Abstract
Objective
This study aims to quantify the crash risk for truck drivers with multiple comorbid medical conditions, after adjusting for confounders.
Methods
This retrospective cohort of 38,184 drivers evaluated concomitant medical conditions and subsequent crash data between 1/1/2005–10/31/2012. Hazard ratios (HRs) and 95% confidence intervals (95% CI) were calculated for any cause and preventable crashes of varying severity.
Results
Drivers with three or more medical conditions had significantly increased risk of preventable Department of Transportation (DOT) reportable crashes (HR=2.53, 95% CI=1.65–3.88) and preventable crashes with injuries (HR=2.23, 95% CI=1.09–5.31) after adjustment for covariates. Similarly, adjusted HRs were 2.55 (95% CI=1.37–4.73) for any cause DOT-reportable crashes and 3.21 (95% CI=1.18–8.75) for any cause crashes with injuries.
Conclusions
Having three concomitant medical conditions may be a statistically significant risk factor for preventable and any cause DOT-reportable crashes and crashes with injuries.
Introduction
Commercial Motor Vehicle (CMV) drivers constitute one of the largest employment categories in the United States with an estimated 5.7 million CMV drivers, most of whom drive trucks.(1) Truck driving is also hazardous, as heavy and tractor trailer truck drivers in the US incurred 22.0 fatal injuries per 100,000 full-time equivalent workers in 2013, as compared to 3.4 per 100,000 full-time equivalent workers across all industries.(2) Every year since records were kept in 1975 through 2014, there has been an more than 3,100 large-truck crash fatalities in the US, with an upward trend over the past 5 years. (1, 3) Approximately 60,000 truck crashes with injuries were reported to the police over the past 5 years with an average cost per crash with injuries estimated to be between $331,000 and $533,000 and the average cost per crash involving a fatality between $7.2 and $11.7 million.(1, 3) It is estimated that 1,000 of the 3,700 yearly fatal truck crashes are believed to be due to the fault of the CMV driver, rather than another vehicle.(4) Some studies suggest these statistics are likely underestimates.(5–7)
CMV drivers are an understudied (8) and medically underserved (9) population, often lacking regular healthcare providers, having poor access to healthcare services and frequently relying on emergency rooms and urgent care centers. A recent systematic review of health promotion interventions among CMV drivers also concluded that they are currently an underserved occupational group in terms of healthcare and health promotion efforts which consistently has high rates of obesity and related co-morbidities.(10) CMV drivers with chronic medical conditions may present public safety concerns due to: (1) the size and speed of their vehicles, (11, 12) (2) the frequently poor functional status of these drivers, (11–14) (3), CMV driver’s poor utilization of the traditional health care system (11–13) and (4) the large numbers and severe impacts of truck crashes on public health and safety.(11, 12) While compared to total crashes, the frequency of truck crashes is relatively low, however, crashes involving trucks are generally more severe.(4)
Commercial Driver Health and Safety
U.S. CMV drivers are required by Federal Motor Carrier Safety Administration (FMCSA) regulations to obtain medical examinations at least every 2 years in order to maintain their commercial driver’s licenses. In spite of these required medical exams for licensure, commercial drivers have some of the highest rates of chronic diseases, occupational fatalities, and occupational injuries compared with other working populations.(15–23) While there are relatively few studies that have examined the association between crash risk and multiple medical condtions among CMV drivers, some published data have indicated an increased crash risk among obese CMV drivers.,(24, 25) cardiovascular disease,(15, 16, 26, 27) diabetes,(28) medication use, (29, 30), and sleep apnea.(31–33) One analysis reported that obese CMV drivers [body mass index (BMI) ≥ 30 kg/m2] have a significantly higher crash rate (>2.0 times) than non-obese CMV drivers.(24) Another study found associations with obesity and crashes among newly recruited CMV drivers.(34)
The poor health status of CMV drivers is commonly attributed to lifestyle (improper diet, inadequate physical activity, and poor sleep hygiene) and work environmental factors, although few data are available to understand the relative importance of these factors.(35–38) Combinations of medical conditions and/or medication use by drivers are suspected to increase their risk of being involved in crashes, however, there are no trucking-related data reported in this regard. (39) The only published study evaluating multiple medical conditions for drivers focused on general population, non-commercial drivers and found significantly increasing risks for crashes with increasing numbers of conditions.(40)
We hypothesized that there is an increased risk of preventable crashes among CMV drivers with multiple medical conditions in a large retrospective cohort after adjustments for confounding factors.
Methods
This study was approved by the University of Utah (IRB #35889) Institutional Review Board. This research linked two data sources using the driver’s commercial driver license number, to investigate relationships between personal and environmental risk factors, and interactions between these factors, while controlling for covariates.
Data Sources
Commercial Driver Medical Exam (CDME) methods for this study have been previously described (41, 42)and thus are only briefly described below. 25,36 Road Ready’s database is a large commercially-maintained dataset of CDMEs on drivers whose employers obtain CDMEs within the Road Ready network. The database includes CDMEs performed by numerous examiners on CMV drivers licensed in all 48 continental US states. Drivers are similar in health profiles (e.g. BMI, age, blood pressure, diabetes mellitus prevalence, etc.) to the overall truck driving population with an employer mix that includes private carriers, independent owner/operator drivers, and leased drivers for private carriers.(9, 15, 16, 20, 23, 43–48)
CDME, employment and crash data from January 1, 2005 to October 31, 2012 were analyzed. Data from before and after these times were not available. Data elements included: demographics (age and gender), medical history (e.g., neurological problems, medications, sleep disorders, diabetes mellitus), measured height, measured weight, calculated body mass index, blood pressure, heart rate, urinalysis, and other medical exams (e.g., vision, cardiovascular, hearing whisper test). For the present investigation, if drivers had multiple CDMEs in the 2005–2012 timeframe, only the first CDME was analyzed. CDMEs from the database were then further restricted to those of drivers from a single large trucking firm in order to match medical information with detailed crash data that would allow for the calculation of accurate estimates of crash risks (see below).
A large U.S. truck company’s database (n~15,000 current drivers, n~70,000 drivers over the past 35 years) was accessed under a non-disclosure agreement. Company data included miles driven, segments driven, driving tenure, vehicle type, and all reported crashes involving the drivers.
Risk Factors
This study used the FMCSA Medical Review Board’s (MRB) multiple conditions matrix to assign drivers to risk groups (left column of Table 1). The purpose of the matrix is to provide guidance regarding CMV driver certification length based on combinations of concomitant diseases and consensus opinion regarding increased risk for CMV crashes. Where exact matrix data were unavailable, comparable data were used for most elements from the CDME (right column of Table 1). As specified by the FMCSA MRB, the thirteen conditions are equally weighted within this matrix and were tallied to represent the number of medical conditions present for these analyses. This tool was selected as the primary measure because it is the only tool designed categorize drivers according to multiple concomitant conditions, with the presumption that there is an increased crash risk with increasing number of conditions. The temporal relationship between concomitant medical conditions and crashes has not been demonstrated.
Table 1.
Multiple Conditions Matrix and Data Used from the Exam Form for each Condition
| Multiple conditions for qualified certification time from the Federal Motor Carrier Safety Administration’s Medical Review Board 31, 32 | Data used in this analysis from the Road Ready database of Commercial Driver Medical Exam forms |
|---|---|
|
| |
| 1. Body mass index>35 kg/m2 | Body mass index>35 kg/m2 |
| 2. Diabetes mellitus requiring medication | Diabetes mellitus controlled by medication |
| 3. Cardiovascular disease or Dysrhythmias | Heart disease, heart surgery or heart abnormalities |
| 4. Hypertension | Elevated blood pressure above 140/90 mmHg, or hypertension medication, or self-reported history of hypertension |
| 5. Requirement for a visual exemption | Corrected vision in both eyes worse than 20/40 or horizontal field of vision <70° degrees in either eye |
| 6. Obstructive sleep apnea | Sleep problems |
| 7. Renal disease | Kidney disease |
| 8. Pulmonary disease with pulmonary function test abnormality | Lung and chest abnormalities |
| 9. Epilepsy seizure free for >10 years | Seizures/epilepsy |
| 10. Musculoskeletal disease requiring medical, surgical or prosthetic treatment | Spine or other musculoskeletal disorder |
| 11. Stroke | Stroke or paralysis |
| 12. Major psychiatric illness (as defined pending formal review by the Medical Review Board) | Nervous or psychiatric disorders |
| 13. Opioid or benzodiazepine use | Opioid or benzodiazepine medication, including generic and trade names, in the record |
Crash Occurrence and Outcomes
Crash data were accessed and the date of the crash was the event date. We considered only those crashes occurring subsequent to the CDME. The available crash data have multiple crash outcomes: 1) any crash, 2) DOT-reportable crash, and 3) DOT-reportable crash resulting in injuries. A crash of any severity was defined by the company as “any time the vehicle comes in contact with any other vehicle, object, person, animal, or property causing damage or injury or any allegation of contact or involvement in any manner, however minor.” DOT-reportable crashes are a subset of total crashes where either: A) there is a fatality, B) one or more persons receives medical treatment away from the site of the crash as a result of injuries sustained from the crash, and/or C) where one or more vehicle(s) are towed from the scene. The most severe crash outcome evaluated is defined as a DOT-reportable crash resulting in either an injury or fatality. Consistent with other large programs in the industry, the company in this study has a crash investigation team that investigates all crashes and determines if the crash was or was not preventable. The determination is made by the company based on driver interviews, police reports, and other data. Preventable crashes are those crashes where the determination is that the crash could have been averted with driver action. Thus, all three crash outcomes were assessed in groups consisting of either preventable crashes, as well as in total (all crashes: both preventable and not preventable).
Covariates
Multiple covariates were assessed and adjusted for in the multivariable models (explained in the next section), including age, and gender, body mass index (BMI). Hazard ratios were also adjusted for: 1) length of medical certification, 2) reported narcotic or habit forming drug use, 3) if a drug test was performed at the time of the crash, 4) diagnosed muscular disease, 5) seat belt use at the time of the crash, 6) seizure history and 7) estimated impact speed of the crash. These were selected a priori based on potential for relationships with increasing number of medical conditions or increased severity of a crash.
Statistical Analyses
Analyses were performed using SAS 9.3 (SAS Institute, Cary NC, USA). Data were analyzed between 3/1/2015–3/28/16. Time-to-event data were available for all drivers. For those drivers not involved in a crash, theirhis or her last observation date in the study was the later of either a) the last date employed by the trucking company or b) the date his or her CDL was revoked due to a failed subsequent CDME. The latter criterion was also the same criterion for those with either single or multiple examinations. Time was calculated as the number of days between the exam and either crash or termination from the company. The analyses resulted in an estimated crash risk and adjusted hazard ratio for potential individual and environmental risk factors.
This study’s unit of analysis is a single crash, with additional analyses of repeated crashes as separate observations. The outcomes are binary (e.g., crash vs. no crash). The main analyses were analyses of the recurrent (repeated) time-to-event data using the Prentice, Williams, Peterson (1981) conditional risk set model (under the proportional hazard) for ordered failure events.
In initial univariate analysis, the continuous variables (e.g., age and BMI) were assessed for linearity. When adjusting for confounder effects, we carefully assessed potential co-linearity between predictors. Model fit were assessed using Markov chain Monte Carlo algorithms and numerical integration using adaptive quadrature methods. Variables included in the model were selected a priori based on factors thought to influence crash and severity risk. The analysis plan was created prior to linking the data and evaluating relationships. All tests are two-sided, a p-value less than 0.05 indicates the statistically significant result. Missing data were excluded from analyses.
Results
There were 38,184 drivers (49,464 records) in the RR database who also had a driving record from the large truck company. There were 13,472 total crashes and 10,350 preventable crashes among these 38,184 drivers. The driver level descriptive statistics are provided in Table 2.
Table 2.
Descriptive Statistics Stratified by Number of Concomitant Medical Conditions
| Variablen (%) or mean ± SD | 0 Conditions (N=32,697, 66.10 %) | 1 Condition (N=14,684, 29.69 %) | 2 Conditions (N=2,001, 4.05%) | 3 or more conditions (N=82, 0.17 %) | Total (N=49,464) |
|---|---|---|---|---|---|
| Age | 47.4 ±10.4 | 47.4 ±10.4 | 48.7 ±10.2 | 50.4 ±11.3 | 47.4 ±10.4 |
| Body Mass Index | 28.1 ±3.9 | 37.8 ±7.3 | 39.7 ±6.7 | 39.7 ±6.3 | 31.4 ±7.1 |
| Gender (male) | 31401 (96.0%) | 13840 (94.2%) | 1922 (96.0%) | 81 (98.8%) | 47244 (98.8%) |
| BMI Category | |||||
| Underweight below 18.5 | 197 (0.60%) | 10 (0.07%) | 0 | 0 | 207 (0.42%) |
| Normal Wt. 18.5–24.9 | 7258 (22.2%) | 590 (4.0%) | 31 (1.6%) | 0 | 7879 (15.9%) |
| Overweight 25.0–29.9 | 13817 (42.3%) | 1605 (10.9%) | 109 (5.4%) | 4 (4.9%) | 15535 (31.4%) |
| Obese 30.0–34.9 | 11408 (34.9%) | 1563 (10.6%) | 103 (5.6%) | 0 | 13074 (26.4%) |
| Morbidly Obese ≥ 35.0 | 17 (0.05%) | 10916 (74.3%) | 1758 (87.9%) | 78 (95.1%) | 12769 (25.8%) |
| Diabetes Mellitus | 1420 (4.3%) | 1396 (9.5%) | 212 (10.6%) | 9 (11.0%) | 3037 (6.1%) |
| Heart Disease | 0 | 238 (1.6%) | 234 (11.7%) | 44 (53.7%) | 516 (1.0%) |
| High Blood Pressure | 3637 (11.1%) | 3600 (24.5%) | 675 (33.7%) | 30 (36.6%) | 7942 (16.1%) |
| Nervous Disorders | 460 (1.4%) | 319 (2.2%) | 39 (2.0%) | 2 (2.4%) | 820 (1.7%) |
| Sleep Disorders | 244 (0.8%) | 539 (3.7%) | 77 (3.8%) | 3 (3.7%) | 863 (1.7%) |
| Chronic Low Back Pain | 157 (0.5%) | 101 (0.7%) | 20 (1.0%) | 0 | 278 (0.6%) |
| Seizure Epilepsy | 18 (0.06%) | 2 (0.01%) | 0 | 0 | 20 (0.04%) |
| Certification Length | |||||
| Failed | 312 (1.0%) | 366 (2.5%) | 118 (5.9%) | 8 (9.8%) | 804 (1.6%) |
| Periodic | 5951 (18.2%) | 6670 (45.4%) | 1549 (77.4%) | 65 (79.3%) | 14235 (28.8%) |
| Qualified | 26059 (79.7%) | 7293 (49.7%) | 227 (11.3%) | 1 (1.2%) | 33580 (67.9%) |
| Temp Disqualified | 375 (1.2%) | 355 (2.4%) | 107 (5.4%) | 8 (9.8%) | 845 (1.7%) |
| Drug Use | 43 (0.1%) | 17 (0.1%) | 2 (0.1%) | 1 (1.2%) | 63 (0.1%) |
| Miles Driven | 74322.9 ±108745.2 | 78715.8 ±112062.7 | 64582.2 ±90563.9 | 29014.5 ±38126.4 | 75234.8 ±109119.1 |
| Drug test | 191 (2.2%) | 95 (2.3%) | 11 (2.2%) | 1 (5.3%) | 298 (2.2%) |
| Speed category | |||||
| 0 | 6822 (20.9%) | 3089 (21.0%) | 379 (18.9%) | 14 (17.1%) | 10304 (20.8%) |
| 1–51 | 1436 (4.4%) | 640 (4.4%) | 76 (3.8%) | 5 (6.1%) | 2157 (4.4%) |
| 51–80 | 631 (1.9%) | 341 (2.3%) | 39 (2.0%) | 0 | 1011 (2.0%) |
| Seatbelt use | 3233 (96.3%) | 1624 (95.5%) | 209 (96.8%) | 7 (77.8%) | 5073 (96.0%) |
| Crash with fatalities | 16 (0.05%) | 8 (0.05%) | 3 (0.2%) | 0 | 27 (0.05%) |
| DOT reportable Crash | 782 (2.4%) | 387 (2.6%) | 43 (2.2%) | 4 (4.9%) | 1216 (2.5%) |
| DOT reportable injuries | 206 (0.6%) | 91 (0.6%) | 13 (0.6%) | 2 (2.4%) | 312 (0.6%) |
| Preventable crashes | 6876 (21.03) | 3092 (21.06) | 369 (18.49) | 13 (15.85) | 10350 (20.92) |
Note Drug use defined as self-reported narcotic or habit forming drug use N=44,182, missing information of seatbelt use at the time of the crash. N=35,992 missing data for drug test after a crash. N=4 missing for heart disease. N=35,992 missing for speed category. N=35,992 missing for DOT reportable injuries.
Any Crash
Among combined crashes of any severity, which includes minor crashes where no vehicles were towed, drivers having 4 or more medical conditions were significantly more likely to be involved in a crash (Table 3). A Kaplan-Meier Survival Curve (Figure 1) visually demonstrates the difference in probability of being crash-free between drivers with increasing number of multiple medical conditions. Our finding was present for the unadjusted model as well as both adjusted models (one model adjusted for age, gender, BMI; a second model adjusted for age, gender, BMI, certification length, drug use, drug test, muscular disease, seatbelt use, seizure history and speed). Univariate analyses, drivers with one medical condition were significantly less likely to be involved in either a crash of any severity or a preventable crash of any severity. However, this protective relationship for drivers with 1 condition was not present in either of the fully adjusted models, or in the partially adjusted model for preventable crashes of any severity, suggesting the lack of an independently protective effect.
Table 3.
Hazard Ratios and Confidence Intervals for Concomitant Medical Conditions and Any Cause or Preventable‡ Crashes
| Number of Conditions | Hazard Ratio | 95% Confidence Interval | Hazard Ratio | 95% Confidence Interval | |||
|---|---|---|---|---|---|---|---|
| Crash of Any severity | Preventable‡ Crash of Any Severity | ||||||
| Unadjusted | 0 | 1.00 | Reference | 1.00 | Reference | ||
| 1 | 0.94 | 0.90 | 0.98 | 0.93 | 0.89 | 0.97 | |
| 2 | 0.92 | 0.84 | 1.01 | 0.89 | 0.80 | 1.00 | |
| 3 | 1.15 | 0.71 | 1.87 | 1.00 | 0.60 | 1.65 | |
| 4 or more | 3.63 | 3.51 | 3.76 | N/A | |||
| Model 1* | 0 | 1.00 | Reference | 1.00 | Reference | ||
| 1 | 1.02 | 0.96 | 1.09 | 1.03 | 0.95 | 1.12 | |
| 2 | 1.01 | 0.91 | 1.13 | 1.01 | 0.89 | 1.15 | |
| 3 | 1.27 | 0.79 | 2.06 | 1.13 | 0.69 | 1.87 | |
| 4 or more | 4.16 | 3.85 | 4.51 | N/A | |||
| Model 2† | 0 | 1.00 | Reference | 1.00 | Reference | ||
| 1 | 1.03 | 0.92 | 1.15 | 1.05 | 0.93 | 1.19 | |
| 2 | 1.08 | 0.91 | 1.3 | 1.11 | 0.90 | 1.35 | |
| 3 | 1.32 | 0.84 | 2.1 | 0.98 | 0.62 | 1.53 | |
| 4 or more | 2.01 | 1.72 | 2.34 | N/A | |||
| DOT Reportable Crash | Preventable‡ DOT Reportable Crash | ||||||
| Unadjusted | 0 | 1.00 | Reference | 1.00 | Reference | ||
| 1 | 0.85 | 0.75 | 0.96 | 0.89 | 0.77 | 1.04 | |
| 2 | 0.97 | 0.76 | 1.24 | 0.9 | 0.55 | 1.47 | |
| 3 | 2.79 | 1.63 | 4.74 | 1.73 | 1.46 | 2.04 | |
| 4 or more | 1.78 | 1.58 | 2.01 | N/A | |||
| Model 1* | 0 | 1.00 | Reference | 1.00 | Reference | ||
| 1 | 0.83 | 0.65 | 1.05 | 1.06 | 0.82 | 1.39 | |
| 2 | 0.94 | 0.67 | 1.32 | 1.11 | 0.63 | 1.93 | |
| 3 | 2.63 | 1.49 | 4.89 | 2.15 | 1.54 | 3.01 | |
| 4 or more | 1.72 | 1.30 | 2.29 | N/A | |||
| Model 2† | 0 | 1.00 | Reference | 1.00 | Reference | ||
| 1 | 0.73 | 0.43 | 1.23 | 1.12 | 0.84 | 1.49 | |
| 2 | 0.97 | 0.53 | 1.75 | 1.2 | 0.66 | 2.20 | |
| 3 | 2.55 | 1.37 | 4.73 | 2.53 | 1.65 | 3.88 | |
| 4 or more | 1.62 | 0.91 | 3.11 | N/A | |||
| DOT Reportable Crash with Injuries | Preventable‡ DOT Reportable Crash with Injuries | ||||||
| Unadjusted | 0 | 1.00 | Reference | 1.00 | Reference | ||
| 1 | 0.86 | 0.66 | 1.11 | 0.96 | 0.70 | 1.32 | |
| 2 | 0.97 | 0.61 | 1.55 | 0.94 | 0.46 | 1.89 | |
| 3 or more | 3.36 | 1.43 | 7.91 | 2.01 | 1.41 | 2.83 | |
| Model 1* | 0 | 1.00 | Reference | 1.00 | Reference | ||
| 1 | 0.78 | 0.46 | 1.32 | 1.01 | 0.47 | 2.15 | |
| 2 | 0.89 | 0.45 | 1.77 | 1.01 | 0.38 | 2.65 | |
| 3 or more | 3.21 | 1.17 | 8.75 | 2.23 | 1.09 | 5.31 | |
Adjusted for Age, Gender and BMI
Adjusted for Age, Gender, BMI, Certification Length, Drug Use, Drug Test, Muscular Disease, Seatbelt Use, Seizure History and Speed
N/A- Not available, there were not enough preventable crashes to create a stable estimate for 4 or more medical conditions.
Preventable crashes are those identified as being preventable by the company’s crash investigation team
Figure 1.
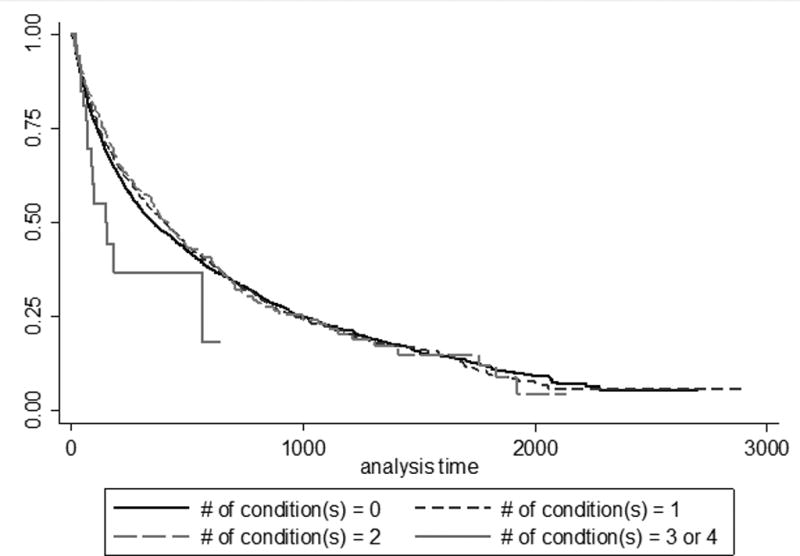
Survival Curve Demonstrating Survival Stratified by the Number of Conditions for Any Crash Event.
DOT Reportable Crashes
Among drivers with DOT-reportable crashes, the drivers with 3 medical conditions or 4 or more medical conditions were significantly more likely to be involved in a DOT-reportable crash and a preventable DOT-reportable crash. The hazard ratio was highest among drivers with 3 conditions and dropped slightly for those with 4 conditions. Drivers with one condition had a significantly protective hazard ratio for being in any DOT-reportable crash as compared to drivers with no medical conditions. Post hoc analyses excluding hypertension as one of the 13 medical conditions found there was no significant relationship between one medical condition and crash outcomes.
DOT Reportable Crashes with Injuries
Among drivers who had DOT-reportable crashes resulting in injuries, those drivers with 3 or more concomitant medical conditions were significantly more likely to be involved in both a crash resulting in injuries and a preventable crash resulting in injuries. These relationships remained after adjusting for potential confounders. It was not possible to adjust for all confounders seen in model 2 for other crash outcomes due to the small number of DOT-reportable crashes resulting in injuries.
There were many drivers who had two or more crashes, with most of them being any crash first followed by a DOT reportable crash or crash with injuries. Additional adjusted analyses were conducted which only included time-to-event to the first crash, then excluded from the study beyond that date. These analyses found meaningfully higher hazard ratios for both preventable DOT reportable crashes with injuries of any cause and preventable DOT crashes with injuries, with HR=5.12 (95% CI 1.14, 23.30) and HR=6.57 (95% CI 2.30, 18.81) respectively. Therefore, the true risk for having a preventable DOT reportable crash appears likely somewhere between the first-event hazard ratio estimate of 5.12 and the repeated-event hazard ratio estimate of 2.53. Similarly, the true risk for having a preventable DOT reportable crash with injuries is likely between the first-event hazard ratio estimate of 6.57 and the repeated-event hazard ratio estimate of 2.23. All of which were statistically significant.
Discussion
This large retrospective cohort study of commercial truck drivers found consistent relationships between multiple medical conditions and three different measures of crashes, including costly DOT-reportable crashes and crashes with injuries, with two- to three-fold increased risk estimates. Risks of being in a crash were elevated among truck drivers with either three, or four or more medical conditions. This is the first study to examine and quantify the assumption that multiple comorbid medical conditions are associated with an increased crash risk among truck drivers. These results support the MRB recommendations in that these drivers warrant increased scrutiny and have an increased risk of crash. Furthermore, these data suggest multiple comorbid medical conditions are preventable causes of injuries and fatalities resulting from crashes.
There was dose response relationship between multiple concomitant medical conditions and DOT-reportable crash risk, but this relationship did not continue into the highest medical condition category (4 or more conditions) although it remained statistically significant yet lower than crash risk for drivers with 3 conditions. This may be due in part to a probable strong survivor bias in these data. Industry wide, if drivers are involved in a more severe crash (e.g., a DOT-reportable crash, particularly a crash with injuries), they are commonly removed from the driving pool, either through citation and loss of licensure, termination from the company, or prohibitive cost of repairing or insuring their vehicle if they are an owner operator. Smaller numbers of drivers with that many conditions may also limit the statistical power for greater numbers of medical conditions. The relative rarity of both numbers of drivers with 3 or more conditions and more severe crashes results in wide confidence bounds around the hazard ratio estimates. However, these hazard ratios are statistically significant and clinically meaningful, demonstrating a potentially causal association between having multiple medical conditions and subsequently having a crash. There is a meaningful difference in the crash risk estimate between those drivers with 2 conditions and those with 3 conditions. This may be due to residual confounding, interactions between multiple medical conditions, or differences in reporting. It is widely believed that there is under-reporting of medical conditions among drivers, therefore our estimates are likely an underestimation of the true risk for crashes. Recent articles reported that when the driver’s BMI is >35 kg/m2, >90% have objectively diagnosed obstructive sleep apnea (OSA) and at BMI of 40 kg/m2 and above almost 100% have OSA.(33, 49) These data have lower self-reported sleep disorders for the number of drivers with BMI above 35 kg/m2. Further research into these complex relationships and potential underreporting is needed.
Additionally, it is likely that these estimates are an underestimate of the true risk due to changes in exposure after having a crash. Drivers who had crashes of any severity and were still employed by the company remained in the risk pool for having a more severe crash. These drivers are given additional driving and crash-avoidance training or paired up with another driver-trainer. Therefore, their risk for a subsequent crash changes meaningfully after the first crash of any severity if they remained employed by the company. The data in the primary analyses in the tables assumes that there is no change in exposure which is not true, but is the most conservative assumption.
This study’s strengths include the use of a large retrospective study with the ability to demonstrate temporality. Data were systematically captured across the population. The study was sufficiently powered to assess risk factor relationships with crash outcomes of three different severity measures. These findings may be generalizable to other trucking companies and other safety sensitive jobs. Another strength is the ability to assess the relationship between multiple comorbid conditions and differing severities of crash, including the DOT-reportable and preventable crashes, which are regarded as the most relevant in the trucking industry. Weaknesses include data that are limited to those collected as part of the CDME and the company. These data are comparable to other studies among commercial truck drivers as well as data from the American Trucking Association survey of members performed in 2010. There is no potential to gather additional data such as primary care provider records, and therefore we are unable to address additional factors that could cause or contribute to crashes that are not addressed in this study and may have importance in the commercial truck driving population. The hazard ratio estimates are calculated from relatively small numbers of drivers with 3 or more medical conditions and few crashes. These small sample sizes result in wider confidence bounds and limited ability to arrive at definitive conclusions. While the hazard ratio estimates may fall within a large range, these demonstrated temporal relationships between multiple conditions and multiple types of crash are statistically significant. Care should be taken when interpreting the true crash risk from multiple medical conditions due to the small sample size and rarity of some crash events. Additionally, although we did statistically adjust for BMI, many of the medical conditions have relationships with obesity. There are demonstrated relationships with increasing BMI and increasing counts of medical conditions.(41) Particularly, the relationship between increasing BMI and higher prevalence of OSA, which has repeatedly shown an association with crash risk, may be partially responsible for the increased risk of having a crash seen in these analyses.(49, 50) Similarly, age and male gender are associated with many of these health factors. We statistically adjusted for these confounding factors as well as BMI, however residual confounding may still exist. While we did perform analyses to control for driving tenure at the company, that was not a meaningful confounder in multivariate models and was not included in final models. However, age was included in final models and is generally collinear with driving experience. Unfortunately, the available data do not include total driving experience as a potential confounding factor, as only the tenure at the individual company was available. We evaluated company tenure and miles driven as potential confounders and found they had limited impact on the relationships between multiple medical conditions and crash risk and were not included in the final model.
Conclusion
Multiple comorbid medical conditions appear to be a risk factor for three different measures of crashes in this large population of CMV drivers. Risk estimates were more than two- to three-fold increased. This study supports the FMCSA Medical Review Board’s recommendations insofar as drivers with multiple conditions are at increased risk of being involved in a crash and therefore, merit additional scrutiny during medical certification examinations. These relationships remained after controlling for important confounders. Further research should focus on the identification of specific conditions from the multiple conditions matrix that increase crash risk, and that may be amenable to more aggressive treatment and more restrictive limits on driver certification that may reduce the risk of preventable crashes and related injuries and fatalities to truck drivers and the traveling public.
Acknowledgments
This study has been funded, in part, by the National Institute for Occupational Safety and Health (NIOSH/CDC), grant 1K01OH009794 and NIOSH Education and Research Center training grant 3TC42OH008414. The CDC/NIOSH was not involved in the design and conduct of the study; collection management analysis and interpretation of the data; and preparation, review or approval of the manuscript.
Footnotes
The authors have no relevant financial disclosures for this manuscript.
References
- 1.Administration FMCS. Commercial Motor Vehicle Facts. Mar, 2013. [Google Scholar]
- 2.U.S. Department of Labor BoLS. Chart 2. Number and rate of fatal occupational injuries, by industry sector, 2013* 2014. [Google Scholar]
- 3.Administration FMCS. Current FMCSA Crash Cost Figures. FMCSA; 2008. [Google Scholar]
- 4.Institute HLD. Large Truck Crash Fatality Facts. Insurance Institute for Highway Safety; 2014. [Google Scholar]
- 5.Sagberg F. Road accidents caused by drivers falling asleep. Acc Anal & Prevn. 1999;31:639–649. doi: 10.1016/s0001-4575(99)00023-8. [DOI] [PubMed] [Google Scholar]
- 6.Dinges DF. An overview of sleepiness and accidents. Journal of sleep research. 1995;4:4–14. doi: 10.1111/j.1365-2869.1995.tb00220.x. [DOI] [PubMed] [Google Scholar]
- 7.Valent F, Schiava F, Savonitto C, Gallo T, Brusaferro S, Barbone F. Risk factors for fatal road traffic accidents in Udine, Italy. Acc Anal & Prevn. 2002;34:71–84. doi: 10.1016/s0001-4575(00)00104-4. [DOI] [PubMed] [Google Scholar]
- 8.Anderson DG. Workplace violence in long haul trucking: occupational health nursing update. AAOHN J: Off J of the Amer Ass of Occ Hlth Nurses. 2004;52:23–27. [PubMed] [Google Scholar]
- 9.Solomon AJ, Doucette JT, Garland E, McGinn T. Healthcare and the long haul: Long distance truck drivers—a medically underserved population. American journal of industrial medicine. 2004;46:463–471. doi: 10.1002/ajim.20072. [DOI] [PubMed] [Google Scholar]
- 10.Ng MK, Yousuf B, Bigelow PL, Van Eerd D. Effectiveness of health promotion programmes for truck drivers: A systematic review. Health Education Journal. 2015;74:270–286. [Google Scholar]
- 11.Leigh JP, Miller TR. Job-related diseases and occupations within a large workers’ compensation data set. American journal of industrial medicine. 1998;33:197–211. doi: 10.1002/(sici)1097-0274(199803)33:3<197::aid-ajim1>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 12.Jones D, Switzer-McIntyre S. Falls from trucks: a descriptive study based on a workers compensation database. Work (Reading, Mass. 2003;20:179–184. [PubMed] [Google Scholar]
- 13.Muscat JE, Wynder EL. Diesel exhaust, diesel fumes, and laryngeal cancer. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 1995;112:437–440. doi: 10.1016/s0194-5998(95)70280-6. [DOI] [PubMed] [Google Scholar]
- 14.Hakkanen H, Summala H. Driver sleepiness-related problems, health status, and prolonged driving among professional heavy-vehicle drivers. Transportation Human Factors. 2000;2:151–171. [Google Scholar]
- 15.Ronna BB, Thiese MS, Ott U, et al. The Association Between Cardiovascular Disease Risk Factors and Motor Vehicle Crashes Among Professional Truck Drivers. Journal of occupational and environmental medicine / American College of Occupational and Environmental Medicine. 2016;58:828–832. doi: 10.1097/JOM.0000000000000806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thiese MS, Ott U, Robbins R, et al. Factors Associated With Truck Crashes in a Large Cross Section of Commercial Motor Vehicle Drivers. Journal of occupational and environmental medicine / American College of Occupational and Environmental Medicine. 2015;57:1098–1106. doi: 10.1097/JOM.0000000000000503. [DOI] [PubMed] [Google Scholar]
- 17.Thiese MS, Moffitt G, Hanowski RJ, Kales SN, Porter RJ, Hegmann KT. Repeated Cross-Sectional Assessment of Commercial Truck Driver Health. Journal of occupational and environmental medicine / American College of Occupational and Environmental Medicine. 2015;57:1022–1027. doi: 10.1097/JOM.0000000000000522. [DOI] [PubMed] [Google Scholar]
- 18.Olson R, Thompson SV, Wipfli B, et al. Sleep, Dietary, and Exercise Behavioral Clusters Among Truck Drivers With Obesity: Implications for Interventions. Journal of occupational and environmental medicine / American College of Occupational and Environmental Medicine. 2016;58:314–321. doi: 10.1097/JOM.0000000000000650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Birdsey J, Sieber WK, Chen GX, et al. National Survey of US Long-Haul Truck Driver Health and Injury: health behaviors. Journal of occupational and environmental medicine / American College of Occupational and Environmental Medicine. 2015;57:210–216. doi: 10.1097/JOM.0000000000000338. [DOI] [PubMed] [Google Scholar]
- 20.Sieber WK, Robinson CF, Birdsey J, et al. Obesity and other risk factors: the national survey of U.S. long-haul truck driver health and injury. American journal of industrial medicine. 2014;57:615–626. doi: 10.1002/ajim.22293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dahl S, Kaerlev L, Jensen A, et al. Hospitalization for lifestyle related diseases in long haul drivers compared with other truck drivers and the working population at large. Work (Reading, Mass. 2009;33:345–353. doi: 10.3233/WOR-2009-0882. [DOI] [PubMed] [Google Scholar]
- 22.Korelitz JJ, Fernandez AA, Uyeda VJ, Spivey GH, Browdy BL, Schmidt RT. Health habits and risk factors among truck drivers visiting a health booth during a trucker trade show. American journal of health promotion : AJHP. 1993;8:117–123. doi: 10.4278/0890-1171-8.2.117. [DOI] [PubMed] [Google Scholar]
- 23.Layne DM, Rogers B, Randolph SA. Health and gender comparisons in the long-haul trucking industry: a pilot study. AAOHN journal : official journal of the American Association of Occupational Health Nurses. 2009;57:405–413. doi: 10.3928/08910162-20090916-01. [DOI] [PubMed] [Google Scholar]
- 24.Stoohs RA, Guilleminault C, Itoi A, Dement WC. Traffic accidents in commercial long-haul truck drivers: the influence of sleep-disordered breathing and obesity. Sleep. 1994;17:619–623. [PubMed] [Google Scholar]
- 25.Anderson JE, Govada M, Steffen TK, et al. Obesity is associated with the future risk of heavy truck crashes among newly recruited commercial drivers. Acc Anal & Prevn. 2012;49:378–384. doi: 10.1016/j.aap.2012.02.018. [DOI] [PubMed] [Google Scholar]
- 26.Häkkänen H, Summala H. Fatal traffic accidents among trailer truck drivers and accident causes as viewed by other truck drivers. Acc Anal & Prevn. 2001;33:187–196. doi: 10.1016/s0001-4575(00)00030-0. [DOI] [PubMed] [Google Scholar]
- 27.Knipling RR. Three large truck crash categories: What they tell us about crash causation. Proceedings of the Driving Assessment 2009 Conference; 2009; pp. 31–37. [Google Scholar]
- 28.Laberge-Nadeau C, Dionne G, Ekoé J-M, et al. Impact of diabetes on crash risks of truck-permit holders and commercial drivers. Diabetes Care. 2000;23:612–617. doi: 10.2337/diacare.23.5.612. [DOI] [PubMed] [Google Scholar]
- 29.Gates J, Dubois S, Mullen N, Weaver B, Bédard M. The influence of stimulants on truck driver crash responsibility in fatal crashes. Forensic science international. 2013;228:15–20. doi: 10.1016/j.forsciint.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 30.Reguly P, Dubois S, Bedard M. Examining the impact of opioid analgesics on crash responsibility in truck drivers involved in fatal crashes. Forensic science international. 2014;234:154–161. doi: 10.1016/j.forsciint.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 31.Teran-Santos J, Jimenez-Gomez A, Cordero-Guevara J. The association between sleep apnea and the risk of traffic accidents. New England Journal of Medicine. 1999;340:847–851. doi: 10.1056/NEJM199903183401104. [DOI] [PubMed] [Google Scholar]
- 32.Stoohs RA, Itoi A, Guilleminault C, Dement WC. Sleep and sleep-disordered breathing in commercial long-haul truck drivers. CHEST Journal. 1995;107:1275–1282. doi: 10.1378/chest.107.5.1275. [DOI] [PubMed] [Google Scholar]
- 33.Burks SV, Anderson JE, Bombyk M, et al. Nonadherence with Employer-Mandated Sleep Apnea Treatment and Increased Risk of Serious Truck Crashes. Sleep. 2016;39:967–975. doi: 10.5665/sleep.5734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Anderson JE, Govada M, Steffen TK, et al. Obesity is associated with the future risk of heavy truck crashes among newly recruited commercial drivers. Accident Analysis & Prevention. 2012;49:378–384. doi: 10.1016/j.aap.2012.02.018. [DOI] [PubMed] [Google Scholar]
- 35.Backman AL. Health survey of professional drivers. Scand J Work Environ Health. 1983;9:30–35. doi: 10.5271/sjweh.2449. [DOI] [PubMed] [Google Scholar]
- 36.Lund AK, Preusser DF, Blomberg RD, Williams AF. Drug use by tractor-trailer drivers. J Forensic Sci. 1988;33:648–661. [PubMed] [Google Scholar]
- 37.Stoohs RA, Bingham LA, Itoi A, Guilleminault C, Dement WC. Sleep and sleep-disordered breathing in commercial long-haul truck drivers. Chest. 1995;107:1275–1282. doi: 10.1378/chest.107.5.1275. [DOI] [PubMed] [Google Scholar]
- 38.Robinson CF, Burnett CA. Truck drivers and heart disease in the United States, 1979–1990. American journal of industrial medicine. 2005;47:113–119. doi: 10.1002/ajim.20126. [DOI] [PubMed] [Google Scholar]
- 39.Hegmann KT, Andersson GB, Greenberg MI, Phillips B, Rizzo M. FMCSA’s Medical Review Board: Five Years of Progress in Commercial Driver Medical Examinations. Journal of Occupational and Environmental Medicine. 2012;54:424–430. doi: 10.1097/JOM.0b013e3182480535. [DOI] [PubMed] [Google Scholar]
- 40.Dow J, Gaudet M, Turmel E. Crash rates of Quebec drivers with medical conditions. Annals of advances in automotive medicine. 2013;57:57. [PMC free article] [PubMed] [Google Scholar]
- 41.Thiese MS, Moffitt G, Hanowski RJ, Kales SN, Porter RJ, Hegmann KT. Commercial driver medical examinations: prevalence of obesity, comorbidities, and certification outcomes. J Occup Environ Med. 2015;57:659–665. doi: 10.1097/JOM.0000000000000422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thiese MS, Moffitt G, Hanowski RJ, Kales SN, Porter RJ, Hegmann KT. Repeated cross-sectional assessment of commercial truck driver health. J Occup Environ Med. 2015;57:1022–1027. doi: 10.1097/JOM.0000000000000522. [DOI] [PubMed] [Google Scholar]
- 43.Angeles R, McDonough B, Howard M, et al. Primary health care needs for a priority population: A survey of professional truck drivers. Work (Reading, Mass. 2013 doi: 10.3233/WOR-131649. [DOI] [PubMed] [Google Scholar]
- 44.Apostolopoulos Y, Sonmez S, Shattell MM, Gonzales C, Fehrenbacher C. Health survey of U.S. long-haul truck drivers: work environment, physical health, and healthcare access. Work (Reading, Mass. 2013;46:113–123. doi: 10.3233/WOR-121553. [DOI] [PubMed] [Google Scholar]
- 45.Birdsey J, Sieber WK, Chen GX, et al. National survey of US long-haul truck driver health and injury: health behaviors. Journal of Occupational and Environmental Medicine. 2015;57:210–216. doi: 10.1097/JOM.0000000000000338. [DOI] [PubMed] [Google Scholar]
- 46.Burks S, Saager K. The Impact of Tenure, Experience, and Type of Work on the Turnover of Newly Hired Drivers at a Large Truckload Motor Carrier [Google Scholar]
- 47.Chen GX, Sieber WK, Lincoln JE, et al. NIOSH national survey of long-haul truck drivers: injury and safety. Accident Analysis & Prevention. 2015;85:66–72. doi: 10.1016/j.aap.2015.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Saberi HR, Moravveji AR, Fakharian E, Kashani MM, Dehdashti AR. Prevalence of metabolic syndrome in bus and truck drivers in Kashan, Iran. Diabetology & metabolic syndrome. 2011;3:8. doi: 10.1186/1758-5996-3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kales SN, Straubel MG. Obstructive sleep apnea in North American commercial drivers. Industrial health. 2014;52:13–24. doi: 10.2486/indhealth.2013-0206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Berger M, Varvarigou V, Rielly A, Czeisler CA, Malhotra A, Kales SN. Employer-Mandated Sleep Apnea Screening and Diagnosis in Commercial Drivers. Journal of Occupational and Environmental Medicine. 2012;54:1017–1025. doi: 10.1097/JOM.0b013e3182572e16. [DOI] [PMC free article] [PubMed] [Google Scholar]


