Abstract
Medical records, which are increasingly directly accessible to patients, contain highly technical terms unfamiliar to many patients. A federally qualified health center (FQHC) sought to help patients interpret their records by embedding context-specific hyperlinks to plain-language patient education materials in its portal. We assessed the impact of this innovation through a 3-year retrospective cohort study. A total of 12,877 (10% of all patients) in this safety net population had used the MPC links. Black patients, Latino patients comfortable using English, and patients covered by Medicaid were more likely to use the informational hyperlinks than other patients. The positive association with black race and Latino ethnicity remained statistically significant in multivariable models that controlled for insurance type. We conclude that many of the sociodemographic factors associated with the digital divide do not present barriers to accessing context-specific patient education information once in the portal. In fact, this type of highly convenient plain-language patient education may provide particular value to patients in traditionally disadvantaged groups.
BACKGROUND
Providing patients with access to their medical records became a national priority with the federal electronic health record incentive program (the “meaningful use” program) mandating various forms of electronic release of data to patients (1–3). To provide patients with records access, healthcare institutions typically offer patient portals, web-based products that give patients access to data from the electronic health record (EHR) (4–7).
However, because medical records are created for medical professionals, they contain technical vocabulary that tends to be unfamiliar to patients, including medication names, diagnoses, and procedures. This vocabulary is particularly challenging for patients with low levels of health literacy (8–10), which has been defined as the ability to obtain, understand, and communicate about health-related information to make informed decisions (10). Low health literacy is associated with increased rates of hospitalization, lower use of preventive care, and among the elderly, worse overall health status and higher mortality (10–12). One-quarter to one-third of Americans are estimated to have limited health literacy, and it is more prevalent among racial and ethnic minorities, the elderly, and those living in poverty (12–14). As a result, many of the patients most in need of information about their health are among those least likely to be able to use it (15).
One potential solution is to provide plain-language explanations of difficult medical terms in context. A precedent is found in the infobutton, a clinician-facing innovation that provides context-specific information in the EHR, which has been shown to help clinicians answer clinical questions quickly at the point of care (16). To provide infobutton-like resources for patients, the National Library of Medicine recently collaborated with EHR vendor Epic Systems Inc. and the Institute for Family Health (IFH), a federally qualified health center. The 3 collaborating institutions developed a service hyperlinking vocabulary terms in the Epic portal with MedlinePlus, the National Library of Medicine’s free online patient education resource (www.nlm.nih.gov/medlineplus). MedlinePlus is an encyclopedia of plain-language explanations of medical diagnoses, medications, and other medical terms, designed to be at the 8th-grade reading level. The service, MedlinePlus Connect, automatically renders medical terms in the electronic patient portal as active hyperlinks. Notably, by hyperlinking unfamiliar terms directly to related information in MedlinePlus, this service helps patients access relevant information without the additional barrier of using a search engine, and without encountering the irrelevant or low quality results that might be produced by a self-directed online search. The service, first implemented at IFH, is now available as a web service and has been implemented in other electronic health record and electronic patient portal systems across the country (https://www.nlm.nih.gov/medlineplus/connect/service.html).
In this study, we sought to evaluate uptake of the innovation by tracking use of the vocabulary hyperlinks by patients over the first 3 years of the service. We hypothesized that use of these vocabulary hyperlinks would be lower among the disadvantaged patient groups affected by the “digital divide” (17).
METHODS
Setting: The Institute for Family Health is a federally qualified health center with 18 sites in Manhattan and the Bronx, as well as clinics in rural areas and smaller towns to the north of the city in the Hudson Valley. Almost all physicians are family practice physicians. An early adopter of EHRs, IFH has offered its patients an English-language electronic patient portal (MyChart) since 2007, with the Spanish-language version added in 2011.
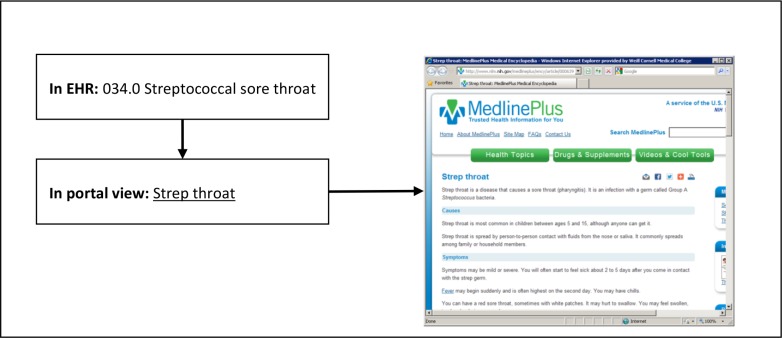
When patients log into their portal account, they can see the conditions listed on their EHR problem list as well as the billing codes from each encounter. Some of these medical conditions are rendered directly as ICD terminology, and a subset are rendered as as “patient-friendly” equivalents (e.g., “strep throat” instead of “streptococcal infection of the throat”).
With MedlinePlus Connect (MPC), all of these medical conditions and procedures are automatically rendered as active hyperlinks. Each hyperlink contains the ICD code associated with the medical term, and automatically links to the most relevant MedlinePlus information, which is also indexed by ICD code. Data collection for this study was conducted before IFH transitioned to ICD-10, so all codes were ICD-9.
Study design and data collection: For this retrospective cohort study, all adult patients with a visit to an IFH site between February 2011 and February 2014 were eligible. The primary outcomes were frequency of patient portal access and frequency of use of MPC. For the predictor variables, deidentified reports of patient data were generated from the Epic database and included age, gender, race, ethnicity, insurance status, preferred language, location, number of clinic visits, and encounter diagnoses (during the course of this study, these were ICD-9 codes). We applied the Johns Hopkins Adjusted Clinical Groups algorithm to the ICD-9 codes to classify patients by number of chronic conditions. We attributed each patient to the provider he or she saw the most frequently (his/her “preferred” provider). As an indicator of the provider’s IFH-specific workload, we produced a count of all patients seen by that provider. The project was approved by the IRBs of Weill Cornell and the Institute for Family Health.
Analysis: Patient characteristics were summarized with descriptive statistics, and assessed for association with (A) portal use and (B) MPC use in bivariate analyses using chi-squared tests or independent sample t-tests as appropriate. We constructed multivariable logistic regression models for MPC use among patient portal users only. Model 1 incorporated variables that were significant at .05 in the bivariate analyses (with the exception of number of chronic conditions, which was so strongly correlated with number of encounters that it raised collinearity concerns and was omitted). Region was not included as it was not a significant predictor in bivariate analyses. However, because of the marked differences in the demographic profile of the 3 regions, we also constructed exploratory multivariable models stratified by region. These models (not shown) revealed a significant interaction between age and region, with age having different effects on MPC use in different regions. We therefore constructed multivariable Model 2 containing all variables included in Model 1 plus region and a region x age interaction term. After confirming that the Akaike information criterion (AIC) for Model 2 was smaller than the AIC for Model 1 suggesting improved fit, we selected Model 2 as the final model for the current paper.
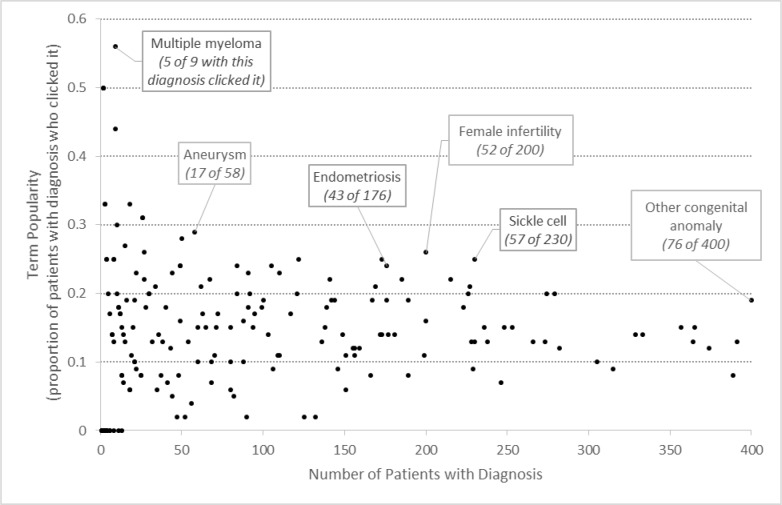
For exploratory purposes, we also computed a “popularity” index for each vocabulary term that was clicked by the patients. This “popularity” index was the number of patients who clicked the term divided by the number of patients in whose medical record the term appeared. To simplify the graph (figure 1), we reduced the number of vocabulary terms by running the ICDs through the AHRQ/HCUP Clinical Classifications grouper, which groups closely related ICD-9 codes into clinical conditions (e.g., diabetes, endometriosis, etc.).
Figure 1:
The ICD term in the EHR problem list or billing code is rendered in the patient portal as the ICD term or substituted with a more familiar term. With MedlinePlus Connect (MPC), the term is automatically rendered as an active hyperlink, with the ICD number embedded in URL. Clicking on the term produces a pop-up window with the corresponding MedlinePlus information.
RESULTS
There were 129,738 adult patients with one or more clinical visits in the study period; 30,692 (24%) had portal accounts. A total of 12,877 (42% of portal users, or 10% of all patients) explored one or more MedlinePlus Connect links. Patients who used the vocabulary hyperlinks clicked a median of 2.0 times (maximum: 97) and a median of 2.0 different terms (maximum, 24). As we have reported elsewhere, portal users were representative of the entire IFH population in terms of racial distribution but were more likely to be privately insured (18).
Sociodemographic predictors of use of MedlinePlus Connect (bivariate)
As demonstrated in Table 1, use of the informational hyperlinks was associated with socioeconomic characteristics but not in the hypothesized direction. (Throughout Table 1, it is important to note that because of the large sample size, very small differences were sometimes statistically significant even if they are unlikely to be clinically significant.) Black patients were more likely to use MPC than white ones (43% compared to 40%), and Latino patients more likely to use the resource than non-Latinos (43% compared to 41%). When Latinos were further subdivided by their preferred language, it became clear that it was the English-preferring Latinos who were driving the use of this resource. Finally, patients covered by Medicaid were more likely to use MPC than privately insured ones (44% versus 43%).
Table 1:
Characteristics of MedlinePlus Connect (MPC) users and nonusers
| Characteristic | Total | Portal users | MPC users as % of portal users | MPC non-users as % of portal users | P | MPC users as % of all patients in category | |
|---|---|---|---|---|---|---|---|
| (Column %) | (Row %) | (Row %) | (Row %) | (Row %) | |||
| N | 129,738 (100) | 30692 (23.7) | 12877 (42.0) | 17815 (58.0) | 12877 (9.9%) | ||
| Age | 18-24 | 24051 (18.5) | 6195 (25.8) | 2436 (39.3) | 3759 (60.7) | <. 001 | 10.1% |
| 25-44 | 56414 (43.5) | 15702 (27.8) | 6608 (42.1) | 9094 (57.9) | 11.7% | ||
| 45-64 | 38921 (30.0) | 7526 (19.3) | 3338 (44.4) | 4188 (55.7) | 8.6% | ||
| 65+ | 10352 (8.0) | 1269 (12.3) | 495 (39.0) | 774 (61.0) | 4.8% | ||
| Gender | Women | 78698 (60.7) | 20708 (26.3) | 9034 (43.6) | 11674 (56.4) | <. 001 | 11.5% |
| Men | 51035 (39.3) | 9984 (19.6) | 3843 (38.5) | 6141 (61.5) | 7.5% | ||
| Race | Black | 29774 (23.0) | 6752 (22.7) | 2910 (43.1) | 3842 (56.9) | <. 001 | 9.8% |
| White | 46417 (35.8) | 11670 (25.1) | 4701 (40.3) | 6969 (59.7) | 10.1% | ||
| All other | 33224 (25.6) | 7926 (23.9) | 3426 (43.2) | 4500 (56.8) | 10.3% | ||
| Unknown | 20323 (15.7) | 4344 (21.4) | 1840 (42.4) | 2504 (57.6) | 9.1% | ||
| Ethnicity by language preference | Latino, prefers Spanish | 10080 (7.8) | 1125 (11.2) | 363 (32.3) | 762 (67.7) | <.001 | 3.6% |
| Latino, not prefer Spanish | 25002 (19.3) | 7116 (28.5) | 3213 (45.2) | 3903 (54.9) | 12.9% | ||
| Not Latino | 79141 (61.0) | 19517 (24.7) | 8084 (41.4) | 11433 (58.6) | 10.2% | ||
| Unknown | 15515 (12.0) | 2934 (18.9) | 1217 (41.5) | 1717 (58.5) | 7.8% | ||
| Insurance | Private | 38885 (30.0) | 13035 (33.5) | 5567 (42.7) | 7468 (57.3) | <. 001 | 14.3% |
| Medicaid | 39706 (30.6) | 9083 (22.9) | 3959 (43.6) | 5124 (56.4) | 10.0% | ||
| Uninsured | 28695 (22.1) | 4395 (15.3) | 1572 (35.8) | 2823 (64.2) | 5.5% | ||
| Medicare | 15478 (11.9) | 2266 (14.6) | 976 (43.1) | 1290 (56.9) | 6.3% | ||
| Unknown | 2474 (1.9) | 427 (17.3) | 174 (40.8) | 253 (59.3) | 7.0% | ||
| Other public or dual | 4500 (3.5) | 1486 (33.0) | 629 (42.3) | 857 (57.7) | 14.0% | ||
| Encounters | >3 | 68850 (53.1) | 21522(31 3) | 10182 (47.3) | 11340 (52.7) | <. 001 | 14.8% |
| Chronic conditions | 1 or more | 67815 (52.3) | 17745 (26.2) | 8439 (47.6) | 9306 (52.4) | <. 001 | 12.4% |
| Region | Hudson Valley | 38016 (29.3) | 5344 (14.1) | 2272 (42.5) | 3072 (57.5) | .60 | 6.0% |
| Bronx | 24631 (19.0) | 6486 (26.3) | 2729 (42.1) | 3757 (57.9) | 11.1% | ||
| Manhattan | 67090 (51.7) | 18862 (28.1) | 7876 (41.8) | 10986 (58.2) | 11.7% | ||
| Workload of “preferred” provider | < 794 patients a year | 32190 (24.8) | 6613 (20.5) | 2679 (40.5) | 3934 (59.5) | <.001 | 8.3% |
| 794 – 1715 | 32276 (24.9) | 8419 (26.1) | 3540 (42.1) | 4879 (58.0) | 11.0% | ||
| 1716 – 2714 | 32130 (24.8) | 7856 (24.5) | 3472 (44.2) | 4384 (55.8) | 10.8% | ||
| 2715 or more | 33142 (25.6) | 7804 (23.6) | 3186 (40.8) | 4618 (59.2) | 9.6% | ||
Clinical predictors of use of MedlinePlus Connect (bivariate)
Use of MPC was associated with clinical characteristics in the expected direction. Women, patients with more encounters, and patients with more chronic conditions were more likely to use the resource. MedlinePlus Connect users were very slightly older than nonusers, due primarily to greater representation in the middle-aged (45-64 years) age bracket.
Health system predictors of use of MedlinePlus Connect (bivariate)
Patients of the least busy and most busy providers were least likely to use MPC. There were no differences by region.
Multivariable model of MedlinePlus Connect use
The final multivariable model included: age, gender, race, ethnicity with preferred language, insurance type, number of encounters, workload of preferred provider, region, and the region x age interaction term (Table 2). In this model, use of the informational hyperlinks remained positively associated associated with older age, female sex, black race, English-preference Latinos, having private insurance, more clinical encounters, and provider workload (with MPC use being more common forms patients of less busy providers).
Table 2:
Multivariable model of MPC use by sociodemographic characteristics
| Characteristic | Level | Adjusted Odds Ratio | CI | P | |
|---|---|---|---|---|---|
| Age | (per 1-year increase) | 1.004 | 1.002 | 1.007 | <.001 |
| Sex | Women | 1.167 | 1.109 | 1.227 | <.001 |
| Men | Reference | ||||
| Race | Black | 1.100 | 1.027 | 1.180 | .007 |
| All other | 1.143 | 1.056 | 1.237 | <.001 | |
| Unknown | 1.106 | 1.010 | 1.211 | .02 | |
| White | Reference | ||||
| Ethnicity with preferred language | Latino, does not prefer Spanish | 1.077 | 1.001 | 1.159 | .045 |
| Latino, prefers Spanish | 0.607 | 0.525 | 0.702 | <.001 | |
| Unknown ethnicity | 0.993 | 0.900 | 1.097 | .89 | |
| Not Latino | Reference | ||||
| Insurance | Medicaid | 0.897 | 0.847 | 0.951 | <.001 |
| Medicare | 0.865 | 0.782 | 0.957 | .005 | |
| Other Public or dual | 0.960 | 0.859 | 1.073 | .47 | |
| Uninsured | 0.766 | 0.711 | 0.824 | <.001 | |
| Unknown | 0.888 | 0.726 | 1.083 | .24 | |
| Private | Reference | ||||
| Encounters | >3 | 2.164 | 2.049 | 2.287 | <.001 |
| Provider workload | < 794 patients a year | 1.093 | 1.022 | 1.169 | .01 |
| 794 – 1715 | 1.173 | 1.094 | 1.257 | <.001 | |
| 1716 – 2714 | 1.034 | 0.965 | 1.109 | .34 | |
| 2715 or more | Reference | ||||
| Region | Hudson Valley | 1.019 | 0.841 | 1.235 | .85 |
| Bronx | 1.379 | 1.161 | 1.639 | <.001 | |
| Manhattan | Reference | ||||
| Interaction | Hudson Valley*Age | 0.997 | 0.993 | 1.001 | .16 |
| Bronx*Age | 0.988 | 0.983 | 0.992 | <.001 | |
| Manhattan*Age | Reference | ||||
Interestingly, when we controlled for race and ethnicity in this multivariable model, patients with Medicaid were less likely to use the MPC resource. The positive relationship in the bivariate analysis was therefore due to the black and Latino patients who were using the resource. The multivariable results suggest that within each racial and ethnic category, patients with Medicaid (the lower income patients) were somewhat less likely to use the MPC resource.
As noted in the methods, we included the interaction term between region and age because we saw different age-related patterns in preliminary bivariate models that were stratified by region (not shown). These models showed that older patients were more likely than younger patients to use MPC in Manhattan but not in other regions. To confirm this finding in the multivariate models, we included an interaction term between region and age, and confirmed that it was statistically significant in the expected direction. In other words, as Manhattanites became older, they were more likely to use MPC, but this pattern was much weaker in the Bronx and not found at all in the Hudson Valley. We attribute this finding to the different demographic patterns in these regions. In Manhattan, the older population contains quite a number of people who are well-educated and have relatively high socioeconomic status, so they might be more likely to do research on their health conditions. By contrast, the Bronx and the small towns where IFH has a presence in the Hudson Valley are much less affluent, and elderly patients in those areas are likely to be less well-educated and less affluent members of minority groups.
Frequently explored terms
Diagnosis “popularity” (or proportion of times a diagnosis term was clicked) was fairly constant at an average of 14.5% regardless of how common the diagnosis was (Figure 2). “Popularity” appeared high for some of the rare conditions, but this was in fact an artifact of the rarity of the condition. For example, multiple myeloma had a very high popularity rating of 56%, but this was because only 9 patients had the condition and 5 of them clicked upon it.
Figure 2:
Each dot represents a diagnosis. Data labels are placed on a small number of “popular” terms for illustrative purposes.
As Figure 2 shows, there was no obvious explanation for term “popularity.” To further explore “popularity,” we retrieved the 10 terms that were clicked by the largest numbers of patients (Table 3). No single unifying principle is immediately apparent to explain why these terms were frequently clicked. It is possible that in some cases, it is because the terms were unfamiliar and technical (“hyperlipidemia,” “unspecified essential hypertension”), prompting patients to seek a definition. It is also possible that people were more likely to click on stigmatized or contested diagnoses (e.g., “obesity,” “depression,” “anxiety”). In other cases, perhaps patients clicked when they were motivated to take action and do more research (“nicotine dependence,” which is likely to appear in the record of the patient already being treated for smoking cessation). A better understanding of why patients seek more information about certain conditions and not others would be a fruitful avenue for future quantitative and qualitative work.
Table 3:
Top 10 most explored terms
| ICD9 code | Diagnosis term | Number of patients who clicked this term | Number of portal users with this diagnosis | Clickers as percent of portal users with diagnosis (“popularity”) |
|---|---|---|---|---|
| V70.0 | General adult medical examination | 4638 | 21,940 | 21.1 |
| 278.00 | Obesity | 929 | 3896 | 23.8 |
| V25.9 | Contraceptive management | 895 | 5471 | 16.4 |
| 272.4 | Hyperlipidemia | 619 | 3560 | 17.4 |
| 401.9 | Unspecified essential hypertension | 407 | 3027 | 13.5 |
| 311 | Depression | 358 | 2216 | 16.2 |
| V62.9 | Psychosocial circumstances | 362 | 1560 | 23.2 |
| 300.00 | Anxiety | 317 | 1962 | 16.2 |
| 305.1 | Nicotine dependence | 306 | 2915 | 10.5 |
| 401.1 | Benign essential hypertension | 242 | 1749 | 13.8 |
DISCUSSION
Although providing patients with access to their medical records could help them better understand their health and healthcare, patients who do not understand the medical language found in these medical records are unlikely to benefit. Our study shows that a plain-language encyclopedia of medical terms, hyperlinked directly to the unfamiliar term, is frequently explored by patients with access to their medical records via an electronic patient portal. About 10% of all patients in this safety net population used the informational hyperlinks. The hyperlinks were appropriately used most by those with the greatest needs for medical information, i.e., those with more medical conditions and visits.
The sociodemographic analysis held some surprises. We and others have expressed concern that because of disparities in computer access as well as disparities in health literacy, any beneficial effects of patient portals are likely to be unequally distributed (19). However, counter to the main hypothesis of the current study, we found positive associations between MPC use, black race, being an English-speaking Latino patient, and being covered by Medicaid. The positive associations with black race and Latino ethnicity remained statistically significant in multivariable models that controlled for insurance type. However, in the multivariable model, Medicaid coverage developed a negative relationship with MedlinePlus Connect use. This can be interpreted to mean that Blacks and English-speaking Latinos within each insurance category are more likely to use the informational hyperlinks, although Medicaid (low income) patients are in general less likely to do so.
Latino patients who indicated that they prefer using Spanish in their clinical encounters were markedly less likely to use the resource. This was despite the availability of a Spanish-language portal and Spanish-language informational resources.
Overall, this study suggests that some of the factors associated with the digital divide which created barriers to accessing the electronic portal were not barriers to using the MedlinePlus Connect informational hyperlinks. However, the language barrier remains indicating the need for additional outreach and services to ensure Spanishspeaking patients have high-quality information about their health.
There are a number of potential explanations for why patients might click terms. One explanation is that patients with low health literacy (9, 11) would be less likely to understand a particular medical term and might be more likely to click to find out more. Unfortunately, because we were using EHR data, we had no assessments of patient health literacy, so we cannot conclude definitively that patients with low health literacy were the ones who were clicking on the hyperlinks. However, the prevalence of low health literacy is known to be higher among minority and low income patients (9, 11), and our findings demonstrate that these groups were particularly likely to use the MPC links. If low health literacy is the explanation, this would suggest that the MedlinePlus Connect links are providing particular value to patients who have less familiarity with medical vocabulary. This could provide an explanation for certain of the most “popular” terms in Figure 2, such as aneurysm and endometriosis, multisyllabic words likely to be unfamiliar to lay audiences.
Other reasons why a patient might click a term could include being highly concerned about a diagnosis, needing more explanation than what the provider discussed, or feeling uncomfortable having an extended conversation with the provider. For example, it is possible that patients with sensitive, stigmatized, or contested diagnoses (20–22) might be interested in finding out more in private after the encounter, when visiting the patient portal. These could explain the high click rates for potentially sensitive terms such as obesity and psychosocial circumstances in Table 3, and for highly concerning diagnoses such as sickle cell in Figure 2.
Limitations
This was a study at a single center providing safety net care, and all patients used a single commercially available patient portal product, so generalizability to other products and populations is unknown. Analyses were limited to data available in log files or the EHR, and therefore no direct measurements of health literacy, access to computers, or patient perceptions were available. This study did not include any measurement of healthcare outcomes, so it is not known whether access to this information actually helped patients manage their own health or their healthcare.
Conclusions
Context-specific hyperlinks that provided plain-language explanations of medical vocabulary were heavily used by electronic patient portal account holders at a federally qualified health center, especially those with multiple office visits and clinical conditions. Socioeconomic factors that presented barriers to access to the portal (such as race and poverty) did not pose barriers to use of the vocabulary hyperlinks within the portal. In fact, hyperlink users were more likely to be black or English-speaking Latino than were non-hyperlink users. We conclude that context-specific medical vocabulary hyperlinks are valuable to patients with the greatest information needs because of greater use of healthcare services, and that they are of particular use to patients in disadvantaged populations.
Acknowledgments
Dr. Ancker is funded by AHRQ K01 HS021531. This evaluation also received funding from the National Library Medicine. However, neither funder played any role in study design, data analysis or interpretation, or review or approval of the manuscript before publication.
The MedlinePlus Connect service was developed by the National Library of Medicine, the Institute for Family Health, and Epic Systems Inc. The authors thank Rob Logan of the NLM for significant contributions to the MPC implementation.
References
- 1.Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. New England Journal of Medicine. 2010;363:501–4. doi: 10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Medicare and Medicaid Services. Department of Health and Human Services. Federal Register; 2010. Jan 13, Medicare and Medicaid Programs; Electronic Health Record Incentive Program; Proposed Rule. [Google Scholar]
- 3.Conn J. Blue Button gains fans, apps. Simple tech from VA puts interoperability to work. Modern Healthcare. 2012;42:14. [PubMed] [Google Scholar]
- 4.Tang PC, Ash JS, Bates DW, Overhage JM, Sands DZ. Personal health records: Definitions, benefits, and strategies for overcoming barriers to adoption. JAMIA. 2006;13(2):121–6. doi: 10.1197/jamia.M2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Halamka JD, Mandl KD, Tang PC. Early experiences with personal health records. JAMIA. 2008;15(1):1–7. doi: 10.1197/jamia.M2562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaelber DC, Jha AK, Johnston D, Middleton B, Bates DW. A research agenda for personal health records (PHRs) JAMIA. 2008;15(6):729–36. doi: 10.1197/jamia.M2547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaelber DC, Shah S, Vincent A, Pan E, Hook JM, Johnston D, et al. Charlestown, MA: Center for Information Technology Leadership, Healthcare Information and Management System Society (HIMSS); 2008. The Value of Personal Health Records. [Google Scholar]
- 8.Nielsen-Bohlman L, Panzer AM, Kindig DA, editors. Health Literacy: A Prescription to End Confusion. Washington, DC: Institute of Medicine. The National Academies Press; 2004. Committee on Health Literacy. [PubMed] [Google Scholar]
- 9.Kutner M, Greenberg E, Jin Y, Paulsen C, White S. Washington, DC: National Center for Health Statistics; 2006. The Health Literacy of America’s Adults: Results from the 2003 National Assessment of Adult Literacy. Contract No.: NCES 2006–483. [Google Scholar]
- 10.DeWalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes: A systematic review of the literature. Journal of General Internal Medicine. 2004;19:1228–39. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sorenson K, Broucke S, Fullam J, Doyle G, Pelikan J, Slonska A, et al. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health. 2012;12(80) doi: 10.1186/1471-2458-12-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berkman M, Sheridan S, Donahue K, Halpern D, Viera A, Crotty K, et al. Rockville, MD: Agency for Healthcare Research and Quality; 2011. Health literacy interventions and outcomes: An updated systematic review. Contract No.: AHRQ Publication Number 11-E006. [PMC free article] [PubMed] [Google Scholar]
- 13.Koh HK, Berwick DM, Clancy CM, Baur C, Brach C, Harris LM, et al. New federal policy initiatives to boost health literacy can help the nation move beyond the cycle of costly ‘crisis care ‘. Health Affairs. 2012;31(2):434–43. doi: 10.1377/hlthaff.2011.1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koh H, Brach C, Harris LM, Parchman ML. A proposed ‘health literate care model’ would constitute a systems approach to improving patients’ engagement in care. Health Affairs. 2013;32(2):357–67. doi: 10.1377/hlthaff.2012.1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Parker RM, Ratzan SC, Lurie N. Health literacy: A policy challenge for advancing high-quality health care. Health Affairs. 2003;22(4):147–53. doi: 10.1377/hlthaff.22.4.147. [DOI] [PubMed] [Google Scholar]
- 16.Del Fiol G, Haug P, Cimino J, Narus S, Norlin C, Mitchell J. Effectiveness of topic-specific infobuttons: a randomized controlled trial. JAMIA. 2008;15(6):752–9. doi: 10.1197/jamia.M2725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fox S. Washington, DC: Pew Internet & American Life Project; 2006. Online Health Search 2006. [Google Scholar]
- 18.Ancker JS, Nosal S, Hauser D, Way C, Calman N. The role of access policy and digital divide in patient access to medical records. under review. 2016.
- 19.Ancker JS, Barron Y, Rockoff M, Hauser D, Pichardo M, Szcerenczy A, et al. Use of an electronic patient portal among disadvantaged populations. Journal of General Internal Medicine. 2011;26(10):1117–23. doi: 10.1007/s11606-011-1749-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ablon J. The nature of stigma and medical conditions. Epilepsy and Behavior. 2002;3:S2–S9. doi: 10.1016/s1525-5050(02)00543-7. [DOI] [PubMed] [Google Scholar]
- 21.Williams J, Gonzalez-Medina D, Le Q. Infectious diseases and social stigma. ATI – Applied Technologies and Innovations. 2011;4(1):58–70. [Google Scholar]
- 22.Koehne K, Hamilton B, Sands N, Humphreys C. Working around a contested diagnosis: borderline personality disorder in adolescence. Health (London, England : 1997) 2013;17(1):37–56. doi: 10.1177/1363459312447253. Epub 2012/06/08. [DOI] [PubMed] [Google Scholar]