Abstract
The molecular signaling mechanisms between glomerular cell types during initiation/progression of diabetic kidney disease (DKD) remain poorly understood. We compared the early transcriptome profile between DKD-resistant C57BL/6J and DKD-susceptible DBA/2J (D2) glomeruli and demonstrated a significant downregulation of essential mitochondrial genes in glomeruli from diabetic D2 mice, but not in C57BL/6J, with comparable hyperglycemia. Diabetic D2 mice manifested increased mitochondrial DNA lesions (8-oxoguanine) exclusively localized to glomerular endothelial cells after 3 weeks of diabetes, and these accumulated over time in addition to increased urine secretion of 8-oxo-deoxyguanosine. Detailed assessment of glomerular capillaries from diabetic D2 mice demonstrated early signs of endothelial injury and loss of fenestrae. Glomerular endothelial mitochondrial dysfunction was associated with increased glomerular endothelin-1 receptor type A (Ednra) expression and increased circulating endothelin-1 (Edn1). Selective Ednra blockade or mitochondrial-targeted reactive oxygen species scavenging prevented mitochondrial oxidative stress of endothelial cells and ameliorated diabetes-induced endothelial injury, podocyte loss, albuminuria, and glomerulosclerosis. In human DKD, increased urine 8-oxo-deoxyguanosine was associated with rapid DKD progression, and biopsies from patients with DKD showed increased mitochondrial DNA damage associated with glomerular endothelial EDNRA expression. Our studies show that DKD susceptibility was linked to mitochondrial dysfunction, mediated largely by Edn1–Ednra in glomerular endothelial cells representing an early event in DKD progression, and suggest that cross talk between glomerular endothelial injury and podocytes leads to defects and depletion, albuminuria, and glomerulosclerosis.
Introduction
Diabetic kidney disease (DKD) is the leading cause of end-stage kidney failure in the U.S. and is increasing in prevalence at an alarming rate worldwide (1). The pathogenesis of DKD is complex, as it implicates genetics and the environment. Although some patients with type 1 diabetes (T1D) develop DKD after 20 years of disease, the majority do not, despite similar levels of hyperglycemia, suggesting important genetic predisposition (2). Differential susceptibilities to DKD have also been observed in well-defined strains of inbred mice (3,4). However, the underlying molecular and genetic components that contribute to differential susceptibilities to DKD are still poorly understood in both patients with diabetes and diabetic rodent models.
Diabetes induces lesions in glomeruli characterized by mesangial expansion and podocyte loss, among others. Loss of podocytes is a strong predictor of glomerular progression of DKD in patients with diabetes (5) and murine models of diabetes (6). Interestingly, in models of glomerulosclerosis and in human DKD, endothelial dysfunction has been recently recognized to play a critical role in the development and progression of glomerular disease (7,8). Glomerular endothelial cells are highly specialized cells with fenestrae and a luminal glycocalyx layer (9,10), which contribute to the filtration barrier (11). Although the mechanisms and manifestations of glomerular endothelial cell injury in diabetes remain poorly understood, we recently showed that in models of primary podocyte–restricted injury, glomerular endothelial cells manifest mitochondrial oxidative stress (mtStress) associated with endothelial dysfunction, which preceded and was essential for subsequent podocyte apoptosis and loss (12). These results suggest a previously unrecognized role for bidirectional podocyte–endothelial cell cross talk in the evolution of nondiabetic glomerulosclerosis (12). In nephrotic syndrome, mitochondrial respiratory chain abnormalities in kidneys have been previously described (13), and in diabetic microvascular complications, including DKD, reactive oxygen species (ROS) (14) and mitochondrial dysfunction could play critical roles in the pathogenesis (15,16) by way of increasing mitochondrial superoxide production consequent to hyperglycemia and damaging mitochondrial DNA (mtDNA), proteins, and activation of apoptotic pathways (17). Podocyte detachment and diminished endothelial cell fenestration promote development and progression of kidney disease in patients with type 2 diabetes (T2D) (18). Endothelial nitric oxide synthetase deficiency accelerates and exacerbates glomerular lesions (19) and podocyte injury (20) in experimental DKD. In addition, podocyte injury was more severe in diabetic mice with loss of function of the endothelial survival factor Krüppel-like factor 2 (21). These observations suggest that cross talk between injured endothelial cells and podocytes contributes to susceptibility of diabetic glomerular lesions and progression.
In this study, we examined DKD in a susceptible and resistant mouse strain and demonstrate that diabetes induces mtStress largely mediated by endothelin-1 (Edn1)/endothelin-1 receptor type A (Ednra) signaling in endothelial cells and causes endothelial injury, which was required for podocyte depletion in DKD-susceptible mice but not in resistant mice, despite similar levels of hyperglycemia. Furthermore, we observed increased mtDNA oxidative damage associated with glomerular endothelial EDNRA expression in biopsies from patients with DKD, and increased urine 8-oxo-deoxyguanosine (8-oxodG) was associated with rapid progression of DKD.
Research Design and Methods
Animal Studies
Eight-week-old inbred DBA/2J (D2) and C57BL/6J (B6) mice (The Jackson Laboratory) received low-dose streptozotocin (STZ; 50 mg/kg in 0.1 mol/L sodium citrate buffer [pH 4.5]) injections intraperitoneally for 5 consecutive days. Eight-week-old male C57BL/6-Ins2Akita/J (Akita-B6) and D2.B6-Ins2Akita/J (Akita-D2; The Jackson Laboratory) were crossed with female wild-type mice, and F1 generation offspring were studied. The onset and extent of diabetes was evaluated by 4–6-h fasting blood glucose (FBG) using blood glucose strips (Ascensia Contour; Bayer). Hyperglycemia was considered when FBG >200 mg/dL. A total of 1 mg/kg/d MitoTEMPO (Enzo Life Sciences International), 0.1 ng/kg/d BQ-123 (Sigma-Aldrich), or saline was delivered by subcutaneous miniosmotic pumps (model 2002; ALZET, Palo Alto, CA). All animal protocols were approved by the Institutional Animal Care and Use Committee at the Icahn School of Medicine at Mount Sinai.
Albuminuria Measurement
Metabolic cages were used to collect 24-h urine from mice. Urinary albumin-to-creatinine ratio (ACR) was measured using mouse albumin-specific ELISA and creatinine companion kits (Exocell Inc., Philadelphia, PA).
Cell Culture
Conditionally immortalized murine glomerular endothelial cells (mGECs) were maintained in RPMI 1640 containing 10% FCS under either permissive (33°C with interferon-γ, 10 units/mL) or nonpermissive conditions (37°C without interferon-γ). mGECs were grown with normal glucose (5 mmol) plus d-mannitol (25 mmol) or with high glucose (hGluc; 30 mmol D-glucose).
Microscopy
Periodic acid-Schiff (PAS) and picrosirius red were performed on paraffin-embedded kidney sections using standard protocols and analyzed under brightfield or polarizing light microscopy for picrosirius red–stained sections.
Gomori methenamine silver staining was performed on paraffin sections using an Accustain silverstain kit (Sigma-Aldrich). Glomerular regions were manually traced, and the area of silver staining positive area (SPA) was defined by a same threshold across all images using MetaMorph software (Molecular Devices).
Immunofluorescence was performed with frozen 4-μm sections of kidneys incubated with anti–8-oxoguanine (8-oxoG) monoclonal antibody (N45.1; Japan Institute for the Control of Aging) as previously described (22) along with goat antisynaptopodin, rabbit anti–Wilms tumor-1 (WT-1), rabbit anti-Ednra, goat anti–TFAM (Santa Cruz Biotechnology), or rat monoclonal anti-CD31 (MEC 7.46; Abcam). The antigen–antibody complexes were visualized with Alexa Fluor secondary antibodies. MitoTracker Red CMXRos (Thermo Fisher Scientific) to visualize mitochondrial networks in cells (23). Images were taken with an Axioplan2 (Carl Zeiss) equipped with a MicroPublisher 3.3 RTV color camera (Qimaging) running QED capture software (MediaCybernetics).
Superresolution was performed on an LSM 880 with Airyscan microscope using Zeiss Zen Black software (Carl Zeiss).
Scanning electron microscopy was performed using 1-mm3 kidney cortex cubes fixed in Karnovsky fixative and mounted in 5% agar noble. Samples were fixed in 1% of osmium tetroxid in 0.1 mol sodium cacodylate, treated with 1% thiocarbohydrazide, then dehydrated, and dried. Sections were mounted on aluminum pins with carbon tabs and coated with palladium. Endothelial morphology index (EMI) was scored in a blinded fashion from open vessels in glomeruli captured at ×10,000 magnification using a 0–3 graded scale: 0, normal endothelial pattern with fenestrations and no visible irregularities; 1, vessels with partly disrupted pattern of endothelial fenestrations in 10–30% of area; 2, vessels containing few visible fenestrations, 30–70% of area; and 3, no endothelial fenestrations present and irregular protrusions.
Oxygen Consumption
mGECs or glomeruli from mice with 1, 7, and 21 days of diabetes were isolated as described in Shi et al. (24). The glomerular fractions were plated in collagen I–coated XF 24-well microplates (Seahorse Bioscience, North Billerica, MA) in DMEM-F12 medium and incubated at 37°C with 5% CO2 overnight. Oxygen consumption rate (OCR) and extracellular acidification rate were analyzed with the XF 24 Extracellular Flux Analyzer (Seahorse Bioscience) in basal conditions and after injections of 1 µmol carbonyl cyanide 4-(trifluoromethoxy) phenylhydrazone (FCCP). Reserve OCR was calculated as the ratio between maximal OCR (FCCP) and average of three baseline OCR measurements (25) to give a reliable and unbiased comparison among highly variable samples.
Quantitative PCR
RT-PCR
Total RNA was prepared from glomeruli and cell lysates using RNeasy mini columns (Qiagen) and then reverse transcribed with SuperScript-II reverse transcriptase (Invitrogen). cDNA amplification was performed in an ABI Prism 7900HYT Sequence Detection System (Thermo Fisher Scientific) and evaluated using SDS 2.0 software (Applied Biosystems). Normalization was to the β-actin gene.
Lesion Frequency: Long Quantitative PCR
Total DNA was extracted using DNeasy mini columns (Qiagen). DNA lesion frequencies were calculated as described previously (26).
Urine 8-oxodG
High-Performance Liquid Chromatography
In mice, urine 8-oxodG was measured by electrochemical detection (27) using a Waters amperometric detector with a glassy-carbon working electrode and Ag/AgCl reference electrode (Waters Corp.). The oxidation potential was 0.4 V. Levels of 8-oxodG were expressed relative to urine creatinine.
ELISA
Human urine 8-oxodG was measured using HT 8-oxodG ELISA Kit (Trevigen) as per the manufacturer’s protocol, and levels were expressed relative to urine creatinine.
Endothelin-1 Assay
Endothelin-1 was determined by enzyme immunosorbent assay Kit (Cayman Chemical) with a VICTOR3 V Multilabel Counter (PerkinElmer), 450 nm in serum and the culture media.
Flow Cytometry
Mitochondrial ROS was measured in cells by MitoSOX (Invitrogen) as per the manufacturer’s instructions.
Cell surface expression was performed as previously described (12) using anti-EDNRA antibody (Santa Cruz Biotechnology) with FITC-conjugated anti-rabbit antibody (Molecular Probes).
Human Renal Biopsies
Deidentified archival frozen human renal biopsy samples of 6 control subjects with no pathological alterations and 14 with mild to advanced DKD were obtained from Dr. Vivette D’Agati (Columbia University), with approval of the local ethics committee. Patient information is provided in Supplementary Table 3.
Statistics
Differences among data groups were evaluated for significance using an independent t test, one-way ANOVA with Tukey posttest to compare control and treatment groups, or two-way ANOVA to examine gene expression of different strains, diabetes, and their interaction over time (Prism 7; GraphPad Software). Data were considered statistically significant when P < 0.05. Correlation analysis was measured by Pearson product-moment correlation coefficient.
Results
Mesangial Expansion and Podocyte Depletion in T1D Are Controlled by Genetic Susceptibility
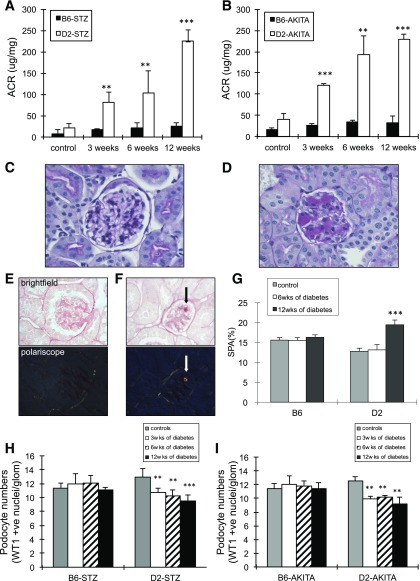
We subjected DKD-resistant B6 mice and DKD-susceptible D2 inbred mice to STZ treatment to induce T1D using protocols established by the Animal Models of Diabetic Complications Consortium (http://www.diacomp.org) (4,28). We also used Akita-B6 and Akita-D2, a genetic model of experimental T1D (4,28). Body weight and 4–6-h FBG were monitored weekly. In both STZ and Akita models, diabetic B6 and D2 mice exhibited significantly lower body weight compared with nondiabetic control mice (Supplementary Fig. 1A and B). Hyperglycemia was comparable between diabetic B6 and D2 mice in both models (Supplementary Fig. 1C and D). Consistent with previous reports (4), urinary albumin excretion rate (Fig. 1A and B) increased progressively during 12 weeks of persistent hyperglycemia in D2 STZ or Akita D2 mice, but not in B6 STZ or Akita mice. Diabetic D2 mice had increased mesangial matrix deposition (Fig. 1D), and picrosirius red staining demonstrated an increase in collagen deposition in 12-week diabetic D2 mice (Fig. 1F) with birefringence, in contrast to 12-week diabetic B6 mice, which show no matrix collagen deposits (Fig. 1C and E). A 52% increase in mesangial extracellular matrix components as determined by SPA score was observed in glomeruli of D2 mice with 12 weeks of diabetes, compared with diabetic B6 and nondiabetic controls (Fig. 1G). Podocytes number was assessed by counting double-positive nuclei for podocyte-specific nuclear marker WT-1 and DAPI in glomerular cross section as previously described (6,12). Compared with nondiabetic age-matched controls, podocyte number decreased significantly after 3 weeks of hyperglycemia in STZ-treated or Akita diabetic D2, but not in diabetic B6 mice (Fig. 1H and I). By 12 weeks of diabetes, podocytes per glomerular section were significantly decreased by 26.8% in STZ-treated and 26.7% in Akita D2 mice (Fig. 1H and I); in contrast, podocyte numbers remained unchanged in diabetic B6 mice. These results suggest that characteristic glomerular lesion development, including podocyte depletion in T1D, is primarily controlled by genetic susceptibility in mice exposed to comparable hyperglycemic levels.
Figure 1.
Diabetes-induced podocyte loss with progressive glomerular disease in D2 mice, not B6. ACR of control and STZ-treated B6 or D2 mice (A) and B6 Akita or D2 Akita mice (B) after 3, 6, and 12 weeks of diabetes (n = 6, ± SEM). Histopathology stain (PAS) of STZ-B6 (C) and STZ-D2 mice (D) after 12 weeks of diabetes (×40 magnification). Note the presence of sclerotic lesions (fibrosis and capillary loop destruction) in D. Picrosirius red staining for matrix deposits in 12-week diabetic B6 (E) and diabetic D2 (F) by brightfield (top) and polariscope (bottom). Arrows indicate large collagen fibers that showed yellow and orange birefringence under polarizing microscopy. G: Percentage glomerular methenamine SPA per glomerular section in control and 6 and 12 weeks of STZ-induced diabetes in B6 and D2 mice (SD). Podocyte number (WT-1–positive cells) per glomerular section in control and STZ-treated B6 or D2 mice (H) and B6 Akita or D2 Akita mice (I) after 3, 6, and 12 weeks of diabetes (mean ± SEM; >50 glomerular profiles/mouse, >5 mice per time point). **P < 0.01; ***P < 0.01.
Mitochondrial Dysfunction and Oxidized mtDNA in Glomerular Endothelial Cells Are Associated With Diabetes-Induced Podocyte Depletion in DKD-Susceptible DBA/2J Mice
We analyzed genome-wide gene expression profiles of glomeruli isolated from nondiabetic control or STZ-treated B6 and D2 mice with 3 and 6 weeks of hyperglycemia using the 430 2.0 mouse genome Gene Chip platform (Affymetrix). Comparing nondiabetic D2 and B6 mice, a total of 2,997 genes was expressed significantly different at baseline, representing inbred strain differences of glomerular gene expression profiling among them. The abundance of 16 and 9 transcripts was significantly different after 3 and 6 weeks of hyperglycemia, respectively, in glomeruli of B6 mice compared with nondiabetic B6 mice. In contrast, in D2 mice, a total of 273 (including 225 upregulated and 48 downregulated) and 1,140 transcripts (including 357 upregulated and 783 downregulated genes) were differentially expressed in glomeruli of diabetic D2 mice, compared with nondiabetic D2 mice, at 3 and 6 weeks of diabetes, respectively. Among differentially expressed transcripts in diabetic D2 mice, genes with well-established functional roles in oxidative phosphorylation and “mitochondrial dysfunction” were most significantly enriched by consistent downregulation (Supplementary Table 1). Supplementary Table 2 shows the main mitochondrial genes and pathways affected. Expression level of antioxidants were downregulated in diabetic D2 mice, including superoxide dismutase (SOD) 2, catalase, and peroxiredoxin 3, suggesting an imbalance of oxidant and antioxidant systems in glomeruli of these mice, contributing to increased oxidative stress (29).
Mitochondrial dysfunction and oxidative stress have been linked to DKD (15–17); we show a significant downregulation of selected respiratory chain complex genes and the mitochondrial SOD2 gene at 3 and 6 weeks of hyperglycemia in glomeruli of D2 mice in Supplementary Fig. 2. Interestingly, SOD1 and SOD3 were differentially regulated among strains only at baseline. This difference could be linked to strain susceptibility, contrary to previous reports (30); our study shows that only mitochondrial SOD2 expression levels were significantly decreased in D2 diabetic mice. Except for SOD2, our data show that some transcripts were also significantly decreased after 6 weeks of diabetes in B6 mice, resulting in loss of interaction response (data not shown), suggesting a possible earlier response by D2 mice with sustained ROS generation and possible accumulation of ROS damage and mitochondrial dysfunction.
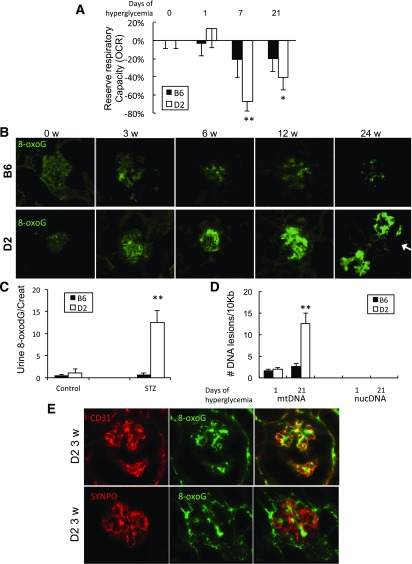
To explore whether diabetes caused impaired mitochondrial function, we assessed glomerular mitochondrial OCR. Mitochondrial respiratory reserve capacity (maximal OCR over baseline OCR) was significantly reduced in STZ-treated D2 mice 7 and 21 days after onset of hyperglycemia compared with control mice (day 0) or to 1 day of hyperglycemia (Fig. 2A). In contrast, reserve respiratory capacity was not significantly different from nondiabetic controls after 1, 7, and 21 days of diabetes in B6 mice (Fig. 2A).
Figure 2.
Decreased mitochondrial function and increased mtDNA damage in glomeruli of diabetic D2 mice. A: Mitochondrial respiratory reserve capacity was measured by OCR (OCR uncoupled respiration [FCCP] over basal respiration) of isolated glomeruli from B6 and D2 controls, STZ-B6, and STZ-D2 mice with diabetes for the days indicated (values are mean percentage reduction in OCR ± SEM; n > 6 mice/time point). B: Immunofluorescent detection of oxidative DNA marker 8-oxoG in glomeruli from B6 (top) and D2 mice (bottom) with 3, 6, 12, and 24 weeks of STZ-induced diabetes and untreated control mice 0 weeks. Arrow indicates 8-oxoG–positive staining in tubular cells. C: Urine 8-oxodG (nmol) relative to urine creatinine (Creat) in B6 and D2 control mice and 3-week diabetic STZ-B6 or STZ-D2 mice. D: Quantification of lesion frequencies in mtDNA and nuclear DNA (nucDNA) by quantitative PCR in isolated glomeruli of B6 and D2 mice after 1 and 21 days of hyperglycemia (n = 6; ±SEM) relative amplification normalized to nondamaged (0 days controls). E: Representative images of double immunofluorescence staining detecting endothelial cell marker CD31 (red, top left), 8-oxoG (green, top middle), and merge (top right) or podocyte marker synaptopodin (SYNPO; red, bottom left), 8-oxoG (green, bottom middle), and merge (bottom right) in glomeruli of 3-week diabetic STZ-D2 mouse. *P < 0.05, **P < 0.01 versus untreated control mice.
Accumulation of oxidative mtDNA lesions is associated with oxidative stress and mitochondrial dysfunction (31). Immunofluorescence labeling of 8-oxoG, a marker for common DNA modification resulting from ROS (32), increased strikingly in glomeruli of D2 mice, but not B6 mice, during 3, 6, and 12 weeks of STZ-induced diabetes (Fig. 2B). Increased glomerular 8-oxoG labeling was associated with increased urinary 8-oxodG detected only in diabetic D2 mice (Fig. 2C). Quantitative analysis of oxidative DNA lesions by quantitative PCR demonstrated a significant accumulation of mtDNA, not nuclear, lesions in glomeruli of 3-week diabetic D2 mice, whereas no lesions were detectable in mtDNA or nuclear DNA of diabetic B6 mice (Fig. 2D).
Seeing as mtStress and dysfunction were characteristic of DKD in mice with a susceptible genetic background, we next determined which glomerular cell types sustain mitochondrial dysfunction and oxidative mtDNA damage. We stained kidney sections for the oxidative DNA marker 8-oxoG together with cell type–specific markers. 8-oxoG–positive staining in diabetic D2 mice was colocalized with the endothelial cell marker CD31 (Fig. 2E, top), but not with the podocyte marker synaptopodin (Fig. 2E, bottom), indicating that diabetes-induced mitochondrial oxidative damage occurs in glomerular endothelial cells of DKD-susceptible D2 mice.
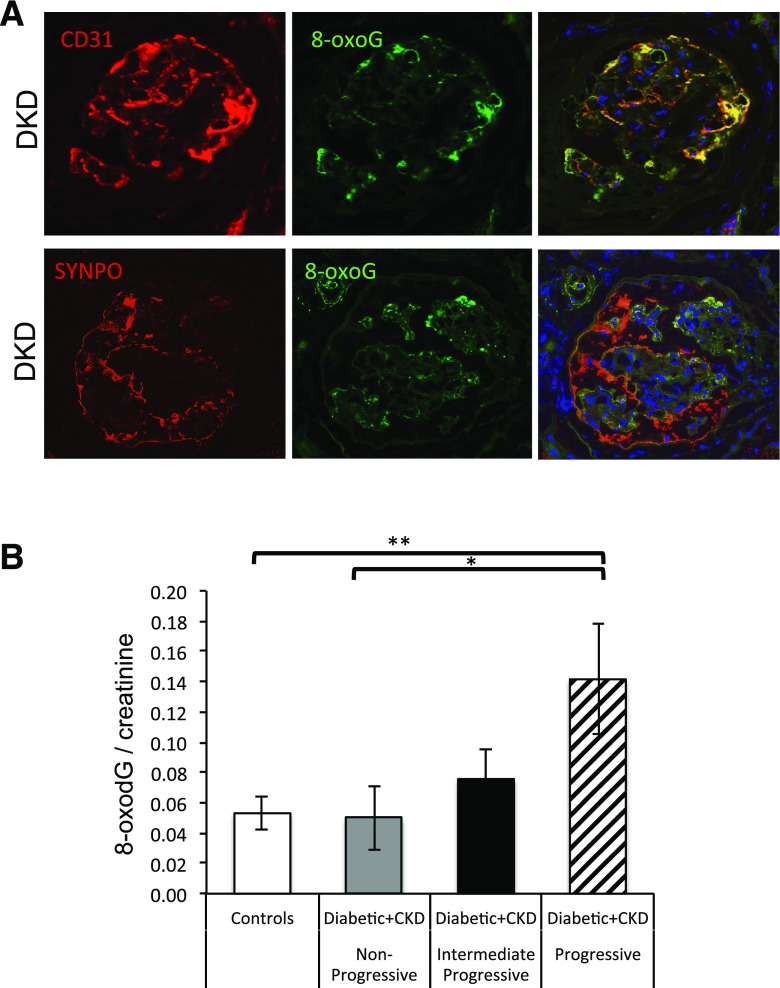
mtStress Is Associated With Injury of Glomerular Endothelial Cells in Patients With Progressive DKD
We examined 8-oxoG labeling in archival kidney biopsies of patients with diabetes with and without kidney disease. Accumulation of 8-oxoG was detectable in CD31-positive glomerular endothelial cells, but not in synaptopodin-positive podocytes of case subjects with moderate-to-severe or advanced histopathology of DKD (Fig. 3A and Supplementary Table 3). In contrast, 8-oxoG was not detectable in glomeruli of kidney biopsies from patients with diabetes without clinical or histopathological evidence for DKD (not shown).
Figure 3.
Diabetes induced mtStress specifically in glomerular endothelial cells. A: Double immunofluorescence staining detecting CD31 (red, top left), 8-oxoG (green, top middle), synaptopodin (SYNPO; red, bottom left), 8-oxoG (green, bottom middle), and merge (top and bottom right) in kidney biopsy from a subject diagnosed with DKD (patient groups in Supplementary Table 2). B: Urine 8-oxodG (nmol) relative to urine creatinine in human control subjects and patients with diabetes with nonprogressive, intermediate progressive, and rapid progressive DKD (Table 1). One-way ANOVA with Tukey posttest was used to compare control patients to patients with progressive, intermediate, and nonprogressive disease. *P < 0.05, **P < 0.01 vs. control subjects. CKD, chronic kidney disease.
In a different cohort, urinary 8-oxodG to creatinine ratio was measured in patients with diabetes with: 1) normal kidney function (control); 2) nonprogressive DKD (Δ estimated glomerular filtration rate [eGFR] <1 mL/min/1.73 m2/year) with mild proteinuria; 3) moderate progressive (ΔeGFR 1–4 mL/min/1.73 m2/year); or 4) progressive DKD (ΔeGFR higher than −4 mL/min/1.73 m2/year) with moderate proteinuria. Detailed clinical and laboratory data for each group are summarized in Table 1. Urinary 8-oxoG/creatinine was comparable between control and case subjects with nonprogressive DKD. In contrast, urine 8-oxodG levels were significantly increased in rapid progressive DKD and showed a trend to increased levels in moderate/intermediate progressive DKD (Fig. 3B). From this small cohort, we cannot attribute all secreted 8-oxodG to glomeruli, as these may come from other regions of the kidney, with oxidative DNA damage affected by diabetes or increased proteinuria. Even so, these results indicate that increased urinary excretion of oxidative DNA damage adducts may be characteristic for DKD with progressive loss of kidney function and proteinuria.
Table 1.
Human case characterization
| Patient characteristics | Control subjects | ΔeGFR <1 | ΔeGFR 1–4 | ΔeGFR >4 |
|---|---|---|---|---|
| N (total 71) | 22 | 14 | 23 | 12 |
| Age (years), mean (SEM) | 54.8 (3.9) | 65.9 (3.7) | 68.3 (2.2) | 63.8 (4.5) |
| Women (%) | 45 | 57 | 52 | 58 |
| Men (%) | 55 | 43 | 48 | 42 |
| Urine protein:creatinine (mg/mg), mean (SEM) | 0.073 (0.01) | 0.309 (0.17) | 1.327 (0.53) | 2.801 (1.13) |
| eGFR (SEM) | 116.4 (14.8) | 51.7 (4.9) | 46.3 (3.7) | 39.3 (3.6) |
Pharmacological Inhibition of mtStress Ameliorates Endothelial Cell Injury, Podocyte Depletion, and Glomerular Histopathology in DKD-Susceptible Diabetic D2 Mice
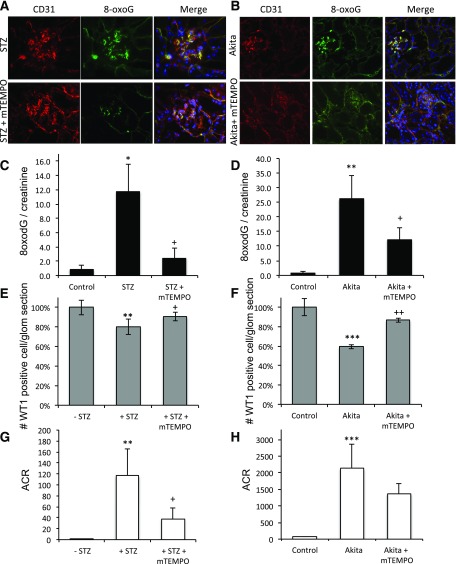
To investigate whether diabetes-induced mitochondrial dysfunction and mtStress of glomerular endothelial cells are required for podocyte loss in DKD-susceptible D2 mice, we implanted osmotic mini-pumps subcutaneously for continuous systemic administration of the mitochondrial-targeted potent antioxidant mitoTEMPO (33) or control vehicle (saline) in STZ-treated D2 and Akita-D2 mice. MitoTEMPO (1 mg/kg/day) used at a dosage to specifically target mitochondria (34) had no effect on blood glucose levels in diabetic animals (Supplementary Fig. 3A). Compared with control vehicle-treated diabetic mice, mitoTEMPO administration during 3 weeks of diabetes prevented 8-oxoG accumulation in glomerular endothelial cells and significantly reduced urinary 8-oxodG levels in STZ D2 mice (Fig. 4A and C) and Akita-D2 mice (Fig. 4B and D). In both experimental models, pharmacological reduction of mtStress was associated with significant amelioration of podocyte depletion and albuminuria (Fig. 4E–H) and improved glomerular histopathology (Supplementary Fig. 3B–G) compared with vehicle-treated mice. These findings show that endothelial mtStress may underlie DKD susceptibility.
Figure 4.
MitoTEMPO prevented diabetes-mediated mtStress in glomerular endothelial cells, podocyte loss, and albuminuria. A: Immunofluorescence detecting CD31-positive glomerular endothelial cell and mtDNA 8-oxoG in kidneys of STZ-D2 mice with 3-week diabetes. STZ treatment showing prominent glomerular 8-oxoG staining (A, top) and STZ cotreated with mitoTEMPO (1 mg/kg/day) showing reduced staining (A, bottom). B: CD31 and 8-oxoG in kidneys of Akita D2 mice after 3 weeks of diabetes (top) or diabetes with mitoTEMPO (1 mg/kg/day) (bottom). Urine 8-oxodG/creatinine of control D2 mice, STZ-D2, or STZ-D2 cotreated with mitoTEMPO (C) and 3-week diabetic Akita-D2 mice or Akita-D2 cotreated with mitoTEMPO (D) (n = 5; ±SEM). Podocyte number (percent of WT-1–positive cells/glomeruli) of control D2 mice, STZ-D2, or STZ-D2 cotreated with mitoTEMPO (E) and Akita-D2 mice or Akita-D2 cotreated with mitoTEMPO (n = 6; ±SEM) (F). ACR of control D2 mice, STZ-D2, or STZ-D2 plus mitoTEMPO (G) or Akita-D2 mice or Akita-D2 plus mitoTEMPO (H) (n = 5; ±SEM). In E and F, the percentage of WT-1–positive cell counts/glomeruli is mean ± SEM of at least 250 glomeruli from 5 to 6 mice per group. *P < 0.05, **P < 0.01, ***P < 0.001 vs. control mice; +P < 0.05, ++P < 0.01 vs. diabetic mice.
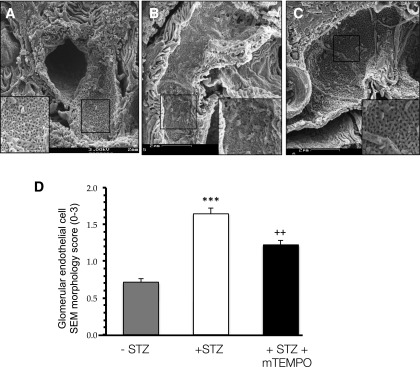
Next, we performed scanning electron microscopy to image the glomerular capillary wall and assess glomerular endothelial cell alterations by applying a semiquantitative EMI. Glomerular capillary endothelia of nondiabetic control mice showed extensive fenestration pattern (Fig. 5A). In contrast, after 3 weeks of diabetes, endothelia had lost fenestration and manifested increased cellular blebbing (Fig. 5B). MitoTEMPO treatment prevented the loss of fenestrations and cellular blebbing in diabetes (Fig. 5C). Average EMI in diabetic D2 mice was significantly increased compared with nondiabetic controls (1.64 ± 0.08 vs. 0.71 ± 0.05), and mitoTEMPO treatment significantly improved EMI to 1.22 ± 0.07 (Fig. 5D). These data demonstrate that pharmacological inhibition of endothelial mtStress in DKD-susceptible D2 mice improves endothelial and podocyte parameters, including endothelial fenestration/injury, podocyte depletion, albuminuria, and glomerular sclerosis.
Figure 5.
Diabetes-mediated glomerular endothelial cell injury is ameliorated by mitoTEMPO. Scanning electron micrographs of control D2 (A), 3-week diabetic STZ-D2 (B), and STZ-D2 mice (C) cotreated with mitoTEMPO (1 mg/kg/day). D: EMI (see research design and methods) of control, 3-week STZ-D2, and STZ-D2 plus mitoTEMPO mice. Mean ± SEM of at least 90 capillary vessels of glomeruli from 5 mice per group. ***P < 0.001 vs. control mice; ++P < 0.01 vs. diabetic mice.
Increased Circulating Endothelin-1 and Expression of Ednra in Endothelial Cells Are Characteristic of DKD-Susceptible Mice and Human DKD
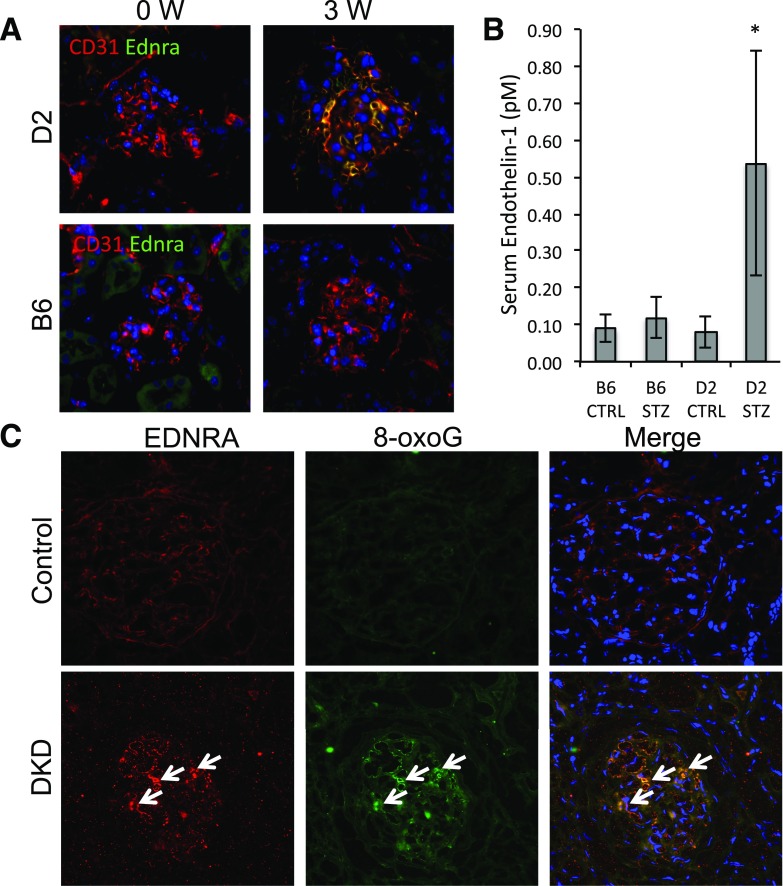
We have previously demonstrated that ligand–receptor pair Edn1 (or ET-1) and Ednra (or ETAR or ETA) mediated glomerular endothelial mtStress, which was essential for subsequent development of podocyte apoptosis, depletion, and glomerulosclerosis in a transgenic mouse model of podocyte-selective transforming growth factor-β signaling (12). Because Edn1 antagonism could be beneficial in treatment of human DKD (35,36), we examined Ednra transmembrane receptor expression. Ednra was detectable and colocalized with CD31 endothelial marker in glomeruli of 3-week diabetic D2 mice, whereas Ednra was not detectable in diabetic B6 mice or nondiabetic control D2 and B6 mice (Fig. 6A) and was undetected in synaptopodin-expressing podocytes (data not shown). Circulating Ednra-ligand/Edn1 levels were comparable between nondiabetic B6 and D2 control and diabetic B6 mice, but significantly increased in diabetic D2 mice (Fig. 6B). Interestingly, there are no overall differences in systolic blood pressure between diabetic B6 and D2 mice (37). These results suggest that upregulation of circulating Edn1 ligand and receptor Ednra is a characteristic feature of DKD-susceptible D2 mice and not of DKD-resistant B6 mice. Consistent with these observations, EDNRA and 8-oxoG were not detectable in glomeruli of normal human kidney. However, EDNRA was detectable in human kidney biopsies of patients with DKD, and it colocalized with glomerular endothelial cells containing mtDNA 8-oxoG lesions (Fig. 6C).
Figure 6.
Expression of Ednra in glomerular endothelial cells, circulating Edn1 exclusively in DKD-susceptible mice, and increased EDNRA expression in glomerular endothelial cells in human DKD. A: Double immunofluorescence detecting Ednra (green) and endothelial cell marker CD31 (red) in glomeruli of 3-week diabetic STZ-D2 and STZ-B6 mice. B: Serum levels of Edn1 from control and 3-week diabetic B6 and D2 mice (n = 5 to 6 mice/group; ±SEM). C: EDNRA (red) and 8-oxoG (green) in kidney biopsy from a human control subject (top) and a patient diagnosed with DKD (bottom). Colocalization indicated by arrows. *P < 0.05 vs. control mice.
Ednra Antagonist Treatment Prevents Endothelial Mitochondrial Oxidative Damage and Ameliorates Diabetes-Induced Glomerular Injury
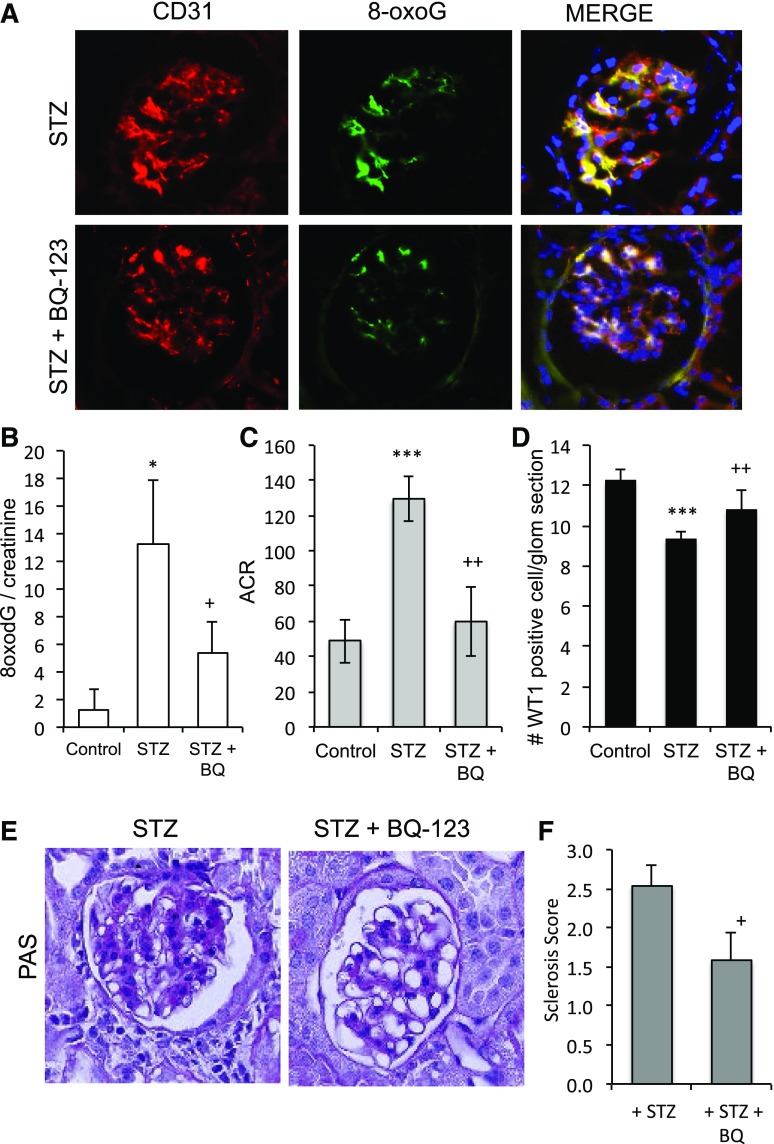
We used the peptide antagonist BQ-123, which specifically inhibits the binding of Edn1 ligand to Ednra receptor (38), to examine whether endothelial Edn1/Ednra signaling could mediate endothelial mtStress in DKD-susceptible D2 mice. BQ-123 administration by osmotic mini-pumps had no effect on FBG (Supplementary Fig. 4), significantly reduced the increase of 8-oxoG staining in glomerular endothelial cells (Fig. 7A), and significantly reduced the urinary excretion of 8-oxodG adducts (Fig. 7B) at 3 weeks of diabetes compared with vehicle-treated mice. BQ-123 significantly reduced urinary albumin excretion (Fig. 7C) and podocyte depletion (Fig. 7D). Glomerular matrix expansion (Fig. 7E) was significantly improved by BQ-123 treatment compared with vehicle-treated diabetic mice (Fig. 7F). Taken together, these results suggest that inhibition of Ednra activation in glomerular endothelial cells ameliorates mtStress and phenocopies the effects of mitochondrial-targeted scavenger in diabetic DKD-susceptible D2 mice.
Figure 7.
Edn1 plus Ednra mediates glomerular endothelial mitochondrial dysfunction and progression of DKD. A: Immunofluorescence detecting mtDNA 8-oxoG in prominent CD31-positive glomerular endothelial cells of 3-week diabetic STZ-D2 (top) and STZ-D2 mice cotreated with BQ-123 (0.1 nmol/kg/day) (bottom). B: Urine 8-oxodG/creatinine levels of control mice, STZ-D2, or STZ-D2 cotreated with BQ-123. ACR (C) and podocyte number (WT-1–positive cells/glomeruli) (D) of control mice, STZ-D2, or STZ-D2 cotreated with BQ-123. E: PAS staining of kidneys from STZ-D2 (3 weeks diabetic; left) and STZ-D2 cotreated with BQ-123 (right). F: The sclerosis index score from STZ-D2 ± BQ-123 was performed as previously described (58), and glomeruli were graded as follows: 0 represents no lesion, 1+ represents sclerosis of <25% of the glomerulus, whereas 2+, 3+, and 4+ represent sclerosis of >25–50, >50–75, and >75% of the glomerulus, respectively. WT-1–positive cell counts/glomeruli per section in D are mean ± SEM of at least 180 glomeruli from 6 mice per group. *P < 0.05, ***P < 0.001 vs. control mice; +P < 0.05, ++P < 0.01 vs. diabetic mice.
hGluc-Induced Glomerular Endothelial Ednra Expression Is Linked to Increased mtStress
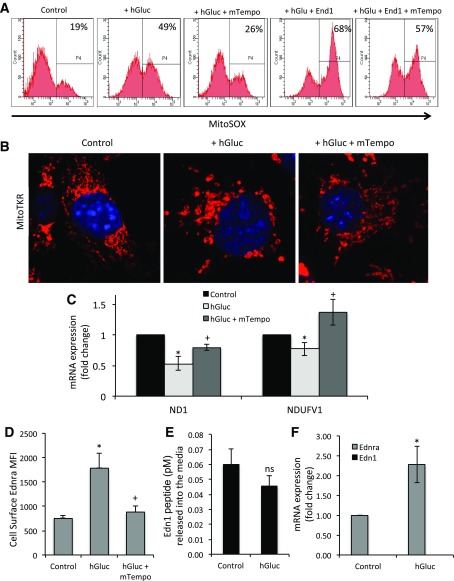
We next examined the relationship between mitochondrial damage and Ednra in mGECs. First, compared with normal glucose (5 mmol) plus 25 mmol d-mannitol as osmotic control, we confirmed that hGluc (30 mmol) treatment for 24 h increased mitochondrial ROS using a MitoSOX probe (Invitrogen) (Fig. 8A). In this study, we show that hGluc-induced mitochondrial ROS was further augmented by cotreatment with Edn1 (Fig. 8A), and this was reduced by mitoTEMPO. mtROS induced by hGluc was accompanied by increased mtDNA 8-oxoG lesions (Supplementary Fig. 5) and mitochondrial fission/fragmentation (Fig. 8B). A decrease in the transcription of mitochondrial-encoded ND1 and nuclear-encoded mitochondrial NDUFV1 expression by hGluc was prevented by cotreatment with mitoTEMPO (Fig. 8C). There was also a reduction of baseline, ATP-linked, and reserve OCR in mGECs treated with hGluc for 24 h and no differences after Nω-nitro-l-arginine methyl ester (l-NAME) treatment of mGECs, although l-NAME as well as hGluc treatment decreased endothelial nitric oxide synthetase activity (Supplementary Fig. 6A and B).
Figure 8.
hGluc–induced glomerular endothelial Ednra expression is linked to increased mitochondrial ROS. A: Percent increase of MitoSOX bright fluorescent mGEC control cells in control (5 μmol glucose plus 25 mmol d-mannitol) or after culture with hGluc (30 mmol) or hGluc plus Edn1 (200 ng/mL) for 24 h in the absence or presence of mitoTEMPO (1 μg/mL). B: Superresolution image of mitochondrial networks by MitoTracker Red in control or hGluc-treated mGECs ± mitoTEMPO. C: mRNA expression of ND1 and NDUFV1 in mGEC controls treated with hGluc or hGluc plus mitoTEMPO for 24 h. D: Mean fluorescence intensity (MFI) of Ednra mGEC surface expression measured by FACS in control RPMI and hGluc in the absence or presence of mitoTEMPO (1 μg/mL). E: Quantification by ELISA of Edn1 release into the culture media after 24 h by control or hGluc-treated mGEC. F: mRNA expression of Edn1 and Ednra in mGEC controls or treated with hGluc for 24 h as indicated. Bars represent mean ± SEM of three to five independent experiments. *P < 0.05 vs. controls; +P < 0.05 vs. hGluc.
hGluc increased mGEC Ednra cell surface expression by 2.5-fold, and this increase was prevented by mitoTEMPO, suggesting that mtStress was required for Ednra upregulation (Fig. 8D). Hyperglycemia can induce Edn1 expression in endothelial cells via downregulation of ERK5 and the transcriptional repressor KLF2 (39). Interestingly, hGluc alone did not induce mRNA expression or production of ligand Edn1 by mGEC (Fig. 8E and F); hence the elevated Edn1 in diabetic D2 mice could be synthesized by other than glomerular endothelial cells as previously suggested (39), and alternatively, factors other than glucose could stimulate Edn1 expression by endothelial cells and release into circulation. Taken together, these in vitro results demonstrate that hGluc induced mitochondria dysfunction and mtDNA instability resulting from increased mitochondrial ROS and contributes to endothelial dysfunction and thereby to DKD susceptibility.
Discussion
We have identified mitochondrial-dependent glomerular endothelial pathomechanisms as essential in mediating experimental diabetic nephropathy characteristic of DKD-susceptible mice. Our conclusion is supported by a series of targeted studies, guided by initial unbiased transcriptomic profiling of glomeruli after onset of diabetes in DKD-susceptible D2 and -resistant B6 inbred mouse strains. First, hallmarks of DKD-susceptible D2 strain, including albuminuria, podocyte depletion, and glomerulosclerosis, were associated with molecular and functional evidence for mtStress and dysfunction selectively in glomerular endothelial cells, but not in podocytes. Second, glomerular endothelial oxidative mtStress and in situ DNA damage marker 8-oxoG were associated with de novo endothelial expression of EDNRA in DKD-susceptible diabetic D2 mice and humans diagnosed with DKD and increased serum Edn1 levels. Third, pharmacological inhibition of Ednra or of oxidative mtStress reduced mtDNA oxidative damage in endothelial cells and in urine 8-oxodG of diabetic D2 mice, and this was associated with improved endothelial morphological injury in situ, including preservation of endothelial fenestration. Fourth, the reduction of endothelial mitochondrial oxidative damage and preservation of endothelial fenestration was associated with ameliorated albuminuria, podocyte depletion, and glomerulosclerosis. Interestingly, increased urinary 8-oxodG excretion was characteristic of patients with diabetes with progressive chronic kidney disease, validating our findings in DKD-susceptible D2 mice. Finally, hGluc was shown to stimulate glomerular endothelial mitochondrial ROS and fragmentation, mtDNA instability, and increased Ednra expression. On the basis of our observations, we propose that DKD susceptibility in mice and human DKD is characterized by an essential role of endothelial injury and dysfunction with loss of fenestrations, mediated partly by EDNRA-induced endothelial mtStress. Our findings are in support of cross talk between stressed glomerular endothelial cells and podocytes and suggest potential therapeutic targets to protect against secondary podocyte damage and eventual loss as progression factors for DKD.
Our conclusion is consistent with observations in humans with T1D and T2D and a wide body of evidence that indicates glomerular endothelial dysfunction and glycocalyx damage represent initiating steps in diabetic albuminuria (40). In a cohort of T1D followed for 10 years, peripheral blood composite biomarker of endothelial dysfunction was correlated with decline of eGFR (41) and determined to predict progression of renal disease in patients with T2D (42). Finally, state-of-the-art morphometric studies in T1D demonstrate that diminished endothelial cell fenestration is related to classic diabetic nephropathy lesions and renal function (43). Furthermore, loss of glycocalyx in diabetic mouse models supports an endothelial involvement in early diabetes (44), and recent studies also suggest a possible link between effects of Edn1 and loss of glycocalyx in mouse models of DKD (45,46). Thus, identification of EDNRA-induced mitochondrial dysfunction and oxidative stress in glomerular endothelial cells as essential mediators of endothelial fenestration loss, albuminuria, podocyte depletion, and glomerulosclerosis may provide a common pathomechanism underlying these observations in humans.
Antagonism of the pluripotent EDN1 signaling system and in particular the cognate receptor EDNRA has emerged as a promising therapeutic strategy in cardiovascular and renal diseases, including DKD (47). Recent promising studies with new, EDNRA-selective antagonists show beneficial modulation of progression markers in diabetic nephropathy (36), and hard-outcome results of the phase III clinical trial Study of Diabetic Nephropathy With Atrasentan (SONAR) are expected in 2018. However, understanding of the basic pathomechanisms by which the EDNRA target may promote progression of diabetic nephropathy remains incomplete to date.
Our results reported in this study suggest an essential role for endothelial cell injury in orchestrating the characteristic glomerular response and lesions of DKD, in particular podocyte injury/depletion, glomerular basement membrane alterations, and mesangial expansion. Consistent with absence of Ednra in normal glomeruli, Ednra is expressed in media of intrarenal vessels in the mouse kidney, but not in endothelial cells or glomeruli (48). In contrast, in DKD-susceptible mice and human case subjects of DKD, we demonstrate de novo glomerular endothelial expression of EDNRA. Increased circulating EDN1 levels have been described in patients with diabetes (49). Interestingly, diabetes significantly increased serum Edn1 in DKD-susceptible D2 mice, and endothelial cells exposed to hGluc also show increased Ednra expression, changes in mitochondrial networks with increased fission, and mitochondrial ROS. Thus, endothelial upregulation of the EDNRA and signaling activation in response to circulating EDN1 is characteristic of DKD susceptibility in mice and humans.
A variety of pathomechanisms, acting in different glomerular cell types through either EDNRA or EDNRB receptors, have been proposed to mediate injurious EDN1 activities in DKD (50). In particular, a recent report (51) describes the use of podocyte-selective double knockout of Ednra and Ednrb in experimental diabetes, and the authors conclude that direct action of Edn1 on podocytes mediated through both receptors promotes diabetic glomerulosclerosis. However, glomerular expression studies of Ednra and Ednrb in vivo are not presented, and functional signaling studies are conducted using whole glomeruli, not podocytes. Only partial knockout of Ednra and Ednrb was demonstrated, and the mice subjected to experimental diabetes were of a mixed genetic background.
Our findings demonstrate that hyperglycemia and EDN1- and EDNRA-mediated mtStress/damage in glomerular endothelium are hallmarks of DKD susceptibility in diabetic mice and human DKD—particularly a reduction in reserve respiratory capacity in endothelial cells, which may be a direct response to oxidative stress (25) and decreased SOD2. Altogether, our findings are consistent with the longstanding model that overproduction of superoxide by the mitochondrial electron transport chain is a unifying central mechanism underlying diabetic complications (52). This hypothesis has been challenged recently in a report suggesting reduced mitochondrial superoxide production in kidney cortex of diabetic mice (53). Some questions have been raised regarding the interpretation of this study (54), and it is important to note that mice used in the study were C57BL/6J DKD-resistant strain. However, consistent with our findings, Dugan et al. (53) also report increased glomerular labeling for the oxidative DNA damage marker 8-oxoG. At present, mitochondrial dysfunction appears to be a consistent finding in DKD, whereas additional investigation is warranted to better understand the contribution of redox processes in DKD susceptibility. Moreover, there are the disappointing results of clinical trials using antioxidants in DKD with conflicting outcomes and some safety concerns (55,56). Potential reasons may include our lack of full understanding of oxidant and antioxidant actions, the use of nonspecific/nonmitochondrial-targeted scavengers, studies performed in poorly defined patient populations, and timing of treatment, among others. Specific targeting of mitochondrial ROS may yet prove to be beneficial in diabetes, as preclinical data with Szeto-Schiller peptides (Bendavia) show benefits in rodent models of DKD by improving mitochondrial bioenergetics (57).
In summary, early diabetes of DKD-susceptible mice strains and patients with progressive DKD is characterized by Edn1-Ednra–mediated mitochondrial oxidative damage of glomerular endothelial cells exclusively and mediates podocyte defects and depletion, albuminuria, and glomerulosclerosis.
Supplementary Material
Article Information
Acknowledgments. The authors thank the Microscopy Shared Facility at the Icahn School of Medicine at Mount Sinai for assistance.
Funding. This work was supported by National Institutes of Health grants 5U01-DK-060995, 5R01-DK-056077 (to E.B.), and R01-DK-097253 (to I.D.)
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. H.Q. conceived and designed the study, analyzed data, and drafted the manuscript. G.C. and S.S. researched, analyzed, and interpreted data. L.Y., K.E., Y.S., and W.Z. researched data and revised the manuscript. V.D. provided biopsy material and revised the manuscript. D.S. and B.H. contributed to analysis and reviewed and edited the manuscript. E.B. designed the study and critically revised the manuscript. I.D. designed the study, researched and analyzed data, and wrote the manuscript. E.B. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article contains Supplementary Data online at http://diabetes.diabetesjournals.org/lookup/suppl/doi:10.2337/db16-0695/-/DC1.
References
- 1.Collins AJ, Kasiske B, Herzog C, et al. Excerpts from the United States Renal Data System 2004 annual data report: atlas of end-stage renal disease in the United States. Am J Kidney Dis 2005;45:A5–A7 [DOI] [PubMed] [Google Scholar]
- 2.Finne P, Reunanen A, Stenman S, Groop PH, Grönhagen-Riska C. Incidence of end-stage renal disease in patients with type 1 diabetes. JAMA 2005;294:1782–1787 [DOI] [PubMed] [Google Scholar]
- 3.Qi Z, Fujita H, Jin J, et al. Characterization of susceptibility of inbred mouse strains to diabetic nephropathy. Diabetes 2005;54:2628–2637 [DOI] [PubMed] [Google Scholar]
- 4.Breyer MD, Böttinger E, Brosius FC 3rd, et al.; AMDCC . Mouse models of diabetic nephropathy. J Am Soc Nephrol 2005;16:27–45 [DOI] [PubMed] [Google Scholar]
- 5.Meyer TW, Bennett PH, Nelson RG. Podocyte number predicts long-term urinary albumin excretion in Pima Indians with type II diabetes and microalbuminuria. Diabetologia 1999;42:1341–1344 [DOI] [PubMed] [Google Scholar]
- 6.Susztak K, Raff AC, Schiffer M, Böttinger EP. Glucose-induced reactive oxygen species cause apoptosis of podocytes and podocyte depletion at the onset of diabetic nephropathy. Diabetes 2006;55:225–233 [PubMed] [Google Scholar]
- 7.Sun YB, Qu X, Zhang X, Caruana G, Bertram JF, Li J. Glomerular endothelial cell injury and damage precedes that of podocytes in adriamycin-induced nephropathy. PLoS One 2013;8:e55027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haraldsson B, Nyström J, Deen WM. Properties of the glomerular barrier and mechanisms of proteinuria. Physiol Rev 2008;88:451–487 [DOI] [PubMed] [Google Scholar]
- 9.Ballermann BJ. Contribution of the endothelium to the glomerular permselectivity barrier in health and disease. Nephron, Physiol 2007;106:19–25 [DOI] [PubMed] [Google Scholar]
- 10.Fogo AB, Kon V. The glomerulus--a view from the inside--the endothelial cell. Int J Biochem Cell Biol 2010;42:1388–1397 [DOI] [PubMed] [Google Scholar]
- 11.Haraldsson B, Nyström J. The glomerular endothelium: new insights on function and structure. Curr Opin Nephrol Hypertens 2012;21:258–263 [DOI] [PubMed] [Google Scholar]
- 12.Daehn I, Casalena G, Zhang T, et al. Endothelial mitochondrial oxidative stress determines podocyte depletion in segmental glomerulosclerosis. J Clin Invest 2014;124:1608–1621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Holthöfer H, Kretzler M, Haltia A, et al. Altered gene expression and functions of mitochondria in human nephrotic syndrome. FASEB J 1999;13:523–532 [DOI] [PubMed] [Google Scholar]
- 14.Forbes JM, Coughlan MT, Cooper ME. Oxidative stress as a major culprit in kidney disease in diabetes. Diabetes 2008;57:1446–1454 [DOI] [PubMed] [Google Scholar]
- 15.Brownlee M. Biochemistry and molecular cell biology of diabetic complications. Nature 2001;414:813–820 [DOI] [PubMed] [Google Scholar]
- 16.Rolo AP, Palmeira CM. Diabetes and mitochondrial function: role of hyperglycemia and oxidative stress. Toxicol Appl Pharmacol 2006;212:167–178 [DOI] [PubMed] [Google Scholar]
- 17.Suzuki S, Hinokio Y, Komatu K, et al. Oxidative damage to mitochondrial DNA and its relationship to diabetic complications. Diabetes Res Clin Pract 1999;45:161–168 [DOI] [PubMed] [Google Scholar]
- 18.Weil EJ, Lemley KV, Mason CC, et al. Podocyte detachment and reduced glomerular capillary endothelial fenestration promote kidney disease in type 2 diabetic nephropathy. Kidney Int 2012;82:1010–1017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhao HJ, Wang S, Cheng H, et al. Endothelial nitric oxide synthase deficiency produces accelerated nephropathy in diabetic mice. J Am Soc Nephrol 2006;17:2664–2669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yuen DA, Stead BE, Zhang Y, et al. eNOS deficiency predisposes podocytes to injury in diabetes. J Am Soc Nephrol 2012;23:1810–1823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhong F, Chen H, Wei C, et al. Reduced Kruppel-like factor 2 expression may aggravate the endolethial injury of diabetic nephropathy. Kidney Int 2015; 87:382–395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ohno M, Oka S, Nakabeppu Y. Quantitative analysis of oxidized guanine, 8-oxoguanine, in mitochondrial DNA by immunofluorescence method. Methods Mol Biol 2009;554:199–212 [DOI] [PubMed] [Google Scholar]
- 23.Casalena G, Bottinger E, Daehn I. TGFβ-induced actin cytoskeleton rearrangement in podocytes is associated with compensatory adaptation of mitochondrial energy metabolism. Nephron 2015;131:278–284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shi S, Yu L, Chiu C, et al. Podocyte-selective deletion of dicer induces proteinuria and glomerulosclerosis. J Am Soc Nephrol 2008;19:2159–2169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dranka BP, Hill BG, Darley-Usmar VM. Mitochondrial reserve capacity in endothelial cells: The impact of nitric oxide and reactive oxygen species. Free Radic Biol Med 2010;48:905–914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ayala-Torres S, Chen Y, Svoboda T, Rosenblatt J, Van Houten B. Analysis of gene-specific DNA damage and repair using quantitative polymerase chain reaction. Methods 2000;22:135–147 [DOI] [PubMed] [Google Scholar]
- 27.Germadnik D, Pilger A, Rüdiger HW. Assay for the determination of urinary 8-hydroxy-2′-deoxyguanosine by high-performance liquid chromatography with electrochemical detection. J Chromatogr B Biomed Sci Appl 1997;689:399–403 [DOI] [PubMed] [Google Scholar]
- 28.Susztak K, Sharma K, Schiffer M, McCue P, Ciccone E, Böttinger EP. Genomic strategies for diabetic nephropathy. J Am Soc Nephrol 2003;14(Suppl. 3):S271–S278 [DOI] [PubMed] [Google Scholar]
- 29.Oberley LW. Free radicals and diabetes. Free Radic Biol Med 1988;5:113–124 [DOI] [PubMed] [Google Scholar]
- 30.Fujita H, Fujishima H, Takahashi K, et al. SOD1, but not SOD3, deficiency accelerates diabetic renal injury in C57BL/6-Ins2(Akita) diabetic mice. Metabolism 2012;61:1714–1724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Daehn I, Brem R, Barkauskaite E, Karran P. 6-Thioguanine damages mitochondrial DNA and causes mitochondrial dysfunction in human cells. FEBS Lett 2011;585:3941–3946 [DOI] [PubMed] [Google Scholar]
- 32.Oka S, Ohno M, Nakabeppu Y. Construction and characterization of a cell line deficient in repair of mitochondrial, but not nuclear, oxidative DNA damage. Methods Mol Biol 2009;554:251–264 [DOI] [PubMed] [Google Scholar]
- 33.Trnka J, Blaikie FH, Smith RA, Murphy MP. A mitochondria-targeted nitroxide is reduced to its hydroxylamine by ubiquinol in mitochondria. Free Radic Biol Med 2008;44:1406–1419 [DOI] [PubMed] [Google Scholar]
- 34.Reily C, Mitchell T, Chacko BK, Benavides G, Murphy MP, Darley-Usmar V. Mitochondrially targeted compounds and their impact on cellular bioenergetics. Redox Biol 2013;1:86–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Andress DL, Coll B, Pritchett Y, Brennan J, Molitch M, Kohan DE. Clinical efficacy of the selective endothelin A receptor antagonist, atrasentan, in patients with diabetes and chronic kidney disease (CKD). Life Sci 2012;91:739–742 [DOI] [PubMed] [Google Scholar]
- 36.de Zeeuw D, Coll B, Andress D, et al. The endothelin antagonist atrasentan lowers residual albuminuria in patients with type 2 diabetic nephropathy. J Am Soc Nephrol 2014;25:1083–1093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gurley SB, Clare SE, Snow KP, Hu A, Meyer TW, Coffman TM. Impact of genetic background on nephropathy in diabetic mice. Am J Physiol Renal Physiol 2006;290:F214–F222 [DOI] [PubMed] [Google Scholar]
- 38.Eguchi S, Hirata Y, Ihara M, Yano M, Marumo F. A novel ETA antagonist (BQ-123) inhibits endothelin-1-induced phosphoinositide breakdown and DNA synthesis in rat vascular smooth muscle cells. FEBS Lett 1992;302:243–246 [DOI] [PubMed] [Google Scholar]
- 39.Wu Y, Feng B, Chen S, Zuo Y, Chakrabarti S. Glucose-induced endothelin-1 expression is regulated by ERK5 in the endothelial cells and retina of diabetic rats. Can J Physiol Pharmacol 2010;88:607–615 [DOI] [PubMed] [Google Scholar]
- 40.Satchell SC, Tooke JE. What is the mechanism of microalbuminuria in diabetes: a role for the glomerular endothelium? Diabetologia 2008;51:714–725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Astrup AS, Tarnow L, Pietraszek L, et al. Markers of endothelial dysfunction and inflammation in type 1 diabetic patients with or without diabetic nephropathy followed for 10 years: association with mortality and decline of glomerular filtration rate. Diabetes Care 2008;31:1170–1176 [DOI] [PubMed] [Google Scholar]
- 42.Persson F, Rossing P, Hovind P, et al. Irbesartan treatment reduces biomarkers of inflammatory activity in patients with type 2 diabetes and microalbuminuria: an IRMA 2 substudy. Diabetes 2006;55:3550–3555 [DOI] [PubMed] [Google Scholar]
- 43.Toyoda M, Najafian B, Kim Y, Caramori ML, Mauer M. Podocyte detachment and reduced glomerular capillary endothelial fenestration in human type 1 diabetic nephropathy. Diabetes 2007;56:2155–2160 [DOI] [PubMed] [Google Scholar]
- 44.Dogné S, Rath G, Jouret F, Caron N, Dessy C, Flamion B. Hyaluronidase 1 deficiency preserves endothelial function and glycocalyx integrity in early streptozotocin-induced diabetes. Diabetes 2016;65:2742–2753 [DOI] [PubMed] [Google Scholar]
- 45.Garsen M, Lenoir O, Rops AL, et al. Endothelin-1 induces proteinuria by heparanase-mediated disruption of the glomerular glycocalyx. J Am Soc Nephrol 2016;27:3545–3551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Boels MG, Avramut MC, Koudijs A, et al. Atrasentan reduces albuminuria by restoring the glomerular endothelial glycocalyx barrier in diabetic nephropathy. Diabetes 2016;65:2429–2439 [DOI] [PubMed] [Google Scholar]
- 47.Lüscher TF, Barton M. Endothelins and endothelin receptor antagonists: therapeutic considerations for a novel class of cardiovascular drugs. Circulation 2000;102:2434–2440 [DOI] [PubMed] [Google Scholar]
- 48.Kitazawa T, Sato T, Nishiyama K, et al. Identification and developmental analysis of endothelin receptor type-A expressing cells in the mouse kidney. Gene Expr Patterns 2011;11:371–377 [DOI] [PubMed] [Google Scholar]
- 49.Takahashi K, Ghatei MA, Lam HC, O’Halloran DJ, Bloom SR. Elevated plasma endothelin in patients with diabetes mellitus. Diabetologia 1990;33:306–310 [DOI] [PubMed] [Google Scholar]
- 50.Mishra R, Emancipator SN, Kern TS, Simonson MS. Association between endothelin-1 and collagen deposition in db/db diabetic mouse kidneys. Biochem Biophys Res Commun 2006;339:65–70 [DOI] [PubMed] [Google Scholar]
- 51.Lenoir O, Milon M, Virsolvy A, et al. Direct action of endothelin-1 on podocytes promotes diabetic glomerulosclerosis. J Am Soc Nephrol 2014;25:1050–1062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nishikawa T, Edelstein D, Du XL, et al. Normalizing mitochondrial superoxide production blocks three pathways of hyperglycaemic damage. Nature 2000;404:787–790 [DOI] [PubMed] [Google Scholar]
- 53.Dugan LL, You YH, Ali SS, et al. AMPK dysregulation promotes diabetes-related reduction of superoxide and mitochondrial function. J Clin Invest 2013;123:4888–4899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nishikawa T, Brownlee M, Araki E. Mitochondrial reactive oxygen species in the pathogenesis of early diabetic nephropathy. J Diabetes Investig 2015;6:137–139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lonn E, Yusuf S, Hoogwerf B, et al.; HOPE Study; MICRO-HOPE Study . Effects of vitamin E on cardiovascular and microvascular outcomes in high-risk patients with diabetes: results of the HOPE study and MICRO-HOPE substudy. Diabetes Care 2002;25:1919–1927 [DOI] [PubMed] [Google Scholar]
- 56.de Zeeuw D, Akizawa T, Audhya P, et al.; BEACON Trial Investigators . Bardoxolone methyl in type 2 diabetes and stage 4 chronic kidney disease. N Engl J Med 2013;369:2492–2503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Birk AV, Liu S, Soong Y, et al. The mitochondrial-targeted compound SS-31 re-energizes ischemic mitochondria by interacting with cardiolipin. J Am Soc Nephrol 2013;24:1250–1261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ma LJ, Fogo AB. Model of robust induction of glomerulosclerosis in mice: importance of genetic background. Kidney Int 2003;64:350–355 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.