Abstract
Diabetes mellitus (DM) is considered one of the major chronic diseases in the world. Long-term hyperglycemia considerably affects the body tissues, and consequently, can lead to morbidity and mortality. Moreover, many oral complications have been observed with DM but little consideration in relation to the placement of dental implants has been investigated. Dental research has analyzed the relation of dental implants and bone osseointegration in diabetic patients. Theoretically, an impaired immune system and delayed wound healing of these patients might decrease the success rate of implant placement; however, with noticeable advances in evidence-based dentistry and statistically significant results, successful implant treatment could be achieved significantly in well-controlled diabetic patients.
Recently, diabetes mellitus (DM) has become one of the most common metabolic disorders in the world.1 There are greater than 25 million people worldwide suffering from this disease.2 For instance, in the United Kingdom, there are 3.9 million people suffering from diabetes.3 Moreover, it is estimated that in 2014, there were 387 million diabetic patients all over the world, and this number is expected to rise to 592 million by 2035.3 These patients suffer from various systemic complications that affect their body organs, such as cardiovascular diseases, increased blood sugar levels, and eye diseases.4 Furthermore, they may have oral complications, such as dry mouth and dental caries.5 It is common for diabetic patients to have multiple missing teeth as a result of periodontal diseases, which are associated with metabolic disorder. Thus, to improve their mastication function, psychological well-being, and cosmetic concerns, replacing missing teeth in these patients is one of the most common dental procedures. Currently, dental implants are increasing in use for replacing missing teeth. According to the American Implant Association, a dental implant is a titanium screw used to support one or more missing teeth.6 It integrates into the jawbone to replace the root of a tooth when it is lost. Diabetic patients are ideal candidates for dental implant placement. However, there is evidence in the literature to suggest that impaired wound healing in diabetic patients is an issue that needs to be considered when performing this procedure in such patients.7 This review aims to discuss different modalities to achieve ultimate oral health status with dental implants in diabetic patients. By using evidence-based dentistry (EBD), we aim to explain the controversial theories of dental implant placement in diabetic patients.
Diabetes mellitus
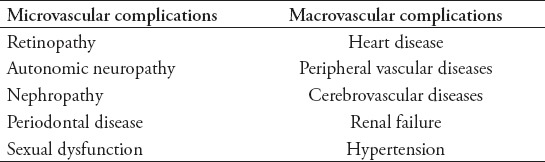
According to the American Diabetes Association, DM is defined as a chronic endocrinal disease characterised by glucose intolerance associated with numerous complications.4 Many studies have assessed oral complications in relation to hyperglycemia (Table 1). Additionally, it is widely accepted that diabetic complications can be microvascular (small blood vessels) and macrovascular (large blood vessels) (Table 2), affecting the oral cavity with subsequent peri-implant bone loss.8 For instance, improper wound healing around the dental implant with weak integration to the jawbone is one of the challenges faced by dentists. Furthermore, the significant metabolic disorder in DM could affect the normal physiological process of healing mechanisms.9 However, dental implant placement needs an ultimate level of integration into the jawbone to achieve successful results and to avoid the complications in medically compromised patients, in particular diabetic patients.10 For this reason, the dental treatment plan has been modified and different treatment modalities have been enhanced to achieve a high quality of oral health services. Implant placement depends on case selection and requires many parameters to achieve positive results and successful treatment for patients. Future complications are expected, and the true longevity of implants might be impossible to achieve.11
Table 1.
Oral complications among diabetic patients.
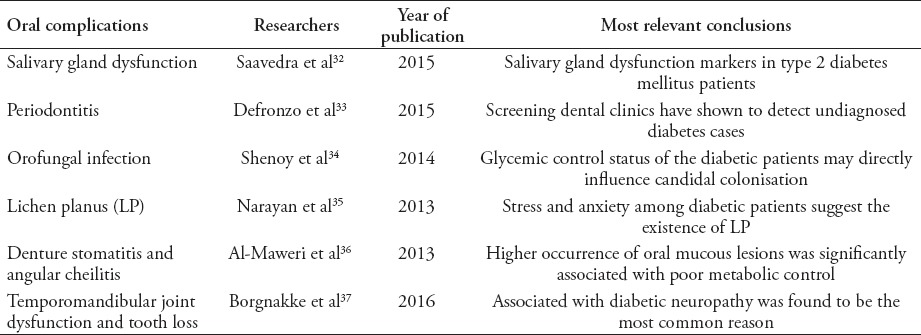
Table 2.
Long-term systemic complications of diabetes mellitus.
Impact of healing process in diabetic patients
Ajami et al12 reported that diabetic patients have a tendency for delayed bone healing and an impaired osteoconduction mechanism around the integrated bone screw, resulting in failure of the dental implant. A systemic literature study13 has proven a successful dental implant osseointegration in well glycemic-controlled diabetic patients in comparison with non-diabetic subjects. In addition, biomedical research has improved the dental implant concept in combination with clinical practice to be more relative to patient outcomes.
Evidence-based dentistry has suggested various medical considerations for diabetic patients to achieve successful bone healing around the dental implant and to overcome the complications of high blood glucose levels. Moreover, well-controlled blood glucose levels will enhance the physiological structure of the whole body at the clinical and subclinical levels, ultimately improving the healing process.14 Recently, a systemic review and meta-analysis published by medical scientists at the University of Malmo observed that well-controlled diabetic patients could be considered as healthy subjects. “The difference between the patients (diabetic versus non-diabetic) did not significantly affect implant failure rates (p=0.65), with a risk ratio of 1.07 (95% confidence interval=0.80, 1.44)”.15
These statistical results illustrate that well-controlled blood glucose levels are regarded as the gold standard to achieve ultimate healing process and to improve the integration of the dental implant in the jawbone. Thus, a dental implant is a relative contraindication in diabetic patients rather than an absolute contraindication.
Rationale of antibiotic prophylaxis in diabetic patients
It seems that diabetic patients have a tendency for dental infection, which is an extremely serious medical condition if it occurs in the bone. Hegab states that diabetic patients are more prone to dental infection due to a dysfunction in their immune system, which means that they may be more prone to bone infection around the dental implant.16 Furthermore, the microorganisms of the mouth may increase the likelihood of infection around the implant.17 However, although diabetic patients have a tendency for dental infection, EBD and biological oral studies provide measurements to decrease the chance of infection and avoid the normal bacteria in the mouth acting as a risk factor.
There is, perhaps, some evidence that the influence of antibiotics in medically compromised patients, such as diabetic subjects, is effective in decreasing dental infection.18 For instance, the use of an antibiotic prophylactic increases the success rate of dental implants by 96.47%.19 Recently, medical scientists at the University of Ohio compared the effectiveness of different types of antibiotics before the surgical placement of the dental implant.20 They found that antibiotics tended to reduce dental infection and minimise inflammation to a greater extent.
It is routinely sufficient to administer 2 g of amoxicillin pre-operatively (one hour before the procedure) as a prophylactic prior to dental implant placement.21 Additional post-operative antimicrobial doses might lead to adverse side effect, such as severe allergic reaction that requires hospital admission.21 Additionally, Escalante et al20 suggested that preoperative administration of 500 mg of azithromycin helps in reducing post-surgical inflammation of dental implant placement more than 2 g of amoxicillin.20 However, there is no obvious agreement and recommendation regarding the type and does of antimicrobial that can be considered prior the dental implant placement.22
These studies clearly showed that prophylactic antibiotics are among the most important factors to accelerate the healing process around the implant by decreasing the risk of infection, thereby significantly increasing the dental implant success rate. Moreover, studies suggest that mouthwash could be used as an antiseptic agent before and after dental implant therapy.23 In addition, researchers at the University of Pisa, Italy,24 assessed the effectiveness of mouthwash on 40 diabetic patients and observed a clear significant effect of 0.12% concentration of antiseptic mouth rinse. Furthermore, they found that there is an obvious clinical enhancement in bone implant integration. Consequently, this clinical study proved that antiseptic mouthwashes could significantly affect the quality of the healing process by decreasing the rate of dental infection.
Impact of glycemic control in the success rate of dental implant
It seems that hyperglycemia, which is an increase in the blood glucose level above the normal level, could affect the success rate of the dental implant. According to Gonnelli et al,25 diabetic patients have a tendency for low bone formation that could result in a bone fracture.25 This poor bone quality is usually caused by inconsistent blood glucose levels, which affect the bone cells that are responsible for bone formation. Furthermore, Alsaadi et al26 claimed that the integration of the implant into the diabetic jawbone is disorganised.26 Thus, the disorganised bone tends to increase the possibility of a bone fracture. However, this study evaluated the quality of the dental implant in diabetic patients with non-controlled diabetes rather than assessing the situation in well-controlled diabetic patients. Moreover, this study examined the validity of implant dentistry in diabetic patients with other systemic diseases.
Nevertheless, although the quality of bone in hyperglycemic patients may affect the integration of the dental implant and the surrounding jawbone, it is worth nothing that most of the failure rates in implant therapy are related to poorly controlled diabetes. There is a distinct lack in the impact of the updated knowledge and advancement in clinical research that has demonstrated positive outcomes of implant therapy in diabetic patients. In accordance with dental research, a clinical study conducted at the University of Texas Health Science Centre in San Antonio stated that the survival rate of dental implants was 99% after one year of follow up in 117 diabetic patients. They received 2 implants with a total 234 dental implants.7 Furthermore, Jadhav et al27 in their systemic review of diabetic patients, made it clear that the success rate of dental implants was determined largely by glycemic control. “Diabetes is no contraindication for implant placement, on condition that it remains under metabolic control.”27
It is recommended to measure the HbA1c (Glycosylated Hemoglobin Assay) prior dental implant placement procedure.27 The HbA1c assists in determining the average blood glucose level during the 2-3 months. It is well known that HbA1c has been classified into 3 different levels (6-8% as well controlled diabetes, 8-10% as moderate, and >10% poorly controlled diabetes).28 Although Khandelwal et al29 reported that poorly controlled diabetes (7.5-11.4%) have successful implant placement, studies30,31 clearly show that well controlled diabetic patients have less peri-implantitis and better implant survival rate.
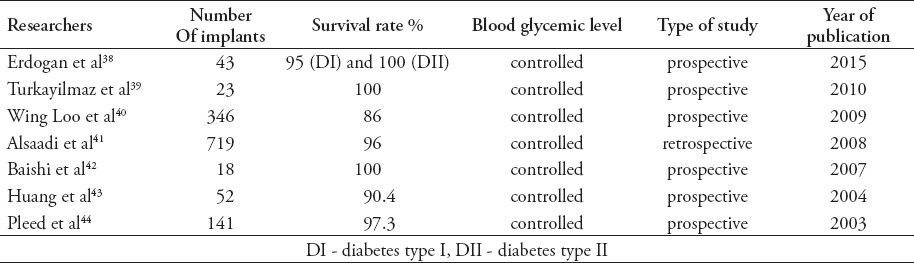
These results have shown that the survival rate of dental implants in diabetic patients has increased significantly. In addition, it has clearly shown that the failure rate of implant therapy in diabetic patients in the previously mentioned studies should be interpreted with caution due to of the lack of knowledge on recent advances in clinical dental research (Table 3).
Table 3.
Studies show successful dental implant placement in well-controlled diabetic patients.
In conclusion, it is clearly shown that the failure rate of dental implant placement in diabetic patients should be interpreted with caution. However, EBD in relation to biomedical clinical studies has proven that successful treatment using dental implants can be achieved significantly in well-controlled diabetic patients. In general, medical considerations for achieving better integration of dental implants in diabetic patients are well controlled HbA1c, use of prophylactic antibiotics and 0.12% antiseptic mouthwash (Figure 1).
Figure 1.
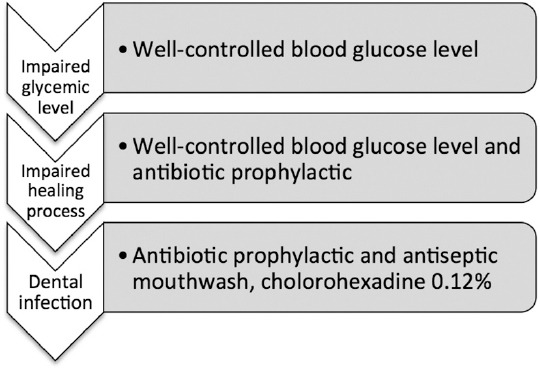
The most common causes of dental implant failure in diabetic patients.
Further clinical trial studies are required in conjunction with regular follow up to assess the longevity of dental implants in human subjects rather than animal models. Moreover, involving other medical professionals and adjusting anti-diabetic medication doses are critical to achieve an ultimate standard of oral healthcare. Studies show other major factors that must be evaluated as it can affect success rate of the treatment such as type of dental implant, placement protocol, and loading protocol. Therefore, dental practitioners must update their knowledge on DM regularly to provide a high standard of dental treatment and to encourage their patients to control their HBA1c, enabling them to be suitable candidates for treatment with dental implants. Additionally, patient education through social media and community campaigns is required to achieve an ultimately effective oral health service.
Footnotes
References
- 1.Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94:311–321. doi: 10.1016/j.diabres.2011.10.029. [DOI] [PubMed] [Google Scholar]
- 2.McCabe L, Zhang J, Raehtz S. Understanding the skeletal pathology of type 1 and 2 diabetes mellitus. Crit Rev Eukaryot Gene Expr. 2011;21:187–206. doi: 10.1615/critreveukargeneexpr.v21.i2.70. [DOI] [PubMed] [Google Scholar]
- 3.Diabetes United Kingdome. Diabetes: facts and stats. Diabetes UK. 2014;3:1–20. [Google Scholar]
- 4.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes care. 2014;37(Suppl 1):S81–S90. doi: 10.2337/dc14-S081. [DOI] [PubMed] [Google Scholar]
- 5.Al-Maskari AY, Al-Maskari MY, Al-Sudairy S. Oral manifestations and complications of diabetes mellitus: A review. Sultan Qaboos Univ Med J. 2011;11:179–186. [PMC free article] [PubMed] [Google Scholar]
- 6.Misch CE. Dental implant prosthetics. 2nd ed. Michigan (US): Elsevier Health Sciences; 2014. pp. 26–461. [Google Scholar]
- 7.Oates TW, Jr, Galloway P, Alexander P, Vargas Green A, Huynh-Ba G, Feine J, et al. The effects of elevated hemoglobin A(1c) in patients with type 2 diabetes mellitus on dental implants: Survival and stability at one year. J Am Dent Assoc. 2014;145:1218–1226. doi: 10.14219/jada.2014.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ghiraldini B, Conte A, Casarin RC, Casati MZ, Pimentel SP, Cirano FR, et al. Influence of Glycemic Control on Peri-Implant Bone Healing:12-Month Outcomes of Local Release of Bone-Related Factors and Implant Stabilization in Type 2 Diabetics. Clin Implant Dent Relat Res. 2016;18:801–809. doi: 10.1111/cid.12339. [DOI] [PubMed] [Google Scholar]
- 9.Swati S. Implants in Diabetic Patients. Int J Oral Implantol. 2013;4:30–35. [Google Scholar]
- 10.Dubey RK, Gupta DK, Singh AK. Dental implant survival in diabetic patients;review and recommendations. Nat J Maxillofac Surg. 2013;4:142–150. doi: 10.4103/0975-5950.127642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pjetursson BE, Asgeirsson AG, Zwahlen M, Sailer I. Improvements in implant dentistry over the last decade: comparison of survival and complication rates in older and newer publications. Int J Oral Maxillofac Implants. 2014;29(Suppl):S308–S324. doi: 10.11607/jomi.2014suppl.g5.2. [DOI] [PubMed] [Google Scholar]
- 12.Ajami E, Mahno E, Mendes V, Bell S, Moineddin R, Davies JE. Bone healing and the effect of implant surface topography on osteoconduction in hyperglycemia. Acta biomater. 2014;10:394–405. doi: 10.1016/j.actbio.2013.09.020. [DOI] [PubMed] [Google Scholar]
- 13.Javed F, Romanos GE. Impact of diabetes mellitus and glycemic control on the osseointegration of dental implants: a systematic literature review. J Periodontol. 2009;80:1719–1730. doi: 10.1902/jop.2009.090283. [DOI] [PubMed] [Google Scholar]
- 14.Katyayan PA, Katyayan M, Shah RJ. Rehabilitative considerations for dental implants in the diabetic patient. J Indian Prosthodont Soc. 2013;13:175–183. doi: 10.1007/s13191-012-0207-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chrcanovic BR, Albrektsson T, Wennerberg A. Diabetes and oral implant failure: a systematic review. J Dent Res. 2014;93:859–867. doi: 10.1177/0022034514538820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hegab A. Dental infection and diabetes: The cycle. Oral Hygiene and Health. 2014:3e110. [Google Scholar]
- 17.Heydenrijk K, Meijer HJ, van der Reijden WA, Raghoebar GM, Vissink A, Stegenga B. Microbiota around root-form endosseous implants: a review of the literature. Int J Oral Maxillofac Implants. 2002;17:829–838. [PubMed] [Google Scholar]
- 18.Little JW, Falace DA, Miller CS, Rhodus NL. Antibiotic prophylaxis in dentistry: an update. Gen Dent. 2008;56:20–28. [PubMed] [Google Scholar]
- 19.Keenan JR, Veitz-Keenan A. Antibiotic prophylaxis for dental implant placement? Evid Based Dent. 2015;16:52–53. doi: 10.1038/sj.ebd.6401097. [DOI] [PubMed] [Google Scholar]
- 20.Escalante MG, Eubank TD, Leblebicioglu B, Walters JD. Comparison of Azithromycin and Amoxicillin Before Dental Implant Placement: An Exploratory Study of Bioavailability and Resolution of Postoperative Inflammation. J periodontal. 2015;86:1190–1200. doi: 10.1902/jop.2015.150024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Arduino PG, Tirone F, Schiorlin E, Esposito M. Single preoperative dose of prophylactic amoxicillin versus a 2-day postoperative course in dental implant surgery: A two-centre randomised controlled trial. Eur J Oral Implantol. 2015;8:143–149. [PubMed] [Google Scholar]
- 22.Deeb GR, Soung GY, Best AM, Laskin DM. Antibiotic Prescribing Habits of Oral and Maxillofacial Surgeons in Conjunction With Routine Dental Implant Placement. J Oral Maxillofac Surg. 2015;73:1926–1931. doi: 10.1016/j.joms.2015.05.024. [DOI] [PubMed] [Google Scholar]
- 23.Pedrazzi V, Escobar EC, Cortelli JR, Haas AN, Andrade AK, Pannuti CM, et al. Antimicrobial mouthrinse use as an adjunct method in peri-implant biofilm control. Braz Oral Res. 2014;28 doi: 10.1590/1807-3107BOR-2014.vol28.0022. Spec No. pii: S1806-83242014000200301. [DOI] [PubMed] [Google Scholar]
- 24.Genovesi A, Barone A, Toti P, Covani U. The efficacy of 0.12% chlorhexidine versus 0.12% chlorhexidine plus hyaluronic acid mouthwash on healing of submerged single implant insertion areas: a short-term randomized controlled clinical trial. Int J Dent Hyg. 2015 doi: 10.1111/idh.12158. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 25.Gonnelli S, Caffarelli C, Giordano N, Nuti R. The prevention of fragility fractures in diabetic patients. Aging Clin Exp Res. 2015;27:115–124. doi: 10.1007/s40520-014-0258-3. [DOI] [PubMed] [Google Scholar]
- 26.Alsaadi G, Quirynen M, Komárek A, Van Steenberghe D. Impact of local and systemic factors on the incidence of oral implant failures, up to abutment connection. J Clin Periodontol. 2007;34:610–617. doi: 10.1111/j.1600-051X.2007.01077.x. [DOI] [PubMed] [Google Scholar]
- 27.Jadhav RD, Sabane AV, Gandhi PV, Thareja A. Dental implant in diabetic patients: Statement of facts. Indian Journal of Oral Sciences. 2015;6:47–50. [Google Scholar]
- 28.Naujokat H, Kunzendorf B, Wiltfang J. Dental implants and diabetes mellitus—a systematic review. International Journal of Implant Dentistry. 2016;2:5. doi: 10.1186/s40729-016-0038-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Khandelwal N, Oates TW, Vargas A, Alexander PP, Schoolfield JD, Alex McMahan C. Conventional SLA and chemically modified SLA implants in patients with poorly controlled type 2 diabetes mellitus--a randomized controlled trial. Clin Oral Implants Res. 2013;24:13–19. doi: 10.1111/j.1600-0501.2011.02369.x. [DOI] [PubMed] [Google Scholar]
- 30.Aguilar-Salvatierra A, Calvo-Guirado JL, González-Jaranay M, Moreu G, Delgado-Ruiz RA, Gómez-Moreno G. Peri-implant evaluation of immediately loaded implants placed in esthetic zone in patients with diabetes mellitus type 2: a two-year study. Clin Oral Implants Res. 2016;27:156–161. doi: 10.1111/clr.12552. [DOI] [PubMed] [Google Scholar]
- 31.Gómez-Moreno G, Aguilar-Salvatierra A, Rubio Roldán J, Guardia J, Gargallo J, Calvo-Guirado JL. Peri-implant evaluation in type 2 diabetes mellitus patients: a 3-year study. Clin Oral Implants Res. 2015;26:1031–1035. doi: 10.1111/clr.12391. [DOI] [PubMed] [Google Scholar]
- 32.Aitken-Saavedra J, Rojas-Alcayaga G, Maturana-Ramírez A, Escobar-Álvarez A, Cortes-Coloma A, Reyes-Rojas M, et al. Salivary gland dysfunction markers in type 2 diabetes mellitus patients. J Clin Exp Dent. 2015:7e501–e505. doi: 10.4317/jced.52329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.DeFronzo RA. Pathogenesis of type 2 diabetes mellitus. In: In DeFronzo RA, Ferrannini E, Zimmet P, Alberti G, editors. International Textbook of Diabetes Mellitus. 4th ed. Chichester (UK): Wiley Blackwell; 2015. pp. 371–400. [Google Scholar]
- 34.Shenoy MP, Puranik RS, Vanaki SS, Puranik SR, Shetty P, Shenoy R. A comparative study of oral candidal species carriage in patients with type1 and type2 diabetes mellitus. J oral Maxillofac Pathol. 2014;18(Suppl 1):S60–S65. doi: 10.4103/0973-029X.141361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Narayan V, Gnanasundaram N, Arvind M. Prevalence of Oral Lichen Planus in Patients with Diabetes Mellitus. Journal of Indian Academy of Oral Medicine and Radiology. 2013;25:261–264. [Google Scholar]
- 36.Al-Maweri SA, Ismail NM, Ismail AR, Al-Ghashm A. Prevalence of oral mucosal lesions in patients with type 2 diabetes attending hospital universiti sains malaysia. Malays J Med Sci. 2013;20:39–46. [PMC free article] [PubMed] [Google Scholar]
- 37.Borgnakke WS, Anderson PF, Shannon C, Jivanescu A. Is there a relationship between oral health and diabetic neuropathy? Curr Diab Rep. 2015;15:93. doi: 10.1007/s11892-015-0673-7. [DOI] [PubMed] [Google Scholar]
- 38.Erdogan Ö, Uçar Y, Tatlı U, Sert M, Benlidayı ME, Evlice B. A clinical prospective study on alveolar bone augmentation and dental implant success in patients with type 2 diabetes. Clin Oral Implants Res. 2015;26:1267–1275. doi: 10.1111/clr.12450. [DOI] [PubMed] [Google Scholar]
- 39.Turkyilmaz I. One-year clinical outcome of dental implants placed in patients with type 2 diabetes mellitus: a case series. Implant Dent. 2010;19:323–329. doi: 10.1097/ID.0b013e3181e40366. [DOI] [PubMed] [Google Scholar]
- 40.Loo WT, Jin L, Cheung MN, Wang M. The impact of diabetes on the success of dental implants and periodontal healing. African Journal of Biotechnology. 2009;8:5122–5127. [Google Scholar]
- 41.Alsaadi G, Quirynen M, Komárek A, van Steenberghe D. Impact of local and systemic factors on the incidence of late oral implant loss. Clin Oral Implants Res. 2008;19:670–676. doi: 10.1111/j.1600-0501.2008.01534.x. [DOI] [PubMed] [Google Scholar]
- 42.Balshi SF, Wolfinger GJ, Balshi TJ. An examination of immediately loaded dental implant stability in the diabetic patient using resonance frequency analysis (RFA) Quintessence Int. 2007;38:271–279. [PubMed] [Google Scholar]
- 43.Huang JS, Zhou L, Song GB. [Dental implants in patients with Type 2 diabetes mellitus: a clinical study] Shanghai Kou Qiang Yi Xue. 2004;13:441–443. Chinese. [PubMed] [Google Scholar]
- 44.Peled M, Ardekian L, Tagger-Green N, Gutmacher Z, Machtei EE. Dental implants in patients with type 2 diabetes mellitus: a clinical study. Implant Dent. 2003;12:116–122. doi: 10.1097/01.id.0000058307.79029.b1. [DOI] [PubMed] [Google Scholar]


