Abstract
The Zika virus outbreaks are unprecedented human threat in relation to congenital malformations and neurological/autoimmune complications. Since this virus has high potential to spread in regions presenting the vectors, improvement in mosquito control is a top priority. Thus, Aedes aegypti laboratory strains will be fundamental to support studies in different research fields implicated on Zika-mosquito interactions which are the basis for the development of innovative control methods. In this sense, our aim was to determine the main infection aspects of a Brazilian Zika strain in reference Aedes aegypti laboratory mosquitoes. We orally exposed Rockefeller, Higgs and Rexville mosquitoes to the Brazilian ZIKV (ZIKVBR) and qRT-PCR was applied to determine the infection, dissemination and detection rates of ZIKV in the collected saliva as well as viral levels in mosquito tissues. The three strains sustain the virus development but Higgs showed significantly lower viral loads in bodies at 14 days post-infection (dpi) and the lowest prevalences in bodies and heads. The Rockefeller strain was the most susceptible at 7 dpi but similar dissemination rates were observed at 14 dpi. Although variations exist, the ZIKVBR RNA shows detectable levels in saliva of the three strains at 14 dpi but is only detected in Rockefeller at 7 dpi. Moreover, saliva samples from the three strains were confirmed to be infectious when intrathoracically injected into mosquitoes. The ZIKVBR kinetics was monitored in Rockefeller mosquitoes and virus could be identified in the heads at 4 dpi but was more consistently detected late in infection. Our study presents the first evaluation on how Brazilian Zika virus behaves in reference Aedes aegypti strains and shed light on how the infection evolves over time. Vector competence and hallmarks of the ZIKVBR development were revealed in laboratory mosquitoes, providing additional information to accelerate studies focused on ZIKV-mosquito interactions.
Introduction
Currently, the world is facing a new outbreak of the emerging Zika virus (ZIKV) [1]. Its association with neurological and autoimmune complications as well as infants born with microcephaly [2,3] has caused a global healthcare crisis. Due to the severe situation, it was launched a document containing an operation plan to help affected countries to establish a strategy to control the disease and improvements in vector control were highlighted as priorities [4].
The outcome of vector infection will rely on the specific interactions between the mosquito and virus genotypes. Therefore, better understanding of the mosquito vectors-ZIKV interactions is the basis to generate the development of innovative strategies that can be added to the arsenal in the combat of ZIKV. Recently studies have reported significant differences in susceptibility for ZIKV infection between wild mosquito populations of Aedes aegypti, Aedes albopictus and other Aedes species [5–7]. These vector competence studies focusing on main vector species as well as variations in susceptibility of different populations from the same species are primordial to delineate improved control programs, prioritizing competent populations.
Although wild populations of the main vector, Ae. aegypti, represent the natural dynamics of the ZIKV infection process in the invertebrate host, the determination of the vector competence of different laboratory strains, which are well-adapted in captivity and readily available for experiments, is also essential to support basic and applied studies in different research fields related to vector-virus interactions. Moreover, some strains are also known to be standard in many laboratories in the world. They are used as reference mosquito strains because the experimental reproducibility is more robust than with field populations [8].
Important advances on mosquito immune responses to dengue virus (DENV) and other human pathogens have been performed on Ae. aegypti laboratory strains and natural mosquito populations for the purposes of comparison [8–10] as well as for the evaluation of insecticide resistance [11,12]. Furthermore, the characterization of the vector competence is relevant for more applied purposes. The development of transgenic mosquitoes mainly uses laboratory reference strains for transformation and the genetic background related to pathogen susceptibility is incorporated to the established lines. Thus, the vector competence of laboratory strains to ZIKV must be also considered in the context of the production and release of transgenic mosquitoes [13].
To generate basic information about the interaction between the Brazilian Zika virus strain (ZIKVBR) and three important laboratory-maintained Ae. aegypti strains, Rockefeller (ROCK), Higgs white eyes (HWE) and Rexville (RED) mosquitoes were analyzed. The ROCK strain, an insecticide-susceptible strain of Caribbean origin that was established in 1930 [14], is commonly used as a reference for insecticides resistance trials and in DENV infection experiments [15,16]. The HWE strain is an eye-pigment-deficient Ae. aegypti, a variant of the Rex-D strain, and it is used as the recipient for mosquitoes germ-line transformations, because the lack of pigment is a desirable phenotype for visual screening of transgenic individuals, which are often marked with a fluorescent protein expressed in the eyes [17]. The RED strain of Ae. aegypti, also a variant from Rex-D strain, is widely used to investigate pathogen-host susceptibility [18].
This report details the ZIKVBR infection, dissemination and the detection rates of ZIKV in the collected saliva and confirms the competence of these three mosquito strains to this virus. This study also reveals the viral kinetics in the ROCK reference strain.
Materials and methods
Ethics statement
The use of human blood or its derivatives products were conducted according to the principles expressed in the Declaration of Helsinki. The out-of-date preserved human blood (anonymized blood bag, expired for human use) was donated by the Fundação Pró-Sangue Hemocentro de São Paulo. No clinical study was conducted with this material and any surplus was discarded as biological waste after mosquito feeding experiment. The authorization of the blood bank was obtained and the approval of the protocol was provided by the Institutional Review Board in Human Research (IRB) (Comissão de Ética em Pesquisa com Seres Humanos do Instituto de Ciências Biomédicas/USP—CEPSH) and National Committee for Ethics in Research (Comissão Nacional de Ética em Pesquisa–CONEP), protocol #503. Number of approval: 914.876 (CAAE 38518114.0.0000.5467).
The Brazilian Zika virus strain, named as ZIKVBR, was previously isolated from a Brazilian clinical case [2] and a lyophilized virus sample was gently provided by the Evandro Chagas Institute in Belém, Pará. The use of the anonymized viral samples was approved by our Institutional Review Board (IRB). The research was approved by the Ethics Committee on the Research with Humans (CEPSH—Off.011616) of the Institute of Biosciences of the University of São Paulo.
Mosquito rearing
The experiments were performed using three Ae. aegypti laboratory strains: ROCK, HWE and RED. These mosquitoes were maintained in a BSL-2 insectary facility in Institute of Biomedical Sciences from University of São Paulo. The rearing conditions were 27 ± 1°C, 75–80% relative humidity with 12/12 hour (light/dark) photoperiod. Adult mosquitoes were maintained ad libitum on 10% sucrose solution (w/v).
Viral amplification and titration
The Brazilian Zika virus strain, named previously as ZIKVBR, was isolated from a Brazilian clinical case [2] and a lyophilized virus sample was gently provided by the Evandro Chagas Institute in Belém, Pará. ZIKVBR was amplified and titrated as recently described [2]. Viral titrated aliquots (5.0 x 106 plaque forming unit [pfu]/mL) of fourth subculture (T4) was provided by the ZIKV São Paulo task force.
Mosquito infection
Pre-mated 7–9 day old Ae. aegypti females were sucrose 10%-deprived for 24 hours prior blood meal. Starved females received ZIKVBR infectious blood meal by using the Glytube artificial feeder [19]. Human concentrated erythrocyte was mixed with ZIKVBR supernatant and inactivated human serum in a 10:10:1 proportion, respectively and the ZIKVBR final titer in this mixture was 2.2 x 106 pfu/mL. The infected-blood was offered to female mosquitoes for 45 minutes. Non-engorged females were removed and engorged ones were kept in plastic cups maintained with 10% sucrose solution until the collection times.
Mosquito saliva and tissue samples
Saliva, heads and bodies from 20 individual females orally exposed to ZIKVBR were collected at 7 and 14 days post-infection (dpi) for virus detection (10 mosquitoes for each strain, two independent experiments performed). For saliva, the forced salivation technique as used as previously described [20,21], with modifications. Mosquitoes were CO2 anaesthetized, transferred to a Petri dish on ice and legs and wings were removed with forceps. A glass slide with a strip of modeling clay was used to support micropipette tips filled with 10 μL of Leibovitz’s L-15 medium (Gibco™) and the proboscis of each live mosquito were inserted into the tip. Insects were allowed to salivate for 45 minutes and total volume was ejected into the 1.5 mL microtube. After salivation, heads were separated from the rest of the bodies using a McPherson-Vannas Scissors #501234 (World Precision Instruments, Sarasota, FL) and each tissue was transferred to a 1.5 mL microtube. Bodies, heads and saliva samples collected at 7 and 14 dpi were immediately frozen in dry ice and stored at -80°C.
Evaluation of ZIKVBR infectivity from the collected saliva
The presence of infectious ZIKVBR in the collected saliva from the 3 different mosquito strains was confirmed as previously described [22] with modifications. Saliva of 10 mosquitoes from each ROCK, HWE and RED strains were collected (as described above) at 7 and 14 dpi. A pool containing 1 μL of each mosquito saliva was immediately prepared and injected intratoracically in 5–7 day old female mosquitoes from HWE strain using the Nanoject II injector (Drummond Scientific Company, cat. no. 3-000-204). For each pool of saliva, an average of 276 nL were inoculated into a female. Between 20–25 mosquitoes were inoculated by each pool of saliva and needle was replaced before the injection of a different saliva sample to prevent contamination. On day 11 post-injection, mosquitoes were collected individually, total RNA was extracted from 5 mosquitoes and virus positivity was checked by qRT-PCR as described in the next sections.
RNA extraction of mosquito samples
Total RNA from individual heads, bodies and saliva were extracted using QIAmp Viral RNA Mini Kit (Qiagen, Valencia, CA, USA) following manufacturer’s recommendations. Total RNA was eluted in 60 μL of elution buffer and kept in -80°C until qRT-PCR analyses.
One-step qRT-PCR analysis
To detect ZIKV and to quantify viral copy numbers, the Power SYBR® Green RNA-to-CT™ 1-Step kit (Applied Biosystems, Foster City, CA, USA) was used in qRT-PCR reactions as described by the manufacturer. Each sample was analyzed in technical duplicates in a 20 μL final volume reactions containing 5 μL of total RNA and 0.5 μM for each ZIKV 835 and ZIKV 911c primers [23]. Negative (RNAse free water) and positive controls (500 ηg of total RNA extracted from ZIKV cell culture supernatant aliquot) were used in each assay. Samples were considered positive for ZIKV only when detected in both analyses. The assays were performed in Mastercycler Realplex 2 thermocycler (Eppendorf) with the following conditions: 48°C for 30 min and 95°C for 10 min followed by 40 cycles of 95°C for 30 sec, 60°C for 30 sec and a melting curve step of 95°C for 1 min, 60°C for 30 sec and 95°C for 1 min, with a temperature ramping from 60°C to 95°C at 0.02°C/sec. Amplicon specificity was evaluated by the peak of the melting curve (79 ± 1°C) and primer pair efficiency ranged from 1.01 to 1.02.
For ZIKV copy number estimation, a standard curve was generated as described [24], with some modification. Briefly, a target plasmid containing a 76 bp ZIKV fragment amplified with ZIKV 835 and ZIKV 911c primer pairs was linearized and nine serial dilutions ranging from 10−9 to 10−17 g were used to produce a standard curve. The limit of detection was experimentally established in 23 copies (10−16 g dilution). The ZIKV absolute copy numbers were extrapolated from the standard curves (R2 ranged from 0.990 to 0.996), adjusted by back-calculation to the total RNA volume (60 μL) and were expressed as copies per tissue.
Analyzes of the infection, dissemination and detection rates of ZIKVBR in the collected saliva
The infection rate (or prevalence) is determined as the proportion of mosquitoes with virus detected in body (abdomen and thorax) among tested ones. Dissemination rate corresponds to the number of mosquitoes with infected heads among infected bodies (abdomen and thorax positive). Since a method to detect viral RNA in saliva was used, the term detection rate of ZIKV in the collected saliva was applied in place of transmission rate (which refers to infectious particles present in saliva), but with equivalent estimation. The detection rate of ZIKV in the collected saliva was estimated as the proportion of mosquitoes with positive saliva among mosquitoes with disseminated infection (positive heads) and was expressed as percentages. The adopted definitions were in conformity with a previous study [5].
Data analysis
Statistical analyses were performed in GraphPad Prism5 software package (Version 5.00) for Windows (San Diego, California, USA) and confidence intervals of 95% were defined for all analyses. Fisher’s exact test were applied in conformity with [22] to detected significant differences in ZIKV positive proportions of the same tissues (bodies or heads or saliva) at 7 or 14 dpi from different mosquito strains and to compare infection proportions during ZIKV kinetics in ROCK strain. Viral levels between different Ae. aegypti lines were compared by using Two-way ANOVA and Bonferroni posttests.
Results
ZIKVBR infection and dissemination rates in orally challenged mosquito strains
To analyze and compare the infection susceptibility of Ae. aegypti laboratory strains to a ZIKV isolated in Brazil, we orally exposed ROCK, HWE and RED mosquitoes with a low-passage ZIKVBR strain. Viral RNA levels were quantified by qRT-PCR assay in individual mosquito bodies and heads at 7 and 14 dpi. These intervals are well-characterized indicators for infection establishment in the abdomen and viral dissemination to the head, respectively, during flavivirus replication progression in Ae. aegypti mosquitoes [25].
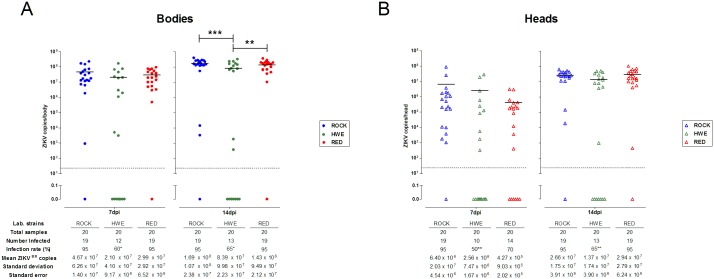
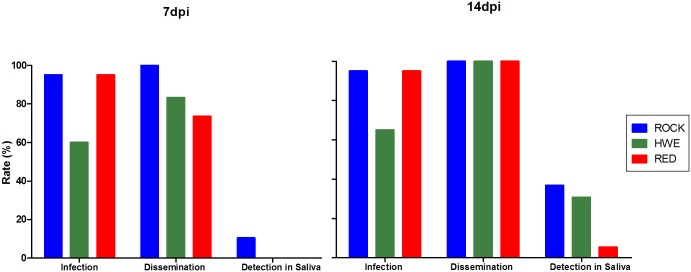
The three strains exhibited high viral levels in the bodies at 7 and 14 dpi, with the mean viral copy numbers fluctuating from 107 at 7 dpi to 108 at 14 dpi (Fig 1A). At 7 dpi, the ROCK and RED strains showed the highest and significantly different body infection rates (number of positive bodies/total mosquitoes tested) (95%) compared to HWE females (60%) (Fisher’s exact test, HWE x ROCK and HWE x RED, p = 0.0197). At 14 dpi, the body infection rate increased in HWE samples (65%) but significant lower prevalence (HWE x ROCK and HWE x RED, p = 0.0436) and viral levels were observed in relation to the ROCK and RED strains (two-way ANOVA followed by Bonferroni post-tests, HWE x ROCK, p<0.001 and HWE x RED, p<0.01), which remained at the same infection rate (95%) at this time (Fig 1A). However, the infection rate of the heads exhibited variation in the number of positive samples among the strains at 7 dpi, with ROCK at 95%, HWE at 50% and RED at 70%. At 14 dpi, the ROCK strain remained with 95% of the tested heads infected and the HWE and RED strains had increases in the percentage of infected heads to 65% and 95%, respectively (Figs 1 and 2). The ZIKV prevalence in heads of the HWE mosquitoes was significantly lower than the ROCK at 7 (HWE x ROCK, p = 0.0033) and the ROCK and RED at 14 dpi (HWE x ROCK and HWE x RED, p = 0.0033) (Fig 1B). With regard to the mean viral levels in the head, we observed that the RED strain had 105 ZIKV copies at 7 dpi and this number increased to 107 at 14 dpi, indicating an increase of 2 logs after 7 days, while the ROCK and HWE strains had infection level increases only 1 log (Fig 1B). When analyzing the dissemination rate (the number of infected heads/number of infected bodies), the ROCK strain had the highest index (100%) analyzed at 7 dpi in comparison with HWE (83%) and RED (74%) (lowest), and all the strains reached the same 100% dissemination rate at 14 dpi (Fig 2).
Fig 1. ZIKVBR infection rates and viral levels in bodies and heads from Ae. aegypti laboratory strains.
The infection rate and viral levels per tissue were individually recorded in ROCK, HWE and RED females at 7 and 14 days following a ZIKV-infected blood meal (dpi). (A) Viral prevalence and infection levels in the bodies. Each body sample is represented by a solid circle. The infection prevalences between HWE x ROCK and HWE x RED at 7 (*p = 0.0197) and 14 dpi (*p = 0.0436) were significant different by Fisher’s exact test. The viral infection levels of the HWE were significantly lower in the bodies at 14 dpi compared to the ROCK (***p<0.001) or RED (**p<0.01) by two-way ANOVA with Bonferroni post-tests. (B) Viral prevalence and infection levels in the heads. Individual heads are indicated by open triangles. The infection prevalences between HWE x ROCK (**p = 0.0033) at 7 dpi and HWE x ROCK and HWE x RED (**p = 0.0033) at 14 dpi were significantly different by Fisher’s exact test. Black bars indicate the mean viral copy numbers and the dashed grey line demonstrates the detection limit.
Fig 2. ZIKVBR infection, dissemination and detection rates of ZIKV in the collected saliva of Ae. aegypti laboratory strains.
The infection rate (number of infected bodies/total bodies analyzed), dissemination rate (number of infected heads/number of infected bodies) and the detection rate of ZIKV in the collected saliva (number of infected saliva sample/number of infected heads) were estimated in females from ROCK, HWE and RED strains at 7 and 14 days following a ZIKV-infected blood meal (dpi). The bars are representing the percentage values.
Prevalence and detection rate of ZIKVBR in mosquito saliva
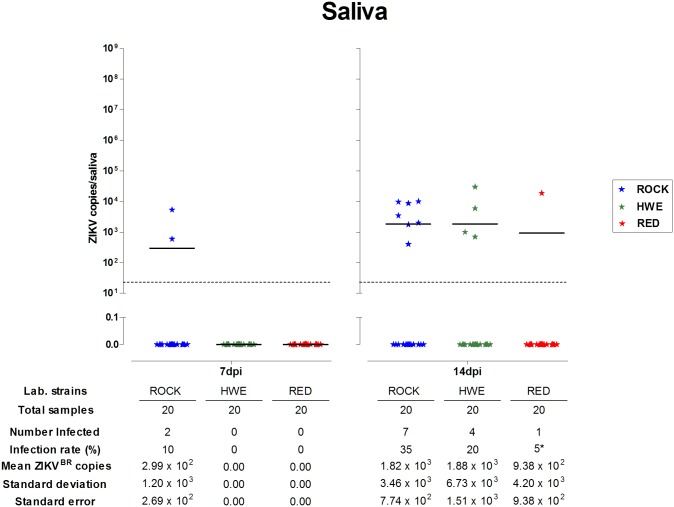
The presence of ZIKVBR and viral level quantitation were assessed directly for each collected saliva sample using the same qRT-PCR assay. ROCK strain females showed two positive saliva samples (10%) at 7 dpi. However, no ZIKVBR copy number was above the detection limit in saliva from HWE and RED mosquitoes at this time point. In contrast, saliva samples from the three strains presented detectable viral levels at 14 dpi. HWE samples were 20% positive for ZIKVBR, while ROCK and RED samples were 35% and 5%, respectively (Fig 3). Accordingly, the highest detection rate of ZIKV in the collected saliva (number of positive saliva samples/total number of infected heads) was observed in the ROCK strain (36.8%), followed by HWE (30.8%) and RED (5.3%) at 14 dpi (Fig 2).
Fig 3. ZIKVBR prevalence and viral levels in the collected saliva from Ae. aegypti laboratory strains.
The prevalence and viral levels per saliva sample were individually recorded in the ROCK, HWE and RED strains at 7 and 14 days following a ZIKV-infected blood meal (dpi). Each saliva sample is represented by a solid star. The prevalence of positive saliva between ROCK x RED was statistically different at 14 dpi (*p = 0.0436). Black bars indicate the mean viral copy numbers and the dashed grey line demonstrates the detection limit.
The mean viral levels in ROCK saliva increased 1 log (102 to 103) between 7 and 14 dpi. However, in comparison with ROCK, it was observed similar mean ZIKV levels in the RED and HWE saliva samples (varying between 9.38 x 102 to 1.88 x 103) at 14 dpi (Fig 3).
As observed in the bodies and heads, saliva samples showed strain variations related to the ZIKVBR detection rates and prevalence (Figs 2 and 3, respectively). The virus prevalence between ROCK and RED was significantly different at 14 dpi (Fisher’s exact test, p = 0.0436). However, no statistically significant differences were detected in the saliva viral levels (two-way ANOVA followed by Bonferroni post-tests, p>0.05) between the ROCK, HWE and RED strains at 7 and 14 dpi (Fig 3).
Confirmation of ZIKV infectivity in the collected saliva
The viability of ZIKVBR particles in the collected saliva was evaluated by intrathoracic injection into Ae. aegypti mosquitoes. Pools of saliva from the ROCK, HWE and RED strains collected at 7 or 14 dpi were capable to infect mosquitoes after 11 days post inoculation, confirming the presence of ZIKV infectious particles (Table 1).
Table 1. Prevalence of ZIKV-infected Ae. aegypti after 11 days post intrathoracic inoculation of saliva.
| Collected salivaa | Pool of saliva from Ae. aegypti strainsb | ||
|---|---|---|---|
| ROCK | HWE | RED | |
| 7dpi | 5/5 (100%) | 0/5 (0%) | 2/5 (40%) |
| 14dpi | 5/5 (100%) | 5/5 (100%) | 0/5 (0%) |
aDays post infection (dpi)
bNumber of positive mosquitoes/total tested (% of prevalence)
The qRT-PCR assay of the injected individuals demonstrated that the pools of saliva from the ROCK strain were infectious to Ae. aegypti mosquitoes (100% of the mosquito tested) when collected at 7 and 14 dpi. The same result was observed for the HWE pool of saliva collected at 14dpi, but no infected mosquito was detected when saliva was collected at 7 dpi. Differently, the pool of saliva from the RED strain was only infectious when collected at 7dpi (Table 1), even without individual saliva samples reaching the ZIKV detection limit (Fig 3), but only 40% of the inoculated mosquito was positive for ZIKV (Table 1). Moreover, the positive mosquitoes had high infection levels after 11 days post inoculation (between 107 to 108) (S1 Fig) indicating ZIKV replication. These results confirm that the ROCK, HWE and RED strains are competent to the ZIKVBR.
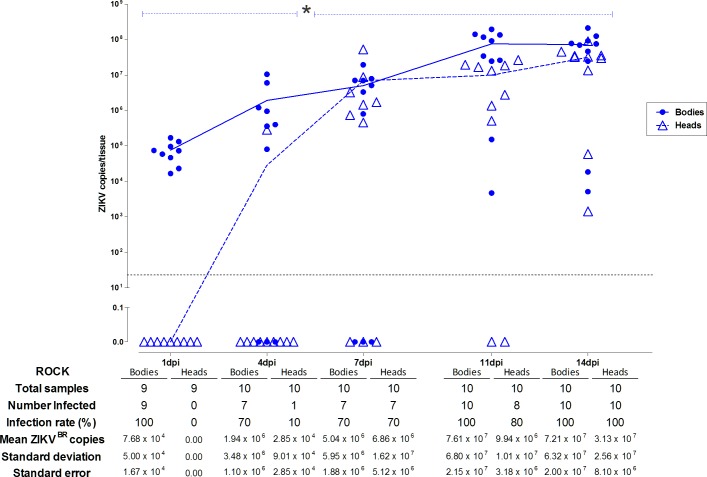
ZIKVBR invasion and establishment kinetics in the ROCK strain
ZIKVBR infection, dissemination and detection rates of ZIKV in the collected saliva were higher in the ROCK strain than the others strains tested (Fig 2). Moreover, the pools of saliva from this strain were infectious when collected at 7 and 14 dpi. This result led us to perform an independent experiment in order to determine the kinetics of ZIKVBR during the establishment and dissemination of infection in females from the ROCK strain. Five time-points post-infected blood meal (1, 4, 7, 11 and 14 dpi) were used to perform a quantitative analysis of the viral levels in the individual bodies and heads (Fig 4).
Fig 4. ZIKVBR kinetics in bodies and heads of Ae. aegypti from the ROCK strain.
The infection rate and viral levels per tissue were individually recorded at 1, 4, 7, 11 and 14 days following a ZIKV-infected blood meal (dpi). Solid circles and open triangles represent each body and head sample, respectively, from the ROCK females. Solid (body) and dashed (head) blue lines indicate the viral infection progression (mean levels) during the time-course experiment. Dashed blue bars indicate early (1 to 4 dpi) and late (7 to 14 dpi) infection stages in heads in which a significant difference in infection prevalence was observed between the two stages using Fisher’s exact test (*, 1 dpi x 7 dpi—p = 0.0031; 1 dpi x 11 dpi—p = 0.0007; 1dpi x 14 dpi—p<0.0001; 4 dpi x 7 dpi—p = 0.0198; 4 dpi x 11 dpi—p = 0.0055; 4 dpi x 14 dpi—p = 0.0001). The dashed grey line demonstrates the detection limit.
As expected, all the body samples analyzed were positive for ZIKVBR at 1 dpi and the mean viral levels was 7.68 x 104 copies. These results probably reflect the viral load ingested during the oral infection of the ROCK females and ZIKVBR particles still present in the infectious blood remaining in the blood bolus inside the midgut. Not surprisingly, none of the heads showed detectable levels of ZIKV in this period.
The detected viral copies increased gradually in the bodies and heads over the experimental time course. At 4 dpi, when the blood had been completely digested, the prevalence was 70% in the bodies and 10% in the heads, indicating that in some ROCK females, ZIKVBR infection can evolve more rapidly, reaching the head and producing high infection intensity in the nervous tissues (105) over a short period after infection (Fig 4).
The amount of infected bodies remained at the same level (70%) at 7 dpi, however, the number of virus-infected heads increased to 70% and the mean viral levels were enhanced by approximately 2 logs. ZIKVBR was detected in the bodies of all analyzed mosquito samples at 11 and 14 dpi. Furthermore, a viral level peak was reached at 11 dpi, and an infection plateau was maintained in the body tissues between the last two sampling times (Fig 4).
The ZIKVBR prevalence was 80% in the heads at 11 dpi and 100% at 14 dpi. The mean viral levels increased during the 14 days of infection from 0.0 to 3.13 X 107 copies in the heads of mosquitoes fed with a viral titer of 2.27 x 106 pfu/mL (final concentration). The infection rates of the ROCK head samples varied significantly between the early (1 dpi and 4 dpi) and late time points of infection (7, 11 and 14 dpi) (Fisher’s exact test, p<0.05).
Discussion
Basic knowledge on the ZIKV interactions with its vectors is one of the priorities in order to create a solid scientific foundation supporting traditional and innovative methods to face the Zika challenge [26]. The literature in this field is expanding with recent studies uncovering the main species naturally infected with ZIKV [27–29] and characterizing the viral susceptibility of the natural populations in regions with the potential for urban transmission [5,30]. As important as these studies including wild or recently colonized mosquitoes are, well-adapted laboratory vector strains will provide a consistent basis for reliable cellular and molecular studies of the virus-mosquito interaction, in which execution feasibility and reproducibility are essential.
Recently, the laboratory-adapted mosquito strains, HWE and Orlando (ORL), were used to describe the infection pattern of chikungunya virus (CHIKV). Both mosquito strains were susceptible to the CHIKV, and viral particles were detected in the saliva only two days after an infectious blood meal. The CHIKV infection pattern in midguts and dissemination rate were significantly lower for the ORL in comparison to the HWE strain until 3 dpi, although the HWE and ORL mosquitoes showed similar rates of virus in the saliva (60 and 65%, respectively) at 7 dpi [31].
Our study also found variations between laboratory-adapted strains during the ZIKV infection. Although Ae. aegypti infection dynamics is more rapid for the CHIKV (an alphavirus member from the Togaviridae family) than the ZIKV (a flavivirus from the Flaviviridae family), the HWE strain demonstrates lower saliva prevalence in comparison to the ROCK strain in early sampling time during ZIKVBR infection. The same pattern was observed in the HWE mosquitoes in relation to the ORL strain when exposed to the CHIKV [31].
CHIKV prevalence into saliva of the HWE increases from 20% at 2 dpi to 60% at 7 dpi, differing from the ORL strain (55% at 2 dpi to 65% at 7 dpi) [31]. Our study also demonstrates that the increase of the detection rates of ZIKVBR in the collected saliva was more pronounced in the HWE infected mosquitoes (0% at 7 dpi to 20% at 14 dpi) in relation to the RED (0% at 7 dpi to 5% at 14 dpi) and similar to the ROCK (10% at 7 dpi to 35% at 14 dpi). This result is surprising since the HWE has the lowest infection rate among the strains at 7 dpi while the ROCK mosquitoes showed ZIKVBR susceptibility that results in faster infection establishment and dissemination. More interestingly, the HWE strain showed the highest ZIKVBR load in the saliva at late infection stage and a similar result was demonstrated for the HWE mosquitoes infected with CHIKV [31].
American populations of Ae. aegypti were orally exposed to an Asian genotype of ZIKV and viral infection and dissemination were observed in the early days post-infection. Although the infection rates were high, dissemination and transmission rates were comparatively low [5]. The infection and detection rates of ZIKV in the collected saliva were similar to our results, but we found high dissemination rates in all Ae. aegypti strains tested.
Consistent with our findings with ZIKVBR infection in Ae. aegypti laboratory strains, other studies found the same high susceptibility in wild mosquito populations infected with different ZIKV strains, highlighting that the reference strains can mimic the infection pattern of wild population [5,32].
The present work adopted qRT-PCR as a rapid and efficient method to characterize vector competence [7] and to precisely measure the viral levels during the infection process [22,33]. Studies have shown a consistent correlation between viral RNA levels and infectious viral particles of different flaviviridae [34,35]. Based on ZIKVBR genome amplification, we measured the detection rates of ZIKV in the collected saliva to verify the ZIKVBR competence of three Ae. aegypti laboratory strains. The detection of virus RNA in the mosquito saliva indicated that salivary gland infection and escape barriers were overcome. These results were confirmed by the inoculation of saliva from the ROCK, HWE and RED strains in mosquitoes, generating late and consistent ZIKVBR infection in challenged females and revealing that Ae. aegypti mosquitoes from the ROCK, HWE and RED strains are competent to ZIKVBR.
Conclusions
The results from our study confirm that ROCK, HWE and RED laboratory strains not only sustain the development of the Brazilian Zika virus but are also competent for virus transmission. Moreover, we demonstrated that ROCK strain has the highest competence to ZIKVBR. These findings provide useful comparisons for future researches and will dictate the strains that suits best for desired experiments. In this sense, this knowledge is fundamental for Zika-invertebrate host studies, especially because we determined the main infection aspects of the ZIKVBR strain in reference Aedes aegypti laboratory mosquitoes. This knowledge is the first step to support the researches aiming to understand ZIKV-vector biology focusing innovative solutions on vector control.
Supporting information
The prevalence and viral levels per mosquito were recorded after 11 days post-injection of saliva pools collected from ROCK, HWE and RED at 7 and 14 dpi. Each mosquito is represented by a solid diamond. Black bars indicate the mean viral copy numbers and the dashed grey line demonstrates the detection limit.
(TIF)
Acknowledgments
We thanks Dr. Pedro Vasconcelos from Evandro Chagas Institute IEC in Belém for providing the lyophilized ZIKV isolate, Carla Torres Braconi for technical advices and Isabel Cristina dos Santos Marques and Ediane Saraiva Fernandes for technical assistance.
Data Availability
All relevant data are within the paper and its Supporting Information file.
Funding Statement
This work was funded by grants #2013/19921-9 and #2014/17766-9 from São Paulo Research Foundation, www.fapesp.br, grant 003/16 from Coordination for the Improvement of Higher Education Personnel, www.capes.gov.br, and National Institute of Science and Technology, Molecular Entomology, www.inctem.bioqmed.ufrj.br. ALCS and BBK were supported by fellowships #1252482 and #1497027 from Postdoctoral National Program of the Coordination for the Improvement of Higher Education Personnel - PNPD/CAPES. HRCA was supported by fellowship #2013/16609-4 from São Paulo Research Foundation. DBLO was supported by fellowship #5126/2015-00 from CAPES. RSI and SRM were supported by fellowships from CAPES. MLC was supported by fellowship #303341/2012-2, productivity in research, from Brazilian National Research Council, cnpq.br. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Musso D, Gubler DJ. Zika Virus. Clin Microbiol Rev. 2016;29: 487–524. 10.1128/CMR.00072-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cugola FR, Fernandes IR, Russo FB, Freitas BC, Dias JLM, Guimarães KP, et al. The Brazilian Zika virus strain causes birth defects in experimental models. Nature. Nature Publishing Group; 2016;534: 267–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mlakar J, Korva M, Tul N, Popović M, Poljšak-Prijatelj M, Mraz J, et al. Zika Virus Associated with Microcephaly. N Engl J Med. 2016;374: 951–958. 10.1056/NEJMoa1600651 [DOI] [PubMed] [Google Scholar]
- 4.WHO. WHO, Zika Strategic Response Framework and Joint Operations Plan. 2016.
- 5.Chouin-Carneiro T, Vega-Rua A, Vazeille M, Yebakima A, Girod R, Goindin D, et al. Differential Susceptibilities of Aedes aegypti and Aedes albopictus from the Americas to Zika Virus. Turell MJ, editor. PLoS Negl Trop Dis. 2016;10: e0004543 10.1371/journal.pntd.0004543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Di Luca M, Severini F, Toma L, Boccolini D, Romi R, Remoli ME, et al. Experimental studies of susceptibility of Italian Aedes albopictus to Zika virus. Eurosurveillance. 2016;21: 30223. [DOI] [PubMed] [Google Scholar]
- 7.Diagne CT, Diallo D, Faye O, Ba Y, Faye O, Gaye A, et al. Potential of selected Senegalese Aedes spp. mosquitoes (Diptera: Culicidae) to transmit Zika virus. BMC Infect Dis. BMC Infectious Diseases; 2015;15: 492 10.1186/s12879-015-1231-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bonizzoni M, Dunn WA, Campbell CL, Olson KE, Marinotti O, James AA. Complex Modulation of the Aedes aegypti Transcriptome in Response to Dengue Virus Infection. PLoS One. 2012;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sim S, Jupatanakul N, Ramirez JL, Kang S, Romero-Vivas CM, Mohammed H, et al. Transcriptomic Profiling of Diverse Aedes aegypti Strains Reveals Increased Basal-level Immune Activation in Dengue Virus-refractory Populations and Identifies Novel Virus-vector Molecular Interactions. Ribeiro JMC, editor. PLoS Negl Trop Dis. 2013;7: e2295 10.1371/journal.pntd.0002295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Colpitts TM, Cox J, Vanlandingham DL, Feitosa FM, Cheng G, Kurscheid S, et al. Alterations in the aedes aegypti transcriptome during infection with west nile, dengue and yellow fever viruses. PLoS Pathog. 2011;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bisset JA, Marín R, Rodríguez MM, Severson DW, Ricardo Y, French L, et al. Insecticide resistance in two Aedes aegypti (Diptera: Culicidae) strains from Costa Rica. J Med Entomol. 2013;50: 352–61. [DOI] [PubMed] [Google Scholar]
- 12.Brito LP, Linss JGB, Lima-Camara TN, Belinato TA, Peixoto AA, Lima JBP, et al. Assessing the Effects of Aedes aegypti kdr Mutations on Pyrethroid Resistance and Its Fitness Cost. Kumar N, editor. PLoS One. 2013;8: e60878 10.1371/journal.pone.0060878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beerntsen BT, James AA, Christensen BM. Genetics of Mosquito Vector Competence. Microbiol Mol Biol Rev. 2000;64: 115–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kuno G. Early history of laboratory breeding of Aedes aegypti (Diptera: Culicidae) focusing on the origins and use of selected strains. J Med Entomol. 2010;47: 957–971. [DOI] [PubMed] [Google Scholar]
- 15.Araújo A, Araujo Diniz D, Helvecio E, de Barros R, de Oliveira CM, Ayres CF, et al. The susceptibility of Aedes aegypti populations displaying temephos resistance to Bacillus thuringiensis israelensis: a basis for management. Parasit Vectors. 2013;6: 297 10.1186/1756-3305-6-297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Londono-Renteria B, Troupin A, Conway MJ, Vesely D, Ledizet M, Roundy CM, et al. Dengue Virus Infection of Aedes aegypti Requires a Putative Cysteine Rich Venom Protein. Brass AL, editor. PLOS Pathog. 2015;11: e1005202 10.1371/journal.ppat.1005202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kojin BB, Costa-da-Silva AL, Maciel C, Henriques DA, Carvalho DO, Martin K, et al. Endogenously-expressed NH2-terminus of circumsporozoite protein interferes with sporozoite invasion of mosquito salivary glands. Malar J. BioMed Central; 2016;15: 153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thathy V, Severson DW, Christensen BM. Reinterpretation of the genetics of susceptibility of Aedes aegypti to P. gallinaceum. J Parasitol. 1994;80: 705–712. [PubMed] [Google Scholar]
- 19.Costa-da-Silva AL, Navarrete FR, Salvador FS, Karina-Costa M, Ioshino RS, Azevedo DS, et al. Glytube: a conical tube and parafilm M-based method as a simplified device to artificially blood-feed the dengue vector mosquito, Aedes aegypti. PLoS One. 2013;8: e53816 10.1371/journal.pone.0053816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Anderson SL, Richards SL, Smartt CT. A Simple Method for Determining Arbovirus Transmission in Mosquitoes. J Am Mosq Control Assoc. 2010;26: 108–111. 10.2987/09-5935.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wong P-SJ, Li MI, Chong C-S, Ng L-C, Tan C-H. Aedes (Stegomyia) albopictus (Skuse): A Potential Vector of Zika Virus in Singapore. Turell MJ, editor. PLoS Negl Trop Dis. 2013;7: e2348 10.1371/journal.pntd.0002348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dutra HLC, Rocha MN, Dias FBS, Mansur SB, Caragata EP, Moreira LA. Wolbachia Blocks Currently Circulating Zika Virus Isolates in Brazilian Aedes aegypti Mosquitoes. Cell Host Microbe. 2016;19: 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lanciotti RS, Kosoy OL, Laven JJ, Velez JO, Lambert AJ, Johnson AJ, et al. Genetic and Serologic Properties of Zika Virus Associated with an Epidemic, Yap State, Micronesia, 2007. Emerg Infect Dis. 2008;14: 1232–1239. 10.3201/eid1408.080287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Costa-da-Silva AL, Kojin BB, Marinotti O, James AA, Capurro ML. Expression and accumulation of the two-domain odorant-binding protein AaegOBP45 in the ovaries of blood-fed Aedes aegypti. Parasit Vectors. 2013;6: 364 10.1186/1756-3305-6-364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Salazar MI, Richardson JH, Sánchez-Vargas I, Olson KE, Beaty BJ. Dengue virus type 2: replication and tropisms in orally infected Aedes aegypti mosquitoes. BMC Microbiol. 2007;7: 9 10.1186/1471-2180-7-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Araújo H, Carvalho D, Ioshino R, Costa-da-Silva A, Capurro M. Aedes aegypti Control Strategies in Brazil: Incorporation of New Technologies to Overcome the Persistence of Dengue Epidemics. Insects. 2015;6: 576–594. 10.3390/insects6020576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grard G, Caron M, Mombo IM, Nkoghe D, Mboui Ondo S, Jiolle D, et al. Zika Virus in Gabon (Central Africa)– 2007: A New Threat from Aedes albopictus? Charrel R, editor. PLoS Negl Trop Dis. 2014;8: e2681 10.1371/journal.pntd.0002681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marchette NJ, Garcia R, Rudnick A. Isolation of Zika virus from Aedes aegypti mosquitoes in Malaysia. Am J Trop Med Hyg. 1969;18: 411–5. [DOI] [PubMed] [Google Scholar]
- 29.Dick GW., Kitchen S., Haddow A. Zika Virus (I). Isolations and serological specificity. Trans R Soc Trop Med Hyg. 1952;46: 509–520. [DOI] [PubMed] [Google Scholar]
- 30.Li MI, Wong PSJ, Ng LC, Tan CH. Oral Susceptibility of Singapore Aedes (Stegomyia) aegypti (Linnaeus) to Zika Virus. Turell MJ, editor. PLoS Negl Trop Dis. 2012;6: e1792 10.1371/journal.pntd.0001792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dong S, Kantor AM, Lin J, Passarelli AL, Clem RJ, Franz AWE. Infection pattern and transmission potential of chikungunya virus in two New World laboratory-adapted Aedes aegypti strains. Sci Rep. Nature Publishing Group; 2016;6: 24729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li MI, Wong PSJ, Ng LC, Tan CH. Oral Susceptibility of Singapore Aedes (Stegomyia) aegypti (Linnaeus) to Zika Virus. Turell MJ, editor. PLoS Negl Trop Dis. 2012;6: e1792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Frentiu FD, Zakir T, Walker T, Popovici J, Pyke AT, van den Hurk A, et al. Limited Dengue Virus Replication in Field-Collected Aedes aegypti Mosquitoes Infected with Wolbachia. Turell MJ, editor. PLoS Negl Trop Dis. 2014;8: e2688 10.1371/journal.pntd.0002688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Richardson J, Molina-Cruz A, Salazar MI, Black W. Quantitative analysis of dengue-2 virus RNA during the extrinsic incubation period in individual Aedes aegypti. Am J Trop Med Hyg. 2006;74: 132–41. [PubMed] [Google Scholar]
- 35.Faye O, Faye O, Diallo D, Diallo M, Weidmann M, Sall A. Quantitative real-time PCR detection of Zika virus and evaluation with field-caught Mosquitoes. Virol J. 2013;10: 311 10.1186/1743-422X-10-311 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The prevalence and viral levels per mosquito were recorded after 11 days post-injection of saliva pools collected from ROCK, HWE and RED at 7 and 14 dpi. Each mosquito is represented by a solid diamond. Black bars indicate the mean viral copy numbers and the dashed grey line demonstrates the detection limit.
(TIF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information file.