Klinefelter syndrome (KS) is a common genetic disorder characterized by an additional X chromosome in males leading to a karyotype of 47,XXY. The clinical syndrome was first described nearly 75 years ago in several males with small testes, tall stature, gynecomastia, and azoospermia.1 Our construct of what KS entails has greatly changed since then with identification of the genetic etiology in 1959, epidemiological studies of birth cohorts in the 1980’s, the development of rodent models, and many observational and interventional clinical studies in boys and men with KS.2–4 Characterization of the neuropsychological profile, along with earlier diagnosis, facilitates earlier developmental evaluation and intervention services.5 Optimizing testosterone treatment may prevent some of the physical manifestations of the “classic KS phenotype.”6 Advanced Reproductive Technology (ART) has made it possible for nearly half of men with KS previously deemed infertile to have an opportunity to have a biological child.7,8 Despite these scientific advances, the underlying molecular mechanisms underlying primary testicular failure and the phenotypic heterogeneity of physical and neurocognitive features observed in KS remains elusive. In this review, we will provide the pediatrician with an update on what is known about the clinical manifestations and current treatment recommendations for boys and men with KS.
Epidemiology and Diagnosis
KS is the most common sex chromosomal aneuploidy with estimated prevalence rates ranging between 1 in 448 to 1 in 917 male births.9–14 A comparative analysis of newborn karyotyping studies published in the 1960–70’s and studies published in 1970’s–80’s reported an increase in the prevalence of KS.14 An increasing prevalence of KS could theoretically be explained by increasing maternal age, environmentally-derived increase of errors in paternal meiosis I, and decreasing rate of elective termination for prenatally diagnosed KS, although this increasing prevalence needs to be confirmed and further evaluated.12,14,15 Epidemiological studies of sex chromosome aneuploidies have been limited to industrialized nationals, and to our knowledge, there have been no reports of ethnic differences in KS prevalence.
Currently, there is a significant discrepancy between the known prevalence of KS based on newborn screening studies and the rate of clinical diagnosis. It is estimated only 25–35% of males with KS are diagnosed in their lifetime, with the remaining 65–75% left undiagnosed. A study in the United Kingdom estimated that of all expected cases, ~10% of diagnoses are made in the prenatal period, 6% in childhood or adolescence, and 19% in adulthood.16 The small number of children who are diagnosed before puberty are typically identified due to underdeveloped genitalia, hypotonia, developmental delays, or learning and behavior problems. Diagnoses made in adolescence are secondary to small testicular size, gynecomastia, or rarely, incomplete puberty. Adults are most commonly diagnosed for infertility, however may present for symptoms of hypogonadism.13 The low rate of diagnosis in the pediatric population is due to a combination of factors, including subtle or underrecognized features that overlap with typical children and genetic testing practices of most pediatricians that do not cover the most common neurodevelopmental features in KS such as reading disabilities or speech-language disorders. Additionally, while the majority of boys with KS will have mild to moderate neurodevelopmental and/or learning difficulties, there is phenotypic heterogeneity and approximately a quarter of boys with KS do not exhibit these challenges.5 Finally, there appears to be a delay in diagnosis relative to when parents first expressed concern about their child to their physician, particularly for concerns of development.17 When initial parental concerns were due to developmental delays, there was on average 4.8 years before genetic testing confirmed KS. The delay in diagnosis was only 2 years when parental concern was pubertal development, microorchidism, or gynecomastia, however the average age of diagnosis in that cohort was still greater than 20 years of age.17 Therefore, recognition of features of KS by the pediatrician can result in increased diagnosis rate and more appropriate care.
The diagnosis of KS is made with pre- or postnatal karyotype or DNA microarray. Historically, prenatal screening by ultrasound and/or maternal serum biochemical markers dramatically increased identification of pregnancies at risk for autosomal aneuploidies, yet KS pregnancies have failed to correlate with these screening markers. However, new prenatal genetic screening technology, referred to as non-invasive prenatal testing (NIPT), analyzes cell-free fetal DNA circulating in maternal blood. This low-risk screening modality is typically performed in the first trimester and can detect sex chromosome aneuploidies (SCA). While sensitivity and specificity of NIPT is high for the detection of autosomal trisomies, there is a lower accuracy for sex chromosome aneuploidies. In a recent study by Meck et al, NIPT specific to XXY was shown to have a positive predictive value of only 67% (CI 22.3–95.7%).18 Moreover, a 2014 study by Wang et al identified that 8% NIPT+ for SCA were due to an abnormal maternal karyotype.19 Thus, in cases of NIPT+ for SCA, both follow-up diagnostic testing (by prenatal chorionic-villous sampling, amniocentesis, and/or postnatal blood testing) and maternal karyotyping are recommended. While a relatively high rate of false positives remain, NIPT creates a landmark opportunity to dramatically increase prenatal ascertainment of KS, with estimates citing the diagnosis rate for infants would increase tenfold if NIPT were to be standard screening for all pregnancies. There has also been discussion about including Fragile X on standard newborn screen, which would also identify some cases of KS.20 With the possible increasing prevalence and significantly increasing childhood ascertainment rate, the pediatrician will likely care for more infants and children with a known diagnosis of KS.
Genetics
Klinefelter syndrome was confirmed to be attributed to the presence of a supernumerary X-chromosome resulting in a karyotype of 47,XXY by Dr. Patricia Jacobs in 1959.21 The supernumerary X-chromosome is acquired randomly predominantly through meiotic nondisjunction events during maternal or paternal gametogenesis or secondarily through post-zygotic nondisjunction during early embryonic mitotic divisions.22 The supernumerary X-chromosome is inherited from the mother in approximately 50% of cases, and from the father in the other 50%.23 Up to half of cases with maternally-derived supernumerary X cases are due to errors in meiosis I and become more common with increasing maternal age, while maternal meiosis II nondisjunction errors and paternal errors are not associated with parental age. The 2008 Morris et al. study describing an increase in the prevalence of KS proposes that environmental factors have led to increased paternal meiosis I errors, however this finding remains controversial.14
Mosaicism
While approximately 90% of KS cases are non-mosaic 47,XXY, mosaicism is identified in approximately 7% of cases, and the other 3% are made up of rare variants.13 Mosaic forms of KS are identified when the XXY cell line is found in the presence of another cell line, such as 46,XY or other karyotypes (ie. 47,XYY or 47,XXX). The phenotypic variability of mosaic KS is dependent upon the karyotype and percentage of the additional cell lines. In cases of XXY/XY mosaicism, phenotypic symptoms may present more mildly and many cases fail to be identified. In cases of XXY mosaicism with abnormal karyotypes, such as XXY/XXYY or XXY/XXXY, phenotypic presentation may be more severe. Routine karyotype studies analyze ~20 cells, however in the case of possible mosaicism, additional testing should be pursued by florescence in situ hybridization (FISH) of the X and Y chromosomes to analyze a larger number of interphase nuclei. A significant limitation to testing for mosaicism is that peripheral blood may not accurately reflect levels of mosaicism across different tissue types, so phenotypic interpretation continues to be heavily dependent upon clinical evaluation.
Since the original 1959 report of KS being caused by a single extra X-chromosome, several other rare sex chromosome variations in males have been identified and characterized by the presence of two or more extra X and Y chromosomes, including 48,XXYY, 48,XXXY and 49,XXXXY syndromes, occurring in 1:18,000–1:100,000 male births. While these syndromes have been labeled as “variants” of KS because of shared features, including hypergonadotropic hypogonadism and tall stature, these syndromes are characterized by a more severe phenotype including additional physical findings, congenital malformations, medical problems and psychological features.24,25
The mechanisms of how the presence of supernumerary X-chromosome(s) impact phenotypic features and variability observed in Klinefelter syndrome continue to be poorly understood. Studies continue to investigate the most implicated mechanisms including gene-dosage, skewed X-inactivation, genetic polymorphisms, and parental origin of the supernumerary X chromosome. Many of these potential mechanisms suggest an important role of epigenetic processes in KS.
Gene dosage and expression
Gene dosage compensation is the mechanism of equalizing gene expression between males (XY) and females (XX) due to the different number of genes contained on the sex chromosomes. This genetic equalization is achieved through a process of X-inactivation, in which one of the X-chromosomes in every female cell is randomly silenced, leaving only one X-chromosome transcriptionally active. In cases of X-chromosome aneuploidy, each X-chromosome in excess of one is inactivated by this same mechanism. However, two homologous regions of the sex chromosomes, known as pseudoautosomal regions (PAR1 & PAR2), as well as an additional 5–15% of X-chromosome genes escape inactivation and are expressed from both X-chromosomes.26,27 An extra copy of these “escapee” genes are therefore transcriptionally active in males with KS, and overexpression then leads to excess mRNA and gene product, subsequently affecting the cellular and developmental pathways affected by these genes. The observation that clinical phenotype progressively deviates as the number of supernumerary sex chromosomes increase further supports this theory. This overexpression of escapee genes continues to be heavily studied as a likely mechanism leading to the phenotype and impacting phenotypic variability in KS.
An example of such an X-linked escapee gene is the short stature homeobox gene (SHOX), which has demonstrated a gene dosage impact in SCA’s. SHOX is located within the pseudoautosomal region (PAR1) of the X-chromosome and encodes a transcription factor expressed in the developing skeleton impacting height. Short stature seen in Turner syndrome (45,X) has been established to result from haploinsufficency of SHOX. While tall stature in Klinefelter syndrome partially results from slower closure of epiphyseal plates secondary to hypogonadism, SHOX overexpression has also been implicated in the accelerated growth velocity and increased height observed in sex chromosome trisomies. 28
Further studies have analyzed differential genetic expression patterns in men with KS compared to male and female controls with the hope of elucidating differences in gene expression and regulation. In 2007, Vawter et al compared 11 men with KS to six XY males by whole genome expression array and identified differential expression of 129 genes, 14 of which were X-linked genes and many of which showed correlation with verbal cognition.29 Additional studies evaluating genetic expression differences in brain, testes, and blood further suggest that autosomal genes are also differentially expressed in KS.30–32 More recently, Zitzmann et al compared gene expression patterns of 132 males with KS to male and female controls. This study identified differential gene expression in 36 total genes (21 X-linked and 15 autosomal) compared to male controls and 86 total genes compared to female controls (46 Y-linked, 10 X-linked, and 30 autosomal).33 Several of these identified X-linked genes are known to escape X-inactivation and are involved in pathways associated with phenotypic physical findings commonly seen in KS and therefore considered likely candidates to the pathophysiology of KS. Understanding the role of differential gene expression differences in KS is made more complex by the recent finding of increased copy number variations of X-chromosome genes in KS compared to typical males and females, most of which were duplications and falling within areas that escape X-inactivation.34 Further work is needed to investigate regulatory mechanisms influencing differential gene expression not only in escapee genes but also across the entire genome as it relates to KS.
Skewed X-inactivation
Another genetic mechanism possibly leading to phenotypic variation in KS is skewed X-inactivation. Typically, X-inactivation is a random process resulting in a ratio of active to inactive X-chromosome alleles (outside of the PARs) of approximately 50%. Skewed X-inactivation, defined as greater than 80% methylation of one allele, results from preferential inactivation of a specific X-chromosome. Studies analyzing skewed X-inactivation in KS patients have ranged in finding below 10 percent to over 40 percent of subjects with skewing, and conflicting results regarding association of phenotypic features with skewing.35–37
In 2014, Skakkebaek’s evaluation of 73 KS males found no association between skewed X inactivation and cognition or psychological phenotypic variation.38 They did however find a significant correlation between skewed X inactivation and smaller grey matter volume in the left insula of the brain. The insular cortex area of the brain plays an important role in social, emotional and mental processing, all of which are variably affected in KS.39 Caution should be taken for interpretation of results from any study of X-inactivation, however, as X-inactivation is typically measured in peripheral blood but can vary between tissues. Further, effects of skewed X-inactivation itself remain dependent on the polymorphisms and activity of the genes expressed from the more active chromosome, which varies between individuals.
Parental Origin
Several studies have analyzed phenotypic variability in KS based on parental origin of the supernumerary X chromosome and possible differential expression of maternal versus paternal alleles. To date these results have been inconsistent. While most studies are unable to establish a significant correlation between parental origin and phenotypic variability,36,38,40,41 some studies have demonstrated a higher incidence of findings when the supernumerary X-chromosome was paternally derived, including developmental problems, altered steroidogenesis, increased hematocrit, later puberty, insulin resistance, and cardiac findings of a shorter QTc time.33,42,43
Gene Polymorphisms
Another gene of interest in KS is the androgen receptor gene (AR), which is located on the X chromosome and contains a highly polymorphic CAG trinuclotide repeat, with a normal range of 9–37 CAG repeats.36,44,45 Studies have correlated the CAG repeat length with physiological androgen effects, in which receptor activity is inversely related to the length of CAG repeat.36 Several studies have demonstrated the CAG repeat length to be correlated with variable characteristics of the KS phenotype. Studies have reported a correlation of long CAG repeat length (low receptor activity) with height, arm span, likelihood for gynecomastia, small testes, HDL cholesterol, hematocrit, and later reactivation of pituitary-testicular axis, all of which are more characteristic of a more “severe” KS phenotype.36,41,46 Additional studies have also demonstrated correlations of short CAG repeat length (high receptor activity) to longer penile length, higher bone density, and higher likelihood of having a stable partnership or professional employment.36,43,47 Not all studies have supported phenotypic correlations with CAG repeat number, however, including a study of 73 men with KS where there was no correlation with psychological phenotypic variation,38 and a study of 50 boys with KS where there was no relationship with cognitive or motor development.48
Genetic Counseling
Genetic counseling in KS is important in multiple settings, including in the setting of a prenatal diagnosis, pediatric/adolescent cases with a new diagnosis, and in adulthood. For parents with an intrauterine diagnosis of KS, it is important for them to know there is no increased risk for miscarriage.49 Prenatal or pediatric counseling should provide a comprehensive depiction of the phenotypic variability in KS, as well as include recommendations for developmental assessments/interventions, neuropsychological assessments/academic supports, social and emotional assessments/supports, indicated medical evaluations including endocrinology evaluation for testosterone replacement, current reproductive options, timing and approach to disclosure, and information regarding both local and national support groups.50
Counseling regarding fertility and options for fathering children in KS has changed significantly in the past decade with advancing reproductive technology. Historically the presence of infertility in KS was considered universal, and azoospermia continues to be present in the vast majority of men with KS. However, research has supported that up to 8% of men with KS have a small number of sperm in ejaculate,51,52 and there are rare case reports of spontaneous pregnancies. Much more promising is the current success rate of 50–60% in fathering biological children using advance reproductive techniques including microsurgical dissection of sperm from the testicle followed by in vitro fertilization, described in more detail in the endocrinology section below. While reported outcomes of children fathered from men with KS have been reassuring overall and most children have normal karyotypes, there have been slightly increased rates of children with KS and autosomal abnormalities reported. Pre-implantation genetic diagnosis is available.53 Due to a relatively young field, these risks require additional research. Regardless, it is important that counseling in all cases of KS emphasize updated information about successes in the field of fertility, since this is a significant area of concern for parents, adolescents, and adults with KS.54–56 It is also important to provide counseling related to other options for fatherhood chosen by many men with KS, including sperm donation and adoption.
Disclosure
With the advances in prenatal screening and increasing attention about KS in the medical literature, rates and ages of ascertainment are bound to improve. As such, pediatricians are often consulted by parents regarding decisions on when and how to disclose the diagnosis to the child. Research into other types of parent-to-child disclosures have identified barriers to communication causing possible avoidance of disclosure, including parents having difficulty understanding and/or being emotionally upset by the information, as well as being uncertain when and how to explain the information to the child and the child’s ability to understand.57–59 A recent study by Dennis et al evaluated the disclosure process of an SCA diagnosis from both parents and individuals, including 68 parents of males with XXY and 58 individuals with XXY.60 Study results identified important common themes and experiences, which led to formulation of recommendations supporting that the disclosure process include discussing the diagnosis gradually, honestly, and simply with age-appropriate terms and a positive attitude. Results further supported telling the child early, such as during childhood or before puberty, possibly prompted by when the child starts asking questions or if interventions are being pursued. Parents and individuals participating in this study encouraged the disclosure process to incorporate elements of support, including pointing out the child’s strengths, encouraging the child to ask questions, recognizing the common prevalence of the condition, and acknowledging research advancements and future possibilities.61 Resources for parents about disclosure are available at www.genetic.org.
Development, Behavior and Psychology
Early Development
There is significant variability in the developmental profiles of boys with KS, however there is an elevated risk for mild to moderate developmental delays for which monitoring is important so interventions can be implemented if needed. Prospective studies of infants with KS diagnosed by newborn screening identified speech-language delays in 75% and motor skills delays in 50%.62–65 Average age of milestones including first words and first steps are each approximately 2–3 months later compared to typical XY peers. While these delays are milder in comparison to other genetic disorders such as Fragile X or Down syndrome, speech and motor deficits do not generally resolve without therapies and thus early intervention is recommended upon identification of a delay in one or more developmental domains. In 25–50% of cases, early development progresses typically without significant developmental concerns or apparent need for intervention.
In young boys with speech delays, language testing most often shows a pattern with receptive language skills higher than expressive skills.62,66,67 An increased frequency of difficulties with oromotor planning and coordination called apraxia or dyspraxia of speech has also been described and can contribute to the expressive language delays in XXY.68 Language difficulties can take a toll early in the development of self-expression and can impact tolerance for frustration, regulation of interpersonal challenges and are often sited as likely contributory factors to behavioral concerns.69 Speech-language evaluation of the young child with KS should occur yearly for the first three years of life or upon diagnosis, and should include assessment of all language domains as well as evaluation for features of apraxia so that appropriate therapy techniques can be implemented.
Motor delays are present in about 50% of boys with KS, and hypotonia is commonly associated. 48,70 Other common features such as mild hypermobility, pes planus with ankle pronation and/or genu valgum can further affect motor development. Motor domains including dexterity, coordination, and graphomotor skills are commonly areas of weakness, which can then lead to difficulties with handwriting and self-care skills such as dressing, tying shoes, and eating.48,70,71 Physical and/or occupational therapy can be helpful for addressing motor and self-care difficulties. Orthotics are often prescribed for pes planus to support motor development and prevent lower extremity pain.
Cognitive, Language and Learning Profiles
Early studies of KS that reported increased rates of intellectual disability were flawed by ascertainment bias as they sampled populations from mental-health settings and long-term care facilities rather than a broader representative sample.72–75 Since that time, our understanding of the cognitive profile in KS has evolved, and studies have established that the average full scale IQ ranges from 90–100, with expected variability around the mean from low to above average following a standard distribution. 3,5,76 In this respect, many individuals with KS will not be significantly impacted by cognitive concerns and will achieve success in academic, personal, and career endeavors. On the other hand, statistically significant discrepancies have been shown relative to the general population and biological sibling controls. The overall mean for individuals with KS falls in the 90’s and 5 to 10 points lower than the population and sibling controls.66,77–79 In most studies, Verbal IQ scores are found to be lower than Performance/Nonverbal IQ scores and it is these deficits in the verbal conceptual domain that account for the downward skewing of Full Scale IQ.76 In this respect, nonverbal, visual perceptual, and spatial reasoning abilities are often an area of strength relative to verbal reasoning weaknesses.
Weaknesses in verbal skills align with speech-language profiles that commonly show difficulties in many language-related domains, and language disorders can be identified in 50–75% of boys with KS through adolescence.66,67,80 Generally, basic receptive and expressive vocabulary skills are intact. As language skills advance and become more complex, higher-level language deficits are common, including poor grasp of verbal concepts, verbal processing difficulties, slow verbal processing speed, decreased verbal fluency, word retrieval problems, social communication difficulties, and difficulty with open-ended narrative construction.62,66,78,80–83 Understanding the behavior of males with KS in the context of their language abilities is important, both in terms of processing language and formulating verbal responses. For example, slower verbal processing can make highly verbal situations such as classroom lectures or interpersonal interactions more challenging or anxiety-provoking, and difficulty with word-retrieval and/or language formulation can then affect speed and content of verbal responses in both educational and social settings. Speech-language therapy can continue to play an important role beyond early language development, and speech-language evaluation is recommended for all children and teens with KS displaying behavioral, social, or educational difficulties to determine if therapies addressing higher-level language skills and social/pragmatic language may be helpful.
In the school-aged years, boys with KS are at higher risk than the general population for language-based learning disabilities, including dyslexia.84,85 Occurrence ranges between 50 and 80%,62,66,79 and family history of learning disability increases this risk.86 More broadly, approximately 80% of boys with KS require some form of specialized support in school for language based learning or reading concerns.62 This is typically provided in the form of an Individualized Education Plan (IEP) or 504 plan, and it is strongly recommended that providers take an assertive stance with regard to advocating for intervention and educational supports. Lapses in support and intervention tend to create significant delays that are difficult to remediate. Evidence-based treatment approaches for reading disorders such as Linda-Mood-Bell or Orton-Gillingham are recommended, either through special education and/or private reading therapy. The high prevalence of learning disabilities in KS justifies periodic neuropsychological evaluation for all children with KS, starting in early grade school when early literacy is developing and deficits are simpler to address. Reassessment of cognitive and academic skills approximately every 3 years is then recommended, since deficits may not arise in some individuals until material becomes more complex and abstract with age. If lack of a formal learning disability diagnosis disqualifies a student from an IEP or educational supports, then advocating for services under the medical/health condition of KS with associated learning and executive functioning deficits is often successful to provide additional support.
Neuropsychological studies in KS have also consistently identified an increased risk for deficits in executive function (EF), including attention, working memory, cognitive flexibility, task initiation, fluency, and inhibition.87–91 Executive dysfunction can have broad effects across home, school, and occupational settings, where additional supports in initiating, organizing, and executing tasks and assignments are often needed. Recent research in KS has also linked decreased EF and inhibition to increased behavioral difficulties including aggression, rule-breaking behavior, and thought problems.92 Neuropsychological and educational assessment in KS should include direct evaluation of EF, and parents and teachers should be educated about behavioral manifestations of EF difficulties, as well as effective interventions and supports, which should be included as part of a comprehensive educational plan.
There is an increased risk for attentional problems, and ADHD diagnosis rates range from 36% to 63%.48,93,94 Distractibility and inattentive symptoms are more common than hyperactivity and impulsivity. It is important for children with KS who have attentional difficulties to have a neuropsychological evaluation that includes assessment of attention and EF, as well as other comorbidities that might present as inattention, such as learning disability, language disorder, or anxiety.78,95,96 There is a positive response to treatment of ADHD symptoms with stimulant or nonstimulant ADHD medication in approximately 75% of patients, and thus a trial of medication(s) should be recommended as per standard ADHD treatment guidelines. However, as with other neurodevelopmental disorders, medications should be started at a lower dose and advanced conservatively while monitoring for side effects, and the contribution of comorbidities such as anxiety or learning disabilities should be considered if there is poor medication response or side effects. In complex or difficult cases, referral to developmental pediatrics or child psychiatry for medication management is recommended.
Behavior/Social-Emotional Development
Studies report a range of behavioral features and psychological risks that can be associated with KS, including behavioral difficulties, social-emotional immaturity, low frustration tolerance, decreased self-esteem, emotional sensitivity, along with higher rates of anxiety and depressive concerns.5,56,69,92,97–100 As with other associated features, there is broad variability in the presence and severity of these symptoms between individuals with KS. Behavioral and emotional concerns should be screened for routinely, with referrals made for further psychological evaluation and therapy/counseling as needed. Counselors and therapists often have to modify therapeutic approaches due to the presence of language disorders and difficulties with self-expression, and thus identifying a therapist with experience working with children with delays or disabilities is helpful. Occupational therapy approaches to teach sensory-based self-regulation strategies are often less verbal and can be very successful for patients with KS throughout childhood. Psychopharmacologic medication treatment should be considered in childhood through adulthood to address behavioral or emotional regulation, anxiety, or depression if these symptoms are affecting home, school, and/or social functioning.
Social difficulties and elevated rates of autism symptoms have also been described in KS.83 Most studies have focused on describing autism symptoms which have identified features such as decreased social attention, decreased empathic skills, difficulty interpreting facial expressions, and social communication difficulties.67,101–103 Studies that have included direct diagnostic assessment for autism spectrum disorders (ASD) are more limited, and report a rate of 27% in a Dutch cohort (n=51) using a standardized diagnostic autism interview called the ADI-R,93 and a rate of 10% in an American cohort (n=20) using a battery including the ADI-R and direct assessment via the Autism Diagnostic Observation Scales (ADOS).5 Two other studies that evaluated rates of previous clinical ASD diagnosis in their cohort with KS also reported approximately 10% with ASD.67,101 Recent important studies comparing autism symptoms and neuroanatomy in XXY to a group with idiopathic autism demonstrated that although behavioral questionnaires indicated similar autism symptoms between the groups, there were significant neuroanatomical differences in XXY compared to idiopathic ASD, suggesting that autism symptoms in the respective groups may have, at least partially, different etiologies.103 Taken together, these studies support that ASD is an important clinical consideration in KS.
Screening for ASD should begin in early childhood as per the American Academy of Pediatrics recommendations, with referral for ASD assessment if indicated by screening results or if there are other concerns for ASD or social development raised by parents, teachers, or other providers. During assessment of social or ASD concerns, it is important and sometimes nuanced to differentiate the atypical social development and decreased reciprocity of ASD from social-emotional immaturity and/or expressive language deficits common in KS that can both also impact social relationships with peers. Further, it is common for concerns about ASD to become more apparent in boys with KS as social interactions become more complex beyond the first few years of life, and thus ASD evaluation should be included within a psychological evaluation for social or behavioral concerns. ASD diagnosis can be important in order to guide services and supports, as well as to help families, educators, and others better understand and support social development for the boy with KS.
Studies that drew subject-participation from clinical settings have reported elevated rates of a number of more complex psychiatric conditions, including bipolar disorder and psychotic spectrum disorders, with symptoms of paranoia, delusional thinking, and hallucinations.93,102,104 Hospitalization for disorders associated with psychosis is reported as small in KS, but increased over the general population. 105 Thus, providers should be aware of this increased risk and make referrals for psychiatric care if patients or parents bring up any concerns.
While we have emphasized many different cognitive, behavioral and social features that can be associated with KS, it is again important to emphasize the variability of the phenotype and the importance of also identifying areas of strengths and talent in each individual. While therapies and supports for areas of difficulty may be needed, it is equally important to encourage constructive opportunities for development in areas of strength and interest for positive self-esteem and quality of life. Parents should be encouraged to balance therapies and interventions with playtime, recreational or community activities, clubs/organizations that interest the child, and other positive activities.
Testicular Development and Function
One of the most commonly recognized features of KS is primary testicular insufficiency, which is present in the large majority of males with KS by early adulthood. The molecular mechanisms underlying this nearly universal manifestation remain elusive, however testicular development seems to be abnormal from very early in life.106 The normal testis is made up of germ cells, Leydig cells, and Sertoli cells. From the limited studies reporting testicular biopsies in KS, germ cells are reduced in number from infancy and the deficit appears to be progressive, particularly after puberty, with only rare pockets of active spermatogonia seen in adulthood.107 Evaluation of Leydig and Sertoli cell function largely relies on measurement of serum hormone concentrations. The Leydig cells produce testosterone, which has important local and systemic effects, and Sertoli cells produce inhibin B and anti-mullerian hormone (AMH), both of which have important local effects but unknown systemic effects. Assessment of serum hormone concentrations, particularly testosterone, is limited by assay variability, insensitivity of the assays in the hormone ranges typical of prepubertal children, and the observation that serum measurements do not necessarily accurately reflect intratesticular hormone concentrations. Regulation of gonadal function is primarily via the hypothalamic-pituitary-gonadal axis in which luteinizing hormone (LH) and follicle stimulating hormone (FSH) stimulate Leydig and Sertoli cells respectively. The hypothalamic-pituitary-gonadal axis is activated in the male during the first 2–3 months of life (often called the mini-puberty period of infancy), then again during puberty and remains active throughout the adult lifespan. There is overlap in testosterone levels in boys with and without KS, however males with KS on average seem to have lower serum testosterone (Figure 1).
Figure 1.
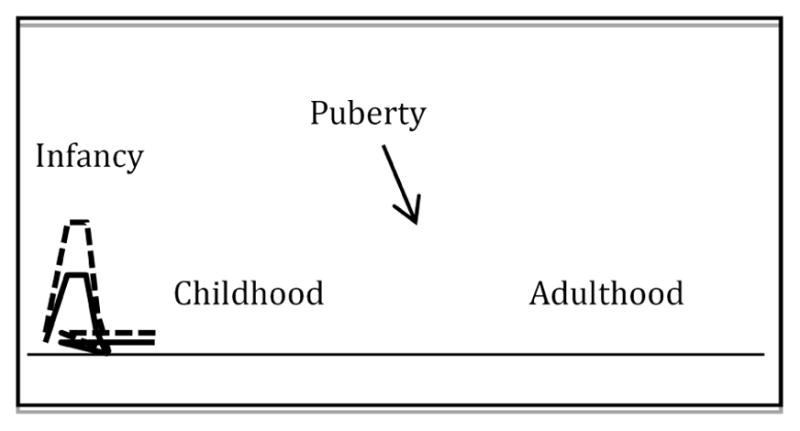
Graphical representation of testosterone concentrations throughout the lifespan in KS (solid) compared to typical 46,XY male (dashed).
Infancy
Hypogonadism in KS may start as early as fetal life or early infancy.108 Evidence to support this includes a higher prevalence of underdeveloped genitalia and cryptorchidism in infants, reduced germ cell number in testicular biopsies, smaller testicular size, and several studies suggesting a blunted testosterone surge during the mini-puberty period of infancy.109–112 Some endocrinologists measure testosterone, LH, and FSH around 6–12 weeks of life during the mini-puberty period of infancy. However, the mini-puberty period in the normal infant is vaguely defined, so it is not clear if this information has prognostic or management implications. Similarly, some providers will give testosterone during the first few months of life in infants with KS, however there is currently insufficient evidence to support this practice.113 Recent report of cognitive and behavioral benefits in males with KS who had previously received testosterone has stimulated a great deal of interest from families,114,115 however these findings have to be replicated with prospective, randomized study designs. A randomized trial of intramuscular testosterone during the mini-puberty period of infancy is currently enrolling (NCT#02408445).
Endocrine evaluation during infancy should include measurement of stretched penile length and documentation of bilateral descended testes. If micropenis is present (<1.9 cm from 0–6 months of life) or the family desires further discussion regarding endocrinologic manifestations in infancy, referral to a pediatric endocrinologist should be sought.116 If cryptorchidism (persistent > 6 months), inguinal hernia, or any other urogenital malformations are present, the infant should be referred to Urology.
Childhood
Before puberty in boys with KS, testicular volume is often less than 2mL and penile growth throughout childhood has been noted to be slow.40,117 The hypothalamic-pituitary-gonadal axis is quiescent in childhood, therefore, evaluation of LH, FSH and testosterone concentrations are generally not clinically useful. However, 10–20% of boys with KS may have prepubertal elevation of FSH, low inhibin B, and/or elevated AMH reflecting abnormal Sertoli cell function.118 Whether prepubertal Sertoli cell function is related to overall gonadal function in puberty and adulthood is yet to be determined. Results from a recently completed randomized controlled trial of oxandrolone (a non-aromatizable androgen) are expected soon. At this time, there are no recommendations for prepubertal hormonal evaluation or treatment.
Puberty
Most studies report a normal age of onset and tempo of early puberty in boys with KS.3,119 Testes begin to enlarge but typically reach a peak volume of no more than 10 mL and then decrease down to < 4 mL.120 Serum testosterone may rise appropriately in boys with KS in early puberty, but often eventually plateaus or even declines when serially monitored.121 FSH rises above the normal range on average a year after pubertal onset and LH approximately two years after pubertal onset. Endogenous testosterone usually supports virilization with penile enlargement and pubic hair development, although some young men with KS will not develop as much body or facial hair as would be expected for family. Fusion of the epiphyses may be delayed, contributing to tall stature. Gynecomastia probably occurs about as often as in pubertal boys without KS (~50%), however may be more likely to persist in KS.122,123 Physical examination should always include palpation for breast tissue, and if present warrants consideration of testosterone supplementation. The pathophysiology of gynecomastia is an abnormal testosterone to estrogen ratio, therefore aromatase inhibitors have been used, however a randomized controlled trial in pubertal boys with physiologic gynecomastia (not KS) did not find benefit of anastrozole compared to placebo.124 Estrogen receptor inhibitors (tamoxifen) have been reported in uncontrolled trials to reduce breast tissue size, however it is unclear if this is superior to the outcome without medication and no studies have been done in boys with KS.125 Surgery can be considered if gynecomastia fails to resolve with time and hormone manipulation, however surgery does have perioperative risks and gynecomastia can recur postoperatively.126
We recommend referral to an endocrinologist around 10 years of age or at the first sign of puberty, whichever is earliest. This initial visit is largely educational and establishes rapport. Boys with KS who have clinical signs of puberty should be monitored with pubertal examination and laboratory evaluation with serum LH, FSH, and testosterone approximately every 6 months. Currently there are no universally accepted guidelines for when (or if) to start androgen replacement. One option is waiting until clear biochemical and/or clinical evidence of hypogonadism with elevated LH, low or falling testosterone, and presence of gynecomastia, poor muscle mass, fatigue, or incomplete virilization. Another approach is to initiating low dose testosterone when LH has risen outside the normal range for pubertal development. A more aggressive option would be initiating testosterone in early puberty prior to any overt evidence of gonadal insufficiency. A randomized controlled trial that is currently enrolling hypothesizes psychosocial and motor benefits to low-dose testosterone treatment in early puberty (NCT#01585831). Until more evidence is available from research studies, the preference of the patient and parents should be greatly considered in determining the timing of androgen replacement.
Although there are many testosterone formulations available, options for adolescents are generally limited to depot injections of testosterone or topical testosterone gel, as other formulations do not allow for small enough dosing increments or are not well tolerated by adolescent boys.7 Injections have been used for decades and most endocrinologists are familiar with their use. Injections can be given at home or in the primary care physician’s office and dosing is typically titrated based on symptomatology and psychical examination. Disadvantages of injections include the presence of peaks and troughs in serum testosterone and the inconvenience and/or pain of shots. Topical testosterone gels are newer and may not be covered by all insurance carriers. If starting with gel, the smallest increment of the lowest potency available is recommended as the starting dose, with the goal of achieving serum testosterone conentrations in the normal range for pubertal stage. Disadvantages of gels include the need for daily application, skin irritation or sensory issues. Occasionally even the lowest available gel doses are too high for some pubertal boys, which may lead to elevated testosterone concentrations and subsequent rapid pubertal progression and/or premature fusion of the growth plates. Long-acting injections or testosterone pellets are being increasingly used in the US, however these are not recommended until late adolescence or adulthood when steady dose needs have been established.
Adulthood
The focus of this review precludes a comprehensive discussion on testicular function in adult men with KS. In brief, testicular size is universally small and usually firm as the germ cells that should make up the bulk of the testis volume in adults are profoundly reduced in KS.123 It is important to note, however, that the male genitalia otherwise has normal structure, size and function. Nearly all untreated men with non-mosaic KS will have elevated LH and FSH, with low or low-normal testosterone and low or undetectable inhibin B and AMH.7 Testosterone replacement should be offered to all men with evidence of hypergonadotropic hypogonadism even if they are asymptomatic, as many manifestations of gonadal insufficiency may be subtle. The Endocrine Society has published guidelines for testosterone replacement in men with hypogonadism.127
Azoospermia is nearly universal, however the concept of “universal infertility” in KS has drastically changed with the advanced reproductive technology technique of testicular sperm extraction (TESE) followed by intracytoplasmic sperm injection (ICSI).8 Using these techniques, small pockets of testicular tissue producing a few sperm can be identified during microsurgery, which are then extracted and injected through ICSI into a retrieved ovum, followed by in vitro fertilization. Currently, success rates of 50–75% are reported in adult men with KS seeking biological paternity using TESE and ICSI.128,129 Studies have not found consistent predictors for which individuals will be more likely to have success with TESE, although mosaicism with a 46,XY cell line may have a more favorable outcome and older age (particularly more than 30 years), has been reported to have a less favorable outcome.130,131 Many centers internationally have explored TESE for sperm cryopreservation from adolescents with KS, and current success rates do not consistently exceed those achieved in adulthood.128,132 Based on this evidence and the relative newness of the field, we recommend that families are informed of the active and promising research in this field, and that consultation with a reproductive urologist is offered for all interested families, adolescents, or adults with KS seeking more information and options related to fertility. Invasive procedures for fertility preservation in childhood or adolescents are not currently routine practice outside of research protocols, although this may change as technology advances. Also important, several studies report similar fertility potential for males with KS with previous exogenous testosterone exposure,128,129,131 therefore testosterone treatment should not be withheld from hypogonadal males for future fertility concerns.
Other Medical Issues
Insulin Resistance and Cardiovascular Disorders
Adults with KS are known to have a high prevalence of disorders related to insulin resistance including type 2 diabetes mellitus, dyslipidemia, and fatty liver disease.133 Metabolic syndrome, a constellation of signs including large waist circumference, dyslipidemia, elevated fasting blood glucose, and high blood pressure, is present in around 50% of men with KS.134–136 The presence of these conditions correlate with abnormal body composition (particularly abdominal adiposity) and hypogonadism. 136 Together, type 2 diabetes and cardiovascular diseases yield a standardized mortality ratio of 5.8 in adults with KS.137
Much less work has been done in children with KS, however recent studies have found a high prevalence of metabolic syndrome features as well as a high body fat percentage in this population.138,139 Importantly, features of metabolic syndrome in boys with KS appear to be independent of age or BMI. Counseling regarding a healthy diet and regular exercise is imperative from an early age. We recommend cholesterol screening with a fasting lipid panel in at age 9–11 years and after puberty is completed (consistent with American Academy of Pediatrics recommendations for all children), and sooner if additional risk factors are present.140 Lipid panel should be repeated in puberty if the previous panel was abnormal or additional risk factors are present such as obesity, untreated hypogonadism, or atypical antipsychotic use.
The risk of peripheral vascular disease and thromboembolic disease is increased in males with KS, resulting in significantly increased mortality.137 Venous stasis and recurrent leg ulcers are also quite common.141,142 Although these conditions are more common with age, we have had several adolescents with KS who developed venous thrombus in at-risk situations such as with a central venous catheter or surgery with immobilization. Consideration of prophylaxis measures should be considered if an adolescent or young adult is in a clinical situation that may predispose to clotting.
Bone Health
Studies in adult men with KS report lower bone mineral density and a higher morbidity and mortality from hip and spine fractures.137,143 It is speculated hypogonadism contributes to these findings, however a mouse model suggests the additional X chromosome itself results in abnormal bone structure.144 A single study in 18 children and adolescents with KS reports normal bone mineral density. 138 In our anecdotal experience, we have not seen a high prevalence of pathologic fractures in children and adolescents with KS, and we do not recommend routine evaluation of bone mineral density. We do recommend attention to standard pediatric guidelines and ensuring adequate calcium and vitamin D intake, regular physical exercise, maintaining a normal BMI, and tobacco avoidance.145 For post-pubertal boys with KS, maintenance of sex steroid levels in the normal range likely helps bone density.146 Chronic or unexplained back pain in an adolescent or adult with KS should raise concern for a vertebral compression fracture and appropriate evaluation undertaken.
Autoimmunity
Many case series and later epidemiological studies have reported an increased prevalence of several autoimmune diseases in KS compared to 46,XY males. A recent medical record linkage study of hospitalized men in England found significantly higher rates of several autoimmune diseases in men with KS including rheumatoid arthritis (RR 3.3), lupus, multiple sclerosis (RR18.1), Addison’s disease (RR 11.7), Sjogren’s syndrome (RR 19.3), autoimmune hypothyroidism (RR 2.7), and type 1 diabetes mellitus (RR 6.1).147 Although these are all significantly higher in adult men with KS compared to men in the general population, most of these autoimmune conditions are known to have a female predominance, and the risk of these autoimmune diseases is similar to women in the general population.148 No studies have evaluated autoimmune diseases in children with KS. Although screening for primary hypothyroidism is often recommended in KS,149 evidence is lacking to recommend this in pediatrics. It is important to be aware of the increased prevalence of autoimmunity in KS and evaluate if suggestive symptoms are present.
Malignancy
An excellent review of the literature of malignancies in KS was published in 2013.150 Despite abundant case reports, there are few epidemiological studies available. Because only a minority of males with KS are diagnosed before adulthood, the natural history of malignancies in children with KS is really not known. The three cancers that are consistently found to be more prevalent in KS compared to males in the general population are breast cancer, extragonadal germ cell tumors, and non-Hodgkin’s lymphoma. No routine screenings are recommended for any of these malignancies in childhood, but suspicious symptoms should be evaluated.
Breast cancer is around 20 times more common in men with KS compared to men without KS, however it is still less common than in women.151 Overall, breast cancer affects ~3–7% of men with KS,152,153 but is very rare in adolescents. Self exams as well as regular physician exams should be routine, and any palpable mass should be evaluated.
Extragonadal germ cell tumors are diagnosed in ~0.1% of males with KS, representing a large increased risk compared to the general population. Unlike breast cancer which does not typically present until adulthood, around half the reported cases of extragonadal germ cell tumors occur in pediatrics with a peak age in adolescence.154 Precocious puberty is the most common presenting symptom in boys <10 years of age, while cough, dyspnea or chest pain was most common in adolescents and adults given the most common tumor location is the mediastinum.155 If these symptoms are present, extragonadal germ cell tumor should be suspected evaluation pursued with a chest x-ray to evaluate for a mediastinal mass as well as measurement of serum β-HCG and alpha-fetoprotein.150
Finally, an association with non-Hodgkin’s lymphoma was reported in a large British cohort, particularly in boys with more than three sex chromosomes (48,XXYY), however this was not found in other studies and requires further investigation.151 There are many case reports of other hematological malignancies in males with KS, however epidemiological studies do not show an increased incidence or mortality from leukemias or other lymphomas in KS.156 It is important to keep in mind, however, that leukemia is most common cancer in childhood and therefore it would still be more likely for a boy with KS to develop leukemia than any of the other malignancies described above.
Other Medical Conditions
Congenital anomalies are more prevalent in infants with KS than in the general population and lead to a higher mortality.137 Congenital anomalies are much more common in boys with more than three sex chromosomes.157 The most frequently reported anomalies include inguinal hernia, congenital heart disease, cleft palate and velopharyngeal insufficiency, and kidney malformations. Dental conditions, particularly taurodontism and frequent caries possibly from enamel defects, are very common,24,158 and children with KS should have regular dental care.
Multiple case series have reported seizures in boys with KS, and a large epidemiological study from Britain found a standardized mortality ratio from epilepsy of 7.2 in males with KS compared to the general population.137 Seizures are present in 15% of males with 48,XXYY syndrome.24 Seizures can present at any age. Tremor is also noted, particularly in males with more than three sex chromosomes starting in adolescence.24,159
Little is reported in the literature on atopy in KS, however we appreciate a high prevalence of asthma and allergies in children with KS. In a study of 95 males with 48XXYY syndrome, 55 and 60% had allergies and asthma respectively.24 Death from chronic lower respiratory disease, which would include asthma, was twice as likely in men with KS compared to the general population in Britain. 137 Further investigation is needed to explore whether this is a true association.
In summary, KS is a common but under-diagnosed genetic condition with significant phenotypic variability in childhood. The pediatrician needs to be aware of the increased risk for neurodevelopmental, psychological, and medical conditions that are associated with an additional X chromosome. Over the next decade we anticipate a sharp increase in diagnoses rates with advances in genetics, particularly prenatal and neonatal diagnoses. In the US, more multidisciplinary clinics are being established to provide comprehensive care for children and adults with KS and other sex chromosome variations.96 More research is needed to further define the natural history of KS in infancy and childhood with these unbiased populations, as well as understand genetic and environmental contributors to phenotypic variability and determine best practice screening and management guidelines for boys with KS.
TABLE 1.
Pediatric Evaluation and Treatment Recommendations for XXY/Klinefelter syndrome
| Neurodevelopmental/Psychological Risk | Recommendation for Follow-Up and Further Evaluation |
|---|---|
|
| |
| Developmental delay (Age 0–3) |
|
|
| |
| Learning Disabilities |
|
|
| |
| ADHD/Executive functioning (EF) problems |
|
|
| |
| Speech-Language disorders |
|
|
| |
| Motor skills |
|
|
| |
| Social skills difficulties |
|
|
| |
| Emotional/Behavioral Difficulties, Anxiety |
|
|
| |
| Adaptive functioning problems |
|
|
| |
| Medical Features/Risks | Recommendation for Follow-Up and Further Evaluation |
|
| |
| Cardiovascular | |
| Congenital anomalies |
|
| Dyslipidemia |
|
| Abdominal obesity, fatty liver disease, insulin resistance, Metabolic syndrome |
|
|
| |
| Dental | |
| Enamel defects/caries Taurodauntism |
|
|
| |
| Endocrinologic | |
| Hypogonadism/Testosterone deficiency |
|
| Gynecomastia |
|
| Subfertility |
|
| Osteopenia/Osteoporosis |
|
|
| |
| Genetics |
|
|
| |
| Genitourinary | |
| Undescended testes, inguinal hernia, hypospadias |
|
| Microphallus |
|
|
| |
| GI/Feeding | |
| Newborn feeding difficulties |
|
| Reflux/Constipation/Abdominal complaints |
|
|
| |
| Hematology/Oncology | |
| Hypercoaguability |
|
| Malignancy risk |
|
|
| |
| Immunology | |
| Autoimmune diseases |
|
|
| |
| Musculoskeletal | |
| Pes Planus (Flat feet)/Ankle pronation |
|
| Tall stature |
|
|
| |
| Neurologic | |
| Seizures |
|
| Tremor |
|
|
| |
| Pulmonary | |
| Allergies/Reactive Airways/Respiratory Infections |
|
| Sleep Apnea |
|
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Shanlee Davis, University of Colorado School of Medicine Department of Pediatrics, Children’s Hospital Colorado, Department of Endocrinology, 13123 East 16th Ave B265, Aurora, CO 80045, Ph 720-777-6073, Fax 720-777-7301.
Susan Howell, University of Colorado School of Medicine Department of Pediatrics, Children’s Hospital Colorado, Developmental Pediatrics, 13123 East 16th Ave B140, Aurora, CO 80045, Ph 720-777-8361, Fax 720-777-7868.
Rebecca Wilson, Children’s Hospital Colorado, Developmental Pediatrics, 13123 East 16th Ave B140, Aurora, CO 80045, Ph 720-777-6630, Fax 720-777-7868.
Tanea Tanda, University of Colorado School of Medicine Department of Pediatrics, Children’s Hospital Colorado, Developmental Pediatrics, 13123 East 16th Ave B140, Aurora, CO 80045, Ph 720-777-7036, Fax 720-777-7868.
Judy Ross, Thomas Jefferson University School of Medicine Department of Pediatrics, A.I. DuPont Hospital for Children, 833 Chestnut St., Philadelphia, PA, 19107.
Philip Zeitler, University of Colorado School of Medicine Department of Pediatrics, Children’s Hospital Colorado, Department of Endocrinology, 13123 East 16th Ave B265, Aurora, CO 80045, Ph 720-777-6028, Fax 720-777-7301.
Nicole Tartaglia, University of Colorado School of Medicine Department of Pediatrics, Children’s Hospital Colorado, Developmental Pediatrics, 13123 East 16th Ave B140, Aurora, CO 80045, Ph 720-777-8087, Fax 720-777-7868.
References
- 1.Klinefelter HF, ECR, Albright F. Syndrome Characterized by Gynecomastia, Aspermatogenesis without Aleydigism, and Increased Excretion of Follicle-Stimulating Hormone. J Clin Endocrinol. 1942;2:615–627. [Google Scholar]
- 2.Lue Y, Rao PN, Sinha Hikim AP, et al. XXY male mice: an experimental model for Klinefelter syndrome. Endocrinology. 2001;142(4):1461–1470. doi: 10.1210/endo.142.4.8086. [DOI] [PubMed] [Google Scholar]
- 3.Robinson A, Bender BG, Linden MG, Salbenblatt JA. Sex chromosome aneuploidy: the Denver Prospective Study. Birth defects original article series. 1990;26(4):59–115. [PubMed] [Google Scholar]
- 4.Klinefelter HF. Klinefelter’s syndrome: historical background and development. Southern medical journal. 1986;79(9):1089–1093. [PubMed] [Google Scholar]
- 5.Tartaglia N, Cordeiro L, Howell S, Wilson R, Janusz J. The spectrum of the behavioral phenotype in boys and adolescents 47,XXY (Klinefelter syndrome) Pediatric endocrinology reviews: PER. 2010;8(Suppl 1):151–159. [PMC free article] [PubMed] [Google Scholar]
- 6.Rogol AD, Tartaglia N. Considerations for androgen therapy in children and adolescents with Klinefelter syndrome (47, XXY) Pediatric endocrinology reviews: PER. 2010;8(Suppl 1):145–150. [PubMed] [Google Scholar]
- 7.Davis SM, Rogol AD, Ross JL. Testis Development and Fertility Potential in Boys with Klinefelter Syndrome. Endocrinology and metabolism clinics of North America. 2015;44(4):843–865. doi: 10.1016/j.ecl.2015.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Plotton I, Brosse A, Cuzin B, Lejeune H. Klinefelter syndrome and TESE-ICSI. Annales d’endocrinologie. 2014;75(2):118–125. doi: 10.1016/j.ando.2014.04.004. [DOI] [PubMed] [Google Scholar]
- 9.Hook E. Prenatal Diagnosis and Screening. Edinburgh: Churchill Livingstone; 1992. Chromosome abnormalities: prevelence, risks and recurrence; pp. 351–392. [Google Scholar]
- 10.Nielsen J. Sex Chromosome Abnormalities found among 34,910 newborn children: results from a 13-year incidence study in Arhus, Denmark. Birth defects original article series. 1990;26(4):209–223. [PubMed] [Google Scholar]
- 11.Coffee B, Keith K, Albizua I, et al. Incidence of fragile X syndrome by newborn screening for methylated FMR1 DNA. American journal of human genetics. 2009;85(4):503–514. doi: 10.1016/j.ajhg.2009.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Herlihy AS, Halliday JL, Cock ML, McLachlan RI. The prevalence and diagnosis rates of Klinefelter syndrome: an Australian comparison. The Medical journal of Australia. 2011;194(1):24–28. doi: 10.5694/j.1326-5377.2011.tb04141.x. [DOI] [PubMed] [Google Scholar]
- 13.Bojesen A, Juul S, Gravholt CH. Prenatal and postnatal prevalence of Klinefelter syndrome: a national registry study. The Journal of clinical endocrinology and metabolism. 2003;88(2):622–626. doi: 10.1210/jc.2002-021491. [DOI] [PubMed] [Google Scholar]
- 14.Morris JK, Alberman E, Scott C, Jacobs P. Is the prevalence of Klinefelter syndrome increasing? Eur J Hum Genet. 2008;16(2):163–170. doi: 10.1038/sj.ejhg.5201956. [DOI] [PubMed] [Google Scholar]
- 15.Boyd PA, Loane M, Garne E, Khoshnood B, Dolk H group Ew. Sex chromosome trisomies in Europe: prevalence, prenatal detection and outcome of pregnancy. Eur J Hum Genet. 2011;19(2):231–234. doi: 10.1038/ejhg.2010.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abramsky L, Chapple J. 47,XXY (Klinefelter syndrome) and 47,XYY: estimated rates of and indication for postnatal diagnosis with implications for prenatal counselling. Prenatal diagnosis. 1997;17(4):363–368. doi: 10.1002/(sici)1097-0223(199704)17:4<363::aid-pd79>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 17.Visootsak J, Ayari N, Howell S, Lazarus J, Tartaglia N. Timing of diagnosis of 47,XXY and 48,XXYY: a survey of parent experiences. American journal of medical genetics. Part A. 2013;161A(2):268–272. doi: 10.1002/ajmg.a.35709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Meck JM, Kramer Dugan E, Matyakhina L, et al. Noninvasive prenatal screening for aneuploidy: positive predictive values based on cytogenetic findings. Am J Obstet Gynecol. 2015;213(2):214, e211–215. doi: 10.1016/j.ajog.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 19.Wang Y, Chen Y, Tian F, et al. Maternal mosaicism is a significant contributor to discordant sex chromosomal aneuploidies associated with noninvasive prenatal testing. Clinical chemistry. 2014;60(1):251–259. doi: 10.1373/clinchem.2013.215145. [DOI] [PubMed] [Google Scholar]
- 20.Tassone F. Newborn screening for fragile X syndrome. JAMA Neurol. 2014;71(3):355–359. doi: 10.1001/jamaneurol.2013.4808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jacobs PA, Strong JA. A case of human intersexuality having a possible XXY sex-determining mechanism. Nature. 1959;183(4657):302–303. doi: 10.1038/183302a0. [DOI] [PubMed] [Google Scholar]
- 22.MacDonald M, Hassold T, Harvey J, Wang LH, Morton NE, Jacobs P. The origin of 47,XXY and 47,XXX aneuploidy: heterogeneous mechanisms and role of aberrant recombination. Hum Mol Genet. 1994;3(8):1365–1371. doi: 10.1093/hmg/3.8.1365. [DOI] [PubMed] [Google Scholar]
- 23.Thomas NS, Hassold TJ. Aberrant recombination and the origin of Klinefelter syndrome. Human reproduction update. 2003;9(4):309–317. doi: 10.1093/humupd/dmg028. [DOI] [PubMed] [Google Scholar]
- 24.Tartaglia N, Davis S, Hench A, et al. A new look at XXYY syndrome: medical and psychological features. American journal of medical genetics. Part A. 2008;146A(12):1509–1522. doi: 10.1002/ajmg.a.32366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Peet J, Weaver DD, Vance GH. 49,XXXXY: a distinct phenotype. Three new cases and review. J Med Genet. 1998;35(5):420–424. doi: 10.1136/jmg.35.5.420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Berletch JB, Yang F, Disteche CM. Escape from X inactivation in mice and humans. Genome Biol. 2010;11(6):213. doi: 10.1186/gb-2010-11-6-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Berletch JB, Yang F, Xu J, Carrel L, Disteche CM. Genes that escape from X inactivation. Human genetics. 2011;130(2):237–245. doi: 10.1007/s00439-011-1011-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ottesen AM, Aksglaede L, Garn I, et al. Increased number of sex chromosomes affects height in a nonlinear fashion: a study of 305 patients with sex chromosome aneuploidy. American journal of medical genetics. Part A. 2010;152A(5):1206–1212. doi: 10.1002/ajmg.a.33334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vawter MP, Harvey PD, DeLisi LE. Dysregulation of X-linked gene expression in Klinefelter’s syndrome and association with verbal cognition. Am J Med Genet B Neuropsychiatr Genet. 2007;144B(6):728–734. doi: 10.1002/ajmg.b.30454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Huang J, Zhang L, Deng H, Chang L, Liu Q, Liu P. Global transcriptome analysis of peripheral blood identifies the most significantly down-regulated genes associated with metabolism regulation in Klinefelter syndrome. Molecular reproduction and development. 2015;82(1):17–25. doi: 10.1002/mrd.22438. [DOI] [PubMed] [Google Scholar]
- 31.Viana J, Pidsley R, Troakes C, et al. Epigenomic and transcriptomic signatures of a Klinefelter syndrome (47,XXY) karyotype in the brain. Epigenetics: official journal of the DNA Methylation Society. 2014;9(4):587–599. doi: 10.4161/epi.27806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.D’Aurora M, Ferlin A, Di Nicola M, et al. Deregulation of sertoli and leydig cells function in patients with klinefelter syndrome as evidenced by testis transcriptome analysis. BMC genomics. 2015;16:1356. doi: 10.1186/s12864-015-1356-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zitzmann M, Bongers R, Werler S, et al. Gene expression patterns in relation to the clinical phenotype in klinefelter syndrome. The Journal of clinical endocrinology and metabolism. 2015;100(3):E518–523. doi: 10.1210/jc.2014-2780. [DOI] [PubMed] [Google Scholar]
- 34.Rocca MS, Pecile V, Cleva L, et al. The Klinefelter syndrome is associated with high recurrence of copy number variations on the X chromosome with a potential role in the clinical phenotype. Andrology. 2016 doi: 10.1111/andr.12146. [DOI] [PubMed] [Google Scholar]
- 35.Tuttelmann F, Gromoll J. Novel genetic aspects of Klinefelter’s syndrome. Molecular human reproduction. 2010;16(6):386–395. doi: 10.1093/molehr/gaq019. [DOI] [PubMed] [Google Scholar]
- 36.Zinn AR, Ramos P, Elder FF, Kowal K, Samango-Sprouse C, Ross JL. Androgen receptor CAGn repeat length influences phenotype of 47,XXY (Klinefelter) syndrome. The Journal of clinical endocrinology and metabolism. 2005;90(9):5041–5046. doi: 10.1210/jc.2005-0432. [DOI] [PubMed] [Google Scholar]
- 37.Iitsuka Y, Bock A, Nguyen DD, Samango-Sprouse CA, Simpson JL, Bischoff FZ. Evidence of skewed X-chromosome inactivation in 47,XXY and 48,XXYY Klinefelter patients. American journal of medical genetics. 2001;98(1):25–31. [PubMed] [Google Scholar]
- 38.Skakkebaek A, Bojesen A, Kristensen MK, et al. Neuropsychology and brain morphology in Klinefelter syndrome - the impact of genetics. Andrology. 2014;2(4):632–640. doi: 10.1111/j.2047-2927.2014.00229.x. [DOI] [PubMed] [Google Scholar]
- 39.Nagai M, Kishi K, Kato S. Insular cortex and neuropsychiatric disorders: a review of recent literature. Eur Psychiatry. 2007;22(6):387–394. doi: 10.1016/j.eurpsy.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 40.Zeger MP, Zinn AR, Lahlou N, et al. Effect of ascertainment and genetic features on the phenotype of Klinefelter syndrome. J Pediatr. 2008;152(5):716–722. doi: 10.1016/j.jpeds.2007.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chang S, Skakkebaek A, Trolle C, et al. Anthropometry in Klinefelter Syndrome - Multifactorial Influences Due to CAG Length, Testosterone Treatment and Possibly Intrauterine Hypogonadism. The Journal of clinical endocrinology and metabolism. 2015;100(3):E508–517. doi: 10.1210/jc.2014-2834. [DOI] [PubMed] [Google Scholar]
- 42.Stemkens D, Roza T, Verrij L, et al. Is there an influence of X-chromosomal imprinting on the phenotype in Klinefelter syndrome? A clinical and molecular genetic study of 61 cases. Clinical genetics. 2006;70(1):43–48. doi: 10.1111/j.1399-0004.2006.00635.x. [DOI] [PubMed] [Google Scholar]
- 43.Wikstrom A, Painter J, et al. Genetic features of the X chromosome affect pubertal development and testicular degeneration in adolescent boys with Klinefelter syndrome. Clinical endocrinology. 2006 doi: 10.1111/j.1365-2265.2006.02554.x. [DOI] [PubMed] [Google Scholar]
- 44.Choong CS, Wilson EM. Trinucleotide repeats in the human androgen receptor: a molecular basis for disease. J Mol Endocrinol. 1998;21(3):235–257. doi: 10.1677/jme.0.0210235. [DOI] [PubMed] [Google Scholar]
- 45.Zitzmann M, Nieschlag E. The CAG repeat polymorphism within the androgen receptor gene and maleness. International journal of andrology. 2003;26(2):76–83. doi: 10.1046/j.1365-2605.2003.00393.x. [DOI] [PubMed] [Google Scholar]
- 46.Bojesen A, Hertz JM, Gravholt CH. Genotype and phenotype in Klinefelter syndrome - impact of androgen receptor polymorphism and skewed X inactivation. International journal of andrology. 2011;34(6 Pt 2):e642–648. doi: 10.1111/j.1365-2605.2011.01223.x. [DOI] [PubMed] [Google Scholar]
- 47.Zitzmann M, Depenbusch M, Gromoll J, EN X-chromosome inactivation patterns and androgen receptor functionality influence phenotype and social characteristics as well as pharmacogenetics of testosterone therapy in Klinefelter patients. The Journal of clinical endocrinology and metabolism. 2004;89(12):6208–6217. doi: 10.1210/jc.2004-1424. [DOI] [PubMed] [Google Scholar]
- 48.Ross JL, Roeltgen DP, Stefanatos G, et al. Cognitive and motor development during childhood in boys with Klinefelter syndrome. American journal of medical genetics. Part A. 2008;146A(6):708–719. doi: 10.1002/ajmg.a.32232. [DOI] [PubMed] [Google Scholar]
- 49.Hook EB, Topol BB, Cross PK. The natural history of cytogenetically abnormal fetuses detected at midtrimester amniocentesis which are not terminated electively: new data and estimates of the excess and relative risk of late fetal death associated with 47,+21 and some other abnormal karyotypes. American journal of human genetics. 1989;45(6):855–861. [PMC free article] [PubMed] [Google Scholar]
- 50.Dondorp W, de Wert G, Bombard Y, et al. Non-invasive prenatal testing for aneuploidy and beyond: challenges of responsible innovation in prenatal screening. Eur J Hum Genet. 2015;23(11):1438–1450. doi: 10.1038/ejhg.2015.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lanfranco F, Kamischke A, Zitzmann M, Nieschlag E. Klinefelter’s syndrome. Lancet. 2004;364(9430):273–283. doi: 10.1016/S0140-6736(04)16678-6. [DOI] [PubMed] [Google Scholar]
- 52.Selice R, Di Mambro A, Garolla A, et al. Spermatogenesis in Klinefelter syndrome. Journal of endocrinological investigation. 2010;33(11):789–793. doi: 10.1007/BF03350343. [DOI] [PubMed] [Google Scholar]
- 53.Staessen C, Tournaye H, Van Assche E, et al. PGD in 47,XXY Klinefelter’s syndrome patients. Human reproduction update. 2003;9(4):319–330. doi: 10.1093/humupd/dmg029. [DOI] [PubMed] [Google Scholar]
- 54.Puck MH, Bender BG, Borelli JB, Salbenblatt JA, Robinson A. Parents’ adaptation to early diagnosis of sex chromosome anomalies. American journal of medical genetics. 1983;16(1):71–79. doi: 10.1002/ajmg.1320160112. [DOI] [PubMed] [Google Scholar]
- 55.Gies I, Tournaye H, De Schepper J. Attitudes of parents of Klinefelter boys and pediatricians towards neonatal screening and fertility preservation techniques in Klinefelter syndrome. Eur J Pediatr. 2015 doi: 10.1007/s00431-015-2657-7. [DOI] [PubMed] [Google Scholar]
- 56.Turriff A, Levy HP, Biesecker B. Prevalence and psychosocial correlates of depressive symptoms among adolescents and adults with Klinefelter syndrome. Genetics in medicine: official journal of the American College of Medical Genetics. 2011;13(11):966–972. doi: 10.1097/GIM.0b013e3182227576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Metcalfe A, Coad J, Plumridge GM, Gill P, Farndon P. Family communication between children and their parents about inherited genetic conditions: a meta-synthesis of the research. Eur J Hum Genet. 2008;16(10):1193–1200. doi: 10.1038/ejhg.2008.84. [DOI] [PubMed] [Google Scholar]
- 58.Sutton EJ, Young J, McInerney-Leo A, Bondy CA, Gollust SE, Biesecker BB. Truth-telling and Turner Syndrome: the importance of diagnostic disclosure. J Pediatr. 2006;148(1):102–107. doi: 10.1016/j.jpeds.2005.08.022. [DOI] [PubMed] [Google Scholar]
- 59.Mac Dougall K, Becker G, Scheib JE, Nachtigall RD. Strategies for disclosure: how parents approach telling their children that they were conceived with donor gametes. Fertility and sterility. 2007;87(3):524–533. doi: 10.1016/j.fertnstert.2006.07.1514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Dennis A, Howell S, Cordeiro L, Tartaglia N. “How Should I Tell my Child?” Disclosing the Diagnosis of Sex Chromosome Aneuploidies. J Genet Couns. 2014 doi: 10.1007/s10897-014-9741-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tremblay I, Van Vliet G, Gonthier M, Janvier A. Partnering with parents to disclose Klinefelter syndrome to their child. Acta paediatrica. 2015 doi: 10.1111/apa.13301. [DOI] [PubMed] [Google Scholar]
- 62.Bender B, Fry E, Pennington B, Puck M, Salbenblatt J, Robinson A. Speech and language development in 41 children with sex chromosome anomalies. Pediatrics. 1983;71(2):262–267. [PubMed] [Google Scholar]
- 63.Linden MG, Bender BG. Fifty-one prenatally diagnosed children and adolescents with sex chromosome abnormalities. American journal of medical genetics. 2002;110(1):11–18. doi: 10.1002/ajmg.10394. [DOI] [PubMed] [Google Scholar]
- 64.Robinson A, Bender BG, Linden MG. Summary of clinical findings in children and young adults with sex chromosome anomalies. Birth defects original article series. 1990;26(4):225–228. [PubMed] [Google Scholar]
- 65.Ratcliffe SG. Speech and learning disorders in children with sex chromosome abnormalities. Developmental medicine and child neurology. 1982;24(1):80–84. doi: 10.1111/j.1469-8749.1982.tb13586.x. [DOI] [PubMed] [Google Scholar]
- 66.Graham JM, Jr, Bashir AS, Stark RE, Silbert A, Walzer S. Oral and written language abilities of XXY boys: implications for anticipatory guidance. Pediatrics. 1988;81(6):795–806. [PubMed] [Google Scholar]
- 67.Bishop DV, Jacobs PA, Lachlan K, et al. Autism, language and communication in children with sex chromosome trisomies. Archives of disease in childhood. 2011;96(10):954–959. doi: 10.1136/adc.2009.179747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Samango-Sprouse C, Rogol A. XXY The Hidden Disability and a Prototype for an Infantile Presentation of Developmental Dyspraxia (IDD) Infants and Young Children. 2002;15(1):11–18. [Google Scholar]
- 69.Bancroft J, Axworthy D, Ratcliffe S. The personality and psycho-sexual development of boys with 47 XXY chromosome constitution. Journal of child psychology and psychiatry, and allied disciplines. 1982;23(2):169–180. doi: 10.1111/j.1469-7610.1982.tb00061.x. [DOI] [PubMed] [Google Scholar]
- 70.Salbenblatt JA, Meyers DC, Bender BG, Linden MG, Robinson A. Gross and fine motor development in 47,XXY and 47,XYY males. Pediatrics. 1987;80(2):240–244. [PubMed] [Google Scholar]
- 71.Martin S, Cordeiro L, Richarson P, Davis S, Tartaglia N. The Association of Motor Skills and Adaptive Functioning in XXY/Klinefelter and XXYY Syndromes. doi: 10.1080/01942638.2018.1541040. Manuscript pending review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Eriksson B. Sex chromatin deviations among school children in special classes. A study of prevalence and an investigation of birth histories. J Ment Defic Res. 1972;16(2):97–102. doi: 10.1111/j.1365-2788.1972.tb01580.x. [DOI] [PubMed] [Google Scholar]
- 73.Singh DN, Osborne RA, Paul JR, et al. Cytogenetic survey of 504 mentally retarded individuals. J Ment Defic Res. 1974;18(4):293–305. doi: 10.1111/j.1365-2788.1974.tb01241.x. [DOI] [PubMed] [Google Scholar]
- 74.Bourgeois M, Benezech M. Cytogenic survey of 600 mentally retarded hospitalized patients. L’Encephale. 1977;3(3):189–202. [PubMed] [Google Scholar]
- 75.Johnston AW, Speed RM, Evans HJ. A chromosome survey of a population of mentally retarded persons. Birth defects original article series. 1974;10(10):30–35. [PubMed] [Google Scholar]
- 76.Leggett V, Jacobs P, Nation K, Scerif G, Bishop DV. Neurocognitive outcomes of individuals with a sex chromosome trisomy: XXX, XYY, or XXY: a systematic review. Developmental medicine and child neurology. 2010;52(2):119–129. doi: 10.1111/j.1469-8749.2009.03545.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ratcliffe SG, Masera N, Pan H, McKie M. Head circumference and IQ of children with sex chromosome abnormalities. Developmental medicine and child neurology. 1994;36(6):533–544. doi: 10.1111/j.1469-8749.1994.tb11884.x. [DOI] [PubMed] [Google Scholar]
- 78.Rovet J, Netley C, Keenan M, Bailey J, Stewart D. The psychoeducational profile of boys with Klinefelter syndrome. Journal of learning disabilities. 1996;29(2):180–196. doi: 10.1177/002221949602900208. [DOI] [PubMed] [Google Scholar]
- 79.Bender B, Puck M, Salbenblatt J, Robinson A. Cognitive development of children with sex chromosome abnormalities. San Diego: College Hill Press; 1986. [Google Scholar]
- 80.Netley C, Rovet J. Verbal deficits in children with 47,XXY and 47,XXX karyotypes: a descriptive and experimental study. Brain and language. 1982;17(1):58–72. doi: 10.1016/0093-934x(82)90005-0. [DOI] [PubMed] [Google Scholar]
- 81.Rovet J, Netley C, Bailey J, Keenan M, Stewart D. Intelligence and achievement in children with extra X aneuploidy: a longitudinal perspective. American journal of medical genetics. 1995;60(5):356–363. doi: 10.1002/ajmg.1320600503. [DOI] [PubMed] [Google Scholar]
- 82.Geschwind DH, Gregg J, Boone K, et al. Klinefelter’s syndrome as a model of anomalous cerebral laterality: testing gene dosage in the X chromosome pseudoautosomal region using a DNA microarray. Developmental genetics. 1998;23(3):215–229. doi: 10.1002/(SICI)1520-6408(1998)23:3<215::AID-DVG7>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 83.Bender BG, Linden MG, Robinson A. Verbal and spatial processing efficiency in 32 children with sex chromosome abnormalities. Pediatric research. 1989;25(6):577–579. doi: 10.1203/00006450-198906000-00004. [DOI] [PubMed] [Google Scholar]
- 84.Pennington BF, Bender B, Puck M, Salbenblatt J, Robinson A. Learning disabilities in children with sex chromosome anomalies. Child development. 1982;53(5):1182–1192. [PubMed] [Google Scholar]
- 85.Bender BG, Linden MG, Robinson A. Neuropsychological impairment in 42 adolescents with sex chromosome abnormalities. American journal of medical genetics. 1993;48(3):169–173. doi: 10.1002/ajmg.1320480312. [DOI] [PubMed] [Google Scholar]
- 86.Samango-Sprouse CA, Stapleton EJ, Mitchell FL, Sadeghin T, Donahue TP, Gropman AL. Expanding the phenotypic profile of boys with 47, XXY: the impact of familial learning disabilities. American journal of medical genetics. Part A. 2014;164A(6):1464–1469. doi: 10.1002/ajmg.a.36483. [DOI] [PubMed] [Google Scholar]
- 87.Boada R, Janusz J, Hutaff-Lee C, Tartaglia N. The cognitive phenotype in Klinefelter syndrome: a review of the literature including genetic and hormonal factors. Developmental disabilities research reviews. 2009;15(4):284–294. doi: 10.1002/ddrr.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Boone KB, Swerdloff RS, Miller BL, et al. Neuropsychological profiles of adults with Klinefelter syndrome. Journal of the International Neuropsychological Society: JINS. 2001;7(4):446–456. doi: 10.1017/s1355617701744013. [DOI] [PubMed] [Google Scholar]
- 89.Lee NR, Wallace GL, Clasen LS, et al. Executive function in young males with Klinefelter (XXY) syndrome with and without comorbid attention-deficit/hyperactivity disorder. Journal of the International Neuropsychological Society: JINS. 2011;17(3):522–530. doi: 10.1017/S1355617711000312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.van Rijn S, Swaab H, Magnee M, van Engeland H, Kemner C. Psychophysiological markers of vulnerability to psychopathology in men with an extra X chromosome (XXY) PloS one. 2011;6(5):e20292. doi: 10.1371/journal.pone.0020292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Temple CM, Sanfilippo PM. Executive skills in Klinefelter’s syndrome. Neuropsychologia. 2003;41(11):1547–1559. doi: 10.1016/s0028-3932(03)00061-7. [DOI] [PubMed] [Google Scholar]
- 92.van Rijn S, Swaab H. Executive dysfunction and the relation with behavioral problems in children with 47,XXY and 47,XXX. Genes, brain, and behavior. 2015;14(2):200–208. doi: 10.1111/gbb.12203. [DOI] [PubMed] [Google Scholar]
- 93.Bruining H, Swaab H, Kas M, van Engeland H. Psychiatric characteristics in a self-selected sample of boys with Klinefelter syndrome. Pediatrics. 2009;123(5):e865–870. doi: 10.1542/peds.2008-1954. [DOI] [PubMed] [Google Scholar]
- 94.Tartaglia N, Davis S, Hansen R, Hagerman R. Abstract: Attention deficit hyperactivity disorder and autism spectrum disorders in males with XXY, XYY, and XXYY syndromes. Journal of Intellectual Disability Research. 2006;50(11):787. [Google Scholar]
- 95.Tartaglia NR, Ayari N, Hutaff-Lee C, Boada R. Attention-deficit hyperactivity disorder symptoms in children and adolescents with sex chromosome aneuploidy: XXY, XXX, XYY, and XXYY. Journal of developmental and behavioral pediatrics: JDBP. 2012;33(4):309–318. doi: 10.1097/DBP.0b013e31824501c8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Tartaglia N, Howell S, Wilson R, et al. The eXtraordinarY Kids Clinic: an interdisciplinary model of care for children and adolescents with sex chromosome aneuploidy. J Multidiscip Healthc. 2015;8:323–334. doi: 10.2147/JMDH.S80242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Bender B, Harmon RJ, Linden MG, Robinson A. Psychosocial Adaptation in 39 Adolescents with Sex Chromosome Abnormalities. Pediatrics. 1995;96:302–308. [PubMed] [Google Scholar]
- 98.Visootsak J, Graham JM., Jr Social function in multiple X and Y chromosome disorders: XXY, XYY, XXYY, XXXY. Developmental disabilities research reviews. 2009;15(4):328–332. doi: 10.1002/ddrr.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Close S, Fennoy I, Smaldone A, Reame N. Phenotype and Adverse Quality of Life in Boys with Klinefelter Syndrome. J Pediatr. 2015;167(3):650–657. doi: 10.1016/j.jpeds.2015.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.van Rijn S, Stockmann L, Borghgraef M, et al. The social behavioral phenotype in boys and girls with an extra X chromosome (Klinefelter syndrome and Trisomy X): a comparison with autism spectrum disorder. Journal of autism and developmental disorders. 2014;44(2):310–320. doi: 10.1007/s10803-013-1860-5. [DOI] [PubMed] [Google Scholar]
- 101.Cordeiro L, Tartaglia N, Roeltgen D, Ross J. Social deficits in male children and adolescents with sex chromosome aneuploidy: a comparison of XXY, XYY, and XXYY syndromes. Research in developmental disabilities. 2012;33(4):1254–1263. doi: 10.1016/j.ridd.2012.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.van Rijn S, Swaab H, Aleman A, Kahn RS. X Chromosomal effects on social cognitive processing and emotion regulation: A study with Klinefelter men (47,XXY) Schizophr Res. 2006;84(2–3):194–203. doi: 10.1016/j.schres.2006.02.020. [DOI] [PubMed] [Google Scholar]
- 103.Goddard MN, Swaab H, Rombouts SA, van Rijn S. Neural systems for social cognition: gray matter volume abnormalities in boys at high genetic risk of autism symptoms, and a comparison with idiopathic autism spectrum disorder. Eur Arch Psychiatry Clin Neurosci. 2015 doi: 10.1007/s00406-015-0623-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.DeLisi LE, Maurizio AM, Svetina C, et al. Klinefelter’s syndrome (XXY) as a genetic model for psychotic disorders. Am J Med Genet B Neuropsychiatr Genet. 2005;135B(1):15–23. doi: 10.1002/ajmg.b.30163. [DOI] [PubMed] [Google Scholar]
- 105.Bojesen A, Juul S, Birkebaek NH, Gravholt CH. Morbidity in Klinefelter syndrome: a Danish register study based on hospital discharge diagnoses. The Journal of clinical endocrinology and metabolism. 2006;91(4):1254–1260. doi: 10.1210/jc.2005-0697. [DOI] [PubMed] [Google Scholar]
- 106.Mikamo K, Aguercif M, Hazeghi P, Martin-Du Pan R. Chromatin-positive Klinefelter’s syndrome. A quantitative analysis of spermatogonial deficiency at 3, 4, and 12 months of age. Fertility and sterility. 1968;19(5):731–739. [PubMed] [Google Scholar]
- 107.Wikstrom AM, Raivio T, Hadziselimovic F, Wikstrom S, Tuuri T, Dunkel L. Klinefelter syndrome in adolescence: onset of puberty is associated with accelerated germ cell depletion. The Journal of clinical endocrinology and metabolism. 2004;89(5):2263–2270. doi: 10.1210/jc.2003-031725. [DOI] [PubMed] [Google Scholar]
- 108.Fennoy I. Testosterone and the child (0–12 years) with Klinefelter syndrome (47XXY): a review. Acta paediatrica. 2011;100(6):846–850. doi: 10.1111/j.1651-2227.2011.02184.x. [DOI] [PubMed] [Google Scholar]
- 109.Lahlou N, Fennoy I, Ross JL, Bouvattier C, Roger M. Clinical and hormonal status of infants with nonmosaic XXY karyotype. Acta paediatrica. 2011;100(6):824–829. doi: 10.1111/j.1651-2227.2011.02280.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Cabrol S, Ross JL, Fennoy I, Bouvattier C, Roger M, Lahlou N. Assessment of Leydig and Sertoli cell functions in infants with nonmosaic Klinefelter syndrome: insulin-like peptide 3 levels are normal and positively correlated with LH levels. The Journal of clinical endocrinology and metabolism. 2011;96(4):E746–753. doi: 10.1210/jc.2010-2103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Lahlou N, Fennoy I, Carel JC, Roger M. Inhibin B and anti-Mullerian hormone, but not testosterone levels, are normal in infants with nonmosaic Klinefelter syndrome. The Journal of clinical endocrinology and metabolism. 2004;89(4):1864–1868. doi: 10.1210/jc.2003-031624. [DOI] [PubMed] [Google Scholar]
- 112.Ross JL, Samango-Sprouse C, Lahlou N, Kowal K, Elder FF, Zinn A. Early androgen deficiency in infants and young boys with 47,XXY Klinefelter syndrome. Hormone research. 2005;64(1):39–45. doi: 10.1159/000087313. [DOI] [PubMed] [Google Scholar]
- 113.Wosnitzer MS, Paduch DA. Endocrinological issues and hormonal manipulation in children and men with Klinefelter syndrome. American journal of medical genetics. Part C, Seminars in medical genetics. 2013;163C(1):16–26. doi: 10.1002/ajmg.c.31350. [DOI] [PubMed] [Google Scholar]
- 114.Samango-Sprouse CA, Sadeghin T, Mitchell FL, et al. Positive effects of short course androgen therapy on the neurodevelopmental outcome in boys with 47,XXY syndrome at 36 and 72 months of age. American journal of medical genetics. Part A. 2013;161A(3):501–508. doi: 10.1002/ajmg.a.35769. [DOI] [PubMed] [Google Scholar]
- 115.Samango-Sprouse C, Stapleton EJ, Lawson P, et al. Positive effects of early androgen therapy on the behavioral phenotype of boys with 47,XXY. American journal of medical genetics. Part C, Seminars in medical genetics. 2015;169(2):150–157. doi: 10.1002/ajmg.c.31437. [DOI] [PubMed] [Google Scholar]
- 116.Hatipoglu N, Kurtoglu S. Micropenis: etiology, diagnosis and treatment approaches. Journal of clinical research in pediatric endocrinology. 2013;5(4):217–223. doi: 10.4274/Jcrpe.1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Ratcliffe SG, Murray L, Teague P. Edinburgh study of growth and development of children with sex chromosome abnormalities. III. Birth defects original article series. 1986;22(3):73–118. [PubMed] [Google Scholar]
- 118.Davis S, Lahlou N, Bardsley MZ, Temple M, Kowal K, Ross JL. Longitudinal Study of Boys with Klinefelter Syndrome Gives Evidence of Prepubertal Testis Defect. The Endocrine Society; San Diego, CA: 2015. [Google Scholar]
- 119.Laron Z, Topper E. Klinefelter’s syndrome in adolescence. Archives of disease in childhood. 1982;57(11):887–888. doi: 10.1136/adc.57.11.887-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Salbenblatt JA, Bender BG, Puck MH, Robinson A, Faiman C, Winter JS. Pituitary-gonadal function in Klinefelter syndrome before and during puberty. Pediatric research. 1985;19(1):82–86. doi: 10.1203/00006450-198501000-00022. [DOI] [PubMed] [Google Scholar]
- 121.Bastida MG, Rey RA, Bergada I, et al. Establishment of testicular endocrine function impairment during childhood and puberty in boys with Klinefelter syndrome. Clinical endocrinology. 2007;67(6):863–870. doi: 10.1111/j.1365-2265.2007.02977.x. [DOI] [PubMed] [Google Scholar]
- 122.Mieritz MG, Raket LL, Hagen CP, et al. A Longitudinal Study of Growth, Sex Steroids, and IGF-1 in Boys With Physiological Gynecomastia. The Journal of clinical endocrinology and metabolism. 2015;100(10):3752–3759. doi: 10.1210/jc.2015-2836. [DOI] [PubMed] [Google Scholar]
- 123.Pacenza N, Pasqualini T, Gottlieb S, et al. Clinical Presentation of Klinefelter’s Syndrome: Differences According to Age. International journal of endocrinology. 2012;2012:324835. doi: 10.1155/2012/324835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Plourde PV, Reiter EO, Jou HC, et al. Safety and efficacy of anastrozole for the treatment of pubertal gynecomastia: a randomized, double-blind, placebo-controlled trial. The Journal of clinical endocrinology and metabolism. 2004;89(9):4428–4433. doi: 10.1210/jc.2004-0082. [DOI] [PubMed] [Google Scholar]
- 125.Lapid O, van Wingerden JJ, Perlemuter L. Tamoxifen therapy for the management of pubertal gynecomastia: a systematic review. Journal of pediatric endocrinology & metabolism: JPEM. 2013;26(9–10):803–807. doi: 10.1515/jpem-2013-0052. [DOI] [PubMed] [Google Scholar]
- 126.Fischer S, Hirsch T, Hirche C, et al. Surgical treatment of primary gynecomastia in children and adolescents. Pediatr Surg Int. 2014;30(6):641–647. doi: 10.1007/s00383-014-3508-8. [DOI] [PubMed] [Google Scholar]
- 127.Bhasin S, Cunningham GR, Hayes FJ, et al. Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. The Journal of clinical endocrinology and metabolism. 2010;95(6):2536–2559. doi: 10.1210/jc.2009-2354. [DOI] [PubMed] [Google Scholar]
- 128.Plotton I, d’Estaing SG, Cuzin B, et al. Preliminary Results of a Prospective Study of Testicular Sperm Extraction in Young Versus Adult Patients With Nonmosaic 47,XXY Klinefelter Syndrome. The Journal of clinical endocrinology and metabolism. 2015;100(3):961–967. doi: 10.1210/jc.2014-3083. [DOI] [PubMed] [Google Scholar]
- 129.Mehta A, Bolyakov A, Roosma J, Schlegel PN, Paduch DA. Successful testicular sperm retrieval in adolescents with Klinefelter syndrome treated with at least 1 year of topical testosterone and aromatase inhibitor. Fertility and sterility. 2013;100(4):970–974. doi: 10.1016/j.fertnstert.2013.06.010. [DOI] [PubMed] [Google Scholar]
- 130.Gies I, De Schepper J, Van Saen D, Anckaert E, Goossens E, Tournaye H. Failure of a combined clinical- and hormonal-based strategy to detect early spermatogenesis and retrieve spermatogonial stem cells in 47,XXY boys by single testicular biopsy. Human reproduction (Oxford, England) 2012;27(4):998–1004. doi: 10.1093/humrep/des002. [DOI] [PubMed] [Google Scholar]
- 131.Rohayem J, Fricke R, Czeloth K, et al. Age and markers of Leydig cell function, but not of Sertoli cell function predict the success of sperm retrieval in adolescents and adults with Klinefelter’s syndrome. Andrology. 2015;3(5):868–875. doi: 10.1111/andr.12067. [DOI] [PubMed] [Google Scholar]
- 132.Nahata L, Yu RN, Paltiel HJ, et al. Sperm Retrieval in Adolescents and Young Adults with Klinefelter Syndrome: A Prospective, Pilot Study. J Pediatr. 2015 doi: 10.1016/j.jpeds.2015.12.028. [DOI] [PubMed] [Google Scholar]
- 133.Jiang-Feng M, Hong-Li X, Xue-Yan W, et al. Prevalence and risk factors of diabetes in patients with Klinefelter syndrome: a longitudinal observational study. Fertility and sterility. 2012;98(5):1331–1335. doi: 10.1016/j.fertnstert.2012.07.1122. [DOI] [PubMed] [Google Scholar]
- 134.Gravholt CH, Jensen AS, Host C, Bojesen A. Body composition, metabolic syndrome and type 2 diabetes in Klinefelter syndrome. Acta paediatrica. 2011;100(6):871–877. doi: 10.1111/j.1651-2227.2011.02233.x. [DOI] [PubMed] [Google Scholar]
- 135.Bojesen A, Host C, Gravholt CH. Klinefelter’s syndrome, type 2 diabetes and the metabolic syndrome: the impact of body composition. Molecular human reproduction. 2010;16(6):396–401. doi: 10.1093/molehr/gaq016. [DOI] [PubMed] [Google Scholar]
- 136.Bojesen A, Kristensen K, Birkebaek NH, et al. The metabolic syndrome is frequent in Klinefelter’s syndrome and is associated with abdominal obesity and hypogonadism. Diabetes care. 2006;29(7):1591–1598. doi: 10.2337/dc06-0145. [DOI] [PubMed] [Google Scholar]
- 137.Swerdlow AJ, Higgins CD, Schoemaker MJ, Wright AF, Jacobs PA United Kingdom Clinical Cytogenetics G. Mortality in patients with Klinefelter syndrome in Britain: a cohort study. The Journal of clinical endocrinology and metabolism. 2005;90(12):6516–6522. doi: 10.1210/jc.2005-1077. [DOI] [PubMed] [Google Scholar]
- 138.Aksglaede L, Molgaard C, Skakkebaek NE, Juul A. Normal bone mineral content but unfavourable muscle/fat ratio in Klinefelter syndrome. Archives of disease in childhood. 2008;93(1):30–34. doi: 10.1136/adc.2007.120675. [DOI] [PubMed] [Google Scholar]
- 139.Bardsley MZ, Falkner B, Kowal K, Ross JL. Insulin resistance and metabolic syndrome in prepubertal boys with Klinefelter syndrome. Acta paediatrica. 2011;100(6):866–870. doi: 10.1111/j.1651-2227.2011.02161.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Daniels SR, Greer FR Committee on N. Lipid screening and cardiovascular health in childhood. Pediatrics. 2008;122(1):198–208. doi: 10.1542/peds.2008-1349. [DOI] [PubMed] [Google Scholar]
- 141.Seth A, Rajpal S, Penn RL. Klinefelter’s syndrome and venous thrombosis. The American journal of the medical sciences. 2013;346(2):164–165. doi: 10.1097/MAJ.0b013e31828318cd. [DOI] [PubMed] [Google Scholar]
- 142.Salzano A, Arcopinto M, Marra AM, et al. MANAGEMENT OF ENDOCRINE DISEASE: Klinefelter syndrome, cardiovascular system and thromboembolic disease. Review of literature and clinical perspectives. European journal of endocrinology/European Federation of Endocrine Societies. 2016 doi: 10.1530/EJE-15-1025. [DOI] [PubMed] [Google Scholar]
- 143.Bojesen A, Gravholt CH. Morbidity and mortality in Klinefelter syndrome (47,XXY) Acta paediatrica. 2011;100(6):807–813. doi: 10.1111/j.1651-2227.2011.02274.x. [DOI] [PubMed] [Google Scholar]
- 144.Liu PY, Kalak R, Lue Y, et al. Genetic and hormonal control of bone volume, architecture, and remodeling in XXY mice. J Bone Miner Res. 2010;25(10):2148–2154. doi: 10.1002/jbmr.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Bachrach LK. Diagnosis and treatment of pediatric osteoporosis. Curr Opin Endocrinol Diabetes Obes. 2014;21(6):454–460. doi: 10.1097/MED.0000000000000106. [DOI] [PubMed] [Google Scholar]
- 146.Jo DG, Lee HS, Joo YM, Seo JT. Effect of testosterone replacement therapy on bone mineral density in patients with Klinefelter syndrome. Yonsei medical journal. 2013;54(6):1331–1335. doi: 10.3349/ymj.2013.54.6.1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Seminog OO, Seminog AB, Yeates D, Goldacre MJ. Associations between Klinefelter’s syndrome and autoimmune diseases: English national record linkage studies. Autoimmunity. 2015;48(2):125–128. doi: 10.3109/08916934.2014.968918. [DOI] [PubMed] [Google Scholar]
- 148.Sawalha AH, Harley JB, Scofield RH. Autoimmunity and Klinefelter’s syndrome: when men have two X chromosomes. J Autoimmun. 2009;33(1):31–34. doi: 10.1016/j.jaut.2009.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Radicioni AF, Ferlin A, Balercia G, et al. Consensus statement on diagnosis and clinical management of Klinefelter syndrome. Journal of endocrinological investigation. 2010;33(11):839–850. doi: 10.1007/BF03350351. [DOI] [PubMed] [Google Scholar]
- 150.De Sanctis V, Fiscina B, Soliman A, Giovannini M, Yassin M. Klinefelter syndrome and cancer: from childhood to adulthood. Pediatric endocrinology reviews: PER. 2013;11(1):44–50. [PubMed] [Google Scholar]
- 151.Swerdlow AJ, Schoemaker MJ, Higgins CD, Wright AF, Jacobs PA, Group UKCC. Cancer incidence and mortality in men with Klinefelter syndrome: a cohort study. J Natl Cancer Inst. 2005;97(16):1204–1210. doi: 10.1093/jnci/dji240. [DOI] [PubMed] [Google Scholar]
- 152.Sasco AJ, Lowenfels AB, Pasker-de Jong P. Review article: epidemiology of male breast cancer. A meta-analysis of published case-control studies and discussion of selected aetiological factors. Int J Cancer. 1993;53(4):538–549. doi: 10.1002/ijc.2910530403. [DOI] [PubMed] [Google Scholar]
- 153.Brinton LA. Breast cancer risk among patients with Klinefelter syndrome. Acta paediatrica. 2011;100(6):814–818. doi: 10.1111/j.1651-2227.2010.02131.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Hasle H, Mellemgaard A, Nielsen J, Hansen J. Cancer incidence in men with Klinefelter syndrome. Br J Cancer. 1995;71(2):416–420. doi: 10.1038/bjc.1995.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Volkl TM, Langer T, Aigner T, et al. Klinefelter syndrome and mediastinal germ cell tumors. American journal of medical genetics. Part A. 2006;140(5):471–481. doi: 10.1002/ajmg.a.31103. [DOI] [PubMed] [Google Scholar]
- 156.Keung YK, Buss D, Chauvenet A, Pettenati M. Hematologic malignancies and Klinefelter syndrome. a chance association? Cancer Genet Cytogenet. 2002;139(1):9–13. doi: 10.1016/s0165-4608(02)00626-x. [DOI] [PubMed] [Google Scholar]
- 157.Tartaglia N, Ayari N, Howell S, D’Epagnier C, Zeitler P. 48,XXYY, 48,XXXY and 49,XXXXY syndromes: not just variants of Klinefelter syndrome. Acta paediatrica. 2011;100(6):851–860. doi: 10.1111/j.1651-2227.2011.02235.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Schulman GS, Redford-Badwal D, Poole A, Mathieu G, Burleson J, Dauser D. Taurodontism and learning disabilities in patients with Klinefelter syndrome. Pediatr Dent. 2005;27(5):389–394. [PubMed] [Google Scholar]
- 159.Lote H, Fuller GN, Bain PG. 48, XXYY syndrome associated tremor. Pract Neurol. 2013;13(4):249–253. doi: 10.1136/practneurol-2012-000438. [DOI] [PubMed] [Google Scholar]


