gilpin EA, Hollenbach KA, Pierce JP. Validation of the WHI brief physical activity questionnaire among women diagnosed with breast cancer. Am J Health Behav. 2007;31:193–202. doi: 10.5555/ajhb.2007.31.2.193. [DOI] [PubMed] [Google Scholar]
- 26.Lamb SE, Jorstad-Stein EC, Hauer K, Becker C. Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. J Am Geriatr Soc. 2005;53:1618–22. doi: 10.1111/j.1532-5415.2005.53455.x. [DOI] [PubMed] [Google Scholar]
- 27.Langer RD, White E, Lewis CE, Kotchen JM, Hendrix SL, Trevisan M. The Women's Health Initiative Observational Study: baseline characteristics of participants and reliability of baseline measures. Ann Epidemiol. 2003;13:S107–21. doi: 10.1016/s1047-2797(03)00047-4. [DOI] [PubMed] [Google Scholar]
- 28.LaStayo PC, Ewy GA, Pierotti DD, Johns RK, Lindstedt S. The positive effects of negative work: increased muscle strength and decreased fall risk in a frail elderly population. J Gerontol A Biol Sci Med Sci. 2003;58:M419–24. doi: 10.1093/gerona/58.5.m419. [DOI] [PubMed] [Google Scholar]
- 29.Lewis ZH, Markides KS, Ottenbacher K, Al Snih S. The Role of Physical Activity and Physical Function on the Risk of Falls in Older Mexican Americans. J Aging Phys Act. 2015 doi: 10.1123/japa.2015-0150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Manson JE, Greenland P, LaCroix AZ, Stefanick ML, Mouton CP, Oberman A, Perri MG, Sheps DS, Pettinger MB, et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. 2002;347:716–25. doi: 10.1056/NEJMoa021067. [DOI] [PubMed] [Google Scholar]
- 31.Mertz KJ, Lee DC, Sui X, Powell KE, Blair SN. Falls among adults: the association of cardiorespiratory fitness and physical activity with walking-related falls. Am J Prev Med. 2010;39:15–24. doi: 10.1016/j.amepre.2010.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Meyer AM, Evenson KR, Morimoto L, Siscovick D, White E. Test-retest reliability of the Women's Health Initiative physical activity questionnaire. Med Sci Sports Exerc. 2009;41:530–8. doi: 10.1249/MSS.0b013e31818ace55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Morley JE, Baumgartner RN, Roubenoff R, Mayer J, Nair KS. Sarcopenia. J Lab Clin Med. 2001;137:231–43. doi: 10.1067/mlc.2001.113504. [DOI] [PubMed] [Google Scholar]
- 34.Nguyen HQ, Herting JR, Kohen R, Perry CK, LaCroix A, Adams-Campbell LL, Beresford SA, Eaton CB, Tinker L. Recreational physical activity in postmenopausal women is stable over 8 years of follow-up. J Phys Act Health. 2013;10:656–68. doi: 10.1123/jpah.10.5.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nikander R, Gagnon C, Dunstan DW, Magliano DJ, Ebeling PR, Lu ZX, Zimmet PZ, Shaw JE, Daly RM. Frequent walking, but not total physical activity, is associated with increased fracture incidence: A 5-year follow-up of an Australian population based prospective study (AusDiab) J Bone Miner Res. 2011 doi: 10.1002/jbmr.363. Feb 15 2011 Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 36.Owen N, Healy GN, Matthews CE, Dunstan DW. Too much sitting: the population health science of sedentary behavior. Exerc Sport Sci Rev. 2010;38:105–13. doi: 10.1097/JES.0b013e3181e373a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Peeters GM, Verweij LM, van Schoor NM, Pijnappels M, Pluijm SM, Visser M, Lips P. Which types of activities are associated with risk of recurrent falling in older persons? J Gerontol A Biol Sci Med Sci. 2010;65:743–50. doi: 10.1093/gerona/glq013. [DOI] [PubMed] [Google Scholar]
- 38.Robbins J, Aragaki AK, Kooperberg C, Watts N, Wactawski-Wende J, Jackson RD, LeBoff MS, Lewis CE, Chen Z, et al. Factors associated with 5-year risk of hip fracture in postmenopausal women. Jama. 2007;298:2389–98. doi: 10.1001/jama.298.20.2389. [DOI] [PubMed] [Google Scholar]
- 39.Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35(2):ii37–ii41. doi: 10.1093/ageing/afl084. [DOI] [PubMed] [Google Scholar]
- 40.Schwartz AV, Nevitt MC, Brown BW, Jr, Kelsey JL. Increased falling as a risk factor for fracture among older women: the study of osteoporotic fractures. Am J Epidemiol. 2005;161:180–5. doi: 10.1093/aje/kwi023. [DOI] [PubMed] [Google Scholar]
- 41.Sims ST, Kubo J, Desai M, Bea J, Beasley JM, Manson JE, Allison M, Seguin RA, Chen Z, et al. Changes in Physical Activity and Body Composition in Postmenopausal Women over Time. Med Sci Sports Exerc. 2013 doi: 10.1249/MSS.0b013e31828af8bd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sims ST, Larson JC, Lamonte MJ, Michael YL, Martin LW, Johnson KC, Sarto GE, Stefanick ML. Physical activity and body mass: changes in younger versus older postmenopausal women. Med Sci Sports Exerc. 2012;44:89–97. doi: 10.1249/MSS.0b013e318227f906. [DOI] [PubMed] [Google Scholar]
- 43.Sorkin DH, Biegler KA, Billimek J. Differences in Self-Reported Physical Activity and Body Mass Index Among Older Hispanic and Non-Hispanic White Men and Women: Findings from the 2009 California Health Interview Survey. J Am Geriatr Soc. 2015;63:2158–63. doi: 10.1111/jgs.13655. [DOI] [PubMed] [Google Scholar]
- 44.Stalenhoef PA, Diederiks JP, Knottnerus JA, Kester AD, Crebolder HF. A risk model for the prediction of recurrent falls in community-dwelling elderly: a prospective cohort study. J Clin Epidemiol. 2002;55:1088–94. doi: 10.1016/s0895-4356(02)00502-4. [DOI] [PubMed] [Google Scholar]
- 45.Thibaud M, Block F, Tournoux-Facon C, Breque C, Rigaud AS, Dugue B, Kemoun G. Impact of physical activity and sedentary behaviour on fall risks in older people: a systematic reveiw and meta-analysis of observational studies. Eur Rev Aging Phys Act. 2012;9:5–15. [Google Scholar]
- 46.Thorngren KG, Norrman PO, Hommel A, Cedervall M, Thorngren J, Wingstrand H. Influence of age, sex, fracture type and pre-fracture living on rehabilitation pattern after hip fracture in the elderly. Disabil Rehabil. 2005;27:1091–7. doi: 10.1080/09638280500056402. [DOI] [PubMed] [Google Scholar]
- 47.Uusi-Rasi K, Patil R, Karinkanta S, Kannus P, Tokola K, Lamberg-Allardt C, Sievanen H. Exercise and Vitamin D in Fall Prevention Among Older Women: A Randomized Clinical Trial. JAMA Intern Med. 2015 doi: 10.1001/jamainternmed.2015.0225. [DOI] [PubMed] [Google Scholar]
- 48.Voukelatos A, Merom D, Sherrington C, Rissel C, Cumming RG, Lord SR. The impact of a home-based walking programme on falls in older people: the Easy Steps randomised controlled trial. Age Ageing. 2015;44:377–83. doi: 10.1093/ageing/afu186. [DOI] [PubMed] [Google Scholar]
- 49.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83. [PubMed] [Google Scholar]


