Abstract
Study objectives
Obstructive sleep apnea is common among patients with atrial fibrillation, but the prevalence and risk factors for atrial fibrillation among patients who are being investigated on suspicion of sleep apnea are not well known. The aim of the study was to estimate the prevalence of atrial fibrillation among patients investigated for suspected obstructive sleep apnea and to identify risk factors for atrial fibrillation among them.
Methods
The prevalence of atrial fibrillation was investigated among 201 patients referred for suspected obstructive sleep apnea. Patients without known atrial fibrillation were investigated with a standard 12-lead ECG at hospital and short intermittent handheld ECG recordings at home, during 14 days.
Results
Atrial fibrillation occurred in 13 of 201 subjects (6.5%), and in 12 of 61 men aged 60 years and older (20%). The prevalence of atrial fibrillation increased with sleep apnea severity (p = 0.038). All patients with atrial fibrillation were men and all had sleep apnea. Age 60 or older, the occurrence of central sleep apnea and diabetes mellitus were independent risk factors for atrial fibrillation after adjustments for body mass index, gender, sleep apnea and cardiovascular disease.
Conclusions
Atrial fibrillation is common among subjects referred for sleep apnea investigation and the prevalence of atrial fibrillation increases with sleep apnea severity. Independent risk factors for atrial fibrillation among patients investigated for suspected obstructive sleep apnea include the occurrence of coexisting central sleep apnea, age 60 years or older and diabetes mellitus.
Introduction
Obstructive sleep apnea with frequent upper airway obstructions followed by transient hypoxia occurs in as many as 80% of patients with atrial fibrillation and nasal continuous positive airway pressure therapy reduces the recurrence of atrial fibrillation after radiofrequency ablation in these patients [1–4]. Risk factors that are common to obstructive sleep apnea and atrial fibrillation include obesity, male gender, diabetes mellitus and age. Atrial fibrillation occurs in about 4% of subjects in the population aged 60–69 years and in about 10% of subjects aged 70–79 years [5, 6]. Atrial fibrillation is a risk factor for ischemic stroke, systemic embolism, heart failure and premature death [7, 8]. Obstructive sleep apnea is also a risk factor for cardiovascular disease and stroke [9–12]. Gami et al., using a questionnaire, suggested that obstructive sleep apnea was overrepresented among patients with atrial fibrillation [13]. Mehra et al. observed that participants in the sleep heart health study with severe sleep apnea had atrial fibrillation 4-times more often than those without sleep apnea [14]. Both Gami et al. and more recently Cadby et al. followed patients with obstructive sleep apnea prospectively and reported an increased risk for atrial fibrillation [15, 16]. The prevalence of atrial fibrillation, among patients seeking medical attention for sleep apnea investigation is however still unknown.
The aim of the present study was to estimate the prevalence of atrial fibrillation among patients under investigation for suspected obstructive sleep apnea and to identify risk factors for atrial fibrillation among these patients.
Materials and methods
Patients
The eligible population comprised 243 consecutive adults referred to the Department of Respiratory Medicine, University Hospital, Umeå, Sweden and to the Stockholm Heart Center, Sweden, for suspected obstructive sleep apnea. Thirty-three patients declined participation. Five patients who did not understand the study information and two who were unable to use a handheld ECG device were excluded. Included were 203 consecutive patients on days when a study nurse was present and handheld ECG devices for atrial fibrillation detection were available from April 2012 until November 2013.
Baseline investigations
All the patients answered a dichotomous questionnaire about a history of atrial fibrillation, congestive heart failure, hypertension, diabetes mellitus, previous stroke or transient ischemic attack, present medication and smoking. Weight, height and blood pressure were measured and all patients answered the Epworth Sleepiness Scale, which measures daytime sleepiness on eight questions with a score of 0–3 [17].
Overnight ambulatory sleep apnea recordings at home (Embletta X10 Systems, Kanata) included continuous recordings of airflow using a nasal flow pressure sensor, thoracic and abdominal respiratory effort (Xact Trace Belts, ResMed), finger pulsoximetry (Nonin Oximeter XPOD, MI) and a body position sensor.
All recordings were scored manually and the duration of sleep was estimated from the recordings. An obstructive apnea was defined as a drop in airflow of at least 90% of the pre-event baseline for ≥ 10 seconds with continuing abdominal and thoracic movements, according to the American Academy of Sleep Medicine [18, 19]. An obstructive hypopnea was defined as a 30% reduction in airflow for ≥ 10 seconds compared with baseline, accompanied by abdominal and thoracic movements, in combination with an oxygen desaturation of 3% or more. Central apneas were scored at absent respiratory effort throughout the entire period of absent airflow for ≥ 10 seconds. Mixed apneas were scored when both central and obstructive components occurred during an apnea. Sleep apnea was considered when the mean number of apneas and hypopneas per hour of sleep, i.e. the apnea-hypopnea index (AHI), was 5 or more. Obstructive sleep apnea was defined when the obstructive apnea-hypopnea index was 5 or more and central sleep apnea was defined when the central and mixed apnea-hypopnea index was 5 or more. Mild sleep apnea was considered when the apnea-hypopnea index was 5 to < 15, moderate sleep apnea when the apnea-hypopnea index was 15 to < 30 and severe sleep apnea when the apnea-hypopnea index was ≥ 30 [18].
Outcome measurements
A previous diagnosis of atrial fibrillation was verified from patient records. Patients without previously diagnosed atrial fibrillation were investigated using a standard 12-lead resting ECG. They were also instructed to record a 30-second ECG with a handheld ECG device (Zenicor-EKG®, Sweden) at home, regularly twice a day and when any cardiac symptom was present, for 14 days. The Zenicor-EKG® registers a bipolar extremity ECG lead I from both thumbs for 30 seconds. All the recordings were transmitted to a web-based central database via a built-in SIM card. Atrial fibrillation was defined as irregular supraventricular extra systoles in series for 30 seconds. The handheld ECG device is validated to a 12-lead ECG with a sensitivity of 96% and a specificity of 92% for a correct diagnosis of atrial fibrillation [20]. The Regional Ethics Committee at Stockholm University approved the study protocols and all the participants gave their written informed consent. The study complies with the Declaration of Helsinki.
Statistical analysis
Continuous variables were presented with the mean and standard deviation (±SD). Categorical variables were presented as numbers and percentages. Binary logistic regression was used for both univariate and multivariate analysis comparing patients with and without atrial fibrillation and variables were presented as the odds ratio (OR) and 95% confidence interval (CI). Covariates were chosen because of their relationship to sleep apnea, atrial fibrillation and stroke. A p-value of < 0.05 was considered significant. SPSS Statistics 22 (IBM Corporation, Route 100, Somers, NY 10589) was used for all calculations. The sample size was estimated at 146 patients plus 22 for potential loss, making 168 patients, to detect a significant difference of p < 0.05 with a power of 80% if the frequency of atrial fibrillation was 5% among patients with sleep apnea and 1.5% in patients without sleep apnea.
Results
The sleep apnea registration failed in two of 203 included patients, leaving 201 subjects for analysis. They had a mean age of 56 ± 12 years, a mean body-mass index of 30 ± 5.4 kg/m2 and 69% were men (Table 1). One hundred and seventy patients (85%) had sleep apnea with an apnea-hypopnea index of ≥ 5 and all but one patient had obstructive sleep apnea. Seventeen patients had central sleep apnea and 16 of these also had obstructive sleep apnea. Thirteen patients had atrial fibrillation, 11 were persistent and two had paroxysmal atrial fibrillation. Ten patients had a previous diagnosis of atrial fibrillation and three were new diagnoses. Among patients with known atrial fibrillation, none had been treated with ablative therapy.
Table 1. Baseline characteristics.
| Men [n, (%)] | 138 | (69) |
| Age [years, mean, SD] | 56 | ±12 |
| Heart Failure [n, (%)] | 9 | (4.6) |
| Hypertension [n, (%)] | 101 | (51) |
| Diabetes mellitus [n, (%)] | 20 | (10) |
| Stroke/Transient Ischemic Attack [n, (%)] | 6 | (3.1) |
| Ischemic heart disease [n, (%)] | 18 | (9.2) |
| Body mass index [kg/m2, mean, SD] | 30 | ±5.4 |
| Smoking [n, (%)] | 16 | (8.1) |
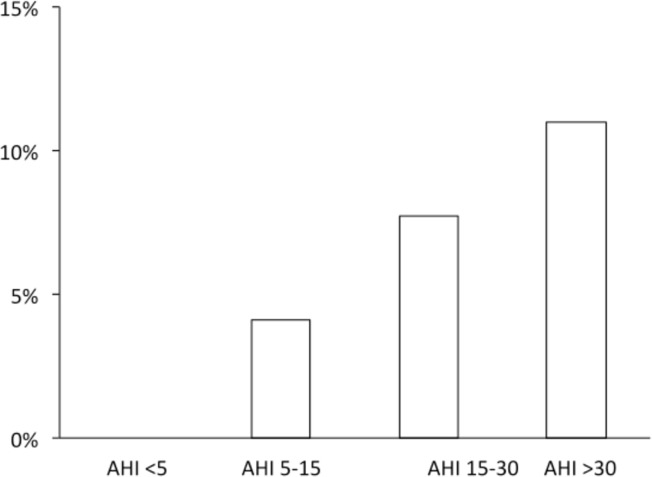
Atrial fibrillation occurred in 13 of 201 investigated patients (6.5%), and in 12 of 61 (20%) men aged 60 years and older. The prevalence of atrial fibrillation increased with the severity of sleep apnea, p = 0.038 (Fig 1).
Fig 1. Prevalence of atrial fibrillation in relation to AHI.
Prevalence of atrial fibrillation in relation to the severity of sleep apnea measured as the apnea-hypopnea index (AHI). (P = 0.038 for the trend).
All the patients with atrial fibrillation were men and they all had sleep apnea. Only one of 113 investigated patients younger than 60 had atrial fibrillation (0.9%), and 12 of 88 patients older than 60 had sleep apnea (14%), p <0.000. Atrial fibrillation occurred in six of 17 patients (35%) with concomitant central sleep apnea.
The occurrence of coexisting central sleep apnea, age over 60 years and diabetes mellitus were independently related to atrial fibrillation after adjustments for gender, body-mass index, sleep apnea and cardiovascular disease, including congestive heart failure, hypertension, ischemic heart disease, stroke and previous transient ischemic attacks (Table 2).
Table 2. Risk factors for atrial fibrillation.
| Unadjusted OR (95% CI) | p-value | Adjusted OR* (95% CI) | p-value | |
|---|---|---|---|---|
| Central sleep apnea | 13.6 (3.89–47.3) | <0.001 | 27.6 (3.84–199) | 0.001 |
| Age ≥ 60 years | 17.7 (2.25–139) | 0.006 | 12.2 (1.09–137) | 0.043 |
| Body mass index (1 unit) | 0.89 (0.78–1.01) | 0.077 | 0.82 (0.67–1.01) | 0.059 |
| Cardiovascular disease† | 1.85 (0.55–6.22) | 0.321 | 0.26 (0.03–2.08) | 0.203 |
| Diabetes mellitus | 4.67 (1.29–17) | 0.019 | 22.0 (2.29–211) | 0.007 |
*Gender and sleep apnea (apnea-hypopnea index ≥ 5) were included in the adjusted analysis, but OR and (95% CI) could not be estimated because of convergence failure, as all patients with atrial fibrillation were men and they all had sleep apnea.
†Cardiovascular disease included congestive heart failure, hypertension, ischemic heart disease and previous stroke or transient ischemic attack.
Discussion
Atrial fibrillation occurred in 7.6% of patients with sleep apnea (13 of 170) among subjects investigated for suspected obstructive sleep apnea. All the patients with atrial fibrillation were men and they all had sleep apnea. Age 60 or older, the occurrence of coexisting central sleep apnea and diabetes mellitus were independent risk factors for atrial fibrillation among those being investigated for a suspicion of sleep apnea. The prevalence of atrial fibrillation also increased with the severity of sleep apnea.
The frequency of sleep apnea among patients with atrial fibrillation has been extensively studied; however, the frequency of atrial fibrillation in sleep apnea has only been investigated in a few previous studies. Leung et al. investigated a subsample of 60 patients with idiopathic central sleep apnea without congestive heart failure, coronary artery disease or a previous stroke and 60 patients with obstructive sleep apnea [21]. They recorded atrial fibrillation during the whole night in 27% of patients with central sleep apnea and in 1.7% of patients with obstructive sleep apnea from a single ECG lead attached to the sleep apnea recordings. Mehra et al. reported that, in the Sleep Heart Health Study, atrial fibrillation occurred in 4.8% of 228 participants with severe disordered breathing versus 0.9% of 338 participants without, p = 0.003 [14]. We investigated a sample of non-selected patients referred for suspected sleep apnea and observed a higher frequency of atrial fibrillation among patients with obstructive sleep apnea. We did not exclude patients with cardiovascular disease and we searched for undiagnosed atrial fibrillation using intermittent recordings with a handheld ECG at home during 14 days, which could explain the higher prevalence of atrial fibrillation in the present study compared with the above-mentioned studies.
We scored apneas and hypopneas manually to distinguish central from obstructive sleep apneas and found that central apneas had a stronger relationship with atrial fibrillation than obstructive apneas. The mechanisms for the association between sleep apnea and atrial fibrillation are, however, still unclear and we can only speculate about them. Obstructive sleep apneas are followed by surges in sympathetic activity and increases in blood pressure and heart rate during apnea [22–24] and previous studies have therefore suggested that obstructive sleep apnea is a risk factor for atrial fibrillation [2, 3, 15]. Central sleep apnea, on the other hand, is generally regarded as the result of congestive heart failure or stroke, because of hypocapnia, reduced cardiac output and enhanced sensitivity to carbon dioxide [25–28]. Atrial fibrillation is highly related to central sleep apnea in heart failure patients and it is suggested that atrial fibrillation is a risk factor for central sleep apnea because it produces a further deterioration in cardiac output [28]. Leung et al. observed a high prevalence of atrial fibrillation also among patients with idiopathic central sleep apnea, i.e. patients without congestive heart failure [21]. They suggested that atrial fibrillation could induce central sleep apnea because of reduced pumping efficiency and raised pulmonary vascular pressure with hyperventilation, hypocapnia and respiratory system instability, or that idiopathic central sleep apnea may predispose some patients to atrial fibrillation because of impaired cardiac electrical stability. A recent study by Ghias et al. supports the hypothesis that central apnea could trigger atrial fibrillation, as they induced atrial fibrillation in anesthetized dogs during atrial and pulmonary vein programmed pacing by turning off a respirator for two minutes [29, 30].
We used a simplified sleep apnea investigation without EEG, which is a limitation when scoring sleep time. Using time in bed as a proxy of sleep time systematically underscores the apnea-hypopnea index. So, in this study, sleep was estimated manually from the respiratory recordings, which is a reliable method compared with polysomnography, with a pooled sensitivity of 93% and specificity of 92% [31]. Another limitation is that thirty-second intermittent ECG recordings could miss some atrial fibrillation episodes compared with continuous ECG recording, thereby underestimating the true prevalence of atrial fibrillation in the studied population.
Oral anticoagulants help to prevent stroke among patients with atrial fibrillation [32–34]. Atrial fibrillation can also be treated with antiarrhythmic drugs and pulmonary vein isolation to restore sinus rhythm. The effect of pulmonary vein isolation is further improved after nocturnal nasal continuous positive airway treatment of concomitant sleep apnea with a 42% relative risk reduction of atrial fibrillation recurrence [4] [35, 36]. Here, we report that atrial fibrillation is common among subjects being investigated for sleep apnea. To prevent stroke, there is evidence not only to search for sleep apnea in patients with atrial fibrillation, but also to search for atrial fibrillation during sleep apnea recordings.
Polysomnography, the golden standard for sleep apnea recordings includes a one-lead ECG (V5), which is often removed in simplified sleep apnea recordings. We suggest that such a one-lead ECG together with an analyzing program should be included also in simplified sleep apnea recordings to detect atrial fibrillation.
Conclusions
Atrial fibrillation is common among subjects who are referred for sleep apnea investigation and the prevalence of atrial fibrillation increases with sleep apnea severity. Independent risk factors for atrial fibrillation among patients investigated for suspected obstructive sleep apnea include the occurrence of coexisting central sleep apnea, age 60 years or older and diabetes mellitus.
Supporting information
(XLSX)
Acknowledgments
Johan Svensson, statistician, Department of Statistics, Umeå University, is acknowledged for statistical advice. Ann Chatrin Edlund, RN, Department of Medicine, Umeå, and Alicia Garcia Värild, RN, Stockholm Heart Center, are acknowledged for data collection.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was supported by grants from the Vinnvård Foundation, the Swedish Heart and Lung Foundation and Umeå University. Zenicor Medical Systems AB, Stockholm, provided handheld ECG devices (Zenicor-EKG®) at a reduced price. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
References
- 1.Kanagala R, Murali NS, Friedman PA, Ammash NM, Gersh BJ, Ballman KV, et al. Obstructive sleep apnea and the recurrence of atrial fibrillation. Circulation. 2003;107(20):2589–94. 10.1161/01.CIR.0000068337.25994.21 [DOI] [PubMed] [Google Scholar]
- 2.Braga B, Poyares D, Cintra F, Guilleminault C, Cirenza C, Horbach S, et al. Sleep-disordered breathing and chronic atrial fibrillation. Sleep Med. 2009;10(2):212–6. 10.1016/j.sleep.2007.12.007 [DOI] [PubMed] [Google Scholar]
- 3.Albuquerque FN, Calvin AD, Sert Kuniyoshi FH, Konecny T, Lopez-Jimenez F, Pressman GS, et al. Sleep-disordered breathing and excessive daytime sleepiness in patients with atrial fibrillation. Chest. 2012;141(4):967–73. PubMed Central PMCID: PMC3318950. 10.1378/chest.11-0975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shukla A, Aizer A, Holmes D, Fowler S, Park DS, Bernstein S, et al. Effect of Obstructive Sleep Apnea Treatment on Atrial Fibrillation Recurrence: A Meta-Analysis JACCCEP. 2015;1(1):41–51. [DOI] [PubMed] [Google Scholar]
- 5.Kannel WB, Wolf PA, Benjamin EJ, Levy D. Prevalence, incidence, prognosis, and predisposing conditions for atrial fibrillation: population-based estimates. Am J Cardiol. 1998;82(8A):2N–9N. [DOI] [PubMed] [Google Scholar]
- 6.Friberg L, Bergfeldt L. Atrial fibrillation prevalence revisited. J Intern Med. 2013;274(5):461–8. 10.1111/joim.12114 [DOI] [PubMed] [Google Scholar]
- 7.Benjamin EJ, Wolf PA, D'Agostino RB, Silbershatz H, Kannel WB, Levy D. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation. 1998;98(10):946–52. Epub 1998/09/16 [DOI] [PubMed] [Google Scholar]
- 8.Falk RH. Atrial fibrillation. N Engl J Med. 2001;344(14):1067–78. Epub 2001/04/05. 10.1056/NEJM200104053441407 [DOI] [PubMed] [Google Scholar]
- 9.Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005;353(19):2034–41. 10.1056/NEJMoa043104 [DOI] [PubMed] [Google Scholar]
- 10.Valham F, Mooe T, Rabben T, Stenlund H, Wiklund U, Franklin KA. Increased risk of stroke in patients with coronary artery disease and sleep apnea: a 10-year follow-up. Circulation. 2008;118(9):955–60. Epub 2008/08/14. 10.1161/CIRCULATIONAHA.108.783290 [DOI] [PubMed] [Google Scholar]
- 11.Marin JM. Sleep apnoea: from numbers to the people. J Intern Med. 2014;276(6):648–50. 10.1111/joim.12300 [DOI] [PubMed] [Google Scholar]
- 12.Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342(19):1378–84. 10.1056/NEJM200005113421901 [DOI] [PubMed] [Google Scholar]
- 13.Gami AS, Pressman G, Caples SM, Kanagala R, Gard JJ, Davison DE, et al. Association of atrial fibrillation and obstructive sleep apnea. Circulation. 2004;110(4):364–7. Epub 2004/07/14. 10.1161/01.CIR.0000136587.68725.8E [DOI] [PubMed] [Google Scholar]
- 14.Mehra R, Benjamin EJ, Shahar E, Gottlieb DJ, Nawabit R, Kirchner HL, et al. Association of nocturnal arrhythmias with sleep-disordered breathing: The Sleep Heart Health Study. Am J Respir Crit Care Med. 2006;173(8):910–6. 10.1164/rccm.200509-1442OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gami AS, Hodge DO, Herges RM, Olson EJ, Nykodym J, Kara T, et al. Obstructive sleep apnea, obesity, and the risk of incident atrial fibrillation. J Am Coll Cardiol. 2007;49(5):565–71. Epub 2007/02/06. 10.1016/j.jacc.2006.08.060 [DOI] [PubMed] [Google Scholar]
- 16.Cadby G, McArdle N, Briffa T, Hillman DR, Simpson L, Knuiman M, et al. Severity of OSA Is an Independent Predictor of Incident Atrial Fibrillation Hospitalization in a Large Sleep-Clinic Cohort. Chest. 2015;148(4):945–52. 10.1378/chest.15-0229 [DOI] [PubMed] [Google Scholar]
- 17.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–5. [DOI] [PubMed] [Google Scholar]
- 18.Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep. 1999;22(5):667–89. [PubMed] [Google Scholar]
- 19.Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8(5):597–619. PubMed Central PMCID: PMC3459210. 10.5664/jcsm.2172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Doliwa PS, Frykman V, Rosenqvist M. Short-term ECG for out of hospital detection of silent atrial fibrillation episodes. Scand Cardiovasc J. 2009;43(3):163–8. Epub 2008/12/20. 10.1080/14017430802593435 [DOI] [PubMed] [Google Scholar]
- 21.Leung RS, Huber MA, Rogge T, Maimon N, Chiu KL, Bradley TD. Association between atrial fibrillation and central sleep apnea. Sleep. 2005;28(12):1543–6. [DOI] [PubMed] [Google Scholar]
- 22.Balfors EM, Franklin KA. Impairment of cerebral perfusion during obstructive sleep apneas. Am J Respir Crit Care Med. 1994;150(6 Pt 1):1587–91. [DOI] [PubMed] [Google Scholar]
- 23.Hedner J, Ejnell H, Sellgren J, Hedner T, Wallin G. Is high and fluctuating muscle nerve sympathetic activity in the sleep apnoea syndrome of pathogenetic importance for the development of hypertension? J Hypertens Suppl. 1988;6(4):S529–31. [DOI] [PubMed] [Google Scholar]
- 24.Somers VK, Dyken ME, Clary MP, Abboud FM. Sympathetic neural mechanisms in obstructive sleep apnea. J Clin Invest. 1995;96(4):1897–904. PubMed Central PMCID: PMC185826. 10.1172/JCI118235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Javaheri S. A mechanism of central sleep apnea in patients with heart failure. N Engl J Med. 1999;341(13):949–54. 10.1056/NEJM199909233411304 [DOI] [PubMed] [Google Scholar]
- 26.Sahlin C, Sandberg O, Gustafson Y, Bucht G, Carlberg B, Stenlund H, et al. Obstructive sleep apnea is a risk factor for death in patients with stroke: a 10-year follow-up. Arch Intern Med. 2008;168(3):297–301. Epub 2008/02/13. 10.1001/archinternmed.2007.70 [DOI] [PubMed] [Google Scholar]
- 27.Parra O, Arboix A, Bechich S, Garcia-Eroles L, Montserrat JM, Lopez JA, et al. Time course of sleep-related breathing disorders in first-ever stroke or transient ischemic attack. Am J Respir Crit Care Med. 2000;161(2 Pt 1):375–80. [DOI] [PubMed] [Google Scholar]
- 28.Sin DD, Fitzgerald F, Parker JD, Newton G, Floras JS, Bradley TD. Risk factors for central and obstructive sleep apnea in 450 men and women with congestive heart failure. Am J Respir Crit Care Med. 1999;160(4):1101–6. 10.1164/ajrccm.160.4.9903020 [DOI] [PubMed] [Google Scholar]
- 29.Ghias M, Scherlag BJ, Lu Z, Niu G, Moers A, Jackman WM, et al. The role of ganglionated plexi in apnea-related atrial fibrillation. J Am Coll Cardiol. 2009;54(22):2075–83. 10.1016/j.jacc.2009.09.014 [DOI] [PubMed] [Google Scholar]
- 30.Asirvatham SJ, Kapa S. Sleep apnea and atrial fibrillation: the autonomic link. J Am Coll Cardiol. 2009;54(22):2084–6. 10.1016/j.jacc.2009.09.017 [DOI] [PubMed] [Google Scholar]
- 31.Franklin KA AS, Rehnqvist N. Obstructive sleep apnoea syndrome Report of a joint Nordic project. (SBU) Sbfmu, editor. Stockholm: Statens beredning för medicinsk utvärdering (SBU); 2007. [Google Scholar]
- 32.Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation—developed with the special contribution of the European Heart Rhythm Association. Europace. 2012;14(10):1385–413. Epub 2012/08/28. 10.1093/europace/eus305 [DOI] [PubMed] [Google Scholar]
- 33.Camm AJ, Kirchhof P, Lip GY, Schotten U, Savelieva I, Ernst S, et al. Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Eur Heart J. 2010;31(19):2369–429. Epub 2010/08/31. 10.1093/eurheartj/ehq278 [DOI] [PubMed] [Google Scholar]
- 34.Wilson D, Frontera A, Thomas G, Duncan E. Screening for atrial fibrillation in patients with obstructive sleep apnoea to reduce ischaemic strokes. Int J Cardiol. 2014;172(2):297–8. Epub 2014/01/29. 10.1016/j.ijcard.2014.01.007 [DOI] [PubMed] [Google Scholar]
- 35.Fein AS, Shvilkin A, Shah D, Haffajee CI, Das S, Kumar K, et al. Treatment of obstructive sleep apnea reduces the risk of atrial fibrillation recurrence after catheter ablation. J Am Coll Cardiol. 2013;62(4):300–5. 10.1016/j.jacc.2013.03.052 [DOI] [PubMed] [Google Scholar]
- 36.Neilan TG, Farhad H, Dodson JA, Shah RV, Abbasi SA, Bakker JP, et al. Effect of sleep apnea and continuous positive airway pressure on cardiac structure and recurrence of atrial fibrillation. J Am Heart Assoc. 2013;2(6):e000421 PubMed Central PMCID: PMCPMC3886742. 10.1161/JAHA.113.000421 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.