Abstract
Regular HIV testing enables early identification and treatment of HIV among at-risk men who have sex with men (MSM). Characterizing HIV testing needs for Internet-using MSM informs development of Internet-facilitated testing interventions. In this systematic review we analyze HIV testing patterns among Internet-using MSM in the United States who report, through participation in an online study or survey, their HIV status as negative or unknown and identify demographic or behavioral risk factors associated with testing. We systematically searched multiple electronic databases for relevant English-language articles published between January 1, 2005 and December 16, 2014. Using meta-analysis, we summarized the proportion of Internet-using MSM who had ever tested for HIV and the proportion who tested in the 12 months preceding participation in the online study or survey. We also identified factors predictive of these outcomes using meta-regression and narrative synthesis. Thirty-two studies that enrolled 83,186 MSM met our inclusion criteria. Among the studies reporting data for each outcome, 85 % (95 % CI 82–87 %) of participants had ever tested, and 58 % (95 % CI 53–63 %) had tested in the year preceding enrollment in the study, among those for whom those data were reported. Age over 30 years, at least a college education, use of drugs, and self-identification as being homosexual or gay were associated with ever having tested for HIV. A large majority of Internet-using MSM indicated they had been tested for HIV at some point in the past. A smaller proportion—but still a majority—reported they had been tested within the year preceding study or survey participation. MSM who self-identify as heterosexual or bisexual, are younger, or who use drugs (including non-injection drugs) may be less likely to have ever tested for HIV. The overall findings of our systematic review are encouraging; however, a subpopulation of MSM may benefit from targeted outreach. These findings indicate unmet needs for HIV testing among Internet-using MSM and identify subpopulations that might benefit from targeted outreach, such as provision of HIV self-testing kits.
Keywords: Homosexuality, Male, Bisexuality, HIV testing, Internet, Social media, Systematic review, Meta-analysis
Introduction
Men who have sex with men (MSM) are disproportionately affected by HIV. In 2014, in the United States, 82 % of the HIV diagnoses among males aged 13 years of age or older were among MSM [1]. Data suggest young MSM and African-American MSM are the least likely to know they are infected [2].
Testing is the key to identifying HIV infection and prompting linkage to care for antiretroviral therapy and support services aimed at preventing secondary transmission [3]. The Centers for Disease Control and Prevention (CDC) recommends MSM in the U.S. be re-screened for HIV at least annually, and some men might benefit from more frequent screening, such as every 3–6-months [4].
The Internet has gained popularity as a platform to conduct HIV research. The Internet may be advantageous for reaching ‘hidden populations’ of MSM—especially young MSM who are not reached through traditional community or venue-based outreach approaches [5, 6], who choose not to visit traditional clinical settings [6–8], or who use the Internet to meet romantic partners and sex partners [9]. Internet-based studies of MSM, however, are subject to several methodological limitations, including sampling bias due to the use of convenience sampling methods, duplicate responses, and misclassification bias from self-reported data [3, 8, 10]. Studies also suggest that compared to MSM recruited through venue-based sampling methods, men recruited on the Internet may be younger, predominately white, have higher levels of education and income, and may have different sexual risk factors and testing behaviors [5, 6]. Therefore, results from studies of internet-using MSM may not be representative of all MSM.
Assessing the HIV testing patterns of Internet-using MSM is warranted due to the paucity of research on HIV testing patterns among this population. Because testing behaviors of Internet-using MSM have not been systematically characterized and remain poorly understood, a greater understanding of this population would guide interpretation of Internet-based research regarding HIV among MSM.
The primary purpose of this systematic review was to assess HIV testing patterns of Internet-using MSM not known to have HIV infection by analyzing data from primary research including quantitative data from cross-sectional surveys and baseline data from intervention studies, as well as quantifiable data on HIV testing from focus groups. We then investigated the associations of demographic and other factors with testing. We defined “Internet use” as participation in Internet-based programs, Internet-based surveys, or by participation in offline programs in which Internet use is explicitly reported. The Internet could be accessed through a computer or a mobile device using a web browser or mobile app. We examined how many of these men have ever tested for HIV, testing frequency, and assessed factors associated with HIV testing that could inform which subpopulations should be targeted for future testing outreach efforts. Studies conducted outside the U.S. were outside the scope of this report; however, the findings for factors associated with testing may be of interest and applicability outside the U.S. because some research suggests that even when testing rates vary by country, demographic associations with testing may not [11].
Methods
We followed the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines for reporting, which is a list of items to report in a systematic review selected based upon evidence and consensus of experts in the field [12].
Literature Search Strategy
We searched PubMed, PsycINFO and CINAHL from 1/1/2005 through 12/16/2014. We derived a combination of free-text terms and controlled vocabulary concepts from the National Library of Medicine’s (NLM’s) Medical Subject Headings (MeSH) for MSM (homosexuality, male; bisexuality; unsafe sex NOT pregnancy; risk-taking) and the Internet (Internet; social media). Supplemental searches included reviews of bibliographies of relevant studies, and searches of “grey literature” including governmental websites, private organizations, and universities known to publish relevant research. (Full strategies are shown in Supplement Table 5).
Data Collection
All electronically identified records were imported into EndNote (Thomson Reuters) and de-duplicated. We systematically selected full-length studies published in the English language between 1/1/2005 and 12/16/2014. We limited publication date to 10 years before the search to promote relevance to current HIV testing patterns and Internet use. The studies had to enroll Internet-using MSM living in the United States who self-reported their HIV status as HIV-negative or unknown and reported one or more outcomes of interest:
The proportion of men ever tested for HIV;
The proportion tested for HIV in the past 12 months; or
The frequency of HIV testing in the past 12 months.
Studies could be any type of research design; however, from intervention studies we only collected baseline data prior to the administration of any intervention, and for qualitative studies, we collected empirical data only. Care was taken to avoid the inclusion of duplicate data: where findings were reported in more than one publication, we included reports on the larger population.
In addition, we collected information on HIV testing location or setting type and type of test (e.g., rapid test). We also extracted study and participant characteristics and HIV-related sexual and drug use behaviors to examine potential confounders on the main testing outcomes. Specific covariates included: study recruitment strategy; study sampling method; dates of data collection; sexual orientation; age; ethnicity or race; education; condomless anal intercourse (CAI); insertive CAI; receptive CAI; CAI with serodiscordant partner(s); multiple sex partners; concurrent sex partners; sexually transmitted infections (STI) diagnoses; and drug use.
When the two analysts disagreed on whether an article met our inclusion criteria, discrepancies were resolved through discussion and adjudication by a third analyst, if needed. Data extraction was performed by one analyst and audited by a second analyst who compared the contents of the data extraction forms to the information presented in each included article.
Analysis Methods
We used a standardized tool, Joanna Briggs Institute’s Critical Appraisal of Quantitative Evidence Tool for Descriptive/Case-Series Studies, to critically appraise studies [13]. Each item in the tool was assessed as a potential covariate in meta-regression. Where at least three studies provided information on a single testing outcome, we pooled data using random-effects meta-analysis [14]. All meta-analyses were performed using comprehensive meta-analysis (Biostat, Englewood, NJ). We assessed statistical heterogeneity using I2 and the Q-statistic [15, 16]. We interpreted an I2 value of 50 % or greater and/or a statistically significant Q-value (p < 0.05) as indicative of substantial heterogeneity.
Where substantial heterogeneity was detected, we investigated whether any potential covariates were associated with the differences in testing pattern among studies using meta-regression. Meta-regressions were performed using STATA 13 (STATA, College Station, TX) using permutation tests [17]. To avoid overfitting regression models, we performed univariable meta-regression only when both primary outcome and covariate data were available from at least 10 studies. We tested multivariable models (2 independent covariates, or more) only where the ratio of covariates to studies was greater than or equal to 1:10 [18, 19].
We used the results of these meta-regressions to assess whether various factors investigated as potential covariates (including items used to critically appraise studies, and demographic and sexual risk factors) were associated with testing patterns. In addition, we extracted data from studies that examined associations between testing patterns and individual participant data on demographic, sexual risk, and other factors. We intended to perform subgroup analyses to assess differences in overall testing rates stratified by characteristics, but data needed to do so were not reported in most of the included studies. We performed a narrative assessment of all potential factors reported by two or more individual studies, because a single study provides an insufficient amount of evidence to support a conclusion [20].
Considering the findings of our critical appraisal (e.g., quality of evidence), quantity of evidence, consistency of the evidence (including statistical consistency in the meta-analyses) and the results of the robustness testing, we drew conclusions and assigned strength of evidence ratings, which indicate the confidence we have in the conclusion and the likelihood that future research will not substantially alter conclusions [21, 22]. (see Table 1) We used a systematic framework to evaluate the studies (see Supplement Table 6).
Table 1.
Strength of evidence assessment ratings and interpretation
| Rating | Interpretation | Criteria |
|---|---|---|
| High | Further research is unlikely to change our confidence in the conclusion | No serious limitations |
| Moderate | Further research is likely to have an important impact on our confidence in the estimate of effect and may change the conclusion | One limitation |
| Low | Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the conclusion | Two limitations, or a serious limitation |
| Very low | Any conclusion is very uncertain | At least three limitations or serious limitations |
| Insufficient | No conclusion is currently possible | Pervasive limitations, or only one study addresses the outcome |
Results
Study Identification, Selection, and Overview
Electronic data base searches identified 3219 unique records, of which 257 were assessed in full-length reports for inclusion and 32 met inclusion criteria (see Fig. 1). Grey literature searches did not yield any additional unique and relevant records. These 32 studies, that enrolled a total of 83,186 Internet-using MSM, comprised the evidence base for this systematic review [23–55]. (Two publications report the same study [53, 54].) Table 2 provides a brief summary of all 32 included (and further details of the included studies are presented in Supplement Table 7).
Fig. 1.

Study selection process
Table 2.
Brief Summary of Included Studies
| Study | Target population | Recruitment | Age (Years)a | Ethnicity/Racea | Education |
|---|---|---|---|---|---|
| Akin et al. [23] | MSM, Hispanic in Miami-Dade County (n = 470) | In-person or Internet-based recruitment from venues and web sites. Enrolled 10/2003–02/2005 | Mean 32 | 100 % Hispanic, immigrants from Latin American countries | Not reported |
| Barriers to Online Prevention Research; Sullivan, et al. [24] | MSM, Internet-using (n = 9005) | Social media banner ads. Ads placed 3/19/2009–4/16/2009 | Mean 24, median 21 (range 18–80) years | n = 8552: 41 % White, non-Hispanic; 15 % Black, non-Hispanic; 33 % Hispanic; 2 % Asian/Pacific Islander; 2 % Native American/Alaska Native; 5 % Multiracial; 2 % Other | 92 % ≥ high school 15 % ≥ college/bachelor’s degree |
| CyBER/M4 M; Rhodes et al. [25] | MSM (n = 210) | Internet chat rooms. Recruitment and intervention over 18 months in 2004 and 2005 | Mean 31 (SD 11) years | n = 202: 56 % White; 38 % Black or African American; 3 % Hispanic or Latino; 0.5 % Asian; 1 % American Indian/Alaska Native; 2 % Multiracial/ethnic | Not reported |
| Dew and Chaney [26] | MSM who use internet chat (n = 513) | Internet chat rooms. Recruitment dates NR | Mean 36 (SD 11) | n = 511 reported: 81 % Caucasian; 6 % African American; 5 % Hispanic; 2 % Asian; 2 % Native American; 3 % Other | 100 % ≥ high school NR ≥ college/Bachelor’s degree |
| Fernandez et al. [27] | MSM, Hispanic, Florida (n = 294 internet-recruited) | Internet chat rooms. Recruitment 10/15/2003–12/19/2004 | Mean 32 | 100 % Hispanic | 75 % ≥ high school 44 % ≥ college/Bachelor’s degree |
| Frontiers in Prevention; Balan et al. [28] | MSM, internet-using, ‘barebacking’ interest, New York City metro (n = 89) | Instant messaging and e-mail blasts. Recruitment April 2005 – March 2006 | Mean 32 (SD 10) years, range 18–63 | 27 % White/European–American; 21 % African-American; 25 % Latino; 18 % Asian/Pacific Islander; 2 % native American; 7 % other | Not reported |
| Grov et al. [29] | MSM with new oral or anal sex partner at last encounter (n = 2865) | Banner Ads. Recruitment 2004–2005 | Median 38 (range 18–78) years | n = 2819: 80 % White, non-Hispanic; 4 % Black, non-Hispanic; 9 % Hispanic/Latino; 3 % Asian/Pacific Islander; 4 % Mixed/Other | Not reported |
| Healthy Young Men’s Study; Kubicek et al. [30] | MSM, aged 18–24 (n = 499) | Public venues. Recruitment dates NR | 29 % 18–19; 37 % 20–21; 34 % 22–24 | 38 % Caucasian; 23 % African American; 39 % Mexican descent | Not reported |
| HIVBIGDEAL pilot; Chiasson [31] | MSM (n = 1003) | Banner Ads. Recruitment October 2005 | n = 830: 22 % 18–29; 36 % 30–39; 42 % > 40 | n = 943: 72 % White; 6 % Black; 14 % Hispanic; 5 % Asian and Other; 2 % multiple | NR ≥ high school 51 % ≥ college/Bachelor’s degree |
| HIVBIGDEAL RCT; Margolis et al. [32] | MSM (n = 8040) | Banner Ad or e-mail. Recruitment April 2008-June 2008 | Median 39 (SD 11.7) (range 18–81) | n = 8004: 82 % White; 3 % Black; 8 % Hispanic; 2 % Asian or Native Hawaiian/Other Pacific Islander; 5 % mixed/other | NR ≥ high school 54 % ≥ college/Bachelor’s degree |
| Horvath et al. [33] | MSM, rural (n = 663) | Banner ads; Internet chat rooms, bulletin boards, groups, Ads, and In-person referrals. Enrollment January 2002 through June 2003 | 33 % 18–24; 27 % 25–34; 23 % 35–44; 18 % > 45 | n = 656: 90 % White; 10 % Non-White | NR ≥ high school 43 % ≥ college/Bachelor’s degree |
| Horvath et al. [34] | MSM (n = 2716) | Banner Ads. September to November 2005 | n = 2713 reported: 36 % 18–24; 25 % 25–29; 27 % 30–39; 9 % 40–49; 3 % ≥ 50 | 27 % White; 16 % Black; 25 % Latino; 19 % Asian; 13 % Other | Not reported |
| Horvath et al. [35] | MSM (n = 1725) | Banner Ads. 3.5 months in 2008 | 7 % 18–20; 41 % 21–30; 24 % 31–40; 28 % 41–70 | n = 1725: 76 % White;15 % Hispanic; 8 % Other | NR ≥ high school 52 % ≥ college/Bachelor’s degree |
| Horvath et al. Diary Studies; Horvath et al. [36] | MSM in Western states (n = 45) | Chat room profile; print Ad. Recruitment dates NR | 22 % 18–23; 11 % 24–27; 38 % 28–36; 29 % ≥ 37 |
76 % White; 24 % Non-White | NR ≥ high school 47 % ≥ college/Bachelor’s degree |
| Jozkowski et al. [37] | MSM (n = 25 159) | E-mail. Recruitment July 2009 | n = 24 900: 14 % 18–23; 18 % 24–29; 23 % 30–39; 28 % 40–49; 13 % 50–59; 3 % 60+ | n = 25 027: 82 % White; 4 % Black; 7 % Hispanic/Latino; 3 % Asian/Pacific Islander; 3 % Other | NR ≥ high school 54 % ≥ college/Bachelor’s degree |
| Khosropour, et al. [38] | MSM, Internet-using, with mobile phone (n = 710) | Banner ads. Recruitment August to December 2010 | 37 % 18–24; 37 % 25–34; 15 % 35–44; 11 % 45–54 | 66 % White; 15 % Black; 19 % Hispanic | Not reported |
| Khosropour and Sullivan [39] | MSM (n = 6104) | Banner ads. Recruitment August to December 2010 | 12 % 18–19; 30 % 20–24; 29 % 25–34; 15 % 35–44; 10 % 45–54; 3 % 55 + | 45 % White, Non-Hispanic; 23 % Black, Non-Hispanic; 15 % Hispanic; 4 % Asian/Pacific Islander; 2 % Native American/Alaska Native; 8 % Multiracial; 4 % other | 96 % ≥ high school 37 % ≥ college/Bachelor’s degree |
| MINTS-II; Wilkerson et al. [40] | MSM (n = 2578) | Banner ads. Recruited for 3 months during 2005 | n = 2575 reported: 37 % 18–24; 26 % 25–29; 26 % 30–39; 11 % > 40 | 25 % Latino American; 19 % Asian American; 16 % Black or African American; 27 % White; 13 % other | NR |
| MINTS-II Latino; Rosser et al. [41] | Latino (n = 1026) | Banner ads. Recruited November–December 2002 | Mean 28 (SD 9) | 100 % Latino | 80 % ≥ high school NR ≥ college/Bachelor’s degree |
| Mustanski [42] | MSM (n = 113) | Internet links. Recruitment dates not reported | 48 % 18–24;12 % 25–29; 20 % 30–39; 20 % > 40 | 85 % White, Non-Hispanic; 4 % Black; 3 % Hispanic; 8 % Other | 100 % ≥ high school 41 % ≥ college/Bachelor’s degree |
| Online Health and Technology Survey Baseline; Wagenaar, et al. [43] | MSM (n = 5980) | Banner ads. Recruitment March and April 2009 | 68 % 18–24; 16 % 25–29; 7 % 30–34; 7 % 35–45; 2 % (n = 135) > 45 | 43 % White, Non-Hispanic; 13 % Black, Non-Hispanic; 32 % Hispanic; 11 % other; 1 % unknown | 93 % ≥ high school 15 % ≥ college/Bachelor’s degree |
| Project SPIN; Grov, et al. [44] | MSM, Internet-using, sexually compulsive, in New York City (n = 183) | Pop-up and banner ads. Recruitment December 2012 | Mean 36 (SD 8) (Range 19–63) | 60 % White/European; 19 % African American; 1 % Arab/Middle Eastern; 2 % Asian/Pacific Islander; 19 % Hispanic/Latino | NR ≥ high school 63 % ≥ college/Bachelor’s degree |
| Rendina Jimenez, et al. [45] | MSM (n = 1351) | Online ads. Recruitment December 2012 | Mean 30 (range 18–67) years | 49 % White; 12 % Black; 21 % Hispanic/Latino; 6 % Asian/Pacific Islander; 10 % Multiracial; 2 % other | Not reported |
| Rucinski et al. [46] | MSM (n = 329) | E-mail blast. Recruitment October and November 2011 | 65 % 18–30; 35 % (31–40) | n = 324 reported: 51 % White, non-Hispanic; 19 %; Black, non-Hispanic; 15 % Hispanic; 15 % other | NR ≥ high school 77 % ≥ college/Bachelor’s degree |
| Schnarrs et al. [47] | MSM, Latino (n = 1880) | E-mail blast to online networkers. Recruitment dates not reported | n = 1861 24 % 18–24; 18 % 25–29; 29 % 30–39; 22 % 40–49; 6 % 50–59; 1 % > 60+ | 100 % Latino | 99 % ≥ high school 45 % ≥ college/Bachelor’s degree |
| Stephenson et al. [48] | MSM (n = 402) | Banner ads. Recruitment dates October and November 2010 | 68 %18–24; 21 % 25–29; 11 % 30–35 | 48 % White/Caucasian; 15 % Black/African American; 37 % Hispanic | 95 % ≥ high school NR ≥ college/Bachelor’s degree |
| Stephenson et al. [49] | MSM (n = 355 US residents) | Banner ads. Recruitment October 1 to November 30 2010 | n = 354: 60 % 18–24; 17 % 25–34; 8 % 35–44; 15 % > 45 | 83 % White; 17 % Other | NR |
| Wagenaar, Sullivan, et al. [50] | MSM (n = 1154 US residents) | Banner ads. Data collected March through April 2009 | Median 26 (IQR 20) | 48 % White non-Hispanic; 33 % Black/non-Hispanic; 9 % Hispanic; 9 % other | NR |
| Wall et al. [51] | MSM (n = 4620) | Banner ads; Data collected between March and July 2010 | 84 % 18–29; 11 % 30–39; 4 % 40–49; 1 % > 50 | 43 % White/Caucasian (non-Hispanic); 13 % Black/African American (non-Hispanic); 32 % Hispanic; 12 % other/unknown | 92 % ≥ high school 15 % ≥ college/Bachelor’s degree |
| Welles et al. [52] | MSM, used Internet to find sex partners (n = 682 US residents) | Banner ads. Recruitment dates not reported | 20 % 18–25; 33 % 26–35; 26 % 36–45; 21 % > 45 | Not reported | NR ≥ high school 53 % ≥ college/Bachelor’s degree |
| WHBS New York; Navejas [53]; Navejas et al. 54] | MSM (n = 1700) [53]; Sex past 12 months (n = 1124) [54] | Banner ads, chat rooms, e-mail. Recruitment April to August 2007 | Mean 29 (SD 9) years | 63 % White; 13 % Black; 29 % Hispanic; 6 % other | Not reported |
| WHBS San Francisco; Raymond et al. [55] | MSM (n = 723) | Banner ads, online message, email. Recruitment November 2003 to December 2004 | 9 % 18–20; 18 % 21–25; 18 % 26–30; 14 % 30–35; 13 % 36–40; 14 % 41–45; 8 % 46–50; 7 % > 50 | n = 716: 72 % Caucasian; 2 % African American; 13 % Latino; 8 % Asian; 0.4 % American Indian; 1 % Native Hawaiian/Pacific Islander; 2 % other; 2 % mixed race | NR ≥ high school 64 % ≥ college/Bachelor’s degree |
Numbers might not add to total in the ‘Target Population’ column because of missing or unknown data
The vast majority of included studies recruited participants and collected data entirely online; however, two included studies convened in-person focus groups in which participants indicated they used the Internet [30, 44]. Banner advertisements on social media web sites or web sites geared to MSM (including social networking, news, and sex-seeking sites) were most commonly used to recruit participants, although some studies used chat-based recruitment [25–27] or community-based recruitment [23, 44].
All studies enrolled MSM in the U.S., and most required that participants be at least 18 years old (see Table 2). The mean or median age reported by included studies was generally in their 30 s, and most participants self-identified as white. The majority of participants reported they were “homosexual” or “gay.” Income data for this review are difficult to generalize due to income not being reported, differences in income reporting methods, and lack of data on number of persons relying upon the respondent’s income.
Among studies reporting it, educational attainment was generally higher than among men aged 25 years and older in the United States. Two studies enrolling only Hispanic or Latino men reported high school graduation rates of 75 [27] and 80 % [41]; however, these rates are higher than the general U.S. Hispanic high school graduation rate of 67 % [56]. The remaining studies reported high school graduation rates of 90–100 %, which is higher than the overall U.S. rate of 88 %. Although a few studies reported college graduation rates as low as 15 % [50] and 17 % [51], most reported rates in the range of 40–60 %, which is higher than the national average of 33 %. As many participants in these samples were under the age of 25 and might be current college students, their overall level of education may be even greater than the U.S. on average, if adjusted for age.
Studies did not report on use of pharmaceutical pre-exposure prophylaxis (PrEP), with the exception of one study that reported 1.5 % use [46]. Included studies were conducted prior to the release of federal recommendations on PrEP in 2014 [57]. Characterization of participants’ sexual risk factors, STI diagnoses, and drug use was complicated by limited reporting among studies, and variation in reporting across studies (e.g., time frame represented, metric used).
Critical Appraisal of Evidence Base
Critical appraisal findings for this evidence base were consistent across studies, and were consistent with general limitations of Internet-based research. These findings are summarized in Table 3.
Table 3.
Assessment of evidence base using Joanna Briggs Institute’s critical appraisal of quantitative evidence tool for descriptive/case-series studies
| Item | Question | Answer | Comments |
|---|---|---|---|
| 1 | Was the study based on a random or pseudo-random sample? (We also considered selection of consecutive or total sample acceptable) | No | Convenience samples in all but two studies [33, 42] |
| 2 | Were the criteria for inclusion in the sample clearly defined? | Yes | Inclusion criteria reported |
| 3 | Were confounding factors identified, and strategies to deal with them stated? | Testing behavior outcomes: no | Factors other than chance alone (e.g., access to health care, risk behavior) among populations could have contributed to differences in observed testing behaviors among studies |
| Identification of factors associated with testing behaviors: yes | Studies usually implemented multivariate analyses to control for confounding effects of other factors when investigating demographic or other factors potentially associated with testing behaviors | ||
| 4 | Were outcomes assessed using objective criteria? | Yes | Outcomes of interest were all objective |
| 5 | If comparisons were being made, was there sufficient description of groups? | Not relevant | All behaviors and analyses were of single-group cohorts |
| 6 | Was follow-up carried out over a sufficient time period? | Not relevant | All samples were cross-sectional without follow-up (or baseline data were assessed as cross-sectional data) |
| 7 | Were the outcomes of people who withdrew described and included in the analysis? | No | There were generally high rates of survey non-completion, and insufficient data for researchers to compare completers to non-completers |
| 8 | Were outcomes measured in a valid and reliable way? | No | Testing behaviors and all data were self-reported. Some required recall (e.g., testing frequency within previous 12 months) |
| 9 | Were appropriate statistical analyses of testing behaviors and factors associated with them reported? (We also considered reporting of appropriate data to calculate testing behaviors acceptable) | Yes | Testing behaviors were reported as the proportion of respondents with that outcome divided by the total number. The studies that assessed factors associated with testing behaviors used regression analyses |
Sampling methods were non-probabilistic and were based on response to online advertisements, generally with low impression (advertisement views) to participation ratios, suggesting high degrees of participant self-selection (item 1). However, the vast majority of studies clearly delineated their participant inclusion criteria (item 2). We also assessed potential confounding (item 3). Although we included studies with different designs, we analyzed all of them as descriptive studies (i.e., for intervention studies we used pre-intervention baseline data). Therefore, all data on testing behaviors in the meta-analysis were unadjusted. Potential confounders influencing testing behaviors might include income, health insurance or other factors impacting financial access to testing. However, the subset of studies that assessed the association between covariates and testing behaviors generally used multivariate models that took into account such confounders. Testing patterns and covariates were objective measures (item 4). Some potential sources of bias were obviated by the fact that testing behaviors were determined in single group cross-sectional studies (items 5, 6, 7). Outcomes were self-reported and therefore subject to potential biases such as recall bias (item 8). Studies uniformly used appropriate statistical analyses to report testing behaviors or investigate factors associated with testing behaviors (item 9).
Outcomes
Ever Tested for HIV
Thirty included studies reported this outcome for 74,395 men. The proportion of Internet-using MSM who had ever tested for HIV (Fig. 2) ranged widely. In each study, between 66 % [42] and 95 % [44] had ever been tested for HIV. Heterogeneity testing confirmed these between study differences were substantial and larger than would be expected due to chance alone (I2 = 0.99, Q = 3303, p (Q) < 0.001). A Random-effects meta-analysis that provides for the pooling of heterogeneous data found that on average, 85 % (95 % CI 82–87 %) of the Internet-using MSM included in this review had been tested at least once within their lifetime. Having said this, the precision of this summary estimate should be considered with some degree of caution because of the high degree of between studies heterogeneity observed.
Fig. 2.
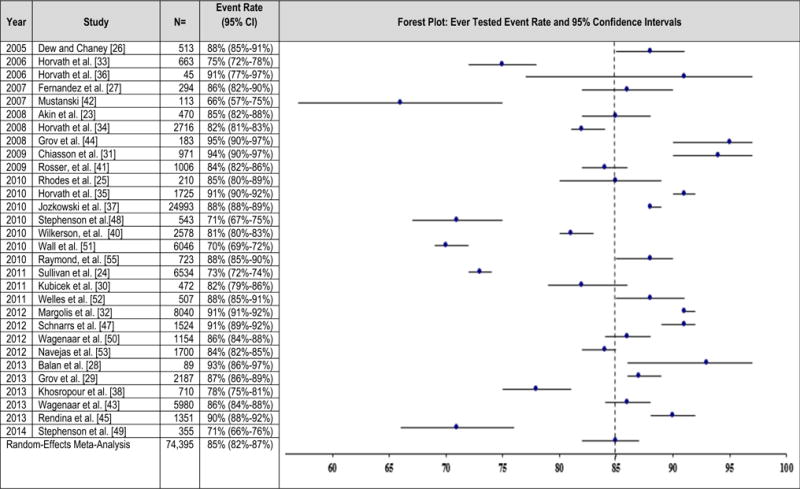
Ever tested for HIV within lifetime
We explored the observed between studies heterogeneity using variables extracted as potential covariates for HIV testing (see Data Collection) in a series of meta-regressions. The number of factors that could be assessed was limited by variability in the reporting of these covariates among included studies; per protocol we only assessed potential covariates reported by at least ten included studies. For most covariates, only a subset of studies reported needed data (κ = number of studies assessed). We investigated and did not find significant associations with any of the critical appraisal tool assessment items (κ = 30), year of study publication (κ = 30), or self-identification as white/European (κ = 29), black/African American (κ = 25), or Hispanic/Latino (κ = 26). Univariate analyses found significant associations for ever having tested for HIV with older age (proportion over 30 years) (κ = 15), college education (κ = 16), and self-identification as homosexual or gay (κ = 25). In multivariate models, we found that self-identification as homosexual or gay, the proportion over 30 years old, and the proportion who had at least a 4-year college diploma, remained significantly associated with ever having tested, but no interaction with race or year of publication was identified, respectively, for any factor. No additional multivariate regressions were possible due to insufficient numbers of studies reporting either of these two variables plus other variables in common.
Tested within Past 12 Months
Fourteen studies that enrolled a total of 36,158 MSM reported on the proportion of men who had been tested for HIV within the 12 months prior to participation in the study (Fig. 3). Estimates ranged widely across studies from 40 % [39] to 71 % [45, 46]. Pooling of these data using random-effects meta-analysis produced a summary effect size estimate of 58 % (95 % CI 53–63 %). Again, the precision of this summary estimate should be considered with some degree of caution because of the high degree of between-study heterogeneity observed (I2 = 0.99, Q = 1035, p(Q) < 0.001). Further, reporting of covariates was too limited to enable a thorough investigation of potential causes of this between studies heterogeneity. Univariate meta-regression analysis found no association with race or ethnicity (κ = 14), self-identification as homosexual or gay (κ = 13), critical appraisal assessment items (κ = 14), or year of study publication (κ = 14). Assessment of additional variables was not possible because too few studies reported our variables of interest, and multivariate analyses were not warranted due to lack of significant univariate findings.
Fig. 3.
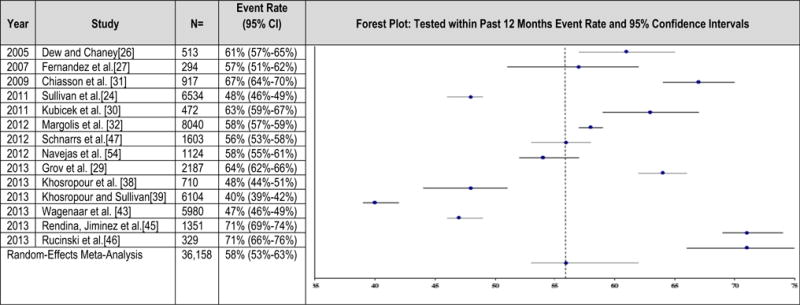
Tested for HIV within past 12 months
Additional Testing Outcomes
We found no evidence regarding the median or mean frequency of testing within the past 12 months or what specific types of HIV tests were used (e.g., rapid test or laboratory-based test). Mustanski et al. [58] reported all participants in their study had been tested in a clinic; however, testing location or setting type was not reported by any other study.
Factors Associated with HIV Testing
To identify demographic and other factors associated with HIV testing, we considered the findings of the meta-regressions (described above) and findings from individual studies that performed analyses on data from individual participants. Relatively few studies investigated factors associated with HIV testing, and only a small number of factors were investigated by more than one study. Findings from individual studies and the meta-regressions are shown in Table 4. Meta-regression and narrative analyses of findings from individual studies identified evidence that older age, self-identification as homosexual or gay, and not using drugs are associated with ever having tested for HIV. Data were sufficient for assessment of race/ethnicity, and CAI, but yielded inconclusive findings. Although no association was found (due to small numbers of studies and conflicting findings among them), the possibility that a relationship actually exists cannot be ruled out based on these data. We found no association between testing patterns and either year of publication or any of the critical appraisal assessment items. Investigation of additional factors for association with HIV testing was precluded by limited reporting.
Table 4.
Summary of factors investigated for association with HIV testing among internet-using MSM
| Factor | Overall assessment and strength of evidence | Testing outcome | Meta-regression findings | Individual studies’ findings (where reported) |
|---|---|---|---|---|
| Age | Younger age is associated with never testing for HIV (Moderate) but is not clearly associated with testing within the last 12 months (Inconclusive) | Ever tested | Proportion of participants age 30 years or younger was significantly associated with never testing (κ = 15, p = 0.016) | Margolis et al. found men 18–24 years were significantly less likely to have been tested (unadjusted and adjusted) [32] and Rendina et al. found increased age was associated with having ever tested (adjusted) [64] |
| Tested past year | Insufficient evidence to support investigation (κ < 10) | Rendina et al. 2013 found a statistically significant association between older age and having tested in the last year (adjusted) [45], and Schnarrs et al. found a similar but non-significant trend (unadjusted) [47] | ||
| Self-reported sexual orientation | Self-identification as Homosexual or Gay is associated with ever testing for HIV (Moderate). Inconsistent findings prevent determination of whether it is associated with testing in the past year (Inconclusive) | Ever tested | Ever testing was significantly associated with self-identification as homosexual (κ = 25, p = 0.014) | Margolis et al. and Rendina et al. [32, 45]. both found MSM who self-identified as gay or homosexual were more likely to have ever tested than those who self-identified as straight, heterosexual, or bisexual in both unadjusted and adjusted models |
| Tested past year | Testing in the past year was not significantly associated with self-identification as homosexual (κ = 14, P = 0.162) | While Schnarrs et al. 2012 found gay men were more likely to have tested than bisexual men (unadjusted OR) [47] Rendina et al. 2013 found no association (adjusted regression) [45] | ||
| Drug use | Drug use is associated with never testing for HIV, but this association does not appear to be independent (Low) | Ever tested | Insufficient evidence to support investigation due to variability in reporting methods | Margolis et al. 2012 and Rendina et al. 2013 [32, 45] found drug use, including noninjection drug use, in the last 2–3 months was significantly associated with never having tested in unadjusted but not adjusted models |
| Race/ethnicity | Race/ethnicity is not convincingly associated with ever testing or testing within the past year; however, there is insufficient evidence to rule this possibility out (Inconclusive) | Ever tested | No association was found between White/European (κ = 29), Black/African American (κ = 25), or Hispanic (κ = 26) self-identification and testing | Rendina et al. 2013 found MSM who reported being black or multicultural were more likely to have ever tested (adjusted) [45], while Margolis et al. 2012 [32] and Khosropour [38] found no association |
| Tested past year | No association was found between White/European American (κ = 14), Black/African American (κ = 14), or Hispanic (κ = 14) self-identification and testing | Neither Rendina et al. [45]. nor Khosropour et al. [38]. found statistically significant associations between race/ethnicity and having tested within the last 12 months, and Rendina et al. reported a non-significant trend toward black race/ethnicity being more likely to have tested in the last 12 months | ||
| Condomless anal intercourse (CAI) | The association between CAI and testing is too inconsistent to determine an association; however, the possibility of an association cannot be ruled out (Inconclusive) | Ever tested | Insufficient evidence to support investigation (κ < 10) | NA |
| Tested past year | Insufficient evidence to support investigation (κ < 10) | Rendina et al. 2013 found CAI in the last 3 months was significantly associated with testing within the last year (adjusted) [45], while Navejas et al. 2102 found no association between CAI in the past year and testing (unadjusted or adjusted) [54] | ||
| Quality assessment items | Methodological sources of potential bias are not convincingly associated with ever testing or associated with testing within the past year; however, there is insufficient evidence to rule this possibility out. (Inconclusive) | Ever tested | No association found for any factor (κ = 30; p > 0.05) | NA |
| Tested past year | No association found for any factor (κ = 14; p > 0.05) | NA | ||
| Year of study publication | No association identified, but insufficient evidence to conclude there is no association. (Inconclusive) | Ever tested | No association (κ = 30; p > 0.05) | NA |
| Tested past year | No association (κ = 14; p > 0.05) | NA | ||
| Education | This meta-regression and one study found college education was associated with ever testing; no studies reported contradictory findings (Low) | Ever tested | Completing a 4-year/Bachelor’s degree was significantly associated with having ever tested. (κ = 30; p = 0.002). Insufficient evidence to assess other education levels | Margolis et al. reported the rate of never testing was higher among college graduates (6 %) than those with less education (12 %), OR 1.24 (95 % 1.02–1.51), even after adjusting for confounding factors (OR 2.2 (95 % CI: 1.72–2.37) [32] |
| One study among Latino men only found no association between testing in the past year and college graduation, which is an insufficient amount of evidence to support a conclusion. (Inconclusive) | Tested past year | Insufficient evidence to support investigation (κ < 10) | Among a Latino-only population, Schnarrs found no relationship with college graduation and having tested in the past year [47] | |
| Income | One study identified an association with low income and never having tested, but this is an insufficient amount of evidence to draw a conclusion from (Inconclusive) | Ever tested | Insufficient evidence to support investigation (κ < 10) | Horvath (2008) reported that men earning less than $10,000/year were less likely to have ever tested [34] |
| Tested past year | Insufficient evidence to support investigation (κ < 10) | NA |
NA not applicable
Conclusions and Discussion
A random-effects meta-analysis found that 85 % of participating Internet-using MSM had been tested for HIV at least once in their life, and 58 % had been tested in the year preceding study participation. The proportion of men testing annually in our analysis was lower compared to a recent national estimate of men in venue-based settings (71 %) [59] but higher than the rate of annual testing from a national probability sample of MSM (42 %) [60]. Internet-using MSM who may be less likely to have tested within their lifetimes include those who self-identify as heterosexual or bisexual, those under age 30, those with less educational attainment than a college degree, and those who use any drugs, including non-injection drugs. Our findings were consistent across two data types (meta-analysis of multiple studies and narrative analysis of individual-level findings from multiple individual studies). Due to insufficient amounts of evidence or conflicting evidence, no additional factors associated with HIV testing patterns were identified.
Our finding of lower rates of HIV testing among non-gay identified men is consistent with other studies [61–65]. Non-gay identified MSM may be more likely to meet sexual partners online compared to those who are gay identified, and therefore could benefit from internet-based interventions such as online motivational videos to encourage testing [66]. Reaching non-gay identified MSM on the internet, however, has its challenges; some studies have found that non-gay identified MSM, especially minority men, may be less likely to click on banner advertisements, a common method used to advertise HIV-related prevention services online [67]. In off-line settings, ensuring HIV testing is a part of routine health care is another way that non-gay identified MSM may be reached for testing [61].
Our analysis also found that younger MSM were less likely to have tested for HIV, a finding supported by HIV surveillance data and studies that have found young MSM have higher rates of undiagnosed HIV infection compared to older MSM [68, 69]. Young MSM may be less likely to test for HIV for a number of reasons, including perceiving themselves at low risk for HIV infection or lacking access to health services, including culturally appropriate services inclusive of LGRTQ youth. Young MSM use the internet to seek out health information and support [70] and may benefit from tailored prevention interventions and content directed towards young men, including setting up health promotion pages on popular social networking sites, and the development of mobile apps or text-messaging services [71].
Having at least a college education has also been previously linked to higher testing rates, possibly due to other socioeconomic factors for which there was insufficient evidence to test for associations such as higher income or having health insurance. For instance, men who have financial means to test but do not wish to visit clinics or healthcare providers due to concerns about privacy, stigma, or due to inconvenience may be more receptive to testing at home with a kit purchased online [72–74].
Evidence associating drug use with having ever tested is weaker because it comes only from primary studies; however, this association is plausible because drug use is a recognized risk factor for HIV, and is associated with increased sexual risk through intoxication and infection by direct parenteral viral transmission, in the case of injection drug use. Data to estimate testing rates stratified by these characteristics were not reported in the original studies; based upon these data it is not possible to estimate testing rates for MSM by subgroup.
Our findings are subject to several limitations. First, there is the potential for sampling bias due to convenience sampling, low solicitation-to-participation rates, and self-selection of participants. Second, data biases due to duplicate or fraudulent response may be present, are difficult to identify in Internet-based research, and may be more likely where incentives are offered. Third, misclassification bias may be present due to misinformed or disingenuous reporting of HIV status and risk behaviors. The effect, if any, of these limitations on testing pattern outcomes in this review is unknown. At this time there appear to be systematic differences between MSM recruited through Internet and MSM recruited through community venues, and we do not suggest these findings be generalized.
Despite these limitations, our findings highlight the importance of devoting resources toward online interventions and testing technologies, as growth of the Internet, social networking websites, and mobile technology have increased especially among the young and minorities. Further research into barriers to using the internet as a method for distributing HIV home test kits, or other interventions or messages to increase testing opportunities for Internet-using MSM, are needed. For instance, men who are motivated to get an HIV test but do not wish to visit clinics or healthcare. Public health officials should investigate ways to provide HIV home tests for MSM who cannot afford to purchase them, and to improve opportunities to link MSM who test HIV-positive to medical care [75]. Future research should also consider changes in demographics of Internet users and the impact of interventions such as PreP [57].
The overall findings of our systematic review are encouraging; however, a subpopulation of MSM may benefit from online interventions such as provision of HIV self-testing kits, delivery of online content encouraging HIV testing and tailored prevention messages to young MSM to take advantage of the increasingly central role that the internet plays in the U.S. and particularly in the MSM community.
Supplementary Material
Acknowledgments
Funding This work was funded by the Centers for Disease Control and Prevention under contract 200-2010-37417 awarded to MANILA Consulting Group, Inc.
Footnotes
Electronic supplementary material The online version of this article (doi:10.1007/s10461-016-1506-7) contains supplementary material, which is available to authorized users.
Conflict of Interest None of the authors declare any potential conflicts of interest.
Disclaimer The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Ethical Approval This article does not contain any studies with human participants or animals performed by any of the authors.
References
- 1.CDC, diagnoses of HIV infection in the United States and dependent areas. HIV surveillance report. 2014 http://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-us.pdf. Accessed 26 May 2016.
- 2.CDC. CDC Fact Sheet: HIV among gay and bisexual men. https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/cdc-msm-508.pdf. Accessed 26 May 2016.
- 3.Sullivan PS, et al. Successes and challenges of HIV prevention in men who have sex with men. Lancet. 2012;380(9839):388–99. doi: 10.1016/S0140-6736(12)60955-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Branson BM, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006;55(RR-14):1–17. quiz CE1–4. [PubMed] [Google Scholar]
- 5.Saxton P, Dickson N, Hughes A. Who is omitted from repeated offline HIV behavioural surveillance among MSM? Implications for interpreting trends. AIDS Behav. 2013;17(9):3133–44. doi: 10.1007/s10461-013-0485-1. [DOI] [PubMed] [Google Scholar]
- 6.Sanchez T, et al. Internet-based methods may reach higher-risk men who have sex with men not reached through venue-based sampling. Open AIDS J. 2012;6:83–9. doi: 10.2174/1874613601206010083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Icard LD. Reaching African-American men on the down low: sampling hidden populations: implications for HIV prevention. J Homosex. 2008;55(3):437–49. doi: 10.1080/00918360802345198. [DOI] [PubMed] [Google Scholar]
- 8.Rhodes SD, Bowie DA, Hergenrather KC. Collecting behavioural data using the world wide web: considerations for researchers. J Epidemiol Commun Health. 2003;57(1):68–73. doi: 10.1136/jech.57.1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Martinez O, et al. Still a hard-to-reach population? Using social media to recruit Latino gay couples for an HIV intervention adaptation study. J Med Internet Res. 2014;16(4):e113. doi: 10.2196/jmir.3311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chiasson MA, Hirshfield S, Rietmeijer C. HIV prevention and care in the digital age. J Acquir Immune Defic Syndr. 2010;55(Suppl 2):S94–7. doi: 10.1097/QAI.0b013e3181fcb878. [DOI] [PubMed] [Google Scholar]
- 11.EMIS. Findings from 38 Countries. European Centre for Disease Prevention and Control; 2013. 2010: The European Men-Who-Have-Sex-With-Men Internet Survey. http://ecdc.europa.eu/en/publications/_layouts/forms/Publication_DispForm.aspx?List=4f55ad51-4aed-4d32-b960-af70113dbb90&ID=760. [Google Scholar]
- 12.Moher D, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The Joanna Briggs Institute. Reviewer’s Manual. 2011. The Joanna Briggs Institute; 2011. [Google Scholar]
- 14.Raudenbush SJ. Analyzing effect sizes: random-effects models. In: Cooper H, Hedges LV, Valentine JC, editors. The handbook of research synthesis and meta-analysis. New York: The Russell Sage Foundation; 2009. pp. 295–316. [Google Scholar]
- 15.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 16.Shadish WR, Haddock CK. Combining estimates of effect sizes. In: Cooper H, Hedges LV, Valentine JC, editors. The handbook of research synthesis and meta-analysis. New York: Russell Sage Foundation; 2009. pp. 257–77. [Google Scholar]
- 17.Harbord RM, Higgins JPT. Meta-regression in Stata. Stata J. 2008;8(4):493–519. http://www.stata-journal.com/sjpdf.html?articlenum=sbe23_1. [Google Scholar]
- 18.Laupacis A, Sekar N, Stiell IG. Clinical prediction rules. A review and suggested modifications of methodological standards. JAMA. 1997;277(6):488–94. [PubMed] [Google Scholar]
- 19.Peduzzi P, et al. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49(12):1373–9. doi: 10.1016/s0895-4356(96)00236-3. [DOI] [PubMed] [Google Scholar]
- 20.Treadwell JR, et al. A system for rating the stability and strength of medical evidence. BMC Med Res Methodol. 2006;6:52. doi: 10.1186/1471-2288-6-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guyatt GH, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Atkins D, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328(7454):1490. doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Akin M, et al. HIV risk behaviors of Latin American and Caribbean men who have sex with men in Miami, Florida, USA. Rev Panam Salud Publica. 2008;23(5):341–8. doi: 10.1590/s1020-49892008000500006. [DOI] [PubMed] [Google Scholar]
- 24.Sullivan PS, et al. Bias in online recruitment and retention of racial and ethnic minority men who have sex with men. J Med Internet Res. 2011;13(2):e38. doi: 10.2196/jmir.1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rhodes SD, Hergenrather KC, Duncan J, Vissman AT, Miller C, Wilkin AM, Stowers J, Eng E. A pilot intervention utilizing Internet chat rooms to prevent HIV risk behaviors among men who have sex with men. Public Health Rep. 2010;125(Suppl 1):29–37. doi: 10.1177/00333549101250S105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dew BJ, Chaney MP. The relationship among sexual compulsivity, internalized homophobia, and HIV at-risk sexual behavior in gay and bisexual male users of internet chat rooms. Sex Addict Compuls. 2005;12(4):259–73. [Google Scholar]
- 27.Fernandez MI, et al. Cruising in cyber space: comparing Internet chat room versus community venues for recruiting Hispanic men who have sex with men to participate in prevention studies. J Ethn Subst Abuse. 2007;6(2):143–62. doi: 10.1300/J233v06n02_09. [DOI] [PubMed] [Google Scholar]
- 28.Balan IC, et al. Are HIV-negative men who have sex with men and who bareback concerned about HIV infection? Implications for HIV risk reduction interventions. Arch Sex Behav. 2013;42(2):279–89. doi: 10.1007/s10508-011-9886-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grov C, et al. Exploring the venue’s role in risky sexual behavior among gay and bisexual men: an event-level analysis from a national online survey in the US. Arch Sex Behav. 2013;42(2):291–302. doi: 10.1007/s10508-011-9854-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kubicek K, et al. Use and perceptions of the internet for sexual information and partners: a study of young men who have sex with men. Arch Sex Behav. 2011;40(4):803–16. doi: 10.1007/s10508-010-9666-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chiasson MAS, Shaw FS, Humberstone M, Hirshfield S, Hartel D. Increased HIV disclosure 3 months after an online video intervention for men who have sex with men (MSM) AIDS Care. 2009;21(9):1081–9. doi: 10.1080/09540120902730013. [DOI] [PubMed] [Google Scholar]
- 32.Margolis ADJ, Joseph H, Belcher L, Hirshfield S, Chiasson MA. ‘Never testing for HIV’ among men who have sex with men recruited from a sexual networking website, United States. AIDS Behav. 2012;16(1):23–9. doi: 10.1007/s10461-011-9883-4. [DOI] [PubMed] [Google Scholar]
- 33.Horvath KJ, Bowen AM, Williams ML. Virtual and physical venues as contexts for HIV risk among rural men who have sex with men. Health Psychol. 2006;25(2):237–42. doi: 10.1037/0278-6133.25.2.237. [DOI] [PubMed] [Google Scholar]
- 34.Horvath KJ, Oakes JM, Rosser BR. Sexual negotiation and HIV serodisclosure among men who have sex with men with their online and offline partners. J Urban Health. 2008;85(5):744–58. doi: 10.1007/s11524-008-9299-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Horvath KJ, Weinmeyer R, Rosser S. Should it be illegal for HIV-positive persons to have unprotected sex without disclosure? An examination of attitudes among US men who have sex with men and the impact of state law. AIDS Care. 2010;22(10):1221–8. doi: 10.1080/09540121003668078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Horvath KJ, Beadnell B, Bowen AM. Sensation seeking as a moderator of Internet use on sexual risk taking among men who have sex with men. Sex Res Soc Policy. 2006;3(4):77–90. [Google Scholar]
- 37.Jozkowski K, et al. Relations between circumcision status, sexually transmitted infection history, and HIV serostatus among a national sample of men who have sex with men in the United States. AIDS Patient Care STDS. 2010;24(8):465–70. doi: 10.1089/apc.2010.0082. [DOI] [PubMed] [Google Scholar]
- 38.Khosropour CM, Johnson BA, Ricca AV, Sullivan PS. Enhancing retention of an Internet-based cohort study of men who have sex with men (MSM) via text messaging: randomized controlled trial. J Med Internet Res. 2013;15(8):e194. doi: 10.2196/jmir.2756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wagenaar BH, et al. Do Men who have Sex with Men (MSM) in the United States understand that HIV Serodiscordance is possible? Open AIDS J. 2013;7:14–6. doi: 10.2174/1874613620130513001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wilkerson JM, Smolenski DJ, Horvath KJ, Danilenko GP, Rosser BRS. Online and offline sexual health-seeking patterns of HIV-negative men who have sex with men. AIDS Behav. 2010;14(6):1362–70. doi: 10.1007/s10461-010-9794-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rosser BR, Miner MH, Bockting WO, Ross MW, Konstan J, Gurak L, Stanton J, Edwards W, Jacoby S, Carballo-Dieguez A, Mazin R, Coleman E. HIV risk and the internet: results of the Men’s INTernet Sex (MINTS) Study. AIDS Behav. 2009;13(4):746–56. doi: 10.1007/s10461-008-9399-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mustanski BS. Are sexual partners met online associated with HIV/STI risk behaviours? Retrospective and daily diary data in conflict. AIDS Care. 2007;19(6):822–7. doi: 10.1080/09540120701237244. [DOI] [PubMed] [Google Scholar]
- 43.Wagenaar BH, Christiansen-Lindquist L, Khosropour C, Salazar LF, Benbow N, Prachand N, Sineath RC, Stephenson R, Sullivan PS. Willingness of US men who have sex with men (MSM) to participate in Couples HIV Voluntary Counseling and Testing (CVCT) PLoS One. 2012;7(8):e42953. doi: 10.1371/journal.pone.0042953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Grov C, et al. Exploring the internet’s role in sexual compulsivity and out of control sexual thoughts/behaviour: a qualitative study of gay and bisexual men in New York City. Cult Health Sex. 2008;10(2):107–25. doi: 10.1080/13691050701564678. [DOI] [PubMed] [Google Scholar]
- 45.Rendina HJ, Jimenez RH, Grov C, Ventuneac A, Parsons JT. Patterns of lifetime and recent HIV testing among men who have sex with men in New York City who use Grindr. AIDS Behav. 2013;18(1):41–9. doi: 10.1007/s10461-013-0573-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rucinski K, et al. Knowledge and use of pre-exposure prophylaxis among an online sample of young men who have sex with men in New York City. AIDS Behav. 2013;17(6):2180–4. doi: 10.1007/s10461-013-0443-y. [DOI] [PubMed] [Google Scholar]
- 47.Schnarrs PW, Rosenberger JG, Schick VR, Novak DS, Herbenick D, Reece M. Gay and bisexual Latino men’s sexual health and behaviors: a national online sample. Int J Men’s Health. 2012;11(1):22–35. [Google Scholar]
- 48.Stephenson R, Khosropour C, Sullivan P. Reporting of intimate partner violence among men who have sex with men in an online survey. West J Emerg Med. 2010;11(3):242–6. [PMC free article] [PubMed] [Google Scholar]
- 49.Stephenson R, et al. Willingness to use couples voluntary counseling and testing services among men who have sex with men in seven countries. AIDS Care. 2013;26(2):191–8. doi: 10.1080/09540121.2013.808731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wagenaar BH, Sullivan PS, Stephenson R. HIV knowledge and associated factors among internet-using men who have sex with men (MSM) in South Africa and the United States. PLoS One. 2012;7(3):e32915. doi: 10.1371/journal.pone.0032915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wall KM, Khosropour CM, Sullivan PS. Offering of HIV screening to men who have sex with men by their health care providers and associated factors. J Int Assoc Phys AIDS Care (Chic) 2010;9(5):284–8. doi: 10.1177/1545109710379051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Welles S, Ross M, Banik S, Fisher L, McFarlane M, Kachur R, Rietmeijer C, Allensworth-Davies D. Demographic and sexual behavior comparisons of Indian and U.S. Internet samples of men who have sex with men. Int J Sex Health. 2011;23(2):90–101. [Google Scholar]
- 53.Navejas M. Sexual risk among men who have sex with men with online sex partners in New York city: Insight using the centers for disease control and prevention’s Web-Based HIV Behavioral Surveillance and national HIV Behavioral Surveillance. ProQuest Information & Learning; US: 2013. [Google Scholar]
- 54.Navejas MN, Neaigus A, Torian L, Murrill C. Participation in online and offline HIV prevention among men who have sex with men who use the internet to meet sex partners in New York City. AIDS Behav. 2012;16(2):389–95. doi: 10.1007/s10461-011-9934-x. [DOI] [PubMed] [Google Scholar]
- 55.Raymond HF, et al. Comparing internet-based and venue-based methods to sample MSM in the San Francisco bay area. AIDS Behav. 2010;14(1):218–24. doi: 10.1007/s10461-009-9521-6. [DOI] [PubMed] [Google Scholar]
- 56.Ryan CL, Bauman K. Educational Attainment in the United States: 2015. U.S. Census Bureau; 2016. https://www.census.gov/content/dam/Census/library/publications/2016/demo/p20-578.pdf. [Google Scholar]
- 57.USPHS, United States Public Health Service. Preexposure prophylaxis for the prevention of HIV infection in the United States—2014 clinical practice guideline. 2014 http://www.cdc.gov/hiv/pdf/prepguidelines2014.pdf.
- 58.Mustanski B, Garofalo R, Monahan C, Gratzer B, Andrews R. Feasibility, acceptability, and preliminary efficacy of an online HIV prevention program for diverse young men who have sex with men: the keep it up! intervention. AIDS Behav. 2013;17(9):2999–3012. doi: 10.1007/s10461-013-0507-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.CDC. Men Who Have Sex With Men—National HIV Behavioral Surveillance, 20 US Cities. HIV Surveillance Special Report 15. 2014 http://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-hssr-nhbs-msm-2014.pdf Accessed 22 June 2016.
- 60.Kwan CK, Rose CE, Brooks JT, Marks G, Sionean C. HIV Testing Among Men at Risk for Acquiring HIV Infection Before and After the 2006 CDC Recommendations. 131:311–319. doi: 10.1177/003335491613100215. http://www.publichealthreports.org/issueopen.cfm?articleID=3505 Accessed 26 May 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Reilly KH, Neaigus A, Jenness SM, Wendel T, Marshall DM, 4th, Hagan H. Factors associated with recent HIV testing among men who have sex with men in New York City. AIDS Behav. 2014;18(Suppl 3):297–304. doi: 10.1007/s10461-013-0483-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Conway DP, Holt M, Couldwell DL, Smith DE, Davies SC, McNulty A, Keen P, Cunningham P, Guy R. Barriers to HIV testing and characteristics associated with never testing among gay and bisexual men attending sexual health clinics in Sydney. J Int AIDS Soc. 2015;18:20221. doi: 10.7448/IAS.18.1.20221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lauby JL, Milnamow M. Where MSM have their first HIV test: differences by race, income, and sexual identity. Am J Mens Health. 2009;3(1):50–9. doi: 10.1177/1557988307313465. [DOI] [PubMed] [Google Scholar]
- 64.Pathela P, Hajat A, Schillinger J, Blank S, Sell R, Mostashari F. Discordance between sexual behaviour and self-reported sexual identity: a population-based survey of New York City men. Ann Intern Med. 2006;146(6):416–25. doi: 10.7326/0003-4819-145-6-200609190-00005. [DOI] [PubMed] [Google Scholar]
- 65.Van Handel M, Lyons B, Oraka E, Nasrullah M, DiNenno E, Dietz P. Factors associated with time Since last HIV test among persons at high risk for HIV infection, National Survey of Family Growth, 2006–2010. AIDS Patient Care STDS. 2015;29(10):533–40. doi: 10.1089/apc.2015.0078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Blas MM, Alva I, Carcamo CP, Cabello R, Goodreau SM, Kimball AM, Kurth AE. Effect of an online video-based intervention to increase HIV testing in men who have sex with men in Peru. PLoS One. 2010;5(5):e10448. doi: 10.1371/journal.pone.0010448. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2862715/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sullivan PS, Khosropour CM, Luisi N, Amsden M, Coggia T, Wingood GM, DiClemente RJ. Bias in online recruitment and retention of racial and ethnic minority men who have sex with men. J Med Internet Res. 2011;13:e38. doi: 10.2196/jmir.1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.CDC, CDC Fact Sheet. HIV Among Youth. http://www.cdc.gov/hiv/group/age/youth/. Accessed 24 June 2016.
- 69.Balaji AB, Bowles KE, Le BC, Paz-Bailey G, Oster AM. High HIV incidence and prevalence and associated factors among young MSM, 2008. AIDS. 2008;27(2):269–78. doi: 10.1097/QAD.0b013e32835ad489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mustanski B, Lyons T, Garcia SC. Internet use and sexual health of young men who have sex with men: a mixed-methods study. Arch Sex Behav. 2010 doi: 10.1007/s10508-009-9596-1. http://www.impactprogram.org/wp-content/uploads/2010/02/Mustanski-Lyons-Garcia-2010.pdf Accessed 24 June 2016. [DOI] [PMC free article] [PubMed]
- 71.National Alliance of State and Territorial AIDS Directors. Reaching them where they are: a guide for using online and social media to conduct sexual health outreach with youth. 2012 http://hiv.rutgers.edu/wp-content/uploads/2016/05/YouthSocialMediaGuidance-1.pdf. Accessed 24 June 2016.
- 72.Chiu CJ, Young SD. Correlates of requesting home HIV self-testing kits on online social networks among African-American and Latino men who have sex with men. AIDS Care. 2016;28(3):389–93. doi: 10.1080/09540121.2015.1090533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Elliot E, Rossi M, McCormack S, McOwan A. Identifying undiagnosed HIV in men who have sex with men (MSM) by offering HIV home sampling via online gay social media: a service evaluation. Sex Transm Infect. 2016 doi: 10.1136/sextrans-2015-052090. ePub ahead of print. [DOI] [PubMed] [Google Scholar]
- 74.Grov C, Cain D, Whitfield TH, Rendina HJ, Pawsob M, Ventuneac A, Parsons JT. Recruiting a U.S. national sample of HIV-negative gay and bisexual men to complete at-home self-administered HIV/STI testing and surveys: challenges and Opportunities. Sex Res Soc Policy. 2016;13(1):1–21. doi: 10.1007/s13178-015-0212-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chavez RPMR, Wesolowski LG, Freeman A, Higa DH, Raiford J, Johnson WD, Margolis A, Belcher L, Ethridge S, Borkowf CB, Owen SM, McNaughten AD, Branson BM. Evaluation of rapid HIV self-testing among men who have sex with men (MSM) in high prevalence cities: the eSTAMP Project. Poster Presentation at 2015 HIV diagnostics conference; Atlanta GA. March 21–24, 2016; https://custom.cvent.com/ADE0EB81B3184D618E2FB8340F1EC28E/files/1a95ece7f4af40708a553b9df48f03ea.pdf. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


