Abstract
We evaluate whether health education integrated into microcredit lending groups reduces health risks by improving health knowledge and self-reported behaviors among urban and rural borrowers in eastern Benin. In 2007, we randomly assigned 138 villages in the Plateau region of Benin to one of four variations of a group liability credit product, varying lending groups' gender composition and/or inclusion of health education using a 2 × 2 design. Women in villages receiving health education, regardless of gender composition of the groups, showed improved knowledge of malaria and of human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS), but not of childhood illness danger signs. No significant changes in health behavior were observed except an increase in HIV/AIDS prevention behavior, a result predominantly driven by an increase in respondents' self-reported ability to procure a condom, likely an indicator of increased perceived access rather than improved preventative behavior. Women in villages assigned to mixed-gender groups had significantly lower levels of social capital, compared with villages assigned to female-only groups. This suggests there may be an important trade-off to consider for interventions seeking improved health outcomes and social capital through provision of services to mixed-gender groups. Although bundling health education with microcredit can expand health education coverage and lower service-delivery costs, the approach may not be sufficient to improve health behaviors.
Introduction
Background.
The potential for microcredit to improve the health and well-being of the poor, typically female clients and their children, has attracted global interest since its inception.1 However, existing studies find very little evidence of positive impacts from standard microcredit programs on health (or income, on average), but have found important impacts on financial access, ability to absorb shocks, and better facilitation of investment and lumpy consumption.2–10
Using the microcredit delivery system as a conduit, many institutions also integrate nonfinancial interventions, such as training or health care, to complement the credit program with an aim of producing direct health benefits.11 This integrated approach may reduce service-delivery costs of health education, as clients already convened for group financial procedures become a captive audience for instruction.12 The social pressures and behavioral contagion effects of existing social groups may increase the likelihood that recipients act on health knowledge, improving health behaviors, with variability across cultures and health topics.13
Furthermore, gender dynamics have been found to play an important role in the successful uptake of health interventions. A literature review looking at how gender dynamics interact with health outcomes finds that involvement of both men and women in nutritional education is critical for achieving improved household nutrition.14 Male involvement in health decisions, due to their role as primary breadwinners, has also been found to be critical in how household members respond to behaviors associated with human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS).15 Although female-only groups can have positive effects for the individuals, for the group, and for society as a whole, female-only (as well as male-only) groups can also result in further isolating women from community involvement and leadership, resulting in reinforced traditional gender roles.16
Evidence is mixed on the effectiveness of bundling health programs with microcredit delivery. Several literature reviews find that in randomized control trials, the integrated approach led to significant improvements in knowledge change, but limited changes in health behaviors.17–19 Evidence from South Africa, Ghana, and Nigeria shows improved HIV/AIDS behaviors,17,20,21 malaria prevention behavior,22 and breastfeeding behaviors,23 respectively, but no behavior changes were observed from programs in Peru, Ethiopia, or India.24–26 In a majority of nonexperimental or quasi-experimental studies, the integrated approach led to significant improvement in client self-reported behavior across a range of health areas, including reproductive health and intimate partner violence,27–29 child health,30 and preventative measures such as screening and immunizations.31,32 Randomized control trial studies do not tend to show as promising results as the nonexperimental designs, which is consistent with meta-analysis.33
Objectives.
We use a cluster randomized design to analyze the causal effects of two group liability loan product variations, integrated health education and mixed-gender loan groups, on health and social outcomes of likely microcredit clients in Benin. We pose two corresponding primary hypotheses: 1) receiving health education sessions improves potential clients' overall health knowledge and self-reported behaviors compared with only receiving loans and 2) offering group loans to mixed-gender groups (compared with the usual female-only practice) may have an impact on women's empowerment, social capital, and social networks. (Perhaps men's support for women grows when sharing in the loan process, or perhaps including men diminishes social bonds that may be stronger in female-only groups.) We note that each of these two hypotheses ignores the presence of the other hypothesis, yet is conducted within the same experiment. If there are heterogeneous treatment effects for one treatment depending on the presence of the other treatment, then we will be estimating the average treatment effect (much like we will be estimating the average treatment effect over other observed and unobserved heterogeneities across people and communities). To tackle the possibility of interaction effects of the treatments, we pose a secondary hypothesis that a combination of treatments may produce a larger effect on the performance of health education in loan groups than the merely additive effect of each treatment alone. Health education may work better in female-only groups (perhaps women learn more, and act accordingly, from speaking more candidly among other women) or in mixed-gender groups (perhaps including men in health discussions and decisions leads to greater behavior change, especially for behaviors involving men).
Methods
Study location.
In 2006, just before this study commenced, average annual income in Benin was US$530, and 33% of the population lived below the national poverty line of US$0.27 a day. Despite improvements in health infrastructure nationwide, communicable diseases still pose a large health burden and account for more than 70% of deaths. Malaria cases account for 40% of doctors' visits, and 23% of deaths among children under 5 years.34 Though HIV/AIDS prevalence is low for the region, at 1.2% in 2006, the gender discrepancy in knowledge about the disease and its transmission is large: 14% of women and 30% of men were considered knowledgeable.35,36
We collaborated with the Association for the Promotion and Development of Microenterprises or the Promotion et l'Appui au Développement de Micro-Entreprises (PADME) in Benin, a nongovernmental organization (NGO) that provides loans to micro-entrepreneurs in large urban areas of Cotonou, Porto Novo, and more recently in Parakou in the North.37 In 2009, with almost 49,000 clients and a US$35 million loan portfolio, PADME had the largest client pool in the country, of which 64% were women.
Intervention.
In 2007, PADME approached Freedom from Hunger to develop a new product, Credit with Education (CwE), combining a group loan and mandatory savings product with health education delivered via the group's meeting structure. CwE was intended to contribute to PADME's social mission by encouraging clients to adopt positive health behaviors, and it was intended to improve loan default rates. PADME identified 138 villages in the Plateau region of eastern Benin for its lending program expansion. Prior to the product rollout, all credit officers were trained by Freedom from Hunger in adult learning principles as well as the content and training techniques needed to facilitate the groups and deliver the health education.
Beginning in fall 2007, PADME solicited village leaders to identify group members who would participate in weekly meetings and agree to group liability on their individual loans. During the group formation process, the treatment assignment was revealed to the village; credit officers only marketed one of the four interventions possible to the potential members as described below in the Randomization section.
In the CwE villages, credit officers facilitated the financial transactions and taught biweekly, half-hour sessions at regular group meetings for an approximate 3- to 4-month loan cycle. The education sessions were delivered prior to conducting the financial transactions to ensure attendance throughout the entire meeting. Although attendance was not tracked, the group meetings are generally mandatory among new groups and penalties are applied by the group members for tardiness or unexcused absences. Groups completed three education modules in the same sequence over 1 year: malaria, childhood illness, and HIV/AIDS. Each module consisted of 8–10 sessions. A self-esteem module was also delivered among groups that completed the first three modules early, so as to continue offering education per the product design. The childhood illness curriculum used the World Health Organization's strategy for Integrated Management of Childhood Illness (IMCI), focused on helping caregivers recognize childhood illness danger signs requiring immediate treatment-seeking behavior. The health education was identical for female-only and mixed-gender groups.
Randomization.
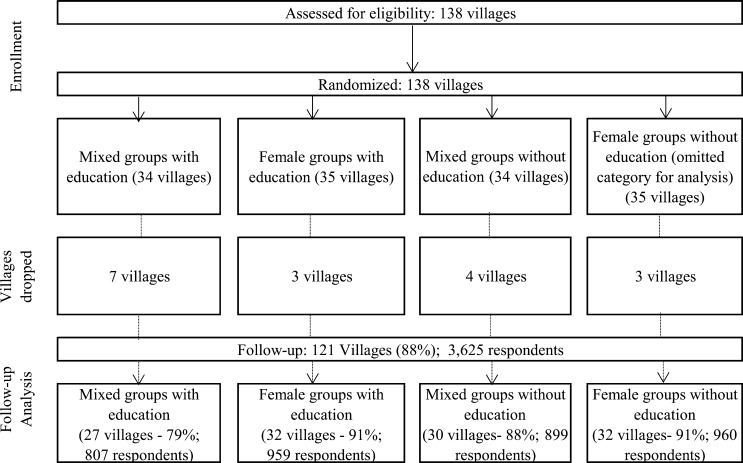
Prior to product rollout, we randomly assigned 138 villages to receive one of four group loan products from PADME, with equal probability: credit with health education to female-only groups, credit with health education to mixed-gender groups, credit only to female-only groups, and credit only to mixed-gender groups. Although all villages received an intervention, we are labeling the villages assigned to receive credit only for female-only as the “control group” since this is the status quo of the lender (and also the more common approach by other microcredit institutions). The randomization was conducted using a computerized random number generator. Seventeen villages were dropped post-randomization because PADME was unable to offer the new product in those villages (Figure 1 ). Reasons for non-implementation included geographic isolation, opposition of village leaders, and insufficient demand (P = 0.39 for rejecting the null of no correlation with assignment to treatments). Although villages initially designated as credit with health education to mixed-gender groups make up slightly more of the villages where no groups were formed, this particular product, along with the credit with health education to female-only groups, was found in practice to be stronger financially with higher average loan sizes, lower portfolio-at-risk rates, and a larger outstanding loan portfolio.38 Therefore, the 17 villages were not included in the data collection, because it did not appear that any one specific treatment was particularly unpopular.
Figure 1.
Trial profile.
During the initial months of implementation, PADME sold subsidized insecticide-treated bednets (ITNs) via CwE credit officers in the first set of villages that received health education,† but then discontinued the ITN sales prior to continuing to roll out the program to the remaining villages. The sale of ITNs in study villages was not anticipated nor did we anticipate that the distribution would stop; therefore, we did not design the experiment to test the impact of this aspect. Exposure to ITNs could increase knowledge due to their use in the household and would influence both self-reported use and observed presence of ITNs in the household. For this reason, we include an additional analysis that compares differences between villages that did and did not have access to the subsidized ITNs to try to detect the impact, if any, of the sale of the ITNs on our key outcomes of interest.
The credit officers built loan groups across three waves of implementation as they expanded their outreach. Wave 1 represents the set of villages where the loan product types were first offered; waves 2 and 3 represent the subsequent sets of villages where the loan product types were eventually rolled out. As randomization of the loan product types offered at the village level was maintained, the variability in the delivery of the education across waves and type of group minimizes. ITN sales were discontinued before the rollout of the loan product types in waves 2 and 3. Because assignment to wave was not randomized, we do not have a cleanly identified method to measure the impact of the sale of subsidized ITNs. We therefore compare the impact of CwE in villages that did and did not receive the ITNs across all study outcomes to understand the possible effect of the ownership of the ITNs on knowledge and behavior (Supplemental Tables A1–A9, Panel C). However, we interpret these with caution: if, for example, the initial villages were selected because of demonstrated eagerness to receive the program, the treatment effect for wave 1 versus waves 2 and 3 may be related to unobserved village-level characteristics, and not differential treatment effects from including, or not, bednets in the program.
Survey participants.
Our sample frame for each of the 121 villages in the follow-up survey included 30 women per village, who were between ages 20 and 45, married, with children under the age of 10. To mitigate selection bias, we surveyed women living near the lending group meeting place, whether they participated in the PADME group or not. This sampling method only requires the assumption that the meeting place location was not determined partly by the treatment group assignment. Of the sample population, 30% were PADME clients. This is a take-up rate that is similar to other credit products.39
Ethics approval was obtained from the Human Research Protection Program at Yale University (IRB Protocol no. 0705002650), and PADME and Innovations for Poverty Action (IPA) ethics committees (IPA IRB Protocol no. 08May-001). Participants gave their oral informed consent to participate in the study and interviews were conducted in the participant's own language. Confidentiality of survey respondent data and human subjects interview protocols were maintained by IPA staff, and procedures adhered to no harm principles.
Measures.
A census was initially conducted to model participation and examine whether treatment assignment led to different selection, though unsuccessful matching made such analysis impossible. Timing, logistics, and budget constraints prevented the use of a baseline survey; instead, the study relied on the follow-up survey only.
We conducted a follow-up survey in March 2010 in 121 of the 138 villages after PADME had launched the credit products and completed the CwE trainings (N = 3,625 in 121 villages).
IPA developed the questionnaire, and Freedom from Hunger contributed survey questions specific to the material taught in the education modules, described in detail below. Many of the survey questions and measures were pulled from Demographic and Health Survey tools including instruments specific to Benin or drawn from women's or domestic violence modules.35
We group outcome indicators into nine indices of health and social outcomes. For each index, we follow the method used by Kling and others.40
Health knowledge and behavior.
We create separate knowledge and behavior indices for each of three health areas covered in the CwE curriculum—malaria, HIV/AIDS, and childhood illness.
The malaria knowledge index includes questions on the causes of the disease, methods of prevention, and vulnerable populations. The HIV/AIDS knowledge index combines questions on familiarity with HIV/AIDS, knowledge of prevention methods, and knowledge of testing and treatment availability. The IMCI (child illness) knowledge index captures knowledge of danger signs of diarrhea, cough, and malaria; treatment of diarrhea, fever, and cough; and the actions expected of a health-care professional assessing a child's health.
The bednet behavior index corresponds to CwE's malaria curriculum and measures mosquito bednet usage: number of mosquito bednets owned by the household, the proportion of household members under age 5 who slept under a net the previous night, whether the household has a net that is 1 year or newer, whether the household has an installed net that is 1 year or newer, and whether the household has a net that has been treated within the past year.‡ The HIV/AIDS access and behavior index combines questions on spousal communication about HIV/AIDS prevention, reported condom use during last sexual intercourse, and the respondent's ability to acquire a condom herself. Although the majority of the respondent population is married and condom use would not be assumed to be high even after the provision of the education unless a respondent herself felt she needed this protective measure, condom use is maintained as an indicator since the goal of the behavior index is to detect whether the education resulted in people using condoms more. Finally, two questions comprise the IMCI behavior index: past use of oral rehydration salts to treat child diarrhea, and, conditional on having a child with a fever in the previous month, attempt to access medical treatment of that child. All behaviors measured are self-reported.
Empowerment, social capital, and social network.
We measure empowerment using an index that sums respondents' self-reported participation in community, household, and work decision-making; partner relationships and freedom of movement; views on women's empowerment; and voting. The social capital index includes questions on group membership, support networks, participation in village meetings and public positions, and influence in the village. The social network index contains three variables that measure the strength of the respondent's social network on a scale from 1 to 10. Prior to the survey, the list of 30 survey respondents per village was created. When each woman was interviewed, the enumerator randomly selected 10 of the 30 survey respondents and asked whether the respondent had received economic support from any other women in the past, the amount she would consider asking for a small loan, if needed, and the amount she would lend to others as a small loan.
Data analysis.
Data were double entered. Statistical analyses were conducted using STATA SE 10.1 for Windows (STATA Corporation, College Station, TX).
Table 1 compares the four survey arms to establish orthogonality of treatment assignment to observable characteristics. Given lack of baseline data, these variables were measured at follow-up and were chosen due to high likelihood of time invariance. Table 1 also presents summary statistics for those who participated in the program, compared with those who did not, so as to understand how participants differed on observables.
Table 1.
Orthogonality tests and summary statistics: respondent time-invariant characteristics, as reported in endline
| Means and standard errors | P value from t test or f test | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mixed groups with education | Female groups with education | Mixed groups without education | Female groups without education | (1) vs. (4) | (2) vs. (4) | (3) vs. (4) | Joint orthogonality test of all | ||||||||
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | ||||||||
| Panel A: orthogonality tests | |||||||||||||||
| Housing characteristics | |||||||||||||||
| Household water source score (0–2, higher is cleaner) | 1.053 | 0.894 | 0.970 | 0.806 | 0.139 | 0.576 | 0.317 | 0.472 | |||||||
| (0.116) | (0.102) | (0.112) | (0.119) | – | – | – | – | ||||||||
| Has higher quality floor materials | 0.366 | 0.347 | 0.357 | 0.320 | 0.476 | 0.679 | 0.547 | 0.889 | |||||||
| (0.051) | (0.051) | (0.047) | (0.042) | – | – | – | – | ||||||||
| Has higher quality roof materials | 0.655 | 0.630 | 0.656 | 0.642 | 0.870 | 0.888 | 0.865 | 0.990 | |||||||
| (0.063) | (0.063) | (0.064) | (0.054) | – | – | – | – | ||||||||
| Education level | |||||||||||||||
| No schooling | 0.838 | 0.860 | 0.858 | 0.853 | 0.639 | 0.828 | 0.895 | 0.906 | |||||||
| (0.023) | (0.023) | (0.025) | (0.022) | – | – | – | – | ||||||||
| Up to primary school | 0.125 | 0.109 | 0.107 | 0.124 | 0.972 | 0.603 | 0.551 | 0.871 | |||||||
| (0.019) | (0.018) | (0.020) | (0.020) | – | – | – | – | ||||||||
| More than primary school | 0.037 | 0.030 | 0.036 | 0.023 | 0.165 | 0.423 | 0.197 | 0.445 | |||||||
| (0.008) | (0.007) | (0.008) | (0.006) | – | – | – | – | ||||||||
| Number of observations | 807 | 959 | 899 | 960 | – | – | – | – | |||||||
| Means and standard errors | All groups | P value from t test or f test | |||||||||||||
| Nonparticipant | Participant | Nonparticipant | Participant | Nonparticipant | Participant | Nonparticipant | Participant | Nonparticipant | Participant | (1) vs. (2) | (3) vs. (4) | (5) vs. (6) | (7) vs. (8) | (9) vs. (10) | |
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) | (11) | (12) | (13) | (14) | (15) | |
| Panel B: selection analysis: mean (participant) − mean (nonparticipant) | |||||||||||||||
| Participation rate | 31.23% | 29.09% | 27.03% | 33.23% | 30.15% | ||||||||||
| Housing characteristics | |||||||||||||||
| Household water source score (0–2, higher is cleaner) | 1.051 | 1.060 | 0.859 | 0.978 | 1.058 | 0.728 | 0.905 | 0.606 | 0.964 | 0.834 | 0.937 | 0.361 | 0.008 | 0.007 | 0.039 |
| (0.122) | (0.138) | (0.101) | (0.148) | (0.113) | (0.132) | (0.123) | (0.125) | (0.057) | (0.073) | – | – | – | – | – | |
| Has higher quality floor materials | 0.369 | 0.361 | 0.358 | 0.320 | 0.354 | 0.366 | 0.323 | 0.313 | 0.350 | 0.338 | 0.872 | 0.613 | 0.829 | 0.854 | 0.666 |
| (0.052) | (0.062) | (0.052) | (0.079) | (0.054) | (0.051) | (0.047) | (0.050) | (0.025) | (0.030) | – | – | – | – | – | |
| Has higher quality roof materials | 0.695 | 0.567 | 0.657 | 0.565 | 0.650 | 0.671 | 0.630 | 0.665 | 0.657 | 0.618 | 0.077 | 0.243 | 0.781 | 0.580 | 0.280 |
| (0.065) | (0.079) | (0.064) | (0.086) | (0.072) | (0.071) | (0.062) | (0.059) | (0.033) | (0.037) | – | – | – | – | – | |
| Education level | |||||||||||||||
| No schooling | 0.819 | 0.881 | 0.856 | 0.870 | 0.856 | 0.863 | 0.854 | 0.852 | 0.847 | 0.866 | 0.044 | 0.715 | 0.830 | 0.946 | 0.281 |
| (0.028) | (0.023) | (0.027) | (0.032) | (0.028) | (0.031) | (0.023) | (0.035) | (0.013) | (0.016) | – | – | – | – | – | |
| Up to primary school | 0.140 | 0.091 | 0.117 | 0.090 | 0.108 | 0.104 | 0.124 | 0.123 | 0.121 | 0.103 | 0.049 | 0.355 | 0.902 | 0.980 | 0.204 |
| (0.024) | (0.017) | (0.021) | (0.024) | (0.024) | (0.024) | (0.024) | (0.027) | (0.012) | (0.012) | – | – | – | – | – | |
| More than primary school | 0.042 | 0.028 | 0.027 | 0.040 | 0.037 | 0.033 | 0.022 | 0.025 | 0.032 | 0.031 | 0.283 | 0.398 | 0.802 | 0.808 | 0.972 |
| (0.009) | (0.011) | (0.007) | (0.014) | (0.010) | (0.011) | (0.006) | (0.012) | (0.004) | (0.006) | – | – | – | – | – | |
| Number of observations | 555 | 252 | 680 | 279 | 656 | 243 | 641 | 319 | 2,532 | 1,093 | – | – | – | – | – |
Panel A standard errors clustered at the village level and reported in parentheses. Above variables chosen due to high likelihood of time invariance, thus used for orthogonality tests, given lack of baseline data. Column 8 reports P value from the f test from the regression of each row's variable on all three treatments (columns 1, 2, and 3).
To estimate treatment effects, we implement two multivariate regression models using ordinary least squares. In the first model (Table 2), we examine the impact of health education on health knowledge and behavior. Panel A includes a binary predictor variable for random assignment to receive health education with the group loan. Panel B includes indicator variables for the two main treatment variations (education and mixed-gender group), and an interaction term between the two that captures the third treatment (both education and mixed-gender group). This specification allows us to isolate the differential impacts of the three treatments. This structure of utilizing Panel A for assessing the impact of education and Panel B to assess the impact of the interaction of gender and education is maintained across all of the tables to facilitate ease of review and analysis.
Table 2.
Indices for health education treatment
| Malaria knowledge score | HIV/AIDS knowledge score | IMCI knowledge score | Bednet behavior score | HIV/AIDS access and behavior score | IMCI behavior score | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β coefficient (95% CI) | P value | β coefficient (95% CI) | P value | β coefficient (95% CI) | P value | β coefficient (95% CI) | P value | β coefficient (95% CI) | P value | β coefficient (95% CI) | P value | |
| (1) | (2) | (3) | (4) | (5) | (6) | |||||||
| Panel A: impact of Credit with Education | ||||||||||||
| Treatment: Credit with Education | 0.140 | 0.040 | 0.138 | 0.058 | 0.036 | 0.622 | 0.016 | 0.798 | 0.139 | 0.035 | 0.019 | 0.795 |
| (0.007, 0.274) | (−0.005, 0.282) | (−0.108, 0.180) | (−0.107, 0.139) | (0.010, 0.268) | (−0.123, 0.160) | |||||||
| Control for stratification variables (wave) | Yes | Yes | Yes | Yes | Yes | Yes | ||||||
| Panel B: impact of Credit with Education and/or mixed-gender treatment | ||||||||||||
| Treatment: Credit with Education | 0.131 | 0.162 | 0.060 | 0.580 | −0.099 | 0.323 | 0.003 | 0.970 | 0.140 | 0.129 | 0.033 | 0.730 |
| (−0.053, 0.316) | (−0.153, 0.272) | (−0.297, 0.099) | (−0.171, 0.177) | (−0.041, 0.322) | (−0.158, 0.225) | |||||||
| Treatment: mixed-gender group | −0.050 | 0.606 | −0.084 | 0.404 | −0.133 | 0.216 | 0.089 | 0.271 | 0.017 | 0.828 | 0.097 | 0.374 |
| (−0.243, 0.142) | (−0.281, 0.114) | (−0.345, 0.079) | (−0.070, 0.248) | (−0.140, 0.175) | (−0.118, 0.312) | |||||||
| Treatment: education × mixed-gender group interaction | 0.016 | 0.904 | 0.168 | 0.247 | 0.281 | 0.054 | 0.033 | 0.789 | −0.001 | 0.994 | −0.027 | 0.851 |
| (−0.253, 0.285) | (−0.118, 0.453) | (−0.005, 0.568) | (−0.209, 0.275) | (−0.262, 0.260) | (−0.311, 0.257) | |||||||
| Control for stratification variables (wave) | Yes | Yes | Yes | Yes | Yes | Yes | ||||||
| Control mean = credit without education, female-only (standard deviation) | 0 | 0 | 0 | 0 | 0 | 0 | ||||||
| (1.000) | (1.000) | (1.000) | (1.000) | (1.000) | (1.000) | |||||||
| Treatment mean (standard deviation), Credit with Education | 0.119 | 0.106 | −0.0337 | 0.0520 | 0.151 | 0.0790 | ||||||
| (0.965) | (1.027) | (0.940) | (1.034) | (1.184) | (1.164) | |||||||
| Treatment mean (standard deviation), mixed-gender group | 0.0225 | 0.0293 | −0.0486 | 0.109 | 0.0884 | 0.109 | ||||||
| (1.002) | (1.018) | (0.999) | (1.029) | (1.114) | (1.323) | |||||||
| Number of observations | 3,619 | 3,625 | 3,356 | 3,625 | 3,624 | 3,270 | ||||||
AIDS = acquired immunodeficiency syndrome; CI = confidence interval; HIV = human immunodeficiency virus; IMCI = Integrated Management of Childhood Illness; ITN = insecticide-treated bednets. Sample contains 3,625 respondents present for the follow-up survey. Robust standard errors clustered at the village level. All specifications include three stratification variables to indicate whether a village participated in wave 1, 2, or 3. Inclusion in wave 1, 2, or 3 is nonrandom, and wave 1 treatment villages received subsidized health products, including insecticide-treated mosquito nets. Each dependent variable is an index of several related questions. Each index is standardized so the control group (credit without education, female-only groups) has a mean of zero and a standard deviation of one. We define index components here and present treatment effects on the individual components in the appendix. Index definitions: For all questions, incorrect answers (not specified here) are assigned the value 0, unanswered survey questions are coded as missing. (1) Malaria knowledge score, three components: Q1: What causes malaria? = 1, if respondent lists “mosquito bites” only; Q2: How does one protect him/herself from getting malaria? = 1, if respondent lists “sleeping under ITN” only; Q3: Which two groups of people are most vulnerable to the effects of malaria? = 1, if respondent lists both “young children” and “pregnant women” only. (2) HIV/AIDS knowledge score, eight components: All questions take the value 1 if respondent answers “Yes.” Q1: Have you heard of AIDS? Q2: In the last few months, have you heard or seen any messages on HIV/AIDS? Q3: Do you personally know someone who is suspected to have the AIDS virus or who has the AIDS virus? Q5: Can people reduce their chances of getting the AIDS virus by using a condom every time they have sex? Q6: Can people reduce their chance of getting the AIDS virus by abstaining from sexual intercourse? Q7: Are there any special medications that people infected with the AIDS virus can get from a doctor or nurse? Q8: Do you know where people can go to get tested for the virus that causes AIDS? Q8: Do you know where to get condoms? (3) IMCI knowledge score, seven components: Q1: What are the critical danger signs of serious illness in children 2 months to 5 years of age? 1 point for each correct answer, up to 6; Q2: How much liquid should you give a child with diarrhea? = 1, if respondent selects “more than usual”; Q3: When a child has diarrhea, what symptoms indicate that you should take him/her for medical care? 1 point for each correct answer, up to 8; Q4: When a child has a cough, what symptoms indicate that you should take him/her for medical care? 1 point for each correct answer, up to 10; Q5: How do you know a child has malaria? = 1, if respondent lists “fever”; Q6: If a child has a fever, how would you recommend that child be treated at home? 1 point for each correct answer, up to 5; Q7: What actions should a doctor/nurse take when assessing the health of your child? 1 point for each correct answer, up to 10. (4) Bednet behavior score, five components: Q1: number of installed bednets in household; Q2: proportion of household members under age 5 who slept under a net the previous night; Q3: household has a net, 1 year or newer; Q4: household has an installed net, 1 year or newer; Q5: household has a net treated within the past year. (5) HIV/AIDS behavior score, three components: All questions take the value 1, if respondent answers “Yes.” Q1: Have you spoken with your husband/companion about ways to avoid contracting HIV/AIDS? Q2: The last time you had sexual intercourse, was a condom used? Q3: If you wanted to, could you yourself get a condom? (6) IMCI behavior score, two components: Q1: respondent has given Orasel or other oral rehydration salts to a child to treat diarrhea; Q2: respondent sought treatment within 3 days for a child who had fever during the previous month.
In the second model (Table 3), we examine the impact of mixed-gender loan groups on empowerment, social networks, and social capital. Panel A includes a binary predictor variable for assignment to mixed-gender loan groups. The Panel B specification is the same as in model one.
Table 3.
Indices for mixed-gender loan groups treatment
| Empowerment score | Social network score | Social capital score | ||||
|---|---|---|---|---|---|---|
| β coefficient (95% CI) | P value | β coefficient (95% CI) | P value | β coefficient (95% CI) | P value | |
| (1) | (2) | (3) | ||||
| Panel A: impact of mixed-gender group | ||||||
| Treatment: mixed-gender Group | −0.097 | 0.179 | −0.028 | 0.795 | −0.171 | 0.027 |
| (−0.238, 0.045) | (−0.238, 0.183) | (−0.322, −0.020) | ||||
| Control for stratification variables (wave) | Yes | Yes | Yes | |||
| Panel B: impact of Credit with Education and/or mixed-gender treatment | ||||||
| Treatment: Credit with Education | 0.036 | 0.720 | −0.193 | 0.189 | 0.205 | 0.064 |
| (−0.163, 0.236) | (−0.482, 0.096) | (−0.012, 0.423) | ||||
| Treatment: mixed-gender group | −0.038 | 0.689 | −0.129 | 0.405 | −0.104 | 0.263 |
| (−0.227, 0.151) | (−0.435, 0.177) | (−0.288, 0.079) | ||||
| Treatment: education × mixed-gender group interaction | −0.121 | 0.398 | 0.203 | 0.331 | −0.129 | 0.389 |
| (−0.403, 0.161) | (−0.209, 0.615) | (−0.426, 0.167) | ||||
| Control for stratification variables (wave) | Yes | Yes | Yes | |||
| Control mean = credit without education, female-only (standard deviation) | 0 | 0 | 0 | |||
| (1.000) | (1.000) | (1.000) | ||||
| Treatment mean (standard deviation), Credit with Education | −0.0358 | −0.149 | 0.104 | |||
| (1.069) | (0.982) | (1.005) | ||||
| Treatment mean (standard deviation), mixed-gender group | −0.0756 | −0.114 | −0.0642 | |||
| (1.078) | (0.981) | (0.940) | ||||
| Number of observations | 3,622 | 3,613 | 3,625 | |||
CI = confidence interval. Sample contains 3,625 respondents present for the follow-up survey. Robust standard errors clustered at the village level. All specifications include three stratification variables to indicate whether a village participated in wave 1, 2, or 3. Inclusion in wave 1, 2, or 3 is nonrandom, and wave 1 treatment villages received subsidized health products, including insecticide-treated mosquito nets. Each dependent variable is an index of several related questions. Unanswered survey questions are coded as missing. Each index is standardized so the control group (credit without education, female-only groups) has a mean of zero and a standard deviation of one. We define index components here and tabulate component outcomes in the appendix. (1) Empowerment score, eight components: Q1: participates in decisions about children's school attendance; Q2: participates in decisions about children's membership in groups; Q3: participates in buying and selling decisions for the household; Q4: participates in decisions about working outside the household; Q5: How often do conflicts with your spouse lead to a) verbal abuse, b) physical abuse, or c) physical abuse against children? For each of a, b, and c, 0 = often, 1 = sometimes, 2 = rarely, 3 = never. Combined score: 0 = often to 9 = never; Q6: ability to go out to a) the market, b) the health center, c) walk with friends, d) the religious center. For each of a, b, c, and d, 0 = never, 1 = cannot when alone, 2 = can when alone. Combined score: 0 = never to 8 = always able to travel alone; Q7: views on women's empowerment: a) decisions in the family should be taken by men, b) if a woman works outside the home, then the husband should help with household chores, c) a married woman must be able to work outside the home if she wishes, d) a married woman should be allowed to express her opinion even when she disagrees with her husband, e) a woman should accept beatings by her husband to preserve the unity of the family, f) it is better to send boys to school than girls. For b, c, and d, Yes = 2, No = 0, Depends = 1; and for a, e, and f, Yes = 0, No = 2, Depends = 1. Combined score: 0 = low empowerment to 12 = high empowerment; Q8: frequency of voting, 0 = never, 1 = sometimes, 2 = always. (2) Social network score, three components: Q1: number of matched respondents who have given economic support, out of 10; Q2: number of matched respondents she could ask for small money, out of 10; Q3: number of matched respondents she would lend small money, out of 10. (3) Social capital score, six components: Q1: number of community groups that the respondent belongs to; Q2: number of groups from whom the respondent got economic support in the last 12 months; Q3: number of groups from whom the respondent got advice in the last 12 months; Q4: has spoken out in a community meeting in last 12 months; Q5: has run for or held an elected community position or office in last 12 months; Q6: feels at least somewhat influential in changing her village.
Supplemental Tables A1–A9 present results on index variables alongside their component variables. Panels A and B match those from the corresponding main index table. One additional panel, Panel C, is added to Supplemental Tables A1–A6 (health outcomes). Here we use two exclusive indicator variables to examine the treatment effect of CwE under two conditions: receipt (wave 1) and nonreceipt (wave 2 or 3) of subsidized mosquito bednets. We conduct a t test of the equality of the two coefficients to detect significant variation in the size of the treatment effect under the two environments.
For all specifications, we suppress the constant and include three stratification variables that identify whether the village participated in wave 1, 2, or 3. Standard errors were calculated allowing for clustering at the unit of randomization, the village (estimated using the cluster option of Stata; chosen because it allows for an unrestricted within-cluster covariance matrix).41 The clustering of standard errors at the village level is important because of the village-level random assignment of treatment.
Results
Respondent characteristics.
Respondents randomized to the four study arms were balanced with respect to water source, quality of floor and roof material, and educational attainment (Table 1). Ninety-nine percent of the respondents were married with an average age of 37 years. Each household had an average of three children. Sixty-six percent identified themselves as Christian and 22% were Muslim. Less than 20% identified themselves as being literate in any language (not shown in table).
Effect of Credit with Education on health knowledge and behavior.
Compared with credit-only villages, CwE led to significant increases in malaria knowledge (P = 0.040) and slight increases in HIV/AIDS knowledge (P = 0.058) (Table 2, Panel A), but had no observable effect on IMCI knowledge. CwE also had a positive impact on the HIV/AIDS access and behavior index (P = 0.035), though this result was driven by the “access” variable: “If you wanted to, could you yourself get a condom?” This may be a proxy for actual usage; however, we observe no statistically significant treatment effect on condom usage at last instance of sexual intercourse (Supplemental Table A5). CwE had no observable impact on the bednet behavior score or the IMCI behavior score.
Comparing groups that received subsidized bednets (wave 1) to groups that did not (waves 2 and 3), we observe only one outcome with a differential CwE impact (Supplemental Tables A1–A6, Panel C): use of mosquito repellant or insecticide over the past 2 weeks (Supplemental Table A4), a substitute behavior for bednet usage. As substitute behaviors, we expect a training encouraging both behaviors to produce higher levels of mosquito repellant usage in the group with lesser access to mosquito bednets. Indeed, the estimated treatment effect on mosquito repellant usage in villages without access to subsidized bednets is greater than the effect in villages with access (0.142 standard deviation increase without bednets and 0.018 standard deviation increase with bednets; P value from t test on equality of coefficients = 0.089). However, since wave 1 did not report higher usage of bednets, and the wave was not randomly assigned, we urge caution in over-interpreting this result on usage of mosquito repellant.
Effect of mixed-gender loan groups on health knowledge and behavior.
In Table 3, “treatment: education × mixed-gender group interaction” reports the additive effect of delivering health education in mixed-gender groups relative to female-only groups. Education was slightly more effective in the mixed-gender setting for IMCI knowledge (P = 0.054). There were no other differential impacts by group gender composition.
Effect of mixed-gender loan groups on empowerment and social capital.
Respondents in villages who were offered the mixed-gender intervention reported on average lower social capital (P = 0.027) scores than did respondents in female-only villages (Table 3, Panel A). The two groups did not display statistically significant differences on empowerment or social network score; neither did the mixed-gender treatment have a differential effect across CwE and credit-only groups.
Discussion
The integrated package of group microcredit and health education led to gains in knowledge of both malaria and HIV/AIDS, but those gains did not translate into significant improvements in health behaviors.
Although women in CwE villages with mixed-gender loan groups had slightly better knowledge of childhood illness than women in CwE villages with female-only groups, this differential effect must be considered in context: overall, CwE did not lead to improvements in IMCI knowledge or behavior. Furthermore, women in villages assigned to form mixed-gender loan groups had significantly lower social capital scores as a result, though their empowerment and social network scores remained unchanged. The negative effect on social capital provides some support for popular policy claims that enabling women to convene empowers them to gain confidence and assert themselves in community matters.17,42
Of the previously cited studies that found positive impacts on health behaviors, two incorporated subsidized or free access to health services24,32; three evaluated the same intervention, IMAGE in South Africa, which used trained health workers to deliver health curricula and included a broader community mobilization component20,21,25,31; two were implemented by Project HOPE, founded as an integrated village health bank that assigns a health officer to conduct trainings at each bank branch26,31; and one used cell phone and voice messages to reinforce breastfeeding messages to groups of women.23
In contrast, PADME's intervention relied on credit officers to both relay health curricula and facilitate financial services and did not systematically incorporate health care, products provision, or text or voice messages. We may not observe behavior change despite increases in corresponding knowledge areas if knowledge was not the key constraint to improving health behaviors in study communities. Limited access to health products and services may have prevented respondents from engaging in behaviors promoted by CwE. This explanation seems unlikely for HIV/AIDS access and behavior considering the strong positive result of CwE on women's self-reported ability to independently procure a condom yet the null result on condom use and considering that almost all respondents were married and may have considered themselves at low risk to HIV/AIDS. Access to mosquito bednets or ITNs could be prohibitive, considering the significant increase in mosquito repellant usage observed in CwE villages that were not sold subsidized mosquito bednets.
Although part of the original study design, the lack of census and baseline data limits the analytical potential for the study. Without these data, we can only compare the level of outcomes for the four group loan products, but cannot compare the changes in outcomes between baseline and endline. More importantly, we are not able to conduct analysis of who participates. The four group loan products may have attracted different types of people, that is, those who want more education on health matters, or individuals with different views on gender roles in the household and community. Furthermore, a baseline would have allowed us to conduct analysis of heterogeneity, to explore village or individual characteristics that are associated with larger treatment effects.
However, the endline assessment was designed in such a way to control for selection differences by surveying a representative set of village members, not merely PADME clients. Thus, we are estimating the treatment effect on the villages on average, irrespective of whether one treatment led to different characteristics of participants. This removes the risk of self-selection bias from the analysis, although it does weaken the statistical precision of the estimated treatment effects as the estimates are diluted by those who did not participate. Also, because this sampling strategy only includes the villages where groups formed successfully, a village-selection bias is a risk for the study design. Geographic isolation, opposition of village leaders, and insufficient demand of the product were key contributors for lack of groups in the 17 villages that did not form groups. If villages more likely to form groups are also different in other regards, such as having village members who are more financially capable, more entrepreneurial, or who have stronger social networks, this introduces a possible selection bias to the study design.
An additional limitation of the design is the relatively short period of time to detect change as well as a disruption to the rollout that occurred during the evaluation period. The baseline was conducted in September and October 2007. Implementation began shortly thereafter. Also, because the program was rolled out in three main waves, waves 2 and 3 had less time to put behaviors into practice by the endline assessment, which occurred in January to March 2010. In fact, the endline was conducted as soon as the villages in wave 3 had participated in all education modules. Having said that, we posit that behavior change is likely to dissipate over time rather than increase, and thus the lack of short-run behavior change is likely indicative of no long-run behavior change as well. Second, implementation could have been affected by internal turmoil: early in 2008, just a few months after the launch of program, the Béninois government seized control of PADME and replaced its leadership. An extensive staff work strike ensued, leading to about 3 months of inactivity in the field and some client confusion. With the new leadership in place, PADME then continued to pursue transformation to a regulated bank, which complicated management attention to the new program. However, the presence of knowledge changes does suggest successful implementation, and that the issue is more about how to convert knowledge increase into behavior change.
This study also should be viewed in the larger context of the impact of microcredit. Because the data were collected for this study, several randomized trials of “plain microcredit” (i.e., no educational add-ons) have been published2,3,5–7,10 and summarized.4 The modest impact of microcredit has led some policymakers, donors, and microcredit institutions to rethink their model to include integrated services (or to innovate further to reach those who are too young, too rural, or too poor, to participate in standard microcredit).43
In conclusion, our study joins a small group of randomized evaluations22,23,27,28 suggesting that, although bundling health education with microcredit is one way to expand health education coverage and lower service-delivery costs, the approach may not be sufficient to improve health behaviors. Further research is needed to determine whether socially motivated microfinance institutions that aim to support client health can achieve their goals better through integrating direct services beyond health education or through provision of specific health financing tools designed to influence positive treatment-seeking behaviors.
Supplementary Material
ACKNOWLEDGMENTS
We thank Innovations for Poverty Action for excellence in conducting field research and collecting survey data, and Association for the Promotion and Development of Microenterprises or the Promotion et l'Appui au Développement de Micro-Entreprises (PADME), Freedom from Hunger's partner in Benin, for their important role implementing the Credit with Education product. We also thank PADME's staff and clients for playing an important role in this evaluation, and the Bill & Melinda Gates Foundation for investing in this program and corresponding research.
Disclaimer: The funder had no role in the study design; in collecting, analyzing, or interpreting the data; in writing the report or in the decision to submit the article for publication.
Footnotes
Financial support: The Bill & Melinda Gates Foundation funded this study.
Conflict of interest: Karlan and Thuysbaert have no conflicts of interest. Gray is employed by Freedom from Hunger, the nonprofit organization that developed the education materials and trains organizations in using them.
Authors' addresses: Dean Karlan and Bram Thuysbaert, Department of Economics, Yale University, New Haven, CT, E-mails: dean.karlan@yale.edu and bthuysbaert@gmail.com. Bobbi Gray, Research, Evaluation and Monitoring, Freedom from Hunger, Davis, CA, E-mail: bgray@freedomfromhunger.org.
We do not have monitoring data to verify that subsidized ITNs were available only to villages with CwE groups, or that ITNs were the only subsidized health products offered.
We exclude from the bednet behavior index an indicator variable for use of mosquito repellants, a substitute behavior for bednet use. We present this related outcome alongside, but separate from the component variables of the bednet behavior index, in column 7 of Supplemental Table A4.
References
- 1.Yunus M. Towards eliminating poverty from the world: Grameen Bank experience. In: Andersen C, Looney J, editors. Making Progress: Essays in Progress and Public Policy. Lanham, MD: Lexington Books; 2002. pp. 371–378. [Google Scholar]
- 2.Angelucci M, Karlan D, Zinman J. Microcredit impacts: evidence from a randomized microcredit program placement experiment by Compartamos Banco. Am Econ J Appl Econ. 2015;7:151–182. [Google Scholar]
- 3.Banerjee A, Duflo E, Glennerster R, Kinnan C. The miracle of microfinance? Evidence from a randomized evaluation. Am Econ J Appl Econ. 2015;7:22–53. [Google Scholar]
- 4.Banerjee A, Karlan D, Zinman J. Six randomized evaluations of microcredit: introduction and further steps. Am Econ J Appl Econ. 2015;7:1–21. [Google Scholar]
- 5.Attanasio O, Augsburg B, De Haas R, Fitzsimons E, Harmgart H. The impacts of microfinance: evidence from joint-liability lending in Mongolia. Am Econ J Appl Econ. 2015;7:90–122. [Google Scholar]
- 6.Augsburg B, De Haas R, Harmgart H, Meghir C. The impacts of microcredit: evidence from Bosnia and Herzegovina. Am Econ J Appl Econ. 2015;7:183–203. [Google Scholar]
- 7.Tarozzi A, Desai J, Johnson K. The Impacts of Microcredit: Evidence from Ethiopia. Am Econ J Appl Econ. 2015;7:54–89. [Google Scholar]
- 8.Karlan D, Zinman J. Microcredit in theory and practice: using randomized credit scoring for impact evaluation. Science. 2011;332:1278–1284. doi: 10.1126/science.1200138. [DOI] [PubMed] [Google Scholar]
- 9.Karlan D, Zinman J. Expanding credit access: using randomized supply decisions to estimate the impacts. Rev Financ Stud. 2010;23:433–464. [Google Scholar]
- 10.Crépon B, Devoto F, Duflo E, Parienté W. Estimating the impact of microcredit on those who take it up: evidence from a randomized experiment in Morocco. Am Econ J Appl Econ. 2015;7:123–150. [Google Scholar]
- 11.Karlan D, Morduch J. Access to finance. In: Rodrik D, Rosenzweig M, editors. Handbook of Development Economics. Vol. 5. Oxford, UK: Elsevier; 2009. pp. 4703–4784.https://www.nyu.edu/projects/morduch/documents/articles/2009-06-HDE_AccesstoFinance.pdf Available at. Accessed June 3, 2016. [Google Scholar]
- 12.Reinsch M, Dunford C, Metcalfe M. Costs and benefits of microfinance institutions offering health protection services to clients. Enterp Dev Microfinance. 2011;22:241–258. [Google Scholar]
- 13.Leatherman S, Saha S, Metcalfe M, Mavalankar D. Integrating microfinance and community health interventions: a narrative review of evidences from India. Int J Dev Res. 2014;4:442–446. [Google Scholar]
- 14.Vlassoff C. Gender differences in determinants and consequences of health and illness. J Health Popul Nutr. 2007;25:47–61. [PMC free article] [PubMed] [Google Scholar]
- 15.Ditekemena J, Koole O, Engmann C, Matendo R, Tshefu A, Ryder R, Colebunders R. Determinants of male involvement in maternal and child health services in sub-Saharan Africa: a review. Reprod Health. 2012;9:32. doi: 10.1186/1742-4755-9-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Inglehart R, Norris P. Rising Tide: Gender Equality and Cultural Change Around the World. New York, NY: Cambridge University Press; 2003. http://www.cambridge.org/us/academic/subjects/politics-international-relations/politics-general-interest/rising-tide-gender-equality-and-cultural-change-around-world Available at. Accessed June 3, 2016. [Google Scholar]
- 17.Isangula KG. Improving women and family's health through integrated microfinance, health education and promotion in rural areas. J Sustain Dev. 2012;5:76. [Google Scholar]
- 18.O'Malley TL, Burke JG. A systematic review of microfinance and women's health literature: directions for future research. Glob Public Health. 2016:1–28. doi: 10.1080/17441692.2016.1170181. [DOI] [PubMed] [Google Scholar]
- 19.Leatherman S, Metcalfe M, Geissler K, Dunford C. Integrating microfinance and health strategies: examining the evidence to inform policy and practice. Health Policy Plan. 2012;27:85–101. doi: 10.1093/heapol/czr014. [DOI] [PubMed] [Google Scholar]
- 20.Pronyk PM, Hargreaves JR, Kim JC, Morison LA, Phetla G, Watts C, Busza J, Porter JD. Effect of a structural intervention for the prevention of intimate-partner violence and HIV in rural South Africa: a cluster randomised trial. Lancet. 2006;368:1973–1983. doi: 10.1016/S0140-6736(06)69744-4. [DOI] [PubMed] [Google Scholar]
- 21.Pronyk PM, Kim JC, Abramsky T, Phetla G, Hargreaves JR, Morison LA, Watts C, Busza J, Porter JD. A combined microfinance and training intervention can reduce HIV risk behaviour in young female participants. AIDS. 2008;22:1659–1665. doi: 10.1097/QAD.0b013e328307a040. [DOI] [PubMed] [Google Scholar]
- 22.De La Cruz N, Crookston B, Gray B, Alder S, Dearden K. Microfinance against malaria: impact of Freedom from Hunger's malaria education when delivered by rural banks in Ghana. Trans R Soc Trop Med Hyg. 2009;103:1229–1236. doi: 10.1016/j.trstmh.2009.03.018. [DOI] [PubMed] [Google Scholar]
- 23.Flax VL, Negerie M, Ibrahim AU, Leatherman S, Daza EJ, Bentley ME. Integrating group counseling, cell phone messaging, and participant-generated songs and dramas into a microcredit program increases Nigerian women's adherence to international breastfeeding recommendations. J Nutr. 2014;144:1120–1124. doi: 10.3945/jn.113.190124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Amin R, St. Pierre M, Ahmed A, Haq R. Integration of an essential services package (ESP) in child and reproductive health and family planning with a micro-credit program for poor women: experience from a pilot project in Rural Bangladesh. World Dev. 2001;29:1611–1621. [Google Scholar]
- 25.Kim JC, Watts CH, Hargreaves JR, Ndhlovu LX, Phetla G, Morison LA, Busza J, Porter JDH, Pronyk P. Understanding the impact of a microfinance-based intervention on women's empowerment and the reduction of intimate partner violence in South Africa. Am J Public Health. 2007;97:1794–1802. doi: 10.2105/AJPH.2006.095521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sherer RD, Bronson JD, Teter CJ, Wykoff RF. Microeconomic loans and health education to families in impoverished communities: implications for the HIV pandemic. J Int Assoc Physicians AIDS Care (Chic) 2004;3:110–114. doi: 10.1177/154510970400300402. [DOI] [PubMed] [Google Scholar]
- 27.Hamad R, Fernald LC, Karlan DS. Health education for microcredit clients in Peru: a randomized controlled trial. BMC Public Health. 2011;11:51. doi: 10.1186/1471-2458-11-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Desai J, Tarozzi A. Microcredit, family planning programs, and contraceptive behavior: evidence from a field experiment in Ethiopia. Demography. 2011;48:749–782. doi: 10.1007/s13524-011-0029-0. [DOI] [PubMed] [Google Scholar]
- 29.Montalvao J, Nair N, Rath S, Mahapatra R, Sinha R, Prost A, Costello A, Tripathy P, Skordis-Worrall J. Health Education and Microfinance: Complements or Substitutes in Reducing Neonatal Mortality? Evidence from a Cluster-RCT in Rural India. 2013. http://discovery.ucl.ac.uk/1407954/ Available at. Accessed June 3, 2016.
- 30.Sherer RD, Bronson JD, Teter CJ, Wykoff RF. Microeconomic loans and health education to families in impoverished communities: implications for the HIV pandemic. J Int Assoc Physicians AIDS Care JIAPAC. 2004;3:110–114. doi: 10.1177/154510970400300402. [DOI] [PubMed] [Google Scholar]
- 31.Smith S. Village baking and maternal and child health: evidence from Ecuador and Honduras. World Dev. 2002;30:707–723. [Google Scholar]
- 32.Ahmed SM, Petzold M, Kabir ZN, Tomson G. Targeted intervention for the ultra poor in rural Bangladesh: does it make any difference in their health-seeking behaviour? Soc Sci Med. 2006;63:2899–2911. doi: 10.1016/j.socscimed.2006.07.024. [DOI] [PubMed] [Google Scholar]
- 33.Ioannidis JP, Haidich AB, Pappa M, Pantazis N, Kokori SI, Tektonidou MG, Contopoulos-Ioannidis DG, Lau J. Comparison of evidence of treatment effects in randomized and nonrandomized studies. JAMA. 2001;286:821–830. doi: 10.1001/jama.286.7.821. [DOI] [PubMed] [Google Scholar]
- 34.WHO Country Cooperation Strategies and Briefs: Benin. 2012. http://www.who.int/countryfocus/cooperation_strategy/ccsbrief_ben_en.pdf Available at. Accessed December 15, 2015.
- 35.Enquête Démographique et de Santé (EDSB-III): Bénin 2006. Calverton, MD: Institut National de la Statistique et de l'Analyse Économique (INSAE) [Bénin] et Macro International Inc; 2007. http://www.dhsprogram.com/pubs/pdf/FR197/FR197.pdf Available at. Accessed June 6, 2016. [Google Scholar]
- 36.World Health Organization Benin: Factsheets of Health Statistics 2010. 2010. https://www.ecoi.net/file_upload/1788_1322490858_benin-statistical-factsheet.pdf Available at. Accessed June 6, 2016.
- 37.Gray B, Ekoue-Kouvahey T. Microfinance and Health Protection Initiative Research Summary Report: PADME. 2010. https://www.freedomfromhunger.org/mahp-research-summary-report-padme 9D: Freedom from Hunger. Available at. Accessed November 14, 2016.
- 38.Reinsch M, Ruaz F. Costs and Benefits of Credit with Education: The Case of PADME in Benin. 2010. https://www.freedomfromhunger.org/sites/default/files/MAHP.CostBenefitPaper.PADME_.Paper10d.Eng_.pdf Available at. Accessed June 29, 2016.
- 39.Beaman L, Karlan D, Thuysbaert B, Udry C. Self-Selection into Credit Markets: Evidence from Agriculture in Mali. National Bureau of Economic Research; 2014. http://www.nber.org/papers/w20387 Available at. Accessed June 7, 2016. [Google Scholar]
- 40.Kling JR, Liebman JB, Katz LF. Experimental analysis of neighborhood effects. Econometrica. 2007;75:83–119. [Google Scholar]
- 41.Rogers W. Regression Standard Errors in Clustered Samples. 1993. http://www.stata.com/products/stb/journals/stb13.pdf Available at. Accessed October 10, 2016.
- 42.UNFPA and Research and Applications for Alternative Financing for Development (RAFAD) Exploring Linkages: Women's Empowerment, Microfinance and Health Education. 2011. http://www.unfpa.org/sites/default/files/pub-pdf/Exploring%20Linkages%20-%20Women%27s%20Empowerment%2C%20Microfinance%20and%20Health%20Education.pdf Available at. Accessed June 7, 2016.
- 43.Karlan D. The Next Stage of Financial Inclusion (SSIR) Stanf Soc Innov Rev. 2014 http://ssir.org/articles/entry/the_next_stage_of_financial_inclusion Available at. Accessed June 3, 2016. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.