Abstract
Objectives
To determine the proportion of diabetic patients who develop adverse glycaemic events when fasting regularly.
Design
Prospective observational study conducted at a tertiary care hospital in South Asia. Five hundred and twenty-three patients were assessed for eligibility, and 150 were included in the final analysis. Diabetic patients over 18 years of age who were willing to fast regularly and make a chart of their daily blood sugar levels were included in the study. The main outcome measures were hypoglycaemic and hyperglycaemic events. Frequencies and percentages were calculated for quantitative variables, while mean±SD were documented for qualitative variables. Relative risk was calculated as a measure of association.
Results
Of a total of 150 individuals, 10% experienced hypoglycaemia, while 3.3% reported hyperglycaemic episodes. Only 8.7% of the participants discontinued one or more fasts; however, none of them required hospitalisation. There is a negative association between a visit to a physician by diabetic patients before they begin to fast regularly and the risk of developing hypoglycaemia (relative risk 0.73).
Conclusions
Many diabetic patients who fast regularly are at high risk of adverse glycaemic events. Most diabetics do not consult their physicians before fasting to adjust medications and lifestyle. Various strategies should be planned and implemented for the awareness and education of such patients to avoid adverse glycaemic events and subsequent complications.
Key questions.
What is already known about this topic?
Retrospective studies show that there is an increase in symptomatic hyperglycaemia and hypoglycaemia in diabetic patients while fasting regularly.
What are the new findings?
This prospective study showed that 1 in 10 diabetic patients experienced hypoglycaemia while fasting regularly and 1 in 3 such patients did not discontinue fasting. About 1 in 30 diabetic patients who fasted developed hyperglycaemia. A pre-Ramadan visit to a physician by diabetic patients who intended to fast decreased the risk of developing hypoglycaemia compared with those who did not have a medical consultation.
Blood sugar levels determined using a glucometer, rather than symptoms, were used to define hyperglycaemia and hypoglycaemia in this study.
Recommendations for policy
A variety of awareness strategies should be planned to educate diabetic patients about glucose monitoring, diet, lifestyle and medication during the month of fasting. Diabetic patients should undergo pre-Ramadan assessment and be counselled by healthcare providers. It is also necessary to educate the family or caregivers of diabetic patients who wish to fast.
There is a need to conduct more research in this area, especially prospective large-scale multicentred studies, and efforts should be made to formulate formal guidelines to manage such patients. Moreover, interventional studies are required to discover more about the optimum dosage of medications during fasting. Non-pharmacological aspects such as diet and exercise should also be studied.
Introduction
It is estimated that 50 million people with diabetes fast each year.1 It is obligatory on all healthy Muslim adults to fast in Ramadan, the 9th month of the lunar calendar. Ramadan can last for either 29 or 30 days a year and involves abstinence from food, water, beverages, oral medications, smoking and coitus from sunrise till sunset. Generally, two major meals accompany Ramadan, one is consumed before dawn, called ‘Suhur’, and the other, at sunset, known as ‘Iftar’. The length of the fast varies from ∼11 to 20 hours, depending on the season and the geographical location. Sick people, especially those who can be adversely affected by fasting, are exempted from this duty by the Qur'an.2 Although diabetic patients are prone to hyperglycaemia and hypoglycaemia (hyper/hypoglycaemia), many still insist on fasting. A large, multicentred, retrospective study, the EPIDIAR study, has shown that 43% of people with type 1 diabetes and 79% of people with type 2 diabetes fast during the month of Ramadan.3 Findings from the same study revealed that, during Ramadan, the frequency of severe hypoglycaemic events increases up to 7.5-fold, and the frequency of severe hyperglycaemic events increases up to fivefold, in patients with diabetes. Uysal et al4 also found an increase in symptomatic hypoglycaemia in diabetic patients during Ramadan. Diabetic patients who fast tend to make the decision of whether to fast or not without discussing it with their physician.5 The EPIDIAR study also found that only 62% of the patients had received advice from their physicians regarding fasting during Ramadan. These figures show that a large percentage of diabetic Muslims fast during Ramadan and they do not receive adequate guidance from their physician, which may be due to either a lack of discussion between the patient and the physician on the topic or the lack of research evidence on the subject.
There is sufficient, but contradictory, evidence on the effect of fasting on the biochemical variables of diabetics.6 However, pragmatic prospective studies evaluating clinically relevant events in diabetic patients who fast are relatively scarce. Most of the studies are either small scale, recruiting even fewer than 60 subjects,4 7 8 or retrospective,3 9 10 and thus formal guidelines on this subject are absent. Clinically relevant events, including hyper/hypoglycaemic events and hospitalisation, should ultimately guide clinical practice, rather than changes in biochemical variables. This study was designed to fill this gap in the literature. It is a prospective study aimed to determine the proportion of diabetic patients who develop hyper/hypoglycaemic episodes, discontinue fasting, or need hospitalisation or an emergency room visit due to adverse glycaemic events while fasting regularly during the month of Ramadan.
Methods
Study setting and design
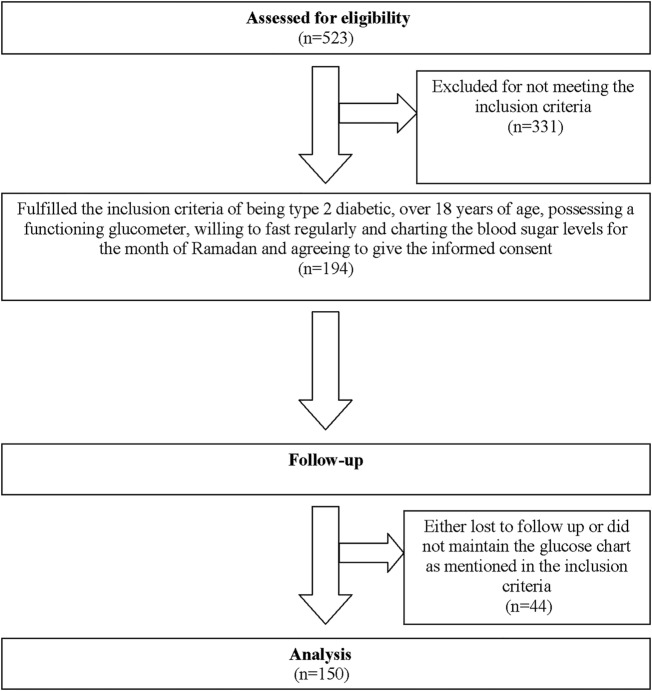
This prospective observational study was conducted at the endocrinology clinic of a tertiary care hospital in Islamabad (Pakistan). We used the patient database at our endocrinology clinic to contact patients by telephone. Five hundred and twenty-three patients were assessed for inclusion in the study. Finally, 150 were included in the analysis. Figure 1 shows the flow diagram of the study participants.
Figure 1.
Flow diagram of study participants.
The sample size was calculated using the sample size calculator for a proportion or descriptive study at http://www.openepi.com (OpenEpi V.3),11 keeping 90% CI. Population size was set as 1 million. Confidence limit was set as 5%. The EPIDIAR study estimated that 86% of patients with type 2 diabetes fast in Ramadan, so the anticipated percentage frequency was set as 86%. The sample size was calculated to be 131. The sample size calculator used the following formula:
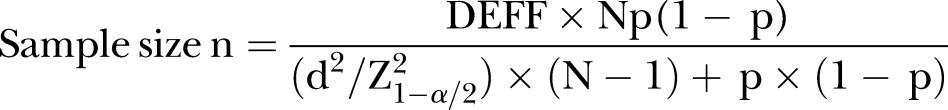 |
Inclusion and exclusion criteria
Patients over 18 years of age with type 2 diabetes mellitus for more than a year, who had a functioning glucometer at home, who could maintain a regular chart of their blood sugar for the month of Ramadan, and who were willing to give informed consent were included in the study. The exclusion criteria were as follows:
could not monitor or chart their blood sugar
could not be reached by telephone
not willing to take part in the study
was an endocrinologist.
Ethics considerations
The study was carried out in accordance with the Declaration of Helsinki and was approved by the institutional review board and ethics committee of our hospital. Fully informed verbal consent was obtained from each participant and documented before the administration of the questionnaire. Before acceptance, the research protocol was extensively reviewed for ethical assurance and ‘oral consent’ was given by the ethics committee, as the study did not pose serious harm to the study population and there was no face-to-face interaction between the researchers and the respondents.
Data collection
Telephone interviews were conducted with the participants at the start and end of the month of Ramadan by a group of medical students using a preformed standardised questionnaire. Three medical students from the same medical school in the clinical years conducted the interviews. Before the study, the questionnaire and the nature of the study were discussed thoroughly with the medical students. These students were trained to administer the questionnaire during two training sessions. Each training session lasted about 40 min. The students then conducted 10 interviews each as a pilot survey. There was a follow-up session lasting about an hour during which concerns of all three interviewers were addressed and they were further trained to maintain uniformity while carrying out interviews. Only the questions listed in the protocol were asked.
Data collected included demographic data, duration of disease, type of medication, adjustments made to the medication, hypoglycaemic events, hyperglycaemic events, number of fasts broken, need for hospitalisation or emergency room visit due to diabetes, and whether a healthcare provider was consulted before fasting.
The participants were requested to measure their blood glucose levels using a glucometer twice a day, with one reading in the fasting state and one reading at a random time, for at least 15 fasting days. The values were charted by the patients and were later communicated to the researchers at the end of the month. A chart to record blood glucose levels was sent via email. The participants were also requested to report any hypo/hyperglycaemic events, the number of fasts broken, and whether they had to visit an emergency room or required hospitalisation due to adverse glycaemic events. For the purpose of this study, regular fasting was defined as observing a fast for 15 or more days.
Hypoglycaemic events were defined as a blood glucose level of <80 mg/dL or <4.4 mmol/L, and hyperglycaemic events were defined as a blood glucose level of >300 mg/dL or >16.7 mmol/L.12 In addition to these primary outcomes, medical consultation at the beginning of fasting was also noted as a secondary outcome.
Statistical analysis
Data were analysed using SPSS V.16. Frequencies and percentages were calculated for quantitative variables, while mean±SD were documented for qualitative variables. Relative risk was calculated as a measure of association between pre-Ramadan medical consultation and hypoglycaemia.
Results
Of the 150 patients (ages 24–75 years), 95 (63.3%) were male and 55 (36.7%) were female. The majority (58%) had to adjust their dose of medication to help them cope with the requirements of observing a fast. However, only 50 (33.3%) went for a review by their physician before they began fasting despite being at a higher risk of adverse glycaemic events. Most took oral antidiabetic drugs (OADs) alone, followed by those who took a combination of OADs and insulin. Six patients did not receive any antidiabetic therapy. Table 1 gives the demographic and medication details of the study participants.
Table 1.
Characteristics of study population (n=150)
| Characteristic | n (%) or mean±SD |
|---|---|
| Gender | |
| Male | 95 (63.3%) |
| Female | 55 (36.7%) |
| Age (years) | 50.8±10.2 |
| Duration of diabetes (years) | 7.8±5.8 |
| Medication adjustment | |
| Yes | 87 (58%) |
| No | 63 (42%) |
| Type of medication | |
| Oral antidiabetic drugs only | 93 (62%) |
| Insulin only | 13 (8.7%) |
| Oral antidiabetic drugs+insulin | 38 (25.3%) |
| No antidiabetic drugs | 6 (4%) |
A total of 15 (10%) patients had one or more hypoglycaemic events, ranging from one to five episodes, during the month. Of these 15 patients, seven had only one episode during the month, five had two episodes, and three had more than two episodes. Only five (3.3%) patients reported episodes of hyperglycaemia, with two having one event and two having two events during the month of Ramadan. Despite the number of hyper/hypoglycaemic events, the number of patients who broke one or more fasts was 13 (8.7%), with the bulk of the patients, seven and four, breaking only one and two fasts, respectively. Furthermore, two of these 13 patients discontinued a fast because of a feeling of weakness, although their blood sugar levels were within the optimum range. Only 10 (6.7%) of the participants who experienced hypoglycaemia discontinued a fast. None of the study participants experienced severe hyper/hypoglycaemia requiring hospitalisation or an emergency room visit.
More women than men and more patients receiving combination therapy (OAD+Insulin) than those receiving single therapy (OAD or insulin alone) experienced hypoglycaemia. Table 2 shows the proportion of study participants in the respective subgroups based on gender and type of antidiabetic medication who experienced hypo/hyperglycaemia.
Table 2.
Proportion of study participants who experienced adverse glycaemic events in subgroups based on gender and type of medication (Islamabad, Pakistan, 10 May 2016)
| Subgroup | Hypoglycaemia (%) | Hyperglycaemia (%) |
|---|---|---|
| Gender | ||
| Male | 7.4 | 3.2 |
| Female | 14.5 | 3.6 |
| Type of medication | ||
| Oral antidiabetic drugs only | 5.4 | 3.2 |
| Insulin only | 15.8 | 5.3 |
| Oral antidiabetic drugs+insulin | 23.1 | 0 |
The strength of association between a pre-Ramadan visit to a physician and the risk of developing hypoglycaemia was measured by calculating the relative risk. Table 3 is the 2×2 table used to calculate the measure of association.
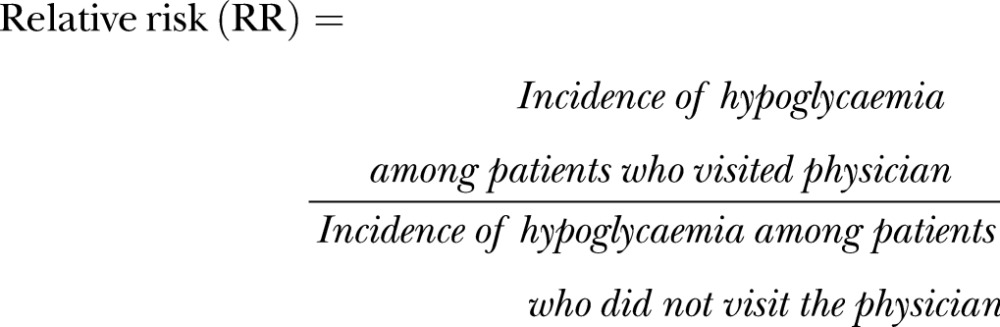 |
 |
Table 3.
The 2×2 table used to calculate the relative risk to measure the association between a pre-Ramadan visit to a physician and the risk of developing hypoglycaemia in our study population (Islamabad, Pakistan, 17 March 2016)
| Pre-Ramadan visit to physician | Developed hypoglycaemia | Did not develop hypoglycaemia | Total |
|---|---|---|---|
| Yes | 4 | 46 | 50 |
| No | 11 | 89 | 100 |
The relative risk was <1, which indicates a negative association between a pre-Ramadan visit to a physician and the risk of developing hypoglycaemia.
Discussion
The results of this study show that 1 in 10 patients with diabetes observing a fast experienced hypoglycaemic events, and about 1 in 30 developed hyperglycaemia. Only 1 in 3 diabetic patients who wished to fast opted for medical consultation before the month of fasting. It is alarming that 1 in 3 patients with hypoglycaemia did not discontinue fasting. A pre-Ramadan visit to the physician decreased the risk of developing hypoglycaemia in diabetic patients who intended to fast compared with those who did not go for a medical consultation. A small difference was observed between men and women in terms of hyperglycaemia, but more women than men experienced hypoglycaemia. Recently, Kautzky-Willer et al,13 in a patient-level pooled analysis of six randomised controlled trials, found that women are more likely to experience hypoglycaemia than men. However, it is not always the case, as shown by a post hoc analysis of six pooled clinical trials on postprandial glucose levels in patients with type 2 diabetes mellitus treated with insulin.14 The reason for the difference is not clear, but it might be due to differences in gender-related body fat distribution and hormones.15 Furthermore, a greater proportion of patients taking a combination of OAD and insulin experienced hypoglycaemia than those receiving single therapy (OAD or insulin alone). Patients on combination therapy might have poor glycaemic control and thus were being treated more aggressively. Our results differ from those of similar previous studies. The differences may be due to variations in study design, sample size, study population, pre-Ramadan counselling/education or definition of hyper/hypoglycaemia on the basis of symptoms rather than blood sugar level.
In our prospective study, fewer diabetic patients (33.3%) consulted a physician before the start of Ramadan than has previously been reported (∼60%).3 8 In addition, a smaller proportion of our study subjects had hypoglycaemic episodes than found in other research,4 9 16–18 with exception of the latest retrospective study conducted by Babineaux et al.10 They found that 8.8% of their study population experienced hypoglycaemia, compared with 10% in our study. Furthermore, fewer of our study participants experienced hyperglycaemic events. In terms of hospitalisation of patients due to adverse glycaemic episodes, our results are in agreement with those of Ahmedani et al.16 17 None of our study participants required hospitalisation, while Babineaux et al reported a low hospitalisation rate of 0.23% among their study sample.
The EPIDIAR study, the largest study to date to investigate diabetic patients during Ramadan, showed that more patients discontinued fasting due to hyperglycaemia than due to hypoglycaemia,3 but this is in contrast with similar studies,16 17 including ours. It further reported that 62% of patients with type 2 diabetes obtained advice from their healthcare providers before starting to fast, whereas only 33% of our study population visited a physician before Ramadan. Moreover, in the EPIDIAR study, 2% of the patients with type 2 diabetes experienced severe hypoglycaemia and 4% experienced severe hyperglycaemia, requiring hospitalisation. In contrast, none of our study participants required hospitalisation due to adverse glycaemic events. These differences may be due to a number of factors. The EPIDIAR study was a retrospective study, whereas ours was a prospective study. Moreover, the EPIDIAR study took into account symptomatic hyper/hypoglycaemia, whereas we used glucometer readings to determine adverse glycaemic events. Furthermore, the EPIDIAR study was published over a decade ago when there were much fewer data on management of diabetes during Ramadan. It is possible that, over the years, healthcare providers and patients have become more aware about managing diabetes during Ramadan. Table 4 compares the results of our study with those of similar previous studies.
Table 4.
Comparison of the present study with previous studies that investigated diabetic patients during Ramadan (Islamabad, Pakistan, 17 March 2016)
| Research study | Pre-Ramadan visit to physician (%) | Hypoglycaemia (%) | Hyperglycaemia (%) | Hospitalisation due to diabetes (%) |
|---|---|---|---|---|
| Present study | 33.3 | 10 | 3.3 | 0 |
| Babineaux et al10 | – | 8.8 | – | 0.23 |
| Siaw et al18 | – | 25.5 | – | – |
| Ahmedani et al17 | – | 23.7 | 16.3 | 0 |
| Peeters et al8 | 56 | – | – | – |
| Ahmedani et al16 | – | 24.5 | – | 0 |
| Ahmedani et al9 | – | 21.7 | 19.8 | – |
| Uysal et al4 | – | 19.5 | – | 0 |
There are a few confounders that might have affected our study results. The medical centre where this research was conducted is located in an urban area, so the majority of our study population was urban and might have more sedentary lifestyles than the rural population. Although we encourage all our patients to have a glucometer at home, there is a possibility that our study participants belong to monetarily stable strata of society, and therefore might have a more luxurious lifestyle. Similarly, those patients who possess a glucometer may be more educated and literate and are thus more aware of strategies to prevent adverse glycaemic events during Ramadan. However, many of our patients did not know how to use a glucometer, and their caregivers or family members helped them to check their blood glucose levels with this instrument.
Throughout the study, we strived to maintain accuracy at every step. Measures were taken to minimise several forms of bias. In a series of meetings before the study, researchers were taught to uniformly administer the questionnaire and ask only those questions mentioned in the protocol. One of the senior researchers periodically checked the data. Data were entered and analysed, and the accuracy was ensured. It should be understood that several forms of bias can be minimised but not eliminated and the possibility of false reporting cannot be neglected. Our study has several limitations. We had no control group. Variables such as physical activity, occupation, education and socioeconomic status that can potentially affect results were not recorded. In addition, only patients with type 2 diabetes were included in the study. Furthermore, study participants were asked to monitor their blood glucose at a random time after Iftar, as it was not feasible for many patients to do this at a designated time each day, for various reasons such as non-availability of their caregiver and post-Iftar commitments. Another limitation of our study is that 44 patients were lost to follow-up. We enrolled 194 patients in our study and 150 were included in the analysis. However, the sample size of the study is still adequate. Moreover, glucometer readings were used for recording of adverse glycaemic events, as the study was conducted in a resource-limited setting. This is not the gold standard method, but several studies have advocated the accuracy of glucometers.19–21
Conclusions
We conclude that patients with diabetes who fast regularly are at risk of adverse glycaemic events. Most of these patients do not consult their physician for reassessment before fasting. Medical consultation before starting to fast has a protective effect against hypoglycaemia, so it is necessary to spread awareness regarding the importance of medical consultation. Every patient should visit their physician to modify the doses of medication and be counselled about lifestyle changes. Blood sugar levels should be closely monitored while fasting. Even though severe hyper/hypoglycaemia that would require hospitalisation or an emergency room visit was not observed, it remains a possibility. Not all patients with adverse glycaemic episodes discontinued fasting, although it should be considered because of the increased risk of complications. Prospective large-scale multicentred studies would confirm these findings. Moreover, there is a need to conduct interventional studies to discover more about optimum dosages of medication during fasting. Formal guidelines that would address the clinical challenge of managing diabetic patients who fast are yet to be published.
Acknowledgments
We would like to thank Dr Shahbaz Bhatti for helping with data analysis and manuscript writing.
Footnotes
Handling editor: Seye Abimbola
Contributors: MJN, HAK, OI and URM designed the study. MJN, QK and SM performed the data collection. MJN and URM performed the data analysis. MJN, AMKM and AKN provided data interpretation. All the authors took part in drafting the manuscript and revising the paper critically for important intellectual content and approved the final version to be published.
Competing interests: None declared.
Ethics approval: This study was approved by the ethics committee of Shifa International Hospitals Ltd, Islamabad.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Mahmoud AI. Managing diabetes during Ramadan. Diabetes Voice 2007;52:19–22. [Google Scholar]
- 2.Qur'an 2:183–5.
- 3.Salti I, Benard E, Detournay B et al. , the EPIDIAR Study Group. A population-based study of diabetes and its characteristics during the fasting month of Ramadan in 13 countries: results of the Epidemiology of Diabetes and Ramadan 1422/2001 (EPIDIAR) study. Diabetes Care 2004;27:2306–11. 10.2337/diacare.27.10.2306 [DOI] [PubMed] [Google Scholar]
- 4.Uysal AR, Erdogan MF, Sahin G et al. Clinical and metabolic effects of fasting in 41 type 2 patients during Ramadan. Diabetes Care 1998;21:2033–4. 10.2337/diacare.21.11.2033 [DOI] [PubMed] [Google Scholar]
- 5.Mygind A, Kristiansen M, Wittrup I et al. Patient perspectives on type 2 diabetes and medicine use during Ramadan among Pakistanis in Denmark. Int J Clin Pharm 2013;35:281–8. 10.1007/s11096-012-9716-1 [DOI] [PubMed] [Google Scholar]
- 6.Benaji B, Mounib N, Roky R et al. Diabetes and Ramadan: review of the literature. Diabetes Res Clin Pract 2006;73:117–25. 10.1016/j.diabres.2005.10.028 [DOI] [PubMed] [Google Scholar]
- 7.Katibi IA, Akande AA, Bojuwoye BJ et al. Blood sugar control among fasting Muslims with type 2 diabetes mellitus in Ilorin. Niger J Med 2001;10:132–4. [PubMed] [Google Scholar]
- 8.Peeters B, Mehuys E, van Tongelen I et al. Ramadan fasting and diabetes: an observational study among Turkish migrants in Belgium. Prim Care Diab 2012;6:293–6. 10.1016/j.pcd.2012.02.003 [DOI] [PubMed] [Google Scholar]
- 9.Ahmedani MY, Riaz M, Fawwad A et al. Glycaemic trend during Ramadan in fasting diabetic subjects: a study from Pakistan. Pak J Biol Sci 2008;11:2044–7. 10.3923/pjbs.2008.2044.2047 [DOI] [PubMed] [Google Scholar]
- 10.Babineaux SM, Toaima D, Boye KS. Multi-country retrospective observational study of the management and outcomes of patients with Type 2 diabetes during Ramadan in 2010 (CREED). Diabet Med 2015;32:819–28. 10.1111/dme.12685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dean AG, Sullivan KM, Soe MM. OpenEpi: Open Source Epidemiologic Statistics for Public Health. http://www.openepi.com/SampleSize/SSPropor.htm (accessed 13Mar 2016).
- 12.Kobeissy A, Zantout MS, Azar ST. Suggested insulin regimens for patients with type 1 diabetes mellitus who wish to fast during the month of Ramadan. Clin Ther 2008;30:1408–15. 10.1016/j.clinthera.2008.08.007 [DOI] [PubMed] [Google Scholar]
- 13.Kautzky-Willer A, Kosi L, Lin J et al. Gender-based differences in glycaemic control and hypoglycaemia prevalence in patients with type 2 diabetes: results from patient-level pooled data of six randomized controlled trials. Diabetes Obes Metab 2015;17: 533–40. 10.1111/dom.12449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jovanovic L. Sex differences in insulin dose and postprandial glucose as BMI increases in patients with type 2 diabetes. Diabetes Care 2009;32:e148 10.2337/dc09-1634 [DOI] [PubMed] [Google Scholar]
- 15.Geer EB, Shen W. Gender differences in insulin resistance, body composition, and energy balance. Gend Med 2009;6(Suppl 1):60–75. 10.1016/j.genm.2009.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ahmedani MY, Haque MS, Basit A et al. Ramadan Prospective Diabetes Study: the role of drug dosage and timing alteration, active glucose monitoring and patient education. Diabet Med 2012;29:709–15. 10.1111/j.1464-5491.2011.03563.x [DOI] [PubMed] [Google Scholar]
- 17.Ahmedani MY, Alvi SF, Haque MS et al. Implementation of Ramadan-specific diabetes management recommendations: a multi-centered prospective study from Pakistan. J Diabetes Metab Disord 2014;13:37 10.1186/2251-6581-13-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Siaw MY, Chew DE, Dalan R et al. Evaluating the effect of Ramadan fasting on Muslim patients with diabetes in relation to use of medication and lifestyle patterns: a prospective study. Int J Endocrinol 2014;2014:308546 10.1155/2014/308546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hamid MH, Chishti AL, Maqbool S. Clinical utility and accuracy of a blood glucose meter for the detection of neonatal hypoglycemia. J Coll Physicians Surg Pak 2004;14:225–8. doi:04.2004/JCPSP.225228 [PubMed] [Google Scholar]
- 20.Ullal A, Parmar GM, Chauhan PH. Comparison of glucometers used in hospitals and in outpatient settings with the laboratory reference method in a tertiary care hospital in Mumbai. Indian J Endocrinol Metab 2013;17:S688–93. 10.4103/2230-8210.123569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tack C, Pohlmeier H, Behnke T et al. Accuracy evaluation of five blood glucose monitoring systems obtained from the pharmacy: a European multicenter study with 453 subjects. Diabetes Technol Ther 2012;14:330–7. 10.1089/dia.2011.0170 [DOI] [PMC free article] [PubMed] [Google Scholar]