Abstract
This paper reports on the numbers of treatment cycles involved in the development of IVF (1969–1978) and their outcomes. We show that between 1969 and 1978: (i) a minimum of 282 women were involved in 495 cycles of potential laparoscopic oocyte retrieval (LOR); (ii) of these cycles, 457/495 proceeded to LOR to attempt egg collection; (iii) of which an outcome was recorded in 436/457; (iv) eggs were recovered in 388/436 of these; (v) inseminations were recorded in 331/388; (vi) embryos were recorded in at least 167; (vii) a total of 112 embryo transfers were attempted; and (viii) a maximum of 11 possible biochemical/preclinical pregnancies plus five clinical pregnancies were observed; (ix) from which two healthy live births resulted.
Keywords: embryo transfers, fertilisation rates, history of IVF, laparoscopic oocyte retrieval, pregnancy outcomes
Introduction
This paper is based upon data sets prepared from studying the L books and laparoscopy sheets, with cross-reference to notebooks T/D and FF in order to confirm dates or any missing information (Elder and Johnson, in this issue-a). Each patient is identifiable in the data by surname and laparoscopy cycle number when available. The same surnames can appear under different treatment cycle numbers, but, via reference to initials, first names and/or age and date of birth, we have been able to establish whether these are the same patients undergoing more than one treatment cycle or different patients who share the same surname. Laparoscopies are listed under 3-digit coding numbers; corresponding 6-digit hospital numbers are recorded separately in Notebook L0 for most patients from January 1969 to 23 March 1970 (L134-226) in blue ink, with the 3-digit L code evidently added later in red ink up to L216. In addition, the 6-digit hospital numbers appear for 89 patients on two sheets of paper (RGE1) with the title “All patients ever admitted to Dr Kershaw’s for oocytes”. By cross-reference to the data files, we deduce that this list represents patients treated during 1971, 1972, 1973 and 1974; we surmise that other named patients from this period, who do not feature on this list, were all treated in Oldham and District General Hospital (ODGH). One named patient from 1971, whose only record is that of a laparoscopy (recorded in Table 4 under a 6-digit number), does not appear elsewhere in any of the notebooks with a 3-digit code, and no further data regarding her cycle were found. Not all L-numbered cycles resulted in a laparoscopy for various reasons. It is also clear from the interview with Grace MacDonald (Suppl. Material: pp.9-10) and the Edwards’ papers (RGE2, 1978) that a number of patients had preliminary assessment laparoscopies without being given L numbers prior to being admitted to the IVF programme. These records are presumably included in the patient’s ODGH clinical notes (now lost) and are not within the data available to us. Throughout this paper, any dates given for cycles are those on which laparoscopy was recorded as having occurred (unless otherwise stated).
Table 4.
Number of attempted laparoscopic oocyte retrievals in which egg recovery was thwarted or for which the outcome was not recorded.
| Year | Reason for not proceeding or no data on outcome | Patients (n) | L number | P number |
|---|---|---|---|---|
| 1969 | – | – | – | – |
| 1970 | Converted to intra-tubal insemination or artificial insemination by husband | 3 | 199, 217, 218 | 34, 58, 59 |
| 1971 | Follicles were aspirated, but no data recorded | 1 | 296778 | 80 |
| 1972 | None | – | – | – |
| 1973 | Converted to artificial insemination Converted to intra-tubal insemination |
1 11 |
388 349, 357, 358, 368, 371, 372, 381, 383, 385, 389, 390 |
114 54, 121, 127, 121 125, 20, 125, 110 141, 143, 144 |
| 1974 | – | – | – | – |
| 1975 | – | – | – | – |
| 1976 | Ovaries not accessible | 3 | 499, 614, 622 | 212, 224, 232 |
| 1977 | – | – | – | – |
| 1978 | Ovaries not accessible | 2 | 680, 682 | 232, 213 |
| Total Thwarted Outcome not recorded |
21 20 1 |
– | – |
Results and discussion
Numbers of laparoscopies for oocyte retrieval
Records of attempted laparoscopic oocyte retrievals (LOR) extend from 9 January 1969 to the last, dated 1 August 1978, after which Steptoe retired from his National Health Service position and the Oldham unit closed (Edwards and Steptoe, 1980, p.155). Initial activity peaked in 1969/70, dipping between 1971 and 1975, before rising to a second peak in 1978 (see Table 5; a finer grained examination of these variations, and the possible explanations underlying them, is discussed in Paper V of this series; Johnson and Elder, 2015b).
Table 5.
Summary of recorded outcomes of laparoscopic oocyte retrieval cycles (LOR) by year.
| Year | Total no. of procedures found | No. of procedures in which LOR was scheduled (Table 1) | No. of LOR that proceeded to attempted egg collection (Table 3) | No. of LOR in which egg recovery was attempted and an outcome was recorded (Table 4) |
|---|---|---|---|---|
| 1969 | 60 | 58 | 58 | 58 |
| 1970 | 64 | 62 | 62 | 59 |
| 1971 | 46 | 41 | 41 | 40 |
| 1972 | 41 | 41 | 40 | 40 |
| 1973 | 45 | 44 | 38 | 26 |
| 1974 | 43 | 37 | 35 | 35 |
| 1975 | 40 | 36 | 34 | 34 |
| 1976 | 58 | 55 | 51 | 48 |
| 1977 | 43 | 43 | 33 | 33 |
| 1978 | 80 | 78 | 65 | 63 |
| Total | 520 | 495 | 457 (92% of scheduled LOR) | 436 (95% of attempts) |
The first laparoscopy is numbered L134 (Patient 1: P1) dated 9 January 1969. The missing numbers L1–133 may represent a series of laparoscopies performed by Steptoe prior to the systematic attempts at LOR, the starting date for which accords with the comment at the end of the Discussion in Edwards et al. (1969, published 13 February 1969; but received 13 December 1968): “Preliminary work using laparoscopy has shown that oocytes can be recovered from ovaries by puncturing ripening follicles in vivo … Improvements in equipment and techniques may give better results…”. The 3-digit cycle numbering runs from L134 to L747, with a few consecutive numbers missing and some duplicated (with a suffix of 'A' etc). The ‘L numbers’ were merged with a second set of ‘H’ numbers (for Hormones) during 1976, so that 99 ‘L numbers’ were skipped (Elder and Johnson, 2015a). In addition, one patient, whose monitoring is recorded under an ‘H number’, was not given an L number when the cycle was cancelled. We were able to find data for a total of 520 potential (numbered and un-numbered; named and unnamed) procedures in these notebooks.
Of the 520 procedures, in 25 cases the intention to proceed to LOR/IVF was apparently not the primary objective (Table 1). Of these 25 cases, follicles were aspirated in ovaries removed during hysterectomy/oophorectomy in one case (L169, P23: 1969) and in ovarian follicles in vivo, where present, in seven cases due for laparoscopic sterilization (1 × 1971, 3 × 1974, 1 × 1976, 2 × 1978). For two of the 1974 cases these oocytes were inseminated resulting in a single 16-cell embryo. We speculate that the remaining cases in Table 1 were given L numbers for the purpose of sample identification, as recorded in Notebook FF. L251/P74 (1970) records 21 names listed as ‘vasectomy patients’. These patients may be concerned with Edwards’ continuing contemporary interest in the immunology of reproduction (Johnson, 2011) and data from them may have contributed to the paper by Coombs et al. (1973) on anti-sperm antibodies after vasectomy. In 1973 and 1974, serum and semen samples for four males are recorded under L numbers (L386, 404, 405 and 406). L404 and 406 were partners of women undergoing treatment (L428/P125 and L401/P130, respectively); no treatment is recorded for women with the surnames for L386 and 405. We record these L numbers in Table 1 for a complete record, and none of these L numbers feature elsewhere in the paper. Notebook L7 records two patients without L numbers who had AIH treatment during 1976 (P227, 228). In addition, four cases are marked as 'sent to Addenbrookes to Mr Robinson' on which there are no further data. Thus we are left with 495 cycles scheduled for laparoscopic egg retrieval.
Table 1.
Patients identified by name or with an L number but not scheduled for laparoscopic oocyte retrieval/IVF in that cycle.
| Year | Procedure | Patients (n) | L number | P number |
|---|---|---|---|---|
| 1969 | Hysterectomy with oophorectomy (follicles pricked out post-operatively, one oocyte retrieved and stained) One unnamed patient recorded as ‘human control’ |
1 1 |
169 188 |
27 43 |
| 1970 | Laparotomy/adhesiolysis 21 names listed as ‘vasectomy patients’ under a single L number and assigned a single P numbera |
1 1 |
238 251a |
67 74 (M)a |
| 1971 | Hydrotubation Unnamed control natural cycle Diagnostic natural cycle Laparoscopic sterilization (no eggs recorded) |
1 1 2 1 |
293b 301 290, 291 293a |
104 106 100b, 101 103 |
| 1972 | None | – | – | – |
| 1973 | Blood tests + seminal anti-sperm antibodiesa | 1 | 386a | 142 (M) |
| 1974 | Anti-sperm antibodies testa Sperm preparation onlya Laparoscopic sterilizations (In 2/3 of these, follicles pricked out post-operatively yielded eggs that were inseminated; 1 × 16-cell embryo resulted) |
1 2 3 |
406a 404a, 405 414, 422, 425 |
130b (M) 125 & 153b (M), 159, 165, 167 |
| 1975 | 'Sent to Addenbrookes to Mr Robinson'a | 4 | 434–437 | 172–175 |
| 1976 | Laparoscopic sterilization (2 eggs recovered: nothing further recorded) Artificial insemination by husband |
1 2 |
497 No L-number |
210 227, 228b |
| 1977 | None | – | – | – |
| 1978 | Laparoscopic sterilizations (four eggs recovered; one fixed; nothing further recorded) | 2 | 677, 695 | 271, 283 |
| Total | 25 | – | – |
(M) indicates ‘patients’ were men, but nonetheless had L numbers; for patient nos. 125 and 130, the men were partners of female patients and assigned their female partner’s P number. For patient nos. 142 and 153, no female partners are evident and so these P numbers are unique to the men. The L numbers were perhaps assigned for the purpose of identifying their blood and semen samples in the records.
See text.
P numbers 100, 125, 130 and 228 are also included in Table 2, because they subsequently had cycles that were prepared for oocyte retrieval, which was not the case for any of the others in this table: P100 (cycles L340 and 399), P125 (L351 and 428), P130 (L366 and 401), and P228 (L715).
Patient numbers and ages
A total of 282 different patient names are identified in the records as scheduled for 495 LOR. These numbers mean that many patients were scheduled, monitored and/or treated for more than one LOR cycle, as summarized in Table 2. Whilst 60% were scheduled for only one LOR, a few were persistent, 21 (7%) volunteering for four or more. There is evidence from Notebook L0 that, when the same patients had two or three LOR cycles, this situation was used to compare outcomes for different stimulation regimes. Patient ages were found for 409 of the 495 possible cycles (83%), and range from 21 to 47 years (47 being an outlier destined for oophorectomy, see below), with a mean ± SD = 31.07 ± 4.48, the distribution being shown in Figure 1.
Table 2.
Number of scheduled treatment cycles per patient, of the 495 scheduled cycles for laparoscopic oocyte retrieval (LOR), for the 282 named patients.
| Scheduled LOR cycles (n) | Patients (n) | Total cycles (n) | Cumulative total of scheduled cycles (n) |
|---|---|---|---|
| 1 | 168 | 168 | 168 |
| 2 | 62 | 124 | 292 |
| 3 | 31 | 93 | 385 |
| 4 | 10 | 40 | 425 |
| 5 | 5 | 25 | 450 |
| 6 | 2 | 12 | 462 |
| 7 | 2 | 14 | 476 |
| 9 | 1 | 9 | 485 |
| 10 | 1 | 10 | 495 |
| Total | 282 | – | 495 |
LOR = laparoscopic oocyte retrieval.
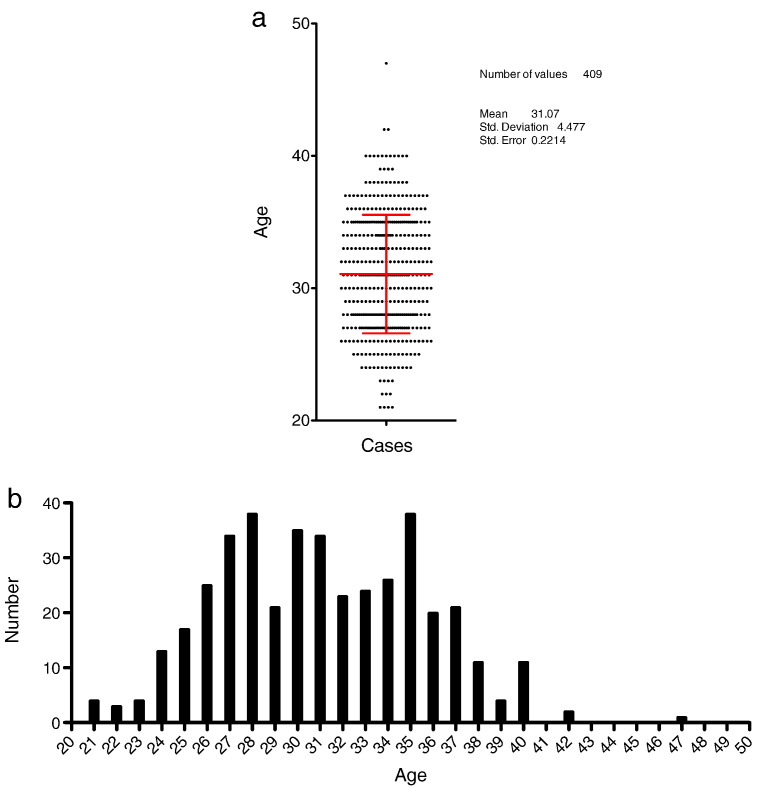
Figure 1.
(a) Plot showing mean and errors of the numbers of potential laparoscopy patients versus age of woman at the date of proposed laparoscopy for the 409 possible cycles for which data have been found; (b) a distribution plot of the same data. Note that the outlier aged 47 was the 1969 patient for oophorectomy (L169/P27; Table 1).
Outcomes
Of the 495 cycles for potential LOR, 38 patients had cycles cancelled prior to laparoscopy for various reasons, as summarized in Table 3, and discussed further in Elder and Johnson (2015b). Of the 457 scheduled treatment cycles that actually went to laparoscopy, 20 were either unsuccessful for various reasons (20/21; Table 4; see Elder and Johnson, 2015b, for discussion) or no data are available about the outcome (1/21; Table 4). This sub-classification of ‘exclusion’ is based on our own reading and interpretation of the data, which show that, for patients for whom the outcome is known, the LOR attempt success rate was 95% (436/457). Table 5 summarises the data from Table 1, Table 3, Table 4. The outcomes of the 436 cycles in which LOR was attempted (and for which we know the outcome) are shown in Table 6. Each of the data columns/lines in Table 6 will be discussed in relation to the underlying clinical objectives and will also be compared with contemporary published data.
Table 3.
Patients for whom laparoscopies were cancelled.
| Year | Stimulation/comment | Patients (n) | L number | P number |
|---|---|---|---|---|
| 1969 | None | – | – | – |
| 1970 | None | – | – | – |
| 1971 | None | – | – | – |
| 1972 | Pneumoperitoneum not achieved | 1 | 336 | 73 |
| 1973 | Clomid stimulation, converted to timed intercourse | 6 | 361–366 | 114, 128, 110, 129, 120, 130 |
| 1974 | Natural cycle + HCG, converted to intrauterine insemination | 1 | 392 | 4 |
| Natural cycle – Return to menstruation | 1 | 393 | 146 | |
| 1975 | Pergonal – poor response (static oestradiol) | 1 | 443 | 179 |
| Husband azoospermic | 1 | No lap no. | 36 | |
| 1976 | Pergonal – poor response | 2 | 481, 502 | 200, 69 |
| Pergonal – patient refused laparoscopy | 1 | 606 | 219 | |
| Pergonal – no reason recorded | 1 | 620 | 213 | |
| 1977 | Pergonal – converted to timed intercourse | 1 | 626 | 235 |
| Pergonal – poor response | 2 | 645, 655 | 250, 254 | |
| Pergonal – patient cancelled laparoscopy | 1 | 641 | 248 | |
| Pergonal – no reason recorded | 5 | 630–634 | 238–242 | |
| Pergonal + LH – no reason recorded | 1 | 643A | 222 | |
| 1978 | Natural cycle – no reason recorded | 1 | 702 | 286 |
| Natural cycle – infection | 1 | 742 | 302 | |
| Natural cycle – no surge detected | 11 | 670, 687, 693 699, 705, 711 726, 730, 732, 734, 747 |
227, 276, 282 284, 269, 234 288, 272, 262, 295, 48 |
|
| Total | 38 | – | – |
Table 6.
Summary of recorded outcomes of attempts at laparoscopic oocyte retrieval by year.
| Year |
Laparoscopic oocyte retrieval cycles (n) |
|||||
|---|---|---|---|---|---|---|
| In which outcome recorded (Table 5) |
In which egg recovery recorded (%) [Egg totals/follicles; %] |
In which insemination recorded (%) [Eggs inseminated/eggs recovered; %] |
In which embryos reported (%) [aEmbryo totals/eggs inseminated; %] |
In which embryo transfer recorded (%) |
In which pregnancy recorded |
|
| 1969 | 58 | 48 (83)b [136/407; 33] |
7 (12)c [27/136; 20] |
1 (3) [1/27; 4] |
0 | 0 |
| 1970 | 59 | 55 (93) [274/519; 53] |
51 (86) [272/274; 99] |
25 (42) [36/272; 13; + 3 × 2PN] |
0 | 0 |
| 1971 | 40 | 36 (90) [175/379; 46] |
36 (90) [175/175; 100] |
13 (33) [18/175; 10 + 1 × 2PN?] |
1 (3) | 0 |
| 1972 | 40 | 39 (98) [187/406; 46] |
35 (88) [179/187; 96] |
10 (25) [15/179 = 8; + 6 × 2PN & 1 × syngamy] |
5 (13; + 1 GIFT) | 0 |
| 1973 | 26 | 25 (96) [86/186; 46] |
20 (77) [81/86; 94] (5 egg + sperm to oviduct) |
8 (31) [8/81; 10; 2x2PN, 3 × 2PN?] |
7 (30; + 5 GIFT) | 0 |
| 1974 | 35 | 28 (80) [85/181; 47] |
28 (80)d [81/85; 95] |
10 (29)e [15/85; 18; + 1 x 2PN] |
9 (26; + 1 GIFT??)f | 0 |
| 1975 | 34 | 33 (97) [117/226; 52] |
33 (97) [117/117; 100] |
15 (44) [17/117; 15; + 1 x 2PN] |
11 (32) | 1 ectopic |
| 1976 | 48 | 44 (94)g [147/309; 48] |
44 (96) [149/149; 100] |
29 (61) [42/149; 29] |
27 (56)h | 1 × biochemical 9?? × EPL |
| 1977 | 33 | 28 (85) [97/220; 44] |
27 (82) [25xSC; 2 × NC] [95/97; 98] |
22 (67) [20xSC; 2xNC] [35/95; 37] |
21 (61) [19xSC; 2 × NC] |
1?? × EPL [SC] 1 × live birth [NC] |
| 1978 | 63 |
l52 (83) [57/97; 59] |
50 (79) [all NC] [60/61; 98] |
32 (54) [34/60; 57] |
31 (51)j | 2 × miscarriage 1 × live birth |
| Total | 436 | 388 (89) [1361/2926; 47] |
331 (76) [1237/1361; 91] |
165 (38) [221/1237; 18a] |
112 (26) [+ 6 (or 7?) GIFT = 29] |
5 clinical (1) [+ 11 possible pre-clinical = 3] |
% values calculated as a proportion of laparoscopic oocyte retrieval cycles with a known outcome.
EPL = early pregnancy loss; GIFT = gamete intrafallopian transfer; NC = natural cycle; SC = stimulated cycle.
i 2 sterilization cases yielded four eggs (not included).i 2 sterilization cases yielded four eggs (not included).
Embryo totals are unclear, especially in early years. Numbers therefore are minima.
The ovary removed in the hysterectomy case (Table 1) yielded 1 MII oocyte (not included).
In 2/7 cases, 5 inseminated eggs were transferred to rabbit oviducts.
In 2/3 of sterilization cases (Table 1), ovaries yielded four eggs that were inseminated (not included).
Plus one 16-cell embryo resulting from 1/4 sterilization eggs (not included).
Includes two embryo transfers via laparoscopy: one into fundus, one intraperitoneal.
one sterilization case produced two eggs (not included).
Includes three transfers via laparoscopy.
Includes one embryo transfer via mini-laparotomy.
Optimization of stimulation and egg recovery regimes
In 1969, the main aim was evidently to optimize both the stimulation regimes and egg recovery techniques. Follicles are recorded in the majority of laparoscopy notes, and egg recovery is documented in the L notebooks from 9 January 1969. However, in many of these cycles few eggs were recovered (column 3): no eggs (10/58 cycles), one egg (18/58 cycles) or two eggs (9/58 cycles), with three to eight eggs in only 21/58 cycles. Of the eggs recovered, those from many cycles are described as being immature, mostly at germinal vesicle (GV) stage or at metaphase I (MI; 14/58 cycles). MII eggs are described explicitly in only 7/58 cycles, often alongside immature forms and in some cases oocytes are described as degenerate or ‘unhappy’. We found no records relating to any egg recovery approaches used in either the notebooks or the loose clinical notes, but laparoscopic recovery details are described in Steptoe and Edwards (1970, p.684):
follicles appeared as thin-walled, bluish-pink rounded swellings from ½ to 3 cm in diameter
a medium-bore needle was introduced in the left lower abdomen…the aspiration needle fitted neatly through the medium-bore needle…
follicles were penetrated separately, their contents being collected in separate chambers…after each follicle had been aspirated, the needle and tubing were cleaned with heparinised saline solution…
and
After aspiration, the follicles rapidly filled with bloody fluid, very little of which escaped…
These descriptions appear to indicate that flushing of follicles, which was used subsequently at Bourn Hall, was not used at all in Oldham, and indeed there is no mention of flushing in any of the records, the clinical notes seeming to represent only a single sample from each follicle. Moreover, pictures of the ‘suction device’ used (see Figure 1 in Johnson and Elder, 2015b) does not show the three-way valve that would be required in order to flush follicles. Finally, Edwards et al. (1980) do not mention flushing under ‘aspiration of follicles’, and in fact suggest that there was only one aspirate from each follicle.
These early egg recoveries are presumably those described in Steptoe and Edwards (1970) and the eggs were mostly analysed structurally and chromosomally after fixation. Steptoe and Edwards (1970, published on 4 April, but submission date not recorded) described the recovery of eggs from 46–49 women (p.685: 46 in text at beginning of Results; 48 in Table 1; 49 in text at end of page) in 59 stimulation cycles. They reported the recovery of a total of 133 eggs from 118 out of 368 aspirated follicles (36%; pp.685–6). Of the 97 eggs examined in detail, the number described as clearly preovulatory was 42, of which only 12 (29%) were at MII. A reconciliation of these figures with our data is rendered difficult by the absence of dates for the cycles on which the 1970 paper is based. However, in 1969 egg recovery is recorded as being attempted in at least 58 cycles from 45 patients, close to the paper report of 59 cycles from 46–49 patients. Steptoe and Edwards (1970) also report an egg-per-follicle rate of 36% for the whole year, and we record 33% in Table 6 for 1969. Thus, it seems likely that the data in Steptoe and Edwards (1970) are based solely on 1969 data.
However, from 1970 onwards, most laparoscopy cycles not only went successfully to laparoscopy (Table 5), but approaching 50% of follicles yielded eggs (Table 6, column 3). Thus, a reasonable level of control of both the stimulation regime and the recovery technique was achieved swiftly.
Attempts at fertilization
The first attempts to fertilize laparoscopically recovered eggs are described in the records as being on 23 October 1969 (P42, one cycle) and 21 to 24 November 1969 (four cycles, P9, 46, 47, 48) (Table 6, column 4). On 8 December 1969, eggs from two further cycles were inseminated and then placed in rabbit oviducts on the following day, by which time all had developed pronuclei according to Edwards et al. (1970); these eggs were recovered on 10 December according to the data set, but no evidence of embryo development was reported therein. From 1970 onwards, eggs, where recovered, were inseminated in most LOR cycles, averaging 76% of cycles (for the whole period including 1969, but 95% if 1969 data are excluded). The insemination rate per egg over the whole period, including 1969, was 91%, and excluding 1969 was 98%.
Edwards et al. (1970, published in September, submitted on 25 August) describe a total of 212 recovered eggs, of which 35 were immature and 14 are described as ‘other’. Of the remaining eggs, 111 (52%) were unfertilized, while 52 (25%) were presumptively fertilized. The data books describe 53 of the 63 procedures listed for 1970 as having been completed by the end of August 1970, and up to this time 228 eggs had been collected. Of these, 36 are recorded as being fertilized so as to produce embryos, with a further three described as being pronuclear: a total of 39. This represents a fertilization rate of 17%. The under-representation in the data set compared with the published data is probably due to the fact that the data on fertilization are recorded only in the L notebooks and are difficult to interpret. When no record was found, the result was interpreted as meaning no fertilization had occurred.
Studies on embryo development
The sole post-fertilization embryo recorded in 1969 is of one egg, stage unspecified but described as ‘fert at 16 hrs’, from an LOR on 21 November (Table 6, column 5). Thereafter, the recorded rate of embryo recovery per oocyte inseminated was low and episodic, never rising above 18% until 1976 when it increased to 29%, rising to 57% by 1978 (average overall 17%; Table 6, column 5). However, the proportion of cycles yielding at least one embryo was much higher from 1970, ranging from 25% to 44% until 1976 from when it exceeded 50% (average overall 38%; Table 6, column 5). A total of 206 embryos were described, of which those from 1969 and 1970 were mostly studied after fixation by structural and chromosomal analysis.
Edwards et al. (1970) describe a total of 34 cleaving embryos, some dividing to 16 cells (7 × 3–4-cell; 16 × 5–8-cell; 11 × 8–16-cell or more). These data must come from those cycles in which insemination was followed by fertilization and embryo scoring in 1970, up to possibly the last cycle on 18 August before manuscript submission on 25 August (19/47 cycles) involving 17 patients. A total of 36 embryos are described in the data set for this period, with remarkably similar distributions of embryo classes, suggesting that these data were indeed used for the paper (8 × 3–4-cell; 18 × 5–8-cell; 10 × 9–16-cell/morula/blastocyst).
Steptoe et al. (1971, published in January, submitted in November 1970) described the advanced culture of six embryos to generate four blastocysts. Of these, two were described as having small cavities and too few cells, but two were well expanded, one with 112 nuclei and 'at least 16 mitoses' and the other with 110 nuclei. The first blastocysts described in the data set (and the only ones preceding the submission of the manuscript in November 1970) also number four from: L247 (P42; ‘?? Blastocyst? – citrate, squashed & fixed’; laparoscopy date 17 August), L248 (P38; ‘large blastocyst 21/8 – citrate, flattened, Ac Etoh’; laparoscopy date 17 August) and L253 (P49; ‘fully expanded blast – 112 nuclei, 18 mitoses; 2nd blast to Camb.’; laparoscopy date 24 September). Thus again, published papers correlate well with the data sets.
Embryo transfers
The first (16-cell) embryo transfer (ET) is recorded after a laparoscopy on 7 December 1971 for P75 (the 169th procedure in the data set), and was conducted 80 hours later, on December 12 1971, via a trans-cervical procedure. Thereafter, dated records of transfers are found every year between 1972 and 1978, increasing steadily year by year to reach in excess of 50% of successful LOR by 1976 (average overall 26%; Table 6, column 6). Altogether, 112 transfers were recorded as being attempted: five were carried out via laparoscopy, one via mini-laparotomy, and the remainder trans-cervically at 2, 3, 4 or 5 days after laparoscopy. In addition, one gamete intra-fallopian transfer (GIFT) procedure ('oocyte + sperm to oviduct') is recorded in 1972 (laparoscopy on 26 April); since a blastocyst and a morula are also recorded in vitro under this L number, we assume that at least two of the four eggs recovered were fertilized in vitro, and one or two used for GIFT. A further five GIFT procedures are recorded in 1973 (laparoscopies on 12 and 30 January and 1 February; L350-354: P38, 125, 114, 110 and 126). One case (L428/P125 (4)) is described in the notes with LOR of two eggs at 13:15 on 30 May 1974, inseminated immediately, and 'T to tube at 9 pm'; we are uncertain whether it was feasible to carry out a second laparoscopy for GIFT in the evening, 8 hours after LOR, or whether the tube in question was not an oviduct? So this case is recorded as ‘GIFT??’. In 1977/78, the majority of the ET are recorded as being carried out late on the evening of day 2, between 22:30 and 23:30, and embryo stages are recorded as 8–16-cell, some noted as 'compacting/?morula'. Some patients (13/91) went to ET in more than one cycle (See Table 7).
Table 7.
Outcomes of 112 embryo transfers (ET) carried out in 91 patients between December 1971 and July 1978.
| Embryo transfers per patient (n) | Patients (n) | Pregnancy outcome, year | ET number (P number) |
|---|---|---|---|
| 1 | 78 | Early pregnancy loss?? × 7, 1976 | 38 (202), 41 (204), 43 (185), 48 (211), 49 (131), 50 (213),55 (207) |
| Early pregnancy loss??, 1977 | 74 (257) | ||
| Biochemical pregnancy, 1976 | 56 (199) | ||
| Louise Brown born, 1978 | 81 (264) | ||
| Miscarriage, 1978 | 82 (267) | ||
| 2 | 9 | Early pregnancy loss??, 1976 | 45 (188) |
| Alastair Montgomery born, 1978 (2nd cycle) | 97 (247) | ||
| 3 | 2 | Miscarriage, 1978 (3rd cycle) | 109 (265) |
| 5 | 2 | Cornual ectopic, 1975 (2nd cycle) | 25 (38) |
| Early pregnancy loss??, 1976 | 54 (28) |
Pregnancies
The first clinical pregnancy is recorded in a Pergonal-stimulated cycle after laparoscopic recovery of four eggs on 19 June 1975, with ET on 23 June (L446/P38, the twenty-fifth ET; Table 6, column 7). This patient’s history is summarized in a typed sheet inserted into one of the notebooks, indicating a viable pregnancy on 14 August 1975. She had had two previous attempts at IVF on 11 August 1971 (L248) and on 13 June 1973 (L350). In July and August 1975, Edwards reported holidaying in the Yorkshire Dales (Edwards and Steptoe, 1980, p.125–6), when he heard from Patrick about this first positive pregnancy test, presumably this pregnancy, which was later found to be ectopic (Steptoe and Edwards, 1976), but no further record of what happened after 14 August has been found in the archived data.
During 1976, a possible biochemical pregnancy (HCG = 57) 2 weeks after ET is noted after a laparoscopy (L612/P199) on 18 September 1976 (also mentioned as occurring ‘after Spring’ in 1976 in Edwards and Steptoe, 1980, p.132–133). Also in 1976, a ‘cluster’ of seven patients (7/13 ET after laparoscopies between 15 June and 3 July, and two more on the 11 and 12 September) is noted as each having a late return to menstruation (RTM; 3–4 weeks post ET) with the comment 'passed material, ?foetal tissue, ?early abortion?'. In 1977, a further early pregnancy loss is recorded in a Pergonal-stimulated cycle after laparoscopy on 10 July 1977 and transfer of an 8-cell embryo on 12 July. 'Passed tissue ?decidua/ chorionic villi?' is noted on 5 August 1977. However, these cycles were during the period when Primolut and other luteal supports were being used (Edwards and Steptoe, 1980, pp.127–138; see also Elder and Johnson, 2015b). Moreover, handwritten histology reports for biopsies taken from three of these patients were present amongst the papers found at Edwards’ home, but these report only ‘decidual reaction, no evidence of embryonic or trophoblastic tissue’, and do not support the diagnosis of early pregnancy loss (RGE3, 1969–1977).
The laparoscopy that led to the first birth on 25 July 1978 (Edwards and Steptoe, 1980, Steptoe and Edwards, 1978, Steptoe et al., 1980) is recorded as a natural cycle (L666/P264: the eighty-first ET after the first ET) under the name Brown on 10 November 1977, with ET at 11.50 pm on 12 November. Transfer of an 8-cell embryo was reported as occurring at midnight on the 12 November in Edwards and Steptoe (1980, p.169–70).
The second birth followed a laparoscopy that was carried out under the name Montgomery on 20 May 1978 (L712/P247: the ninety-seventh transfer after the first ET), with transfer of 'a very nice 8c' at 11.15 pm on 23 May. Notes in book H9 report that the results of a pregnancy test were 'too low' on 16–17 July 1978 and 'LH dropped from 69,000 to 37,400; sl. discharge, brown, 11/6, 14/6, 30/6'. The patient concerned had an estimated delivery date of 14 February 1979, and her baby was born one month early, on 14 January 1979 (Steptoe et al., 1980). The patient has confirmed these dates orally to us (Suppl.Material: GM pp.21–23). Both babies resulted from non-stimulated, monitored natural cycles.
Two further pregnancies were established in natural cycles during 1978, but both miscarried. The first was after laparoscopy on 14 January, (L673/P267) with embryo transfer at 10.30 pm on 16 January. An ultrasound scan on 23 February showed a 9–10-week gestational sac, but there was no further growth by 1 March. Evacuation of retained products of conception (ERPOC) was carried out on 28 March, and the fetus was diagnosed as triploid (Steptoe et al., 1980). The second miscarriage occurred after laparoscopy on 16 July 1978 (L738/P268) and transfer of a 'beautiful 12-16c' embryo at 10.50 pm on 19 July. The patient was admitted to hospital on 17 November 1978, and suffered a spontaneous miscarriage on 26 November. “A living male fetus weighing 600 g was delivered at 5 months. He was normal and survived for two hours. Postmortem examination showed all systems to be normal.” (Steptoe et al., 1980).
General discussion
This account is the first to review objectively the work leading to the births of Louise Brown and Alastair Montgomery. Several issues are raised by our research. In this discussion we focus on the clinical outcomes and in the accompanying papers on the scientific, socio-ethical and logistic/financial aspects.
Numbers of patients and procedures
Hitherto, the actual number of patients and treatment cycles involved in the clinical work in Oldham has not been entirely clear. Corea (1985, p.113) claimed, on the basis of an unverified interview with Steptoe, that a total of ‘almost 80’ women were involved between 1971 and 1977, and that from 1977, using natural cycles, laparoscopies were performed on 68 women plus eight more transfers early in 1978 after two pregnancies had been confirmed (pp. 114–5): a total of 156 patients. Here we show that a larger number of women were involved, a minimum of 282 women being identified in connection with 495 prospective LOR cycles between 1969 and 1978.
It is possible to validate at least some of the numbers produced here by reference to those in papers published by Edwards and Steptoe (Table 8). Thus, with the exception of fertilization rates (see earlier for discussion as to why this might be), the data for 1969 and 1970 agree with published numbers in Steptoe and Edwards (1970), Edwards et al. (1970) and Steptoe et al. (1971). Likewise, the number of embryo transfers in stimulated cycles between the first transfer on 7 December 1971 and the last on 11 October 1977 is broadly supported in Steptoe et al. (1980). Thus, that paper reports in Table IX that in natural cycle patients, an LH surge was detected in 68/79 patients, and single egg recovery was achieved successfully in 45/68 patients. Fertilization failed in 10 of these and cleavage failed in three more, resulting in a total of 32 embryo transfers, and four clinical pregnancies. In comparison, the data set for monitored natural cycles between December 1977 and July 1978 records details for 81 cycles scheduled for 61 patients. Fifteen cycles did not go to LOR, leaving 66, from which eggs were found in 57. Eggs are recorded as 'tiny', damaged or degenerate in three cycles. Of the 54 inseminated eggs, the data do not make a clear distinction between 'failed fertilization' and 'failed cleavage', but 36 embryos are recorded for which transfer procedures are documented with date, time, and embryo stages for 34, two cycles having '2-4c' embryos on day 3, which were not transferred. 'Mock ET' was carried out in another two cycles in which embryos failed to develop.
Table 8.
A comparison of the numbers in the data set with those ascertained from various papers by Edwards, Steptoe and Purdy.
| Date | Data in notebooks | Data in papers | Reference |
|---|---|---|---|
| 1969 | 58 cycles, 46 patients | 59 cycles, 46–48 patients | Steptoe and Edwards (1970) |
| 7 December 1971 to 11 October 1977 (all stimulated cycles) | |||
| 268 cycles 24 cancelled = 244 (Table 3) 17 LOR thwarted = 227 (Table 4) 21 no eggs = 206 24 not inseminated = 182 123 no embryos = 59 79 embryo transfers |
77 embryo transfers | Edwards et al. (1980) | |
| 9 November 1977 to 1 August 1978 (all natural cycles) | |||
| 81 cycles (61 Patients) 66 to LOR (Table 3, Table 4) 57 eggs recovered 54 inseminated 36 embryos 34 embryo transfers |
79 ‘Patients’ = cycles 68 to LOR (Table IX) 45 eggs recovered 45 inseminated 32 embryos 32 embryo transfers |
Edwards et al. (1980) Table IX |
LOR = laparoscopic oocyte retrieval.
Likewise, for stimulated patients, Steptoe et al. (1980) report (p.742) “embryos were placed into a total of 77 … patients treated with gonadotrophins. The embryos were placed via the cervix in 74 of them, and surgically in three of them.” However, no data are presented for stimulated cycles in which ET was not attempted. The data set from the notebooks records a total of 72 ET after Pergonal-stimulated cycles, and seven ET between December 1973 and April 1974 in natural cycles + Pregnyl to induce ovulation: a total of 79 ET. These data are summarised in Table 8, which also records the unpublished information on non-ET cycles. Thus, where comparable data exist, the fit is reasonably good, which encourages us to believe that the non-published data are similarly correct. The other striking feature of the data is the pregnancy rate. The records indicate a total of 16 possible pregnancies, only five of which were clinical, and from which only two live births resulted. It could be argued with hindsight that, although providing proof of principle, these data offered a slim basis for launching the international IVF programmes that followed (Cohen et al., 2005), and for the change in funding attitude and policy by the Medical Research Council (Johnson et al., 2010). However, the independent report of a third IVF pregnancy and birth from Victoria, Australia (Lopata et al., 1980) was probably a crucial demonstration that, despite the difficulties, the approach could indeed deliver. Moreover, amid the hullabaloo attendant on Louise Brown’s birth, the relative rarity of this event was overlooked by the media. Indeed, the details were not immediately available until published by Steptoe et al. (1980), by which time the notion of ‘successful IVF’ was becoming firmly embedded.
The data on which our analysis is based are anonymised and recorded in The anonymised summary database on which much of this analysis is based, Explanatory details relating to the Supplementary Table. The scientific, ethical and social issues raised by these various data are described and analysed in the accompanying papers (Elder and Johnson, 2015b, Johnson and Elder, 2015a, Johnson and Elder, 2015b, Johnson and Elder, 2015c).
The following are the supplementary data related to this article.
Acknowledgements
We thank Grace MacDonald for giving us permission to publish the details contained in this paper and Dr Chi Wong for his help with data plotting. The research was supported by grants from the Wellcome Trust (088708, 094985 and 100606), which otherwise had no involvement in the research or its publication.
Biography

Kay Elder joined Bourn Hall in 1984 as Clinical Assistant to Patrick Steptoe, directing the Out-Patient Department from 1985 – 1987. Her scientific background as a research scientist at Imperial Cancer Research Fund prior to a medical degree at Cambridge University naturally led her to Bob Edwards and the IVF laboratory, where she worked as a senior embryologist from 1987. A programme of Continuing Education for IVF doctors, scientists and nurses at Bourn Hall was established in 1989, which she directed for 16 years. During this period she also helped to set up and run two Master’s degree programmes in Clinical Embryology, and she continues to mentor and tutor postgraduate students of Clinical Embryology at the University of Leeds. In her current role as Senior Research Scientist at Bourn Hall she co-ordinates research collaborations with the MRC Laboratory of Molecular Biology in Cambridge and the MRC National Institute for Medical Research in Mill Hill.
Contributor Information
Kay Elder, Email: kay.elder@bourn-hall.com.
Martin H. Johnson, Email: mhj21@cam.ac.uk.
References
- Cohen J., Trounson A., Dawson K., Jones H., Hazekamp J., Nygren K.G., Hamberger L. The early days of IVF outside the UK. Hum. Reprod. Update. 2005;11:439–459. doi: 10.1093/humupd/dmi016. [DOI] [PubMed] [Google Scholar]
- Coombs R.R.A., Rumke Ph., Edwards R.G. Immunoglobulin classes reactive with spermatozoa in the serum and seminal plasma of vasectomised and infertile men. In: Bratanov K., Edwards R.G., Vulchanov V.H., Dikov V., Somlev B., editors. Immunology of Reproduction. Bulgarian Academy of Sciences Press; Sofia: 1973. pp. 354–358. [Google Scholar]
- Corea G. Harper and Row; New York: 1985. The Mother Machine: Reproductive technologies from artificial insemination to artificial wombs. [Google Scholar]
- Edwards R.G., Steptoe P.C. The Story of IVF – a Medical Breakthrough; Hutchinson, London: 1980. A Matter of Life. [Google Scholar]
- Edwards R.G., Bavister B.D., Steptoe P.C. Early stages of fertilization in vitro of human oocytes matured in vitro. Nature. 1969;221:632–635. doi: 10.1038/221632a0. [DOI] [PubMed] [Google Scholar]
- Edwards R.G., Steptoe P.C., Purdy J.M. Fertilization and cleavage in vitro of preovulatory human oocytes. Nature. 1970;227:1307–1309. doi: 10.1038/2271307a0. [DOI] [PubMed] [Google Scholar]
- Edwards R.G., Steptoe P.C., Purdy J.M. Establishing full-term human pregnancies using cleaving embryos grown in vitro. Br. J. Obstet. Gynaecol. 1980;87:737–756. doi: 10.1111/j.1471-0528.1980.tb04610.x. [DOI] [PubMed] [Google Scholar]
- Elder K., Johnson M.H. The Oldham Notebooks: an analysis of the development of IVF 1969-1978. I. Introduction, Materials and Methods. Reprod. Biomed. Soc. 2015;1:3–8. doi: 10.1016/j.rbms.2015.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder K., Johnson M.H. The Oldham Notebooks: an analysis of the development of IVF 1969-1978. III. Variations in procedures. Reprod. Biomed. Soc. 2015;1:19–33. doi: 10.1016/j.rbms.2015.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson M.H. Robert Edwards: the path to IVF. Reprod. BioMed. Online. 2011;23:245–262. doi: 10.1016/j.rbmo.2011.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson M.H., Elder K. The Oldham Notebooks: an analysis of the development of IVF 1969-1978. IV. Ethical aspects. Reprod. Biomed. Soc. 2015;1:34–45. doi: 10.1016/j.rbms.2015.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson M.H., Elder K. The Oldham Notebooks: an analysis of the development of IVF 1969-1978. V. The role of Jean Purdy reassessed. Reprod. Biomed. Soc. 2015;1:46–57. doi: 10.1016/j.rbms.2015.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson M.H., Elder K. The Oldham Notebooks: an analysis of the development of IVF 1969-1978. VI. Sources of support and patterns of expenditure. Reprod. Biomed. Soc. 2015;1:58–70. doi: 10.1016/j.rbms.2015.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson M.H., Franklin S.B., Cottingham M., Hopwood N. Why the Medical Research Council refused Robert Edwards and Patrick Steptoe support for research on human conception in 1971. Hum. Reprod. 2010;25:2157–2174. doi: 10.1093/humrep/deq155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopata A., Johnston I., Hoult I., Speirs A. Pregnancy following intrauterine implantation of an embryo obtained by in vitro fertilization of a preovulatory oocyte. Fertil. Steril. 1980;33:117–120. doi: 10.1016/s0015-0282(16)44529-2. [DOI] [PubMed] [Google Scholar]
- RGE1 . Patient Matters, Folder 19. 1971. List of 89 patients (130 cycles) giving name, address and hospital number; described as “All patients ever admitted to Dr Kershaw’s for oocytes”. Each cycle is given a 4-digit hospital number. No date, but probably compiled in early 1971, as all but one patient appears elsewhere with a 3-digit L-number. [Google Scholar]
- RGE2 . Patient Matters, Folder 8. 1978. Patient question sheets contain evidence of at least two preliminary laparoscopic explorations on patients prior to them entering the programme. [Google Scholar]
- RGE3 . Patient Matters, Folder 11. 1969–77. Lists of approximately 120 curettings/biopsies from 1969–1977, plus lists of biopsies from 1970; includes hand written notes on the histopathology reports on 1977 pre-clinical pregnancies. [Google Scholar]
- Steptoe P.C., Edwards R.G. Laparoscopic recovery of preovulatory human oocytes after priming of ovaries with gonadotrophins. Lancet. 1970;i:683–689. doi: 10.1016/s0140-6736(70)90923-2. [DOI] [PubMed] [Google Scholar]
- Steptoe P.C., Edwards R.G. Reimplantation of a human embryo with subsequent tubal pregnancy. Lancet. 1976;i:880–882. doi: 10.1016/s0140-6736(76)92096-1. [DOI] [PubMed] [Google Scholar]
- Steptoe P.C., Edwards R.G. Birth after the reimplantation of a human embryo. Lancet. 1978;ii:366. doi: 10.1016/s0140-6736(78)92957-4. [DOI] [PubMed] [Google Scholar]
- Steptoe P.C., Edwards R.G., Purdy J.M. Human blastocysts grown in culture. Nature. 1971;229:132–133. doi: 10.1038/229132a0. [DOI] [PubMed] [Google Scholar]
- Steptoe P.C., Edwards R.G., Purdy J. Clinical aspects of pregnancies established with cleaving embryos grown in vitro. Br. J. Obstet. Gynaecol. 1980;87:757–768. doi: 10.1111/j.1471-0528.1980.tb04611.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.