Abstract
Objective
To study the temporal distribution and causes of hospitalizations after heart failure (HF) diagnosis.
Patients and Methods
Hospitalizations were studied in 1972 Olmsted County, Minnesota residents with incident HF from 2000 to 2011. All hospitalizations were examined for the 2 years following incident HF and each was categorized as due to HF, other cardiovascular, or non-cardiovascular causes. Negative binomial regression examined associations between time periods (0–30, 31–182, 183–365, and 366–730 days after diagnosis) and hospitalizations.
Results
Over the 2 years after diagnosis, 3495 hospitalizations were observed among 1336 of the 1972 HF patients. The age- and sex-adjusted rates of hospitalizations were highest in the first 30 days after index (3.33 per person-year vs. 1.33, 1.07, and 1.00 per person-year for 31–182, 183–365, and 366–730 days, respectively). The rates of hospitalizations were similar across sex, presentation of HF (inpatient, outpatient), and type of HF (preserved, reduced ejection fraction). Patients diagnosed as inpatients who had long hospital stays (>5 days) experienced more than a 30% increased risk of re-hospitalization within 30 days of dismissal. Importantly, most hospitalizations (64%) were due to non-cardiovascular causes and a minority (13%) were due to HF. The rates of non-cardiovascular hospitalizations were higher than HF or other cardiovascular hospitalizations across all follow-up for all time periods after HF.
Conclusion
Patients with HF experience high rates of hospitalizations, particularly within the first 30 days, and mostly for non-cardiovascular causes. To reduce hospitalizations in HF patients an integrated approach focusing on comorbidities will be required.
Keywords: heart failure, hospitalization, re-admission
INTRODUCTION
Heart failure (HF) is a major clinical and public health concern. The aging population and improved survival has led to the continued increase in HF prevalence, as well as the resulting high burden of hospitalizations and health care costs among individuals with HF.1 Notably, the course of HF is characterized by clinical exacerbations leading to hospitalizations.2 As such, the Hospital Readmissions Reduction Program, created under the Affordable Care Act, requires the Centers for Medicare and Medicaid Services (CMS) to reduce payments to hospitals with excess 30-day readmissions for HF. Most prior studies assessing rates of hospitalization in HF have restricted to patients with an initial hospitalization for HF, thus pooling incident and prevalent HF and missing patients diagnosed in the outpatient setting.3–5 There is a paucity of data describing rates of hospitalizations over the course of the HF syndrome after the initial diagnosis of HF, including patients who were diagnosed as outpatients.
In addition, most studies have a short follow-up of 30 days5 or 1 year after index.4,6 Thus, there is insufficient data to determine whether the first 30 days are the most important time frame for increased risk of hospitalization after HF diagnosis. In addition, a change in the case mix over the recent decade has resulted in an increased proportion of HF with preserved ejection fraction (EF).7 These recent community data suggest that the shift in case mix has resulted in an increase in hospitalizations for non-cardiovascular causes.7 This shift has profound implications for patients and clinicians, yet a full understanding of the patterns and distributions of types of hospitalizations over the course of the HF syndrome and whether these patterns are affected by EF remains largely unknown.
We aim to address the aforementioned gaps in knowledge by examining the patterns of hospitalizations over the course of the HF syndrome, identifying whether there are periods of increased vulnerability to hospitalizations, and assessing how these patterns may differ according to the case mix of HF (preserved or reduced EF) in a geographically defined community cohort of patients with HF.
METHODS
Study Population
This study was conducted in Olmsted County, Minnesota utilizing the resources of the Rochester Epidemiology Project (REP), a records-linkage system allowing virtually complete capture of health care utilization and outcomes in county residents.8–11 The retrieval of nearly all health care related events occurring in Olmsted County is possible because this area is relatively isolated from other urban centers, and few providers, including Mayo Clinic, Olmsted Medical Center, and their affiliated hospitals, deliver most health care to local residents. Demographic and ethnic characteristics of Olmsted County are representative of the state of Minnesota and the Midwest region of the US.9 Furthermore, broad disease trends and age- and sex-specific mortality rates in Olmsted County are similar to national data.9 This study was approved by the Mayo Clinic and Olmsted Medical Center Institutional Review Boards.
Identification of the Incident Heart Failure Cohort
HF diagnoses among Olmsted County residents between 2000 and 2011 were identified using International Classification of Diseases-9th Revision, Clinical Modification (ICD-9-CM) code 428 assigned during either an outpatient visit or a hospitalization.12,13 A random sample of 50% of the HF diagnoses given between 2000 and 2006 were selected and reviewed; 100% of the HF diagnoses given from 2007 to 2011 were reviewed. HF diagnoses were validated by trained nurse abstractors using the Framingham Criteria,14 and incidence status was determined after review of the entire medical record which, on average, spanned 4 decades.15 Patients with prevalent HF were excluded.
Clinical Data Collection
Clinical notes were reviewed to abstract height, weight, and smoking status at the time of incident HF. Body mass index (BMI) was calculated as weight (in kg) divided by height (in meters) squared. Comorbidities were ascertained electronically by retrieving inpatient and outpatient diagnostic codes and requiring at least 2 occurrences of a code (either the same code or 2 different codes within the same code set) within the 5 years prior to incident HF. The code sets were based on a modification of the Charlson comorbidities16,17 and were validated against manually abstracted data in 1418 incident HF patients (Supplemental Table 1). The closest serum creatinine value within 1 year of the index HF date was obtained and the estimated glomerular filtration rate (GFR) was calculated using the Modification of Diet in Renal Disease Study (MDRD) equation.18 Left ventricular ejection fraction (LVEF) (%) was determined using values collected from any echocardiogram, angiogram, multigated acquisition scan, or sestamibi scan performed within 3 months of the incident HF date. When multiple values were available, the value closest to the HF date was used; the average was used when multiple values were measured on the same day. HF with preserved EF was defined as LVEF greater than or equal to 50%, while HF with reduced EF was defined as LVEF less than 50%.19
Outcomes Ascertainment
All hospitalizations occurring within the 2 years following incident HF were obtained from the REP. The principal discharge diagnosis for each hospitalization was obtained and each hospitalization was categorized as due to HF (ICD-9 code 428), other cardiovascular causes (ICD-9 codes 390–427, 429–459), or non-cardiovascular causes.
Statistical Analysis
Analyses were performed using SAS statistical software, version 9.4 (SAS Institute Inc., Cary, NC). Characteristics of the patients with heart failure are provided as means and frequencies. Follow-up after the incident date of HF was divided into discrete time periods (epochs): 0–30, 31–182, 183–365, and 366–730 days. For patients who were hospitalized at incident HF, the date of discharge from the hospital was considered day 0. A likelihood ratio test revealed that overdispersion was present in the Poisson regression model; thus, negative binomial regression was used to estimate rates and rate ratios of hospitalizations by epochs of follow-up time. In addition, to assess the impact of survivor bias on the rates of hospitalization per epoch of follow-up time, a random effects generalized linear mixed model was run. The parameter estimates and rate ratios from the random effects model were nearly identical to estimates from the negative binomial model; thus, the negative binomial results are presented. Rates and rate ratios are presented overall, by sex, by presentation at incident HF (inpatient, outpatient), and by type of HF (preserved EF, reduced EF). In addition, separate negative binomial models were run to estimate rates and rate ratios by epochs of follow-up time for different types of hospitalization (due to HF, due to other cardiovascular causes, and due to non-cardiovascular causes). Finally, Cox proportional hazards regression models were used to determine predictors of hospitalization within the first 30 days after adjustment for age and sex.
RESULTS
Among the 1972 incident HF patients (mean age 76.3 years, 44.2% male), 46.4% had an EF <50% and 1344 (68%) were hospitalized at index (Table 1). Over the 2 year follow-up, 3495 hospitalizations were observed among 1336 patients, and 427 patients (32%) were hospitalized within 30 days of incident HF. Among those hospitalized within 30 days, the median time from HF to hospitalization was 9 days. The age- and sex-adjusted rates of hospitalizations were highest in the first 30 days after index (3.33 per person-year) and much lower thereafter (1.33, 1.07, and 1.00 per person-year for 31–182 days, 183–365 days, and 366–730 days, respectively; Table 2). No differences were observed between men and women, those who presented with incident HF as inpatients or outpatients, and those with preserved or reduced EF.
TABLE 1.
Baseline Characteristics of the Heart Failure Patients
| N=1972 | |
|---|---|
| Age, years mean ±SD | 76.3 ±13.5 |
| Male | 871 (44.2) |
| Body mass index mean ±SD, kg/m2 | 29.8 ±7.4 |
| Smoking status | |
| Never | 852 (43.2) |
| Current | 244 (12.4) |
| Former | 876 (44.4) |
| Ejection fraction <50% | 730 (46.4) |
| Estimated glomerular filtration rate | |
| mean ±SD, mL/min per 1.73 m2 | 59.9 ± 23.6 |
| Hospitalized at index | 1344 (68.2) |
| Hypertension | 1551 (78.7) |
| Diabetes | 606 (30.7) |
| Myocardial infarction | 380 (19.3) |
| Cerebrovascular disease | 415 (21.0) |
| Peripheral vascular disease | 218 (11.1) |
| Chronic obstructive pulmonary disease | 376 (19.1) |
| Renal disease | 191 (9.7) |
| Liver disease | 36 (1.8) |
| Dementia | 121 (6.1) |
| Rheumatologic disease | 116 (5.9) |
| Hemiplegia/paraplegia | 57 (2.9) |
| Malignancy | 370 (18.8) |
| Metastatic solid tumor | 66 (3.3) |
Values are N (%) for categorical variables and mean (SD) for continuous variables.
TABLE 2.
Ratesa of Hospitalizations by Time Period after Incident Heart Failure
| 0–30 Days | 31–182 Days | 183–365 Days | 366–730 Days | P-valueb | |
|---|---|---|---|---|---|
| Overall | 3.33 | 1.33 | 1.07 | 1.00 | --- |
| Sex | .92 | ||||
| Male | 3.46 | 1.38 | 1.11 | 1.04 | |
| Female | 3.24 | 1.29 | 1.04 | 0.97 | |
| Presentation at Incident Heart Failure | .13 | ||||
| Inpatient | 3.68 | 1.46 | 1.19 | 1.10 | |
| Outpatient | 2.64 | 1.05 | 0.85 | 0.79 | |
| Heart Failure Typec | .34 | ||||
| Preserved EFd | 3.70 | 1.42 | 1.11 | 0.99 | |
| Reduced EFd | 3.59 | 1.38 | 1.08 | 0.96 | |
Rates per person-year. Sex-specific rates are adjusted for age; the remaining rates are adjusted for age and sex.
P-interaction.
Rates are among the 1574 (79.8%) patients who had ejection fraction measured.
EF = Ejection Fraction
After adjusting for demographics and comorbidities, the rate ratios for hospitalizations were significantly lower for the later time periods compared to the first 30 days (Table 3). Overall, compared to the first 30 days after HF, the rate ratios (RR) (95% confidence interval (CI)) were 0.39 (0.35–0.45), 0.32 (0.28–0.36), and 0.29 (0.26–0.33) for 31–182 days, 183–265 days, and 366–730 days after HF index, respectively. The rate ratios were similar across sex, presentation, and HF type.
TABLE 3.
Rates Ratiosa (95% CI) of Hospitalizations by Time Period after Incident Heart Failure
| 0–30 Days | 31–182 Days | 183–365 Days | 366–730 Days | P-valueb | |
|---|---|---|---|---|---|
| Overall | 1.00 (ref) | 0.39 (0.35–0.45) | 0.32 (0.28–0.36) | 0.29 (0.26–0.33) | --- |
| Sex | .95 | ||||
| Male | 1.00 (ref) | 0.39 (0.33–0.47) | 0.32 (0.27–0.39) | 0.30 (0.24–0.36) | |
| Female | 1.00 (ref) | 0.39 (0.34–0.46) | 0.31 (0.26–0.37) | 0.30 (0.25–0.35) | |
| Presentation at Incident Heart Failure | .12 | ||||
| Inpatient | 1.00 (ref) | 0.42 (0.37–0.49) | 0.32 (0.27–0.37) | 0.31 (0.27–0.36) | |
| Outpatient | 1.00 (ref) | 0.33 (0.26–0.41) | 0.32 (0.25–0.40) | 0.26 (0.21–0.33) | |
| Heart Failure Typec | .35 | ||||
| Preserved | 1.00 (ref) | 0.43 (0.36–0.51) | 0.32 (0.27–0.39) | 0.29 (0.24–0.34) | |
| Reduced | 1.00 (ref) | 0.33 (0.27–0.40) | 0.27 (0.22–0.33) | 0.23 (0.19–0.28) | |
Rate ratios are adjusted for age, sex (except sex-specific models), body mass index, hypertension, diabetes, prior myocardial infarction, chronic pulmonary disease, cerebrovascular disease, peripheral vascular disease, renal disease, liver disease, hemiplegia, metastatic and nonmetastatic cancers (excluding nonmelanoma skin cancers), estimated glomerular filtration rate, and smoking.
P-interaction.
Rate ratios are among the 1574 (79.8%) patients who had ejection fraction measured.
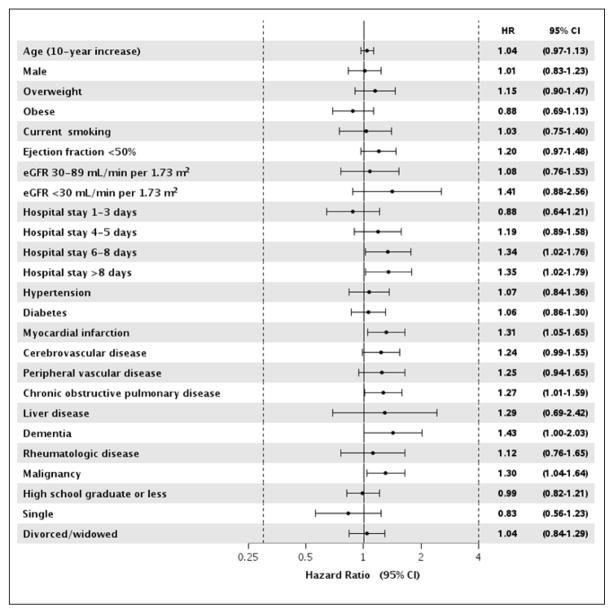
After adjustment for age and sex, the following comorbidities were predictive of being re-hospitalized within the first 30 days: prior myocardial infarction and the presence of chronic obstructive pulmonary disease, cancer, and dementia (Figure 1). In addition, patients who were diagnosed with HF as an inpatient and whose hospital stay was more than 5 days experienced more than a 30% increased risk of re-hospitalization within 30 days compared to those who were diagnosed with HF as an outpatient.
Figure 1. Age- and sex-adjusted predictors of hospitalizations within the first 30 days after incident heart failure.
The estimate for age is adjusted for sex and the estimate for sex is adjusted for age; all other estimates are adjusted for age and sex.
The majority of hospitalizations were due to non-cardiovascular causes (63.6% vs. 12.6% due to HF, and 23.8% due to other cardiovascular causes; Table 4). However, a larger proportion of HF and other cardiovascular hospitalizations were observed within the first 30 days (51.5% non-cardiovascular, 16.6% HF, 31.9% other cardiovascular) compared to the other time periods. After adjustment for demographics and comorbidities, the rate ratios for hospitalizations due to HF and other cardiovascular conditions were similar, whereas higher rate ratios were observed for non-cardiovascular hospitalizations for all time periods (Table 5).
TABLE 4.
Frequency and Ratesa of Type of Hospitalizations by Time Period after Incident Heart Failure
| 0–30 Days | 31–182 Days | 183–365 Days | 366–730 Days | |
|---|---|---|---|---|
| Total number of people alive/at risk | 1972 | 1879 | 1699 | 1601 |
| Total number of hospitalizations | 495 | 923 | 818 | 1259 |
| Number (%) by Type of Hospitalization | ||||
| Heart failure | 82 (16.6) | 131 (14.2) | 93 (11.4) | 134 (10.6) |
| Other cardiovascular | 158 (31.9) | 213 (23.1) | 192 (23.5) | 270 (21.5) |
| Non-cardiovascular | 255 (51.5) | 579 (62.7) | 533 (65.1) | 855 (67.9) |
| Rates by Type of Hospitalization | ||||
| Heart failure | 0.55 | 0.18 | 0.11 | 0.10 |
| Other cardiovascular | 1.08 | 0.29 | 0.23 | 0.19 |
| Non-cardiovascular | 1.65 | 0.84 | 0.70 | 0.66 |
Rates per person-year. Rates are adjusted for age and sex.
TABLE 5.
Rates Ratiosa (95% CI) of Types of Hospitalizations by Time Period after Incident Heart Failure
| 0–30 Days | 31–182 Days | 183–365 Days | 366–730 Days | |
|---|---|---|---|---|
| Type of Hospitalization | ||||
| Heart failure | 1.00 (ref) | 0.34 (0.25–0.45) | 0.21 (0.15–0.30) | 0.18 (0.13–0.25) |
| Other cardiovascular | 1.00 (ref) | 0.27 (0.21–0.33) | 0.21 (0.17–0.27) | 0.17 (0.14–0.22) |
| Non-cardiovascular | 1.00 (ref) | 0.51 (0.43–0.59) | 0.43 (0.36–0.50) | 0.41 (0.35–0.48) |
Rate ratios are adjusted for age, sex, body mass index, hypertension, diabetes, prior myocardial infarction, chronic pulmonary disease, cerebrovascular disease, peripheral vascular disease, renal disease, liver disease, hemiplegia, metastatic and nonmetastatic cancers (excluding nonmelanoma skin cancers), estimated glomerular filtration rate, and smoking.
DISCUSSION
This contemporary community study of patients with incident HF described the burden and timing of hospitalizations occurring over the 2 years following the diagnosis of HF. We found that the rates of hospitalization were highest during the first 30 days and much lower thereafter and did not differ by sex, type of HF (preserved vs. reduced EF) or presentation (inpatient vs. outpatient). Patients with myocardial infarction, chronic obstructive pulmonary disease, cancer, and dementia, as well as those diagnosed with HF as inpatients and who had long hospital stays (>5 days) had an increased risk of being hospitalized within 30 days. While the proportions of hospitalizations due to HF or other cardiovascular causes were highest during the first 30 days, more than half of all hospitalizations were due to non-cardiovascular causes and few were due to HF.
Hospitalizations in Patients with Heart Failure
Patients with HF are experiencing frequent hospitalizations causing a major burden on patients and care systems. While contemporary data on the epidemiology of HF are scarce, data from more than a decade ago indicate that the incidence of HF remained largely stable over time.13,20,21 In addition, these older data indicate increasing HF incidence among older persons,13,20,22 gradually displacing the burden of the HF syndrome toward older individuals. Furthermore, improvement in survival13,20,22 has increased the number of elderly survivors with prevalent HF who are candidates for recurrent hospitalizations.
Contemporary community data from Olmsted County, MN suggest an overall decline in HF incidence between 2000 and 2010 with a change in the case mix toward an increasing proportion of HF patients with preserved EF in recent years.7 A decline over time in HF-specific hospitalization rates among Medicare beneficiaries has also been observed, although patients with HF treated in the outpatient setting were not captured.23,24 Nevertheless, evidence suggests the frequency of all-cause hospitalizations in patients with HF has not declined over time,25 but the shift in case mix toward increasing proportions of patients with preserved EF has resulted in an increase in hospitalizations for non-cardiovascular causes.7 This information, in combination with the observations that HF patients with preserved EF have a higher burden of comorbidities than those with reduced EF,26,27 and most hospitalizations in patients with HF are not attributed to HF,12 suggests that the HF syndrome is characterized by an epidemic of hospitalizations.
Timing of Hospitalizations after Heart Failure
While there is convincing evidence that patients with HF are experiencing an epidemic of hospitalizations, previous studies assessing whether this burden of hospitalizations differs according to the timing after HF diagnosis have limitations. Indeed, restriction to only hospitalized HF patients, including both incident and prevalent cases, capturing only cardiovascular hospitalizations, and counting only the first hospitalization occurring over follow-up all substantially limit inference. Among Medicare patients, within the first 30 days after a HF hospitalization, readmissions were common, the majority occurred within the first 15 days (median of 12 days), and the minority were due to HF (35%).5 In addition, the overall pattern of diagnoses responsible for readmission did not differ over time or by patient demographics.5 Similarly, we observed a median time to 30-day readmission of 9 days, and no differences in the burden of hospitalizations by sex. However, we found a markedly lower proportion of 30-day hospitalizations attributed to HF (17%), which may reflect differences in the patient populations, or ascertainment relying on clinical data rather than claims data. Our study identified patients at the time of incident HF diagnosis, including all patients (those diagnosed as inpatients and outpatients) and captured all hospitalizations after HF diagnosis, whereas the aforementioned study excluded outpatients and captured only the first rehospitalization within 30 days.
Another study among Medicare beneficiaries with a hospitalization for HF were followed up to 1 year until the first hospitalization for any cause, reporting the highest rates of readmission early on with continued reduction in the rates over time for the first year.4 A study utilizing a large commercial insurance database, Optum Laboratories, followed patients with incident HF (inpatients or outpatients) for 1 year for all hospitalizations, reporting the highest rates of hospitalizations within the first 30 days and 13% of hospitalizations within the first year being due to HF.6 In the Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study with Tolvaptan (EVEREST) program, the majority of hospitalizations over a median of 9.9 months of follow-up were due to cardiovascular causes, with 46% due to HF; however, this study only enrolled patients hospitalized with worsening HF and EF ≤40%, which likely explains the much higher proportion of hospitalizations due to HF observed in this study.28 Finally, patients hospitalized for HF and enrolled in phase 1 of the Enhanced Feedback For Effective Cardiac Treatment (EFFECT) study were followed over their lifetime, revealing 2 periods of increased hospitalizations: within the first and last decile of survival duration, which given the median survival of 1.8 years corresponds roughly to the first 2 months after hospital discharge and the last 2 months before death.3 Our study followed incident HF patients for 2 years after their first diagnosis of HF (not restricted to hospitalized HF), and we similarly observed differences over time in the rates of hospitalizations with an increased vulnerability for hospitalizations during the first 30 days after the diagnosis of HF. We also found that the rates of hospitalizations over time did not differ by type of HF (preserved vs. reduced EF). Similar to the Optum study, we also observed that 13% of all hospitalizations occurring over the 2-year follow-up were due to HF; however, our study identified a higher proportion (17%) of HF-specific hospitalizations during the first 30 days after the diagnosis of HF. Nevertheless, we observed that a very small proportion of hospitalizations were due to HF and 63% were due to non-cardiovascular causes.
Since the majority of hospitalizations ocurring in HF patients are due to non-cardiovascular causes, increased focus on management of non-cardiovascular conditions in HF may help reduce the rates of hospitalizaiton in these patients. Within the first 30 days after diagnosis of HF, we identified few predictors of rehospitalization, with prior myocardial infarction being the only cardiovascular comorbidity that was predictive of being hospitalized within 30 days. The remaining predictors were non-cardiovascular conditions, including chronic obstructive pulmonary disease, cancer, and dementia. Not surprisingly, patients initially diagnosed with HF as inpatients and who had long hospital stays were also at an increased risk of rehospitalization within 30 days. Taken collectively, our findings highlight the importance of identifying more comprehensive interventions for patients with HF to reduce the burden of hospitalizations in these patients.
Clinical Implications
One-third of HF patients are hospitalized within 30 days of diagnosis, with similar rates across HF types (preserved vs. reduced EF) and presentation (diagnosed as an inpatient vs. outpatient). Importantly, the minority of re-hospitalizations are due to HF, with nearly 2/3 due to non-cardiovascular causes. Thus, screening and aggressive management of comorbidities should be routine in these patients. Indeed, interventions targeting comorbidities in patients with HF may be more effective at preventing hospitalizations than HF-specific interventions. Furthermore, as patients diagnosed with HF as outpatients are at a similar risk of hospitalization as those who present as inpatients, interventions to reduce hospitalizations should not focus soley on hospitalized patients but should be targeted at all HF patients.
Limitations and Strengths
The following limitations should be taken into consideration when interpreting the study results. Some hospitalizations occurring outside of Olmsted County may have been missed; however, we expect any missing hospitalizations to have been minimal since Olmsted County is relatively isolated and the majority of health care for residents is provided by the few medical centers within the county. Although we used only the principal discharge diagnosis code to classify the types of hospitalization, some misclassification for the types of hospitalization may have occurred due to coding practices or inaccuracies in assigning codes.
Our study also has several strengths. In particular, we have captured the experience of community HF patients, including those diagnosed as inpatients and outpatients, without restriction on type of HF (preserved or reduced EF), age, or insurance status or Medicare enrollment. Furthermore, all hospitalizations occurring over a long follow-up (2 years) were included, providing a more comprehensive description of the burden of hospitalizations over the course of the HF syndrome.
Conclusions
Patients with HF experience a large burden of hospitalizations. The rates of hospitalizations are highest within the first 30 days after diagnosis and the majority of hospitalizations are due to non-cardiovascular causes. Because a minority of hospitalizations are due to HF, employing integrated interventions, including improved management of comorbid conditions, will be more effective at reducing hospitalizations than interventions focused solely on HF.
Supplementary Material
Acknowledgments
Funding: This study was supported by the National Institutes of Health (R01 HL120859, R21 AG045228, and R01 AG034676), and the Mayo Clinic CTSA through grant number UL1 TR000135 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health. The funding sources played no role in the design, conduct, or reporting of this study.
We thank Susan Stotz, RN, and Deborah Strain for their study support.
ABBREVIATIONS
- EF
ejection fraction
- HF
heart failure
- LVEF
left ventricular ejection fraction
Footnotes
Disclosures: Dr. Chamberlain reports grants from the National Institutes of Health, grants from the National Center for Advancing Translational Sciences, during the conduct of the study and is a co-investigator on the Rochester Epidemiology Project (R01 AG034676). Dr. Roger reports grants from the National Institutes of Health, and grants from the National Center for Advancing Translational Sciences during the conduct of the study. All other authors have nothing to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Heidenreich PA, Albert NM, Allen LA, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6(3):606–619. doi: 10.1161/HHF.0b013e318291329a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics--2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chun S, Tu JV, Wijeysundera HC, et al. Lifetime analysis of hospitalizations and survival of patients newly admitted with heart failure. Circulation. Heart failure. 2012;5(4):414–421. doi: 10.1161/CIRCHEARTFAILURE.111.964791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dharmarajan K, Hsieh AF, Kulkarni VT, et al. Trajectories of risk after hospitalization for heart failure, acute myocardial infarction, or pneumonia: retrospective cohort study. BMJ. 2015:350h411. doi: 10.1136/bmj.h411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355–363. doi: 10.1001/jama.2012.216476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sangaralingham LR, Shah ND, Yao X, Roger VL, Dunlay SM. Incidence and early outcomes of heart failure in commercially insured and Medicare Advantage patients, 2006 to 2014. Circ Cardiovasc Qual Outcomes. 2016;9(3):332–337. doi: 10.1161/CIRCOUTCOMES.116.002653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gerber Y, Weston SA, Redfield MM, et al. A contemporary appraisal of the heart failure epidemic in Olmsted County, Minnesota, 2000 to 2010. JAMA Intern Med. 2015;175(6):996–1004. doi: 10.1001/jamainternmed.2015.0924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rocca WA, Yawn BP, St Sauver JL, Grossardt BR, Melton LJ., 3rd History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clin Proc. 2012;87(12):1202–1213. doi: 10.1016/j.mayocp.2012.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.St Sauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LJ, 3rd, Rocca WA. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc. 2012;87(2):151–160. doi: 10.1016/j.mayocp.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.StSauver JL, Grossardt BR, Yawn BP, Melton LJ, Rocca WA. Use of a medical records linkage system to enumerate a dynamic population over time: the Rochester Epidemiology Project. Am J Epidemiol. 2011;173(9):1059–1068. doi: 10.1093/aje/kwq482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.StSauver JL, Grossardt BR, Yawn BP, et al. Data resource profile: the Rochester Epidemiology Project (REP) medical records-linkage system. Int J Epidemiol. 2012;41(6):1614–1624. doi: 10.1093/ije/dys195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dunlay SM, Redfield MM, Weston SA, et al. Hospitalizations after heart failure diagnosis a community perspective. J Am Coll Cardiol. 2009;54(18):1695–1702. doi: 10.1016/j.jacc.2009.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roger VL, Weston SA, Redfield MM, et al. Trends in heart failure incidence and survival in a community-based population. JAMA. 2004;292(3):344–350. doi: 10.1001/jama.292.3.344. [DOI] [PubMed] [Google Scholar]
- 14.Ho KK, Anderson KM, Kannel WB, Grossman W, Levy D. Survival after the onset of congestive heart failure in Framingham Heart Study subjects. Circulation. 1993;88(1):107–115. doi: 10.1161/01.cir.88.1.107. [DOI] [PubMed] [Google Scholar]
- 15.Roger VL, Weston SA, Gerber Y, et al. Trends in incidence, severity, and outcome of hospitalized myocardial infarction. Circulation. 2010;121(7):863–869. doi: 10.1161/CIRCULATIONAHA.109.897249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 17.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 18.Levey AS, Coresh J, Greene T, et al. Using standardized serum creatinine values in the Modification of Diet in Renal Disease Study equation for estimating glomerular filtration rate. Ann Intern Med. 2006;145(4):247–254. doi: 10.7326/0003-4819-145-4-200608150-00004. [DOI] [PubMed] [Google Scholar]
- 19.Yturralde RF, Gaasch WH. Diagnostic criteria for diastolic heart failure. Prog Cardiovasc Dis. 2005;47(5):314–319. doi: 10.1016/j.pcad.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 20.Levy D, Kenchaiah S, Larson MG, et al. Long-term trends in the incidence of and survival with heart failure. N Engl J Med. 2002;347(18):1397–1402. doi: 10.1056/NEJMoa020265. [DOI] [PubMed] [Google Scholar]
- 21.McCullough PA, Philbin EF, Spertus JA, Kaatz S, Sandberg KR, Weaver WD. Confirmation of a heart failure epidemic: findings from the Resource Utilization Among Congestive Heart Failure (REACH) study. J Am Coll Cardiol. 2002;39(1):60–69. doi: 10.1016/s0735-1097(01)01700-4. [DOI] [PubMed] [Google Scholar]
- 22.Barker WH, Mullooly JP, Getchell W. Changing incidence and survival for heart failure in a well-defined older population, 1970–1974 and 1990–1994. Circulation. 2006;113(6):799–805. doi: 10.1161/CIRCULATIONAHA.104.492033. [DOI] [PubMed] [Google Scholar]
- 23.Chen J, Normand SL, Wang Y, Krumholz HM. National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries, 1998–2008. JAMA. 2011;306(15):1669–1678. doi: 10.1001/jama.2011.1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Krumholz HM, Normand SL, Wang Y. Trends in hospitalizations and outcomes for acute cardiovascular disease and stroke, 1999–2011. Circulation. 2014;130(12):966–975. doi: 10.1161/CIRCULATIONAHA.113.007787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ross JS, Chen J, Lin Z, et al. Recent national trends in readmission rates after heart failure hospitalization. Circ Heart Fail. 2010;3(1):97–103. doi: 10.1161/CIRCHEARTFAILURE.109.885210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chamberlain AM, St Sauver JL, Gerber Y, et al. Multimorbidity in heart failure: a community perspective. Am J Med. 2015;128(1):38–45. doi: 10.1016/j.amjmed.2014.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fonarow GC, Stough WG, Abraham WT, et al. Characteristics, treatments, and outcomes of patients with preserved systolic function hospitalized for heart failure: a report from the OPTIMIZE-HF Registry. J Am Coll Cardiol. 2007;50(8):768–777. doi: 10.1016/j.jacc.2007.04.064. [DOI] [PubMed] [Google Scholar]
- 28.O'Connor CM, Miller AB, Blair JE, et al. Causes of death and rehospitalization in patients hospitalized with worsening heart failure and reduced left ventricular ejection fraction: results from Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study with Tolvaptan (EVEREST) program. Am Heart J. 2010;159(5):841–849. e841. doi: 10.1016/j.ahj.2010.02.023. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.