Abstract
Background
Substance use disorders consistently rank among the most stigmatized conditions worldwide. Thus, substance use stigma fosters health inequities among persons with substance use disorders and remains a key barrier to successful screening and treatment efforts. Current efforts to measure substance use stigma are limited. This study aims to advance measurement efforts by drawing on stigma theory to develop and evaluate the Substance Use Stigma Mechanisms Scale (SU-SMS). The SU-SMS was designed to capture enacted, anticipated, and internalized substance use stigma mechanisms among persons with current and past substance use disorders, and distinguish between key stigma sources most likely to impact this target population.
Methods
This study was a cross-sectional evaluation of the validity, reliability, and generalizability of the SU-SMS across two independent samples with diverse substance use and treatment histories.
Results
Findings support the structural and construct validity of the SU-SMS, suggesting the scale was able to capture enacted, anticipated, and internalized stigma as distinct stigma experiences. It also further differentiated between two distinct stigma sources (family and healthcare providers). Analysis of these mechanisms and psychosocial metrics suggests that the scale is also associated with other health-related outcomes. Furthermore, the SU-SMS demonstrated high levels of internal reliability and generalizability across two independent samples of persons with diverse substance use disorders and treatment histories.
Conclusion
The SU-SMS may serve as a valuable tool for better understanding the processes through which substance use stigma serves to undermine key health behaviors and outcomes among persons with substance use disorders.
Keywords: Stigma, Measures, Psychometrics, Substance use, Substance disorder, Substance abuse treatment
1. INTRODUCTON
1.1 The Harms of Substance Use Stigma among Persons with Substance Use Disorders
Drug addiction and alcoholism consistently rank among the most devalued stigmatized characteristics worldwide (Room, 2005). Compared with other stigmatized mental and physical illnesses (e.g., schizophrenia, HIV), limited research has addressed substance use stigma, or social devaluation and discrediting associated with substance use (Goffman, 1963). Similar to other illnesses, however, stigma associated with substance use is considered a significant barrier to detection and treatment efforts, and research is needed to understand and address this issue (Kulesza et al., 2013). One reason why research on substance use stigma may be lagging is the lack of a multidimensional theory-driven scale to measure experiences of substance use stigma among people with substance use disorders (SUDs).
As a multi-level phenomenon, stigma exists when negative labeling, stereotyping, status loss, and discrimination occur within a power structure that ultimately maintains and reproduces social inequities among marked populations (Link and Phelan, 2006). As such, substance use stigma can manifest at the structural, social, and individual-level. Substance use stigma at the structural and social level reflect a core consensus that society, as a whole, devalues persons with SUDs and legitimizes collective action to penalize this population through institutionalized systems, policies, and practices (Pryor and Reeder, 2011; Bos et al., 2013). Such actions may restrict access to SUD treatment through community-driven ‘not in my back yard’ campaigns (Tempalski et al., 2007), or restrict harm reduction efforts such as the 2011 ban on use of federal funds to support needle and syringe exchange programs. These actions not only perpetuate social, economic, and health inequities in this population but virtually communicate that persons with SUDs are not worthy of protection or opportunities to address their condition (Strathdee et al., 2012).
While these publically sanctioned collective actions against persons with SUDs certainly shape individual health and well-being (Link et al, 1997; Link and Phelan, 2006; Ahern et al., 2007), the ways in which these actions manifest as stigma within the stigmatized individual reflect a distinct and equally important process. Specifically, stigma theory suggests that structural and social stigma associated with substance use is experienced by individuals as enacted, anticipated, and internalized stigma (Earnshaw and Chaudoir, 2009). Recent findings in HIV stigma research suggests these three stigma mechanisms are related to health outcomes in unique ways, with enacted and anticipated stigma relating to worse physical health (e.g., CD4 count ≤ 200 cells/mm3) and internalized stigma relating to worse affective (e.g., HIV-related emotional distress) and behavioral (e.g., poor retention in HIV care) health (Earnshaw et al., 2013a). Future research differentiating between these three stigma mechanisms may yield a similar nuanced understanding of how substance use stigma impacts persons with SUDs.
1.2. Individual Manifestations of Substance Use Stigma
We draw from the Stigma Framework, which synthesizes extant stigma theory and makes recommendations for stigma measurement at the individual-level. The Stigma Framework draws on theoretical conceptualizations of stigma from a range of fields, including medical anthropology, sociology, and psychology, that have been applied to a variety of socially devalued and discredited characteristics, including HIV, mental illness, race, and gender (Allport, 1954; Goffman, 1963; Link, 1987; Meyer, 1995; Link and Phelan, 2001; Parker and Aggleton, 2003; Herek et al., 2003; Brewer, 2007; Phelan et al., 2008). The sociological and anthropological theories describe stigma as a social process dependent on social context, which ultimately maintains social inequity between groups of people (Link and Phelan, 2001; Parker and Aggleton, 2003). The psychological theories describe ways in which individual people living with and without socially devalued and discredited characteristics enact, perpetuate, and perceive this social process (Allport, 1954; Meyer, 1995; Brewer, 2007). The Stigma Framework identifies measurable stigma mechanisms from this literature, which reflect an individual’s distinct psychological responses to the knowledge that they possess a socially devalued and discredited characteristic, including: enacted stigma, anticipated stigma, and internalized stigma (Earnshaw and Chaudoir, 2009). These stigma mechanisms are ultimately related to physical, mental, and behavioral health outcomes. The Stigma Framework further specifies that these mechanisms are related to, but function independent of each other, and are important to measure given their unique associations with the health and well-being of stigmatized individuals (Earnshaw et al., 2013a).
Enacted Stigma reflects personal experiences of stereotyping, prejudice, and/or discrimination from others in the past or present due to one’s stigmatized attribute. As examples, people with SUDs may be denied services from healthcare workers who assume they are pill shopping or have been told they are not trusted to be alone in their family home because they might steal something (Earnshaw et al., 2013b). These past experiences may or may not influence one’s expectation of future stigma regarding their substance use status or influence negative self-perceptions of one’s SUD status.
Anticipated Stigma reflects expectations of stereotyping, prejudice, and/or discrimination from others in the future due to one’s stigmatized attributes. For example, people with SUDs may expect that healthcare providers will not take their medical needs seriously, or that friends and family will think that they are going to steal from them. People with SUDs may anticipate stigma as a result of their own past experiences. They may also anticipate stigma as a result of observing the experiences of others and/or being aware of societal stigma toward people with SUDs. People with SUDs therefore don’t necessarily have to have personally experienced stigma in order to anticipate it in their future.
Internalized Stigma is seen in the endorsement and application of negative feelings and beliefs about people with SUDs to oneself. Because substance use is a socially devalued characteristic that is acquired only as someone transitions into non-socially sanctioned levels of substance misuse and abuse, people engaging in substance use may have already held negative personal beliefs and/or feelings towards people with SUDs before developing their own SUD. Upon gaining the SUD label, they are forced to confront these negative beliefs and feelings. This process may result in the internalization of stigma, or devaluing and discrediting of oneself, due to one’s SUD status.
Within these stigma mechanisms, both enacted and anticipated stigma reflect interpersonal processes. Thus, they are experienced in relation to other people. Past work suggests that the sources of stigma also matter (Stutterheim et al., 2009; Jackson et al., 2010; Earnshaw et al., 2012). As such, the Stigma Framework hypothesizes stigma will manifest differently from different people (e.g., stereotypes about pill shopping from doctors, discrimination via lack of trust and social distancing from family members), and the impact of stigma may differ depending on from whom it is experienced. Among people with SUDs, family members and healthcare providers may be particularly important to focus on given that stigma from these sources can critically impact the health and well-being of people with SUDs. In past work, people with SUDs have identified family members as a particularly harmful source of stigma in the context of active recovery (e.g., methadone maintenance therapy; Earnshaw et al, 2013b). Moreover, people with SUDs describe significant stigma from healthcare providers, which may act as a barrier to SUD treatment.
1.3 The State of Substance Use Stigma Measurement
Given the increased recognition of the need to understand substance use stigma among people with SUDs, there has been a burgeoning increase in stigma-related scales that have been adapted or developed for this purpose. Building on a recent systematic review of substance use related stigma by Kulesza and colleagues (2013), we employed the Stigma Framework’s definitions of enacted, anticipated, and internalized stigma as a theory-based, clearly articulated, benchmark for evaluating ways in which these studies have measured individual-level substance use stigma to date. Of the 13 stigma measures administered to persons with SUDs across 15 samples reviewed by Kulesza and colleagues, most were evaluated among drug- or alcohol-using populations, and only two (Link et al., 1997; Luoma et al., 2010) examined substance using populations more broadly (both of which were in treatment for SUDs). After examining the content of these stigma measures, we observed that none collectively measured enacted, anticipated, and internalized substance use stigma as distinct constructs. In addition, none of the enacted or anticipated stigma measures contained sub-scales that could be used to examine stigma across diverse sources (e.g., family and friends vs. healthcare providers).
Although an in-depth review of these measures is beyond the scope of this article, most studies utilized measures of perceived stigma in isolation (Fortney et al., 2004; Keyes et al., 2010; Smith et al., 2010) or in conjunction with other measures (Link et al., 1997; Semple et al., 2005; Ahern et al., 2007; Luoma et al., 2010). Perceived stigma is the process through which stigmatized individuals recognize the prevalence of stigmatizing attitudes and actions in the general public towards individuals who belong to their stigmatized group (Link et al., 1997; Luoma et al, 2010). Such measures of perceived stigma are limited in that they only speak to an individuals’ general awareness of stigma, rather than their personal experiences with stigma. We argue that these personal experiences are more proximate predictors of health. Moreover, three measures broadly assessed shame as a proxy for internalized stigma (O’Connor et al., 1994; Dearing et al., 2005), which cannot speak to the self-devaluation process as it relates to one’s stigmatized attribute per se. In addition, most studies developed or adapted measures that conflated enacted, anticipated, and/or internalized stigma items as a single stigma construct (Latkin et al., 2010) or included factors in their operationalization of stigma that are related to, but distinct from, individual-level stigma mechanisms (e.g., needing to prove oneself to others, stereotype agreement, social withdrawal; Minior et al., 2003; Ross et al., 2007; Luoma et al., 2010; Schomerus et al., 2011).
In sum, the current state of substance use stigma measurement is problematic in that it lacks consensus in the operationalization of individual-level stigma mechanisms and frequently conflates distinct stigma constructs. To date, no measures offer a way to assess the contributions of different stigma sources (i.e., family members vs. healthcare workers). Limited testing of scales across both in-treatment and out-of-treatment substance-using populations further limits generalizability. These limitations impede the potential for comparison between substance use stigma studies (Earnshaw and Chaudoir, 2009; Kulesza et al., 2013).
1.4 Current Work
To address this gap, we seek to evaluate the reliability and validity of the Substance Use Stigma Mechanisms Scale (SU-SMS), a measure based on the Stigma Framework, across two samples with diverse histories of substance use behaviors and treatment histories. Specifically the SU-SMS is structured to measure enacted, anticipated, and internalized substance use stigma as distinct constructs and provide sub-scales reflecting enacted and anticipated stigma from relevant stigma sources commonly identified in the extant literature (i.e., family members and healthcare workers; Earnshaw and Chaudoir, 2009; Smith et al., 2012; Earnshaw et al., 2013b).
2. MATERIALS AND METHODS
2.1 Study Design
Two pre-existing study protocols, with independent samples, provided an opportunity for the current cross-sectional study to assess the structural validity, reliability, and generalizability of the Substance Use Stigma Mechanisms Scale (SU-SMS). Structural validity was assessed using the hypothesized 5-factor structure of the scale for the three primary stigma mechanisms (2nd order scales) and two external stigma sources (1st order sub-scales) using confirmatory factor analysis. Additional support for this factor structure was assessed by examining the correlations between the stigma mechanisms scales and stigma source subscales. Reliability of the SU-SMS and its subscales was assessed using Cronbach’s Alpha as an indicator of internal consistency. Support for generalizability of the scale to assess levels of substance use stigma across diverse substance use histories was performed by ensuring equal levels of internal consistency between samples, while observing predicted differences in mean levels of reported substance use stigma between the two samples.
Construct validity of the SU-SMS was assessed using responses to available psychosocial measures in the second sample, which consisted of HIV clinic participants’ responses to mental health, HIV stigma, and substance use queries. Convergent and discriminant validity was examined to assess the extent to which substance use stigma mechanisms were correlated with constructs that were theoretically related or unrelated. We hypothesized that manifestations of substance use stigma would not be associated with experiencing mental illness in general, but that both enacted and internalized stigma would be uniquely associated with symptoms of depression, while anticipated stigma might be associated with symptoms of anxiety. We expected low, but significant associations between reported experiences of HIV stigma and substance use stigma, suggesting similarity between the mechanisms through which stigma manifests (e.g., enacted, anticipated, internalized) but substantial difference between the two types of stigmatized identities. We further hypothesized that higher rates of substance use stigma would be observed for participants with moderate- to high-risk substance use profiles. This sub-study had Institutional Review Board approval.
2.2 Participants and Procedures
2.2.1 MMT Sample
The first sample was recruited from an existing parent study evaluating the efficacy of a group-based HIV prevention intervention for patients enrolled in methadone maintenance therapy (MMT). Eligible participants enrolled in the parent grant were ≥ 18 years of age, HIV-negative, diagnosed as opioid dependent, and enrolled in daily outpatient MMT. Ninety-three participants returning for their final post-intervention 12-month follow up assessment at the methadone clinic were invited to take the supplemental SU-SMS assessment ($10 remuneration). Participants had the option of self-administering the assessment via paper and pencil, or having the SU-SMS measure administered in-person by a trained interviewer in English. No significant (p ≤ .10) differences were observed on participant responses to the SU-SMS measure when comparing participants randomized to the parent grant’s intervention or wait-list control arm.
2.2.2 HIV Clinical Care Sample
The second sample consisted of HIV-positive patients accessing clinical care in an inner city community clinic setting who were recruited into an existing larger prospective study of retention in HIV care. All participants were ≥ 18 years of age, HIV-positive, and accessing HIV clinical care and/or Buprenorphine for opiate replacement therapy (ORT) from clinic providers. Participants who reported a lifetime history of problematic substance use (e.g., having a ‘friend or relative ever express concern” or having “ever tried and failed to control, cut down, or stop using” a specific substance) or reported active substance use in the past 3 months, were administered the SU-SMS measure as part of the standard survey instrument ($15 remuneration). Of the 101 participants enrolled in the parent study, 85 (84.2%) were administered the SU-SMS, reflecting a diverse community-based substance-involved population recruited outside of a defined substance use treatment program. All measures were administered in-person by a trained interviewer in either English or Spanish. These measures, including the SU-SMS, were translated into Spanish by a professional translator (native of Columbia), and back translated into English by a US-born native bilingual graduate student (Spanish - Puerto Rican dialect / English). Any discrepancies were resolved by consensus in person between the two translators and the lead author. The items were then reviewed for clarity by two bilingual clinic staff to ensure they would be easily understood by their Spanish-speaking patients (predominantly of Puerto Rican, Dominican, and Mexican origin).
2.3 Measures
2.3.1 Social Demographics
Select demographics assessed among both parent studies were used to characterize participants’ socio-demographic characteristics.
2.3.2 Substance Use Stigma Mechanisms Scale (SU-SMS)
Informed by the Stigma Framework (Earnshaw and Chaudoir, 2009), the Substance Use Stigma Mechanisms Scale (SU-SMS; see Supplementary Material1) was developed in parallel with the HIV Stigma Mechanisms Scale (HIV-SMS) (Earnshaw et al., 2013a). Both scales differentiate between enacted, anticipated, and internalized stigma, as suggested by the Stigma Framework, with unique items (Earnshaw and Chaudoir, 2009). We adapted Stigma Framework to assess enacted (6-items; “Healthcare workers have not listened to my concerns”) and anticipated (6-items; “Family members will look down on me”) stigma from family and healthcare workers, the two common stigma sources most likely to impact both the existing MMT and HIV clinical care samples. Based on previous qualitative work (Smith et al., 2012; Earnshaw et al., 2013b), additional items examined a third source of stigma that might hinder access to life-stabilizing resources (i.e., a ‘gatekeepers’ type construct) in the target samples (‘employers’ for MMT participants, ‘Case Managers/Social Workers’ for HIV clinical care participants). However, as measured on the SU-SMS, we found that concern for stigma from these sources did not generalize across samples, where MMT participants viewed employers as a credible stigma source, and few if any HIV-positive patients viewed Case Managers/Social Workers as a potential source of stigma. Given these differences, we did not include these third sources of stigma from our respective samples in the validation of the SU-SMS. Internalized stigma items were also assessed (6-items; “Having used alcohol and/or drugs makes me feel like I’m a bad person”).
Aside from the structure of the stigma mechanisms and the stigma sources as listed above, specific item content for the SU-SMS and the HIV-SMS were informed by their respective literatures and through collaborative discussions with researchers and providers that served these distinct populations. For example, the ways in which stigma may manifest from family members (FAM) or healthcare workers (HCW) towards persons with SUDs (FAM: ‘Family members have thought I cannot be trusted’; HCW: ‘Healthcare workers have thought that I’m pill shopping, or trying to con them into giving me prescription medications to get high or sell’) may be different than how it manifests towards persons living with HIV (FAM: ‘Family members will avoid me’; HCW: ‘Healthcare workers will avoid touching me’). While the ways in which stereotypes, prejudice, and discrimination towards persons with SUDs and persons living with HIV may differ, items for the internalized stigma scales were kept the same to reflect the general process of self-devaluation (‘I feel ashamed of having HIV ’ and ‘I feel ashamed of having used alcohol and/or drugs’), a hallmark of the internalization mechanism.
The SU-SMS was independently pilot tested in both samples (n = 12 MMT clients; n = 10 HIV-positive patients) using cognitive interviewing (Beatty and Willis, 2007), a qualitative technique performed via individual interviews to ensure comprehension and acceptability of items (Earnshaw et al., 2013b). Cognitive interviewing aims to identify the cognitive process used by participants when responding to survey items. These processes reflect the comprehension of the individual survey items, the retrieval of an individual’s response(s) from memory, factors that may inhibit the response process (i.e., sufficient motivation to answer items accurately and social desirability concerns regarding sensitive topics), and the mapping of the individual’s response to the available item’s response options. From this process, the enacted and anticipated stigma from family member items was amended to reflect ‘loss of trust’ which emerged an important manifestation of substance use stigma. Item responses were given on a 5-point Likert-type scale with higher scores indicating greater substance use stigma. Composite scores were created by taking the average of participants’ enacted, anticipated, and internalized substance use stigma item responses respectively.
2.3.3 Substance Use Measures
For both samples, responses regarding lifetime and recent use of illicit substances (opiates, crack/cocaine), injection drug use, and ORT status were used to create composite variables (1= yes, 0= no) for comparing substance use histories across the two independent samples. The time frame characterizing a recent occurrence of these behaviors was different between the two samples’ existing study protocols. Recent use was defined as the past 30 days for the MMT sample and as the past 3 months for the HIV clinical care sample. All participants in the MMT sample were defined as opioid dependent, based on inclusion criteria of the parent study. Additional metrics of substance use type and severity were available for the HIV clinical care sample, who completed the WHO Assist version 3.0 (Humeniuk et al., 2008) as part of their participation in the parent study. Note, ‘drug of choice’ was not assessed. Using the WHO Assist guidelines, substance use severity was calculated to reflect low-, moderate-, or high risk of addiction-related harms. A substance use severity score was calculated for each substance type a participant reported using (i.e., alcohol, marijuana, cocaine, crack, opiates, sedatives, amphetamines, other substances).
2.3.4 Psychosocial Measures
Psychosocial measures were unavailable for the MMT sample. For the HIV clinical care sample, such measures reflect mental health and HIV stigma constructs assessed as part of the larger study. Participants self-reported having ever been diagnosed with a mental illness, specifying type of diagnosis. Responses were categorized as reporting any diagnosed mental health condition, and specifically reporting a diagnosed anxiety related disorder (1= yes, 0= no). The CESD-10 was used to classify number of depression-related symptoms experienced in the past week (Irwin et al., 1999; Robison et al., 2002). CESD-10 items were reverse scored as needed, then summed so that higher scores reflected more depressive symptoms. Finally, responses of enacted (6-items) and anticipated (6 items) HIV stigma from family members and healthcare workers, as well as, responses of internalized HIV stigma (6-items) were averaged to create composite scores that could be compared to participants’ SU-SMS responses. Similarly, responses to the HIV-SMS were assessed on 5-point Likert-type scale, with higher scores indicating greater HIV stigma (Earnshaw et al., 2013a).
3. RESULTS
3.1 Participant Characteristics
Common demographic characteristics and substance use histories are presented for all 178 participants in Table 1. The overall sample was diverse in terms of demographic characteristics, and socio-economically vulnerable. Notably, differences in race/ethnicity and language are reflective of the recruitment communities, with the majority of MMT participants identifying as non-Hispanic White, and the majority of HIV clinical care participants identifying as Hispanic or non-Hispanic Black. More HIV clinical care participants also identified as Gay or Bisexual, likely reflecting differences in HIV status between the two samples. More HIV clinical care participants reported receipt of disability and slightly fewer reported an annual income of less than $20,000 per year. Anticipated differences between the two samples’ substance use histories were also observed. MMT participants reported higher rates of lifetime and recent use of illicit substances, injecting, and being on ORT. In contrast, the HIV clinical care sample reported using a range of illicit and recreational substances (see Table 2). Most HIV clinical care participants were classified as moderate- to low-risk users, very few participants were classified as high-risk users; compared to the MMT sample all of whom were opioid dependent.
Table 1.
Participant characteristics within and between pooled and independent samples (N = 178)
| Total N (%) |
MMT Clinic n (%) |
HIV Care n (%) |
Difference Test t-test or χ2 value |
|
|---|---|---|---|---|
| Sample size | N=178 | n = 93 | n = 85 | n/a |
| Mean Age (SD) | 43.51 (11.33) | 38.10 (10.21) | 49.43 (9.34) | −7.68 ** |
| Gender | 0.40 | |||
| Male | 94 (52.8%) | 47 (50.5%) | 47 (53.3%) | |
| Female | 84 (47.2%) | 46 (49.5%) | 38 (44.7%) | |
| Race/Ethnicity | ||||
| Hispanic | 60 (33.7%) | 13 (14.0%) | 47 (55.3%) | 33.93*** |
| non-Hispanic Black | 46 (25.8%) | 13 (14.0%) | 33 (38.8%) | 14.30*** |
| non-Hispanic White | 64 (36.0%) | 63 (67.7%) | 1 ( 1.2%) | 85.45*** |
| non-Hispanic Other | 8 ( 4.5%) | 4 ( 4.3%) | 4 ( 4.7%) | 0.02 |
| Primary Language | 25.16*** | |||
| English | 143 (80.3%) | 88 (94.6%) | 55 (64.7%) | |
| non-English | 35 (19.7%) | 5 ( 5.4%) | 30 (35.3%) | |
| Sexual Orientation§ | 5.53 * | |||
| Heterosexual | 144 (85.2%) | 77 (91.7%) | 67 (78.8%) | |
| Gay or Bisexual | 25 (14.8%) | 7 ( 8.3%) | 18 (21.2%) | |
| SES Factors | ||||
| No GED/Diploma | 67 (37.6%) | 30 (32.3%) | 37 (43.5%) | 2.40 |
| Unemployed§ | 126 (74.6%) | 62 (73.8%) | 64 (75.3%) | 0.50 |
| On disability/SSI§ | 66 (39.1%) | 17 (20.2%) | 49 (57.6%) | 24.84*** |
| Income < $20K/yr.§ | 137 (88.1%) | 74 (88.1%) | 63 (74.1%) | 5.38 * |
| Unstable housing§ | 15 ( 8.9%) | 8 ( 9.5%) | 7 ( 8.2%) | 0.07 |
| Injection Drug Use | ||||
| Lifetime | 99 (55.6%) | 73 (78.5%) | 26 (30.6%) | 41.29*** |
| Recent † | 16 ( 9.0%) | 11 (11.8%) | 5 ( 5.9%) | 1.92 |
| Opiate Use | ||||
| Lifetime | 130 (73.0%) | 93 (100%) | 37 (43.5%) | 97.91*** |
| Recent † | 27 (15.2%) | 20 (21.5%) | 7 ( 8.2%) | 6.08 * |
| Crack/Cocaine Use | ||||
| Lifetime | 145 (81.5%) | 89 (95.7%) | 56 (65.9%) | 26.14*** |
| Recent † | 40 (22.5%) | 31 (33.3%) | 9 (10.6%) | 13.19*** |
| Opiate Replacement Therapy | ||||
| History of ORT | 111 (62.4%) | 82 (88.2%) | 29 (35.1%) | 55.28*** |
| Currently on ORT | 103 (57.9%) | 83 (89.2%) | 20 (23.5%) | 78.67*** |
9 participants in MMT sample had missing values on this variable.
Recent use (MMT = past 30 days, HIV = past 3 mo.).
Difference test is significant at the 0.001 (***), 0.01 (**), or 0.05 (*) level (2-tailed).
Table 2.
Generalizability of substance use and severity of use experiences in HIV Care Sample (n = 85).
| Type of Reported Substance Use | WHO Assist Substance Use Severity Risk Score | |||
|---|---|---|---|---|
| Substance Type | n (%) | Low (n) | Medium (n) | High (n) |
| Alcohol | 74 (87.1%) | 65 | 7 | 2 |
| Marijuana | 62 (72.9%) | 34 | 27 | 1 |
| Cocaine | 53 (62.4%) | 29 | 24 | 0 |
| Crack | 36 (42.4%) | 16 | 19 | 1 |
| Opiates | 37 (43.5%) | 13 | 22 | 2 |
| Sedatives | 21 (24.7%) | 17 | 4 | 0 |
| Amphetamines | 5 ( 5.9%) | 2 | 3 | 0 |
| Other | 10 (11.8%) | 9 | 1 | 0 |
The diverse demographic and substance use profiles observed across these two samples offer confirmation that the Substance Use Stigma Mechanisms Scale (SU-SMS) was successfully implemented in two distinct drug-involved populations, which afford greater insights into the generalizability of the measure than either sample alone.
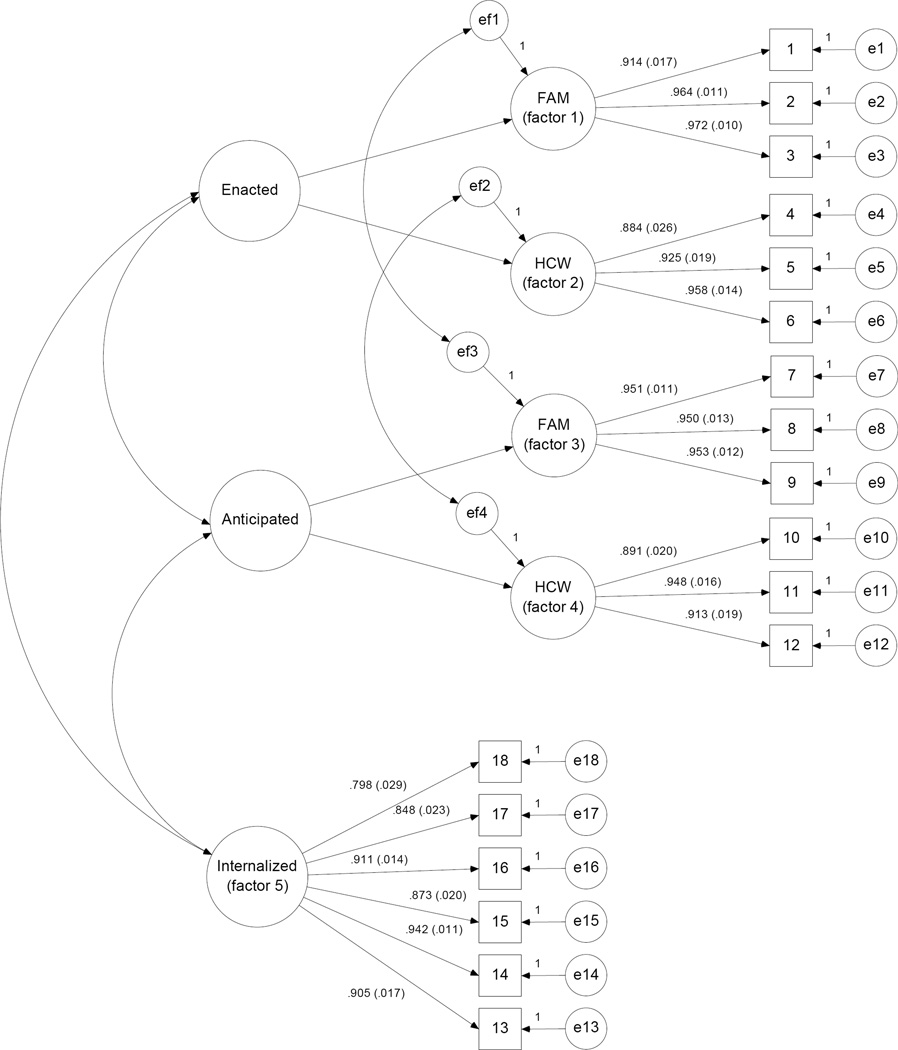
3.2 Structural Validity
As depicted in Figure 1, a 5-factor model solution was assessed to capture participants’ experiences of the three stigma mechanisms (2nd Order Factors: enacted, anticipated, internalized) from the two external stigma sources (1st Order Factors: family and healthcare workers). Correlated error variance was specified for reported experiences of enacted and anticipated stigma from the same sigma source (e.g., enacted and anticipated stigma from family). Confirmatory factor analysis was conducted in MPlus 7.0 based on the covariance matrix using maximum likelihood (ML) estimation, using data observed from the pooled sample (N = 178). The 5-factor model converged, suggesting good model fit (RMSEA = 0.071, 90%CI = 0.057 – 0.84, p-close = .009; CFI = 0.991; TLI = 0.990). Standardized parameter estimates for the 5-factor model are presented in Table 3, which demonstrate all items from the SU-SMS significantly (p < .001) and substantially (factor loadings range: .798 - .972) load on their hypothesized constructs. The model explained a substantial amount of item variance within the hypothesized Enacted (R2 = .718 - .946), Anticipated (R2 = .794 - .908), and Internalized (R2 = .637 - .888) stigma mechanisms. In addition, modification indices suggested that model fit would not be improved by altering our hypothesized 5-factor model. In sum, the data suggest that the SU-SMS is structurally valid.
Figure 1.
Structural Validity: 5- Factor Latent Variable Measurement Model with Standardized Factor Loadings (N = 178)
NOTE: SU-SMS items correspond to the item numbers that appear in boxes (observed variables), SU-SMS latent factors appear as circles, and measurement error variance ‘e’ is represented for each SU-SMS item and first order factor. FAM = ‘Family members’ stigma source, HCW = ‘Healthcare Workers’ stigma source.
Table 3.
Structural Validity: Five-factor SU-Stigma Mechanism model standardized estimates (N =178)
| Construct | Source | Item | Factor Loading (SE) | ||
|---|---|---|---|---|---|
| Enacted | |||||
| Factor 1 | FAM | 1. | Family members have thought that I cannot be trusted. |
0.914*** | (0.017) |
| FAM | 2. | Family members have looked down on me. | 0.964*** | (0.011) | |
| FAM | 3. | Family members have treated me differently. | 0.972*** | (0.010) | |
| Factor 2 | HCW | 4. | Healthcare workers have not listened to my concerns. |
0.884*** | (0.026) |
| HCW | 5. | Healthcare workers have thought that I’m pill shopping, or trying to con them into giving me prescription medications to get high or sell. |
0.925*** | (0.019) | |
| HCW | 6. | Healthcare workers have given me poor care. | 0.958*** | (0.014) | |
| Anticipated | |||||
| Factor 3 | FAM | 7. | Family members will think that I cannot be trusted. | 0.951*** | (0.011) |
| FAM | 8. | Family members will look down on me. | 0.950*** | (0.013) | |
| FAM | 9. | Family members will treat me differently. | 0.953*** | (0.012) | |
| Factor 4 | HCW | 10. | Healthcare workers will not listen to my concerns. | 0.891*** | (0.020) |
| HCW | 11. | Healthcare workers will think that I’m pill shopping, or trying to con them into giving me prescription medications to get high or sell. |
0.948*** | (0.016) | |
| HCW | 12. | Healthcare workers will give me poor care. | 0.913*** | (0.019) | |
| Internalized | |||||
| Factor 5 | SELF | 13. | Having used alcohol/drugs makes me feel like I’m a bad person. |
0.905*** | (0.017) |
| SELF | 14. | I feel I’m not as good as others because I use alcohol/drugs. |
0.942*** | (0.011) | |
| SELF | 15. | I feel ashamed of having used alcohol/drugs. | 0.873*** | (0.020) | |
| SELF | 16. | I think less of myself because I used alcohol/drugs. | 0.911*** | (0.014) | |
| SELF | 17. | Having used alcohol/drugs makes me feel unclean. | 0.848*** | (0.023) | |
| SELF | 18. | Having used alcohol/drugs is disgusting to me. | 0.798*** | (0.029) | |
FAM = ‘Family members’ stigma source, HCW = ‘Healthcare Workers’ stigma source.
Factor loading is significant at 0.001 (***), 0.01(**), or 0.05(*) level (2-tailed).
Further support for the hypothesized 5-factor model is provided via correlations between subscales of the SU-SMS in the pooled sample. In order to allow for equal comparisons between scales and subscales, three HIV clinical care participants with missing values on the SU-SMS were excluded (N = 175). Specifically, Table 4 shows a correlation that is large in effect size but below .800 between the Enacted and Anticipated subscales indicating that they are closely related but distinct constructs (Brown, 2006). Correlations between the Enacted and Anticipated subscales with the Internalized subscale were also large in effect size, but of a slightly smaller magnitude, suggesting internalized stigma is a unique but related stigma construct. Correlations between family and healthcare workers stigma source subscales measuring Enacted and Anticipated stigma from different sources were medium-to-large in effect size but below .800, indicating that they are related but non-overlapping (Brown, 2006). In sum, the data suggest that the SU-SMS assesses three distinct stigma mechanisms stemming from unique sources.
Table 4.
Structural Validity: Associations within and between the substance use stigma mechanisms scale in the pooled sample (N = 175)
| Stigma Mechanisms: | Enacted | Anticipated | Internalized | |||||
|---|---|---|---|---|---|---|---|---|
| Scale (subscales): | Total | FAM | HCW | Total | FAM | HCW | Total | |
| Enacted | Total | 1.00 | ||||||
| FAM subscale | .901** | 1.00 | ||||||
| HCW subscale | .844** | .528** | 1.00 | |||||
| Anticipated | Total | .731** | .637** | .673** | 1.00 | |||
| FAM subscale | .625** | .637** | .472** | .907** | 1.00 | |||
| HCW subscale | .658** | .461** | .733** | .882** | .602** | 1.00 | ||
| Internalized | Total | .544** | .481** | .513** | .544** | .512** | .432** | 1.00 |
FAM = ‘Family members’ stigma source sub-scale. HCW = ‘Healthcare Workers’ stigma source sub-scale.
Correlation is significant at the 0.001 (***), 0.01(**), or 0.05(*) (2-tailed).
3.3 Scale Reliability and Generalizability
As an indicator of reliability, we assessed the internal consistency of the SU-SMS and its subscales with Cronbach’s Alpha (see Table 5). In the pooled sample of participants with no missing values on the SU-SMS (N = 175), high internal consistency was achieved across all stigma mechanisms scales (α = .90 - .93) and sub-scales (α = .90 - .95). Good scale reliability was maintained across both independent samples (MMT participants: α = .84 - .94; HIV clinical care participants: α = .83 - .94). The SU-SMS scale was therefore an internally reliable measure among two diverse samples of substance-involved adults.
Table 5.
Scale Reliability: Internal consistency and mean stigma levels observed within and between pooled and independent samples (N = 175)
| Total (N = 175) | MMT Clinic (n = 93) | HIV Care (n = 82) | Difference test | |||||
|---|---|---|---|---|---|---|---|---|
| Scales (subscales) | M (SD) | α | MMMT (SD) | α | MMMT (SD) | α | | MMMT- MHIV| | |
| Enacted Stigma | (k=6) | 2.30 (1.16) | .90 | 2.92 (1.01) | .84 | 1.60 (0.89) | .86 | 1.32 *** |
| Family Members | (k=3) | 2.63 (1.47) | .95 | 3.29 (1.24) | .92 | 1.88 (1.34) | .94 | 1.41 *** |
| Healthcare Workers | (k=3) | 1.97 (1.97) | .90 | 2.55 (1.23) | .88 | 1.30 (0.70) | .83 | 1.25 *** |
| Anticipated Stigma | (k=6) | 2.40 (1.12) | .91 | 2.90 (1.06) | .90 | 1.83 (0.90) | .87 | 1.07*** |
| Family Members | (k=3) | 2.47 (1.33) | .95 | 2.94 (1.24) | .94 | 1.94 (1.22) | .93 | 1.00 *** |
| Healthcare Workers | (k=3) | 2.33 (1.18) | .90 | 2.86 (1.17) | .89 | 1.73 (0.87) | .85 | 1.13 *** |
| Internalized | (k=6) | 2.75 (1.10) | .93 | 3.23 (1.04) | .92 | 2.20 (0.90) | .89 | 1.03*** |
k = number of items in the scale or subscale, respectively.
Independent samples t-test was used to evaluate significant differences in scale means by sample.
Mean difference between samples is significant at the 0.001 (***), 0.01(**), or 0.05(*) level (2-tailed).
As an additional indicator of generalizability, we compared mean scores on the SU-SMS and its subscales between MMT participants and HIV clinical care participants (see Table 5). As hypothesized, mean levels of substance use stigma were significantly higher among the MMT participants than the HIV clinical care participants. Participants of both samples had higher mean scores on the Internalized substance use stigma subscale than the Enacted or Anticipated substance use stigma subscales. Moreover, mean scores on Enacted and Anticipated substance use stigma were higher from family than from healthcare workers.
3.4 Construct Validity
Construct validity of the SU-SMS was evaluated by assessing correlations between participant scores on the SU-SMS with scores on psychosocial constructs hypothesized to be related to, but distinct from Enacted, Anticipated, and Internalized substance use stigma. No psychosocial constructs were assessed in the MMT parent study; therefore, we present associations between the SU-SMS and psychosocial constructs only among the HIV clinical care participants. Table 6 presents convergent and divergent associations with constructs assessed for participants with no missing values on the SU-SMS (n = 82). In support of convergent validity, there were positive correlations between Enacted and Internalized substance use stigma with depressive symptoms. Anticipated substance use stigma was positively correlated with reporting a diagnosed anxiety disorder, although this correlation was marginally statistically significant (p = .06). Similarly, in respect to divergent validity, neither Enacted, Anticipated, nor Internalized stigma was associated with reporting a diagnosis of any mental health disorders in general. This pattern suggests specific mechanisms may have unique associations with specific cognitive-affective expressions. In further support of convergent validity, substance use stigma was moderately correlated with experiences of HIV stigma as measured by the HIV-SMS (Earnshaw et al., 2013a). Specifically, Enacted and Anticipated substance use stigma were positively correlated with Enacted and Anticipated HIV stigma, and Internalized substance use stigma was positively correlated with Internalized HIV stigma.
Table 6.
Construct Validity: Convergent and divergent associations with related constructs in HIV Clinical Care Sample (n = 82).
| Substance Use Stigma Mechanisms: | Enacted | Anticipated | Internalized | |
|---|---|---|---|---|
| Total | Total | Total | ||
| Mental Health Constructs | ||||
| CES-D 10 Score | .232* | −.012 | .221* | |
| Self-report any Mental Health Disorders | .073 | −.042 | .132 | |
| Self-report any Anxiety Disorders | .157 | .185± | .092 | |
| HIV Stigma Constructs | ||||
| Enacted HIV Stigma | .478** | .419** | .178 | |
| Anticipated HIV Stigma | .344** | .329** | .180 | |
| Internalized HIV Stigma | −.017 | −.022 | .272* | |
| WHO Moderate-High Risk Use | ||||
| Opiates, Cocaine, Crack | .270** | .000 | .204* | |
| Alcohol, Marijuana | .163 | .049 | .144 | |
| Substance Use Treatment | ||||
| Lifetime | .424** | .194* | .232* | |
| Past 30 days | .183 | .099 | .177 | |
Correlation is significant at the 0.001 (***), 0.01(**), or 0.05(*), or trends at the .06 (±) level (2-tailed).
As previously noted, lower rates of substance use severity were observed among HIV clinical care participants. Participants whose use of illicit drugs (opiates, cocaine, crack) was classified as moderate-to-high-risk (vs. low-risk) were positively associated with higher reported levels of Enacted and Internalized substance use stigma compared to moderate-to-high-risk users of substances seen as more socially acceptable or ‘recreational’ in nature (alcohol and marijuana). Similarly, Enacted, Anticipated, and Internalized substance use stigma were positively correlated with having a lifetime history of substance use treatment. The SU-SMS was not associated with recent substance use treatment.
4. DISCUSSION
The current study evaluated the psychometric properties of a new measure, the Substance Use Stigma Mechanisms Scale (SU-SMS), designed to measure theoretically distinct individual-level manifestations of substance use stigma across different stigma sources. The measure was successfully evaluated in two diverse populations with varying degrees of substance use severity and substance use treatment histories. Across these samples, data suggest the SU-SMS is a structurally valid, internally reliable scale for measuring three distinct stigma mechanisms (enacted, anticipated, and internalized stigma) from key stigma sources (family members and healthcare workers). As hypothesized, psychometrics of the SU-SMS were generalizable across the two independent samples, and reflect higher levels of substance use stigma associated with persons who would be characterized as engaging in misuse or abuse of more socially devalued substances and severity of use. In particular, associations between the SU-SMS mechanisms and available psychosocial metrics suggest the substance use stigma mechanisms are likely differentially associated with cognitive and affective outcomes.
Despite the SU-SMS’s theoretical and psychometric strengths, there are several limitations of the current validation study. While our sample size was within the acceptable range for confirmatory factor analysis with models of minimal to moderate complexity (N = 100–200; Kelloway, 2014), future evaluations of the SU-SMS’s structural validity could benefit from a larger pooled sample. Some assessment metrics (in-person interviews vs. paper and pencil), measures (self-report mental health diagnoses, differing time frames in recalling ‘recent’ substance use), and language preference of participants (n = 5 requested the Spanish version of the SU-SMS) were limited by pre-existing study protocols, restricting our abilities to assess for possible response differences between modes of administration. Future validation work would be enhanced by controlling route of administration across diverse samples, and assessing additional convergent/discriminant validity by incorporating clinically diagnostic mental health measures, as well as other related constructs such as shame, perceived stigma, self-efficacy, and self-esteem. Samples were also limited to substance using populations in the Northeastern United States and may not be generalizable to other settings across the US and abroad. These samples also did not reflect the experiences of younger persons with active SUDs nor persons with clinical chemical dependency who are not in treatment. Future work should validate the SU-SMS in other populations.
As a cross-sectional validation study, we anticipate future prospective work with this measure will help to support the unique predictive contributions of these three stigma mechanisms. In particular, with cross-sectional analyses it is not surprising to observe higher correlations between enacted and anticipated stigma. We hypothesize this reflects the interpersonal nature of these mechanism (vs. internalized stigma) and may tap into ways in which past experiences of enacted stigma might heighten anticipation that similar events may occur in the future. In drawing on the Stigma Framework, we would further expect that despite these observed correlations, enacted and anticipated stigma may have differential effects on the health and well-being of persons with SUDs (e.g., willingness to access substance use treatment/adopt safer injection practices [anticipated stigma] vs. sustained treatment success/HIV or Hepatitis C status [enacted stigma]). Similarly, we may find that distinguishing between stigma sources helps to identify a more nuanced understanding of how and from whom stigma presents as a barrier to accessing such services [anticipated stigma from providers] vs. maintaining optimal treatment and health outcomes [enacted stigma from family].
As a whole, the results suggest that the SU-SMS may be helpful in future work to assess substance use stigma among populations with a wide range of substance use histories, including in-treatment and out-of-treatment populations with SUDs. It is hoped that such work using the SU-SMS will help inform research critical to understanding the health and well-being of populations with SUDs. Future work examining engagement and retention in substance use treatment and harm reduction programs may also benefit from identifying whether substance use stigma mechanisms and stigma sources differentially predict treatment compliance or duration of treatment (Kulesza et al., 2013).
Substance use stigma is a recognized and pervasive barrier to improving health inequities among substance-involved populations (Room, 2005; Link and Phelan, 2006; Strathdee et al., 2012). The current work found the SU-SMS to be a valid and highly reliable measure to document experiences of substance use stigma. Through extending the current work to address noted limitations, the SU-SMS is positioned as a valuable tool for identifying which individual stigma mechanisms in which social contexts will be necessary to target via stigma reduction or stigma buffering interventions to improve the individual opportunities afforded to people with SUDs. Such efforts are critical to reduce social, health, and economic related inequities among substance-affected communities.
Supplementary Material
HIGHLIGHTS.
The current study evaluates a novel theory-based substance use stigma scale.
Generalizability of responses was observed in two independent diverse substance-using samples.
Results supports the validity and reliability of the substance use stigma scale.
Acknowledgments
The authors wish to thank the participants as well as the MMT and HIV care providers and clinic staff for their support of and contributions to this project.
Role of funding: A seed grant from the University of Connecticut’s Center for Health Intervention and Prevention partially funded this work. Grants from the National Institutes of Health supported the implementation and evaluation (F31MH093264, Smith; K02DA033139, Copenhaver; K24DA036955 and R25DA023021, Cunningham) and evaluation (K01DA039767, Smith) efforts of this work.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:.
Contributors: LRS and VAE are responsible for the conceptual development and analysis of the current, all authors (LRS, VAE, MMC, COC) contributed to the study implementation and interpretation of results.
Author Disclosure Statements:
Conflict of Interest: The authors have no conflicts of interests to declare.
REFRENCES
- Ahern J, Stuber J, Galea S. Stigma, discrimination and the health of illicit drug users. Drug Alcohol Depend. 2007;88:188–196. doi: 10.1016/j.drugalcdep.2006.10.014. [DOI] [PubMed] [Google Scholar]
- Allport G. The Nature of Prejudice. Cambridge, MA: Perseus Books; 1954. [Google Scholar]
- Beatty PC, Willis GB. Research synthesis: the practice of cognitive interviewing. Public Opin. Q. 2007;71:287–311. [Google Scholar]
- Bos AE, Pryor JB, Reeder GD, Stutterheim SE. Stigma: addvances in theory and research. Basic Appl. Soc. Psychol. 2013;35:1–9. [Google Scholar]
- Brewer MB, editor. The Social Psychology Of Intergroup Relations: Social Categorization, Ingroup Bias, And Outgroup Prejudice. New York, NY: Guilford Press; 2007. [Google Scholar]
- Brown T. Confirmatory Factor Analysis for Applied Research. New York: The Guilford Press; 2006. [Google Scholar]
- Dearing RL, Stuewig J, Tangney JP. On the importance of distinguishing shame from guilt: relations to problematic alcohol and drug use. Addict. Behav. 2005;30:1392–1404. doi: 10.1016/j.addbeh.2005.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: a review of HIV stigma mechanism measures. AIDS Behav. 2009;13:1160–1177. doi: 10.1007/s10461-009-9593-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among plwh: a test of the hiv stigma framework. AIDS Behav. 2013a;17:1785–1795. doi: 10.1007/s10461-013-0437-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw V, Smith L, Copenhaver M. Drug addiction stigma in the context of methadone maintenance therapy: an investigation into understudied sources of stigma. Int. J. Mental Health Addict. 2013b;11:110–122. doi: 10.1007/s11469-012-9402-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Quinn DM, Park CL. Anticipated stigma and quality of life among people living with chronic illnesses. Chronic Illn. 2012;8:79–88. doi: 10.1177/1742395311429393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortney J, Mukherjee S, Curran G, Fortney S, Han X, Booth BM. Factors associated with perceived stigma for alcohol use and treatment among at-risk drinkers. J. Behav. Health Serv. Res. 2004;31:418–429. doi: 10.1007/BF02287693. [DOI] [PubMed] [Google Scholar]
- Goffman E. Stigma: Notes on the Management of Spoiled Identity. New York: Touchstone; 1963. [Google Scholar]
- Herek GM, Capitanio JP, Widaman KF. Stigma, social risk, and health policy: public attitudes toward HIV surveillance policies and the social construction of illness. Health Psychol. 2003;22:533. doi: 10.1037/0278-6133.22.5.533. [DOI] [PubMed] [Google Scholar]
- Humeniuk R, Ali R, Babor TF, Farrell M, Formigoni ML, Jittiwutikarn J, De Lacerda RB, Ling W, Marsden J, Monteiro M. Validation of the alcohol, smoking and substance involvement screening test (ASSIST) Addiction. 2008;103:1039–1047. doi: 10.1111/j.1360-0443.2007.02114.x. [DOI] [PubMed] [Google Scholar]
- Irwin M, Artin KH, Oxman MN. Screening for depression in the older adult: criterion validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D) Arch. Intern. Med. 1999;159:1701–1704. doi: 10.1001/archinte.159.15.1701. [DOI] [PubMed] [Google Scholar]
- Jackson L, Parker J, Dykeman M, Gahagan J, Karabanow J. The power of relationships: Implications for safer and unsafe practices among injection drug users. Drugs Educ. Prev. Policy. 2010;17:189–204. [Google Scholar]
- Kelloway EK. Using Mplus for Structural Equation Modeling: A Researcher’s Guide. SAGE Publications; 2014. [Google Scholar]
- Keyes KM, Hatzenbuehler ML, McLaughlin KA, Link B, Olfson M, Grant BF, Hasin D. Stigma and treatment for alcohol disorders in the United States. Am. J. Epidemiol. 2010;172:1364–1372. doi: 10.1093/aje/kwq304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulesza M, Larimer ME, Rao D. Substance use related stigma: what we know and the way forward. J. Addict. Behave. Ther. Rehabil. 2013;27:2. doi: 10.4172/2324-9005.1000106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin C, Srikrishnan AK, Yang C, Johnson S, Solomon SS, Kumar S, Celentano DD, Solomon S. The relationship between drug use stigma and HIV injection risk behaviors among injection drug users in Chennai, India. Drug Alcohol Depend. 2010;110:221–227. doi: 10.1016/j.drugalcdep.2010.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG. Understanding labeling effects in the area of mental disorders: an assessment of the effects of expectations of rejection. Am. Sociol. Rev. 1987:96–112. [Google Scholar]
- Link BG, Phelan JC. Conceptualizing stigma. Ann. Rev. Sociol. 2001:363–385. [Google Scholar]
- Link BG, Struening EL, Rahav M, Phelan JC, Nuttbrock L. On stigma and its consequences: evidence from a longitudinal study of men with dual diagnoses of mental illness and substance abuse. J. Health Soc. Behav. 1997:177–190. [PubMed] [Google Scholar]
- Link BG, Phelan JC. Stigma and its public health implications. Lancet. 2006;367:528–529. doi: 10.1016/S0140-6736(06)68184-1. [DOI] [PubMed] [Google Scholar]
- Luoma JB, O’Hair AK, Kohlenberg BS, Hayes SC, Fletcher L. The development and psychometric properties of a new measure of perceived stigma toward substance users. Subst. Use Misuse. 2010;45:47–57. doi: 10.3109/10826080902864712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH. Minority stress and mental health in gay men. J. Health Soc. Behav. 1995;36:38–56. [PubMed] [Google Scholar]
- Minior T, Galea S, Stuber J, Ahern J, Ompad D. Racial differences in discrimination experiences and responses among minority substance users. Ethn. Dis. 2003;13:521–527. [PubMed] [Google Scholar]
- O’Connor LE, Berry JW, Inaba D, Weiss J, Morrison A. Shame, guilt, and depression in men and women in recovery from addiction. J. Subst. Abuse Treat. 1994;11:503–510. doi: 10.1016/0740-5472(94)90001-9. [DOI] [PubMed] [Google Scholar]
- Parker R, Aggleton P. HIV and AIDS-related stigma and discrimination: a conceptual framework and implications for action. Soc. Sci. Med. 2003;57:13–24. doi: 10.1016/s0277-9536(02)00304-0. [DOI] [PubMed] [Google Scholar]
- Phelan JC, Link BG, Dovidio JF. Stigma and prejudice: one animal or two? Soc. Sci. Med. 2008;67:358–367. doi: 10.1016/j.socscimed.2008.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pryor J, Reeder G. HIV-related stigma. PMPH-USA. 2011:790–806. [Google Scholar]
- Robison J, Gruman C, Gaztambide S, Blank K. Screening for depression in middle-aged and older Puerto Rican primary care patients. J. Gerontol. A. Biol. Sci. Med. Sci. 2002;57:M308–M314. doi: 10.1093/gerona/57.5.m308. [DOI] [PubMed] [Google Scholar]
- Room R. Stigma, social inequality and alcohol and drug use. Drug Alcohol Rev. 2005;24:143–155. doi: 10.1080/09595230500102434. [DOI] [PubMed] [Google Scholar]
- Ross MW, Timpson SC, Williams ML, Amos C, Bowen A. Stigma consciousness concerns related to drug use and sexuality in a sample of street-based male sex workers. Int. J. Sex. Health. 2007;19:57–67. [Google Scholar]
- Schomerus G, Corrigan PW, Klauer T, Kuwert P, Freyberger HJ, Lucht M. Self-stigma in alcohol dependence: consequences for drinking-refusal self-efficacy. Drug Alcohol Depend. 2011;114:12–17. doi: 10.1016/j.drugalcdep.2010.08.013. [DOI] [PubMed] [Google Scholar]
- Semple SJ, Grant I, Patterson TL. Utilization of drug treatment programs by methamphetamine users: the role of social stigma. Am. J. Addict. 2005;14:367–380. doi: 10.1080/10550490591006924. [DOI] [PubMed] [Google Scholar]
- Smith LR, Fisher JD, Cunningham CO, Amico KR. Understanding the behavioral determinants of retention in HIV care: a qualitative evaluation of a situated information, motivation, behavioral skills model of care initiation and maintenance. AIDS Patient Care STD. 2012;26:344–355. doi: 10.1089/apc.2011.0388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith SM, Dawson DA, Goldstein RB, Grant BF. Examining perceived alcoholism stigma effect on racial-ethnic disparities in treatment and quality of life among alcoholics. J. Stud. Alcohol Drugs. 2010;71:231–236. doi: 10.15288/jsad.2010.71.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strathdee SA, Shoptaw S, Dyer TP, Quan VM, Aramrattana A Substance Use Scientific Committee of the HIV Prevention Trials Network. Towards combination HIV prevention for injection drug users: addressing addictophobia, apathy and inattention. Curr. Opin. HIV AIDS. 2012;7:320–325. doi: 10.1097/COH.0b013e32835369ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stutterheim SE, Pryor JB, Bos AE, Hoogendijk R, Muris P, Schaalma HP. HIV-related stigma and psychological distress: the harmful effects of specific stigma manifestations in various social settings. AIDS. 2009;23:2353–2357. doi: 10.1097/QAD.0b013e3283320dce. [DOI] [PubMed] [Google Scholar]
- Tempalski B, Friedman R, Keem M, Cooper H, Friedman SR. NIMBY localism and national inequitable exclusion alliances: the case of syringe exchange programs in the United States. Geoforum. 2007;38:1250–1263. doi: 10.1016/j.geoforum.2007.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.