Abstract
Aerosolisation performance of hygroscopic particles of colistin could be compromised at elevated humidity due to increased capillary forces. Co-spray drying colistin with a hydrophobic drug is known to provide a protective coating on the composite particle surfaces against moisture-induced reduction in aerosolisation performance; however, the effects of component ratio on surface coating quality and powder aerosolisation at elevated relative humidities are unknown. In this study, we have systematically examined the effects of mass ratio of hydrophobic azithromycin on surface coating quality and aerosolisation performance of the co-spray dried composite particles. Four combination formulations with varying drug ratios were prepared by co-spray drying drug solutions. Both of the drugs in each combination formulation had similar in vitro deposition profiles, suggesting that each composite particle comprise two drugs in the designed mass ratio, which is supported by XPS and ToF-SIMS data. XPS and ToF-SIMS measurements also revealed that 50 % by weight (or 35 % by molecular fraction) of azithromycin in the formulation provided a near-complete coating of 96.5 % (molar fraction) on the composite particle surface, which is sufficient to prevent moisture-induced reduction in FPFrecovered and FPFemitted. Higher azithromycin content did not increase coating coverage, while contents of azithromycin lower than 20 %w/w did not totally prevent the negative effects of humidity on aerosolisation performance. This study has highlighted that a critical amount of azithromycin is required to sufficiently coat the colistin particles for short-term protection against moisture.
Keywords: Dry powder inhaler, respiratory infection, combination antibiotics, amorphous particle, hygroscopicity, moisture protection, surface coating, surface chemistry characterization, X-ray photoelectron spectroscopy, time-of-flight secondary ion mass spectrometry
INTRODUCTION
Respiratory infections are difficult to treat because only limited amounts of drugs become available at the infection sites in the lower airways after traditional oral or parenteral drug administration (1). Consequently, high doses of drugs are required to maintain drug levels above the minimum inhibitory concentrations (MIC) in the airways (2, 3). For many antibiotics, systemic therapies can cause severe adverse effects. Colistin has been used as an antibiotic for many respiratory infections caused by multidrug resistant (MDR) Gram-negative bacilli as a last resort, but intravenous administration of high-dose colistin can lead to dose-limiting nephrotoxicity in more than half of the treated cystic fibrosis (CF) patients (4). Pulmonary delivery of antibiotics is advantageous as high drug concentrations may be attained in the airways while minimising systemic exposure (5–7). Yapa et al. has reported that nebulised colistin methanesulphonate (CMS) solution (4 million IU) achieved significantly higher colistin concentrations in the sputum (Cmax 4 – 16 mg/L) of CF patients; the colistin concentrations were maintained above MIC for 12 h with low systemic exposure (Cmax in plasma < 0.5 mg/L) (8).
Dry powder inhalers (DPIs) have gained increasing interest for the delivery of high-dose antibiotics directly to the respiratory tract as DPI devices are generally more portable than than traditional jet nebulisers and drug powders are more stable than liquid forms of drugs. (6, 9). However, inhalation of high-dose powders could cause local side effects such as cough and throat irritation (1, 3, 10). Fine drug particles produced by conventional jet-milling are often cohesive with poor flow and dispersion properties (11). Addition of free-flowing coarse carriers is a common approach to manufacture dry powder formulations of low-dose therapeutics (12); but this approach increases the mass and volume of each dose and make inhalers bulky for high-dose or multi-dose medications (6). To formulate high-dose antibiotics, particle engineering is essential to generate free-flowing and highly dispersible fine drug powders (13). Spray drying is a popular approach to engineer inhalable drug particles with a superior capability to manipulate particulate properties (14). Spray drying is scalable and has been employed for the manufacture of insulin (Exubera®, Pfizer), tobramycin (TOBI® Podhaler®, Novartis) and mannitol (Aridol®, Pharmaxis) DPIs. The addition of amino acids has been reported to reduce powder cohesion and improve aerosolisation performance of spray-dried powders by decreasing free surface energy (15, 16). Porous fine drug particles with satisfactory flow and dispersion behaviour can also be produced via spray drying (17, 18).
One of the challenges in the production of inhalable drug particles by spray drying is that the spray-dried amorphous particles are often hygroscopic and can absorb significant amounts of water upon exposure to humidity (19). The aerosolisation performance of such hygroscopic particles can be compromised under elevated humidities due to increased capillary forces between particles in contact. In our earlier study, inhalable powder formulations of colistin were developed by the spray drying approach without any additives (20). The spray-dried amorphous colistin powder absorbed up to 30 %w/w water when it was stored at high RH > 60 %. In a subsequent study, combination formulation of colistin with hydrophobic rifampicin (in a mass ratio of 1:1 or molecular ratio of approximately 1.7:1) was shown to prevent the moisture-induced deterioration in aerosolisation (21). The moisture protection effects were attributed to the surface coating of hydrophobic rifampicin. However, the effects of drug ratio in the spray drying feed solution on the surface coating and aerosolisation are unknown. In this study, colistin was co-spray-dried with a hydrophobic antibiotic, azithromycin, at various mass ratios as such combination has shown synergy in antimicrobial effects (22, 23). Surface coating coverage by azithromycin on particle surfaces was characterised by two surface analytical techniques, X-ray photoelectron spectroscopy (XPS) and time-of-flight secondary ion mass spectrometry (ToF-SIMS). The effects of surface coating on moisture protection were evaluated. The outcome of the present study could provide insights into the stability of hygroscopic DPI formulations under humid conditions.
MATERIALS AND METHODS
Chemicals
Colistin sulfate was purchased from Zhejiang Shenghua Biology Co., Ltd (Hangzhou, Zhejiang, China) and azithromycin was supplied from Hangzhou ICH Imp & Exp Co. Ltd. (Hangzhou, Zhejiang, China). Trifluoroacetic acid was purchased from Sigma-Aldrich (Castle Hill, NSW, Australia). Acetonitrile, ethanol and methanol (high-performance liquid chromatography, HPLC grade) were supplied by Fisher Scientific (Fair Lawn, NJ, USA).
Production of Powder Formulation by Spray Drying
A spray drying feed solution (10 mg/mL total solutes) containing azithromycin and colistin sulphate in mass ratios of 1:9, 1:4, 1:1, and 4:1 was prepared by dissolving two drugs in a solvent mixture of water and ethanol with a volumetric ratio of 1:1. The drug solution was pumped into the spray dryer (B-290 mini spray-dryer, Büchi Labortechnik AG, Falwil, Switzerland) at a feed rate of 2 mL/min. The spray dryer was operated under the following conditions: inlet air temperature 60 °C; atomizer setting 700 NL/h and aspirator flow rate 40 m3/h (21). The spray-dried powders were stored in a desiccator containing silica gel at 20 ± 3 °C till further use.
Particle Size
Laser diffraction (Mastersizer 2000, Malvern Instruments, Worcestershire, UK) was used to measure particle size distribution by the dry powder dispersion approach. Compressed air (4 bar) were applied to disperse powders (21). D10 (diameter at 10 % undersize), D50 (diameter at 50 % undersize), and D90 (diameter at 90 % undersize) were calculated using a software. Measurements for each sample were carried out in triplicate.
Particle Morphology
Particle morphology was assessed by scanning electron microscopy (SEM, Carl Zeiss SMT AG, Oberkochen, Germany). Each sample was mounted on an SEM stub and followed by sputter-coating of gold (K550X sputter coater, Quorum Emitech, Kent, UK).
Crystallinity
X-ray powder diffraction (XRPD) (Shimadzu XRD-6000, Shimadzu Corporation, Kyoto, Japan) was used for evaluating powder crystallinity with Cu-Kα radiation at 40 kV and 30 mA. The 2θ method was used for the measurement and data were recorded at 2 °/min in the scanning range of 5–50 °.
Dynamic Water Vapour Sorption
Moisture sorption behavior was measured by a dynamic vapour sorption system (DVS-1, Surface Measurement Systems Ltd., London, UK). Each sample was placed in the measurement chamber where the relative humidity (RH) values were maintained ranging from 0–90 %. The environmental RH was increased from 0 to 90 % for the sorption cycle and then decreased from 90 to 0 % for desorption cycle at 10 % RH increments. Equilibrium moisture content at each testing RH was determined by a dm/dt of 0.002 % per minute (20).
X-ray Photoelectron Spectroscopy
X-ray photoelectron spectroscopy (XPS) analysis was performed using an AXIS Ultra DLD Spectrometer (Kratos Analytical Ltd., Manchester, U.K.), equipped with a monochromated Al Kα source at a power of 180 W (12 mA, 15 kV). Each sample was filled into powder sample holders (24). Charging of the samples during irradiation was compensated by an electron flood gun in combination with a magnetic immersion lens. A reference binding energy of 285.0 eV for the aliphatic hydrocarbon C 1s component was used to correct for any remaining offsets due to charge neutralization of specimens under irradiation (25). The pressure in the main vacuum chamber during analysis was typically 10−6 Pa. Spectra were recorded with the nominal photoelectron detection normal to the sample surface. However, in the case of powders of random orientations, the microscopic emission angle is ill-defined. As a consequence, the sampling depth might vary between 0 nm and 5 – 10 nm depending on the kinetic energy of the measured photoelectrons. The area analyzed on each sample had approximate dimensions of 0.3 mm × 0.7 mm. The elemental composition of the samples was obtained from survey spectra (160 eV pass energy) using sensitivity factors supplied by the manufacturer. High-resolution spectra of individual peaks were recorded at 20 eV pass energy which results in a peak width (full width at half maximum) of typically 0.9 – 1.1 eV for organic polymeric materials.
In order to determine relative fractions of colistin and azithromycin on the surface of the composite particles, reference data were acquired from the two pure compounds. The data obtained from the combination particles were then compared to the reference data and fractions of the pure compounds estimated as follows. The atomic concentration of each of the present elements (C, O, N and S) in the combination particles was assumed to be a linear combination of the corresponding concentrations in the pure compounds, appropriately scaled and normalized using the number of respective atoms in one molecule of colistin or azithromycin. This method is particularly reliable in cases where the concentrations in the pure compounds are quite different (N and S) but rather unreliable in cases where concentrations are similar (C and O). However, in the case of C and O the high resolution 1s spectra for the two compounds are quite different because of the different chemical structures. This allows the surface fractions of colistin and azithromycin in the combination particles to be estimated using curve-fitting: the reference spectra of colistin and azithromycin can be used as two model-fit components to calculate optimized curve-fits of the spectra of the combination particles. A representative C 1s curve-fit is shown in Supplement 2. This yields the relative number of either C or O atoms which are present as part of either colistin or azithromycin (24). Scaled using the respective number of C or O atoms in one molecule of the pure compounds, these fractions can be converted to relative molecular fractions of colistin or azithromycin.
Time-of-flight Secondary Ion Mass Spectrometry
Time-of-flight secondary ion mass spectrometry (ToF-SIMS) experiments were performed using a PHI TRIFT V nanoTOF instrument (Physical Electronics Inc., Chanhassen, MN, USA) equipped with a pulsed liquid metal 79+Au primary ion gun (LMIG), operating at 30 keV energy. Dual charge neutralization was provided by an electron flood gun and 10 eV Ar+ ions. Spatial resolution was optimized for the collection of images by utilizing “unbunched” Au1 instrument settings. Raw data were collected in positive SIMS mode at a number of locations, typically using a 50 × 50 micron raster area, with 4 minute acquisitions (24).
Analysis of colistin and rifampicin standards identified characteristic peak fragments for use in mapping the components in the combination powders. Peaks corresponding to the protonated molecular ion signal for each antibiotic were of low intensity; hence higher intensity characteristic fragments were used instead. For colistin, the sum of peaks at m/z ~ 30 atomic mass unit (amu) and ~86 amu were selected, corresponding to CH4N+ and C5H12N+ fragments respectively. For azithromycin, the desosamine fragment at m/z ~ 158 amu (C8H16NO2+) and further fragment at m/z ~ 98 amu (C6H12N+) were selected. Sample spectra and images were processed using WincadenceN software (Physical Electronics Inc., Chanhassen, MN, USA).
Powder storage
Effect of humidity on aerosolisation was examined by storing the spray-dried formulations under two RH conditions (60 % for the moderate RH and 75 % for the elevated RH) which were selected based on previous work (20). Each formulation (approximately 100 – 200 mg) was spread in a thin layer on an open-top plastic container (3 cm in diameter) and stored in a humidity chamber set at 60 % RH or in a desiccator containing saturated sodium chloride solution (75 % RH) at 25 °C for 24 hours. Based on water sorption studies carried out using the DVS, 24 hours is more than sufficient for the powders to attain water vapour sorption equilibrium. Aerosolisation performance of the powder formulations after storage under the two different RH were measured as described below.
In vitro Aerosol Performance
In vitro aerosol performance was measured using a multi-stage liquid impinger (Apparatus C, British Pharmacopeia 2012, Copley, Nottingham, UK) with a USP induction port (USP throat) according to pharmacopeial dispersion procedure : to achieve a pressure drop of < 4 kPa across the device, 4 L of air was drawn by a vacuum pump through the inhaler device at an airflow rate of 100 L/min for 2.4 s (17). The cut-off diameters of stages 1–4 of the liquid impinger at 100 L/min were 10.4, 4.9, 2.4 and 1.2 μm, respectively.
An accurately-weighed amount of each spray-dried powder (10 ± 2 mg) was loaded into a capsule (size 3 hydroxypropyl methylcellulose capsules, Capsugel, West Ryde, NSW, Australia) and dispersed through an Aerolizer® in an enclosed chamber with the RH maintained at 60 % or 75 % RH at 20 ± 3 °C. The dispersion was repeated with a second capsule containing a similar amount of the spray-dried powder. The dose chosen here is to generate sufficient drug concentration in each stage of impactor for chemical assay. The clinically relevant dose of each drug could be higher than the dose chosen in this study. The Aerolizer® was used because it is an inhaler device with a low resistance that allows patients to comfortably generate sufficient high airflow rates to effectively disperse powder formulations. Four replicated experiments were carried out for each formulation, with each experiment comprising sequential dispersions of two filled capsules.
Drug particles deposited in the capsules, inhaler, USP throat, stages 1–4 of the liquid impinger and the filter were collected using appropriate volumes of a 1:1 solvent mixture of 0.02 M phosphate buffer (pH 5.0) and methanol. The emitted dose (ED) was defined as the total amount of drug collected in the throat, stages 1–4 of the impinger and the final filter stage expressed as a percentage of the total recovered amount of drug. Fine particle fraction (FPFrecovered) was defined as the total amount of drug particles with an aerodynamic diameter smaller than 4.9 μm (cut-off diameter of the stage 2) expressed as a percentage of the total recovered amount of drug. FPFemitted was defined as the FPF over the emitted dose.
Drug Quantification
After dispersion, the concentrations of colistin and azithromycin in the collecting solvent were determined by high performance liquid chromatography (HPLC) using a method modified from previous studies (20, 26). A Shimadzu CBM-20A controller, LC-20AT pump, SIL-20A HT autosampler, SPD-20A UV/VIS detector (Shimadzu, Kyoto, Japan) and a PhenoSphere-Next 5 μm C18 150×4.60 mm column (Phenomenex, Torrance, CA) were used.
Two drugs in the collecting solvents are analysed separately. For colistin sulphate, the mobile phase consisted of 0.05 % trifluoroacetic acid (A) and methanol (C). The injection volume for each run was 50 μL and colistin sulphate was eluted using a gradient program of 30 % C to 80 % C in 25 min, followed by 80 % C to 30 % C in 3 min at a flow rate of 1 mL/min (20). The mobile phase for azithromycin consisted of 20 % 0.02 M phosphate buffer (pH 8.0) and 80 % methanol flowing at 1 mL/min (26). The injection volume was 100 μL. The calibration curves, prepared for colistin and azithromycin in a 1:1 solvent mixture of 0.02 M phosphate buffer (pH 5.0) and methanol, were linear (r2 > 0.999) over the concentration range of approximately 0.005–0.3 mg/mL.
Statistical Analysis
One-way analysis of variance (ANOVA) with a Tukey post hoc analysis or independent sample t-test was employed for statistical analysis. Probability (p) values < 0.05 were considered as a statistically significant difference.
RESULTS
Physicochemical Properties
The size distributions of spray-dried particles are presented in Table 1. All the spray-dried samples had fine physical particle sizes (D90 < 2.90 μm). Pure COL had the highest D10, D50 and D90 values; while the formulation 1COL:4AZI had the lowest particle size.
Table 1.
Particle size distribution of powder formulations measured by laser diffraction. Mean ± SD, n = 3.
| D10 (μm) | D50 (μm) | D90 (μm) | |
|---|---|---|---|
| Pure COL | 0.80 ± 0.10 | 1.50 ± 0.10 | 2.90 ± 0.10 |
| 1AZI+9COL | 0.67 ± 0.01 | 1.33 ± 0.13 | 2.51 ± 0.45 |
| 1AZI+4COL | 0.56 ± 0.10 | 1.10 ± 0.02 | 1.98 ± 0.25 |
| 1AZI+1COL | 0.56 ± 0.09 | 1.23 ± 0.01 | 2.51 ± 0.33 |
| 4AZI+1COL | 0.47 ± 0.01 | 0.81 ± 0.02 | 1.49 ± 0.08 |
| Pure AZI | 0.51 ± 0.05 | 0.91 ± 0.07 | 1.66 ± 0.17 |
From the SEM micrographs (Fig. 1a), it can be observed that the spray-dried particles of 4COL:1AZI exhibited a near-spherical shape with corrugated surfaces, which appeared similar to spray-dried pure colistin (20). Spray-dried pure azithromycin had a spherical shape with slightly rough surfaces (Fig. 1d). When the colistin mass ratio was increased to 20 %, the particle surface became rougher (Fig. 1c). It is interesting to note that spray-dried composite particles with a mass ratio of 1:1 had a wrinkled shape that was distinct to both pure spray-dried colistin and azithromycin. From the SEM images, all spray-dried particles are approximately 1 – 2 μm, which agree with the laser diffraction results.
Figure 1.
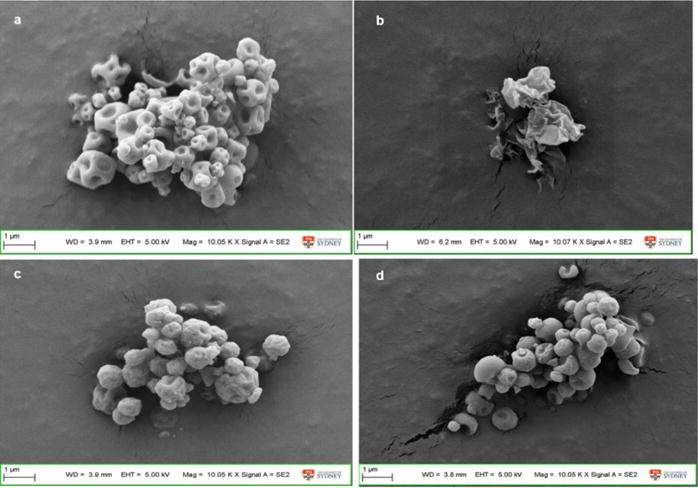
SEM micrographs of spray-dried powder formulations: a) 4COL:1AZI; b) 1COL:1AZI; c) 1COL:4AZI; d) pure AZI.
XRPD data showed crystalline peaks for the supplied pure azithromycin powder (Supplement 1). No crystalline peak was detected for all spray-dried formulations, which indicated that they were substantially amorphous. More importantly, no crystalline peaks were detected for the 1COL:1AZI formulation after storage at RH 75 % and 20 °C for 21 days.
Data from previous studies showed that water absorption of amorphous spray-dried pure colistin powder can be as high as 30 % w/w at high RH up to 90 % (20). In contrast, the water absorption of the spray-dried pure azithromycin formulation was substantially lower with only 6 % of water absorbed at the RH of 90 % (Fig. 2). The water sorption isotherm was decreasing gradually when the colistin ratio in the combination was reduced. For the 1COL:4AZI formulation, the absorbed water was less than 10 % even at the high RH of 80 %. Mass change of all formulations was zero at the end of desorption indicating no moisture-induced re-crystallisation or permanent water absorption occurred.
Figure 2.
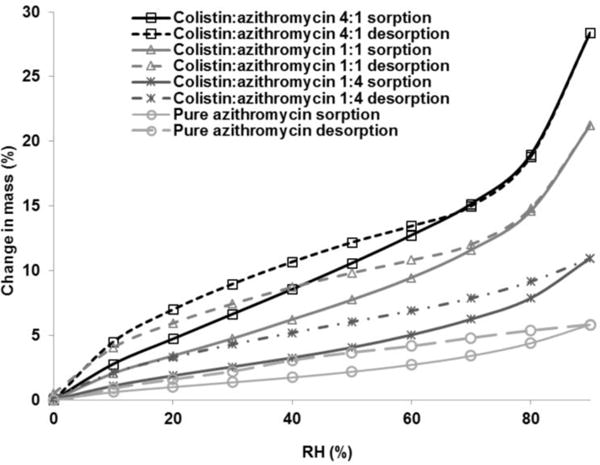
Dynamic water sorption behavior of the composite powder formulations.
Particle Surface Chemistry
XPS
Table 2 compiles the elemental compositions of the two pure drugs, colistin (COL) and azithromycin (AZI), as well as those of the composite formulations, as measured by XPS. The surface composition of the composite formulations qualitatively reflects the changing ratio of the two constituents. Using the measured compositions of two pure compounds, the elemental compositions of the combination formulations can be converted to relative molar fractions of colistin and azithromycin as described in the Materials and Methods section. The resulting estimates are also presented in Table 2 (last two rows).
Table 2.
Elemental composition of colistin (Col), azithromycin (AZI) and the combination formulations, as measured by XPS. Concentrations are expressed as atomic ratios X/C (atomic concentration of element X relative to that of C). Also shown are estimates of molar fractions of colistin and azithromyxin in the combination formulations, based on the elemental composition (last two rows). Mean ± SD, n = 3.
| Pure AZI | 1Col:4AZI | 1Col:1AZI | 4Col:1AZI | Pure Col | |
|---|---|---|---|---|---|
| O/C | 0.299 ± 0.006 | 0.301 ± 0.001 | 0.302 ± 0.002 | 0.334 ± 0.002 | 0.365 ± 0.006 |
| N/C | 0.057 ± 0.001 | 0.060 ± 0.001 | 0.075 ± 0.001 | 0.176 ± 0.000 | 0.285 ± 0.004 |
| S/C | 0.000 ± 0.000 | 0.001 ± 0.000 | 0.004 ± 0.000 | 0.020 ± 0.000 | 0.040 ± 0.001 |
|
| |||||
| Col | 0.0 % | 1.0 % | 3.5 % | 28.0 % | 100.0 % |
| AZI | 100.0 % | 99.0 % | 96.5 % | 72.0 % | 0.0 % |
The relative molar fractions of the two drugs in various formulations were confirmed by employing the second method outlined in the Materials and Methods section, via curve-fitting of high-resolution spectra using model spectra of colistin and azithromycin as fit components, followed by appropriate scaling. Here we presented the C1s data as an example. Supplement 2 shows a C 1s spectrum curve-fitted with model spectra. Supplement 3 lists the resulting estimates of the molar fractions of colistin and azithromycin, which are in good agreement with those calculated in Table 2.
XPS data clearly indicate that azithromycin dominates the surfaces of composite particles comprising 50% w/w AZI and above. In the formulation 1AZI: 1COL, 96.5 % of the surface was azithromycin. Even in the formulation of 4COL:1AZI where AZI represents only 20 % mass of the bulk concentration, its surface fraction was measured as 72.0 %.
ToF-SIMS
The surface sensitivity of ToF-SIMS is even higher than that of XPS, the intensity and distribution of detected species represents their abundance within the top 1–2 nm of the surface. Hence, the data showed enrichment of azithromycin on the outermost particle surfaces with an increase in azithromycin bulk concentration (Fig. 3). For the formulation 4COL:1AZI, signals of azithromycin were apparently more than those of colistin although only 20 %w/w of azithromycin was incorporated in the combination powder. When azithromycin content was increased to 50 %w/w, it overwhelmingly dominated the surface of composite particles. Such coverage of azithromycin on the particle surfaces was near complete when colistin bulk concentration was reduced to 20 %w/w. These findings are consistent with the XPS data revealing the presence of a small proportion of colistin on the combination particle surfaces for all examined formulations.
Figure 3.
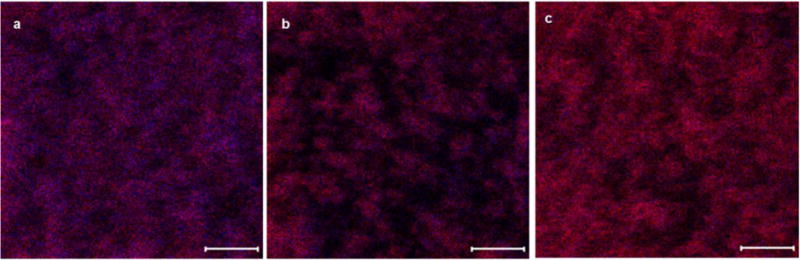
Distribution of colistin (blue) and azithromycin (red) on the surface of composite particles measured by ToF-SIMS: a) colistin:azithromycin 4:1; b) colistin:azithromycin 1:1; c) colistin:azithromycin 1:4 (scale bar represents 10 μm).
In vitro aerosolisation performance at 60 % RH
The aerosol deposition profiles of the combination and pure spray-dried azithromycin powders at two RHs are shown in Fig. 4. The corresponding FPFrecovered and FPFemitted values of colistin and azithromycin obtained from the deposition profiles are summarised in Fig 5 and Fig 6, respectively. Using the data obtained for pure colistin (PURE COL) obtained in previous work (20) as a comparison, the gradual increase of azithromycin in the formulation resulted in a decrease in the FPFrecovered of colistin at 60 % RH (Fig. 5a). The FPFrecovered of colistin decreased from 80.1 % for pure colistin, to 46.7 % for the formulation containing 20 %w/w of colistin (4AZI:1COL). In between these concentrations, the FPFrecovered of colistin varied between 57.0 % and 70.3 %. From the perspective of azithromycin, it appeared that the incorporation of colistin to azithromycin improved the aerosolisation performance of azithromycin at 60 % RH (Fig. 5b). This could be inferred from the increase in FPFrecovered from 55.7 % for pure azithromycin to 71.7 % for the formulation with 10 % w/w azithromycin (1AZI:9COL).
Figure 4.
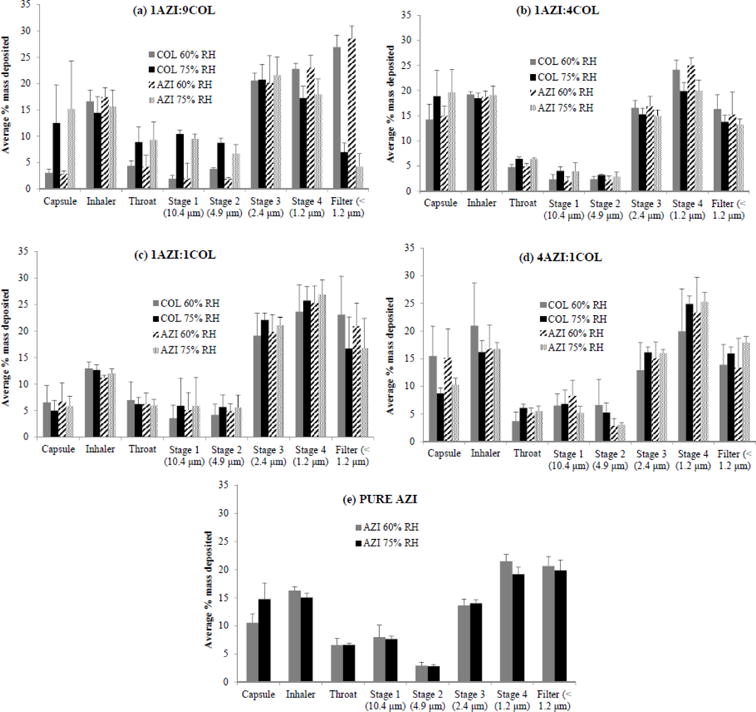
Aerosol deposition profiles of the different formulations of colistin-azithromycin combination powders and pure spray-dried azithromycin at different RHs (mean ± SD, n=4).
Figure 5.
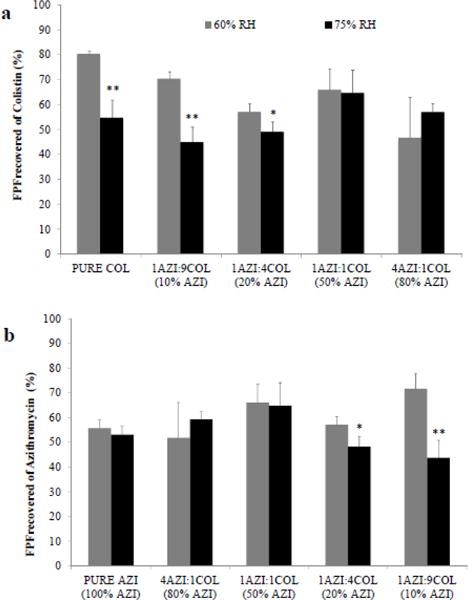
Aerosolisation performance of (a) colistin, and (b) azithromycin from the combination powders as reflected by their FPFrecovered values at different RHs (mean ± SD, n=4; *, p < 0.05; **, p < 0.001).
Figure 6.
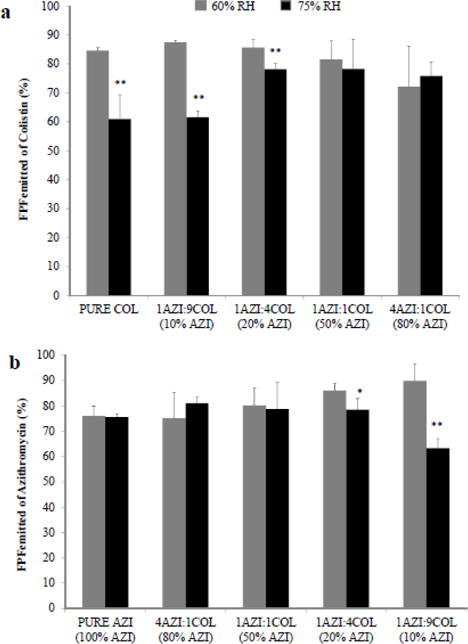
Aerosolisation performance of colistin and azithromycin from the combination powders as reflected by their FPFemitted values at different RHs (mean ± SD, n=4; *, p < 0.05; **, p < 0.001).
Similar trends were also observed in FPFemitted. With an increase in colistin content, the FPFemitted of azithromycin in the combination formulations was improved from 75.2 % for 4AZI:1COL to 90 % for 1AZI:9COL; and the FPFemitted of colistin was increased from 72.1 % for 4AZI:1COL to 87.4 % for 1AZI:9COL.
Effect of Humidity on Aerosolisation
As reported previously (20), the aerosolisation performance of pure spray-dried colistin becomes poorer at the elevated RH of 75 % due to the hygroscopic nature of the drug. In this study, the aerosolisation performance of two formulations containing predominantly colistin, namely, 1AZI:9COL (90 %w/w colistin) and 1AZI:4COL (80 %w/w colistin), were likewise sensitive to the change in relative humidity. This could be inferred from the lower (p < 0.05) FPFrecovered of colistin at 75 % RH compared to 60 % RH for these formulations (Fig. 5a). The disparities in the FPFrecovered of colistin at different RH decreased with increasing azithromycin content in the formulations. When the content of azithromycin was increased to 50 % and 80 %w/w, the FPFrecovered values of colistin at 75 % RH increased and became comparable to those at 60 % RH. For the formulations 1AZI:1COL and 4AZI:1COL, no significant differences (p > 0.05) were observed in the FPFrecovered values of colistin at 60 and 75 % RH. These data suggested that these two formulations were sufficiently robust and capable of withstanding conditions of elevated humidity with minimal compromise on the aerosolisation properties of hygroscopic colistin.
Unlike colistin, the aerosolisation performance of azithromycin, a poorly water-soluble drug, is unaffected by changes in relative humidity. This is evident from Fig. 5b which showed consistent FPFrecovered values for pure spray-dried azithromycin at both 60 and 75 % RH. Formulations with comparatively lower contents of azithromycin, namely, those with 80 %w/w (4AZI:1COL) and 50 %w/w (1AZI:1COL) azithromycin, demonstrated similar resistance to moisture, with no significant differences (p > 0.05) detected in the FPFrecovered of azithromycin at 60 % and 75 % RH. However, when the proportion of azithromycin was further decreased to 20 %w/w and 10 %w/w, the combination powders became sensitive to moisture, with significantly lower (p < 0.05) FPFrecovered values of azithromycin at 75 % RH compared to those at 60 % RH.
The FPFemitted data of combination formulations showed the same trend to those of FPFrecovered. For azithromycin content of 50 %w/w and higher, there were no significant differences in FPFemitted between two RHs. However, the azithromycin content of 20 % w/w and less resulted in significantly lower FPFemitted for 75 % RH. It is also noteworthy that there is no significant difference in FPFrecovered of the 1AZI:1COL formulation between those stored at RHs of 60 % and 75 % for 21 days (p > 0.05).
DISCUSSION
Composite particles for DPI of colistin combinations
Colistin has been used as the last-line antibiotic therapy for many infections caused by multi-drug resistant bacteria; however, mono-drug therapy may lead to the development of drug resistance. Resistance to colistin has been increasingly reported around the world (27). Recently, plasmid-mediated colistin-resistance gene MCR-1 has been found in the bacteria from both animals and humans in many countries (28). There is a fear that colistin-resistance will develop and spread, with no antibiotics being effective against “superbugs” in the near future. One of the practical strategies to combat colistin-resistance is to use combination therapies (27). In the present study, combination formulations have been developed by co-spray drying. Spray drying is a viable and continuous production technique for producing pharmaceutical solids, which has been widely adopted by the pharmaceutical industry (11).
It is noteworthy that the deposition profiles of azithromycin and colistin in each stage of the impinger were almost identical, suggesting that each composite particle comprised both drugs in the designed ratio rather than a physical particle mixture. This hypothesis is also supported by the XPS and ToF-SIM data that > 96 % (molecular fraction) of the composite particle surfaces are covered by azithromycin with an overall drug mass ratio of 1:1 (molecular ratio of 1.9:1) because a physical mixture of two drugs would lead to a 37 % (molecular fraction) of azithromycin on the particle surface of the mixture powder. A potential benefit of such composite particles is that two drugs can deposit on the same infection sites in the airways and act simultaneously, thus, maximising synergistic antimicrobial effects.
Parenteral administration of high-dose colistin can cause dose-limiting severe nephrotoxicity (4). Inhalation therapy of colistin aerosols have shown superior in vivo activity against bacteria in the airways; however, inhalation of high-dose colistin also caused local respiratory irritation and coughing (1). Improving aerosol efficiency of inhaled therapy can significantly reduce the drug dose and minimise the adverse effects. In our studies, we have shown that at moderate RH, the FPFrecovered and FPFemitted of the 1AZI:1COL formulation were relatively high, above 65 % and 80 %, respectively. The superior in vitro aerosol performance may indicate improved clinical performance with a higher lung dose and lower oropharyngeal deposition; this may lead to lower systemic exposure and thus a reduction in the possibility of side effects.
Effects of azithromycin on the surface coating coverage and moisture-induced reduction in aerosolisation
Based on FPFemitted and FPFrecovered, the effects of azithromycin coating on drug aerosolisation at elevated RH is clearly formulation-dependent. It appeared that formulations containing 50 %w/w or higher proportions of azithromycin exhibited similar FPFemitted and FPFrecovered values between 60 and 75 % RH, indicating that aerosolisation is not compromised at a high RH. However, the formulations containing lower contents (20 % and 10 %w/w) of azithromycin exhibited lower FPFs when stored and aerosolised at the 75 % RH compared to those stored at the 60 % RH. These results indicated that overall contents of azithromycin at only 50 % w/w (35 % by molecular fraction) in the combinations is sufficient to protect hygroscopic colistin against moisture-induced deterioration in the aerosolisation properties. This is because hydrophobic azithromycin occupies the particle surface of spray-dried composite powder, supported by the XPS data that the molar fraction of azithromycin on the particle surface of 1:1 formulation was 96.5 % (Table 2). ToF-SIMS images also confirmed that azithromycin signals overwhelmingly dominate the particle surface (Fig 3). During the drying process, water-insoluble azithromycin is abundant on the liquid-vapour interface and precipitates first on the particle surface, which result in a hydrophobic coating layer (14). It is possible that azithromycin content lower than 50 %w/w is sufficient to offer the moisture protection. Future studies are warranted to examine more drug ratios between 1:1 and 4:1 COL:AZI to determine the exact ratio that could prevent moisture-induced reduction in FPF.
Effect of particle size on the aerosolisation performance of the combination powders at 60 % RH
At the outset, it was found that aerosolisation performance of the different formulations at 60 % RH, as reflected by the FPFrecovered of both colistin and azithromycin (Fig. 5), were significantly affected by the composition, which in turn affected the physical size and surface morphology of the spray-dried particles. This is clearly shown in Fig. 7, where distinct linear relationships could be observed between particle sizes (D10, D50 and D90) and FPFrecovered of both drugs at 60 % RH, with increased particle size bringing about a corresponding increase in the FPFrecovered of both colistin and azithromycin. When the size of the spray-dried particles increased, their specific surface area decreased and this minimised the cohesive forces between the particles. Reduced powder cohesiveness improved the fluidisation and dispersion of powder. However, it is noted that both surface roughness and composition may also have influence on surface roughness of the spray-dried particles. In general, with an increase in azithromycin, the particle surface became rougher, with the exception of 1AZI:1COL which had a wrinkled shape. There was a trend that a rougher surface led to higher FPFrecovered (Fig. 5a) because of the reduced contact area (29).
Figure 7.
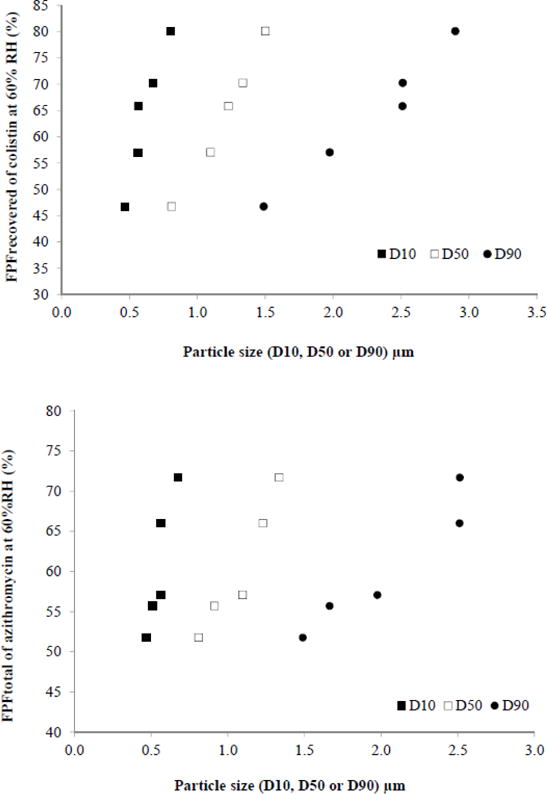
Linear relationships between particle size and FPFrecovered of: (a) colistin and (b) azithromycin in five tested formulations at 60 % RH.
Effect of azithromycin on aerosolisation performance of the composite powders at 75 % RH
No relationships were observed between particle size and FPFrecovered at 75 % RH. This could be related to the moisture-sensitive nature of formulations comprising higher proportions of colistin (1AZI:4COL and 1AZI:9COL). Moisture uptake by colistin at 75 % RH resulted in increased capillary forces between particle surfaces, particularly for the formulation containing the highest content of colistin (90 %w/w colistin in 1AZI:9COL). A previous study by Zhou et al. also reported visible clumping of pure spray-dried colistin stored at 90 % RH (21). The increased capillary forces may diminish the effect of primary particle size on the flow, dispersion and aerosolisation properties of the combination powders at the elevated humidity. The particle sizes of pure spray-dried colistin (previously reported in Zhou et al. (20), D50 = 1.5 μm) and the formulation containing the highest proportion of colistin (D50 = 1.33 μm for 1AZI:9COL) were the largest amongst all formulations investigated (Table 1). Increased capillary forces of these powders at 75 % RH brought about a further increase in their effective size by forming agglomerates, possibly to a range that was not suitable for deposition in the lower respiratory tract (30), as corroborated by the dispersion data. It can be observed from Fig. 4 that for the formulation containing the highest fraction of colistin (1AZI:9COL), the proportion of drug deposited on the capsule, throat, stages 1 and 2 were close to 2-fold higher than those of the other formulations. The proportion of drug deposition at these locations for pure spray-dried colistin was even higher (20).
Instead of particle size, the content of azithromycin of the spray-dried particles appeared to play a greater role in influencing the aerosolisation properties of the two drugs at 75 % RH. As can be seen from Fig. 5, an increase in azithromycin content from 20 to 50 %w/w brought about a significant increase (t-test, p < 0.05) in the FPFrecovered of both drugs from just under 50 % to around 65 %. A further increase in azithromycin content beyond 50 % did not bring about a corresponding increase in the FPFrecovered values (t-test, p > 0.05). These results suggested that the presence of azithromycin at or above 50 %w/w in the combination powders rendered the powders more resistant to the environmental moisture, thereby mitigating its deleterious effects on drug aerosolisation at higher humidity.
CONCLUSIONS
Hygroscopicity is a common undesirable property of many spray-dried amorphous particles (11). Absorption of large amounts of water at the elevated RH by the hygroscopic particles can cause a significantly compromised aerosol performance due to increased inter-particulate capillary forces (31). In our previous studies, we demonstrated that storage of hygroscopic colistin powder at the RH of 75 % led to a significant reduction of approximately 30 % in FPFrecovered. Co-spray drying colistin with another hydrophobic drug at a mass ratio of 1:1 showed the prevention of such deterioration in FPFrecovered through surface coating. However, the key question had not been answered: how much hydrophobic drug in the combination is sufficient to prevent the moisture-induced reduction in the FPF of hygroscopic particles?
In the present study, we examined the effects of drug ratio in the combination on surface coating coverage and moisture-induced change in aerosolisation. XPS and ToF-SIMS data showed that azithromycin occupied 96.5 % of particle surface with only 50 %w/w (35 % by molecular fraction) content in the combination formulation. Surface coating of azithromycin with 50 % of mass content and above was shown to be effective to prevent the moisture-induced decrease in aerosolisation. Such moisture protection was effective for those powders stored at RH of 75 % for at least 21 days. The azithromycin content < 50 % led to an incomplete coating on the surface of composite particles, which is unable to totally prevent the effects of moisture on aerosol performance. The previously developed combination powder formulations of colistin and rifampicin are physically and chemically stable after storage under 20 °C and 60 % RH for one month. In this study the 1COL:1AZI formulation showed physical and chemical stability after storage under a higher RH of 75 % for at least 21 days. The long-term physical and chemical stability tests of the composite formulations produced in the present study are ongoing to confirm the suitability of co-spray drying to develop stable combination powder formulations of colistin and azithromycin. This study has also demonstrated the importance of advanced surface chemistry characterization techniques, such asXPS and ToF-SIMS, in understanding the critical relationship between particle surface chemistry and aerosol performance.
Supplementary Material
Acknowledgments
The authors acknowledge the financial support from the Australian Research Council’s Discovery Project funding scheme (DP120102778) and the National Health and Medical Research Council’s (NHMRC) Project Grant funding scheme (APP1065046). Jian Li is an NHMRC Senior Research Fellow and is funded by grants from the National Institute of Allergy and Infectious Diseases of the National Institutes of Health (R01 AI098771 and AI111965). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Allergy and Infectious Diseases or the National Institutes of Health. The authors are grateful for the scientific and technical assistance, of the Australian Microscopy & Microanalysis Research Facility at the Australian Centre for Microscopy and Microanalysis, The University of Sydney and the Future Industries Institute, University of South Australia.
References
- 1.Velkov T, Nusaibah AR, Zhou Q, Chan H-K, Li J. Inhaled antimicrobial chemotherapy for respiratory tract infections: Successes, challenges and the road ahead. Advanced Drug Delivery Reviews. 2015;85:65–82. doi: 10.1016/j.addr.2015.04.010. [DOI] [PubMed] [Google Scholar]
- 2.Traini D, Young PM. Delivery of antibiotics to the respiratory tract: an update. Expert Opinion on Drug Delivery. 2009;6(9):897–905. doi: 10.1517/17425240903110710. [DOI] [PubMed] [Google Scholar]
- 3.Weers J. Inhaled antimicrobial therapy–Barriers to effective treatment. Advanced Drug Delivery Reviews. 2015;85:24–43. doi: 10.1016/j.addr.2014.08.013. [DOI] [PubMed] [Google Scholar]
- 4.Garonzik SM, Li J, Thamlikitkul V, Paterson DL, Shoham S, Jacob J, et al. Population pharmacokinetics of colistin methanesulfonate and formed colistin in critically ill patients from a multicenter study provide dosing suggestions for various categories of patients. Antimicrob Agents Chemother. 2011;55(7):3284–94. doi: 10.1128/AAC.01733-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schuster A, Haliburn C, Döring G, Goldman MH, Group ftFS Safety, efficacy and convenience of colistimethate sodium dry powder for inhalation (Colobreathe DPI) in patients with cystic fibrosis: a randomised study. Thorax. 2013;68(4):344–50. doi: 10.1136/thoraxjnl-2012-202059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhou Q, Leung SSY, Tang P, Thaigarajan P, Loh Z, Chan HK. Inhalation formulation and drug delivery systems for respiratory infections. Advanced Drug Delivery Reviews. 2015;85:83–99. doi: 10.1016/j.addr.2014.10.022. [DOI] [PubMed] [Google Scholar]
- 7.Cipolla D, Blanchard J, Gonda I. Development of Liposomal Ciprofloxacin to Treat Lung Infections. Pharmaceutics. 2016;8(1):6. doi: 10.3390/pharmaceutics8010006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yapa S WS, Li J, Patel K, Wilson JW, Dooley MJ, George J, et al. Pulmonary and systemic pharmacokinetics of inhaled and intravenous colistin methanesulfonate in cystic fibrosis patients: targeting advantage of inhalational administration. Antimicrob Agents Chemother. 2014;58(5):2570–9. doi: 10.1128/AAC.01705-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhou QT, Tang P, Leung SSY, Chan JGY, Chan H-K. Emerging inhalation aerosol devices and strategies: Where are we headed? Advanced Drug Delivery Reviews. 2014;75:3–17. doi: 10.1016/j.addr.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 10.Cipolla D, Froehlich J, Gonda I. Comment on: Inhaled antimicrobial therapy—Barriers to effective treatment, by J. Weers, Inhaled antimicrobial therapy — Barriers to effective treatment. Advanced Drug Delivery Reviews. 2015;85:e6–e7. doi: 10.1016/j.addr.2015.04.015. [DOI] [PubMed] [Google Scholar]
- 11.Lin Y-W, Wong J, Qu L, Chan H-K, Zhou QT. Powder production and particle engineering for dry powder inhaler formulations. Current Pharmaceutical Design. 2015;21(40):5802–14. doi: 10.2174/1381612821666150820111134. [DOI] [PubMed] [Google Scholar]
- 12.Marriott C, Frijlink HW. Lactose as a carrier for inhalation products: breathing new life into an old carrier. Advanced Drug Delivery Reviews. 2012;64(3):217–9. doi: 10.1016/j.addr.2011.11.003. [DOI] [PubMed] [Google Scholar]
- 13.de Boer AH, Chan HK, Price R. A critical view on lactose-based drug formulation and device studies for dry powder inhalation: Which are relevant and what interactions to expect? Advanced Drug Delivery Reviews. 2012;64(3):257–74. doi: 10.1016/j.addr.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 14.Vehring R. Pharmaceutical particle engineering via spray drying. Pharmaceutical Research. 2008;25(5):999–1022. doi: 10.1007/s11095-007-9475-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sou T, Kaminskas LM, Nguyen TH, Carlberg R, McIntosh MP, Morton DAV. The effect of amino acid excipients on morphology and solid-state properties of multi-component spray-dried formulations for pulmonary delivery of biomacromolecules. European Journal of Pharmaceutics and Biopharmaceutics. 2013;83(2):234–43. doi: 10.1016/j.ejpb.2012.10.015. [DOI] [PubMed] [Google Scholar]
- 16.Sou T, Orlando L, McIntosh MP, Kaminskas LM, Morton DAV. Investigating the interactions of amino acid components on a mannitol-based spray-dried powder formulation for pulmonary delivery: A design of experiment approach. International Journal of Pharmaceutics. 2011;421(2):220–9. doi: 10.1016/j.ijpharm.2011.09.018. [DOI] [PubMed] [Google Scholar]
- 17.Haynes A, Nakamura J, Heng C, Heuerding S, Thompson G, Malcolmson R. Aerosol performance of tobramycin inhalation powder. Respiratory Drug Delivery. 2010:701–6. [Google Scholar]
- 18.Edwards DA, Hanes J, Caponetti G, Hrkach J, Ben-Jebria A, Eskew ML, et al. Large Porous Particles for Pulmonary Drug Delivery. Science. 1997;276(5320):1868–72. doi: 10.1126/science.276.5320.1868. [DOI] [PubMed] [Google Scholar]
- 19.Adi H, Young PM, Chan H-K, Agus H, Traini D. Co-spray-dried mannitol–ciprofloxacin dry powder inhaler formulation for cystic fibrosis and chronic obstructive pulmonary disease. European Journal of Pharmaceutical Sciences. 2010;40(3):239–47. doi: 10.1016/j.ejps.2010.03.020. [DOI] [PubMed] [Google Scholar]
- 20.Zhou Q, Morton D, Yu HH, Jacob J, Wang JP, Li J, et al. Colistin powders with high aerosolisation efficiency for respiratory infection: preparation and in vitro evaluation. Journal of Pharmaceutical Sciences. 2013;102(10):3736–47. doi: 10.1002/jps.23685. [DOI] [PubMed] [Google Scholar]
- 21.Zhou Q, Gengenbach T, Denman JA, Yu HH, Li J, Chan HK. Synergistic Antibiotic Combination Powders of Colistin and Rifampicin Provide High Aerosolization Efficiency and Moisture Protection. AAPS Journal. 2014;16(1):37–47. doi: 10.1208/s12248-013-9537-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nageeb W, Metwally L, Kamel M, Zakaria S. In vitro antimicrobial synergy studies of carbapenem-resistant Acinetobacter baumannii isolated from intensive care units of a tertiary care hospital in Egypt. Journal of Infection and Public Health. 2015;8(6):593–602. doi: 10.1016/j.jiph.2015.05.007. [DOI] [PubMed] [Google Scholar]
- 23.Lin L, Nonejuie P, Munguia J, Hollands A, Olson J, Dam Q, et al. Azithromycin Synergizes with Cationic Antimicrobial Peptides to Exert Bactericidal and Therapeutic Activity Against Highly Multidrug-Resistant Gram-Negative Bacterial Pathogens. Ebiomedicine. 2015;2(7):690–8. doi: 10.1016/j.ebiom.2015.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhou QT, Denman JA, Gengenbach T, Das S, Qu L, Zhang H, et al. Characterization of the surface properties of a model pharmaceutical fine powder modified with a pharmaceutical lubricant to improve flow via a mechanical dry coating approach. Journal of Pharmaceutical Sciences. 2011;100(8):3421–30. doi: 10.1002/jps.22547. [DOI] [PubMed] [Google Scholar]
- 25.Beamson G, Briggs D. High Resolution XPS of Organic Polymers. 1st. Chichester: John Wiley & Sons; 1992. [Google Scholar]
- 26.Wallace SJ, Nation RL, Li J, Boyd BJ. Physicochemical aspects of the coformulation of colistin and azithromycin using liposomes for combination antibiotic therapies. Journal of pharmaceutical sciences. 2013;102(5):1578–87. doi: 10.1002/jps.23508. [DOI] [PubMed] [Google Scholar]
- 27.Cai Y, Chai D, Wang R, Liang BB, Bai N. Colistin resistance of Acinetobacter baumannii: clinical reports, mechanisms and antimicrobial strategies. Journal of Antimicrobial Chemotherapy. 2012;67(7):1607–15. doi: 10.1093/jac/dks084. [DOI] [PubMed] [Google Scholar]
- 28.Paterson DL, Harris PNA. Colistin resistance: a major breach in our last line of defence. The Lancet Infectious Diseases. 2016;16(2):132–3. doi: 10.1016/S1473-3099(15)00463-6. [DOI] [PubMed] [Google Scholar]
- 29.Chew NY, Tang P, Chan H-K, Raper JA. How much particle surface corrugation is sufficient to improve aerosol performance of powders? Pharmaceutical Research. 2005;22(1):148–52. doi: 10.1007/s11095-004-9020-4. [DOI] [PubMed] [Google Scholar]
- 30.Price R, Young PM, Edge S, Staniforth JN. The influence of relative humidity on particulate interactions in carrier-based dry powder inhaler formulations. International Journal of Pharmaceutics. 2002;246(1–2):47–59. doi: 10.1016/s0378-5173(02)00359-9. [DOI] [PubMed] [Google Scholar]
- 31.Zhu K, Tan RB, Ng WK, Shen S, Zhou Q, Heng PW. Analysis of the influence of relative humidity on the moisture sorption of particles and the aerosolization process in a dry powder inhaler. Journal of Aerosol Science. 2008;39(6):510–24. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


